Summary Statement
Simulation in multiple contexts over the course of a 10-week period served as a core learning strategy to orient experienced clinicians before opening a large new urban freestanding emergency department. To ensure technical and procedural skills of all team members, who would provide care without on-site recourse to specialty backup, we designed a comprehensive interprofessional curriculum to verify and regularize a wide range of competencies and best practices for all clinicians. Formulated under the rubric of systems integration, simulation activities aimed to instill a shared culture of patient safety among the entire cohort of 43 experienced emergency physicians, physician assistants, nurses, and patient technicians, most newly hired to the health system, who had never before worked together. Methods throughout the preoperational term included predominantly hands-on skills review, high-fidelity simulation, and simulation with standardized patients. We also used simulation during instruction in disaster preparedness, sexual assault forensics, and community outreach. Our program culminated with 2 days of in-situ simulation deployed in simultaneous and overlapping timeframes to challenge system response capabilities, resilience, and flexibility; this work revealed latent safety threats, lapses in communication, issues of intake procedure and patient flow, and the persistence of inapt or inapplicable mental models in responding to clinical emergencies.
Key Words: Emergency medicine; Systems integration; Freestanding emergency departments; New healthcare facilities; Health care quality improvement, Latent safety threats; Patient flow; Patient safety, standardized patient simulation, safety management; Disaster preparedness, sexual assault forensics; Community outreach; Cadaveric tissue; Curriculum development; Patient satisfaction; Employee engagement
Freestanding emergency departments (FEDs) represent a significant trend in providing health care to underserved populations in the United States.1,2 In most cases open 24/7 365 days a year, FEDs (sometimes referred to as satellite EDs or freestanding satellite EDs3) are distinct from urgent care centers, which are often privately owned, exclusively treat conditions of low to moderate acuity, and keep office hours.4 In general, board-certified emergency physicians and nurses staff FEDs, which are fully equipped and provide on-site laboratory and imaging services, receive patients by ambulance, and evaluate and treat or transfer to full-service facilities. In the United States, the Centers for Medicare and Medicaid Services recognized FEDs in 2004 (42 Certified First Responders §§ 482.1 through 482.57) and clarified issues of state certification in 2008 (Directive S&C-08-08)5; most states have issued guidelines or some form of regulation.6 With few exceptions, FEDs meet requirements set out in the federal Emergency Medical Treatment and Active Labor Act.7
We report on extensive and intensive use of simulation as an integral part of a strategic training plan to ensure patient safety and patient-centric care before opening a large urban full-service FED associated with an established tertiary hospital that forms part of a large nonprofit health system. For a facility to be staffed with experienced clinicians, we used simulation to assess and assure competencies, enable and promote teamwork, validate protocols, detect latent safety threats (LSTs), and optimize patient flow. Conceived during the FED planning stages and foreseen as a major component of the curriculum throughout the training period, this multimodal use of simulation represented a systems integration approach to patient safety, consonant with accreditation of Northwell Health (formerly North Shore-LIJ) in that domain by the Society for Simulation in Healthcare (SSH).8 As an aspect of systems engineering and outgrowth of human factors engineering, systems integration is specifically suited to deploying simulation in the design and operation of new facilities.9
With respect to in situ simulation, the culminating component of our program, we note that emergency departments, pediatric units, and obstetrics/perinatal facilities have reported on a decade and more of its use in pilot studies and research-based efforts to improve teamwork, refine organization of supplies and procedures, detect LSTs, and address knowledge and performance gaps.10–12 Simulation research includes several recent efforts to evaluate patient safety in wholly new units and facilities,13,14 including one report of a prospective pilot investigation that used both high fidelity and in situ simulation before opening a pediatric satellite emergency department associated with a children's hospital.15
To the best of our knowledge, ours is the first report on the systematic use of simulation in an onboarding and orientation curriculum before opening an FED.
Background and Demographics
Demographic trends in healthcare, and economic and market forces, help explain the recent proliferation of FEDS. One survey counted 80 FEDs operating in 2007 (1.6% of all US EDs)1; subsequently, the American Hospital Association reported 222 in 2009, 191 of which were hospital affiliated or “satellite” units16; more recently, the New York State Department of Health found more than 400 in 45 states.2 However, as Simon et al recently observed, research involving FEDS has yet to yield a precise definition.17 When they first opened in the 1960s and until the 21st century, FEDs were located in rural and outer-ring suburban areas18; only recently have facilities opened, and not always successfully, in urban settings.6 Increasing numbers of FEDs also reflect an effort to address in-hospital emergency room overcrowding, an issue of importance for clinical outcomes.19–21
In the case at hand, repeated bankruptcies of a tertiary hospital in New York City culminated in its definitive closing, leaving a unique neighborhood in the borough of Manhattan underserved and creating a prolonged “surrogate medical surge event” for nearby hospitals.22,23 A new full-service facility did not prove economically feasible, but needs assessment indicated that an FED could offer a solution, providing emergency and nonemergency care on a full-service basis, intake 24/7, serve as a 911 facility, and coordinating transfer of patients requiring inpatient or a higher level of care.
Lenox Health-Greenwich Village (LH-GV), as the FED would be known, was to be established as a division of Lenox Hill Hospital, a 652-bed facility located on Manhattan's Upper East Side. Modeling projected it could expect to receive more than 30,000 emergency patients annually by its third year of operation.
Demography influences the planning, design, and hiring of personnel of FEDs, and also affects decisions concerning the use of simulation. Greenwich Village in New York City, the densely populated central neighborhood for the catchment area, is home to a diverse set of ethnic groups, local cultures, and a wide range of income groups. To help overcome both doubts of the public at large and a heterogeneous group of vocal residents who complained of loss of their historic tertiary hospital, the new facility would provide a full-service community healthcare “front door.” It would offer subspecialty care and ambulatory surgical care in addition to laboratory and advanced imaging services; but it would not aim to compete with neighborhood primary care providers.
Physical Design
In line with recent FEDs, the design called for 4 functional zones: intake, treatment, clinical support, and administration.24,25 In addition, various features addressed the need for operational flexibility.26 The plan provided for 26 patient rooms, 24 of which were to be fully equipped for emergency use, including 2 dedicated resuscitation units; in addition, 2 rooms for behavioral health patients would be purposely bare of equipment. The open, glass-faced rooms surround a core work area of computer-equipped provider and administrative stations that offer unobstructed sight lines without office partitions. Each room is sufficiently large and equipped to accept 2 patients in case of crowded conditions or disaster service. LH-GV was designed to facilitate direct-to-room triage with registration at bedside; a traditional waiting room was to be used only when the facility operated at capacity.27,28 In addition, a separate results-waiting area would enable prompt and comfortable discharge of patients who were not admitted or transferred.
METHODS
Systems Integration
The Patient Safety Institute (PSI) at Northwell Health (formerly North Shore-LIJ) provides an organizational structure for creating simulation activities that execute the strategic and concrete goals of the entire health system. The Patient Safety Institute operates as a division of the system's corporate university, the Center for Learning and Innovation (CLI), which among other goals evaluates expansion projects and develops macroinstitutional solutions on a systems and human factors engineering basis, with a view to implementing programs that meet pedagogic and clinical aims, enhance patient safety, and maximize effectiveness and efficiency across the entire range of clinical activities.29,30
Such a strategy operated with respect to LH-GV. Whereas under construction, CLI/PSI personnel, in collaboration with the facility's leadership, offered input concerning the design elements previous described, continued to consult through planning stages, and eventually embedded a learning strategy within a comprehensive curriculum that aligned with federal and state-sanctioned requirements for FEDs and the institutional standards for establishing it within a unique urban community. This global approach significantly shaped prospective health care delivery operations and clinical practice, and included extensive use of simulation.
Simulation activities as part of a blended learning program before opening an FED have a clear fit both with emergency medicine and the broader issue of patient safety. Concerted use of simulation is becoming well established in emergency medicine, with specially devised curricula, based on an accepted model of clinical practice now standard for residents in training.31–33 In addition, the nature and extent of hazards associated with opening a new FED may be extrapolated from several studies conducted with new emergency medicine and obstetrics facilities over the past decade.14,15,34 Studies and initiatives such as these support the orchestration of both high-fidelity and immersive “in situ” simulation to expose LSTs, including issues with team communications, systems protocols, patient flow, and electronic record keeping.13
Specific considerations with respect to the new FED also shaped the curriculum. The relatively large size of the standalone facility, together with projected volume and pace of patient reception, called for an extensive learning program to ensure operational competency from the day it opened. The newly hired clinicians had neither worked together before nor been employed by the same health system. Although LH-GV leadership evaluated candidate clinicians for education and experience, the details of individual competencies could not be known nor expected to be uniform across the entire group. Diverse backgrounds and work histories created challenges for orientation.
Structural Goals and Clinical Aims
Hiring decisions, unique aspects of design and mission, including the FED's physical location and layout, all provided inputs for the use of simulation in the preopening 10-week curriculum. Just because experienced personnel comprised the medical staff, we envisioned addressing clinical issues with regard to shared mental models, teamwork, and scope of practice across a wide range of emergency procedures and protocols. In addition, LH-GV's location in a densely urban environment where there exist long-standing and well-founded concerns over severe weather-related emergencies,35,36 and terrorism suggested further training objectives.37,38 Cultural diversity and the presence of a substantial lesbian, gay, bisexual, and transgender community were further considerations.39
The Center for Learning and Innovation/PSI, LH-GV, and our health system's emergency services leadership examined the core competencies as delineated in publications of the American College of Emergency Physicians and the Emergency Nurses Association.40–42 These documents may be viewed as complementary: specific supportive roles for nurses augment the detailed procedures outlined for physicians. As a consequence, the curriculum we devised used interprofessional learning throughout; all clinicians working in teams would learn about resources, equipment, workflow patterns, and one another to develop a thorough collective knowledge of FED resources, including transfer capabilities and protocols. Clinicians' ability to perform the whole range of emergency assessments and procedures without benefit of on-site specialty units demanded validation. Team-based simulation with deliberate practice would also promote familiarity with system-specific protocols for both common and infrequent procedures, and for high-risk interventions.
Curriculum Development
A working collaboration among nursing and emergency physician leadership and CLI/PSI detailed the 10-week curriculum, including refresher courses (Table 1). Designed on a modular and chronological basis, it would interface with administrative preparations, including information technology tutorials and vendors' on-site instructions for the use of equipment.
TABLE 1.
Preopening Blended Learning Curriculum for All Clinicians: Modalities and Objectives
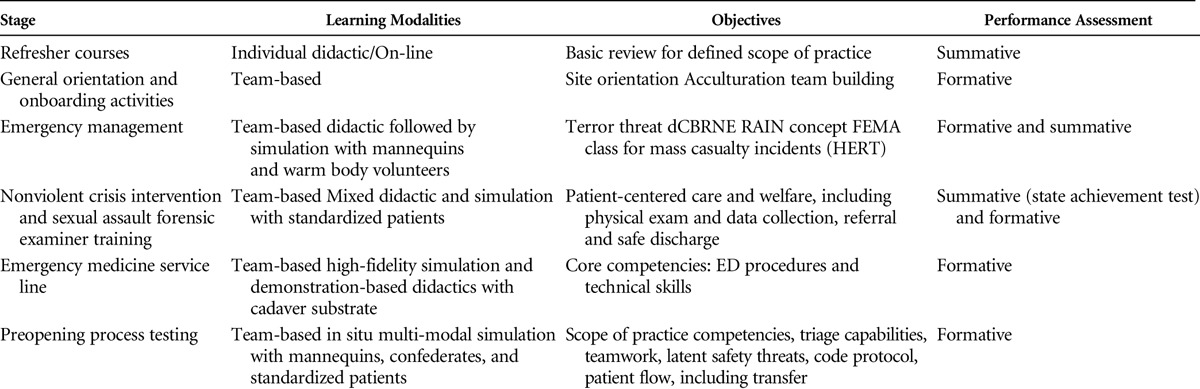
Into this plan, we built a total of 3 weeks of dedicated simulation activities. We planned to use high-fidelity simulation and cadaver-based training, simulation with standardized patients and hybrid scenarios. We also projected 2 days of intensive in situ simulation that would run overlapping scenarios in compressed time frames to effectively stress-test the FED, assumed to be operating at medium capacity. Postsimulation team “debriefing with good judgment” was used throughout the cycle.43
Participants and Teams
The curriculum served the entire complement of 43 clinicians, all but 6 new to the system. Recruited locally and regionally, not preferentially from the Northwell Health (formerly North Shore-LIJ) health system, they were experienced emergency medicine providers. The initial hiring grid called for 10 emergency physicians and physician assistants, 25 nurses, and 8 patient care technicians; additional hires included laboratory and pharmacy personnel and administrative and support staff. As part of the hiring process, we assessed qualifications together with candidates' perceived and documented ability to work in cohesive teams, to operate according to the full scope of practice required for emergency medicine, and to work comfortably with a highly diverse patient population.
Teams of clinicians, which were in all typical cases comprised of a physician, physician assistant, nurse, and patient technician, carried out the simulation activities and debriefings even when the principle focus was to ensure an individual provider's skills through deliberate practice.
Settings
For simulation activities, the curriculum unfolded in 3 venues: (1) the clinical and procedure simulation laboratories of PSI; (2) the cadaver laboratory of the Northwell Health (formerly North Shore-LIJ) Bioskills Education Center; and, for both emergency disaster training and in situ activities, (3) the facilities and treatment rooms at LH-GV.
Onboarding Activities
Our curriculum began with organizational basics associated with human resources initiatives. Socialization activities, recognized as a component of onboarding in health care management, included both team building and orientation activities.44,45 One portion of the program was didactic in nature, did not make use of simulation, and clinicians worked individually:
For physicians, a refresher course based on scope of practice guidelines issued by the American Colleges of Emergency Physicians (ACEP)41
For nurses, a review course offered by the Emergency Nurses Association (ENA)46
For interprofessional teams, other parts of the curriculum addressed technical training in specific topics relevant to the local culture and circumstances:
Sexual assault: all clinicians took the basic 4-hour New York State Sexual Assault Forensic Examiner (SAFE) course,47 with LH-GV certification as a Center of Excellence and individual certification
The proprietary nonviolent crisis intervention program developed by the Crisis Prevention Institute.48
Simulation for Mass Emergency and Disaster Preparedness
Emergency management at Northwell Health (formerly North Shore-LIJ) provided Standardized Awareness Authorized Training (SAAT) for all participants. This program teaches the range of appropriate responses to terrorist incidents, including chemical, biological, radiological, nuclear, and high-yield explosive events.38,49 We augmented this module with Hospital Emergency Response Training for mass casualty incidents, a 3-day course developed by the Federal Emergency Management Agency (FEMA) that includes structured lessons, including simulated scenarios, in response to the presence of chemical, biological, radiological, nuclear, and high-yield explosive CBRNE-associated hazards and materials.50
For Hospital Emergency Response Training, we engaged in 2 days of simulation with level 3 personal protective equipment drills after 1 day of didactic and tabletop instruction. On day 1 of simulation, teams learned how to select and wear level C personal protective equipment, which equips caregivers for airborne emergencies in which substance type and concentration are known values. Equipment includes a full-face air-purifying respirator, chemical-resistant gloves, and disposable chemical-resistant outer boots. Wearing this equipment, teams practiced such procedures as IV insertion and intubation, which are known to require deliberate practice to achieve efficient airway management.51
An 8-hour hybrid simulation took place on day 2. We applied moulage to 10 training mannequins to indicate signs of a chemical attack. Teams were challenged to evaluate, assess, decontaminate, and treat, while communicating appropriate information to one another and to administrators, and arranging for transfer as necessary. With 2 high-fidelity mannequins, we demonstrated such symptoms as pinpoint pupils, diarrhea, nausea, vomiting, and other signs of chemical attack. In addition, we engaged 20 high school students to serve as walking wounded for a scenario in which there was an explosion during a school football game and patients presented for triage at an emergency treatment area. The mannequins themselves were decontaminated, their clothes cut off, and washed. Transfer was arranged and fully carried out, with mannequins transported by ambulance to a nearby tertiary hospital. To track individual patients, we used the New York State Evacuation of Facilities in Disasters System (NYS e-FINDS), a computer-based system inaugurated in 2013 after a major hurricane created a statewide disaster.52
Cadaveric Tissue for Technical Skills Refresher/Training
Although the LH-GV clinicians were all experienced, most were newly hired to the health system, and we needed to ensure competencies for all clinicians across the entire range of procedures they would be expected to carry out. These included (1) both common and infrequent interventions for high-acuity patients, (2) moderate- to high-frequency procedures for specific conditions, and (3) low-frequency but high-risk interventions that carry serious risk for patient harm if performed incorrectly (Table 2). Tabas et al53 note that formal training in such invasive procedures, even for emergency residents, is frequently suboptimal. Related to the importance of validating clinical expertise and experience were health system–specific issues concerning equipment, custom, and approach to various procedures.
TABLE 2.
Technical Skills and Procedural Refresher Training
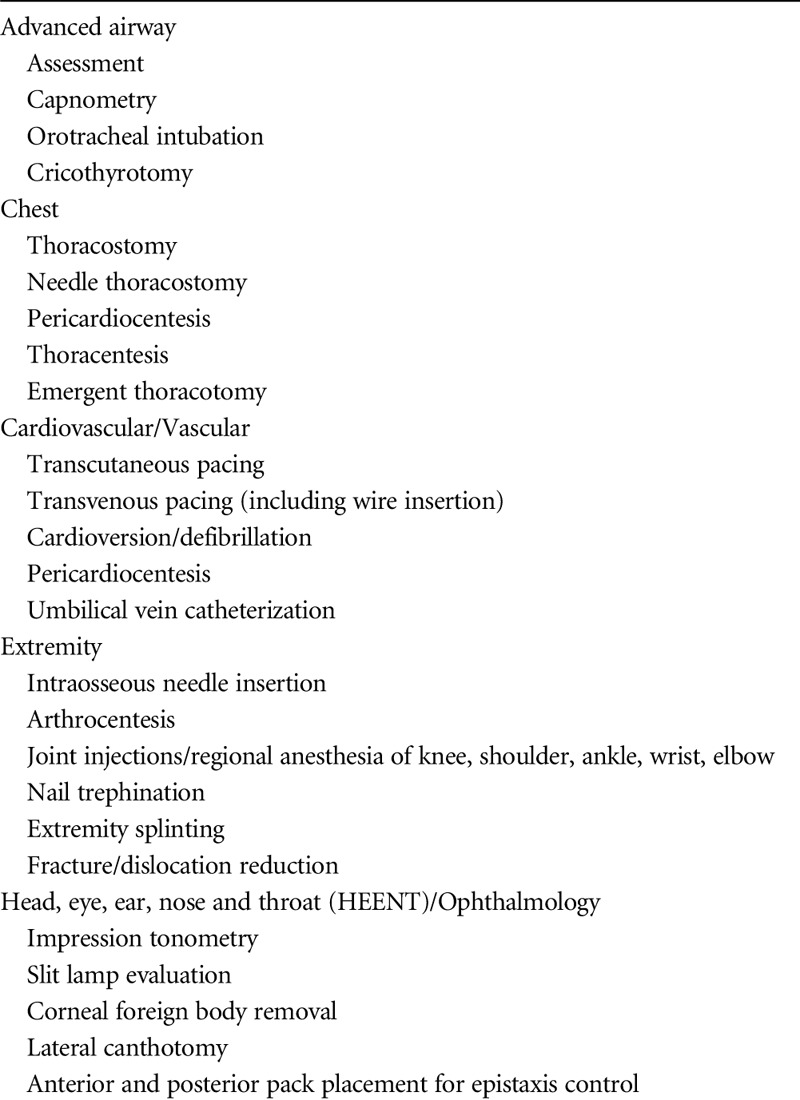
Viewed not as a problem of individualized training and evaluation but as an integral component of the broader mandate to provide interprofessional adult learning before opening LH-GV, we decided on a team approach that used simulation activities, principally with fresh-frozen and unembalmed cadaveric tissue as substrate. In general, for procedure-specific training, such as arthroscopy and other minimally invasive interventions, the use of human cadaver tissue is widely accepted, although it is most frequently used for basic educational purposes.54,55 Although research concerning the comparative effectiveness of this modality in emergency contexts is limited,56,57 it has been described as providing “a high-fidelity model in which the exact anatomical relationships present in live surgical patients are preserved, with almost identical tissue handling and spatial relations to that of live surgery.”58 In simulation, perceptual, psychological, and action fidelity with cadaver tissue may be described as high; mechanical fidelity is less so.59 On balance, based on experience in our own laboratory and on the literature,56 we believed there could be cognitive and kinesthetic advantages to the use of cadaver tissue for a substantial subset of specific emergency procedures.
In our partly didactic approach, teams comprised of physicians, physician assistants, nurses, and patient technicians attended sessions in a laboratory setting. Experienced faculty discussed and demonstrated current techniques for a selection of the emergency and life-saving procedures listed in Table 2, performed in collaboration with the LH-GV emergency medicine physicians. In the laboratory, 5 stations with cadavers served 5 teams, with faculty rotating from station to station, explaining specific details of procedures as performed as Northwell Health (formerly North Shore-LIJ). We modeled this methodology, which did not use scenarios, on our procedural training program for emergency medicine residents,32 adapted to interprofessional use.60 It provided physicians the opportunity to practice specific procedures with current instrumentation, but it also enabled teams to demonstrate the various ancillary tasks while imparting to nurses and patient technicians contextual knowledge, including visual and tactile information.
Preoperational In Situ Simulation
We conducted 2 successive days of in situ simulation 1 month before LH-GV formally opened. Our focus in this phase was on teamwork, communication, and clinical decision making. The entire clinical staff (n = 43) was present and worked and formed STAT teams of 4 to 5 in shifts (2 per day). Facilitated debriefings with good judgment took place after each shift and at the end of each day. Registration and pharmacy personnel also participated, but laboratory staff was not yet hired; we also employed CT and EMS personnel as confederates and, to facilitate one scenario, also made use of distraction to test intake procedures. On day 1, we assigned specific scenarios and roles to 21 standardized patients and employed LH-GV leadership in various observational capacities; on day 2, with fewer standardized patients (SPs) available, LH-GV personnel served as patients in some situations.
Information Gathering and Scenario Development
General plans for the 2-day in situ simulation phase began with PSI visits to the facility, while it was still under construction, to learn about the design and gather suggestive clues about scenarios that might expose LSTs or issues affecting security, patient flow, transfer capabilities, and challenges to communication and responsive teamwork. We intended from the start to simultaneously use high-fidelity simulation, simulation with standardized patients, and mixed or hybrid simulations. The process of adapting and crafting scenarios was based on the request from LH-GV leadership to simulate a full-service FED without hospital backup short of transfer. The director of standardized patients held 2 separate sessions with experienced SPs to assign roles and explain logistics.
Organization
Patient Safety Institute staff (n=6), SPs (n=21) together with a supervisor and staff providers (n=3), and LH-GV leadership (n=3) met with clinician teams at LH-GV for prebriefing on the first full day of in situ simulation; the meeting also included unit clerks, computed tomography technicians, and security personnel. Mannequins and associated equipment had been predelivered and prepared for deployment; so too were related props. SPs were cloistered out of sight and off the clinical floor; from this “backstage” location they could be called upon as needed. One of us (R.K.) served as operations director and worked with high-fidelity simulation technicians and observers to initiate scenarios, to curate their development as needed, and decide when they would conclude.
Scenarios for FED Operations
The Patient Safety Institute possesses a library of scenarios, a number of which could be adapted for in situ use in an FED. We developed new or chose and amended preexisting scenarios to ensure relevance and balance; most included several interrelated objectives with regard to patient load and severity. Case categories included: ambulatory triage patient, EMS triage patient, incumbent patient, and utility role (Table 3). This typology could accommodate the broad range of patients and issues associated with FEDs and emphasize the use of situation, background, assessment, and recommendation as a communications technique to contend with volatility, uncertainty, complexity, ambiguity, and delayed feedback.61
TABLE 3.
In Situ Scenarios
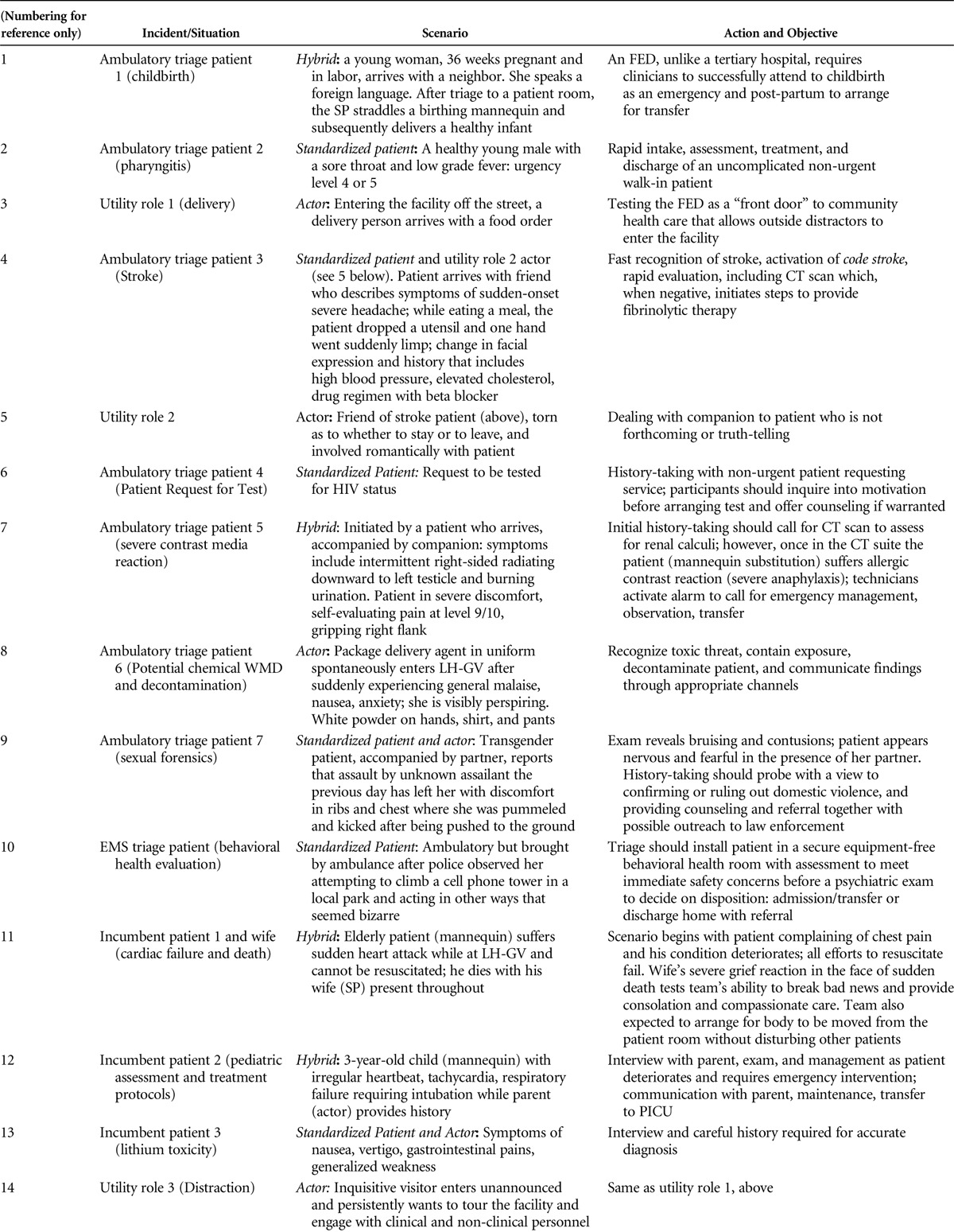
Freestanding EDs should be considered small but complex facilities in which clinicians will be confronted with both straightforward and complex cognitive challenges. As a consequence, we planned to simulate patient loads of varied intensity and severity, and coordinated the play of scenarios so as to implement them on an articulated but improvisational basis: articulated with regard to simulating traffic in an emergency facility on a relatively busy day or night, improvisational because deployment decisions depended on on-the-spot assessments of stress in the system and readiness to receive new patients or situations.
RESULTS
A full-scale research program at a freestanding, fairly large newly constructed emergency facility presents challenges in potential interference with the host of assessment-related activities to which newly hired clinicians are subject. However, we conducted a postonboarding survey 8 months after the facility opened (Table 4), with qualitative questions and a quantitative 5-point Likert scale survey concerning simulation at PSI and the Bioskills Laboratory (team-based training with cadaveric tissue). Sent to 35 participants, we received 10 responses, including 3 from physicians and 5 from nurses, as summarized in Figure 1. Eight of ten responders noted team building as a significant advantage in response to an open-ended question about the learning experience. Responses overall suggest the program met the goals articulated in the blended learning curriculum.
TABLE 4.
Comments About Perceived Value of Simulation in 2 Contexts
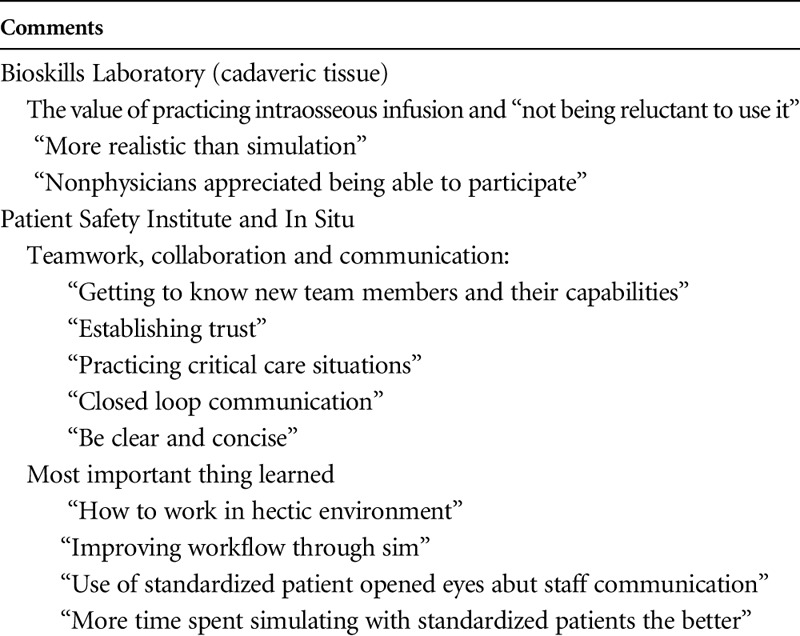
FIGURE 1.
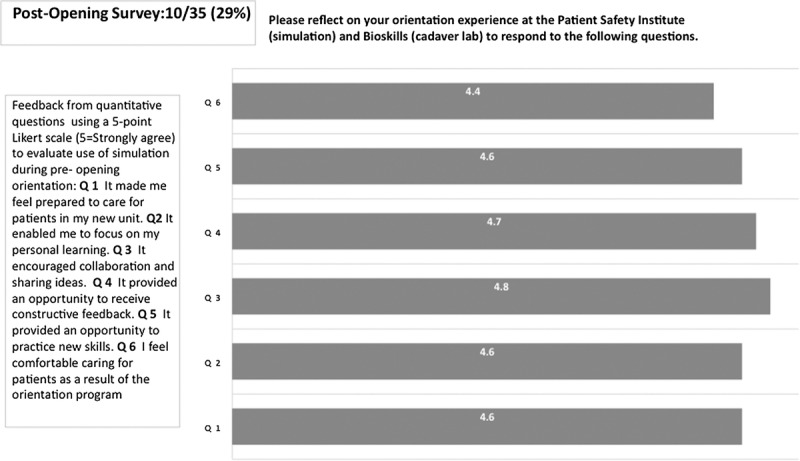
Postopening survey.
Patient Satisfaction and Clinician Engagement
With regard to use and access, LH-GV opened in July 2014 and during the first 6 months received 12,700 patients for an average of 71 per day. Using the 5-point Emergency Severity Index (ESI),62 the accepted triage tool for grading ED visits, the average severity for LH-GV arrivals was 3+. With 47% of arrivals by ambulance (53% as walk-ins), the profile of patients received comports well with the use of emergency rooms nationwide.21 Wait time to see a physician was 13 minutes, more than adequate when compared with 67 minutes for large metro central emergency departments in the most recent US/CDC data set.63 Reliable statistics that compare FEDs with respect to triage and wait times have yet to appear in the literature.
Although patient satisfaction metrics are multifactorial, they play an acknowledged role in emergency medicine, both as an indicator of quality of care and as shaping patient perceptions of the entire associated healthcare system.64 Earliest Press Ganey data indicated high rates of satisfaction (96%–99%) among 270 patients who returned survey requests. Although some portion of satisfaction would likely be attributable to a honeymoon effect of the state-of-the-art environment and reestablishment of a health care facility in the community, we note that recent data from a substantial study indicate that patients do discriminate the quality of clinical care apart from the features of comfortable new surroundings.65
Similarly, employee engagement (EE) represents an additional context for a systems integration approach to curricula design and the use of simulation. Employee engagement, which may be defined as “the emotional commitment of the employee towards the organization”66 affects the non-negligible issues of cost-effectiveness and employee retention as well as patient safety. All-clinician and physician favorability scores in 3 EE-related categories (teamwork, tools and resources, and quality of patient care) ranged from 89% to 100%. These preliminary data with employees new to an organization must also clearly be greeted with caution and the role of simulation cannot be extrapolated from them, but they signal a further avenue for investigation.67,68 Formulated originally through investigation of burnout and studied as a topic in psychology, human resources, adult education, and organizational management, EE is an evolving concept pertinent to the broader success of simulation in the future of health care.69,70
We should note several limitations to our report. The simulation components we incorporated into our curriculum were based on validated methodologies but the need for more rigorous research is widely acknowledged.71,72 In addition, although we tested several tools and technologies during in situ simulations, this activity took place before vendor instructions and demonstrations of new equipment. Similarly, not all supplies were in place. Scheduling did not permit a second round of in situ simulation before opening the facility several weeks later, which might have enabled comparative process revisions.14
DISCUSSION
Application of Systems Integration
Multimodal use of simulation formed a central instrumental component in the design and launch of a curriculum before opening a new FED. This application of a systems integrative approach, a “consistent, planned, collaborative, integrated, and iterative application of sim-based assessment and teaching activities”,9 uses principles of systems engineering and aims to deliver patient-centric care. Both a learning and assessment strategy, simulation in this context helps to identify and resolve issues of safety, efficiency, and effectiveness in ways that optimize outcomes and improve patient satisfaction. Its programs are allied with other instruments that comprise a toolkit derived from human factors and adult and experiential learning theory. In this way, it aims to align with the business goals of the health care organization as a whole, conceived as a complex adaptive system.73–75
Although systems integration is a new concept in health care, it is scarcely without precedent or a historical trajectory that, in fact, coincides with the use of simulation. Henry Plummer, who envisaged becoming an engineer before entering medicine, introduced engineering principles into the functional operations of the Mayo Clinic in the mid-20th century,9,76 and in the 1960s, Avedis Doanabedian described the Structure-Process-Outcome model,77 which in turn formed a basis for the development of the recent Systems Engineering Initiative for Patient Safety (SEIPS).78 The SEIPS model, a research program formulated in response to recommendations in the IOM report To Err Is Human,79 owes explicitly to human factors and ergonomics. In a recent article, Carayon et al note that simulation in anesthesia, initiated in the late 1980s, represented a prior and exceptional use of human factors and ergonomics; its conceptual roots in the aviation industry effectively prefigured and soon explicitly aligned with the contemporary patient safety movement.80
Systems integration requires administrative structure and support. Within our health care system, the simulation facility (PSI) is located within the corporate university (CLI) that serves as a platform for process improvement and employee education. Past instances of the use of systems integration at our institution include development of a new cardiothoracic intensive care unit in a facility previously limited to community care,81 a nurse fellowship program to improve employee retention,82 a long-term comprehensive safety initiative in a regional perinatal center,83 and a systemwide program to reduce sepsis.84 In developing these programs as well as the present one, PSI/CLI operated in a participatory fashion beginning in the planning stages, aided by heightened awareness of simulation among both administrative and clinical personnel.
With respect to LH-GV, throughout the preopening curriculum, we designed simulation activities that operated upon all 6 components described in the revised SEIPS model of the sociotechnical work system: persons (which include teams), tasks, tools and technology, organization, and internal and external environments.85 We used simulation to assess competencies, improve patient flow, evaluate the internal environment, and integrate the use of tools and instruments. Team-based simulation tested FED operations with attention to social context, including community interface, disaster, and transfer capabilities.
Yield From In Situ Simulation
The culminating phase of our curriculum consisted of 2 days (4 shifts) of immersive in situ simulation and debriefing, approximately 3 weeks before opening. Our multipurposed scenarios, deployed in compressed and overlapping timeframes, aimed to “stress the system” in an intensive effort to evaluate team behavior and to identify LSTs and related clinical issues. Our experience with this phase seems to accord with in situ efforts reported in other health systems, including their impact on team actions, attitudes, and behavior.11,14
Patient Flow
The original plan to use direct-to-room triage called for an immediate bedside conference with the patient and the entire team (physician, nurse, physician assistant, patient technician, and registration assistant). During most in situ scenarios, SPs consistently found this approach confusing and at times overwhelming, a potential contributor to patient dissatisfaction. On day 2 of in situ simulation, clinicians themselves (acting as patients) confirmed the impressions from SPs on day 1.
Similarly, protocol for receiving patients by ambulance called for the on-duty security guard to alert clinical staff to arrivals. We suspected that this plan, which might be appropriate for a rural or suburban FED, established an idealized auxiliary role for security that would not have a good fit with real contingencies in the workplace. In fact, this proved to be the case when the security guard was distracted (intentionally) before arrival of an ambulance. Confederates included EMT personnel, who attended the debriefing and described their own reactions and behavior in cases where ambulance reception is inadequate.
Physical Design/Layout
Beginning with our initial inspection of the facility, we also designed scenarios to test safety in relation to the physical layout. Notably, the radiology suite, although equipped with an external flashing alarm, was located in a corridor adjacent to but outside the sight lines of people in the clinical workspace. The ambulatory triage patient in scenario 7 demonstrated this LST when significant time elapsed (after mannequin substitution) for an SP who showed signs and symptoms of an anaphylactic reaction to contrast medium.
Community Access
In providing a “front door” to the local neighborhood, LH-GV is designed for patient comfort and ease of access; these features distinguish FEDs from most hospital-based EDs. However, the inability to control ingress by patients and others, a characteristic virtually unique to emergency settings,86 remains a concern, all the more because its reception-friendly design creates the potential for walk-in individuals to disrupt patient flow while at the same time providing an open door to emergencies of high urgency. We tested both situations. Standardized patients entered as distractors in scenarios 3 and 14; and scenario 8 presented an ambulatory triage patient who arrived “out of the blue” with possible toxic contamination.
Birth and Death
One unique aspect of ED culture is the inevitable occurrence of ultimate but unforeseeable events. In all such cases, lack of customary backup in an FED requires modification of usual ED protocols and the ability to contend with powerfully emotional events that constitute potentially serious or unexpected adverse outcomes. We developed hybrid scenarios to contend with both instances and included clinical, interpersonal, and administrative objectives. Scenario 1 required clinical staff to deliver an infant, provide postpartum care, and arrange for transfer. In scenario 11, an elderly patient died in the presence of his wife. The task of the clinical team included both appropriate measures, first to give cardiopulmonary resuscitation and take all appropriate steps to save the patient's life, then to console the survivor. The team also was required to move the body from the patient room to the morgue without disturbing other patients.
Rule-based Errors
The ED in general (and an FED by extension) may be described as a “natural laboratory for the study of medical error”; and Chisholm and Croskerry86 underscore the potential for compromised safety owing to the pressure of time and unpredictability upon cognitive workload. In addition to revealing LSTs and misaligned communications, as previously described, in situ simulation also indicated clinicians' persistent tendency when under stress to use internal cognitive frames, or mental models, that were once appropriate to their workplace but are no longer applicable. The most striking example was scenario 7, when a clinician misinterpreted the emergency signal from the radiology suite as an indication of code blue and so prematurely began cardiopulmonary resuscitation on a patient “actually” having an anaphylactic reaction. Similarly, in response to stroke symptoms in scenario 4, the initial response was: “We'll send [the patient] up to the neuro ICU.” In scenario 12, the physician initiated patient transfer to the hospital where he had transferred pediatric cases from his previous workplace
Errors of this kind, effectively owing to impaired information processing in a new and acutely stressful environment, should not be surprising, but they represent an area for further investigation. Just as teams in a new facility may need to regularize terminology and language, they can also benefit from focal attention on circumstances surrounding specific cues, code alerts, and transfer capabilities to overcome the persistence of unsuitable mental models.
Resistance
When in situ safety efforts take place, for example, in a pediatric unit during working hours and unannounced in advance, they frequently generate resistance, conveyed by clinicians' exasperation, anger, and reticence.87 In the context of a new pediatric ED, Patterson et al88 also reported performance anxiety and reluctance as substantial challenges for in situ scenarios. We also noted the persistence of what James Reason describes as the “person approach” (as contrasted to a system approach) to clinical error, expressed as apprehension of reproach and blame. Although both leadership and clinicians were in principle fully convinced of the value of simulation, and the facility's STAT teams had worked together for 2 months, we nevertheless encountered fear of potential “embarrassment” both before and during the in situ portion of the curriculum. Our preliminary efforts to allay concern seemed to be only partly successful because initial reactions to the various scenarios included anger, bewilderment, mistrust, and the impression that scenarios were designed to find fault with clinicians. Negative responses during debriefings, relatively simple to conduct because clinicians by that time had experienced weeks of simulation on an almost daily basis, offered an opportunity to address these impressions. We noted improved understanding over time of in situ simulation goals and rationale.
We also encountered a special instance of clinician's anger in response to scenario 11, which culminated in cardiac failure and death and required immediate care for the patient's grieving spouse. Leadership at LH-GV had requested that outcome because death is an inevitable aspect of emergency care, and clinicians may have received minimal exposure to its various ramifications.89 Although it represents a challenge, especially when unexpected and occurring after lengthy efforts to resuscitate, its use was justified with experienced clinicians in a high-acuity context.90 As the scenario played out, the attending physician expressed immediate irritation while nevertheless appropriately resolving its multiple objectives.
At present, there do not exist best practice guidelines for simulated death.91 In immersive simulation, however, we note that purposefully employing a highly trained SP to add realism to such scenes may carry a positive benefit for a clinician's prospective encounters with death and dying.92 (See Video, Supplemental Digital Content).
CONCLUSION
Freestanding EDS represent a growing institutional adaptation in healthcare that is reflective of several broader trends, including efforts to address ED overcrowding and urban hospital closures.93,94 To what extent future opportunities enable randomized controlled studies of simulation used in new FEDs remains to be seen, but the systematic use of simulation to test preparedness ahead of opening a new service line or facility is uncommon, to judge from the existing literature.14,18,95,96
Our experience in providing a simulation-based curriculum and learning strategy offers a basic template for some issues that warrant further investigation. Basic elements seem consonant with those implemented by Adler et al97 when opening a new facility. Simulation programs and personnel should enter the process in the planning stages, see early to crafting useful scenarios, integrate simulation activities into the broader learning strategy, and make every effort to emphasize team building. External constraints (such as delivery of equipment) and changes in scheduling should be expected. Our timeline (Fig. 2) provides a basic outline of activities that foreground simulation activities as they were scheduled within a more complex educational plan.
FIGURE 2.
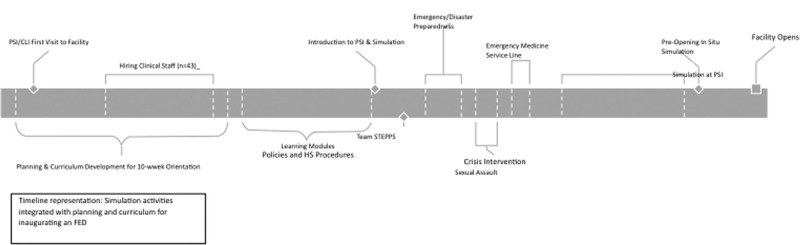
Timeline representation: simulation activities integrated with planning and curriculum for inaugurating an FED.
Simulation deployed in the context of systems integration aims to optimize health care conceived as a complex adaptive system. When applied to a new facility, it validates and improves the performance of providers and teams, and tests issues of preparedness, design, and the organization of the facility itself. Our blended learning curriculum included components designed to (1) test and augment clinicians' preexisting knowledge of specific procedures, (2) impart new knowledge concerning specific protocols such as sexual forensics and mass casualty incidents, (3) orient clinicians to operations in a new facility of a type with which none were previously familiar, and (4) enhance teamwork and team building.
ACKNOWLEDGMENTS
The team at the Patient Safety Institute and Center for Innovative Learning (PSI/CLI) thank the staff at LH-GV for their cooperation and participation in the simulation activities described in this article. We are grateful to Eric Cruzen, MD, Director, Emergency Medicine at LH-GV and Jennifer Siller, MSN, NP, Nursing Director, for invaluable assistance and expertise in developing the preopening curriculum; our thanks extend to executive director Alex Hellinger, Jeffrey Kraut, MBA, at Northwell Health (formerly North Shore-LIJ), Jane Wickey, director of clinical skills at PSI/CLI, and Carleigh Gustafson, RN BSN.
Footnotes
The authors declare no conflict of interest.
REFERENCES
- 1.Sullivan AF, Bachireddy C, Steptoe AP, et al. A profile of freestanding emergency departments in the United States, 2007. J Emerg Med 2012;43:1175–1180. [DOI] [PubMed] [Google Scholar]
- 2.New York State Department of Health. Free Standing Emergency Departments, New York: 2013. [Google Scholar]
- 3.Emergency Medicine Practice Committee. Freestanding Emergency Departments: American College of Emergency Physicians; Irving, Texas: 2013. [Google Scholar]
- 4.Libassi P. A new front door. Expanding the hospital's reach with freestanding EDs. Health Facil Manage 2013;26:28–33. [PubMed] [Google Scholar]
- 5.CMS S&C Memo 08–08. Requirements for Provider-based Off-campus Emergency Departments and Hospitals that Specialize in the Provision of Emergency Services. January 11, 2008, 2008. [Google Scholar]
- 6.Williams M, Pfeffer M. Freestanding Emergency Departments: Do They Have a Role in California? 2009. [Google Scholar]
- 7.Rosenbaum S. The enduring role of the Emergency Medical Treatment and Active Labor Act. Health Aff (Millwood) 2013;32:2075–2081. [DOI] [PubMed] [Google Scholar]
- 8.Society for Simulation in Healthcare. SIM Center Directory.
- 9.Dunn W, Maxworthy J, Gallo K, et al. Systems integration. In: Levine A DSJ, Schwartz AD, Sim AJ, eds. The Comprehensive Textbook of Healthcare Simulation. New York: Springer; 2013:95–110. [Google Scholar]
- 10.Gardner AK, Ahmed RA, George RL, et al. In situ simulation to assess workplace attitudes and effectiveness in a new facility. Simul Healthc 2013;8:351–358. [DOI] [PubMed] [Google Scholar]
- 11.Miller KK, Riley W, Davis S, et al. In situ simulation: a method of experiential learning to promote safety and team behavior. J Perinat Neonatal Nurs 2008;22:105–113. [DOI] [PubMed] [Google Scholar]
- 12.Small SD, Wuerz RC, Simon R, et al. Demonstration of high-fidelity simulation team training for emergency medicine. Acad Emerg Med 1999;6:312–323. [DOI] [PubMed] [Google Scholar]
- 13.Bender GJ. In situ simulation for systems testing in newly constructed perinatal facilities. Semin Perinatol 2011;35:80–83. [DOI] [PubMed] [Google Scholar]
- 14.Ventre KM, Barry JS, Davis D, et al. Using in situ simulation to evaluate operational readiness of a children's hospital-based obstetrics unit. Simul Healthc 2014;9:102–111. [DOI] [PubMed] [Google Scholar]
- 15.Geis GL, Pio B, Pendergrass TL, et al. Simulation to assess the safety of new healthcare teams and new facilities. Simul Healthc 2011;6:125–133. [DOI] [PubMed] [Google Scholar]
- 16.Simon EL, Griffin PL, Jouriles NJ. The impact of two freestanding emergency departments on a tertiary care center. J Emerg Med 2012;43:1127–1131. [DOI] [PubMed] [Google Scholar]
- 17.Simon EL, Medepalli K, Williams CJ, et al. Freestanding emergency departments and the trauma patient. J Emerg Med 2015;48:152–157. [DOI] [PubMed] [Google Scholar]
- 18.Fulks C, McFarlin S, Stolley JM. Start a freestanding emergency center. Nurs Manage 2000;31:41–42. [PubMed] [Google Scholar]
- 19.Bernstein SL, Aronsky D, Duseja R, et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med 2009;16:1–10. [DOI] [PubMed] [Google Scholar]
- 20.Hsia RY, Kellermann AL, Shen YC. Factors associated with closures of emergency departments in the United States. JAMA 2011;305:1978–1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Institute of Medicine. Hospital-Based Emergency Care: At the Breaking Point. Washington, DC: The National Academies Press, 2007. [Google Scholar]
- 22.Romero D, Kwan A, Swearingen J, et al. Impact of the closure of a large urban medical center: a qualitative assessment (part I). J Community Health 2012;37:982–994. [DOI] [PubMed] [Google Scholar]
- 23.Adalja AA, Watson M, Wollner S, et al. Response to the sudden closure of St. Vincent's Hospital: learning from a real, no-notice, prolonged surge event. Biosecur Bioterror 2011;9:153–161. [DOI] [PubMed] [Google Scholar]
- 24.Sayah A, Rogers L, Devarajan K, et al. Minimizing ED waiting times and improving patient flow and experience of care. Emerg Med Int 2014;2014:981472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nestor C. Community developments. Essentials of freestanding emergency centers. Health Facil Manage 2008;21:23–27. [PubMed] [Google Scholar]
- 26.Ward MJ, Ferrand YB, Laker LF, et al. The nature and necessity of operational flexibility in the emergency department. Ann Emerg Med 2014;65:156–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bertoty DA, Kuszajewski ML, Marsh EE. Direct-to-room: one department's approach to improving ED throughput. J Emerg Nurs 2007;33:26–30 quiz 93. [DOI] [PubMed] [Google Scholar]
- 28.Scrofine S, Fitzsimons V. Emergency department throughput: strategies for success. J Nurs Adm 2014;44:375–377. [DOI] [PubMed] [Google Scholar]
- 29.Simmons JG. Launching PSI: establishing a culture of patient safety. In: Gallo KG, Smith LG, eds. Building a Culture of Patient Safety Through Simulation. New York: Springer; 2014:13–28. [Google Scholar]
- 30.Gallo KG, Smith LG. Patient safety and simulation: present and future. In: Gallo KG, Smith LG, eds. Building a Culture of Patient Safety. New York: Springer; 2014:3–12. [Google Scholar]
- 31.Binstadt ES, Walls RM, White BA, et al. A comprehensive medical simulation education curriculum for emergency medicine residents. Ann Emerg Med 2007;49:495–504, 504.e1–11. [DOI] [PubMed] [Google Scholar]
- 32.Cassara M, Kerner R, Drozd A. Creating high-fidelity and hybrid simulations for residents. In: Gallo KG, Smith LG, eds. Building a Culture of Patient Safety Through Simulation. New York: Springer; 2014:79–99. [Google Scholar]
- 33.Bloch SA, Bloch AJ. Simulation training based on observation with minimal participation improves paediatric emergency medicine knowledge, skills and confidence. Emerg Med J 2015;32:195–202. [DOI] [PubMed] [Google Scholar]
- 34.Kobayashi L, Shapiro MJ, Sucov A, et al. Portable advanced medical simulation for new emergency department testing and orientation. Acad Emerg Med 2006;13:691–695. [DOI] [PubMed] [Google Scholar]
- 35.Lien C, Raimo J, Abramowitz J, et al. Community healthcare delivery post-Hurricane Sandy: lessons from a mobile health unit. J Community Health 2014;39:599–605. [DOI] [PubMed] [Google Scholar]
- 36.Teperman S. Hurricane Sandy and the greater New York health care system. J Trauma Acute Care Surg 2013;74:1401–1410. [DOI] [PubMed] [Google Scholar]
- 37.Boscarino JA, Adams RE, Figley CR, et al. Fear of terrorism and preparedness in New York City 2 years after the attacks: implications for disaster planning and research. J Public Health Manag Pract 2006;12:505–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Perry RW, Lindell MK. Hospital planning for weapons of mass destruction incidents. J Postgrad Med 2006;52:116–120. [PubMed] [Google Scholar]
- 39.Moll J, Krieger P, Moreno-Walton L, et al. The prevalence of lesbian, gay, bisexual, and transgender health education and training in emergency medicine residency programs: what do we know? Acad Emerg Med 2014;21:608–611. [DOI] [PubMed] [Google Scholar]
- 40.Hockberger RS, Binder LS, Graber MA, et al. The model of the clinical practice of emergency medicine. Ann Emerg Med 2001;37:745–770. [DOI] [PubMed] [Google Scholar]
- 41.Hockberger RS, Binder LS, Chisholm CD, et al. The model of the clinical practice of emergency medicine: a 2-year update. Ann Emerg Med 45:659–674. [DOI] [PubMed] [Google Scholar]
- 42.Emergency Nurses Association (ENA) Emergency nursing scope of practice. J Emerg Nurs 1989;15:361–364. [PubMed] [Google Scholar]
- 43.Rudolph JW, Simon R, Dufresne RL, et al. There's no such thing as "nonjudgmental" debriefing: a theory and method for debriefing with good judgment. Simul Healthc 2006;1:49–55. [DOI] [PubMed] [Google Scholar]
- 44.Lynch K, Buckner-Hayden G. Reducing the new employee learning curve to improve productivity. J Healthc Risk Manag 2010;29:22–28. [DOI] [PubMed] [Google Scholar]
- 45.Rollag K, Parise S, Cross R. Getting new hires up to speed quickly. MIT Sloan Manager Rev 2005;26:35–41. [Google Scholar]
- 46.Jordan KS. Emergency Nursing Core Curriculum. 6th ed Philadelphia, PA: Saunders; 2008. [Google Scholar]
- 47.New York State Department of Health. Sexual Assault Forensic Examiner (SAFE) Program Available at: www.health.ny.gov/professionals/safe. Accessed July 1, 2016.
- 48.Calabro K, Mackey TA, Williams S. Evaluation of training designed to prevent and manage patient violence. Issues Ment Health Nurs 2002;23:3–15. [DOI] [PubMed] [Google Scholar]
- 49.Hsu EB, Jenckes MW, Catlett CL, et al. Effectiveness of hospital staff mass-casualty incident training methods: a systematic literature review. Prehosp Disaster Med 2004;19:191–199. [DOI] [PubMed] [Google Scholar]
- 50.FEMA. Hospital Emergency Response Training for Mass Casualty Incidents. Available at: https://cdp.dhs.gov/training/courses/HERT. Accessed July 1, 2016.
- 51.Castle N, Pillay Y, Spencer N. Comparison of six different intubation aids for use while wearing CBRN-PPE: a manikin study. Resuscitation 2011;82:1548–1552. [DOI] [PubMed] [Google Scholar]
- 52.Redlener I, Reilly MJ. Lessons from Sandy—preparing health systems for future disasters. N Engl J Med 2012;367:2269–2271. [DOI] [PubMed] [Google Scholar]
- 53.Tabas JA, Rosenson J, Price DD, et al. A comprehensive, unembalmed cadaver-based course in advanced emergency procedures for medical students. Acad Emerg Med 2005;12:782–785. [DOI] [PubMed] [Google Scholar]
- 54.Madan SS, Pai DR. Role of simulation in arthroscopy training. Simul Healthc 2014;9:127–135 10.1097/SIH.0b013e3182a86165. [DOI] [PubMed] [Google Scholar]
- 55.Blaschko SD, Brooks HM, Dhuy SM, et al. Coordinated multiple cadaver use for minimally invasive surgical training. Jsls 2007;11:403–407. [PMC free article] [PubMed] [Google Scholar]
- 56.Lineberry M, Walwanis M, Reni J. Comparative research on training simulators in emergency medicine: a methodological review. Simul Healthc 2013;8:253–261. [DOI] [PubMed] [Google Scholar]
- 57.Hall AB. Randomized objective comparison of live tissue training versus simulators for emergency procedures. Am Surg 2011;77:561–565. [DOI] [PubMed] [Google Scholar]
- 58.Thomas MP. The role of simulation in the development of technical competence during surgical training: a literature review. International Journal of Medical Education 2013;4:48–58. [Google Scholar]
- 59.Khan K, Tolhurst-Cleaver S, White S, et al. Simulation in Healthcare Education: Building a Simulation Program, a Practical Guide. Association for Medical Education in Europe: Dundee, UK; 2011. [Google Scholar]
- 60.Watters C, Reedy G, Ross A, et al. Does interprofessional simulation increase self-efficacy: a comparative study. BMJ Open 2015;5:e005472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Satish U, Streufert S. Value of a cognitive simulation in medicine: towards optimizing decision making performance of healthcare personnel. Qual Saf Health Care 2002;11:163–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gilboy NTT, Travers D, Rosenau AM. Emergency Severity Index (ESI): A Triage Tool for Emergency Department Care, Version 4. Implementation Handbook. Rockville, MD: Agency for Healthcare Research and Quality; 2012:2011. [Google Scholar]
- 63.National Center for Health Statistics. Health, United States. 2012: With special feature on emergency care. Hyattsville, MD, 2013. [PubMed] [Google Scholar]
- 64.Trout A, Magnusson AR, Hedges JR. Patient satisfaction investigations and the emergency department: what does the literature say? Acad Emerg Med 2000;7:695–709. [DOI] [PubMed] [Google Scholar]
- 65.Siddiqui ZK, Zuccarelli R, Durkin N, et al. Changes in patient satisfaction related to hospital renovation: experience with a new clinical building. J Hosp Med 2015;10:165–171. [DOI] [PubMed] [Google Scholar]
- 66.Jeve YB, Oppenheimer C, Konje J. Employee engagement within the NHS: a cross-sectional study. Int J Health Policy Manag 2015;4:85–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Boswell WR, Shipp AJ, Payne SC, et al. Changes in newcomer job satisfaction over time: examining the pattern of honeymoons and hangovers. J Appl Psychol 2009;94:844–858. [DOI] [PubMed] [Google Scholar]
- 68.Lowe G. How employee engagement matters for hospital performance. Healthc Q 2012;15:29–39. [DOI] [PubMed] [Google Scholar]
- 69.Gaba DM. The future vision of simulation in health care. Qual Saf Health Care 2004;13(Suppl 1):i2–i10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Halm B. Employee engagement: a prescription for organizational transformation. Adv Health Care Manag 2011;10:77–96. [DOI] [PubMed] [Google Scholar]
- 71.McGaghie WC, Issenberg SB, Petrusa ER, et al. A critical review of simulation-based medical education research: 2003–2009. Med Educ 2010;44:50–63. [DOI] [PubMed] [Google Scholar]
- 72.Dieckmann P, Phero JC, Issenberg SB, et al. The First Research Consensus Summit of the Society for Simulation In Healthcare: conduction and a synthesis of the results. Simul Healthc 2011;6:S1–S9. [DOI] [PubMed] [Google Scholar]
- 73.Karsh BT, Holden RJ, Alper SJ, et al. A human factors engineering paradigm for patient safety: designing to support the performance of the healthcare professional. Qual Saf Health Care 2006;15(Suppl 1):i59–i65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Building a Better Delivery System: A New Engineering/Health Care Partnership. Reid P, Compton W, Grossman J, Fanjiaj G, Eds. The National Academies Press: Washington, DC, 2005. [PubMed] [Google Scholar]
- 75.Begun JW, Zimmerman B, Dooley K. Health care organizations as complex adaptive systems. In: Mick SE, Wyttenback M, eds. Advances in Health Care Organization Theory. San Francisco, CA: Jossey-Bass; 2003:253–288. [Google Scholar]
- 76.McConahey WM, Pady DS. Henry Stanley Plummer. Endocrinology 1991;129:2271–2273. [DOI] [PubMed] [Google Scholar]
- 77.Donabedian A. The quality of care. How can it be assessed? 1988. Arch Pathol Lab Med 1997;121:1145–1150. [PubMed] [Google Scholar]
- 78.Carayon P, Schoofs Hundt A, Karsh BT, et al. Work system design for patient safety: the SEIPS model. Qual Saf Health Care 2006;15(Suppl 1):i50–i58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kohn LT, Corrigan J, Donaldson MS. To err is human: building a safer health system. Washington, D.C.: National Academy Press, 2000. [PubMed] [Google Scholar]
- 80.Carayon P, Wetterneck TB, Rivera-Rodriguez AJ, et al. Human factors systems approach to healthcare quality and patient safety. Appl Ergon 2014;45:14–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hartman A, Bello S, Rojas K, et al. Safety from the outset: creating an interprofessional team in a cardiothoracic intensive care unit. In: Gallo KG, Smith LG, eds. Building a Culture of Patient Safety Through Simulation. New York: Springer; 2014. [Google Scholar]
- 82.Friedman MI, Cooper AH, Click E, et al. Specialized new graduate RN critical care orientation: retention and financial impact. Nurs Econ 2011;29:7–14. [PubMed] [Google Scholar]
- 83.Kaufman L, Fleisher A, Friedman M, et al. Essential maneuvers: simulation as part of a long-term comprehensive perinatal safety initiative. In: Gallo KaS L, ed. Building a Culture of Patient Safety Through Simulation. NY: Springer; 2014. [Google Scholar]
- 84.Friedman MI, Doerfler M, Tamuz M. Safety hub: research and role of a simulation center in a system-wide initiative to reduce sepsis. In: Gallo KG, Smith LG, eds. Building a Culture of Patient Safety Through Simulation. NY: Springer; 2014:45–52. [Google Scholar]
- 85.Holden RJ, Carayon P, Gurses AP, et al. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics 2013;56:1669–1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chisholm CD, Croskerry P. Crticial processes in the emergency department. In: Croskerry P, Cosby KS, Schenkel SM, Wear R, eds. Patient Safety in Emergency Medicine. Philiadelphia, PA: Wolters Kluwer; 2009:89–95. [Google Scholar]
- 87.Gangadharan SR. Pediatric emergencies: targeted programs and crafted scenarios. In: Gallo KG, Smith LG, eds. Building a Culture of Patient Safety Through Simulation. New York: Springer; 2015:115–125. [Google Scholar]
- 88.Patterson MD, Geis GL, Falcone RA, et al. In situ simulation: detection of safety threats and teamwork training in a high risk emergency department. BMJ Qual Saf 2013;22:468–477. [DOI] [PubMed] [Google Scholar]
- 89.Shoenberger JM, Yeghiazarian S, Rios C, et al. Death notification in the emergency department: survivors and physicians. West J Emerg Med 2013;14:181–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Gaba DM. Simulations that are challenging to the psyche of participants: how much should we worry and about what? Simul Healthc 2013;8:4–7. [DOI] [PubMed] [Google Scholar]
- 91.Corvetto MA, Taekman JM. To die or not to die? A review of simulated death. Simul Healthc 2013;8:8–12. [DOI] [PubMed] [Google Scholar]
- 92.Szauter K. Adding the human dimension to simulation scenarios. Simul Healthc 2014;9:79–80. [DOI] [PubMed] [Google Scholar]
- 93.Garg N, Husk G, Nguyen T, et al. Hospital Closure and Insights into Patient Dispersion: The Closure of Saint Vincent's Catholic Medical Center in New York City. Appl Clin Inform 2015;6:185–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Pitts SR, Pines JM, Handrigan MT, et al. National trends in emergency department occupancy, 2001 to 2008: effect of inpatient admissions versus emergency department practice intensity. Ann Emerg Med 2012;60:679–686.e3. [DOI] [PubMed] [Google Scholar]
- 95.Scott J. Introducing a freestanding emergency department. Radiol Manage 2012;34:41–42. [PubMed] [Google Scholar]
- 96.Zuckerman A. Are Freestanding Emergency Centers an Idea Whose Time Has Come? Healthc Financ Manage. 2007;61:114–116. [PubMed] [Google Scholar]
- 97.Adler MD, Mobley BL, Eppich WJ, et al. Use of simulation to test systems and prepare staff for a new hospital transition. J Patient Saf 2015. [DOI] [PubMed] [Google Scholar]


