Abstract
Psychiatric genetic counseling (PGC) is an emerging specialty discipline within the genetic counseling profession. A specialist PGC service was founded in 2012 in Vancouver, Canada, and though patient benefits have been demonstrated, many physicians do not regularly refer patients to the service despite awareness of its availability. We conducted a qualitative study involving semi-structured telephone interviews with Vancouver-based physicians who were aware of the PGC service to explore this phenomenon. Interviews were audio-recorded, transcribed verbatim, coded, and analysed for emergent themes. Consistent with a grounded theory approach, constant comparison was employed throughout data collection and analysis. Analyses of interviews conducted with 12 physicians revealed that referral practices were informed by perceptions about the purpose of PGC and interpretation of patient cues. Physicians perceived PGC as an information-focused intervention, and considered referral when patients explicitly expressed desire for information about recurrence risk or etiology that they feel unable to adequately address themselves. Even when physicians identified psychotherapeutic benefits of PGC, patient needs of this nature were not perceived as cues prompting referral to PGC. These data suggest that further work is necessary to position PGC in physicians’ minds as a service that could potentially benefit most individuals with psychiatric disorders and their families, and that encompasses more than information provision. It is important to increase physicians’ awareness of the complementary role that genetic counselors can play to that of the physician in providing psychotherapeutically oriented counselling about illness etiology.
Keywords: Psychiatric genetic counseling, psychiatry, genetic counseling, referral practices
Introduction
Over recent years there has been increasing emphasis on integrating genetics into all aspects of healthcare (Austin and Honer, 2007; Brand et al., 2008; Hudson, 2011). However, questions remain about how to integrate genomic medicine into clinical practice, such that patients reap the greatest possible benefits from increased understanding about the role of genetics in the conditions they live with or for which they are at risk. Many commentators have suggested that perhaps the optimal strategy for effective integration of genomics into all aspects of healthcare is to develop interdisciplinary collaborations between genetic counselors and physicians, including those engaged in family practice as well as specialists (Omenn, 2000; Greendale and Pyeritz, 2001; Guttmacher et al., 2001; Erskine et al., 2013; Austin et al., 2014).
Psychiatric disorders are complex conditions resulting from a combination of both genetic and environmental factors (Vogel, 1991). Psychiatrists recognize the need to incorporate genetics into psychiatric practice (Finn et al., 2005; Hoop et al., 2008), but many lack expertise and/or confidence in this area (Finn et al., 2005; Abbate et al., 2014). Given growing evidence indicating that people with psychiatric disorders and their families would like to receive genetic counseling (DeLisi and Bertisch, 2006; Lyus, 2007; Austin and Honer, 2008; Peay et al., 2009), psychiatry is an area of practice that potentially presents an ideal scenario for fruitful interdisciplinary collaboration between physicians and genetic counselors (Thompson et al 2015). Indeed, clear benefits have been demonstrated for individuals who have received genetic counseling for psychiatric illnesses, including improved understanding of causes of mental illness, reduced concern about other relatives becoming affected, and feeling more hopeful, in control, better able to cope and help, and reduced anxiety, self-blame and guilt (Austin and Honer, 2008; Costain et al., 2012, 2014; Inglis et al., 2014).
The world’s first specialist service providing psychiatric genetic counseling (PGC) service of its kind was established in 2012 in Vancouver, British Columbia to provide genetic counseling to individuals with mental illness and their family members. A naturalistic study of patient outcomes after being seen in the clinic showed statistically significant increases in empowerment among individuals with mental illness and their families, and increased self-efficacy among individuals with mental illness (Inglis et al., 2014).
Through a large number of presentations and grand rounds were conducted to raise awareness of the clinic among local physicians, and to highlight the service and the benefits of PGC for patients, strikingly, the large majority (76%) of patients who accessed the PGC service during its first year were self-referred (Inglis et al., 2014). This raised the question about how physicians make decisions about when to refer patients to the PGC clinic.
The purpose of this qualitative study was to explore the factors that determine physicians’ decisions about referring to PGC. Understanding the process through which physicians make decisions about referrals to genetic counseling is crucial to improving interdisciplinary collaboration and increasing the number of patients who are able to benefit from genetic counseling services.
Materials and Methods
Design
Given the limited knowledge about how physicians decide to refer to genetic counselling, we decided that a qualitative approach would be most informative for developing a rich and deep understanding of the issue (McAllister, 2001). More specifically, we opted to be guided and informed by grounded theory, which is ideally suited for exploring processes (e.g. decision making)(Strauss and Corbin, 1998). The study was approved by the University of British Columbia Ethics Review Board (H13-03175).
Recruitment and procedure overview
British Columbia (BC)-based physicians were eligible to participate if they had: a) referred at leastone patient to the PGC clinic in the past, or b) received a consult report from the PGC clinic together with an information package about the service after an appointment for a patient who self-referred, or c) explicitly expressed intent to refer patients to PGC after learning about it (e.g. at a grand rounds presentation) but had not regularly referred their patients to the service. Eligible participants were contacted by mail with a package including an introductory letter explaining the reason for contact, a consent form, and a $5 gift card. Two weeks later, participants were contacted by telephone and/or email to discuss the study and to schedule an interview time, if they expressed interest in participating. Following completion of the interview described below, participants were sent a follow-up package by mail with an additional $5 gift card.
Interviews
After obtaining verbal consent, a semi-structured telephone interview was conducted with each participant, consisting of broad, open-ended questions designed to address the two areas described above (see supplemental information for interview guide), and topic-specific prompts to further explore responses. All interviews were conducted by a genetic counseling graduate student (E.L.L) who had no prior relationship with the participants, and who was not a member of the PGC service delivery team. The interview guide was revised during data collection to reflect emerging preliminary results to optimize further data collection. Demographic information (age, biological sex, location, and length of practice) and number of referrals made to PGC were self-reported by participants at the beginning of the interview. Interview recordings were transcribed verbatim, then the transcripts were checked for accuracy and de-identified prior to analysis.
Analysis
First, we performed open coding of the transcripts as they were gathered, that is, transcripts were examined and, line-by-line, specific concepts were given codes. Initial emergent themes were identified, and relationships between them explored. Throughout analysis of all transcripts, we used the constant comparative method, in which data were continuously compared and contrasted both within and between transcripts (Charmaz, 2006; Braun and Clarke, 2008). Any outlying or new concepts that emerged were used to revisit and revise the initial coding scheme. All transcripts were coded by E.L.L. and a subset was coded independently by E.M. and all discrepancies were discussed and resolved. Recruitment continued until saturation of primary themes was achieved; that is, we reached a point where collection of new data did not reveal any new insights into the major concepts we had identified. Through examining the relationships between the major concepts, a conceptual framework representing criteria that physicians apply to decide which patients to refer for PGC was developed.
Results
Participants
Participants were recruited between September, 2014 and March, 2015. Thirty-seven initial contact packages were mailed to eligible physicians, and interviews (each of 15–30 minutes) were conducted with 12 physicians (for demographic information, see Table 1). Participants were classified as ‘rare referrers’ if they reported having referred less than five patients, or ‘frequent referrers’ if they had referred five or more patients.
Table 1.
Demographic data of 12 participants who participated in interviews about their perceptions of PGC.
| Demographic factor | n | % |
|---|---|---|
|
| ||
| Biological sex | ||
| Male | 7 | 58% |
| Female | 5 | 42% |
|
| ||
| Ethnicity | ||
| Caucasian | 6 | 50% |
| Other | 6 | 50% |
|
| ||
| Location | ||
| Vancouver | 10 | 83% |
| Greater-Vancouver Area | 1 | 8% |
| Interior BC | 1 | 8% |
|
| ||
| Area of medical practice | ||
| Psychiatry | 10 | 83% |
| Family medicine | 2 | 17% |
|
| ||
| Referral behavior | ||
| Frequent referrer (≥5 referrals) | 3 | 25% |
| Rare referrer (<5 referrals) | 9 | 75% |
|
| ||
| Mean | Range | |
|
| ||
| Age | 46.2 | 34–61 |
|
| ||
| Years of practice | 13.8 | 1–35 |
Ten participants had initially learned about the PGC service directly from members of the PGC team, either through a presentation, (e.g. grand rounds), or having met members of the clinic personally. Two participants had heard about the service through other means, one through an information package they received via the mail and the other found the service through an internet search.
Overview of the conceptual framework describing how physicians make referrals to PGC
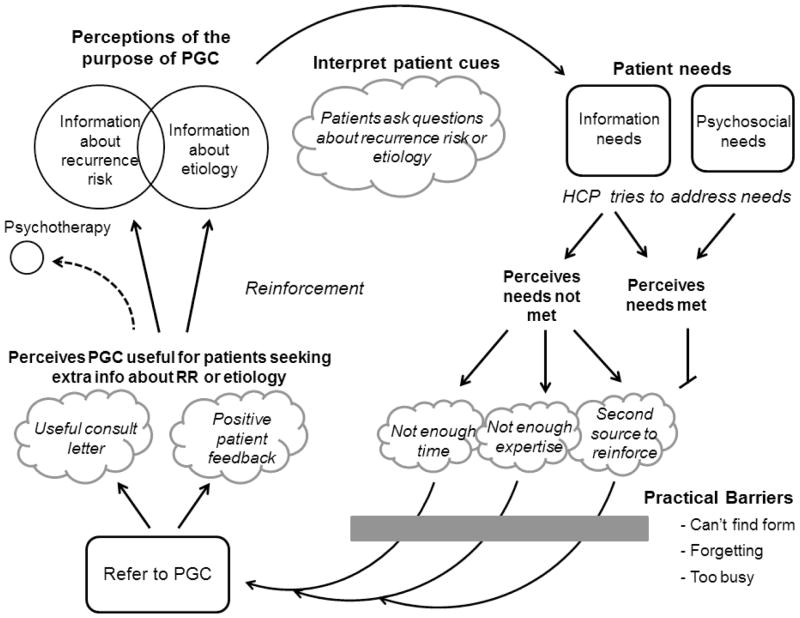
The criteria that physicians use to determine which patients to refer for PGC are defined by the way in which they conceptualize the purpose, process, and benefits of PGC (Figure 1). Specifically, physicians’ behavior in referring to PGC is compelled by what seem to be deeply-rooted perceptions of genetic counseling as a primarily or exclusively information focused service. Physicians tend to consider referring patients after they explicitly articulate relevant informational needs that the physician themself feels personally unable to adequately meet. The key components of this framework are described and illustrated (in Figure 1) in more detail below.
Figure 1.
Decision-making framework to illustrate how physicians decide whether or not to refer a patient for PGC.
Themes
Physicians perceived PGC to be primarily about information provision
Physicians identified recurrence risk, and etiology of mental illness as the most important areas where they felt PGC could provide patients with information.
“To help you with when parents ask for, or when patients ask about, ‘What’s the possibility of my kid transmitting this schizophrenia gene?’ so to speak, and you read the literature, it’s not quite clear.” - Participant 4, rare referrer
“Parents might want to know the course or might want to understand why their child developed this mental illness or might have their own kind of etiological explanation that …that may be, you know, biased and would benefit from further exploration.” - Participant 9, rare referrer
Patient cues drive referral for PGC
Patient cues emerged as a key component of physicians’ decision-making process about making referrals to PGC. Consistent with participants’ perceptions of PGC as an information-focused intervention, cues from patients indicating that they were seeking genetics-related information, such as specific questions about recurrence risk or patients expressing misconceptions about the causes of mental illness, were important precursors to PGC referral. For example:
“If they seem to have limited understanding about illness or that kind of thing […] or if I feel like they can benefit from some extra education.” - Participant 2, frequent referrer
Patient emotions (e.g., guilt, helplessness, or worry) were occasionally interpreted as cues for the provider to consider a possible referral to PGC, but usually only when directly connected to a gap in patient knowledge, for example:
“The patient has to have some fear and it’s usually about, ‘Will I be able to be a parent?’ or ‘Is my baby going to be affected?’” - Participant 3, frequent referrer
More often, physicians regarded patient emotions about cause of illness or chances for children to develop psychiatric problems not as primary indicators for referral in themselves, but as issues that may be addressed as a secondary consequence of the information provided in genetic counseling.
“I thought this patient would benefit from education, and, I know there was some family history in his case, and I thought it would just kind of maybe put things in context to help him cope better.” - Participant 12, rare referrer
For some providers, patient cues were exquisitely important, and had to be very specific in order for a referral to PGC to be considered. Some providers voiced discomfort with discussing the service with their patients, if they had not explicitly asked:
Participant 3, frequent referrer: “…if the patients sort of ask for it…”
Interviewer: “So you feel more comfortable if the patient initiated the conversation?”
Participant 3: “Personally, yes, yeah.”
Relatedly, some participants reported actively seeking out specific cues regarding patients’ potential needs that they thought might benefit from a referral to PGC. The nature of the questions participants asked in their assessment of needs was strongly driven by their perceptions of PGC being an information-focused, risk communication-based intervention. For example:
“I do a few screening questions for people in reproductive years. I inquire about their plans for becoming parents and whether they have any concerns about their children experiencing the condition.” - Participant 11, rare referrer
“They have to actually express their concerns about how their mental illness would affect their ability to be parents or how their mental illness may- you know, are their kids at risk. I don’t think of the clinic as the first option unless patients actually specifically talk about that.” - Participant 3, frequent referrer
Some physicians also reported asking about the patient’s family history, because a “strongly genetic” family history was considered a cue for referral to PGC.
“I would think individuals where they have an illness that has a strong genetic component, individuals that have a strong family history of some kind of psychiatric condition.” - Participant 7, rare referrer
“One of the patients that I referred had a parent and a sibling. So, like two first degree relatives with schizophrenia, and was obviously concerned about risks for her children.” - Participant 1, rare referrer
Participants considered patients emotional needs associated with their mental illness, such as feelings of guilt or self-stigma, however, the physician would typically attempt to address the emotional needs themselves rather than initiating a referral to PGC.
“As a psychiatrist, some of the stuff about causes of mental illness and stigma and things like that, hopefully we can help discuss and address with the patient […] I think that’s something that we would have some expertise in as well.” - Participant 1, rare referrer
PGC referral considered after physician’s own attempt to address the patient’s needs
Once the presence of a patient’s information-based needs was established, the physicians typically reported attempting to address the need themselves.
“I would do some preliminary sort of education around, ‘Yes, the child is at an increased risk’.” - Participant 3, frequent referrer
When physicians identified cues indicating a patient need for information related to recurrence risk or etiology, many participants reported that they would provide counseling on these topics themselves. When patient informational needs were determined to be adequately met by the provider, a referral to PGC is no longer considered.
“If there was a family history, I think I wouldn’t refer a patient like that because I could deal with it myself.” - Participant 12, rare referrer
When physicians considered that their patient’s information-based need had not been adequately met by their own efforts, they considered the possibility of referral to PGC. Physicians articulated several reasons for which they may feel that their patient’s needs were not satisfied by their own efforts:
-
The physician did not have enough time.
“We as psychiatrists don’t have enough time to look at the background, don’t have the time to address the concerns of parents, do not have time to address the guilt issues with parents and relatives” - Participant 4, rare referrer -
The physician felt they lacked the expertise to address the need.
“Obviously the profession involves some expertise that I don’t have, you know, in more advanced genetics.” - Participant 8, frequent referrer“If a family was wanting more information above and beyond that or had more specific questions, then that’s when I would think about referring them.” - Participant 9, rare referrer -
The physician sought another provider to reinforce their message about etiology, and methods to protect mental health.
“We know that you guys will be on our team for reinforcing certain messages that we are trying to give.” - Participant 2, frequent referrer
Practical barriers to making a referral to PGC
When a physician had decided that a referral to PGC may be a useful option for a particular patient, logistical barriers became relevant, such as difficulty locating and completing a referral form, forgetting, or being too busy.
“Our problem here is time and it’s just forms that need to be filled out and we need to give the patients any information, it’s easier for us if we can just hand them a paper and say, ‘Oh, this is a great clinic and if you are interested, call there.” - Participant 3, frequent referrer
The impact of feedback from PGC on subsequent referrals
Participants expressed that they perceived the PGC clinic visit to be useful, either for themselves through receiving a consultation letter, or for the patients through the feedback they received, or both.
“I’ve had a couple of patients that I’ve referred and uh, you know, found it very helpful.” - Participant 1, rare referrer
“They get to ask a bunch of questions that they actually don’t think about asking us. When I see that they were able to disclose some things that they were worried about, which they hadn’t disclosed to us, which is nice.” - Participant 2, frequent referrer
“This adds to the overall quality of service we can offer.” – Participant 3, frequent referrer
Interestingly, some participants identified psychotherapeutic benefits of PGC after a patient attended an appointment, but this did not tend to inform decision making around future referrals. For example, one participant described their perception of the purpose of PGC as follows:
“It’s more than just giving somebody a percentage […] I feel the patients are more empowered after they have the consultation.” - Participant 3, frequent referrer
However, when asked shortly after about when they would consider referring in future, they said:
“If I wanted them to have more definitive percentages, or if I want them to have more information about how to maybe lessen the chance of the child being affected, I would refer.” - Participant 3, frequent referrer
Participants expressed the importance and value of feedback regarding positive patient outcomes of PGC as something that would motivate them to refer in the future.
“We want to know, ‘I’m doing this intervention, did it make a difference?’ I think that’s useful for physicians to know that it’s helpful to patients if we do this.” - Participant 1 rare referrer
“If I’m made more aware of exactly what sort of help the patients and the family can receive then maybe that would influence me to refer more knowing that there’s going to be some value added.” - Participant 6, rare referrer
Discussion
Our data indicate that physicians’ decisions regarding referring patients to PGC are influenced by: their perceptions of PGC as primarily (or even exclusively) being concerned with information-provision; patient cues – particularly the explicit expression of interest in receiving the types of information that the physician associates with genetic counselling; and their sense of whether they have been able to address their patient’s need themselves. Our finding regarding the importance of patients’ explicitly expressed interest is in line with data from previous studies in other settings (Hayflick et al., 1998; Aalfs et al., 2003). However, our data extend previous insights by revealing that physicians in this study were actively seeking out patient cues that would prompt a referral, and that the cues they choose are directly related to their perception of PGC.
The patient cues that physicians reported using to initiate a referral to PGC related primarily to patients explicitly stating their informational needs. It is worth noting that patients may be more able (and therefore likely) to explicitly articulate needs for information than they are able to voice some of the emotional issues, like guilt, shame, stigma, fear, (Ritsher et al., 2003; Dinos et al., 2004; Lannin et al., 2015) with which PGC is ideally placed to help. However, patients’ emotional needs were rarely seen by physicians as primary reasons for referral to PGC, partly because PGC was perceived as an information provision service, but also because participants (who were primarily psychiatrists) – of course correctly – felt that addressing patients’ emotional needs falls within their own scope of practice. Participants’ confidence to address psychosocial needs themselves combined with the belief that PGC is primarily an information-giving service, perhaps, is an explanation for why referrals to PGC to address primarily psychosocial needs appear infrequent.
Physicians’ perceptions of the potential overlap between their own scope of practice and that of the genetic counselor primarily related to educational activities – they saw genetic counselors as a “second source to reinforce” information that they wanted to convey. The awareness of the role that genetic counselors could play as a “second source” for psychotherapeutic support was less obvious. And, while participants acknowledged the psychotherapeutic benefits of PGC after a patient had received these services, going forward, this did not seem to influence their perceptions of which of their patients might benefit from a referral – they seemed to continue to regard PGC as primarily an information-giving service. Perhaps some kind of self-selecting feedback loop is at play - if the majority of a physician’s referrals were related to recurrence risk estimates or discussions about genetic information, then physicians only observed these types of patients benefiting from the service, thus reinforcing their pre-existing perception of only those limited indications as suitable for referral.
While minimizing practical barriers that may impede physicians making referrals to genetic counseling services is undoubtedly important, at least in this study, these issues emerged as having more minor, downstream impact.
Previous literature (Javalgi et al., 1993; Kinchen et al., 2004; Barnett et al., 2012) exploring factors that influence referral practices point to the importance of relationships, and of a physician having previous positive experiences referring to a specific health care provider. These ideas came thought in our study - with participants describing sentiments suggesting that they felt positive about their established relationships with the PGC clinic.
It is important to note that first, although saturation was reached in terms of the primary emergent themes, it is possible that more nuance and depth could be uncovered through interview of a larger number of physicians. Second, it is possible that the scope of practice overlap perceived by physicians who participated in this study (primarily psychiatrists) related to addressing patients’ emotional needs, may not be perceived by physicians in other specialty areas of practice – this may be worthy of future exploration.
Although this study focused on referrals to a psychiatric genetics specialty service, it is plausible that similar issues influence physician’s referrals to other specialties of genetic counseling. Development and implementation of strategies for physician engagement around the full scope of what PGC and the genetic counseling profession as a whole has to offer may help make genetic counseling services accessible to a broader range of patients. It also seems that there is a need for continued communication between genetic counselors and referring physicians to allow for full knowledge of the breadth of issues (emotional as well as informational) addressed through genetic counseling. Increasing physicians’ awareness about the role of genetic counselors beyond simple provision of information is critical, given increasing expectations for physicians across all disciplines to become more comfortable discussing genetics with patients, and the availability of easily accessible print and web-based informational materials.
The theoretical framework described here may be applicable to other specialty areas of genetic counseling and provide insight into how and when physicians decide to make referrals to genetic counseling. These data highlight the need for increased awareness among other health professionals regarding the genetic counselor’s broad skill set, and the psychotherapeutic benefits of genetic counseling, as ultimately, collaboration between genetic counselors and physicians will be crucial in allowing for the effective integration genomics into all aspects of healthcare.
Supplementary Material
Acknowledgments
The authors were grateful to receive funding support for this study through the National Society of Genetic Counselors (NSGC) Research Special Interest Group and the University of British Columbia Genetic Counselling Training Program. Interview transcription was performed by: Mingshu Dong, Vicky Hsieh, and Sarah Gerrard. JA was supported by the Canada Research Chairs program and BC Mental Health and Substance Use Services.
Footnotes
Human Studies and Informed Consent: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). Informed consent was obtained from all individual participants included in the study The study was approved by the University of British Columbia Ethics Review Board (H13-03175).
Conflict of Interest Authors: EL, AI, EM, HW, AL and JA declare that they have no conflict of interest
Animal Studies: No animal studies were carried out by the authors for this article
References
- Aalfs CM, Smets EMA, de Haes HCJM, Leschot NJ. Referral for genetic counselling during pregnancy: Limited alertness and awareness about genetic risk factors among GPs. Fam Pract. 2003;20:135–141. doi: 10.1093/fampra/20.2.135. [DOI] [PubMed] [Google Scholar]
- Abbate KJ, Chung WK, Marder K, Ottman R, Taber KJ, Leu C-S, Appelbaum PS. Psychiatrists’ views of the genetic bases of mental disorders and behavioral traits and their use of genetic tests. J Nerv Ment Dis. 2014;202:530–8. doi: 10.1097/NMD.0000000000000154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin J, Inglis A, Hadjipavlou G. Genetic counseling for common psychiatric disorders: an opportunity for interdisciplinary collaboration. Am J Psychiatry. 2014;171:584–585. doi: 10.1176/appi.ajp.2014.13101421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin JC, Honer WG. Psychiatric genetic counselling for parents of individuals affected with psychotic disorders: A pilot study. Early Interv Psychiatry. 2008;2:80–89. doi: 10.1111/j.1751-7893.2008.00062.x. [DOI] [PubMed] [Google Scholar]
- Austin JC, Honer WG. The genomic era and serious mental illness: a potential application for psychiatric genetic counseling. Psychiatr Serv. 2007;58:254–261. doi: 10.1176/ps.2007.58.2.254. [DOI] [PubMed] [Google Scholar]
- Barnett ML, Keating NL, Christakis NA, O’Malley AJ, Landon BE. Reasons for choice of referral physician among primary care and specialist physicians. J Gen Intern Med. 2012;27:506–512. doi: 10.1007/s11606-011-1861-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand A, Brand H, Schulte in den Bäumen T. The impact of genetics and genomics on public health. Eur J Hum Genet. 2008;16:5–13. doi: 10.1038/sj.ejhg.5201942. [DOI] [PubMed] [Google Scholar]
- Braun V, Clarke V. Using thematic analysis in psychology Using thematic analysis in psychology. Qual Res Psychol. 2008:37–41. [Google Scholar]
- Charmaz K. Constructing grounded theory: a practical guide through qualitative analysis. 2006:208. [Google Scholar]
- Costain G, Esplen MJ, Toner B, Hodgkinson Ka, Bassett AS. 2012 Evaluating Genetic Counseling for Family Members of Individuals with Schizophrenia in the Molecular Age. Schizophr Bull. 2012;40:88–99. doi: 10.1093/schbul/sbs124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costain G, Esplen MJ, Toner B, Scherer SW, Meschino WS, Hodgkinson Ka, Bassett AS. Evaluating genetic counseling for individuals with schizophrenia in the molecular age. Schizophr Bull. 2014;40:78–87. doi: 10.1093/schbul/sbs138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLisi LE, Bertisch H. A preliminary comparison of the hopes of researchers, clinicians, and families for the future ethical use of genetic findings on schizophrenia. Am J Med Genet - Neuropsychiatr Genet. 2006;141B:110–115. doi: 10.1002/ajmg.b.30249. [DOI] [PubMed] [Google Scholar]
- Dinos S, Stevens S, Serfaty M, Weich S, King M. Stigma: The feelings and experiences of 46 people with mental illness - Qualitative study. Br J Psychiatry. 2004;184:176–181. doi: 10.1192/bjp.184.2.176. [DOI] [PubMed] [Google Scholar]
- Erskine KE, Griffith E, Degroat N, Stolerman M, Silverstein LB, Hidayatallah N, Wasserman D, Paljevic E, Cohen L, Walsh CA, McDonald T, Marion RW, Dolan SM. An interdisciplinary approach to personalized medicine: case studies from a cardiogenetics clinic. Per Med. 2013;10:73–80. doi: 10.2217/pme.12.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finn CT, Wilcox MA, Korf BR, Blacker D, Racette SR, Sklar P, Smoller JW. Psychiatric genetics: A survey of psychiatrists’ knowledge, opinions, and practice patterns. J Clin Psychiatry. 2005;66:821–830. doi: 10.4088/jcp.v66n0703. [DOI] [PubMed] [Google Scholar]
- Greendale K, Pyeritz RE. Empowering primary care health professionals in medical genetics: How soon? How fast? How far? Am J Med Genet - Semin Med Genet. 2001;106:223–232. doi: 10.1002/ajmg.10010. [DOI] [PubMed] [Google Scholar]
- Guttmacher AE, Jenkins J, Uhlmann WR. Genomic medicine: Who will practice it? A call to open arms. Am J Med Genet - Semin Med Genet. 2001;106:216–222. doi: 10.1002/ajmg.10008. [DOI] [PubMed] [Google Scholar]
- Hayflick SJ, Eiff MP, Carpenter L, Steinberger J. Primary care physicians’ utilization and perceptions of genetics services. Genet Med. 1998;1:13–21. doi: 10.1097/00125817-199811000-00005. [DOI] [PubMed] [Google Scholar]
- Hoop JG, Roberts LW, Hammond KAG, Cox NJ. Psychiatrists’ attitudes, knowledge, and experience regarding genetics: a preliminary study. Genet Med. 2008;10:439–449. doi: 10.1097/GIM.0b013e318177014b. [DOI] [PubMed] [Google Scholar]
- Hudson KL. Genomics, health care, and society. N Engl J Med. 2011;365:1033–1041. doi: 10.1056/NEJMra1010517. [DOI] [PubMed] [Google Scholar]
- Inglis a, Koehn D, McGillivray B, Stewart SE, Austin J. Evaluating a unique, specialist psychiatric genetic counseling clinic: uptake and impact. Clin Genet. 2014:1–7. doi: 10.1111/cge.12415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Javalgi R, Joseph WB, Gombeski WR, Lester JA. How physicians make referrals. J Health Care Mark. 1993;13:6–17. [PubMed] [Google Scholar]
- Kinchen KS, Cooper LA, Levine D, Wang MY, Powe NR. Referral of patients to specialists: Factors affecting choice of specialist by primary care physicians. Ann Fam Med. 2004;2:245–252. doi: 10.1370/afm.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lannin DG, Vogel DL, Brenner RE, Tucker JR. Predicting Self-Esteem and Intentions to Seek Counseling: The Internalized Stigma Model. Couns Psychol. 2015;43:64–93. [Google Scholar]
- Lyus VL. The importance of genetic counseling for individuals with schizophrenia and their relatives: Potential clients’ opinions and experiences. Am J Med Genet Part B Neuropsychiatr Genet. 2007;144:1014–1021. doi: 10.1002/ajmg.b.30536. [DOI] [PubMed] [Google Scholar]
- McAllister M. Grounded Theory in Genetic Counseling Research. J Genet Couns. 2001;10:233–250. [Google Scholar]
- Omenn GS. Public health genetics: an emerging interdisciplinary field for the post-genomic era. Annu Rev Public Health. 2000;21:1–13. doi: 10.1146/annurev.publhealth.21.1.1. [DOI] [PubMed] [Google Scholar]
- Peay HL, Hooker GW, Kassem L, Biesecker BB. Family risk and related education and counseling needs: Perceptions of adults with bipolar disorder and siblings of adults with bipolar disorder. Am J Med Genet Part A. 2009;149:364–371. doi: 10.1002/ajmg.a.32696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritsher JB, Otilingam PG, Grajales M. Internalized stigma of mental illness: Psychometric properties of a new measure. Psychiatry Res. 2003;121:31–49. doi: 10.1016/j.psychres.2003.08.008. [DOI] [PubMed] [Google Scholar]
- Strauss A, Corbin J. Basics of qualitative research: Techniques and procedures for developing grounded theory. 2 1998. [Google Scholar]
- Thompson C, Hamilton SP, Hippman C. Psychiatrist attitudes towards pharmacogenetic testing, direct-to-consumer genetic testing, and integrating genetic counseling into psychiatric patient care. Psychiatry Res. 2015 Mar 30;226(1):68–72. doi: 10.1016/j.psychres.2014.11.044. [DOI] [PubMed] [Google Scholar]
- Vogel F. Schizophrenia genesis: The origins of madness. Am J Hum Genet. 1991;48:1218. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.