Abstract
Background and Objectives
The Affordable Care Act intended to “extend affordable coverage” and “ensure access” for vulnerable patient populations. This investigation examined whether the type of insurance (Medicaid, Medicare, BlueCross, cash pay) carried by trauma patients influences access to pain management specialty care.
Methods
Investigators phoned 443 board certified pain specialists, securing office visits with 235 pain physicians from 8 different states. Appointments for pain management were for a patient that sustained an ankle fracture requiring surgery and experiencing difficulty weaning off opioids. Offices were phoned 4 times assessing responses to the 4 different payment methodologies.
Results
53% of pain specialists contacted (235 of 443) were willing to see new patients to manage pain medication. Within the 53% of positive responses, 7.2% of physicians scheduled appointments for Medicaid patients, compared with 26.8% for cash paying patients, 39.6% for those with Medicare, and 41.3% with BlueCross (P < 0.0001). There were no differences in appointment access between states that had expanded Medicaid eligibility for low-income adults versus states that had not expanded Medicaid eligibility. Neither Medicaid nor Medicare reimbursement levels for new patient visits correlated with ability to schedule an appointment or influenced wait times.
Conclusions
Access to pain specialists for management of pain medication in the postoperative trauma patient proved challenging. Despite the Affordable Care Act, Medicaid patients still experienced curtailed access to pain specialists and confronted the highest incidence of barriers to receiving appointments.
INTRODUCTION
In this new era of the Patient Protection and Affordable Care Act (PPACA), this study examined influences of different types of insurances (Medicaid, Medicare, BlueCross, or cash pay) carried by patients and their ability to secure appointments to see a fellowship trained pain management specialist in the postoperative trauma setting. The study was designed to identify barriers that patients experience as well as determine if Medicaid reimbursement rates are responsible for the decreased likelihood of Medicaid patients from securing office visits. It was hypothesized that despite passage of the PPACA, Medicaid patients would experience increased difficulty in obtaining access compared to trauma patients carrying other reimbursement methods.
In addition to access of care issues, trauma surgeons often struggle with balancing pain control along with risks of potential opioid addiction.1 There are no published guidelines regarding appropriate length of time to administer analgesics in the postoperative trauma patient.2 Trauma surgeons are not prepared to manage some complexities (ie, hyperalgesia, chronic pain, narcotic addiction) of postoperative pain in patients who return to the clinic several months after surgery still dependent on opioids for pain control, often at ever-increasing doses. Furthermore, this group of patients would benefit from the specialized care of pain management physicians and/or drug addiction specialists.
For the general patient population, there may also be challenges of gaining access to pain management specialists, but the literature demonstrates that the majority of these patients are usually managed by their primary care providers, and only 0.5% to 2% are referred to pain management specialists.3 Further examination of the literature reveals that racial and ethnic differences may also exist on access to pain management in the general population. For example, patients with low access were found to have financial concerns4 and a national mail survey of PCPs, pain physicians, chiropractors, and acupuncturists found that 52% of patients with chronic pain were managed by primary care physicians with only 2% being managed by pain physicians.5
The PPACA expanded Medicaid eligibility coverage from those with incomes of 61% of the federal poverty level to individuals with incomes up to 138% of the poverty level.6 In addition, the United States Supreme Court ruled that each state could decide whether or not to expand Medicaid coverage. As of June 2016, 30 states and the District of Columbia have increased eligibility. This has resulted in those from states without expanded Medicaid eligibility with a medical care coverage gap.6 The design of this study searched to identify differences in access for patients in states with expanded Medicaid eligibility versus those without expanded Medicaid coverage.
METHODS
The study was submitted and approved by the Institutional Review Board office. The study was conducted from June through July 2015, and included offices of board-certified pain management specialists from 8 states (California, Massachusetts, Ohio, New York, Florida, Georgia, Texas, and North Carolina). These states were selected because they represented diverse geographic areas and patient populations as well as different healthcare marketplace settings. The American Board of Medical Specialties “Certification Matters” website7 was used to generate an alphabetized list of physicians board certified in pain medicine from each state. Out of 443 offices contacted, a total of 235 individual offices from 8 different states (29 – 30 physicians per state) were enrolled. A total of 45 to 71 pain specialist offices were phoned per state to find at least 29 physicians whose practice included management of opioid pain medications. Of the 235 offices enrolled, a total of 940 phone conversations were conducted (235×4). Each physician office was randomly paired with a study number defining the order offices were called. If an office phone number was inaccurate, it was excluded from the investigation calling list.
Investigators called each office requesting an appointment for a fictitious 60-year-old (70 year-old in the case of a Medicare patient) parent (ie, father) who suffered a traumatic ankle fracture and had undergone surgical repair several months prior. The caller added that the patient was having difficulty weaning off opioid analgesics. The caller read from a standardized script to limit intra- and inter-office variation (Supplemental Data Content 1). Callers confirmed, with each scenario, that the physician responsible was a qualified pain management specialist trained in treating patients taking opioid pain medication. If the physician was not capable of performing medical management of pain, office responses were removed from the dataset and the next number was called until 29 physician offices per state were called. The caller indicated whether the patient had Medicaid, Medicare, BlueCross, or was planning on making cash payments. The scenario was repeated with 4 calls to each office, each separated by at least a 7-day period until all 4 payment mechanisms had been advocated.
Data recorded with each attempt at making an appointment included date phone call was initiated and date of the scheduled appointment, if one was provided. Offices not willing to provide appointments were asked for reasons why an appointment was denied. In those instances of an appointment denial for patients with Medicaid, the office was also asked for a referral to another pain specialist who might be willing to accept Medicaid. For scenarios of cash paying patients, information about initial consultation fees and subsequent follow-up fees were recorded. Barriers to obtaining an initial pain management consultation appointment, such as requiring a referral from a primary care physician (PCP), were considered unsuccessful attempts at making an appointment. The waiting period for an appointment was recorded as the time between the date of the call and the date of appointment. No appointments were ever actually scheduled. Data tabulating appointment success rates along with waiting period times were divided into 2 groups: states with expanded Medicaid eligibility (California, Massachusetts, New York, Ohio) and states without expanded Medicaid eligibility (Florida, North Carolina, Georgia, Texas).
Medicaid reimbursement rates for level 3 new patient visits were obtained by querying each state’s reimbursement rate using the Current Procedural Terminology (CPT) code 99203. Corresponding Medicare reimbursement rates for CPT code 99203 of each state were obtained from the Center for Medicare and Medicaid Services.8 A level 3 new patient visit is for a patient presenting with problems of mild-to-moderate complexity and needs to include: a) Documentation of a detailed medical history, b) Detailed physical exam, and c) Low complexity medical decision making.
Statistical analysis was performed using SPSS Statistics (IBM SPSS Statistics for Windows, Version 21.0; IBM Corp., Armonk, New York). Chi-square test or Fisher exact test was used to analyze differences in appointment acceptance rate based on insurance type. When comparing time period to appointments received, an independent samples t-test was used after applying natural log transformation, as the data were not normally distributed. Multiple regression analysis was performed to detect whether the Medicaid type(s) of physician compensation were a significant predictor for successfully making an appointment for those with such insurance. Unless otherwise stated, all statistical testing was performed 2-tailed at an alpha-level of 0.05.
Results
It required that 45–71 pain specialist offices be phoned per state to find at least 29 physicians per state whose practices included management of opioid analgesic medications (Fig. 1). Those excluded were pain specialty practices that did not treat patients prescribed opioid analgesics and offices focusing only on interventional pain medicine. Of the 8 states selected, North Carolina proved the most difficult to secure an initial office visit for pain management specialty care of a new patient regardless of payment method, requiring that 71 offices needed to be phoned and Florida proved to be the easiest with 45 offices called before the minimum of 29 offices agreed to see new patients.
Figure 1.
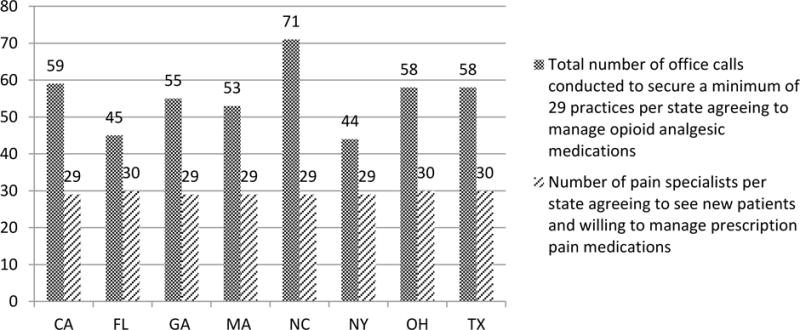
Number of phone calls per state and proportions of pain medicine specialty office practices willing to manage opioid analgesic pain medications
Of all 235 physician pain specialty offices from 8 states, the rates for successfully obtaining an appointment were 7% for Medicaid patients, 27% in those offices willing to accept cash payments for services rendered, 40% for patients with Medicare, and 41% for those with Blue Cross (Table 1A). In states with expanded Medicaid eligibility and increased access to Medicaid for low-income adults, appointment success rates were 9% for Medicaid patients, 28% for cash paying patients, 39% for those with Medicare, and 44% for patients with Blue Cross. In states without expanded Medicaid eligibility, appointment success rates were 5% for Medicaid patients, 25% for cash paying patients, 39% for those with Blue Cross and 40% for those with Medicare. Appointment success rates were significantly lower for Medicaid patients when compared to those with Medicare (P< 0.0001), BlueCross (P < 0.0001), or cash paying patients (P < 0.0001) regardless if the state elected to expand Medicaid eligibility or not (Table 1A). There were minor differences in appointment success rates in states with expanded access to Medicaid for low-income adults compared to states with non-expanded Medicaid eligibility. Results revealed there were differences between offices willing to make a new patient appointment for those with Medicaid in states with expanded Medicaid eligibility (9.4%) versus those states without expanded Medicaid eligibility (5.1%), but results were not statistically significant (Table 1B).
Table 1A.
Success rates: pain medicine physicians willing to provide appointments to new patients according to the 4 different payment mechanisms
| Patient payment method | Medicaid (n=235) |
Medicare (n=235) |
Private insurance (n=235) |
Cash pay (n=235) |
|---|---|---|---|---|
| All states: offices willing to see new patients | ||||
| Yes (%) | 17 (7.2%) | 93 (39.6%) | 97 (41.3%) | 63 (26.8%) |
| No (%) | 218 (92.8%) | 142 (60.4%) | 138 (58.7%) | 172 (73.2%) |
| P-value* | < 0.0001 | < 0.0001 | < 0.0001 | |
| States w/expanded Medicaid eligibility: offices willing to see new patients | Medicaid (n=117) |
Medicare (n=117) |
Private (n=117) |
Cash pay (n=117) |
| Yes (%) | 11 (9.4%) | 46 (39.3%) | 51 (43.6%) | 33 (28.2%) |
| No (%) | 106 (90.6%) | 71 (60.7%) | 66 (56.4%) | 84 (71.8%) |
| P-value* | < 0.0001 | < 0.0001 | < 0.0001 | |
| States w/o expanded Medicaid eligibility: offices willing to see new patients | Medicaid (n=118) |
Medicare (n=118) |
Private (n=118) |
Cash pay (n=118) |
| Yes (%) | 6 (5.1%) | 47 (39.8%) | 46 (39.0%) | 30 (25.4%) |
| No (%) | 112 (94.9%) | 71 (60.2%) | 72 (61.0%) | 88 (74.6%) |
| P-value* | < 0.0001 | < 0.0001 | < 0.0001 |
Comparison to Medicaid
Table 1B.
Appointment success rate(s) in expanded versus non-expanded Medicaid states
| Offices willing to see new Medicaid patients | Expanded Medicaid states (n=117) | Non-expanded Medicaid states (n=118) | P-value |
|---|---|---|---|
| Yes (%) | 11 (9.4%) | 6 (5.1%) | 0.201 |
| No (%) | 106 (90.6%) | 112 (94.9%) |
One frequent barrier to obtaining a pain management specialty appointment was due to the lack of a PCP referral for pain medicine care (Table 2A). Patients with private insurance coverage (43%) and without a PCP referral were found to have the easiest time in securing appointments as a new client by specialty trained pain physicians when compared to those with Medicaid (15.7%) as well as other payment methods. For patients without a PCP referral, those with Medicaid (84%) were statistically more likely to be denied an initial appointment when compared to individuals with Medicare (58%; P <0.0001), and patients with BlueCross insurance (57%; P <0.0001), and when compared to those making cash payments (63%; P <0.0001).
Table 2A.
Pain medicine specialty practices requiring patients be provided with a PCP referral before being seen by a pain management specialist
| Medicaid (n=108) |
Medicare (n=221) |
Private insurance (n=230) |
Cash pay (n=177) |
|
|---|---|---|---|---|
| All states | ||||
| Pain practices requiring a PCP referral (n=462; %) | 91 (84.3%) | 128 (57.9%) | 131 (57.0%) | 112 (63.3%) |
| Pain practices willing to see new patients regardless of a PCP referral (n=274; %) | 17 (15.7%) | 93 (42.1%) | 99 (43.0%) | 65 (36.7%) |
| P-value* | < 0.0001 | < 0.0001 | < 0.0001 | |
| States w/expanded Medicaid eligibility | ||||
| Pain practices requiring a PCP referral (%) | 53 (82.8%) | 64 (58.2%) | 62 (54.4%) | 51 (60.0%) |
| Pain practices willing to see new patients regardless of a PCP referral (%) | 11 (17.2%) | 46 (41.8%) | 52 (45.6%) | 34 (40.0%) |
| P-value* | < 0.0001 | < 0.0001 | < 0.0001 | |
| States w/o expanded Medicaid eligibility | ||||
| Pain practices requiring a PCP referral (%) | 38 (86.4%) | 64 (57.7%) | 69 (59.5%) | 61 (66.3%) |
| Pain practices willing to see new patients regardless of a PCP referral (%) | 6 (13.6%) | 47 (42.3%) | 47 (40.5%) | 31 (33.7%) |
| P-value* | < 0.0001 | < 0.0001 | < 0.0001 |
PCP- primary care practitioner,
Comparison to Medicaid
In states that elected to increase access to Medicaid for low-income adults, patients with private insurance coverage (45.6%) found it easier to be seen as a new client by pain physicians. However, in those states without expanded Medicaid eligibility, it was the trauma patient population covered by Medicare (42.3%) that found it easier to be seen as a new patient by pain-care physicians when compared to other types of payment methods (Table 2A).
There were minor differences seen in referral requirements for those with Medicaid in states with increased access when compared to states without expanded Medicaid eligibility, but were not statistically significant (Table 2B).
Table 2B.
Pain medicine specialty practices requiring patients be provided with a PCP referral before being seen by a pain management specialist in expanded versus non-expanded Medicaid states
| All states | Expanded states | Non-expanded states | P-value |
|---|---|---|---|
| Pain practices requiring a PCP referral (%) | 53 (82.8%) | 38 (86.4%) | 0.619 |
| Pain practices willing to see new patients regardless of a PCP referral (%) | 11 (17.2%) | 6 (13.6%) |
For Medicaid patients not successful in receiving an initial pain consultation appointment (due to Medicaid insurance not being accepted), the majority of these offices phoned indicated that they were not able to refer patients to another pain management specialist who might be willing to accept Medicaid. There were no differences in the waiting periods for receiving a pain management office appointment regardless of insurance type (Medicaid 12.2 days, Medicare 12.9 days P = 1, Private 13.1 days P = 1, Cash pay 9.4 days P = 1). In states without expanded access to Medicaid for low-income adults and families, there was a longer waiting period before receiving an appointment, but it was not statistically significant compared with states with expanded access for Medicaid patients.
Medicaid and Medicare reimbursement rates ($) for a level 3 new patient visit varied across the 8 states examined (Table 3). North Carolina Medicaid rates paid the highest at $80.9 while the same level 3 visit in Florida paid the lowest at $48.7. Georgia Medicare rates paid the highest ($151.6) while Texas Medicare rates paid the lowest ($114). Neither the acceptance rate for securing a pain management specialist appointment or waiting periods for obtaining such visits revealed any correlation to reimbursement rates as revealed by logistic regression analysis.
Table 3.
Medicaid and Medicare reimbursements for a level 3 new patient pain management care work-up/evaluation in 2014.
| State | Medicaid | Medicare |
|---|---|---|
| CA* | $57.2 | $124 |
| FL | $48.7 | $119.3 |
| MA* | $77.9 | $122.3 |
| NC | $80.9 | $114.3 |
| NY* | $56.9 | $115.1 |
| OH* | $74.2 | $114.9 |
| GA | $76.53 | $151.6 |
| TX | $61.6 | $114 |
State with expanded Medicaid eligibility
DISCUSSION
The primary purpose of this study was to measure a trauma patient’s ability to gain access to specialized pain management care and for treatment of opioid analgesic dependence used for postoperative pain control. Three different insurance types (Medicaid, Medicare, and BlueCross) were evaluated along with a cash payment model. Medicaid patients in the 8 different states included in this nationwide access study received less access to pain medicine specialty care when compared with those patients with Medicare or BlueCross insurance, or those paying cash (7.2% versus 39.6%, 41.3%, 26.9%, respectively). It was also shown that fewer physicians were willing to accept Medicaid coverage, and those who did accept Medicaid insurance created barriers for these patients to obtain timely appointments. Additionally, many physicians required that Medicaid patients first have a PCP referral prior to obtaining an appointment, but these same requirements were placed on those with Medicare and BlueCross insurance less frequently.
Four states had expanded Medicaid eligibility (California, Massachusetts, New York, Ohio) and 4 states were without expanded Medicaid eligibility (Florida, North Carolina, Georgia, Texas). Conclusions from the 8 represented states revealed that there were no statistically significant differences between Medicaid access in expanded versus non-expanded states. It is believed that this is the first investigation of its kind evaluating a trauma patient’s access to consultation with a pain management specialist across multiple states since passage of the PPACA.
Rationale for designing this investigation was due to the overwhelming concerns of the current opioid analgesic epidemic.9, 10 This opioid abuse epidemic was in addition to anecdotal reports experienced by orthopedic trauma surgeons, primary care physicians (PCPs), and patients who were unable to schedule appointments with pain management specialists for treatment of opioid analgesic dependence. The hypothesis was that patients with Medicaid insurance coverage would have reduced access to medical care by pain management specialists, despite the passage of the PPACA.
Medicaid policies from several offices of 4 states included in the study (Massachusetts, North Carolina, Texas, and New York) required a PCP referral in order to see a pain management specialist. However, it was also found that many of these same pain practices within these states were willing to schedule appointments for Medicaid patients without a PCP referral, which might suggest that such decisions depended on individual office practice policies. In addition, the majority of offices in these states cited that they simply did not accept Medicaid as an insurance policy, which was consistent with results from previous investigations.11–13
The analysis of the study showed that initial office visit acceptance rates, referral rates, and waiting periods were not significantly correlated with new patient visit reimbursements. A possible explanation is that the reimbursement under PPACA for level 3 new patient clinical visits is too small and outweighed other complex issues related to treating opioid-dependent patients. Medicaid insurance lower reimbursement rates are likely to be one reason physicians are not willing to accept such patients. Pain practices also indicated that those using Medicaid consume more medical care resources and are increasingly likely to be involved in litigation.14 In addition, Medicaid patients are often thought to represent members from underserved communities and likely to live in environments with increased substance abuse, factors which could make opioid medication management yet another conceivable barrier.
There are several reasons why it can be challenging to schedule an appointment with a pain specialist, including those physicians limiting their scope of practice to interventional techniques (Table 4). Almost half of all pain medicine physicians contacted stated that they were only practicing interventional pain techniques and not structured to manage analgesic medication prescriptions or opioid-addicted patients. Analysis of the study results demonstrated that Medicaid patients waited longer time periods for office appointments than those with Medicare, BlueCross, and cash payment mechanisms. However, these findings were not statistically significant, but this trend could suggest that pain physicians were likely to have fewer appointment times available for Medicaid patients. This investigation also demonstrated lower success rates for Medicaid patients gaining access to pain management specialty care when compared with other insurance models. This resulted in making it difficult for those with Medicaid insurance to find pain specialists willing and able to manage pain medication and opioid analgesic addiction on a timely basis.
Table 4.
Factors influencing pain specialty practices focusing on interventional techniques
| Pain management practices are becoming increasingly sub-specialized in interventional pain techniques17–19 |
| Pain management specialists find it costly and more consuming of healthcare resources to care for patients who require pain medication management18, 20–23 |
| Pain management specialists can be increasingly burdened with legal ramifications associated with prescribing opioid analgesic medications24–27 |
| Fewer medical students from U.S. medical schools are choosing pain management as a sub-speciality25, 27 |
The original power analysis was for a study including 8 states representing different geographical areas within the United States. This study was limited as 8 states were included in the analysis and may have been more impactful if additional regions had been contacted. It was determined that the sample size needed to consist of 241 pain management specialists in order to detect an effect size of at least 0.2 between the acceptance rate of Medicaid versus other insurance types at a power of 80%. Expanding the study size may have more accurately determined any effects of patient acceptance rates also based on influence of the waiting periods when determining if there were any correlation(s) to reimbursement rates. In addition, the regression analyses and statistical significance of waiting periods may have provided more details if a larger number of individual pain medicine physicians had been contacted. Other confounding factors and information such as day of the week an office was phoned or pain medicine physician vacation schedules should have been captured.
To minimize for potential bias created by office schedulers identifying the callers, each call was separated by at least > 7 days, and the majority of calls to the same office were made by different callers to reduce voice recognition. Even if there may have been some bias on the part of the office staff(s) receiving the calls, none of staff chose to further inquiry or bring it to the attention of any of the callers during each conversation or during subsequent calls. In addition, none of the offices phoned were ever informed about the purpose of any repeat calls, none of the offices inquired about change(s) in patient insurance type(s), repeat calls were made regardless if the preceding call was or was not successful in securing a patient appointment, no information about the repeat call(s) was ever volunteered to any of the office personal, and none of the offices contacted ever inquired as to why repeat calls were being conducted. There were no considerations for differences between multiple physician group practices versus a solo pain specialty practice design. Benefit of randomization to type of patient health care coverage (i.e. insurance or cash pay), when making each of the 4 office phone calls, could have reduced both caller and office staff potential for bias.
Descriptions by patients that they intend to make cash payment could be regarded as a sign of an opioid seeking and doctor shopping individual. To minimize this influence, the phone scenario reflected a patient who was trying to stop opioid pain medication dependence and needed the assistance of a specialist, rather than an individual seeking opioid prescription medication. Additionally and regardless of which of the 4 payment methodologies used, to further reduce bias against patients seeking referral, offices calling were also asked if they accepted individuals for opioid medication management. Only after confirming that the specialty practice managed opioid medications did further discussion about specific insurance/payment type was conducted to reduce bias. The authors realized they inconvenienced these medical care offices, but also realized that by phoning and speaking directly with the office could provide for better quantity and quality of data collected than could have ever been achieved by written letters or an email survey.
The success rates for trauma patients gaining access to pain management specialists in the perioperative period needs to be re-evaluated since more than half of the pain management groups contacted were not willing to see postoperative patients for the purpose of managing prescription pain medications. Even with the PPACA, increased medical care coverage for patients has not translated into improved access to care as this investigation revealed that less than 8% of Medicaid patients were able to schedule appointments with pain management specialists. Within the United States, trauma patients tend to make up a large proportion of individuals with Medicaid insurance coverage.15 Those individuals of the trauma patient population are increasingly being confronted with a medical landscape that is ill prepared to manage all aspects associated with postoperative surgical pain. This becomes even more challenging as PCPs, orthopedic surgeons and pain management specialists will change how opioid prescription behavior can vary in response to individual state prescription monitoring services16, ever-present concerns of legal ramifications associated with prescribing opioid analgesics, inappropriate management of chronic opioid dependent patients, and an increasing awareness of the many negative consequences associated with opioid analgesic medications.
Supplementary Material
Acknowledgments
Sources of Funding:
No funding sources were used for this study and the study was approved by the Yale University Institutional Review Board (#13637).
Footnotes
Conflicts of Interest:
None of the authors has a conflict of interest.
References
- 1.Parran T., Jr Prescription drug abuse. A question of balance. Med Clin North Am. 1997;81:967–978. doi: 10.1016/s0025-7125(05)70558-7. [DOI] [PubMed] [Google Scholar]
- 2.Holman JE, Stoddard GJ, Horwitz DS, Higgins TF. The effect of preoperative counseling on duration of postoperative opiate use in orthopaedic trauma surgery: a surgeon-based comparative cohort study. J Orthop Trauma. 2014;28:502–506. doi: 10.1097/BOT.0000000000000085. [DOI] [PubMed] [Google Scholar]
- 3.Mills S, Torrance N, Smith BH. Identification and management of chronic pain in primary care: a review. Curr Psychiatry Rep. 2016;18:22-015-0659-9. doi: 10.1007/s11920-015-0659-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nguyen M, Ugarte C, Fuller I, Haas G, Portenoy RK. Access to care for chronic pain: racial and ethnic differences. J Pain. 2005;6:301–314. doi: 10.1016/j.jpain.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 5.Breuer B, Cruciani R, Portenoy RK. Pain management by primary care physicians, pain physicians, chiropractors, and acupuncturists: a national survey. South Med J. 2010;103:738–747. doi: 10.1097/SMJ.0b013e3181e74ede. [DOI] [PubMed] [Google Scholar]
- 6.Kaiser Family Foundation. Medicaid Moving Forward. Kaiser Family Foundation; Accessed October 10, 2014. [Google Scholar]
- 7.American Board of Medical Specialties. Certification Matters | Find Out if Your Doctor is Board Certified | ABMS. Accessed June, 2015. [Google Scholar]
- 8.Centers for Medicare and Medicaid Services. Physician Fee Schedule Search. Accessed June, 2015. [Google Scholar]
- 9.Howell D, Kaplan L. Statewide Survey of Healthcare Professionals: Management of Patients With Chronic Noncancer Pain. J Addict Nurs. 2015;26:86–92. doi: 10.1097/JAN.0000000000000075. [DOI] [PubMed] [Google Scholar]
- 10.Franklin G, Sabel J, Jones CM, et al. A comprehensive approach to address the prescription opioid epidemic in Washington State: milestones and lessons learned. Am J Public Health. 2015;105:463–469. doi: 10.2105/AJPH.2014.302367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim CY, Wiznia DH, Wang Y, et al. The effect of insurance type on patient access to carpal tunnel release under the Affordable Care Act. J Hand Surg Am. 2016;41:503–509. doi: 10.1016/j.jhsa.2016.01.007. [DOI] [PubMed] [Google Scholar]
- 12.Kim CY, Wiznia DH, Hsiang WR, Pelker RR. The effect ofinsurance type on patient access to knee arthroplasty and revision under the Affordable Care Act. J Arthroplasty. 2015;30:1498–1501. doi: 10.1016/j.arth.2015.03.015. [DOI] [PubMed] [Google Scholar]
- 13.Kim CY, Wiznia DH, Roth AS, Walls RJ, Pelker RR. Survey of Patient Insurance Status on Access to Specialty Foot and Ankle Care Under the Affordable Care Act. Foot Ankle Int. 2016 doi: 10.1177/1071100716642015. [DOI] [PubMed] [Google Scholar]
- 14.Hinman A, Bozic K. Impact of Payer Type on Resource Utilization, Outcomes and Access to Care in Total Hip Arthroplasty. J Arthroplasty. 2008;23:9–14. doi: 10.1016/j.arth.2008.05.010. [DOI] [PubMed] [Google Scholar]
- 15.Wiznia DH, Averbukh L, Kim CY, Goel A, Leslie MP. Motorcycle helmets: the economic burden of an incomplete helmet law to medical care in the state of Connecticut. Conn Med. 2015;79:453–459. [PubMed] [Google Scholar]
- 16.Manasco AT, Griggs C, Leeds R, et al. Characteristics of state prescription drug monitoring programs: a state-by-state survey. Pharmacoepidemiol Drug Saf. 2016;25:847–851. doi: 10.1002/pds.4003. [DOI] [PubMed] [Google Scholar]
- 17.Manchikanti L, Pampati V, Falco FJ, Hirsch JA. An updated assessment of utilization of interventional pain management techniques in the Medicare population: 2000 – 2013. Pain Physician. 2015;18:E115–27. [PubMed] [Google Scholar]
- 18.Manchikanti L. The growth of interventional pain management in the new millennium: a critical analysis of utilization in the medicare population. Pain Physician. 2004;7:465–482. [PubMed] [Google Scholar]
- 19.Zerzan JT, Morden NE, Soumerai S, et al. Trends and geographic variation of opiate medication use in state Medicaid fee-for-service programs, 1996 to 2002. Med Care. 2006;44:1005–1010. doi: 10.1097/01.mlr.0000228025.04535.25. [DOI] [PubMed] [Google Scholar]
- 20.Manchikanti L, Hirsch JA. Obamacare 2012: prognosis unclear for interventional pain management. Pain Physician. 2012;15:E629–640. [PubMed] [Google Scholar]
- 21.Manchikanti L, Singh V, Pampati V, Smith HS, Hirsch JA. Analysis of growth of interventional techniques in managing chronic pain in the Medicare population: a 10-year evaluation from 1997 to 2006. Pain Physician. 2009;12:9–34. [PubMed] [Google Scholar]
- 22.Manchikanti L, Pampati V, Singh V, Boswell MV, Smith HS, Hirsch JA. Explosive growth of facet joint interventions in the Medicare population in the United States: a comparative evaluation of 1997, 2002, and 2006 data. BMC Health Serv Res. 2010;10:84. doi: 10.1186/1472-6963-10-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Manchikanti L, Abdi S, Atluri S, et al. American Society of Interventional Pain Physicians (ASIPP) guidelines for responsible opioid prescribing in chronic non-cancer pain: Part I–evidence assessment. Pain Physician. 2012;15:S1–65. [PubMed] [Google Scholar]
- 24.Macintyre PE, Huxtable CA, Flint SL, Dobbin MD. Costs and consequences: a review of discharge opioid prescribing for ongoing management of acute pain. Anaesth Intensive Care. 2014;42:558–574. doi: 10.1177/0310057X1404200504. [DOI] [PubMed] [Google Scholar]
- 25.Nathan JI. Chronic pain treatment: a high moral imperative with offsetting personal risks for the physician–a medical student’s perspective. Pain Pract. 2009;9:155–163. doi: 10.1111/j.1533-2500.2008.00257.x. [DOI] [PubMed] [Google Scholar]
- 26.Benjamin DM. Prosecution of physicians for prescribing opioids to patients. Clin Pharmacol Ther. 2007;81:797–798. doi: 10.1038/sj.clpt.6100115. [DOI] [PubMed] [Google Scholar]
- 27.Reidenberg MM, Willis O. Prosecution of physicians for prescribing opioids to patients. Clin Pharmacol Ther. 2007;81:903–906. doi: 10.1038/sj.clpt.6100127. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


