Abstract
Background
For patients with in-hospital cardiac arrests due to non-shockable rhythms, delays in epinephrine administration beyond 5 minutes is associated with worse survival. However, the extent of hospital variation in delayed epinephrine administration and its impact on hospital-level outcomes is unknown.
Methods
Within Get with the Guidelines-Resuscitation, we identified 103,932 adult patients (≥18 years) at 548 hospitals with an in-hospital cardiac arrest due to a non-shockable rhythm who received at least 1 dose of epinephrine between 2000 to 2014. We constructed two-level hierarchical regression models to quantify hospital variation in rates of delayed epinephrine administration (>5 minutes) and its association with hospital rates of survival to discharge and survival with functional recovery.
Results
Overall, 13,213 (12.7%) patients had delays to epinephrine, and this rate varied markedly across hospitals (range: 0% to 53.8%). The odds of delay in epinephrine administration were 58% higher at one randomly selected hospital compared to a similar patient at another randomly selected hospitals (median odds ratio [OR] 1.58; 95% C.I. 1.51 – 1.64). Median risk-standardized survival rate was 12.0% (range: 5.4% to 31.9%) and risk-standardized survival with functional recovery was 7.4% (range: 0.9% to 30.8%). There was an inverse correlation between a hospital’s rate of delayed epinephrine administration and its risk-standardized rate of survival to discharge (ρ= −0.22, P<0.0001) and survival with functional recovery (ρ= −0.14, P=0.001). Compared to a median survival rate of 12.9% (interquartile range 11.1% to 15.4%) at hospitals in the lowest quartile of epinephrine delay, risk-standardized survival was 16% lower at hospitals in the quartile with the highest rate of epinephrine delays (10.8%, interquartile range: 9.7% to 12.7%).
Conclusions
Delays in epinephrine administration following in-hospital cardiac arrest are common and varies across hospitals. Hospitals with high rates of delayed epinephrine administration had lower rates of overall survival for in-hospital cardiac arrest due to non-shockable rhythm. Further studies are needed to determine if improving hospital performance on time to epinephrine administration, especially at hospitals with poor performance on this metric will lead to improved outcomes.
Keywords: cardiac arrest, hospital performance, pulseless electrical activity, asystole, epinephrine
More than 80% of in-hospital cardiac arrests are due to a non-shockable rhythm – namely asystole and pulseless electrical activity (PEA).1 Clinical guidelines recommend epinephrine within 3–5 minutes of onset of cardiac arrest for improving survival for asystole and PEA.2,3 However, delays in epinephrine administration are common,4 and incremental delays in administration of epinephrine in non-shockable in-hospital cardiac arrests are associated with progressively worse survival.4,5 Based on these studies, some have advocated for adopting time to epinephrine administration as a hospital quality-metric for in-hospital resuscitation care.
It is conceivable that hospital efforts aimed at improving timely administration of epinephrine could potentially improve survival in this population where survival rates have been traditionally poor. The extent of hospital variation in delayed epinephrine administration, however, remains largely unknown. Quantifying hospital variation in delayed epinephrine administration, and its association with hospital factors and outcomes, would be important to understand in order to determine whether this gap in care is pervasive across hospitals or isolated to specific hospital groups.
To address this gap in knowledge, we used data from the Get With The Guidelines-Resuscitation registry to examine hospital-level variation in rates of delayed epinephrine administration and whether certain hospital characteristics are associated with higher or lower rates of delays. Moreover, we examined the implications of hospital variation by determining the association between a hospital’s rate of delayed epinephrine treatment and its rate of overall survival and survival with functional recovery for patients with non-shockable in-hospital cardiac arrest.
Methods
Data Sources
We used data from the the American Heart Association's Get With The Guidelines®-Resuscitation, a large prospective, hospital-based clinical registry of in-hospital cardiac arrest. The design of the registry has been described previously.1 Briefly, all patients with an in-hospital cardiac arrest, defined as absence of pulse, apnea, and unresponsiveness, without do-not-resuscitate orders, and who received cardiopulmonary resuscitation are identified and enrolled by trained personnel. To ensure completeness, multiple case-finding approaches are used, including a centralized collection of cardiac arrest code-sheets, review of hospital paging system logs, pharmacy records, hospital billing charges for resuscitation medication supplies, and routine checks of code carts.6 Data collection in the registry is based on the Utstein template, which is a standardized template of reporting on cardiac arrest.7,8 A number of measures have been implemented to further ensure data completeness and accuracy. These include rigorous training and certification of hospital staff, use of standardized software with internal logic checks, and periodic re-abstraction of data to ensure submitted records are accurate, with one particular data audit revealing an error rate of 2.4%.6 Matched data from American Hospital Association survey was used to obtain corresponding information on hospital characteristics.
Study population and variables
We identified 123,649 adults (≥18 years) with an index in-hospital cardiac arrest due to asystole or PEA in a hospital ward or intensive care unit (ICU) from January 1, 2000 to December 31, 2014. Given the different etiologies, staffing, and circumstances associated with cardiac arrest in the emergency department and procedural areas, cardiac arrests in these locations were not included in our study. Since our primary focus was to evaluate delays in epinephrine administration, we restricted our cohort to 107,139 patients who received at least one dose of epinephrine during resuscitation, did not receive vasopressin before epinephrine, and had available information regarding timing of epinephrine administration. We further excluded patients with missing data on the primary outcome of survival to discharge, and hospitals with low case-volume (< 10 cases) and missing data on hospital characteristics. Our final cohort comprised 103,932 patients at 548 hospitals (eFigure 1).
Study Variables and Outcomes
The primary exposure variable was time to administration of epinephrine, which was calculated as the difference between the time of first epinephrine administration and the time of cardiac arrest in whole minutes. Epinephrine administration >5 minutes after the recognition of cardiac arrest was defined as delayed, based on current guideline recommendations for administration of epinephrine within 3–5 minutes of cardiac arrest.2,3
The primary study outcome was survival to discharge, and the secondary outcome was survival with functional recovery. The latter was defined as cerebral performance category (CPC) scores 1 (mild or no neurological disability) or 2 (moderate neurological disability).
Patient-level information included demographics (age, sex, race), cardiac arrest characteristics (initial rhythm - asystole or PEA, location [ICU, telemetry, non-monitored ward]), use of hospital-wide code alert, time of day [daytime vs. after-hours] and day of the week [weekday vs. weekend]), time to initiation of chest compressions (≤1 vs. > 1 minute), co-morbidities (e.g. diabetes, hypertension, myocardial infarction, major trauma, acute stroke, heart failure, hepatic and renal insufficiency, metastatic malignancy, sepsis, hypotension and fluid/electrolyte disorders), and interventions in place at the time of cardiac arrest (e.g. mechanical ventilation, vasopressors and hemodialysis). In addition, information regarding hospital characteristics were obtained from the American Hospital Association database, and the included variables were hospital admission volume, total number of hospital beds, proportion of ICU beds, geographic region and teaching status. These patient. arrest, and hospital characteristics are defined in eTable 1 (online supplement).
Statistical analyses
Rates of delayed epinephrine administration for each hospital were calculated, and hospital variation in rates of delayed epinephrine was examined. Hospitals were then categorized into quartiles based on their rate of delayed epinephrine administration. Differences in patient- and hospital-characteristics across hospital quartiles of delayed epinephrine were evaluated using Cochrane-Armitage test for categorical variables and simple linear regression for continuous variables.
Next, we constructed a multivariable hierarchical regression model (patient- and hospital-level) to examine the relationship of delayed epinephrine administration with patient and hospital factors. Such models account for clustering of patients within each hospital. In these models, we included hospital site as a random effect and adjusted for the above listed patient characteristics as fixed effects. We used the median odds ratio to quantify the extent of hospital variation in rates of delayed administration of epinephrine. The median odds ratio is obtained from a hierarchical model with only patient-level variables, is calculated using the estimate of the variance of the random hospital intercept, and is always greater than 1. For example, a median odds ratio of 1.5 suggests that the odds of delay in epinephrine administration for a patient are 50% higher at one randomly selected hospital compared to another randomly selected hospital for a similar patient. After quantifying the extent of hospital variation in delayed epinephrine administration, we then added hospital characteristics to the hierarchical regression model to identify which hospital characteristics were associated with a hospital’s rate of delayed epinephrine administration.
Finally, to examine the association between a hospital’s rate of delayed epinephrine administration and its rate of survival to discharge, we first calculated risk-standardized rates of survival to discharge for each hospital using a previously validated methodology.9 To accomplish this, we constructed a multivariable hierarchical regression model with survival to discharge as the dependent variable. This model adjusted for patient factors, including demographics (age and sex), cardiac arrest characteristics (e.g., initial rhythm and location of arrest – monitored/non-monitored bed), delayed chest compressions (> 1 minute), comorbidities (e.g. myocardial infarction during hospitalization, major trauma, heart failure, diabetes, hepatic and renal insufficiency, metastatic malignancy, sepsis and fluid/electrolyte disorders), interventions in place at the time of cardiac arrest (e.g., mechanical ventilation, vasopressors and hemodialysis) based on the patient-level predictors of survival for in-hospital cardiac arrest in prior reports.9 We calculated a hospital’s risk-standardized survival rate (RSSR) as the ratio of predicted-to-expected number of survivors at each hospital multiplied by the unadjusted survival rate.
The correlation between a hospital’s rate of delayed epinephrine administration with its risk-standardized survival was then evaluated using Pearson’s correlation. Differences in risk-standardized survival across hospital quartiles by rates of delayed epinephrine use were then described. Additionally, we quantified the proportion of the hospital variation in survival explained by hospital-level differences in rates of delayed epinephrine by including rates of delayed epinephrine use as an additional covariate in the hierarchical risk-adjustment model for survival.10 Finally, we included hospital characteristics (hospital teaching status, number of beds, proportion of ICU beds, case volume, and hospital quartile of delayed epinephrine) as independent variables in the above hierarchical regression model to determine their association with hospital risk-standardized survival rate. All analyses were then repeated for our secondary outcome of survival with functional recovery.
Sensitivity analyses
We conducted a number of additional analyses to determine the robustness of our findings. First, in order to determine whether our findings were influenced by our definition of delayed epinephrine administration, we repeated the analysis of our primary outcome using a threshold of 3 minutes instead of 5 minutes to define delayed epinephrine administration. Second, given that delays in epinephrine administration and other aspects of resuscitation response may differ in patients who arrest in an ICU compared to patients who arrest outside an ICU, we repeated our primary analyses of hospital variation in epinephrine administration and its association with risk-standardized survival after restricting our cohort only to patients who arrested outside an ICU. Finally, since patients on vasopressor therapy prior to the onset of cardiac arrest may not derive benefit from additional epinephrine bolus, we repeated our analyses of hospital-level relationships after excluding patients receiving vasopressor therapy at the time of cardiac arrest.
All analyses were conducted using SAS software, version 9.4 (Cary, NC). Level of significance was set at P<0.05. The study was reviewed by the University of Iowa Institutional Review Board, which waived the requirement for informed consent because the study used deidentified data.
Results
Overall, administration of epinephrine was delayed in 12.7% of patients. The proportion of patients with delayed epinephrine treatment varied widely across hospitals and ranged from 0% to 53.8% (Median 13.5%, interquartile range: 9.5% – 19.0%, Figure 1). Hospitals were categorized into quartiles based on the proportion of patients with delayed epinephrine as follows: Q1:0–9.5%, Q2:9.5–13.5%; Q3:13.5–18.9%; Q4:19.0–53.8%.
Figure 1.
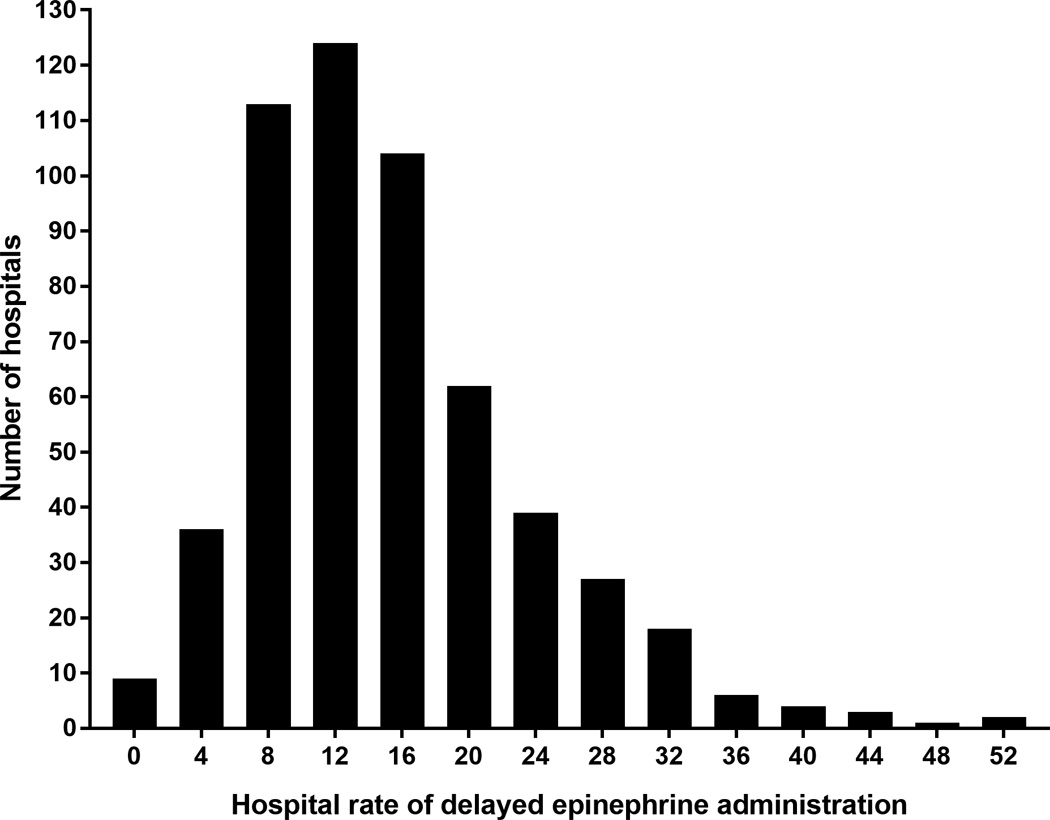
Rates of delayed epinephrine administration among non-shockable cardiac arrests across hospitals.
Tables 1 and 2 summarize patient and hospital characteristics across hospital quartiles of delayed epinephrine use. Compared to patients at hospitals in the lowest quartile of delay (Q1), patients at hospitals in the highest delay quartile (Q4) were older (mean age 66.0 years in Q1 vs. 66.8 years in Q4), less likely to be women (43.1% in Q1 vs. 41% in Q4), and more likely to have renal insufficiency (39.2% in Q1 vs. 34.4% in Q4), hepatic insufficiency (9.6% in Q1 vs. 8.8% in Q4), septicemia (21.2% in Q1 vs. 16.7% in Q4), PEA as the initial pulseless rhythm (57.7% in Q1 vs. 55.9% in Q4), or be located in the ICU at the time of arrest (62.7% in Q1 vs. 52.0% in Q4) (Ptrend < 0.0001 for all). They were also less likely to be receiving vasopressors (30.0% in Q1 vs. 23.5% in Q4) or mechanical ventilation (36.4% in Q1 vs. 25.6% in Q4) at the time of cardiac arrest (Ptrend < 0.0001 for both). Hospitals in the highest quartile of epinephrine delay had lower non-shockable cardiac arrest volume (median volume in Q1, 151 vs. 45 in Q4), lower overall admission volume (proportion of hospitals with annual volume <10,000: 22.6% in Q1 vs. 52.2% in Q4), fewer beds (<250 beds: 28.5% in Q1 vs. 57.3% in Q4), and were more likely to be non-teaching hospitals (42.3% in Q1 vs. 55.8% in Q4) (Ptrend < 0.0001 for all)
Table 1.
Baseline patient characteristics by hospital quartile for delay.
| Patient characteristics | OVERALL | Q1 6.5% (0 – 9.5%) |
Q2 11.4% (9.5% – 13.5%) |
Q3 16.2% (13.5% – 18.9%) |
Q4 26.6% (19.0% – 53.8%). |
P-value (trend) |
|---|---|---|---|---|---|---|
| Number of hospitals | 548 | 137 | 137 | 136 | 138 | |
| Number of patients | 103932 | 32577 | 33114 | 25649 | 12592 | |
| Age (mean) | 66.2±15.9 | 66.0±16.2 | 65.9±16.0 | 66.6±15.5 | 66.8±15.6 | <.0001 |
| Sex (Female%) | 42.4 | 43.1 | 42.9 | 41.5 | 41.0 | |
| Race | <.0001 | |||||
| White | 67.8 | 67.6 | 66.7 | 69.8 | 67.1 | |
| Black | 22.8 | 22.8 | 24.4 | 20.1 | 24.3 | |
| Others | 3.4 | 4.2 | 3.1 | 3.0 | 3.0 | |
| Missing/unknown | 6.0 | 5.4 | 5.8 | 7.1 | 5.6 | |
| Admission illness | <.0001 | |||||
| Cardiac, medical | 30.0 | 28.9 | 29.9 | 31.0 | 31.6 | |
| Cardiac, surgical | 5.9 | 6.3 | 5.4 | 6.5 | 4.8 | |
| Non-cardiac | 64.1 | 64.8 | 64.7 | 62.5 | 63.6 | |
| Comorbidities | ||||||
| Diabetes | 31.7 | 31.7 | 30.8 | 32.7 | 32.3 | <0.0001 |
| Heart failure | 21.4 | 21.4 | 21.4 | 21.6 | 21.2 | 0.73 |
| Acute stroke | 4.2 | 4.4 | 4.4 | 3.8 | 4.0 | 0.0005 |
| Acute myocardial infarction | 13.4 | 12.4 | 13.5 | 14.8 | 12.8 | <0.0001 |
| Hepatic insufficiency | 8.7 | 9.6 | 8.7 | 7.7 | 8.8 | <0.0001 |
| Renal insufficiency | 37.6 | 39.2 | 37.7 | 37.0 | 34.4 | <0.0001 |
| Metabolic/Electrolyte abnormality |
18.9 | 18.6 | 19.8 | 18.1 | 18.6 | <0.0001 |
| Hypotension/Hypoperfusion | 27.8 | 27.4 | 28.8 | 27.8 | 26.0 | <0.0001 |
| Major trauma | 3.8 | 4.3 | 4.4 | 3.3 | 2.3 | <0.0001 |
| Metastatic or hematologic malignancy |
14.1 | 14.1 | 14.1 | 13.9 | 14.7 | 0.18 |
| Septicemia | 19.7 | 21.2 | 20.6 | 18.2 | 16.7 | <0.0001 |
|
Procedures/Interventions in place at the time of cardiac arrest |
||||||
| Mechanical ventilation | 32.6 | 36.4 | 34.1 | 29.3 | 25.6 | <0.0001 |
| Dialysis | 3.8 | 4.2 | 3.7 | 3.5 | 3.2 | <0.0001 |
| Vasopressor | 27.8 | 30.0 | 29.1 | 25.6 | 23.5 | <0.0001 |
|
Cardiac Arrest Characteristics |
||||||
| Event location | <0.0001 | |||||
| ICU | 58.4 | 62.7 | 59.4 | 54.8 | 52.0 | |
| Telemetry | 20.0 | 18.9 | 19.8 | 21.4 | 20.3 | |
| Non-monitored ward | 21.6 | 18.4 | 20.8 | 23.8 | 27.7 | |
| Weekend or Holiday (%) | 33.9 | 33.8 | 33.8 | 34.0 | 34.4 | 0.64 |
| Nighttime (%) | 36.0 | 34.9 | 35.5 | 36.9 | 38.4 | <0.0001 |
| PEA, first rhythm (%) | 57.5 | 57.7 | 58.3 | 57.0 | 55.9 | <0.0001 |
| Hospital wide Response activation |
84.0 | 82.4 | 85.1 | 84.3 | 84.7 | <0.0001 |
Q1–Q4: Hospital quartiles for proportion of patients with delayed epinephrine use, Q1 (0 – 9.5%), Q2 (9.5 – 13.5%), Q3 (13.5 – 19.0%) and Q4 (19.0 – 53.8%).
Table 2.
Baseline hospital characteristics by hospital quartile for delay.
| Hospital characteristics | Overall | Q1 6.5% (0 – 9.5%) |
Q2 11.4% (9.5% – 13.5%) |
Q3 16.2% (13.5% – 18.9%) |
Q4 26.6% (19.0% – 53.8%) |
P-value (trend) |
|---|---|---|---|---|---|---|
| Number of hospitals | 548 | 137 | 137 | 136 | 138 | |
| Median hospital cardiac arrest volume (IQR) |
151 (34– 318) |
157 (75 – 332) |
116 (52 – 251) |
45 (26 – 100) |
||
| Proportion with median cardiac arrest volume < 100 (%) |
49.8 | 46.0 | 33.6 | 44.8 | 74.6 | <0.0001 |
| Overall admissions | <0.0001 | |||||
| <10,000 | 31.0 | 22.6 | 19.7 | 29.4 | 52.2 | |
| 10,000 – 30,000 | 56.2 | 63.5 | 65.7 | 58.1 | 37.7 | |
| >30,000 | 12.8 | 13.9 | 14.6 | 12.5 | 10.1 | |
| Total beds | <0.0001 | |||||
| <250 | 38.1 | 28.5 | 27.7 | 39.0 | 57.3 | |
| 250 – 499 | 39.8 | 46.7 | 45.3 | 39.7 | 27.5 | |
| 500+ | 22.1 | 24.8 | 27.0 | 21.3 | 15.2 | |
| Number of cardiac ICU bed (%) | 0.49 | |||||
| <2.5 | 55.4 | 56.0 | 52.8 | 51.2 | 61.8 | |
| 2.5–10 | 41.7 | 41.6 | 44.1 | 47.1 | 34.1 | |
| >10 | 2.8 | 2.4 | 3.2 | 1.7 | 4.1 | |
| Teaching status | 0.11 | |||||
| Major teaching | 21.9 | 26.3 | 20.4 | 25.0 | 15.9 | |
| Minor teaching | 31.0 | 31.4 | 37.2 | 27.2 | 28.3 | |
| Non-teaching | 47.1 | 42.3 | 42.3 | 47.8 | 55.8 | |
| Geographic location | 0.53 | |||||
| North Mid-Atlantic | 16.1 | 19.0 | 16.8 | 16.2 | 12.3 | |
| South Atlantic* | 25.6 | 27.0 | 28.5 | 21.3 | 25.4 | |
| North Central | 21.5 | 17.5 | 19.7 | 28.7 | 20.3 | |
| South Central | 18.6 | 19.0 | 17.5 | 19.1 | 18.8 | |
| Mountain/Pacific | 18.2 | 17.5 | 17.5 | 14.7 | 23.2 | |
also includes Puerto Rico
Q1–Q4: Hospital quartiles for proportion of patients with delayed epinephrine use, Q1 (0 – 9.5%), Q2 (9.5 – 13.5%), Q3 (13.5 – 19.0%) and Q4 (19.0 – 53.8%)
The median odds ratio for delayed epinephrine use after adjusting for differences in patient characteristics across hospitals was 1.58 (95% confidence interval 1.51, 1.64) suggesting that the odds of delay in epinephrine administration were 58% higher at one randomly selected hospital compared to a similar patient at another randomly selected hospital. Among hospital structural characteristics, low hospital case-volume (<100 cases) was the only factor that was associated with delayed epinephrine administration (odds ratio [OR} 1.30, 95% C.I. 1.17, 1.44; P<0.0001; eTable 2 in the online supplement). Hospital teaching status, total number of beds and proportion of ICU beds were not associated with delay in epinephrine administration. After additionally adjusting for hospital characteristics, substantial variation in delayed epinephrine administration persisted (median odds ratio 1.52 (95% C.I: 1.46, 1.58).
Table 3 presents unadjusted and risk-adjusted study outcomes. Overall patient-level rate of survival to discharge was 12.3%, and survival with functional recovery was 7.8%. Hospital rate of delayed epinephrine was inversely correlated with unadjusted rates of survival to discharge (ρ=−0.22, P<0.0001) and survival with functional recovery (ρ=−0.14, P=0.0005). After adjustment of patient characteristics across hospitals, the median hospital RSSR was 10.8% at hospitals in the highest delay quartile (interquartile range [IQR]: 9.7% – 12.7%) compared to 12.9% in the lowest delay (best) quartile (IQR: 11.1% – 15.4%, Table 3, Figure 2). Notably, addition of the variable, hospital rates of delayed epinephrine, explained 10% of the observed hospital variation in risk-standardized survival. Hospital performance on epinephrine administration was significantly associated with its RSSR even after adjusting for hospital volume, with lower survival at hospitals with more frequent delays (Q1: referent, Q2: 0.91 [0.81, 1.02], Q3: 0.86 [0.77, 0.97], Q4: 0.69 [0.60, 0.78]; Ptrend 0.03). Similarly, risk-standardized rates of survival with functional recovery were lower in the worst hospital quartile for delayed epinephrine administration (median 6.6%, IQR: 5.0% – 8.6%) as compared with the best quartile (median 8.3%, IQR: 5.1% – 12.0%, Ptrend 0.003).
Table 3.
Outcomes by quartiles of delayed epinephrine use, reported as medians and corresponding interquartile ranges (in parenthesis)
| Hospital characteristics | Q1 | Q2 | Q3 | Q4 | P-value (trend) |
|---|---|---|---|---|---|
|
Unadjusted hospital-level survival |
|||||
| To discharge | 12.0% (8.7% – 15.6%) | 11.3% (7.8% – 15.9%) | 11.6% (7.4% – 15.2%) | 8.1% (5.6% – 12.8%) | <0.0001 |
| With CPC 1 or 2 | 6.6% (3.0% – 10.0%) | 6.4% (3.2% – 8.9%) | 6.2% (3.2% – 9.7%) | 5.3% (0 – 7.8%) | 0.0026 |
|
Hospital risk-standardized survival |
|||||
| To discharge | 12.9% (11.1% – 15.4%) | 12.3% (10.4% – 15.7%) | 12.4% (10.5% –14.7%) | 10.8 (9.7% – 12.7%) | <0.0001 |
| With CPC 1 or 2 | 8.3% (5.1% – 12.0%) | 8.0% (5.2% – 11.0%) | 7.4% (4.9% – 11.1%) | 6.6% (5.0% – 8.6%) |
0.0032 |
Q1–Q4: Hospital quartiles for proportion of patients with delayed epinephrine use, Q1 (0 – 9.5%), Q2 (9.5 – 13.5%), Q3 (13.5 – 19.0%) and Q4 (19.0 – 53.8%)
Abbreviations: CPC – cerebral performance category score
Figure 2.
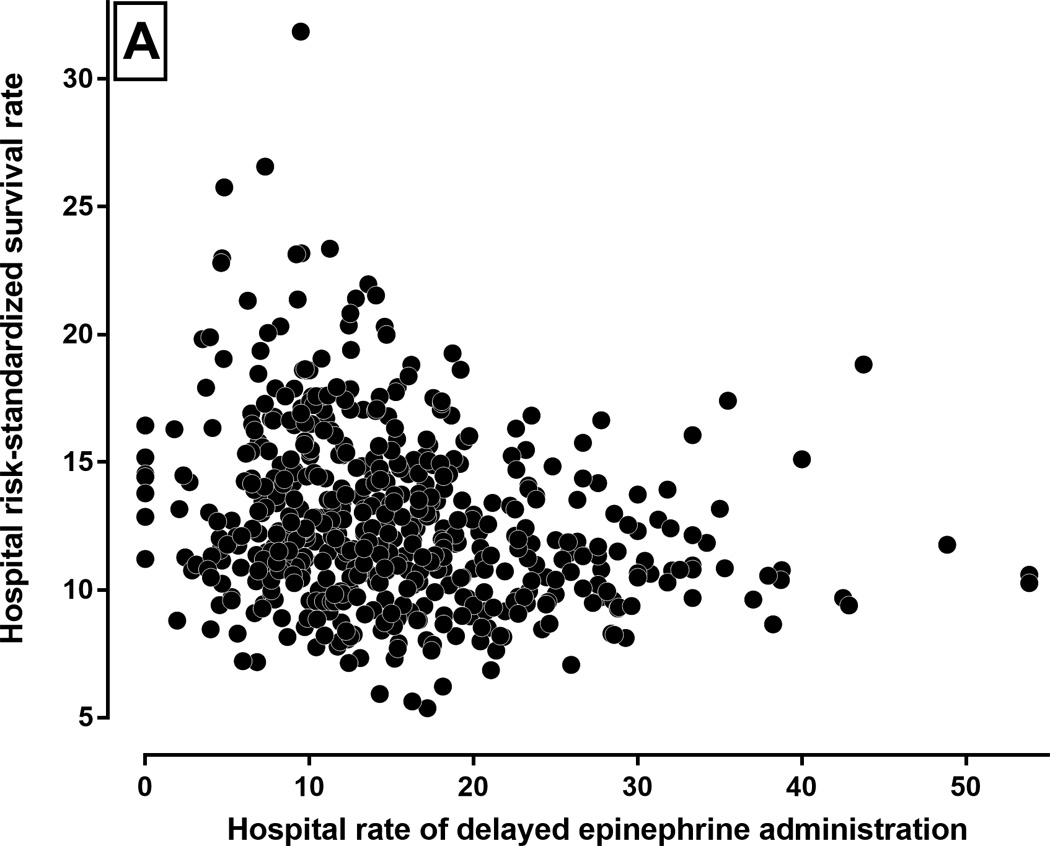
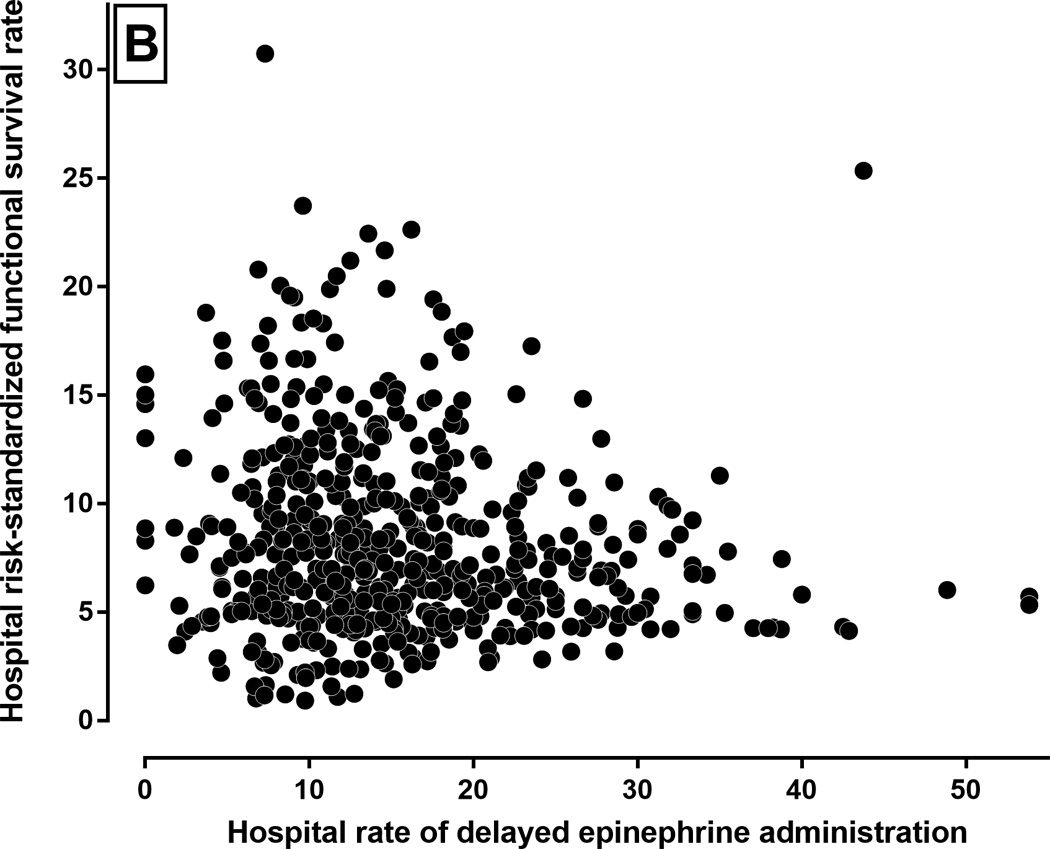
Hospital delayed epinephrine administration rate and risk standardized survival. Relationship between a hospital’s rate of delayed epinephrine administration and its rates of (A) risk-standardized survival-to-discharge (ρ= −0.22, P<0.0001), (B) risk-standardized survival with functional recovery (ρ= −0.14,P=0.001). Each circle represents a hospital in the study.
The results of our sensitivity analyses closely aligned with those of our primary analysis. We redefined delayed epinephrine administration using a cut-off of > 3 min after onset of cardiac arrest. In these analyses, delayed epinephrine administration remained inversely correlated with risk-standardized survival to discharge (ρ= −0.24, P<0.0001), as in our main analyses (eTable 3 in the online supplement). Similarly, after restricting our sample to arrests outside of the ICU, we observed a wide variation in rates of delayed epinephrine use (median OR 1.48, 95% C.I. 1.42, 1.54, eFigure 2), which was inversely correlated to the hospital risk-standardized cardiac arrest survival rate (ρ= −0.19, P-value <.0001, eFigure 3). Finally, in analyses limited to patients not receiving vasopressor therapy at the time of cardiac arrest, we observed a wide hospital-variation in delayed epinephrine use (median OR 1.51, 95% C.I. 1.44, 1.57, eFigure 4) as well as an inverse association between a hospital’s rate of delayed epinephrine administration and its risk standardized survival rate (ρ=−0.22, P-value <.0001, eFigure 5), consistent with the results of our primary analysis.
Discussion
In a large, multicenter registry of in-hospital cardiac arrests, we found large variation in timely administration of epinephrine for patients with an initial non-shockable rhythm of pulseless electrical activity or asystole. Differences in patient and cardiac arrest characteristics only partly explain the observed hospital-level differences in delayed epinephrine administration. Moreover, rates of overall survival and survival with functional recovery were lower at hospitals with more frequent delays in epinephrine administration compared to hospitals where such delays were less common. In sensitivity analysis, we demonstrated a similar relationship for a definition of epinephrine delays as >3 minutes, with significantly higher mortality in poorly performing hospitals. A number of our findings are important and merit further consideration.
In a recent patient-level analysis, there was a strong inverse association between delay in epinephrine administration and survival following non-shockable in-hospital cardiac arrest.4 This study also suggested improved rates of return of spontaneous circulation (ROSC) and survival with functional recovery with timely administration of epinephrine. Our study adds to this growing literature, by showing marked hospital-level variation in delays to epinephrine treatment. Hospitals with lower rates of delays to epinephrine had higher rates of risk-standardized survival and survival with functional recovery.
Timely administration of epinephrine in patients with non-shockable rhythm has been proposed as a metric to assess hospital resuscitation quality, similar to time to defibrillation in patients with a shockable rhythm. However, contemporary evidence regarding the efficacy of epinephrine remains uncertain. The only randomized controlled trial that has evaluated epinephrine against placebo in patients with out-of-hospital cardiac arrest was terminated early due to poor enrolment. Only 600 patients were enrolled, compared to a projected sample size of 5000 patients.11 Treatment with epinephrine compared to placebo was associated with a nearly three-fold improvement in rates of ROSC (23.5% with epinephrine use vs. 8.4% with placebo). Survival to hospital discharge was also numerically higher in the epinephrine arm (4.0% vs. 1.9%) but was not statistically significant.11 Similar findings were noted in the subgroup of 289 patients with non-shockable rhythms, with higher rates for ROSC (20.9% vs. 3.7%, P<0.001) and survival to admission (23.5% vs. 11.0%) with epinephrine use.
At the same time, data from observational studies of epinephrine use in cardiac arrest are conflicting. While some studies have suggested worse survival,12,13 others have suggested a benefit.4,5,14,15 A key limitation of studies that showed a detrimental effect of epinephrine was that many of them included patients who did not receive epinephrine as the comparator group, leading to selection bias.12,13 Moreover, timing of epinephrine administration – an important confounder, was not accounted for in the analyses.12,13 Despite the uncertainty related to epinephrine in clinical studies, recent guidelines recommend administration of epinephrine as soon as feasible after cardiac arrest with initial non-shockable rhythm.2 Therefore, the large variation in rate of delayed epinephrine administration observed in our study was particularly striking, with a median odds ratio of 1.61. Moreover, delays in epinephrine administration were more common at hospitals with low cardiac arrest case-volume compared to high volume hospitals. This may point toward a lack of institutional experience at low volume sites with regards to resuscitation care as an important underlying factor. We did not find an association between hospital structural factors such as teaching status, or hospital bed size with delays in epinephrine administration. However, this finding wasn’t altogether surprising. In a previous study, substantial hospital variation was noted in rates of delayed defibrillation for in-hospital cardiac arrest due to shockable rhythm.16 However, delays in defibrillation were not associated with hospital structural characteristics, except bed size in that study. These findings suggest that hospital processes of care are likely more important in determining hospital quality. Previous studies have shown that strategies such as more frequent CPR training and participation in simulation or mock codes may help improve retention of CPR skills, improve CPR quality and minimize treatment delays.17–19 Understanding hospital-level determinants of delay in epinephrine administration, which may differ across sites, is an important next step.
The Institute of Medicine has recommended focused research on identifying and implementing best practices from hospitals with high survival rates for cardiac arrest to improve cardiac arrest outcomes across all hospitals.20,21 However, survival for cardiac arrests with an initial rhythm of PEA or asystole remains dismally low at less than 15%.1 Moreover, few interventions have been effective in reducing the high mortality associated with non-shockable cardiac arrests. Given that patients with asystole or PEA comprise more than 80% of in-hospital cardiac arrests, efforts are urgently needed to identify processes of care that can improve survival in this high-risk population. Although, we found that hospital rate of delayed epinephrine administration was associated with survival outcomes for patients with non-shockable rhythms, our findings suggest a potential target for quality improvement but does not demonstrate causality. Future studies are needed to assess whether interventions directed at improving timeliness of epinephrine administration at poor-performing hospitals leads to an improvement in survival rates at these hospitals.
Our findings should be interpreted in the light of the following limitations. First, while the registry includes detailed information on patient characteristics, there is potential of unmeasured residual confounding in our study due to its observational design. Although we used a robust risk-adjustment methodology, our study doesn’t suggest causality. It is possible that delays in epinephrine administration are confounding by other components of cardiopulmonary resuscitation efforts, including quality of chest compressions, which is difficult to quantify and is not measured in the Get With The Guidelines – Resuscitation. Second, functional status has been inferred from CPC scores at discharge. While favorable CPC score at discharge is associated with improved long-term survival,22 patient performance on dedicated scales for neurological assessment were not available and we were therefore only able to assess functional status. Third, the time to epinephrine administration is obtained from retrospective hospital records, and is subject to discrepancy due to recording of time from multiple clocks in a code (e.g. the monitor, defibrillator, etc.).23 Any misclassification in documentation of times, however, would have biased our findings toward the null. Fourth, while there is information on preceding events and comorbid conditions, the specific etiology for cardiac arrest (e.g. trauma) are not reported. Finally, since participation in the Get With The Guidelines-Resuscitation registry is optional, our data may not be applicable to hospitals outside of those participating in this quality improvement registry.
Conclusions
In conclusion, we found marked variation in the rates of delayed epinephrine administration across hospitals for in-hospital cardiac arrests due to asystole and PEA. This variation is only partly explained by differences in patient-, cardiac arrest- and hospital-characteristics across hospitals. Moreover, hospitals that performed poorly on this metric had worse survival outcomes. Further investigations are needed to identify the reasons for delayed epinephrine administration at poorly performing hospitals, and to understand if reducing delays to epinephrine treatment results in improved outcomes.
Supplementary Material
Clinical Perspective.
What is New?
In a large national registry, we found that delays in epinephrine administration (>5 minutes) for non-shockable in-hospital cardiac arrest varied substantially across hospitals.
Hospitals with higher rates of delays in epinephrine treatment had worse survival outcomes for its cardiac arrest patients.
What are the Clinical Implications?
While current resuscitation guidelines recommend prompt delivery of epinephrine treatment to patients with in-hospital cardiac arrest due to asystole and pulseless electrical activity, there is substantial practice variation across hospitals.
Our findings suggest that hospitals with low survival rates for these cardiac arrest rhythms may benefit from quality improvement efforts that include minimizing delays in epinephrine administration.
Acknowledgments
Sources of Funding: Drs. Girotra (K08HL122527) and Chan (K23HL102224, R01HL123980) are supported by the National Heart, Lung, and Blood Institute. Dr. Khera received support from the National Center for Advancing Translational Sciences of the National Institutes of Health under award UL1TR001105. The funding agency had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Drs. Khera and Girotra had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: All authors
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Khera, Girotra.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Khera, Girotra.
Obtained funding: Girotra.
Administrative, technical, or material support: Girotra.
Study supervision: Girotra.
Disclosures: None.
References
- 1.Girotra S, Nallamothu BK, Spertus JA, Li Y, Krumholz HM, Chan PS American Heart Association Get with the Guidelines-Resuscitation I. Trends in survival after in-hospital cardiac arrest. The New England journal of medicine. 2012;367:1912–1920. doi: 10.1056/NEJMoa1109148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Link MS, Berkow LC, Kudenchuk PJ, Halperin HR, Hess EP, Moitra VK, Neumar RW, O'Neil BJ, Paxton JH, Silvers SM, White RD, Yannopoulos D, Donnino MW. Part 7: Adult Advanced Cardiovascular Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132:S444–S464. doi: 10.1161/CIR.0000000000000261. [DOI] [PubMed] [Google Scholar]
- 3.Neumar RW, Otto CW, Link MS, Kronick SL, Shuster M, Callaway CW, Kudenchuk PJ, Ornato JP, McNally B, Silvers SM, Passman RS, White RD, Hess EP, Tang W, Davis D, Sinz E, Morrison LJ. Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S729–S767. doi: 10.1161/CIRCULATIONAHA.110.970988. [DOI] [PubMed] [Google Scholar]
- 4.Donnino MW, Salciccioli JD, Howell MD, Cocchi MN, Giberson B, Berg K, Gautam S, Callaway C American Heart Association's Get With The Guidelines-Resuscitation I. Time to administration of epinephrine and outcome after in-hospital cardiac arrest with non-shockable rhythms: retrospective analysis of large in-hospital data registry. Bmj. 2014;348:g3028. doi: 10.1136/bmj.g3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Andersen LW, Berg KM, Saindon BZ, Massaro JM, Raymond TT, Berg RA, Nadkarni VM, Donnino MW American Heart Association Get With the Guidelines-Resuscitation I. Time to Epinephrine and Survival After Pediatric In-Hospital Cardiac Arrest. JAMA. 2015;314:802–810. doi: 10.1001/jama.2015.9678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peberdy MA, Kaye W, Ornato JP, Larkin GL, Nadkarni V, Mancini ME, Berg RA, Nichol G, Lane-Trultt T. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 7.Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, Cassan P, Coovadia A, D'Este K, Finn J, Halperin H, Handley A, Herlitz J, Hickey R, Idris A, Kloeck W, Larkin GL, Mancini ME, Mason P, Mears G, Monsieurs K, Montgomery W, Morley P, Nichol G, Nolan J, Okada K, Perlman J, Shuster M, Steen PA, Sterz F, Tibballs J, Timerman S, Truitt T, Zideman D International Liaison Committee on R, American Heart A, European Resuscitation C, Australian Resuscitation C, New Zealand Resuscitation C, Heart, Stroke Foundation of C, InterAmerican Heart F, Resuscitation Councils of Southern A, Arrest ITFoC, Cardiopulmonary Resuscitation O. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa) Circulation. 2004;110:3385–3397. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 8.Cummins RO, Chamberlain D, Hazinski MF, Nadkarni V, Kloeck W, Kramer E, Becker L, Robertson C, Koster R, Zaritsky A, Bossaert L, Ornato JP, Callanan V, Allen M, Steen P, Connolly B, Sanders A, Idris A, Cobbe S. Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: the in-hospital 'Utstein style'. American Heart Association. Circulation. 1997;95:2213–2239. doi: 10.1161/01.cir.95.8.2213. [DOI] [PubMed] [Google Scholar]
- 9.Chan PS, Berg RA, Spertus JA, Schwamm LH, Bhatt DL, Fonarow GC, Heidenreich PA, Nallamothu BK, Tang F, Merchant RM Investigators AG-R. Risk-standardizing survival for in-hospital cardiac arrest to facilitate hospital comparisons. J Am Coll Cardiol. 2013;62:601–609. doi: 10.1016/j.jacc.2013.05.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Girotra S, van Diepen S, Nallamothu BK, Carrel M, Vellano K, Anderson ML, McNally B, Abella BS, Sasson C, Chan PS in collaboration with CSG, the HeartRescue P. Regional Variation in Out-of-Hospital Cardiac Arrest Survival in the United States. Circulation. 2016;133:2159–2168. doi: 10.1161/CIRCULATIONAHA.115.018175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jacobs IG, Finn JC, Jelinek GA, Oxer HF, Thompson PL. Effect of adrenaline on survival in out-of-hospital cardiac arrest: A randomised double-blind placebo-controlled trial. Resuscitation. 2011;82:1138–1143. doi: 10.1016/j.resuscitation.2011.06.029. [DOI] [PubMed] [Google Scholar]
- 12.Hagihara A, Hasegawa M, Abe T, Nagata T, Wakata Y, Miyazaki S. Prehospital epinephrine use and survival among patients with out-of-hospital cardiac arrest. JAMA. 2012;307:1161–1168. doi: 10.1001/jama.2012.294. [DOI] [PubMed] [Google Scholar]
- 13.Dumas F, Bougouin W, Geri G, Lamhaut L, Bougle A, Daviaud F, Morichau-Beauchant T, Rosencher J, Marijon E, Carli P, Jouven X, Rea TD, Cariou A. Is epinephrine during cardiac arrest associated with worse outcomes in resuscitated patients? J Am Coll Cardiol. 2014;64:2360–2367. doi: 10.1016/j.jacc.2014.09.036. [DOI] [PubMed] [Google Scholar]
- 14.Goto Y, Maeda T, Goto Y. Effects of prehospital epinephrine during out-of-hospital cardiac arrest with initial non-shockable rhythm: an observational cohort study. Crit Care. 2013;17:R188. doi: 10.1186/cc12872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nakahara S, Tomio J, Takahashi H, Ichikawa M, Nishida M, Morimura N, Sakamoto T. Evaluation of pre-hospital administration of adrenaline (epinephrine) by emergency medical services for patients with out of hospital cardiac arrest in Japan: controlled propensity matched retrospective cohort study. Bmj. 2013;347:f6829. doi: 10.1136/bmj.f6829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chan PS, Nichol G, Krumholz HM, Spertus JA, Nallamothu BK American Heart Association National Registry of Cardiopulmonary Resuscitation I. Hospital variation in time to defibrillation after in-hospital cardiac arrest. Arch Intern Med. 2009;169:1265–1273. doi: 10.1001/archinternmed.2009.196. [DOI] [PubMed] [Google Scholar]
- 17.Sutton RM, Niles D, Meaney PA, Aplenc R, French B, Abella BS, Lengetti EL, Berg RA, Helfaer MA, Nadkarni V. Low-dose, high-frequency CPR training improves skill retention of in-hospital pediatric providers. Pediatrics. 2011;128:e145–e151. doi: 10.1542/peds.2010-2105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sullivan NJ, Duval-Arnould J, Twilley M, Smith SP, Aksamit D, Boone-Guercio P, Jeffries PR, Hunt EA. Simulation exercise to improve retention of cardiopulmonary resuscitation priorities for in-hospital cardiac arrests: A randomized controlled trial. Resuscitation. 2015;86:6–13. doi: 10.1016/j.resuscitation.2014.10.021. [DOI] [PubMed] [Google Scholar]
- 19.Hunt EA, Shilkofski NA, Stavroudis TA, Nelson KL. Simulation: translation to improved team performance. Anesthesiol Clin. 2007;25:301–319. doi: 10.1016/j.anclin.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 20.Becker LB, Aufderheide TP, Graham R. Strategies to Improve Survival From Cardiac Arrest: A Report From the Institute of Medicine. JAMA. 2015;314:223–224. doi: 10.1001/jama.2015.8454. [DOI] [PubMed] [Google Scholar]
- 21.The Institute of Medicine (June 2015) Strategies to Improve Cardiac Arrest Survival: A Time to Act. [Accessed February 15, 2016]; http://iom.nationalacademies.org/~/media/Files/Report%20Files/2015/Cardiac-Arrest/CardiacArrestReportBrief.pdf. [Google Scholar]
- 22.Chan PS, Nallamothu BK, Krumholz HM, Spertus JA, Li Y, Hammill BG, Curtis LH American Heart Association Get with the Guidelines-Resuscitation I. Long-term outcomes in elderly survivors of in-hospital cardiac arrest. The New England journal of medicine. 2013;368:1019–1026. [Google Scholar]
- 23.Kaye W, Mancini ME, Truitt TL. When minutes count--the fallacy of accurate time documentation during in-hospital resuscitation. Resuscitation. 2005;65:285–290. doi: 10.1016/j.resuscitation.2004.12.020. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


