Abstract
Background
Stroke is a chronic disease. Standardized assessment is essential in order to determine areas for treatment. Individuals with aphasia are often excluded from research, because it is believed that their language impairments may impact their ability to provide informed consent. Thus, right spatial neglect could be under-diagnosed.
Objective
This study was developed to (1) determine the frequency of spatial neglect in chronic left-brain stroke survivors with aphasia, (2) determine the clinical utility of an aphasia-friendly consent form, and (3) determine any differences between neglect and no-neglect groups regarding activities of daily living (ADL) performance and community independence.
Methods
Forty-six people were consented at community center. Three were screen failures secondary to the exclusion criteria. A novel, aphasia-friendly consent form was developed to facilitate participation of individuals with aphasia. This enabled 93% or 40 out of the 43 recruited participants to be included in this study. The Behavioral Inattention Test-conventional and the Catherine Bergego Scale via Kessler Foundation Neglect Assessment Process (CBS via KF-NAP) were utilized to determine neglect. The Life Space Questionnaire was used to determine community mobility and independence. The Barthel Index (BI) was used for objective clarification of performance in ADL.
Results
Successful use of the consent form resulted in determination that five out of 40 (12.5%) met criteria for spatial neglect; (on the CBS via KF-NAP). The neglect group had lower scores on the Life Space, suggesting less community mobility and independence, however, it was not statistically significant (p = 0.16). Differences in BI scores were also not significant (p = .013) but the neglect group did have reduced independence.
Conclusions
This study demonstrates the need to administer functional neglect assessments in left-brain stroke and to include individuals with aphasia in research.
Keywords: Stroke, Aphasia, Right spatial neglect, Left spatial neglect, Spatial neglect, Assessment
Introduction
Approximately, 800,000 Americans have a stroke each year, which can result in significant changes to their overall health and well-being.1 Many stroke survivors are affected by lifelong disabilities as a result. Spatial neglect, the inability to orient or respond to stimuli in the hemispace contralesional to a brain injury, is one of many functional disabilities which can be particularly challenging.1–3 The literature reports that spatial neglect, after right-brain injury, initially is predictive of poorer outcomes including decreased functional independence at discharge, greater safety risks, and substantial healthcare costs.4–6 However, the prevalence of right-sided spatial neglect in left-brain stroke survivors with aphasia has not been adequately studied – most research was performed in case study designs.7–12 The purpose of this study was to investigate the frequency of spatial neglect in a community-dwelling sample of chronic left-brain stroke survivors from an outpatient aphasia center. We intend to stress the importance of neglect assessments as a standard stroke care practice, even when the damage affects the left hemisphere.
Literature review
Stroke is one of the leading causes of long-term disability in the United States. In 2010 alone, stroke affected eight million individuals.1,2 Functional deficits following a stroke contribute to the development of long-term disability, and can include hemiparesis, decreased independence in activities of daily living (ADLs), impairments in cognition, vision, communication, and spatial neglect.5,13–16 The presence of spatial neglect in stroke survivors is predictive of decline in overall participation in life compared to other stroke survivors.4–6
Spatial neglect can affect different stages of cognitive processing, and can present as (a) reduced arousal by, attention to, and processing of stimuli from the contralesional hemispace, (b) abnormal imagery or internal representations of contralesional space17, or (c) a decreased propensity to move or act in contralesional space. Spatial neglect can affect the contralesional body, as well as contralesional space.3 In general, right spatial neglect results from a lesion in the left hemisphere, and left spatial neglect, from a lesion in the right hemisphere.18 The prevalence of spatial neglect in stroke survivors is 30–70% after right-brain damage, and 20–60% after left-brain damage.6, 8, 19–23 Variability in prevalence rates of spatial neglect may be partially due to different assessments and criteria being used to define neglect.24 Variability may also be related to different sensitivity of standard assessments to certain neglect symptoms, especially motor-intentional or motor-exploratory errors.25
Aphasia is an impairment commonly occurring after left-brain stroke that affects communication via spoken and/or written language.26 About 38% of acute stroke survivors have aphasia, with 40–60% of this population continuing to have aphasia in the chronic phase of stroke recovery.27 Previous spatial neglect studies may not have been adapted to the communication needs of people with aphasia, and thus these people may have been underrepresented in neglect research, distorting available information about the prevalence of neglect after left-brain stroke.7, 8, 10, 11, 24, 26, 28–31 Because people with communication disorders may have unique needs for spatial neglect rehabilitation, it is tremendously important to evaluate how frequently these people experience post-stroke spatial neglect symptoms. Different stages of spatial processing may also be affected if the lesion is in the left hemisphere – for example, because the left brain is generally dominant for skilled learned purposive movement,32 neglect after left-brain injury may be more likely to manifest motor-intentional, “aiming” spatial neglect symptoms.3 Thus, in this study, the objective to learn how many people in a community-dwelling sample of stroke survivors with aphasia would also be affected by spatial neglect, and what kind of symptoms these people would experience.
Methods
Study design
A descriptive, cohort, comparison, quantitative study design was used and took place at the Adler Aphasia Center in Maywood, New Jersey. This is a community center for persons with aphasia. Its leadership includes people with aphasia, researchers and speech language pathologists. Most of the groups are centered on enhancing communication and engaging in fulfilling activities to improve quality of life.
Subjects
A convenience sample was recruited through fliers, word of mouth, and phone calls to all members of the center. After obtaining IRB approval, we recruited a total of 46 participants (73% of the center’s active membership). Inclusion criteria consisted of having a left-brain stroke and aphasia, being a member of the center, and being able to consent. Three people were excluded who had a history of other neurological or visual disorders (other than visual acuity correction with glasses), or learning disabilities. Three people could not complete the consenting process.
Procedures
Participants were assessed between September 2013 and February 2015. Informed consent, observed by a witness, was obtained from participants prior to their participation. We used both a traditional and an aphasia-friendly consent form, simplified by including minimal text and pictures to depict important information in describing the research study (Fig. 1). To confirm understanding of the purpose and intent of the study, we had participants take a three-question quiz at the end of the consenting process, also including minimal text and descriptive images. An occupational therapist or research assistants administered and scored the assessments. These study staff received training on all assessment administration as well as how to communicate with aphasic people. The consenting process and administration of assessments took 1–1½ h to complete for each participant.
Figure 1.
Example of one page of the aphasia-friendly consent form.
Neglect assessment
Participants were classified as having spatial neglect if there was a positive score on at least one of the following assessments. We tested participants with the Behavioral Inattention Test-conventional subtest (BIT-C)33 and also used the Kessler Foundation Neglect Assessment Process (KF-NAP)34 to administer the Catherine Bergego Scale (CBS).35–37
The conventional BIT-C is a six-item paper-and-pencil assessment including a line cancellation array, a letter cancellation task, a star cancellation array, figure and shape copying, line bisection, and representational drawing.33 The subtests of the BIT-C are tested and scored individually. The highest possible score is 146, with a score ≤129 consistent with the presence of spatial neglect.38 The literature shows the BIT-C to have excellent test retest reliability, inter-rater reliability,42 as well as high construct and predictive validity.38
The KF-NAP34 is a set of instructions and guidelines to score functional performance on the CBS36 through direct observation. All items are completed during one session and in a specific order. The KF-NAP includes a scoring sheet and manual that standardizes the administration of the CBS and allows clinicians to provide more reliable reports of an individual’s performance in ADLs.34 Specifically, the tool asks the examiner to assesses (using non-spatially biased directions) an individual’s limb awareness, gaze orientation, auditory attention, identification of personal belongings, frequency of collisions, and performance during dressing, grooming, eating, cleaning after a meal, and navigation tasks.39, 40 Each item is scored 0–3, higher score indicating more severe symptoms. A total score of 0 indicates no neglect, 1–10 indicates mild neglect, 11–20 indicates moderate neglect, and 21–30 indicates severe neglect.36 For even more information about the CBS via the KF-NAP, a web-based tutorial is available on the World Wide Web (www.kflearn.org).
Community mobility and independence
To collect preliminary information about participants’ community mobility and independence, we administered the Life Space Questionnaire41 and the Barthel Index (BI).42 The Life Space Questionnaire assesses self-reported functional mobility within an individual’s surroundings. Respondents were asked to report how often they went outside the following spaces: bedroom, house or apartment, driveway, neighborhood, and town, state, and country. The Life Space Questionnaire has strong test–retest reliability, good construct and criterion validity. 43 Lower scores represent a smaller life space, indicating reduced community participation and mobility.44 The Barthel Index (BI) is a self reported measure of an individual’s independence in 10 activities of daily living (ADLs) including toilet use, transfers, grooming, mobility, stairs, dressing, feeding, bathing, bowel management, and bladder management.42, 45, 46 The BI is reported to have excellent inter-rater reliability, excellent internal consistency, and good construct validity.47
Results
We attempted to learn whether patients with left-brain stroke and aphasia could be assessed for spatial neglect and whether people with neglect had problems with function, community mobility, and independence. Based on this apriori hypothesis, we used a one-tailed t-test and reported analyses as significant only if they remained so after correcting for multiple comparisons.
After the aphasia-friendly adapted consenting process, only 3 of the 43 eligible people with aphasia recruited had difficulty responding to the consent quiz to assess understanding. Thus, we concluded that the aphasia-friendly consenting process was successful, as 93% of the participants demonstrated understanding of the contents of the consent form and the purpose of the study.
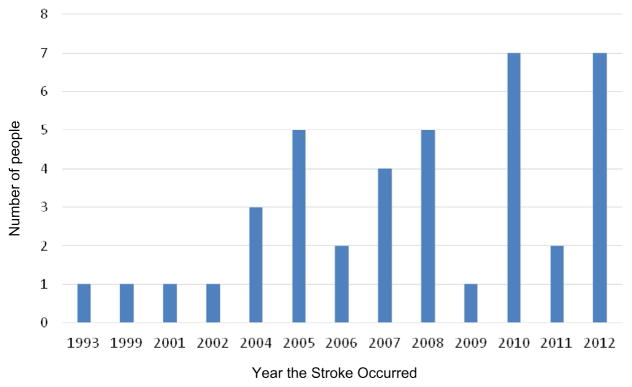
The BIT-C, the CBS via KF-NAP, the Life Space Questionnaire, and the BI were administered to all 40 participants. The process of using strategies like writing words or pointing to pictures was completed if the person required this form of communication. The person was able to determine this for the administrator because the strategies were routine and familiar. This cohort has been living with the aphasia for many years (Figure 2).
Figure 2.
Demographics on chronic stroke chort.
Neglect assessment
Behavioral Inattention Test-conventional
In this study, all participants scored above 129; thus no participants met criterion for spatial neglect by BIT-C score.
Catherine Bergego Scale via Kessler Foundation Neglect Assessment Process
We found the CBS via KF-NAP identified five participants as having mild right spatial neglect, a 12.5% frequency rate (Table 1). All participants identified with spatial neglect were men, with an average age of 70. The mean scores were 3 (SD = 2.00) and p value of 0.014 (Table 2). The abnormal items for these five participants were grooming (occurred for 3 participants), cleaning after meals (1 participant), limb awareness (1 participant), gaze orientation (1 participant), collisions (2 participants), and auditory attention (1 participant).
Table 1.
Neglect assessment information
| Participants | All: n = 40 | Without neglect: n = 35 | With neglect: n = 5 |
|---|---|---|---|
| Males | 31 (77.5%*) | 26 (74%) | 5 (12.5%*) |
| Females | 9 (22.5%*) | 9 (26%) | 0 |
| Average age | 61 | 66 | 70 |
| Age range | 40–90 | 40–90 | 64–77 |
| Average male age | 59 | 57 | 70 |
| Average female age | 69 | 73 | N/A |
Percentage of total participants.
Table 2.
Participant test scores and comparison of means
| Measure | HPS | w/o neglect score range | w/o neglect score avg. (SD) | w/neglect score range | w/neglect score avg. (SD) | One-tailed independent samples t-test* unequal variance |
|---|---|---|---|---|---|---|
| Life Space Questionnaire | 40 | 11–36 | 24.2 (7.5) | 11–28 | 20.7 (6.8) | p = 0.160 |
| The Barthel Index | 100 | 5–100 | 92.4 (19.3) | 40–100 | 76.0 (27.3) | p = 0.127 |
| BIT | 146 | 130–146 | 142.7 (4.1) | 138–146 | 143.6 (3.4) | p = 0.278 |
| CBS via KF-NAP | 30 | 0.00 | 0.00 (0.00) | 1–6 | 3.00 (2.00) | p = 0.014 |
Notes: HPS = highest possible score; w/o = without; w/ = with; avg. = average; SD = standard deviation; sig. = significance; BIT = conventional behavioral inattention test; CBS = Catherine Bergego Scale; KF-NAP = Kessler Foundation Neglect Assessment Process.
p < .05.
Community mobility and independence
The Life Space Questionnaire
In our study (see Table 2), participants who did not meet criteria for neglect (n = 35) had a mean score of 24.2, (SD = 7.50). The participants who met criteria for neglect (n = 5) had a mean score of 20.7 (SD = 6.80). These results were consistent with previous reports of lower Life Space scores in right stroke patients with left neglect.48 Although the five participants with spatial neglect had lower scores (suggesting less mobility) the difference in scores between groups did not reach significance (p = 0.16) (one-tailed independent samples t-test with adjustment for unequal variance) (Table 2).
The Barthel Index
In the five of participants without neglect, the mean BI was 92.4 (SD = 19.3). While the mean score in the group of participants with neglect was lower (76.0, SD = 27.3), consistent with reduced independence, the difference in mean scores between groups did not reach significance (p = 0.13) (Table 2).
Discussion
This study aimed to add to the current literature by exploring the prevalence of spatial neglect in a group of chronic left-brain stroke survivors with aphasia. Individuals with aphasia are often excluded from research, because it is believed that their language impairments may impact their ability to provide informed consent and participate in the subsequent research process.30 Unfortunately, because this has reduced available systematic study of the prevalence and impact of spatial neglect after left-brain stroke in people with aphasia, many clinicians assume that spatial neglect does not occur in combination with aphasia, or that right-sided spatial neglect symptoms are rare. In the current study of community-dwelling people with aphasia, we identified 12.5% with symptoms of mild spatial neglect. This is striking, because the participants in our study were in the chronic phases of stroke recovery. The participants in our study may also have been more independent than many stroke survivors with aphasia, because they were participating in community-based activities. Thus, our sample may have underestimated the true population rate of spatial neglect after left-brain stroke.
We were able to screen participants with left-brain stroke and aphasia for symptoms of spatial neglect using an aphasia-adapted consent form process, similar to prior studies that reduced text and incorporated pictures.31 We also used questions at the end of the consent form to assess comprehension. The aphasia-adapted consent process was both easily implemented by our researcher team, and successful in enabling people with aphasia to consent to participate in research (40 of 43 people eligible were able to indicate understanding).
People with both spatial neglect and aphasia may be at a distinct disadvantage in functioning independently and self-advocating for treatment. This is why we wanted to look at the two groups and see if there was a difference between their ADL status and community independence. Based on our results, we suggest that larger studies are needed to investigate the co-occurrence of spatial neglect and aphasia after left-brain stroke. Future research should investigate the needs and priorities for rehabilitative care that are unique to this group of stroke survivors. Our findings also strongly support using adapted consent processes to include individuals with aphasia in these and other research studies.7, 31, 32, 49 Adapted informed consent processes are also likely to be needed in many medical care settings.
The small number of participants in this pilot study did not allow for us to evaluate differences in community mobility or independence, and differences between people with neglect in our study and those not having neglect did not reach significance for these parameters, our results suggest further research with larger, representative groups is needed. There may also be a need for these assessments to be changed to include questions about spatial function and communication. For example, the Life Space measure emphasizes mobility, but does not identify the cause of reduced mobility. A prior study was unclear whether difficulty with navigation, fear of getting lost or having safety problems limited community mobility directly because of the neglect being (this was with right-brain stroke and spatial neglect, relative to stroke survivors not having neglect).39 Spatial neglect has been demonstrated to be associated with lesser independence as assessed by the Barthel Index.4, 17, 45
Participants in the study met criteria for spatial neglect on the CBS, as assessed with the KF-NAP.40 No participants, however, met criteria for spatial neglect based on assessment with the BIT-C. We feel it is likely that the CBS, which is a functional performance assessment, is more sensitive to mild spatial neglect, as others suggested. 23 The CBS via the KF-NAP can detect personal neglect and also, to some extent, may assess spatial neglect in far extrapersonal space, beyond reaching distance; 48 the BIT-C is limited to peripersonal and near space assessment. The CBS via the KF-NAP may also be more “aphasia-friendly,” since the verbal instructions for this instrument are given in the context of real-life, familiar objects and situations. This may enhance comprehension of test instructions and functional communication for people with aphasia. In contrast, it is a challenge to instruct people with aphasia on aspects of the BIT-C, for example, how to draw a butterfly from memory. This is because the person may not be able to fully understand verbal language without demonstration or visual representation. The lower average scores on the BI in the spatial neglect group, consistent with “moderate dependence” (mean 76.0, SD 27.3), contrasted with the average scores consistent with “mild dependence” in the group of participants without spatial neglect (mean 92.4, SD 19.3). This suggests that spatial neglect scores were not the result of random variation (even though the results were not statistically significant). However, additional research is needed to confirm that the CBS via KF-NAP may be a more sensitive screening tool than the BIT-C in community-dwelling people with aphasia after left-brain stroke.
Limitations
The current study was limited due to the use of convenience sampling and small sample size. Although the aphasia-friendly consent process was deemed successful, three participants failed the quiz, likely due to the severity of their comprehension deficits and aphasia. Thus, it is likely not possible to include all individuals with aphasia in spatial neglect research. Additionally, while the aphasia-friendly consent form allowed most participants to understand the purpose of the study, via images and simplified text, the consenting process took more time. This could have contributed to increased frustration and fatigue of participants.
The assessments used in this study have psychometric merit, yet we encountered barriers to paper-and-pencil visuospatial testing with the BIT-C in people with aphasia, as described above. Additionally, because we performed the CBS assessment in a community aphasia center rather than the participants’ homes, participants did not have access to all of their personal belongings, such as clothing, hair brushes, and other grooming items. Increased task complexity, within the natural home environment, might have resulted in more functional performance errors consistent with spatial neglect. Lastly, we did not assess instrumental activities of daily living such as cooking, driving, taking medications, or interpreting written material for work or financial tasks, which may be problem areas for people who have aphasia and spatial neglect. Future studies should address these important community-based functions.
Conclusions
The findings suggest that further research is necessary for the accurate assessment of the prevalence of spatial neglect due to the need for including a larger, more representative group of left-brain stroke survivors with aphasia. Differences in common spatial neglect symptoms and rehabilitative needs unique to people with both spatial neglect and aphasia, impacting both simple self-care tasks, and instrumental activities of daily living, need to be studied further. Aphasia-friendly forms and communication books as accompaniments to traditional client intake documents, interviews, assessment forms, and home exercise programs can better include individuals with aphasia as active stakeholders in their care and participation in research. We strongly advise that assessment for neglect should occur regularly following a left-brain stroke, as is typical practice following a right-brain stroke. Furthermore, assessment should include direct observation of functional performance, such as the CBS via KF-NAP. Aphasia-friendly functional neglect assessments will enable health professions to reach out to all individuals with stroke and aphasia, and allow for opportunities to help individuals with stroke to live life to the fullest.
Acknowledgments
We are very grateful to the Adler Aphasia Center staff members, especially Wendy Greenspan and Karen Tucker, for their help and support. We would also like to thank the Adler Aphasia Center members for donating their time and participating in our study.
Footnotes
ORCID
Kimberly Hreha http://orcid.org/0000-0002-8277-3992
Contributors
KH conceived and designed the study, obtaining funding and ethics approval, analyzed the data, wrote the article in whole, and revised the article. CM collected and analyzed the data, wrote the article in part, and revised the article. MG, TJ, NG, LO, and AS collected and analyzed the data. GS and CD collected the data. AMB-conceived and designed the study, wrote the article in part, and revised the article.
References
- 1.Centers for Disease Control and Prevention. Prevalence of stroke-United States, 2006–2010. MMWR: Morb Mortal Wkly Rep. 2012;61(20):379–382. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Prevalence and most common causes of disability among adults – United States, 2005. MMWR: Morb Mortal Wkly Rep. 2009;58(16):421–426. [PubMed] [Google Scholar]
- 3.Riestra AR, Barrett AM. Rehabilitation of spatial neglect. Handb Clin Neurol. 2013;110:347–355. doi: 10.1016/B978-0-444-52901-5.00029-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Di Monaco M, Schintu S, Dotta M, Barba S, Tappero R, Gindri P. Severity of unilateral spatial neglect is an independent predictor of functional outcome after acute inpatient rehabilitation in individuals with right hemispheric stroke. Arch Phys Med Rehabil. 2011;92:1250–1256. doi: 10.1016/j.apmr.2011.03.018. [DOI] [PubMed] [Google Scholar]
- 5.Jehkonen M, Laihosalo M, Kettunen JE. Impact of neglect on functional outcome after stroke: a review of methodological issues and recent research findings. Restor Neurol Neurosci. 2006;24(4):209–215. [PubMed] [Google Scholar]
- 6.Wee JYM, Hopman WM. Comparing consequences of right and left unilateral neglect in a stroke rehabilitation population. Stroke. 2008;87(11):910–920. doi: 10.1097/PHM.0b013e31818a58bd. [DOI] [PubMed] [Google Scholar]
- 7.Beis JM, Keller C, Morin N, Bartolomeo P, Bernati T, Chokron S, et al. Right spatial neglect after left hemisphere stroke: qualitative and quantitative study. Neurology. 2004;63(9):1600–1605. doi: 10.1212/01.wnl.0000142967.60579.32. [DOI] [PubMed] [Google Scholar]
- 8.Chen R, Maniscalco JS, Williamson DS, Barrett AM. Assessment of spatial neglect and spatial biases in left brain stroke survivors. [Abstract] Neurology. 76(9 Suppl 4):A502. Abstract presented at the American Academy of Neurology Annual Meeting; 2011 Apr; Honolulu, HI. [Google Scholar]
- 9.Kleinman JT, Newhart M, Davis C, Heidler-Gary J, Gottesman RF, Hillis AE. Right hemispatial neglect: frequency and characterization following acute left hemisphere stroke. Brain and Cognition. 2007;64(1):50–59. doi: 10.1016/j.bandc.2006.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bultitude JH, Rafal RD. Amelioration of right spatial neglect after visuo-motor adaptation to leftward-shifting prisms [Supplemental material] Cortex. 2010;46:404–406. doi: 10.1016/j.cortex.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Branch Coslett HB, Schwartz MF, Goldberg G, Haas D, Perkins J. Multi-modal hemispatial deficits after left hemisphere stroke. Brain. 1993;116(3):527–554. doi: 10.1093/brain/116.3.527. [DOI] [PubMed] [Google Scholar]
- 12.van Dijck J-P, Gevers W, Lafosse C, Fias W. Right-sided representational neglect after left brain damage in a case without visuospatial working memory deficits. Cortex. 2013;49(9):2283–2293. doi: 10.1016/j.cortex.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 13.Fortis P, Chen P, Goedert K, Barrett AM. Effects of prism adaptation on motor-intentional spatial bias in neglect. NeuroReport. 2011;22(14):700–705. doi: 10.1097/WNR.0b013e32834a3e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fortis P, Goedert KM, Barrett AM. Prism adaptation differently affects motor-intentional and perceptual-attentional biases in healthy individuals. Neuropsychologia. 2011;49:2718–2727. doi: 10.1016/j.neuropsychologia.2011.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rode G, Klos T, Courtois-Jacquin S, Rosetti Y, Pisella L. Neglect and prism adaptation: a new therapeutic tool for spatial cognition disorders. Restor Neurol Neurosci. 2006;24:347–356. [PubMed] [Google Scholar]
- 16.Turton AJ, O’Leary K, Gabb J, Woodward R, Gilchrist ID. A single blinded randomised controlled pilot trial of prism adaptation for improving self-care in stroke patients with neglect. Neuropsychol Rehabil. 2010;20(2):180–196. doi: 10.1080/09602010903040683. [DOI] [PubMed] [Google Scholar]
- 17.Barrett AM, Goedert KM, Basso JC. Prism adaptation for spatial neglect after stroke: translational practice gaps. Nat Rev Neurol. 2012;8(10):567–577. doi: 10.1038/nrneurol.2012.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bisiach E, Luzzatti C. Unilateral neglect of representational space. Cortex. 1978;14(1):129–133. doi: 10.1016/s0010-9452(78)80016-1. [DOI] [PubMed] [Google Scholar]
- 19.Fortis P, Maravita A, Gallucci M, Ronchi R, Grassi E, Senna I, et al. Rehabilitating patients with left spatial neglect by prism exposure during a visuomotor activity. Neuropsychology. 2010;24(6):681–697. doi: 10.1037/a0019476. [DOI] [PubMed] [Google Scholar]
- 20.Fullerton KJ, McSherry D, Stout RW. Albert’s test: a neglected test of perceptual neglect. The Lancet. 1986;327(8478):430–432. doi: 10.1016/s0140-6736(86)92381-0. [DOI] [PubMed] [Google Scholar]
- 21.McGlone J, Losier BJ, Black SE. Are there sex differences in hemispatial visual neglect after unilateral stroke? Neuropsychiatry, Neuropsychol Behav Neurol. 1997;10(2):125–134. [PubMed] [Google Scholar]
- 22.Ringman JM, Saver JL, Woolson RF, Clarke WR, Adams HP. Frequency, risk factors, anatomy, and course of unilateral neglect in an acute stroke cohort. Neurology. 2004;63(3):468–474. doi: 10.1212/01.wnl.0000133011.10689.ce. [DOI] [PubMed] [Google Scholar]
- 23.Stone SP, Wilson B, Wroot A, Halligan PW, Lange LS, Marshall JC, Greenwood RJ. The assessment of visuo-spatial neglect after acute stroke. J Neurol Neurosurg Psychiatry. 1991;54(4):345–350. doi: 10.1136/jnnp.54.4.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bowen A, McKenna K, Tallis RC. Reasons for variability in the reported rate of occurrence of unilateral spatial neglect after stroke. Stroke. 1999;30(6):1196–1202. doi: 10.1161/01.str.30.6.1196. [DOI] [PubMed] [Google Scholar]
- 25.Goedert KM, Chen P, Botticello A, Masmela JR, Adler U, Barrett AM. Psychometric evaluation of neglect assessment reveals motor-exploratory predictor of functional disability in acute-stage spatial neglect. Arch Phys Med Rehabil. 2012;93:137–142. doi: 10.1016/j.apmr.2011.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.National Aphasia Association. Aphasia definitions. 2015 Available from http://www.aphasia.org/aphasia-definitions/
- 27.Arene NE, Hillis AE. Rehabilitation of unilateral spatial neglect and neuroimaging. Europa Medicophysica. 2007;43(2):255–269. [PubMed] [Google Scholar]
- 28.Meinzer M, Djundja D, Barthel G, Elbert T, Rockstroh B. Long-term stability of improved language functions in chronic aphasia after constraint-induced aphasia therapy. Stroke. 2005;36(7):1462–1466. doi: 10.1161/01.STR.0000169941.29831.2a. [DOI] [PubMed] [Google Scholar]
- 29.Brady MC, Fredrick A, Williams B. People with aphasia: capacity to consent, research participation and intervention inequalities. Int J Stroke. 2013;8(3):193–196. doi: 10.1111/j.1747-4949.2012.00900.x. [DOI] [PubMed] [Google Scholar]
- 30.Kagan A, Kimelman MDZ. Informed consent in aphasia research: myth or reality? Clin Aphasiology. 1995;23:65–75. [Google Scholar]
- 31.Brennan A, Worrall L, McKenna K. The relationship between specific features of aphasia-friendly written material and comprehension of written material for people with aphasia: an exploratory study. Aphasiology. 2005;19(8):693–711. [Google Scholar]
- 32.Heilman KM, Watson RT, Gonzalez-Rothi LJ. Praxis. In: Goetz CG, editor. Textbook of clinical neurology. 3. Philadelphia, PA: Saunders Elsevier; 2007. pp. 55–62. [Google Scholar]
- 33.Wilson B, Cockburn J, Halligan P. Development of a behavioral test of visuospatial neglect. Arch Phys Med Rehabil. 1987;68(2):98–102. [PubMed] [Google Scholar]
- 34.Chen P, Hreha K, Fortis P, Goedert K, Barrett A. Functional assessment of spatial neglect: a review of the Catherine Bergego scale and an introduction of the Kessler foundation neglect assessment process. Top Stroke Rehabil. 2012;19(5):423–435. doi: 10.1310/tsr1905-423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Azouvi P, Marchal F, Samuel C, Morin L, Renard C, Bergego C. Functional consequences and awareness of unilateral neglect: study of an evaluation scale. Neuropsychol Rehabil. 1996;6(2):133–150. [Google Scholar]
- 36.Azouvi P, Samuel C, Louis-Dreyfus A, Bernati T, Bartolomeo P, Beis JM, et al. Sensitivity of clinical and behavioural tests of spatial neglect after right hemisphere stroke. J Neurol Neurosurg Psychiatry. 2002;73(2):160–166. doi: 10.1136/jnnp.73.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Azouvi P, Bartolomeo P, Beis JM, Perennou D, Pradat-Diehl P, Rousseaux M. A battery of tests for the quantitative assessment of unilateral neglect. Restor Neurol Neurosci. 2006;24:273–285. [PubMed] [Google Scholar]
- 38.Halligan PW, Cockburn J, Wilson BA. The behavioural assessment of visual neglect. Neuropsychol Rehabil. 1991;1(1):5–32. [Google Scholar]
- 39.Chen P, Hreha K. Kessler foundation neglect assessment process: KF-NAP 2015 manual. West Orange, NJ: Kessler Foundation; 2015. [Google Scholar]
- 40.Chen P, Chen C, Hreha K, Goedert KM, Barrett AM. Kessler foundation neglect assessment process uniquely measures spatial neglect during activities of daily living. Arch Phys Med Rehabil. 2015;96:869–876. doi: 10.1016/j.apmr.2014.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stalvey BT, Owsley C, Sloane ME, Ball K. The life space questionnaire: a measure of the extent of mobility of older adults. J Appl Gerontol. 1999;18(4):460–478. [Google Scholar]
- 42.Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Md State Med J. 1965;14:61–65. [PubMed] [Google Scholar]
- 43.Baker PS, Bodner EV, Allman RM. Measuring life-space mobility in community-dwelling older adults. J Am GeriatrSoc. 2003;51(11):1610–1614. doi: 10.1046/j.1532-5415.2003.51512.x. [DOI] [PubMed] [Google Scholar]
- 44.Lewis C, Shaw K. The (original) Barthel index of ADLs. Geriatr Funct. 2006;17(21):8. [Google Scholar]
- 45.Shah S, Vanclay F, Cooper B. Improving the sensitivity of the Barthel index for stroke rehabilitation. J Clin Epidemiol. 1989;42(8):703–709. doi: 10.1016/0895-4356(89)90065-6. [DOI] [PubMed] [Google Scholar]
- 46.Hsueh IP, Lee MM, Hsieh CL. Psychometric characteristics of the Barthel activities of daily living index in stroke patients. J Formos Med Assoc. 2001;100(8):526–532. [PubMed] [Google Scholar]
- 47.Hartman-Maeir A, Katz N. Validity of the behavioral inattention test (BIT): relationships with functional tasks. Am J Occup Ther. 1995;49:507–516. doi: 10.5014/ajot.49.6.507. [DOI] [PubMed] [Google Scholar]
- 48.Oh-Park M, Hung C, Chen P, Barrett AM. Severity of spatial neglect during acute inpatient rehabilitation predicts community mobility after stroke. PMR. 2014;6(8):716–722. doi: 10.1016/j.pmrj.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Plummer P, Morris ME, Dunai J. Assessment of unilateral neglect. Phys Ther: J Am Phys Ther Assoc. 2003;83(8):732–740. [PubMed] [Google Scholar]