Abstract
To determine the relationships among body mass index (BMI), and HIV-associated neurocognitive impairment and the potential mediating effects of inflammatory cytokines. Among the HIV-infected individuals (N=90) included in this study, obesity was associated with slower processing speed (β = −.229, standard error (SE) = 2.15, p = .033), compared to participants with a normal BMI, after controlling for psychosocial and HIV clinical factors. Serum concentrations of the interleukin-16 (IL-16) cytokine were significantly associated with slowed processing speed (β = −.235, standard error (SE) = 1.62, p = .033) but did not mediate the relationship between obesity and processing speed These findings suggest that obesity may contribute to cognitive processing speed deficits in HIV-infected adults. Elevated concentrations of IL-16 are also associated with slowing, though the results suggest that obesity and IL-16 may exert independent effects.
Keywords: HIV, Cytokines, Inflammation, Body mass index, Neurocognition
1. Introduction
HIV-infected people are living longer (Yeni, 2006) with life expectancy approaching that of the general population(Samji et al., 2013). Accordingly, the focus of clinical care has shifted to the management of a chronic illness. Many HIV-infected people have particular concern that as they live longer they may experience HIV-Associated Neurocognitive Disorders (HAND)(Antinori et al., 2007; Heaton et al., 2010). HAND has been shown to significantly interfere with activities of daily living such as driving, financial management, and adherence to medication regimens (Heaton et al., 2004; Thames et al., 2013). HIV-infection is associated with the release of neurotoxic pro-inflammatory cytokines which are hypothesized to play a role in the pathogenesis of HAND (Lindl et al., 2010; Yuan et al., 2013). Thus, it is important to identify risk factors and mechanisms for the development of cognitive impairment in HIV-infected people.
Comorbid conditions in HIV-infected adults such as depressive symptoms, substance use, and hepatitis C infection significantly affect neurocognitive function(Fialho et al., 2013; Grant, 2008; Martin-Thormeyer and Paul, 2009). HIV-related factors, including HIV-RNA level and CD4 nadir, also negatively impact on neurocognition (Childs et al., 1999; Ferrando et al., 1998). Additionally, emerging evidence suggests a high prevalence of overweight and obesity among HIV-infected adults, ranging from 17% to 32% (Crum-Cianflone et al., 2010; Kim et al., 2012; Mariz et al., 2011). Previous research has linked overweight and obesity to diminished performance on tests of executive functioning, verbal fluency, motor speed, and memory (Gunstad et al., 2010, 2007; Sabia et al., 2009; Waldstein and Katzel, 2006). However, few studies have investigated the association between obesity or overweight and neurocognitive impairment among HIV-infected adults.
Overweight and obesity is associated with cardiometabolic factors such as hypertension and diabetes, which are in turn associated with neurocognitive impairment and as such has been proposed as a potential pathway whereby overweight and obesity may adversely impact neurocognitive function(Dahl and Hassing, 2012; Smith et al., 2011). However, previous studies have found that the relationship between overweight and obesity and neurocognitive impairment is not attenuated when accounting for cardiometabolic factors, suggesting that other potential pathways may explain this relationship(Dahl et al., 2010, 2013). Recent investigations hypothesize that increased body fat is associated with the production and release of a variety of pro-inflammatory cytokines (Cottam et al., 2004; Fantuzzi, 2005). Elevated pro-inflammatory cytokines are also related to neurocognitive impairment in older adults and individuals with mild cognitive impairment, Alzheimer’s disease, and Parkinson’s disease (Galimberti et al., 2006; Magaki et al., 2007; Menza et al., 2010; Schram et al., 2007; Yaffe et al., 2003). Studies among HIV-infected adults have also demonstrated an inverse relationship between levels of inflammatory cytokines (IL-6, TNF-α, and IFN-γ) and performance on neuropsychological tests of memory, executive functioning, and processing speed (Cohen et al., 2011; Pedersen et al., 2013; Woods et al., 2006). However the current literature is contradictory, as reduced concentrations of IL-1-β and IL-18 have been correlated with poorer performance on tasks of executive functioning (Cohen et al., 2011).
The current investigation extends previous work by examining whether an overweight or obese BMI is associated with neurocognitive impairment in a sample of HIV-infected adults receiving ART. Additionally, we examined whether pro-inflammatory factors mediate this relationship. We hypothesized that obesity will be associated with worse performance on tasks of processing speed, executive function, learning, and memory and that these associations will be mediated by pro-inflammatory cytokines.
2. Material and Methods
2.1. Participants and Procedures
Participants were 125 HIV-infected adults recruited between 2007 and 2010 as part of a larger NIH-sponsored longitudinal study of HIV-associated brain dysfunction at The Miriam Hospital/Brown University. Detailed description of the study participants have been previously published (Devlin et al., 2012). The study was approved by the institutional review boards of The Miriam Hospital and Brown University, and informed consent was obtained from each participant before enrollment. Of the total sample, 15 did not undergo a neurological assessment and 20 did not have data on cytokines; thus the sample for the present analysis included 90 HIV-infected adults. There were no significant differences in the distribution of age, gender, race, education and BMI status between the participants excluded (n=35) and those included (n=90) in the final study sample. HIV infection was documented by enzyme-linked immunosorbent assay (ELISA) and confirmed by Western blot test. Exclusionary criteria for the parent study were as follows: history of (1) head injury with loss of consciousness longer than 10 minutes, (2) history of neurological conditions including dementia, seizure disorder, stroke, and opportunistic infection of the brain (e.g., neurosyphilis), (3) severe psychiatric illness that might impact brain function, (e.g., schizophrenia), and (4) current (6-month) substance dependence or positive urine toxicology screen for cocaine, opiates, or illicit stimulants or sedatives.
2.2. Measures
2.2.1. Demographic characteristics
Race (White/non-White), age in years, gender, and education completed (Less than high school/High school/Greater than high school) were obtained through self-report.
Physiological and clinical measures
Body mass index (BMI) was obtained via the most recent medical history examination and was categorized according to the Centers for Disease Control and Prevention guidelines (CDC, 2014)(“Obesity and Overweight for Professionals,” n.d.) as normal (< 24.9 kg/m2), overweight (25 – 29.9 kg/m2), and obese (BMI ≥ 30 kg/m2). We did not include an underweight category (i.e. <18.5 kg/m2) due to the small number participants (n=2). The medical record was used to obtain information about duration of HIV-infection in years, CD4 nadir, current CD4, and current ART use. Current hepatitis C (HCV) infection was defined as detectable serum HCV RNA by PCR.
2.2.2. Cytokine measurement
Plasma blood samples for each participant were obtained once during the parent study on the same day that their neurocognitive assessment was performed. Plasma was separated from participant’s blood samples and cytokine levels were measured using the xMAP multiplexed bead array immunoassay with florescence intensity measured using the Luminex-100 system (Luminex Corp., Austin, TX). Table 4 displays the seven pro-inflammatory (TNF-α, INF-γ, IL-1, IL-6, IL-8, IL-16, and IL-18) and anti-inflammatory (IL-10) cytokines used and their associated functions.
Table 4.
Characteristics of cytokinesa
| Name | Source | Biological role |
|---|---|---|
| Interleukin – 18 (IL-18) | Produced by macrophages and monocytes | Pro-inflammatory cytokine interacts with IL-12 to induce cell-mediated immune response with microbial infection and LPS, inducing severe inflammatory reactions. Stimulates NK and T cell release of IFN-γ, which activates macrophages. |
| Interleukin – 8 (IL-8) | Produced macrophages and some epithelial and endothelial cells | Role in innate immune response. Major role in chemotaxis of Neutrophils. Also mediates inflammatory response and angiogenesis. |
| Interleukin – 1-beta (IL-1β) | Produced by activated macrophages | Mediates inflammatory responses, cell proliferation, apoptosis. Induces Cox-2 in CNS, causing inflammatory pain. |
| Interleukin – 10 (IL-10) | Produced by monocytes. Pleiotropic cytokine | An anti-inflammatory cytokine, it inhibits macrophage and dendritic cell function, suppresses TNF-α. Acquires pro-inflammatory activity during immune response with IFN-α stimulation. |
| Interferon gamma-soluble cytokine (IFN-γ) | Produced by innate NK cells, acquired antigen-specific cytotoxic CD4+ and effector CD8+ T cells. | Activates macrophages and critical for innate and adaptive immune responses to intracellular pathogens, tumor control, and inhibition of viral replication. |
| Tumor Necrosis factor-alpha (TNF-α) | Secreted by macrophages, monocytes, neutrophils, T cells, NK cells after stimulation with LPS. | CD4+ cells secrete TNF-α. Also made by astrocytes, microglial cells, smooth muscle cells, and fibroblasts. Mediates systemic inflammation, inhibits viral replication, and inhibits tumorigenesis. |
| Interleukin – 6 (IL-6) | Secreted by T cells and macrophages; | Triggers inflammation, acute phase response, fever. Anti-inflammatory effects include inhibiting TNF-α and IL-1, and activating IL-1ra and IL-10 |
2.2.3. Neurocognitive assessments
The following domains of neurocognitive functioning was assessed: speed of information processing, attention/working memory/executive functioning, learning, memory, and psychomotor speed. The battery was comprised of the following tests, which were chosen for their sensitivity to HAND: Hopkins Verbal Learning Test – Revised(Benedict et al., 1998, 1996); Brief Visuospatial Memory Test –Revised(Benedict, 1997); Controlled Oral Word Association Test(Benton et al., 1994); Stroop Color and Word Test(Golden, n.d.); Trail Making Test, Parts A and B(Reitan, 1992); Grooved Pegboard Test(Kløve, 1963); and the Digit Symbol – Coding, Symbol Search, and Letter-Number Sequencing tests from the Wechsler Adult Intelligence Scale – Third Edition(Wechsler, 1997). Demographically corrected t-scores were calculated using established norms(Benedict et al., 1998, 1996; Heaton et al., 2004). Domain composite scores were calculated by averaging the t-scores of all tests in the domain. Deficit scores were calculated for all domains and domain specific tests using a range of 0–5 for each encompassing cognitive test [0 (t score > 40, 1 (t score < 40), 2 (t score < 35), 3 (t score < 30), 4 (t score < 25), 5 (t score < 20] and then averaging the domain test scores, in order to calculate the total domain deficit score.
2.2.4. Psychosocial measure
The Center for Epidemiologic Studies Depression (CES-D) scale, was used to measure clinically significant symptoms of depression(Radloff, 1977). The Mini-International Neuropsychiatric Interview (M.I.N.I.) was used to assess lifetime substance abuse or dependence(Sheehan et al., 1998). We further classified lifetime substance abuse/dependence based on type of substance (no abuse/dependence; alcohol abuse/dependence only; illicit substance abuse/dependence only; alcohol and illicit substance abuse/dependence).
2.3. Statistical Analysis
Demographic characteristics, HIV-related clinical and psychosocial measures, cytokines, and neurocognitive assessments were compared by BMI status using Chi-square for categorical variables and analysis of variance (ANOVA) for continuous variables. As cytokine measurements were conducted once for each participant across the three assessment periods, the time point of cytokine data collection was used to assess neurocognitive outcomes, BMI status, and covariate assessments. A variable was created to indicate which time point was used to control for potential confounding. Multivariable linear regressions were conducted to assess the effect of BMI status on each neurocognitive domain, without inclusion of inflammatory cytokines. Covariates included in the models include: lifetime substance abuse and dependence, current antiretroviral treatment, current HCV infection, duration of HIV infection, CD4 nadir, and depressive symptoms. As demographically corrected t-scores were used in analyzing the neurocognitive domains, gender, race, and age were not included in the multivariable linear regressions to prevent over adjustment of effects. If a significant relationship (p≤.05) was found between adjusted BMI status and a specific neurocognitive domain, post hoc hierarchical regressions including the cytokines were conducted. Cytokines and CD4 nadir were natural logarithm transformed to approximate to a normal distribution. Cytokines were entered into a starting model before exclusion of the least significant in a backwards stepwise manner and the model a significant p-value for cytokine was retained. Once the final model was chosen, a mediation assessment of the direct and indirect effect of BMI status, through the set of plasma cytokines, on specific neurocognitive functions domains was conducted using bootstrapping methods, adjusting for covariates (Hayes and Preacher, 2014). All statistical analyses were conducted in SPSS software (IBM).
3. Results
3.1. Demographic and Clinical Characteristics
The sample consisted of 90 HIV-infected adults, with a mean age of 46 years, 35.6% were male, and 64.4% were white. Majority completed high school (41.1%) or some college (40.0%) and most were receiving ART (86.7%). Twenty percent of the sample had no lifetime history of substance abuse or dependence. Mean CD4 nadir was 188.2 cells/mm3 and about 34% had a current HCV co-infection. Figure 1 displays the distribution of BMI values by each BMI category. About 46% of the sample was within a normal BMI range (18.5–24.9), 37% were overweight (25–29.9), and 15% were obese (> 29.9).
Figure 1.
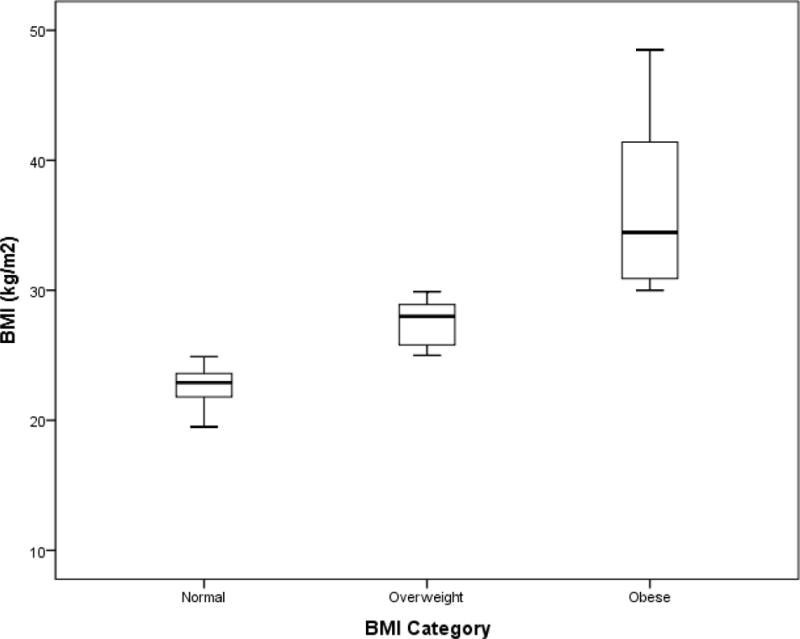
Boxplot of BMI stratified by BMI category among 90 HIV-Infected Individuals
Processing speed was the only neurocognitive domain that significantly differed by BMI status (Table 2; p<.05). Those of normal weight featured the best functioning on processing speed. Thus, subsequent multivariable analysis focused on processing speed.
Table 2.
Multivariable linear regression of the association between BMI and processing speed.
| Regression coefficient | SE | Standardized β | p-value | |
|---|---|---|---|---|
| BMI | ||||
| Overweight vs. Normal | −1.82 | 1.68 | −.188 | .282 |
| Obese vs. Normal | −5.19 | 2.19 | −.254 | .021 |
| Current ARTa | ||||
| Yes vs. No | 4.39 | 2.71 | .201 | .110 |
| HIV Duration | 0.169 | .123 | .158 | .175 |
| CD4 Nadir | 0.009 | .005 | .202 | .089 |
| Current Hepatitis C Infection | ||||
| Yes vs. No** | −6.88 | 1.91 | −.436 | .001 |
| Abuse/Dependence – Lifetime | ||||
| Alcohol Only vs. None | −2.42 | 2.55 | −.118 | .346 |
| Illicit Only vs. None | 2.37 | 2.50 | .135 | .345 |
| Alcohol and Illicit Only vs. None | 4.06 | 2.34 | .267 | .087 |
| Depression (CESDb) | −.084 | .061 | −.145 | .171 |
p< .05,
p<.0001,
SE = standard error, CESD = Centers for Epidemiologic Studies Depression Scale;
Antiretroviral Therapy
3.2. Effect of BMI status on processing speed
Compared to those of normal weight, obesity was significantly associated with poorer processing speed [Standardized (β) = −.254, SE=2.19, p= .021, Table 2]; overweight was not significantly associated with processing speed (β = −.188, SE=1.68, p= .28). In this model, current HCV was associated with slowed processing speed (β = −.436, SE=1.91, p= .001). In secondary analysis that excluded subjects with a current HCV infection (n=31), an obese BMI was not associated with slowed processing speed (β = −1.587, SE = 2.68, B=−.084, p = .558).
3.3. Inflammatory cytokines, obesity and processing speed
The best fitting model from the hierarchical multivariable linear regression included only the inflammatory biomarker IL-16 which was found to be associated with processing speed (β = −.235, p= .033).While the effect of obesity was not reduced to non-significance, it seemed that IL-16 could be a partial mediator in this relationship. In accordance with showing evidence that the indirect effect is significantly difference from zero supports the potential for a mediation effect(Hayes and Preacher, 2014).
3.4. Mediation Analysis
In the mediation analysis to investigate the role of IL-16 in the relationship between obesity and processing speed, the results for the obese model, demonstrated a significant total effect of obesity (compared to normal weight) on processing speed (β = −.563, p = .033) and a significant direct effect of IL-16 on processing speed (β = −.491, p= .038). However, the indirect effects via IL-16 was not significant (β = −.0200, p>.05).
4. Discussion
The current findings suggest that both obesity and systemic inflammation may contribute to cognitive dysfunction among HIV-infected adults. People who met CDC criteria for obesity exhibited slowed cognitive processing compared to people whose weight was within the normal range. This was not the case for HIV-infected adults with elevated BMI that was below the threshold for obesity (i.e., overweight). Slowed processing speed among obese HIV-infected adults is consistent with findings from a number of other studies of obesity and cognition conducted in HIV seronegative cohorts (Dahl et al., 2013; Hassing et al., 2010; Stanek et al., 2013).
Past studies of obesity among HIV-infected adults have suggested a more complex relationship between elevated BMI, obesity and neurocognitive impairment in HIV (Gustafson et al., 2013; McCutchan et al., 2012). McCutchan et al., 2012, found a protective effect of increased BMI on an overall global measure of neurocognitive impairment, whereas higher waist circumference, was predictive of neurocognitive impairment after correcting for a diagnosis of AIDS or diabetes and serum triglycerides among 130 participants of the CHARTER study(McCutchan et al., 2012; Sattler et al., 2014). However, this study did not assess specific cognitive domains by BMI status. In another study, where specific neurocognitive domains where assessed, there was no significant association between obesity at mid-life, compared to normal weight on measures of processing speed, among HIV-infected women. However, the authors found that obesity was associated better performance on the Trail Making Test B, but worse performance on the Stroop Interference task(Gustafson et al., 2013) – both measures of executive function. The contrasting findings may be explained by differences in the study samples, such as HIV-disease history, as well as the presence of other cardiometabolic factors, and other comorbidities, including HCV co-infection.
The association between obesity and slowed cognitive processing could occur from a number of pathophysiological factors linked to obesity. Increased systemic inflammation has been well described in past studies of obesity. It is well established that overweight or obesity is associated with a chronic low-grade systemic inflammation(Gregor and Hotamisligil, 2011). This pro-inflammatory profile is associated with the release of neurotoxic pro-inflammatory cytokines, which reach the brain and initiate local inflammation as well as microglial proliferation which may be associated synaptic remodeling and neuronal health which may influence cognitive function(Miller and Spencer, 2014). Notably, obesity and IL-16 concentrations were associated with slowed cognitive processing in this study. Findings were in accord with prior evidence of a relationship between IL-16 and attention-executive, learning and memory, and psychomotor speed among HIV-infected adults (Cohen et al., 2011; Correia et al, 2013). This finding suggests that both obesity and systemic inflammation may adversely affect neurocognitive performance among HIV-infected adults. Initial hierarchical regression analyses examining all of the pro-inflammatory cytokines suggested that only IL-16 might be a potential mediator of this relationship. Yet, a significant indirect relationship between obesity and processing speed via IL-16 concentrations was not observed in our mediation analysis.
While we expected to find that IL-16 mediated the association between obesity and cognitive processing, the lack of a mediation effect is not altogether surprising. Increased systemic inflammation occurs not only as a function of obesity, but also secondary to various factors that affect immune response, including HIV itself. Furthermore, systemic inflammation is but one of potential pathway that may mediate the relationship between obesity and cognition.
Obesity also leads to alterations in glucose and insulin metabolism, vascular function and hormonal factors (Sharma & Kavuru, 2010). In sum, the effects of obesity on cognition may occur as a byproduct of various cardiometabolic factors (e.g., leptin and adiponectin) that also play a role in brain health(Sturman et al., 2008). Furthermore, BMI alone may not be the best determinant of obesity-related health risk. Increased waist circumference, quantity of subcutaneous and/or liver adipose tissue, vascular comorbidity, and the presence of metabolic syndrome or diabetes have all been linked to brain dysfunction (Singh et al., 2004). Nonetheless, the fact that IL-16 and no other inflammatory cytokine remained in the model suggests the possibility of other complex pathways other than inflammation. Among multifaceted interactions, IL-16 binds to CD4 co-receptors and selectively chemoattracts CD4+ T Th1 cells. This interaction can impact on viral replication because of their close relationship with CCR5(Skundric et al., 2006). Finally, in animal models IL-16 has been associated with both glucose metabolism and risk of diabetes, which can explain our observations(Meagher et al., 2010). Unfortunately, our study lacked information about glycemic profile and diabetes limiting our capacity to pursue additional analyses. In summary, IL-16 deserves additional research to dissert the mechanisms mediating the close relationship between IL-16 and cognitive impairments among HIV-infected persons.
There are some limitations to the current study. Its cross-sectional design limits the ability to infer casual associations. The current study was not originally designed or powered to examine obesity effects per se, but rather these findings emerged in the context of a project aimed at characterizing factors influencing the interaction of HIV and aging on brain function and cognitive performance. Also, our sample was relatively small to detect significant differences in some of the neurocognitive domains and for mediation analysis, thus it is possible that with a much larger sample; pro-inflammatory cytokines would have been shown to have some mediational effect on the relationship between obesity and cognition. In the current study HCV infection emerged a strong predictor of slowed processing speed (Table 2). This result is consistent with prior research suggesting that HIV/HCV coinfection is associated with poorer cognitive function (Fialho et al., 2015). Also, in the present study, those in the normal BMI group more likely to have completed high school or more than the other groups. Thus it is possible that our results may have been influenced by HCV infection and education, but the small sample size precluded from testing interactions. Furthermore, our sample was predominantly female and included a high proportion of individuals with a history of alcohol/illicit substance abuse/dependence.
5. Conclusion
The current findings suggest an association between obesity and slowed cognitive processing in a sample of HIV-infected adults. Concentrations of IL-16, a systemic pro-inflammatory cytokine were also associated with slowed cognitive processing, but did not mediate the relationship obesity and slowed processing speed. The results suggest that obesity and IL-16 may exert independent influences on cognitive performance. Future longitudinal studies specifically designed to examine the association between obesity and HIV-associated brain dysfunction that employ a larger and more diverse sample are needed to achieve greater understanding of the complex relationships between obesity, inflammatory processes, and cognitive performance among HIV-infected adults.
Table 1.
Characteristics of study participants by BMI status
| Characteristics | Normal (n=42) |
Overweight (n=34) |
Obese (n=14) |
Total (n=90) |
|---|---|---|---|---|
| Mean (SD) | ||||
|
| ||||
| Age (in years) | 47 (10.4) | 45.3 (9.4) | 44.3 (5.7) | 45.9 (9.4) |
| HIV Duration (in years) | 13.8 (7.4) | 13.3 (6.5) | 12.7 (7.5) | 13.5 (7.0) |
| CD4 Nadir (cells/mm3) | 202.0 (163.6) | 163.1 (162.4) | 208.4 (166.9) | 188.2 (163) |
| Current CD4 (cells/mm3)* | 404.7 (192.7) | 533.4 (283.2) | 499.8 (269.9) | 467.0 (247.3) |
| Depression (CESDa) | 17.9 (11.5) | 16.3 (14.1) | 23.4 (13.4) | 18.1 (12.9) |
|
| ||||
| Frequency (%) | ||||
|
| ||||
| Gender** | ||||
| Male | 34 (19.0) | 19 (44.1) | 5 (64.3) | 32 (35.6) |
| Female | 8 (81.0) | 15 (55.9) | 9 (35.7) | 58 (64.4) |
| Race | ||||
| White | 29 (69.0) | 21 (61.8) | 8 (57.1) | 58 (64.4) |
| Non-White | 13 (31.0) | 13 (38.2) | 6 (42.9) | 32 (35.6) |
| Education*† | ||||
| < High school | 4 (9.5) | 10 (29.4) | 3 (21.4) | 17 (18.9) |
| High school | 16 (38.1) | 15 (44.1) | 6 (42.9) | 37 (41.1) |
| > High school | 22 (52.4) | 9 (26.5) | 5 (35.7) | 36 (40.0) |
| Current ARTb | ||||
| No | 7 (16.7) | 3 (8.8) | 2 (14.3) | 12 (13.3) |
| Yes | 35 (83.3) | 31(91.2) | 12 (85.7) | 78 (86.7) |
| Current Hepatitis C Infection | ||||
| No | 31 (73.8) | 20 (58.8) | 8 (57.1) | 59 (65.6) |
| Yes | 11 (26.2) | 14 (41.2) | 6 (42.9) | 31 (34.4) |
| Abuse/Dependence – Lifetime | ||||
| None | 7 (16.7) | 10 (29.4) | 1 (7.1) | 18 (20.0) |
| Alcohol Only | 10 (23.8) | 2 (5.9) | 2 (14.3) | 14 (15.6) |
| Illicit Drugs Only | 9 (21.4) | 8 (23.5) | 4 (28.6) | 21 (23.3) |
| Alcohol and Illicit Drugs | 16 (38.1) | 4 (41.2) | 7 (50.0) | 37 (41.1) |
|
| ||||
| Mean (SD) | ||||
|
| ||||
| Inflammatory Biomarkersc | ||||
| IL-1β | 2.07 (0.69) | 1.93 (0.49) | 2.05 (0.47) | 2.02 (0.58) |
| TNF-α | 1.94 (0.41) | 1.83 (0.42) | 1.92 (0.39) | 1.90 (0.41) |
| IL-16 | 4.03 (0.48) | 4.03 (0.53) | 4.07 (0.48) | 4.03 (0.50) |
| IL-8 | 3.31 (0.93) | 3.08 (0.57) | 3.24 (0.57) | 3.22 (0.76) |
| IFN-γ | 1.49 (0.53) | 1.38 (0.51) | 1.45 (0.39) | 1.44 (0.50) |
| IL-10 | 2.95 (0.26) | 2.89 (0.36) | 2.95 (0.32) | 2.93 (0.31) |
| IL-18 | 4.50 (0.76) | 4.35 (0.90) | 4.57 (0.92) | 4.46 (0.83) |
| IL-6 | 2.30 (0.85) | 2.15 (0.64) | 2.53 (0.53) | 2.29 (0.74) |
| Neurocognitive Domainsc | ||||
| Speed* | 49.9 (7.5) | 48.0 (7.4) | 44.4 (6.6) | 48.3 (7.5) |
| Attention and Executive | 49.4 (5.6) | 47.6 (5.5) | 46.0 (4.8) | 48.2 (5.5) |
| Learning | 40.8 (12.3) | 42.7 (11.0) | 40.5 (10.7) | 41.4 (11.5) |
| Memory | 39.9 (14.8) | 42.5 (13.4) | 41.8 (12.2) | 41.2 (13.8) |
p< .05,
p<.01,
Fisher’s Exact Test,
SD = standard deviation,
Centers for Epidemiologic Studies Depression Scale;
Antiretroviral Therapy,
Values are natural logarithm-transformed.
Acknowledgments
Primary support for this project came from the National Institutes of Mental Health, R01 MH074368 “Age Effects on HIV-Associated Brain Dysfunction” and the National Institute of Alcohol Abuse and Alcoholism (NIAAA; P01 AA019072) to Dr. Cohen. The McKnight Brain Research Foundation also provides an endowment to Dr. Cohen which supports his Center for Cognitive Aging and Memory at UF. Dr. Cook also received support from NIAAA, U24AA02002 (Robert Cook, PI). This research was facilitated by the infrastructure and resources provided by the Brown University Center for Alcohol and Addiction Studies (P01 AA019072) and the Lifespan/Tufts/Brown Center for AIDS Research (P30 AI042853), and also The Miriam Hospital Infectious Medicine Clinic. The authors would like to thank our participants who graciously volunteered their time. Chukwuemeka Okafor received support from NIDA, F31DA03981 (Chukwuemeka Okafor).
Footnotes
Conflicts of Interest
None declared
References
- Antinori A, Arendt G, Becker JT, Brew BJ, Byrd DA, Cherner M, Clifford DB, Cinque P, Epstein LG, Goodkin K, Gisslen M, Grant I, Heaton RK, Joseph J, Marder K, Marra CM, McArthur JC, Nunn M, Price RW, Pulliam L, Robertson KR, Sacktor N, Valcour V, Wojna VE. Updated research nosology for HIV-associated neurocognitive disorders. Neurology. 2007;69:1789–1799. doi: 10.1212/01.WNL.0000287431.88658.8b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benedict RHB. Brief Visuospatial Memory Test - Revised. 1997 doi: 10.1080/13803395.2022.2069231. [DOI] [PubMed] [Google Scholar]
- Benedict RHB, Schretlen D, Groninger L, Brandt J. Hopkins Verbal Learning Test – Revised: Normative Data and Analysis of Inter-Form and Test-Retest Reliability. Clin Neuropsychol. 1998;12:43–55. doi: 10.1076/clin.12.1.43.1726. [DOI] [Google Scholar]
- Benedict RHB, Schretlen D, Groninger L, Dobraski M, Shpritz B. Revision of the Brief Visuospatial Memory Test: Studies of normal performance, reliability, and validity. Psychol Assess. 1996;8:145–153. doi: 10.1037/1040-3590.8.2.145. [DOI] [Google Scholar]
- Benton AL, Hamsher K, Sivan AB. Multilingual Aphasia Examination 1994 [Google Scholar]
- Childs EA, Lyles RH, Selnes OA, Chen B, Miller EN, Cohen BA, Becker JT, Mellors J, McArthur JC. Plasma viral load and CD4 lymphocytes predict HIV-associated dementia and sensory neuropathy. Neurology. 1999;52:607–613. doi: 10.1212/wnl.52.3.607. [DOI] [PubMed] [Google Scholar]
- Cohen RA, de la Monte S, Gongvatana A, Ombao H, Gonzalez B, Devlin KN, Navia B, Tashima KT. Plasma cytokine concentrations associated with HIV/hepatitis C coinfection are related to attention, executive and psychomotor functioning. J Neuroimmunol. 2011;233:204–210. doi: 10.1016/j.jneuroim.2010.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cottam DR, Mattar SG, Barinas-Mitchell E, Eid G, Kuller L, Kelley DE, Schauer PR. The Chronic Inflammatory Hypothesis for the Morbidity Associated with Morbid Obesity: Implications and Effects of Weight Loss. Obes Surg. 2004;14:589–600. doi: 10.1381/096089204323093345. [DOI] [PubMed] [Google Scholar]
- Crum-Cianflone N, Roediger MP, Eberly L, Headd M, Marconi V, Ganesan A, Weintrob A, Barthel RV, Fraser S, Agan BK, Infectious Disease Clinical Research Program HIV Working Group Increasing rates of obesity among HIV-infected persons during the HIV epidemic. PloS One. 2010;5:e10106. doi: 10.1371/journal.pone.0010106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahl A, Hassing LB, Fransson E, Berg S, Gatz M, Reynolds CA, Pedersen NL. Being Overweight in Midlife Is Associated With Lower Cognitive Ability and Steeper Cognitive Decline in Late Life. J Gerontol A Biol Sci Med Sci. 2010;65A:57–62. doi: 10.1093/gerona/glp035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahl AK, Hassing LB. Obesity and Cognitive Aging. Epidemiol Rev. 2012 doi: 10.1093/epirev/mxs002. [DOI] [PubMed] [Google Scholar]
- Dahl AK, Hassing LB, Fransson EI, Gatz M, Reynolds CA, Pedersen NL. Body mass index across midlife and cognitive change in late life. Int J Obes. 2013;37:296–302. doi: 10.1038/ijo.2012.37. 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devlin KN, Gongvatana A, Clark US, Chasman JD, Westbrook ML, Tashima KT, Navia B, Cohen RA. Neurocognitive effects of HIV, hepatitis C, and substance use history. J Int Neuropsychol Soc JINS. 2012;18:68–78. doi: 10.1017/S1355617711001408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fantuzzi G. Adipose tissue, adipokines, and inflammation. J Allergy Clin Immunol. 2005;115:911–919. doi: 10.1016/j.jaci.2005.02.023. quiz 920. [DOI] [PubMed] [Google Scholar]
- Ferrando S, van Gorp W, McElhiney M, Goggin K, Sewell M, Rabkin J. Highly active antiretroviral treatment in HIV infection: benefits for neuropsychological function. AIDS Lond Engl. 1998;12:F65–70. doi: 10.1097/00002030-199808000-00002. [DOI] [PubMed] [Google Scholar]
- Fialho R, Pereira M, Bucur M, Fisher M, Whale R, Rusted J. Cognitive impairment in HIV and HCV co-infected patients: a systematic review and meta-analysis. AIDS Care. 2015:1–14. doi: 10.1080/09540121.2015.1108385. [DOI] [PubMed] [Google Scholar]
- Fialho RM, Pereira M, Mendonça N, Ouakinin S. Depressive symptoms and neurocognitive performance among HIV-infected women. Women Health. 2013;53:117–134. doi: 10.1080/03630242.2013.767301. [DOI] [PubMed] [Google Scholar]
- Galimberti D, Fenoglio C, Lovati C, Venturelli E, Guidi I, Corrà B, Scalabrini D, Clerici F, Mariani C, Bresolin N, Scarpini E. Serum MCP-1 levels are increased in mild cognitive impairment and mild Alzheimer’s disease. Neurobiol Aging. 2006;27:1763–1768. doi: 10.1016/j.neurobiolaging.2005.10.007. [DOI] [PubMed] [Google Scholar]
- Golden C. Stroop Color and Word Test. Chicago: Stoelting; n.d. [Google Scholar]
- Grant I. Neurocognitive disturbances in HIV. Int Rev Psychiatry Abingdon Engl. 2008;20:33–47. doi: 10.1080/09540260701877894. [DOI] [PubMed] [Google Scholar]
- Gregor MF, Hotamisligil GS. Inflammatory Mechanisms in Obesity. Annu Rev Immunol. 2011;29:415–445. doi: 10.1146/annurev-immunol-031210-101322. [DOI] [PubMed] [Google Scholar]
- Gunstad J, Lhotsky A, Wendell CR, Ferrucci L, Zonderman AB. Longitudinal Examination of Obesity and Cognitive Function: Results from the Baltimore Longitudinal Study of Aging. Neuroepidemiology. 2010;34:222–229. doi: 10.1159/000297742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunstad J, Paul RH, Cohen RA, Tate DF, Spitznagel MB, Gordon E. Elevated body mass index is associated with executive dysfunction in otherwise healthy adults. Compr Psychiatry. 2007;48:57–61. doi: 10.1016/j.comppsych.2006.05.001. [DOI] [PubMed] [Google Scholar]
- Gustafson DR, Mielke MM, Tien PC, Valcour V, Cohen M, Anastos K, Liu C, Pearce L, Golub ET, Minkoff H, Crystal HA. Anthropometric measures and cognition in middle-aged HIV-infected and uninfected women. The Women’s Interagency HIV Study. J Neurovirol. 2013;19:574–585. doi: 10.1007/s13365-013-0219-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassing LB, Dahl AK, Pedersen NL, Johansson B. Overweight in midlife is related to lower cognitive function 30 years later: a prospective study with longitudinal assessments. Dement Geriatr Cogn Disord. 2010;29:543–552. doi: 10.1159/000314874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF, Preacher KJ. Statistical mediation analysis with a multicategorical independent variable. Br J Math Stat Psychol. 2014;67:451–470. doi: 10.1111/bmsp.12028. [DOI] [PubMed] [Google Scholar]
- Heaton RK, Clifford DB, Franklin DR, Jr, Woods SP, Ake C, Vaida F, Ellis RJ, Letendre SL, Marcotte TD, Atkinson JH, Rivera-Mindt M, Vigil OR, Taylor MJ, Collier AC, Marra CM, Gelman BB, McArthur JC, Morgello S, Simpson DM, McCutchan JA, Abramson I, Gamst A, Fennema-Notestine C, Jernigan TL, Wong J, Grant I, CHARTER Group HIV-associated neurocognitive disorders persist in the era of potent antiretroviral therapy: CHARTER Study. Neurology. 2010;75:2087–2096. doi: 10.1212/WNL.0b013e318200d727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heaton RK, Marcotte TD, Mindt MR, Sadek J, Moore DJ, Bentley H, McCutchan JA, Reicks C, Grant I, HNRC Group The impact of HIV-associated neuropsychological impairment on everyday functioning. J Int Neuropsychol Soc JINS. 2004;10:317–331. doi: 10.1017/S1355617704102130. [DOI] [PubMed] [Google Scholar]
- Kim DJ, Westfall AO, Chamot E, Willig AL, Mugavero MJ, Ritchie C, Burkholder GA, Crane HM, Raper JL, Saag MS, Willig JH. Multimorbidity patterns in HIV-infected patients: the role of obesity in chronic disease clustering. J Acquir Immune Defic Syndr. 2012;61:600–605. doi: 10.1097/QAI.0b013e31827303d5. 1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kløve H. Grooved pegboard. Lafayette, IN: Lafayette Instruments; 1963. [Google Scholar]
- Lindl KA, Marks DR, Kolson DL, Jordan-Sciutto KL. HIV-Associated Neurocognitive Disorder: Pathogenesis and Therapeutic Opportunities. J Neuroimmune Pharmacol. 2010;5:294–309. doi: 10.1007/s11481-010-9205-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magaki S, Mueller C, Dickson C, Kirsch W. Increased production of inflammatory cytokines in mild cognitive impairment. Exp Gerontol. 2007;42:233–240. doi: 10.1016/j.exger.2006.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mariz C de A, Albuquerque M de FPM de, Ximenes RA de A, Melo HRL de, Bandeira F, Oliveira TGBE, Carvalho EH de, Silva AP da, Miranda Filho D de B. Body mass index in individuals with HIV infection and factors associated with thinness and overweight/obesity. Cad Saúde Pública. 2011;27:1997–2008. doi: 10.1590/s0102-311x2011001000013. [DOI] [PubMed] [Google Scholar]
- Martin-Thormeyer EM, Paul RH. Drug abuse and hepatitis C infection as comorbid features of HIV associated neurocognitive disorder: neurocognitive and neuroimaging features. Neuropsychol Rev. 2009;19:215–231. doi: 10.1007/s11065-009-9101-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCutchan JA, Marquie-Beck JA, Fitzsimons CA, Letendre SL, Ellis RJ, Heaton RK, Wolfson T, Rosario D, Alexander TJ, Marra C, Ances BM, Grant I, CHARTER Group Role of obesity, metabolic variables, and diabetes in HIV-associated neurocognitive disorder. Neurology. 2012;78:485–492. doi: 10.1212/WNL.0b013e3182478d64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meagher C, Beilke J, Arreaza G, Mi QS, Chen W, Salojin K, Horst N, Cruikshank WW, Delovitch TL. Neutralization of interleukin-16 protects nonobese diabetic mice from autoimmune type 1 diabetes by a CCL4-dependent mechanism. Diabetes. 2010;59:2862–2871. doi: 10.2337/db09-0131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menza M, Dobkin RD, Marin H, Mark MH, Gara M, Bienfait K, Dicke A, Kusnekov A. The role of inflammatory cytokines in cognition and other non-motor symptoms of Parkinson’s disease. Psychosomatics. 2010;51:474–479. doi: 10.1176/appi.psy.51.6.474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller AA, Spencer SJ. Obesity and neuroinflammation: A pathway to cognitive impairment. Brain Behav Immun. 2014;42:10–21. doi: 10.1016/j.bbi.2014.04.001. [DOI] [PubMed] [Google Scholar]
- Obesity and Overweight for Professionals: Adult: Defining - DNPAO - CDC. [WWW Document], n.d. URL http://www.cdc.gov/obesity/adult/defining.html (accessed 11.9.14)
- Pedersen KK, Pedersen M, Gaardbo JC, Ronit A, Hartling HJ, Bruunsgaard H, Gerstoft J, Ullum H, Nielsen SD. Persisting inflammation chronic immune activation but intact cognitive function in HIV-infected patients after long-term treatment with combination antiretroviral therapy. J Acquir Immune Defic Syndr. 2013;63:272–279. doi: 10.1097/QAI.0b013e318289bced. 1999. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale A Self-Report Depression Scale for Research in the General Population. Appl Psychol Meas. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Reitan RM. Trail Making Test. Reitan Neuropsychology Laboratory 1992 [Google Scholar]
- Sabia S, Kivimaki M, Shipley MJ, Marmot MG, Singh-Manoux A. Body mass index over the adult life course and cognition in late midlife: the Whitehall II Cohort Study. Am J Clin Nutr. 2009;89:601–607. doi: 10.3945/ajcn.2008.26482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samji H, Cescon A, Hogg RS, Modur SP, Althoff KN, Buchacz K, Burchell AN, Cohen M, Gebo KA, Gill MJ, Justice A, Kirk G, Klein MB, Korthuis PT, Martin J, Napravnik S, Rourke SB, Sterling TR, Silverberg MJ, Deeks S, Jacobson LP, Bosch RJ, Kitahata MM, Goedert JJ, Moore R, Gange SJ, for The North American AIDS Cohort Collaboration on Research and Design (NA-ACCORD) of IeDEA Closing the Gap: Increases in Life Expectancy among Treated HIV-Positive Individuals in the United States and Canada. PLoS ONE. 2013;8:e81355. doi: 10.1371/journal.pone.0081355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sattler F, He J, Letendre S, Wilson C, Sanders C, Heaton R, Ellis R, Franklin D, Aldrovandi G, Marra CM, Clifford D, Morgello S, Grant I, Mccutchan JA, for the CHARTER Group Abdominal Obesity Contributes to Neurocognitive Impairment in HIV Infected Patients with Increased Inflammation and Immune Activation. J Acquir Immune Defic Syndr. 2014 doi: 10.1097/QAI.0000000000000458. 1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schram MT, Euser SM, de Craen AJM, Witteman JC, Frölich M, Hofman A, Jolles J, Breteler MMB, Westendorp RGJ. Systemic markers of inflammation and cognitive decline in old age. J Am Geriatr Soc. 2007;55:708–716. doi: 10.1111/j.1532-5415.2007.01159.x. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. 57. [PubMed] [Google Scholar]
- Skundric DS, Cai J, Cruikshank WW, Gveric D. Production of IL-16 correlates with CD4+ Th1 inflammation and phosphorylation of axonal cytoskeleton in multiple sclerosis lesions. J Neuroinflammation. 2006;3:13. doi: 10.1186/1742-2094-3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith E, Hay P, Campbell L, Trollor JN. A review of the association between obesity and cognitive function across the lifespan: implications for novel approaches to prevention and treatment. Obes Rev. 2011;12:740–755. doi: 10.1111/j.1467-789X.2011.00920.x. [DOI] [PubMed] [Google Scholar]
- Stanek KM, Strain G, Devlin M, Cohen R, Paul R, Crosby RD, Mitchell JE, Gunstad J. Body mass index and neurocognitive functioning across the adult lifespan. Neuropsychology. 2013;27:141–151. doi: 10.1037/a0031988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sturman MT, de Leon CFM, Bienias JL, Morris MC, Wilson RS, Evans DA. Body mass index and cognitive decline in a biracial community population. Neurology. 2008;70:360–367. doi: 10.1212/01.wnl.0000285081.04409.bb. [DOI] [PubMed] [Google Scholar]
- Thames AD, Arentoft A, Rivera-Mindt M, Hinkin CH. Functional disability in medication management and driving among individuals with HIV: A 1-year follow-up study. J Clin Exp Neuropsychol. 2013;35:49–58. doi: 10.1080/13803395.2012.747596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldstein SR, Katzel LI. Interactive relations of central versus total obesity and blood pressure to cognitive function. Int J Obes. 2006;30:201–207. doi: 10.1038/sj.ijo.0803114. 2005. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Adult Intelligence Scale-III (WAIS-III) 1997 [Google Scholar]
- Woods SP, Morgan EE, Marquie-Beck J, Carey CL, Grant I, Letendre SL. Markers of Macrophage Activation and Axonal Injury are Associated With Prospective Memory in HIV-1 Disease. Cogn Behav Neurol Off J Soc Behav Cogn Neurol. 2006;19:217–221. doi: 10.1097/01.wnn.0000213916.10514.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaffe K, Lindquist K, Penninx BW, Simonsick EM, Pahor M, Kritchevsky S, Launer L, Kuller L, Rubin S, Harris T. Inflammatory markers and cognition in well-functioning African-American and white elders. Neurology. 2003;61:76–80. doi: 10.1212/01.wnl.0000073620.42047.d7. [DOI] [PubMed] [Google Scholar]
- Yeni P. Update on HAART in HIV. J Hepatol. 2006;44:S100–103. doi: 10.1016/j.jhep.2005.11.021. [DOI] [PubMed] [Google Scholar]
- Yuan L, Qiao L, Wei F, Yin J, Liu L, Ji Y, Smith D, Li N, Chen D. Cytokines in CSF correlate with HIV-associated neurocognitive disorders in the post-HAART era in China. J Neurovirol. 2013;19:144–149. doi: 10.1007/s13365-013-0150-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


