Abstract
Background
Infection after total knee arthroplasty (TKA) can result in disastrous consequences. Previous research regarding injections and risk of TKA infection have produced conflicting results and in general have been limited by small cohort size.
Questions/purposes
The purpose of this study was to evaluate if intraarticular injection before TKA increases the risk of postoperative infection and to identify if time between injection and TKA affect the risk of TKA infection.
Methods
The Humana data set was reviewed from 2007 to 2014 for all patients who received a knee injection before TKA. Current Procedural Terminology (CPT) codes and laterality modifiers were used to identify patients who underwent knee injection followed by ipsilateral TKA. Postoperative infection within 6 months of TKA was identified using International Classification of Diseases, 9th Revision/CPT codes that represent two infectious endpoints: any postoperative surgical site infection (encompasses all severities of infection) and operative intervention for TKA infection (surrogate for deep TKA infection). The injection cohort was stratified into 12 subgroups by monthly intervals out to 12 months corresponding to the number of months that had elapsed between injection and TKA. Risk of postoperative infection was compared between the injection and no injection cohorts. In total, 29,603 TKAs (35%) had an injection in the ipsilateral knee before the TKA procedure and 54,081 TKA cases (65%) did not. The PearlDiver database does not currently support line-by-line output of patient data, and so we were unable to perform a multivariate analysis to determine whether other important factors may have varied between the study groups that might have had a differential influence on the risk of infection between those groups. However, the Charlson Comorbidity index was no different between the injection and no injection cohorts (2.9 for both) suggesting similar comorbidity profiles between the groups.
Results
The proportion of TKAs developing any postoperative infection was higher among TKAs that received an injection before TKA than in those that did not (4.4% versus 3.6%; odds ratio [OR], 1.23; 95% confidence interval [CI], 1.15-1.33; p < 0.001). Likewise, the proportion of TKAs developing infection resulting in return to the operating room after TKA was also higher among TKAs that received an injection before TKA than those that did not (1.49% versus 1.04%; OR, 1.4; 95% CI, 1.3-1.63; p < 0.001). Month-by-month analysis of time between injection and TKA revealed the odds of any postoperative infection remained higher for the injection cohort out to a duration of 6 months between injection and TKA (ORs ranged 1.23 to 1.46 when 1-6 months between injection and TKA; p < 0.05 for all) as did the odds of operative intervention for TKA infection when injection occurred within 7 months of TKA (OR ranged from 1.38 to 1.88 when 1-7 months between injection and TKA; p < 0.05 for all). When the duration between injection and TKA was longer than 6 or 7 months, the ORs were no longer elevated at these endpoints, respectively.
Conclusions
Injection before TKA was associated with a higher risk of postoperative infection and appears to be time-dependent with closer proximity between injection and TKA having increased odds of infection. Further research is needed to better evaluate the risk injection before TKA poses for TKA infection; a more definitive relationship could be established with a multivariate analysis to control for other known risk factors for TKA infection.
Level of Evidence
Level III, therapeutic study.
Introduction
Osteoarthritis of the knee is a common musculoskeletal disorder affecting nearly 27 million adults in the United States [10]. Treatment of patients with knee osteoarthritis relies mainly on symptom management because there are no current disease-modifying treatments available for this disease. As a result, intraarticular knee injections with corticosteroid, hyaluronic acid, or other formulations have commonly been used as a means of knee osteoarthritis symptom management. It has been estimated that approximately 30% of patients have received an intraarticular corticosteroid injection before TKA [11]. The efficacy and safety of these injections have been relatively well studied in native knees with a Cochrane review finding intraarticular corticosteroids to provide some symptom relief in the short term (2-4 weeks) with no clinically important response in the long term and no major safety issues detected [1]. However, the American Academy of Orthopaedic Surgeons recently released their updated clinical practice guidelines for treatment of osteoarthritis of the knee and those guidelines did not recommend for or against the use of corticosteroid injection for patients with symptomatic osteoarthritis of the knee (recommendation 8), but they made a strong recommendation against use of hyaluronic acid injections for knee osteoarthritis symptoms (recommendation 9) [8]. Nonetheless, the effects these injections can have on outcomes after TKA, specifically risk of TKA infection, have not been well characterized. Given the devastating and costly consequences of TKA infection [14], it is of utmost importance to better understand whether injection of a native knee before TKA increases the risk of subsequent infection.
Previous research on TKA infection after recent corticosteroid injection has been relatively limited with conflicting results [3–5, 9, 15]. Of these studies, two raised concern for increased infection rates after TKA in patients with previous injection [3, 15]. However, given that the risk of infection after TKA is estimated to be approximately 0.8% to 3% [2, 7, 12, 16, 19], these studies are underpowered with only one of these studies having more than 100 patients with corticosteroid injections before TKA included in the analysis. The recent study by Cancienne et al. [3] evaluated 22,240 Medicare patients who had an injection (although the specific medication was not characterized) within 1 year of TKA; they demonstrated an increased odds of infection for those who had an injection within 3 months of TKA (odds ratio [OR], 2.0 [1.6-2.5] for infection within 3 months after TKA and OR 1.5 [1.2-1.8] for infection within 6 months after TKA). These are very important data but they are somewhat limited in their broad applicability given that they were drawn from a Medicare-only population, they were limited by how the definitions of TKA infection were coded, and the study had only a 3-month interval analysis of the effects of timing between injection and TKA.
Given these limitations and the discrepant results with the prior underpowered studies, the purpose of the present study was to analyze a large database of commercially insured patients of all age groups to answer the following study questions: (1) Does injection before TKA increase the risk of postoperative TKA infection? (2) Does the amount of time between preoperative injection and TKA affect the proportion of patients who develop a postoperative TKA infection?
Materials and Methods
The PearlDiver Research Program (www.pearldiverinc.com; PearlDiver Inc, Fort Wayne, IN, USA) was used to query the Humana Inc administrative claims database for the information presented in this study. The Humana Inc data set is an administrative claims database consisting of medical insurance claims on procedures, diagnoses, inpatient encounters, and outpatient encounters to Humana Health Insurance from approximately 16 million covered lives. The data set includes both private/commercially insured as well as data from patients who elected to purchase their Medicare Advantage plans (Medicare Part C) through Humana Health Insurance. Medicare Parts A and B data are not included within this data set because this only includes data obtained from this specific commercial insurer. All data within this database are Health Insurance Portability and Accountability Act-compliant and were thus deemed exempt by the University of Iowa Human Subjects Office from institutional review board approval.
The Humana Inc administrative claims database was queried for right and left primary TKA cases using the Current Procedural Terminology (CPT) code 27447 and laterality modifiers. Laterality designation was determined from billing modifiers included in the CPT coding of TKA and injection (CPT 20610) procedures; thus, records without laterality designation were not extracted from the database with this query and therefore not included in the analysis. Using Boolean coding within the database, the right and left TKA cohorts were further divided into injection and no injection cohorts based on whether or not an ipsilateral injection had been performed within 1 year before TKA. If a right TKA had underwent an injection on the right within 1 year before right TKA, this was included in the cohort-designated injection cohort. If a right TKA had no history of injection in the ipsilateral knee within 1 year before surgery, this TKA was included in the no injection cohort. The same filtering for history of ipsilateral injection before TKA versus no injection was applied to the left TKA cohort. The right and left injection cohorts were then each stratified into 12 subgroups by monthly intervals out to 12 months corresponding to the number of months that had elapsed between injection and TKA.
A retrospective cohort study design was used for this study given that the cohorts were defined by exposure (injection or no injection) and tracked longitudinally for the occurrence of a TKA infection. It should be noted that current CPT coding does not allow differentiation of anatomic site of injection and the CPT code 20610 used in this study includes all major joints (shoulder, hip, and knee). Additionally, as a result of the nature of the coding, the specific contents of the injection (corticosteroid, hyaluronic acid, etc) are not known. It was estimated by the PearlDiver program that approximately 91.4% of patients undergoing primary TKA remain active within the Humana data set at a minimum of 6 months after their TKA.
Each cohort was then queried for basic demographic data (age, sex) and Charlson Comorbidity Index (CCI) was calculated by the PearlDiver Research Program for both cohorts. Additionally, the primary diagnosis associated with the insurance claims linked to the TKAs in this study was identified. Given that a single procedure often has multiple insurance claims linked to that procedure, and each claim has a primary diagnosis, there are more primary diagnoses than number of TKAs. Therefore, the top five primary diagnoses for each cohort are presented as a percentage of the total primary diagnoses for that specific cohort.
The risk of postoperative surgical site infection and TKA infection resulting in operative intervention was then established using Boolean coding to identify the occurrence of an International Classification of Diseases, 9th Revision (ICD-9) and/or CPT code within 6 months of the index right or left TKA that represents these outcome measures. The variable designated postoperative surgical site infection was defined by the following ICD-9/CPT codes and was designed to encompass all severities of surgical site infection: ICD-9 99859 (other postoperative infection [ie, stitch abscess, wound infection]), 99851 (infected postoperative seroma), 99666 (infection and inflammatory reaction resulting from internal joint prosthesis), 8604 (incision and drainage of skin and subcutaneous tissue), 8006 (arthrotomy for removal of prosthesis without replacement, knee), 0084 (revision of total knee replacement, tibial liner), and CPT 27488 (removal of prosthesis, including total knee prosthesis, methylmethacrylate with or without insertion of spacer, knee), 10180 (incision and drainage, complex, postoperative wound infection), 20005 (incision and drainage of soft tissue abscess, subfascial), 27310 (arthrotomy, knee, with exploration, drainage, or removal of foreign body [ie, infection]), 11981 (insertion, nonbiodegradable drug delivery implant [ie antibiotic cement spacer]), and 29871 (arthroscopy, knee, surgical; for infection, lavage, and drainage). The variable designated operative procedure for TKA surgical site infection was created from a subset of the ICD-9/CPT codes used for the variable postoperative surgical site infection (CPT 27488, 10180, 20005, 27310, 11981, 29871 and ICD-9 8604, 8006, 0084) that represented an operative procedure for TKA infection. This variable was created to more specifically identify deep postoperative TKA infection by including only operative ICD-9/CPT codes to eliminate superficial, conservatively managed infection (ie, stitch abscess, cellulitis, etc).
All data analyses were performed using of SAS software (Version 9.4; SAS Institute, Cary, NC, USA). The chi square test was applied for categorical variables to determine significant differences, whereas an independent two-sample t-test was used for continuous variables. ORs with corresponding 95% confidence intervals (CIs) were used to compare incidence of postoperative infection. These were calculated based on the number of TKAs with infection in the injection cohort compared with those in the no injection cohort relative to the noninfected TKA cases for each group. ORs were calculated for the infectious endpoints for the two cohorts as a whole and for each interval of the subgroup analysis. Statistical significance was set at p < 0.05 for all tests.
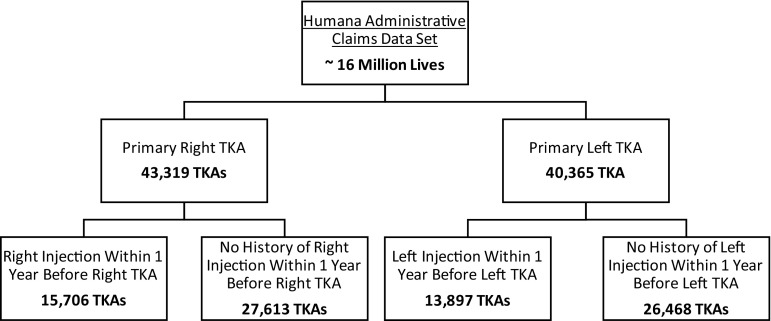
In total, 83,684 primary TKAs were included in this analysis (43,319 right TKAs and 40,365 left TKAs). Of these TKA cases, 29,603 (35%; 15,706 right TKAs and 13,897 left TKAs) had an ipsilateral injection at least 1 year before the TKA and 54,081 TKAs (65%; 27,613 right TKAs and 26,468 left TKAs) had no history of prior ipsilateral injection within 1 year before TKA (Fig. 1). The sex distribution was approximately two to one for both cohorts with 63% female and 38% male in the no injection cohort and 67% and 33% female and male in the injection cohort, respectively (p < 0.001). The PearlDiver database does not currently support line-by-line output of patient data, and so we were unable to perform a multivariate analysis to determine whether other important factors may have varied between the study groups that might have had a differential influence on the risk of infection between those groups. However, the CCI was no different between the injection and no injection cohorts (2.9 for both) suggesting similar comorbidity profiles between the groups. The average age at the time of TKA for both cohorts fell within the 65- to 69-year-old age group. The no injection cohort had a higher percentage of patients in the age group 55 to 69 years, whereas the injection cohort had more patients in the 70- to 89-year age group (Table 1). When comparing percentage of patients younger than 50 years old versus patients 50 years and older, there were no differences between the two cohorts (p = 0.147). Evaluation of the primary diagnoses associated with the insurance claims linked to the TKAs in this study demonstrated the top five most common primary diagnoses for both cohorts to be (injection cohort versus no injection cohort): osteoarthritis (97.3% versus 96.7%, p < 0.001), leg pain (0.74% versus 0.73%, p < 0.001), unspecified arthropathy (0.38% versus 0.61%, p < 0.001), rheumatoid arthritis (0.32% versus 0.34%, p < 0.001), traumatic arthropathy (0.16% versus 0.27%, p < 0.001), and other (1.14% versus 1.36%, p < 0.001).
Fig. 1.
Flowchart shows creation of the injection and no injection cohorts.
Table 1.
Demographics at the time of TKA
| Demographic | No injection | Percent | Injection | Percent | p value |
|---|---|---|---|---|---|
| Total TKAs | 54,081 | 29,603 | |||
| Female | 33,782 | 62.5 | 19,740 | 66.7 | < 0.001 |
| Male | 20,299 | 37.5 | 9863 | 33.3 | < 0.001 |
| Age (years) | |||||
| ≤ 39 | 65 | 0.1 | 23 | 0.1 | 0.07 |
| 40-44 | 203 | 0.4 | 103 | 0.4 | 0.87 |
| 45-49 | 633 | 1.2 | 328 | 1.1 | 0.42 |
| 50-54 | 1816 | 3.4 | 942 | 3.3 | 0.17 |
| 55-59 | 3503 | 6.5 | 1789 | 6.0 | 0.01 |
| 60-64 | 5226 | 9.7 | 2564 | 8.7 | < 0.001 |
| 65-69 | 14,137 | 26.1 | 6994 | 23.6 | < 0.001 |
| 70-74 | 13,222 | 24.5 | 7590 | 25.6 | < 0.001 |
| 75-79 | 9068 | 16.8 | 5316 | 18.0 | < 0.001 |
| 80-84 | 4421 | 8.2 | 2755 | 9.3 | < 0.001 |
| 85-89 | 823 | 1.5 | 675 | 2.3 | < 0.001 |
| ≥ 90 | 964 | 1.8 | 524 | 1.8 | 0.89 |
| CCI score | 2.9 | 2.9 | 0.12 |
CCI = Charlson Comorbidity Index.
Results
TKA infection occurred more frequently when knee injection was performed before ipsilateral primary TKA. The risk of any postoperative surgical site infection within 6 months after TKA was higher for TKAs that received an injection before ipsilateral TKA than those that did not (4.4% versus 3.59%; OR, 1.23; 95% CI, 1.15-1.33; p < 0.001). Likewise, the risk of a postoperative infection resulting in return to the operating room within 6 months after TKA was also higher for TKAs that received an injection before ipsilateral TKA than those that did not (1.49% versus 1.04%; OR, 1.4; 95% CI, 1.3-1.63; p < 0.001).
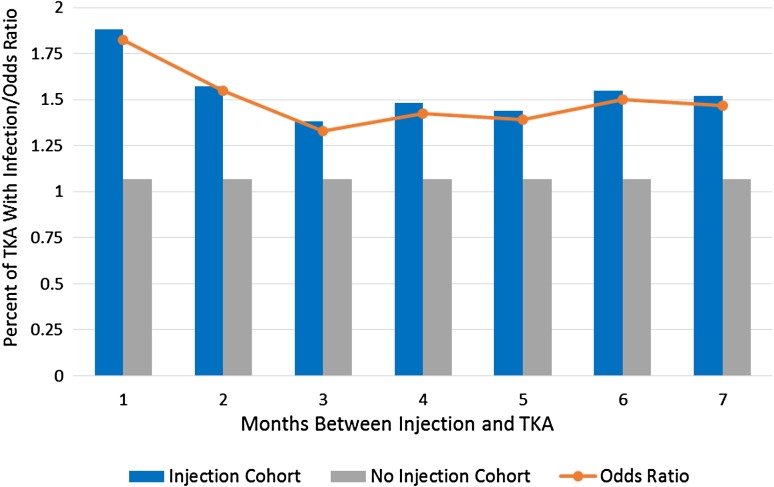
Evaluation of the data to determine the point in time at which there was no longer an association between injection and postoperative TKA infection found the cutoff point to be 6 months for the endpoint of any postoperative surgical site infection and 7 months for the endpoint of TKA infection resulting in operative intervention (Tables 2 and 3). When the injection occurred within 6 months of TKA, the incidence of any postoperative infection ranged from 4.4% to 5.2% depending on time between injection and TKA compared with 3.59% for those who did not receive an injection (OR, 1.23-1.46; p < 0.05 for all; Table 2). Similarly, when injection occurred within 7 months of TKA, the incidence of operative intervention for infection ranged from 1.38% to 1.88% depending on the time interval analyzed compared with 1.04% for those who did not have an injection (OR, 1.33-1.83; p < 0.05 for all; Table 3; Fig. 2).
Table 2.
Any postoperative surgical site infection within 6 months of TKA
| Time between injection and TKA | Total TKA | TKA with infection (%) | Unadjusted OR (95% CI) | p value |
|---|---|---|---|---|
| 1 month | 1804 | 83 (4.6) | 1.29 (1.03-1.62) | 0.024 |
| 2 months | 5031 | 220 (4.4) | 1.23 (1.06-1.42) | 0.005 |
| 3 months | 5659 | 247 (4.4) | 1.23 (1.07-1.40) | 0.003 |
| 4 months | 4197 | 192 (4.6) | 1.28 (1.11-1.50) | 0.001 |
| 5 months | 3259 | 150 (4.6) | 1.30 (1.09-1.54) | 0.003 |
| 6 months | 2444 | 126 (5.2) | 1.46 (1.21-1.76) | < 0.001 |
| 7 months | 1839 | 70 (3.8) | 1.06 (0.83-1.35) | 0.625 |
| 8 months | 1477 | 51 (3.5) | 0.96 (0.72-1.27) | 0.779 |
| 9 months | 1257 | 55 (4.4) | 1.23 (0.93-1.62) | 0.141 |
| 10 months | 1053 | 36 (3.4) | 0.95 (0.68-1.33) | 0.766 |
| 11 months | 850 | 29 (3.4) | 0.95 (0.65-1.38) | 0.781 |
| 12 months | 733 | 28 (3.8) | 1.07 (0.73-1.56) | 0.741 |
| No injection | 54,081 | 1942 (3.6) | Reference |
OR = odds ratio; CI = confidence interval.
Table 3.
Operative intervention for TKA infection within 6 months of TKA
| Time between injection and TKA | Total TKA | TKA with infection (%) | Unadjusted OR (95% CI) | p value |
|---|---|---|---|---|
| 1 month | 1804 | 34 (1.9) | 1.83 (1.29-2.59) | 0.001 |
| 2 months | 5031 | 79 (1.6) | 1.55 (1.22-1.96) | 0.0003 |
| 3 months | 5659 | 78 (1.4) | 1.33 (1.05-1.69) | 0.019 |
| 4 months | 4197 | 62 (1.5) | 1.43 (1.09-1.85) | 0.009 |
| 5 months | 3259 | 47 (1.4) | 1.39 (1.03-1.88) | 0.031 |
| 6 months | 2444 | 38 (1.6) | 1.50 (1.08-2.09) | 0.016 |
| 7 months | 1839 | 28 (1.5) | 1.47 (1.01-2.15) | 0.048 |
| 8 months | 1477 | 16 (1.1) | 1.04 (0.63-1.72) | 0.875 |
| 9 months | 1257 | 4 (0.3) | 0.31 (0.12-0.83) | 0.019 |
| 10 months | 1053 | 13 (1.2) | 1.19 (0.68-2.07) | 0.541 |
| 11 months | 850 | 0 (0.0) | 0.06 (0.01-0.89) | 0.042 |
| 12 months | 733 | 4 (0.6) | 0.54 (0.20-1.45) | 0.22 |
| No injection | 54081 | 563 (1.0) | Reference |
CI = confidence interval.
Fig. 2.
Graphic representation of the percent of TKA requiring operative intervention for TKA infection as well as ORs for this endpoint comparing both the injection and no injection cohorts with results delineated by time between injection and TKA. Results included are only those that were different (p < 0.05).
Once the duration between injection and TKA was longer than 6 or 7 months, depending on the respective infectious endpoint, the ORs for TKA infection were no longer higher for the injection cohort (Tables 2, 3).
Discussion
Approximately 30% of patients have received an intraarticular injection before TKA [11]. Whether an intraarticular injection increases the risk of infection after TKA has not been extensively studied with most data on the subject being extremely limited by small cohort size [4, 5, 9, 15]. Only one other large database study has been performed on this subject [3]; however, limitations from a Medicare-only population, selected coding for definitions of TKA infection, and only a 3-month interval analysis of the effects of timing between injection and TKA in that report suggested the need for the further research performed here to better understand the possible association between injection and TKA infection. Thus, the purpose of this study was to identify if the risk of postoperative infection is increased after preoperative knee injection and if time between injection and TKA is consequential to this risk by analyzing a large database of privately insured patients from all age groups. In the present study, the odds of any postoperative TKA infection were higher in patients with a history of injection before ipsilateral TKA than those without as were the odds of infection requiring operative intervention after TKA. Analysis of timing between injection and TKA demonstrated that the increased risk of infection associated with the injection was no longer present once the injection was performed more than 6 or 7 months before TKA depending on the respective infectious endpoint.
This study had a number of limitations. First, the PearlDiver database does not currently support line-by-line output of patient data; thus, a multivariate analysis was unable to be performed to control for other known risks of postoperative TKA infection. It seems possible, if not likely, that those who received injection were different from those who did not, perhaps in important ways. For example, one can imagine surgeons trying to delay surgery in patients who have diabetes, morbid obesity, severe vascular disease, smoking, or other conditions that might increase the risk of infection. However, similar CCI scores in both groups give us some reassurance that there were not substantial differences in overall medical comorbidities between the study groups. Additionally, although there was a slightly lower percentage of males in the injection cohort relative to the no injection cohort, the authors feel that this is unlikely to clinically impact the conclusions of this study given that the injection cohort still had a higher risk of infection despite male sex having been demonstrated to be an independent predictor of TKA infection [6, 14, 18]. Further demographic limitations include confounding effects from differences in underlying diagnosis for the TKA. However, both cohorts had the same top five diagnoses and the injection cohort had slightly less diagnoses of rheumatoid arthritis, which would have been most likely to confound the results given that patients with inflammatory arthritis are more prone to infection.
Also, the limitations that apply to administrative claims database projects naturally apply here, in particular the study’s dependence on proper coding and documentation. Although the accuracy of this specific administrative claims data set has not been formally studied, some studies detailing the sensitivity of administrative claims data for detecting orthopaedic-specific complications or revision surgery have been performed. For example, a systematic review published by Singh et al. [17] summarized validated coding algorithms to identify orthopaedic hip and knee arthroplasty revision procedures from administrative claims data with sensitivity and specificity ranging from 77.7% to 87.2% and 97.6% to 99.0%, respectively. Additionally, a study by Murphy et al. [13] assessed the use of claims data in identifying infection 6 months after anterior cruciate ligament (ACL) reconstruction. They reported a sensitivity of 75% for infection management procedure codes in identifying postoperative ACL infection and a sensitivity of 68% when using only infection diagnosis codes to identify ACL infections [13].
Another limitation with administrative claims data is potential fluctuation within that data set from patients entering and leaving the insurance provider during the time period of the study. Although the fluctuation within this specific cohort is not known, it has been estimated that approximately 91.4% of patients remain active within Humana administrative claims database at least 6 months after primary TKA. An additional limitation is that Health Insurance Portability and Accountability Act-compliant databases are unable to report exact numbers when the value of the endpoint of interest lies between 0 and 10, thus limiting detailed analysis of smaller cohorts. Given that the cohorts in this study are quite large, this limitation likely had little effect on the outcomes of the study. Additional limitations include inability to obtain culture-positive documentation of deep TKA infection; however, the authors believe operative intervention for TKA infection serves as an appropriate surrogate for this essential endpoint. Arguably the largest limitation to this study is that current CPT coding does not allow differentiation of anatomic site of injection and the CPT code 20610 used in this study includes all major joints (shoulder, hip, and knee). However, given that the sequence of major joint injection followed by ipsilateral TKA in patients with symptomatic knee pain (assumed based on the need for TKA) was confirmed for all patients in the injection cohort, the authors feel that assuming the vast majority of these injections included in this analysis occurred in the knee is a valid assumption. Lastly, the specific medication injected into the knee is not available within the data set. However, despite this information not being available, the data still allow for conclusions to be made regarding the impact an injection itself before TKA may have on the risk of postoperative infection. Although the risk of any postoperative infection is slightly higher than that reported from other large database studies, it is important to note that this risk is for infection occurring out to 6 months postoperatively as opposed to the initial hospital stay or the first postoperative month, which is the timeframe many large databases are limited to.
We found only five other studies that investigated risk of TKA infection after intraarticular steroid injection [3–5, 9, 15]. Of these studies, four were underpowered given the relatively low frequency of postoperative TKA infection with only 64 to 250 patients included in the analysis, likely contributing to the discrepant results found within these studies [4, 5, 9, 15]. Among these five studies, there was only one other large database study that had a large enough cohort to sufficiently evaluate the risk of TKA infection after intraarticular injection. This study was performed by Cancienne et al. [3], who analyzed 35,890 unique Medicare patients undergoing primary TKA. In general, the findings of the present study corroborated those of Cancienne et al. [3] who reported an increased odds of infection at both 3 and 6 months after TKA for patients with a history of ipsilateral knee injection within 3 months before TKA (ORs of 2.0 and 1.5 for those time points, respectively). They reported no difference in infection risks if the injection had occurred 3 to 6 months or 6 to 12 months before TKA [3]. Although these results are overall supportive of results in our study, limitations with this analysis necessitated further research on this topic to better characterize the risk injection may pose to TKA infection. The study by Cancienne et al. [3] was performed on a Medicare-only cohort, thus limiting the broader applicability of their results to the younger population and the non-Medicare demographic of patients undergoing TKA. Additionally, the analysis of the Humana data set allowed for a larger number of TKA cases in both the injection and noninjection cohorts, thus further increasing the power of this analysis. Furthermore, as a result of the manner in which the data from Medicare are provided to PearlDiver for research, the tracking of patients before 2010 within the Medicare data is limited to tracking in 3-month time blocks, thus preventing a more detailed month-by-month analysis of the effects of time between injection and TKA and the subsequent risk of TKA infection. Lastly, the authors of the present study believe the use of two different definitions of infection (all postoperative TKA infections and operative intervention for infection), as opposed to one inclusive definition, allows for a more detailed analysis of the effects injection may have on TKA infection, specifically the use of a definition limited to operative intervention of infection, which presumably helps to eliminate the inclusion of small wound complications that are likely captured in the more inclusive definitions used in Cancienne et al.’s [3] study and the present study’s definition of all postoperative TKA infection as evidenced by the higher risk of infection identified with these endpoints. Nonetheless, both the current study and the study by Cancienne et al. [3] have adequately raised concern for the effect a preoperative injection may have on the risk of TKA infection and have identified an important relationship in need of further research.
The data from this current study suggest that there is an increased risk of postoperative TKA infection when patients have undergone an ipsilateral knee injection before undergoing primary TKA. The risk of postoperative infection also appears to be time-dependent with closer proximity between injection and TKA having a higher odds of infection out to a 6- to 7-month duration between injection and TKA. If time between injection and TKA becomes longer than 6 to 7 months, we found no increased risk of infection after subsequent TKA. Despite these findings, further research is needed to better clarify this relationship between injection and TKA infection, which would best be studied with a multivariate analysis to control for other known risk factors for TKA infection or with a prospective, multicenter study design.
Footnotes
One of the authors (JJC), or a member of his or her immediate family, has or may receive payments or benefits, during the study period, an amount of more than USD 1,000,001, from royalties and consulting for DePuy (Warsaw, IN, USA) for intellectual property transfer for hip and knee implant designs and an amount of less than USD 10,000, for royalties from Wolters Kluwer (Baltimore, MD, USA) for books edited.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
This work was performed at the University of Iowa, Iowa City, IA, USA.
References
- 1.Bellamy N, Campbell J, Robinson V, Gee T, Bourne R, Wells G. Intraarticular corticosteroid for treatment of osteoarthritis of the knee. Cochrane Database Syst Rev. 2006;2:CD005328. [DOI] [PubMed]
- 2.Blom AW, Brown J, Taylor AH, Pattison G, Whitehouse S, Bannister GC. Infection after total knee arthroplasty. J Bone Joint Surg Br. 2004;86:688–691. doi: 10.1302/0301-620X.86B5.14887. [DOI] [PubMed] [Google Scholar]
- 3.Cancienne JM, Werner BC, Luetkemeyer LM, Browne JA. Does timing of previous intra-articular steroid injection affect the post-operative rate of infection in total knee arthroplasty? J Arthroplasty. 2015;30:1879–1882. doi: 10.1016/j.arth.2015.05.027. [DOI] [PubMed] [Google Scholar]
- 4.Desai A, Ramankutty S, Board T, Raut V. Does intraarticular steroid infiltration increase the rate of infection in subsequent total knee replacements? Knee. 2009;16:262–264. doi: 10.1016/j.knee.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 5.Horne G, Devane P, Davidson A, Adams K, Purdie G. The influence of steroid injections on the incidence of infection following total knee arthroplasty. N Z Med J. 2008;121:U2896. [PubMed] [Google Scholar]
- 6.Jamsen E, Huhtala H, Puolakka T, Moilanen T. Risk factors for infection after knee arthroplasty: a register-based analysis of 43,149 cases. J Bone Joint Surg Am. 2009;91:38–47. doi: 10.2106/JBJS.G.01686. [DOI] [PubMed] [Google Scholar]
- 7.Jamsen E, Varonen M, Huhtala H, Lehto MU, Lumio J, Konttinen YT, Moilanen T. Incidence of prosthetic joint infections after primary knee arthroplasty. J Arthroplasty. 2010;25:87–92. doi: 10.1016/j.arth.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 8.Jevsevar DS, Brown GA, Jones DL, Matzkin EG, Manner PA, Mooar P, Schousboe JT, Stovitz S, Sanders JO, Bozic KJ, Goldberg MJ, Martin WR, 3rd, Cummins DS, Donnelly P, Woznica A, Gross L. The American Academy of Orthopaedic Surgeons evidence-based guideline on: treatment of osteoarthritis of the knee, 2nd edition. J Bone Joint Surg Am. 2013;95:1885–1886. doi: 10.2106/00004623-201310160-00010. [DOI] [PubMed] [Google Scholar]
- 9.Joshy S, Thomas B, Gogi N, Modi A, Singh BK. Effect of intra-articular steroids on deep infections following total knee arthroplasty. Int Orthop. 2006;30:91–93. doi: 10.1007/s00264-005-0035-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, Gabriel S, Hirsch R, Hochberg MC, Hunder GG, Jordan JM, Katz JN, Kremers HM, Wolfe F. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58:26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marsland D, Mumith A, Barlow IW. Systematic review: the safety of intra-articular corticosteroid injection prior to total knee arthroplasty. Knee. 2014;21:6–11. doi: 10.1016/j.knee.2013.07.003. [DOI] [PubMed] [Google Scholar]
- 12.Minnema B, Vearncombe M, Augustin A, Gollish J, Simor AE. Risk factors for surgical-site infection following primary total knee arthroplasty. Infect Control Hosp Epidemiol. 2004;25:477–480. doi: 10.1086/502425. [DOI] [PubMed] [Google Scholar]
- 13.Murphy MV, Du D, Hua W, Cortez KJ, Butler MG, Davis RL, DeCoster T, Johnson L, Li L, Nakasato C, Nordin JD, Ramesh M, Schum M, Von Worley A, Zinderman C, Platt R, Klompas M. The utility of claims data for infection surveillance following anterior cruciate ligament reconstruction. Infect Control Hosp Epidemiol. 2014;35:652–659. doi: 10.1086/676430. [DOI] [PubMed] [Google Scholar]
- 14.Nero DC, Lipp MJ, Callahan MA. The financial impact of hospital-acquired conditions. J Health Care Finance. 2012;38:40–49. [PubMed] [Google Scholar]
- 15.Papavasiliou AV, Isaac DL, Marimuthu R, Skyrme A, Armitage A. Infection in knee replacements after previous injection of intra-articular steroid. J Bone Joint Surg Br. 2006;88:321–323. doi: 10.1302/0301-620X.88B3.17136. [DOI] [PubMed] [Google Scholar]
- 16.Rasouli MR, Restrepo C, Maltenfort MG, Purtill JJ, Parvizi J. Risk factors for surgical site infection following total joint arthroplasty. J Bone Joint Surg Am. 2014;96:e158. doi: 10.2106/JBJS.M.01363. [DOI] [PubMed] [Google Scholar]
- 17.Singh JA, Kundukulam JA, Bhandari M. A systematic review of validated methods for identify orthopedic implant removal and revision using administrative data. Pharmaoepidemiol Drug Saf. 2012;21(Suppl 1):265–273. doi: 10.1002/pds.2309. [DOI] [PubMed] [Google Scholar]
- 18.Willis-Owen CA, Konyves A, Martin DK. Factors affecting the incidence of infection in hip and knee replacement: an analysis of 5277 cases. J Bone Joint Surg Br. 2010;92:1128–1133. doi: 10.1302/0301-620X.92B8.24333. [DOI] [PubMed] [Google Scholar]
- 19.Wilson MG, Kelley K, Thornhill TS. Infection as a complication of total knee-replacement arthroplasty. Risk factors and treatment in sixty-seven cases. J Bone Joint Surg Am. 1990;72:878–883. doi: 10.2106/00004623-199072060-00013. [DOI] [PubMed] [Google Scholar]