Abstract
Background
Physicians have consistently shown poor adverse-event reporting practices in the literature and yet they have the clinical acumen to properly stratify and appraise these events. The Spine Adverse Events Severity System (SAVES) and Orthopaedic Surgical Adverse Events Severity System (OrthoSAVES) are standardized assessment tools designed to record adverse events in orthopaedic patients. These tools provide a list of prespecified adverse events for users to choose from—an aid that may improve adverse-event reporting by physicians.
Questions/Purposes
The primary objective was to compare surgeons’ adverse-event reporting with reporting by independent clinical reviewers using SAVES Version 2 (SAVES V2) and OrthoSAVES in elective orthopaedic procedures.
Method
This was a 10-week prospective study where SAVES V2 and OrthoSAVES were used by six orthopaedic surgeons and two independent, non-MD clinical reviewers to record adverse events after all elective procedures to the point of patient discharge. Neither surgeons nor reviewers received specific training on adverse-event reporting. Surgeons were aware of the ongoing study, and reported adverse events based on their clinical interactions with the patients. Reviewers recorded adverse events by reviewing clinical notes by surgeons and other healthcare professionals (such as nurses and physiotherapists). Adverse events were graded using the severity-grading system included in SAVES V2 and OrthoSAVES. At discharge, adverse events recorded by surgeons and reviewers were recorded in our database.
Results
Adverse-event data for 164 patients were collected (48 patients who had spine surgery, 51 who had hip surgery, 34 who had knee surgery, and 31 who had shoulder surgery). Overall, 99 adverse events were captured by the reviewers, compared with 14 captured by the surgeons (p < 0.001). Surgeons adequately captured major adverse events, but failed to record minor events that were captured by the reviewers. A total of 93 of 99 (94%) adverse events reported by reviewers required only simple or minor treatment and had no long-term adverse effect. Three patients experienced adverse events that resulted in use of invasive or complex treatment that had a temporary adverse effect on outcome.
Conclusion
Using SAVES V2 and OrthoSAVES, independent reviewers reported more minor adverse events compared with surgeons. The value of third-party reviewers requires further investigation in a detailed cost-benefit analysis.
Level of Evidence
Level II, therapeutic study.
Introduction
Accurate reporting and tracking of adverse events is essential to understanding complications, and subsequently implementing programs to decrease morbidity and mortality. Adverse events can have a substantial economic burden on the healthcare system and a negative effect on overall patient outcomes [21, 29]. Not only is this important regarding the value of care provided to patients but also to overall patient experience and the capacity to improve quality [3, 27]. Although surgeons understand the importance of adverse events, tracking and reporting are weaknesses in the clinical and research environment [2, 25, 43]. A major contributor to these weaknesses lies in the lack of standardized definitions of adverse events [22, 34], with variations of the same adverse events identified across studies [4, 5, 9, 22, 34]. In response to this deficiency, standardized definitions of adverse events have been proposed [16, 17], with the Clavien-Dindo classification being commonly used and reported [7, 10].
Specifically in orthopaedics, Rampersaud et al. developed [32] and validated [33] the Spine Adverse Events Severity System (SAVES), where adverse events are divided in 14 intraoperative and 22 postoperative events, and an “Others” section, with each event graded on a severity scale from 1 to 6. Finally, based on the recorded events, users are prompted to estimate the effect on length of stay. The Orthopaedic Surgical Adverse Events Severity System (OrthoSAVES) is a modification of SAVES that provides events that are applicable to orthopaedics in general as opposed to being spine-specific. The provided list of adverse events in SAVES and OrthoSAVES serves as a prompt for users while also improving convenience of reporting; rather than writing out specific adverse events, users simply check them off on the form. Combined, these features may prove helpful in improving adverse-event reporting by physicians.
The primary objective of this study was to compare the rate of adverse-event reporting by surgeons versus independent clinical reviewers using SAVES and OrthoSAVES in elective orthopaedic procedures.
Methods
This study was a prospective observational analysis of patients undergoing elective orthopaedic spine, hip, knee, and shoulder surgery at a tertiary academic teaching hospital during a 10-week period between June 29, 2015 and September 4, 2015. All patients scheduled for elective surgery, inpatient and outpatient, during this period with the six participating surgeons (GD, PL, PP, EKW, SPK, PEB) were included. Exclusion criteria included patients with trauma or oncologic surgery. This study was approved by the local institutional ethics review board.
During the 10-week study period, 164 patients (48 undergoing spine surgery, 51 having hip surgery, 34 undergoing knee surgery, and 31 having shoulder surgery) underwent elective surgery with participating surgeons. Adverse-event data were reported with SAVES Version 2 (SAVES V2) for patients having spine surgery and OrthoSAVES for patients having hip, knee, or shoulder surgery.
In the hip and knee, arthroplasty accounted for the majority of the procedures. THA (including hip resurfacing) and revisions together accounted for 69% of hip procedures, while knee arthroplasties, including total and unicompartmental, accounted for 88% of knee procedures. In the shoulder, only 10 of 31 procedures (32%) were arthroplasties whereas 19 of 31 (61%) arthroscopic procedures were in the shoulder. This is in contrast to the lower proportion of arthroscopic procedures in the hip (24%) and knee (6%) (Table 1). Among all sites, four revision surgeries were performed: one hip arthroplasty, one hip resurfacing, and two shoulder arthroplasties (Table 2).
Table 1.
Patient demographics and operative details
| Variable | Spine (n = 48 patients) | Hip (n = 51 patients) | Knee (n = 34 patients) | Shoulder (n = 31 patients) |
|---|---|---|---|---|
| Age (years) | 56 (15) | 49 (17) | 59 (14) | 54 (13) |
| Male gender | 25 (52%) | 29 (57%) | 14 (41%) | 15 (48%) |
| BMI, kg/m2 | 30 (6) | 27 (5) | 29 (5) | 28 (7) |
| Smokers | 10 (21%) | 6 (12%) | 4 (12%) | 10 (32%) |
| Time of operation (minutes) | 211 (128–294) | 79 (66–96) | 72 (62–77) | 78 (62–107) |
| Outpatient surgery | 16 (33%) | 13 (26%) | 8 (24%) | 19 (62%) |
| Arthroscopic surgery | N/A | 12 (24%) | 2 (6%) | 19 (61%) |
Data presented as mean (SD), median (Quartile 1- Quartile 3), or frequency (%); N/A = not applicable
Table 2.
Procedures performed at each site (spine, hip, knee, and shoulder)
| Site | Number of procedures |
|---|---|
| Spine | |
| Discectomy & fusion | 22 |
| Microdiscectomy | 14 |
| Mixed laminectomy and discectomy & fusion | 5 |
| Minimally invasive discectomy & fusion | 2 |
| Laminectomy & fusion | 2 |
| Discectomy | 1 |
| Mixed discectomy and corpectomy & fusion | 1 |
| Corpectomy & fusion | 1 |
| Hip | |
| THA | 22 |
| Hip resurfacing | 11 |
| Arthroscopy – chondroosteoplasty head neck junction, acetabular rim trimming | 9 |
| Periacetabular osteotomy | 4 |
| Arthroscopy – labral chondroosteoplasty, débridement | 3 |
| Revision hip arthroplasty and resurfacing | 2 |
| Knee | |
| TKA | 17 |
| Unicompartmental knee arthroplasty | 13 |
| Arthroscopy – ACL reconstruction, medial patellofemoral ligament reconstruction | 2 |
| Patellar tendon repair | 1 |
| Open débridement and polyethylene liner exchange | 1 |
| Shoulder | |
| Arthroscopy – rotator cuff repair, biceps release | 16 |
| Total shoulder arthroplasty, including reverse | 8 |
| Arthroscopy – labral repair, débridement | 3 |
| Open Bankart repair | 2 |
| Revision shoulder arthroplasty | 2 |
Adverse-event data were prospectively and independently collected by clinical reviewers (BPC, KG [two first-year medical students]) and surgeons (GD, PL, PP, EKW, SPK, PEB [either attending staff surgeon or orthopaedic surgical resident]). Each team was blinded to the other’s data. SAVES V2 and OrthoSAVES forms were included in the patients’ charts and surgeons recorded adverse events on an ongoing basis based on their clinical interactions and knowledge of their patients. Reviewers thoroughly reviewed the patients’ physical and electronic charts on a daily basis from the time of surgery until discharge to extract adverse-event data. In addition, they had access to all healthcare professionals involved in the patients’ care, except for the surgeons. The reviewers were not involved in the patients’ care and did not interact with the patients. Surgeons and reviewers consulted the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP®) manual [1] for the definition and criteria for individual adverse events. Adverse events were graded using the six-point classification system included in the SAVES V2 and OrthoSAVES tools [42]. Grade 1 is defined as an event that does not require treatment and has no adverse effect. Grade 2 events require simple or minor treatment, but have no long-term effect on patient outcome. Grades 3 and 4 events require invasive or complex treatment (eg, surgery or monitored bed). Grade 3 events have a temporary (< 6 month) adverse effect while Grade 4 events have a prolonged (> 6 month) adverse effect. Grade 5 events are life or limb threatening or necessitate institutional investigation. Grade 6 is an event resulting in patient death. Minor complications were defined as Grade 1 and Grade 2, while Grade 3 and higher were considered major complications.
Neither reviewers nor surgeons received specific training in using the SAVES V2 and OrthoSAVES tools or adverse-event reporting. If SAVES V2 or OrthoSAVES forms were not completed in full by the surgeons by the time the patient was discharged, the forms were returned to the attending surgeon immediately to be completed. The primary outcome was the number of adverse events recorded by surgeons and reviewers. Secondary outcomes included complication rate and severity of adverse events. Patients were considered to have experienced a complication if at least one adverse event was recorded. Statistical analysis was performed using SAS® version 9.4 (SAS Institute, Cary, NC, USA). Chi-square and McNemar’s tests were used to compare categorical variables, and the Wilcoxon signed-rank test was used to compare adverse events per patient. Data are presented in median (SD), median (Quartile 1-Quartile 3), or frequency (%) unless otherwise indicated. A two-tailed p value less than 0.05 was considered statistically significant.
Results
Reviewers recorded more total and postoperative adverse events than surgeons (p < 0.001). In total, reviewers recorded 99 adverse events in 57 patients while surgeons recorded 14 adverse events in 12 patients (Table 3). Of the 99 adverse events recorded by reviewers, four were intraoperative and 95 were postoperative. Surgeons recorded two intraoperative and 12 postoperative events. All intraoperative events were in patients having spine procedures and no difference was found between reviewers and surgeons with the sample size available (p = 0.500). At the spine, hip, and knee, reviewers recorded more total adverse events than surgeons (spine, 45 vs 8, p < 0.001; hip, 23 vs 2, p < 0.001; knee, 21 vs 2, p < 0.001), but no difference was found in patients undergoing shoulder procedures with the available sample size (10 vs 2, p = 0.125). Most patients had Grade 1 or 2 adverse events; only three patients had an adverse event more severe than Grade 2. While reviewers recorded more Grades 1 and 2 adverse events than surgeons (Grade 1, 31 vs 2, p < 0.001; Grade 2, 62 vs 8, p < 0.001), there was no difference in capturing Grade 3 adverse events (6 vs 4, p = 0.5). Reviewers and surgeons recorded six and four Grade 3 adverse events, respectively. All four Grade 3 adverse events recorded by the surgeons also were recorded by the reviewers. Reviewers recorded two additional Grade 3 adverse events (pseudoaneurysm and neurologic deterioration) that were not recorded by surgeons. Neurologic deterioration was not recorded by surgeons at all, whereas pseudoaneurysm was recorded, albeit rated as Grade 2 rather than Grade 3 (Table 4).
Table 3.
Number of adverse events per patient
| Frequency | Median (Quartile 1-Quartile 3) | Mean (SD) | p Value | ||||
|---|---|---|---|---|---|---|---|
| Variable | Reviewer | Surgeon | Reviewer | Surgeon | Reviewer | Surgeon | |
| Total adverse events | 99 | 14 | 0 (0–1) | 0 (0–0) | 0.604 (1.08) | 0.0854 (0.340) | < 0.0001 |
| Intraoperative | 4 | 2 | 0 (0–0) | 0 (0–0) | 0.0244 (0.155) | 0.0122 (0.110) | 0.500 |
| Postoperative | 95 | 12 | 0 (0–1) | 0 (0–0) | 0.579 (1.02) | 0.0732 (0.284) | < 0.0001 |
| Comparison by site | |||||||
| Spine | 45 | 8 | 0 (0–1.5) | 0 (0–0) | 0.938 (1.39) | 0.167 (0.519) | < 0.0001 |
| Hip | 23 | 2 | 0 (0–1) | 0 (0–0) | 0.451 (0.673) | 0.0390 (0.196) | < 0.0001 |
| Knee | 21 | 2 | 0 (0–1) | 0 (0–0) | 0.618 (1.21) | 0.0590 (0.239) | 0.0005 |
| Shoulder | 10 | 2 | 0 (0–0) | 0 (0–0) | 0.323 (0.832) | 0.0650 (0.250) | 0.125 |
| Severity* | |||||||
| Grade 1 | 31 | 2 | 0 (0–0) | 0 (0–0) | 0.189 (0.502) | 0.0122 (0.110) | < 0.0001 |
| Grade 2 | 62 | 8 | 0 (0–1) | 0 (0–0) | 0.378 (0.729) | 0.0488 (0.216) | < 0.0001 |
| Grade 3 | 6 | 4 | 0 (0–0) | 0 (0–0) | 0.0366 (0.330) | 0.0244 (0.246) | 0.500 |
Reviewer versus surgeon compared with Wilcoxon signed-rank test;* based on severity grading system provided in SAVES and OrthoSAVES.
Table 4.
Summary of reported Grade 3 adverse events
| Patient | Procedure | Reviewer-reported | Surgeon-reported |
|---|---|---|---|
| 1 | Revision decompression (L4-L5) via laminectomy, discectomy, and foraminotomy |
Dural tear Cerebrospinal fluid leak/ meningocele Hematoma Neurologic deterioration |
Dural tear Cerebrospinal fluid leak/ meningocele Hematoma |
| 2 | TKA | Pseudoaneurysm | None |
| 3 | TKA | Pulmonary embolism | Pulmonary embolism |
Surgeon also recorded pseudoaneurysm, but rated it as Grade 2 rather than Grade 3.
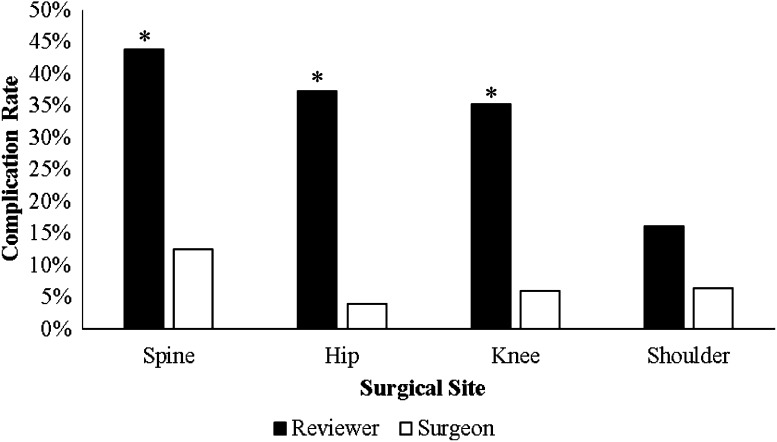
At the spine, hip, and knee, the adverse-event rate was higher when relying on event data from the reviewers compared with from the surgeons (spine, 21/48 [44%] vs 6/48 [13%], p < 0.001; hip, 19/51 [37%] vs 2/51 [4%], p < 0.001; knee, 12/34 [35%] vs 2/34 [6%], p = 0.002), but with the numbers available, we found no differences in patients undergoing shoulder surgery (5/31 [16%] vs 2/31 [7%], p = 0.25) (Fig. 1).
Fig. 1.
The complication rates based on adverse-event data provided by the reviewers and the surgeons are shown. *p < 0.01 compared with surgeons at the corresponding site.
Most commonly reported adverse events differed by type of procedure. Using the reviewers’ data, in the spine, serous drainage and postoperative neuropathic pain accounted for 13% and 11% of all adverse events, respectively. In the hip and knee, the most common adverse event was urinary retention, accounting for 14 of 23 and eight of 21 events, respectively. In the shoulder, airway or ventilation and hypotension each accounted for three of 10 adverse events (Table 5).
Table 5.
Adverse events experienced by patients
| Site | Number of events |
|---|---|
| Spine | |
| Serous drainage | 6 |
| Postoperative neuropathic pain | 5 |
| Hypertension | 4 |
| Emesis | 3 |
| Headache | 3 |
| Cardiac arrest/failure/arrhythmia | 2 |
| Dysphagia | 2 |
| Paresthesia | 2 |
| Epigastric pain | 2 |
| Anemia | 2 |
| Anesthesia-related | 1 |
| Dural tear | 1 |
| Hardware malposition requiring revision | 1 |
| Vascular injury | 1 |
| Cerebrospinal fluid leak/meningocele | 1 |
| Hematoma | 1 |
| Neurologic deterioration | 1 |
| Spasms | 1 |
| Fall | 1 |
| Hyponatremia | 1 |
| Muscle cramp | 1 |
| Urinary retention | 1 |
| Hypotension | 1 |
| New foot drop | 1 |
| Hip | |
| Urinary retention | 14 |
| Hypotension | 5 |
| Cutaneous injury | 2 |
| Airway/ventilation | 1 |
| Postoperative neuropathic pain | 1 |
| Knee | |
| Urinary retention | 8 |
| Hypotension | 3 |
| Hypertension | 2 |
| Cutaneous injury | 2 |
| Decreased level of consciousness | 1 |
| Airway/ventilation | 1 |
| Pulmonary embolism | 1 |
| Serous drainage | 1 |
| Anemia | 1 |
| Pseudoaneurysm | 1 |
| Shoulder | |
| Airway/ventilation | 3 |
| Hypotension | 3 |
| Fever | 2 |
| Anemia | 1 |
| Urinary retention | 1 |
On review, 40% of forms were not fully completed at discharge and had to be returned to the attending surgeon. Among the 65 patients for whom forms were incomplete by the time of discharge and thus retrospectively completed by the surgeon, five had adverse events recorded, translating to a complication rate of 7.7%. This is comparable to the adverse-event rate of the other 99 patients for whom surgeons completed the forms prospectively and by the time of discharge. Among these 99 patients, seven (7.1%) had at least one adverse event.
Discussion
Adverse events are becoming increasingly relevant given that the population is aging and postoperative complications increase with age [11, 12, 15, 28, 31, 32]. Although the clinical importance of minor adverse events is controversial [14], the economic burden should be considered. While minor adverse events are less costly individually, they appear with high frequency, thus contributing to more than half of the total costs of adverse events [18, 44]. Furthermore, these events are the most potentially preventable [18], further enhancing the rationale for addressing them. Unfortunately, poor adverse-event reporting by physicians is well-documented in the literature [24, 35, 37]. SAVES and OrthoSAVES may help tackle this issue as the list of adverse events serves as a prompt while also improving convenience of reporting. In the current study, reviewers documented 99 adverse events in patients undergoing elective spine, hip, knee, and shoulder surgery during a 10-week period, of which 93 were Grade 1 or 2 events. In comparison, surgeons reported only 14 adverse events in the same cohort of patients. Another argument for reviewers to prospectively collect adverse event data is the ability to foster timely “point-of-care” interventions. Not only can reviewers serve to improve adverse-event tracking, but they also could inform the clinical team of any patient safety concerns. Whether these benefits are worth the cost of reviewers is unclear and requires further investigation.
Our study had several limitations. First, no formal training was provided to the reviewers or surgeons on the use of SAVES and OrthoSAVES. Thus they learned as the study progressed, which may result in increasing adverse-event capture rates as they became more familiar with the tools. This trend was not observed in our study however. With the first half of the patients, reviewers and surgeons collected 46 and eight adverse events, respectively, while with the second half of the patients, 52 and six adverse events were collected by reviewers and surgeons, respectively. This shows that SAVES and OrthoSAVES are easy-to-use tools that require minimal training. Another limitation is the lack of a gold standard for comparison, which makes it difficult to determine whether surgeons underreported, reviewers overreported, or perhaps a combination of both. However, given that adverse events currently are poorly tracked, it is debatable regarding whether there is a true gold standard and whether such comparisons are useful. Finally, our study was of short duration (10 weeks). A longer duration may lead to better orientation to the tool for surgeons and reviewers and allow for clearer assessment of its long-term viability.
Our finding of poor reporting of adverse events by physicians (in particular, poor reporting of minor adverse events) is congruent with the work of others [24, 35, 37]. In an analysis of 92,547 error and adverse-event reports submitted through an electronic reporting system, only 1.4% of reports were submitted by physicians, compared with 47% submitted by registered nurses [24]. Similarly, in another analysis of 266,244 reports, physicians and nurses submitted 1% and 45% of reports, respectively [35]. Physicians were more likely to report events of higher effect and severity [35, 37], which is also in line with our findings. Schectman and Plews-Ogan [36] surveyed physicians to assess their perceptions of hospital safety and barriers to reporting adverse events. Several important reasons for failure to report these events include being unsure of the reporting mechanism, no actual harm was done to the patient, and the process of reporting being too time consuming. Surveyed physicians believed that allowing electronic reporting of adverse events, clarifying reporting mechanisms, and defining what constitutes an adverse event would likely increase reporting of events [36]. These barriers may help explain the low capture rate of minor adverse events by surgeons in our study. Despite their awareness of the ongoing study, they may not have fully understood what events were reportable; this may be particularly relevant where minor events that cause no harm or adverse effect to the patient are concerned.
In our study, 38% of SAVES V2 and OrthoSAVES forms were not completed by the surgeons by the time of patient discharge. In another study that also relied on surgeons and healthcare staff to collect adverse-event data prospectively using the SAVES V2, the rate of incompletion by the time of discharge was 22% [42]. In both studies, substantial proportions of forms were not completed by the time of patient discharge, requiring the forms to be returned to the attending surgeons to be completed retrospectively. This weakens the quality of adverse-event reporting as the underlying premise is that the data collected prospectively are superior to retrospective data [6, 8, 42]. Our data showed similar complication rates among prospectively and retrospectively collected data. Any interpretation of these values must be done with caution however, as the total number of adverse events recorded by surgeons is small. Furthermore, because attending surgeons usually completed the forms within a few days after discharge, during which time they likely have a strong recollection of the patient’s course in the hospital, it is not expected that adverse-event capture rates should differ importantly.
Among patients having spine surgery, we reported an overall complication rate of 44% using reviewer-collected adverse-event data. This is lower than the complication rate of 87% among patients having spine procedures reported by Street et al. [42]. They also used SAVES V2, but instead of having independent reviewers track adverse events, surgeons, nurses, and other healthcare professionals involved in the patients’ care met on a weekly basis to discuss each patient and record adverse events. Another important difference is that their study included patients treated emergently or for oncologic surgery, whereas we included only patients having elective nononcologic and nontrauma surgery. Emergency cases, as reported by Street et al. [42], were associated with increased intraoperative adverse-event rates and accounted for 95% (19 of 20) of mortalities. Their patients treated with oncologic surgery, electively and emergently, experienced higher rates of postoperative adverse events [42].
In 2004, Dindo et al. [10] developed a classification system for surgical complications, which subsequently has been adapted to several surgical specialties. High interobserver and intraobserver reliabilities have been reported for a version of this classification adapted for orthopaedic surgery [39, 40]. Other instruments, such as the Memorial Sloan Kettering and the Accordion severity grading systems [23, 41], are similar in that severity is graded based on the extent of treatment required and patient outcome. The SAVES and OrthoSAVES tools use a similar severity grading scale, but the key advantage is that specific adverse events common to orthopaedic surgery are listed to prompt users. Perhaps a more modern alternative to these reporting systems relies on automated processes. A study using natural language processing to identify postoperative complications showed higher sensitivity compared with discharge coding with patient safety indicators, albeit with lower specificity [26].
Historically, numerous reports of surgical adverse events were derived retrospectively [13, 19, 20, 30, 38]; our study was prospective. Prior work suggests that retrospective collection of adverse-event data results in underreporting [8, 42]. In a prospective study of adverse events experienced by patients who had undergone emergency spinal surgery for metastatic spine disease, Dea et al. [8] reported an overall complication rate of 76%, higher than previously reported rates of 7% to 39% in retrospective studies [13, 19, 20, 30, 38]. Similarly, Street et al. [42] showed that complication rates, particularly postoperatively, were higher when data were collected prospectively rather than retrospectively. One may argue that since the bulk of adverse-event data reported by the reviewers in our study were extracted from the patients’ charts, there is no difference regarding whether this is done prospectively or retrospectively. However, nurses, physiotherapists, and other healthcare professionals who were knowledgeable about the patients were an important resource for the reviewers that should not be overlooked. This access allowed the reviewers to clarify any issues immediately, which cannot be done if data were collected retrospectively.
We showed that using SAVES V2 and OrthoSAVES in elective orthopaedic surgery, reviewers captured more adverse events compared with surgeons. Although most of the differences were found in reporting of minor complications, these complications can be associated with substantial cumulative costs [18]. However, the cost-benefit of third-party reviewers is unclear. Future studies should aim to provide detailed analysis of the costs of reviewers and the cost savings that they bring by capturing minor complication. Such studies also should evaluate whether identification of these events in real time can assist the clinicians in reducing the frequency of these events or minimizing the costs associated with treating them.
Acknowledgments
We thank Tinghua Zhang MSc (Methods Center, Ottawa Hospital Research Institute) for assistance with statistical analysis.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that a waiver of informed consent for the study was obtained.
This study was performed at the Division of Orthopaedic Surgery, The Ottawa Hospital.
A comment to this article is available at http://dx.doi.org/10.1007/s11999-016-5142-3.
References
- 1.American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP®). Chapter 4: Variables & Definitions. ACS NSQIP®Operations Manual. Available at: http://www.aast.org/Assets/fe526f57-5bd3-4700-94bc-497b035551db/635282483441930000/nsqip-definitions-7-1-2013-pdf. Accessed July 29, 2016.
- 2.Bilimoria KY, Kmiecik TE, DaRosa DA, Halverson A, Eskandari MK, Bell RH Jr, Soper NJ, Wayne JD. Development of an online morbidity, mortality, and near-miss reporting system to identify patterns of adverse events in surgical patients. Arch Surg. 2009;144:305–311; discussion 311. [DOI] [PubMed]
- 3.Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468:57–63. doi: 10.1007/s11999-009-1119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bruce J, Krukowski ZH, Al-Khairy G, Russell EM, Park KG. Systematic review of the definition and measurement of anastomotic leak after gastrointestinal surgery. Br J Surg. 2001;88:1157–1168. doi: 10.1046/j.0007-1323.2001.01829.x. [DOI] [PubMed] [Google Scholar]
- 5.Bruce J, Russell EM, Mollison J, Krukowski ZH. The quality of measurement of surgical wound infection as the basis for monitoring: a systematic review. J Hosp Infect. 2001;49:99–108. doi: 10.1053/jhin.2001.1045. [DOI] [PubMed] [Google Scholar]
- 6.Campbell PG, Malone J, Yadla S, Chitale R, Nasser R, Maltenfort MG, Vaccaro A, Ratliff JK. Comparison of ICD-9-based, retrospective, and prospective assessments of perioperative complications: assessment of accuracy in reporting. J Neurosurg Spine. 2011;14:16–22. doi: 10.3171/2010.9.SPINE10151. [DOI] [PubMed] [Google Scholar]
- 7.Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibanes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–196. doi: 10.1097/SLA.0b013e3181b13ca2. [DOI] [PubMed] [Google Scholar]
- 8.Dea N, Versteeg A, Fisher C, Kelly A, Hartig D, Boyd M, Paquette S, Kwon BK, Dvorak M, Street J. Adverse events in emergency oncological spine surgery: a prospective analysis. J Neurosurg Spine. 2014;21:698–703. doi: 10.3171/2014.7.SPINE131007. [DOI] [PubMed] [Google Scholar]
- 9.Dekutoski MB, Norvell DC, Dettori JR, Fehlings MG, Chapman JR. Surgeon perceptions and reported complications in spine surgery. Spine (Phila Pa 1976). 2010;35(9 suppl):S9–21. [DOI] [PubMed]
- 10.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Etzioni DA, Liu JH, Maggard MA, Ko CY. The aging population and its impact on the surgery workforce. Ann Surg. 2003;238:170–177. doi: 10.1097/01.SLA.0000081085.98792.3d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fang M, Noiseux N, Linson E, Cram P. The effect of advancing age on total joint replacement outcomes. Geriatr Orthop Surg Rehabil. 2015;6:173–179. doi: 10.1177/2151458515583515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fu KM, Smith JS, Polly DW, Jr, Perra JH, Sansur CA, Berven SH, Broadstone PA, Choma TJ, Goytan MJ, Noordeen HH, Knapp DR, Jr, Hart RA, Zeller RD, Donaldson WF, 3rd, Boachie-Adjei O, Shaffrey CI. Morbidity and mortality in the surgical treatment of 10,329 adults with degenerative lumbar stenosis. J Neurosurg Spine. 2010;12:443–446. doi: 10.3171/2009.11.SPINE09531. [DOI] [PubMed] [Google Scholar]
- 14.Glassman SD, Hamill CL, Bridwell KH, Schwab FJ, Dimar JR, Lowe TG. The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine (Phila Pa 1976). 2007;32:2764–2770. [DOI] [PubMed]
- 15.Gruson KI, Accousti KJ, Parsons BO, Pillai G, Flatow EL. Transfusion after shoulder arthroplasty: an analysis of rates and risk factors. J Shoulder Elbow Surg. 2009;18:225–230. doi: 10.1016/j.jse.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 16.Healy WL, Della Valle CJ, Iorio R, Berend KR, Cushner FD, Dalury DF, Lonner JH. Complications of total knee arthroplasty: standardized list and definitions of the Knee Society. Clin Orthop Relat Res. 2013;471:215–220. doi: 10.1007/s11999-012-2489-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Healy WL, Iorio R, Clair AJ, Pellegrini VD, Della Valle CJ, Berend KR. Complications of total hip arthroplasty: standardized list, definitions, and stratification developed by The Hip Society. Clin Orthop Relat Res. 2016;474:357–364. doi: 10.1007/s11999-015-4341-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hellsten EK, Hanbidge MA, Manos AN, Lewis SJ, Massicotte EM, Fehlings MG, Coyte PC, Rampersaud YR. An economic evaluation of perioperative adverse events associated with spinal surgery. Spine J. 2013;13:44–53. doi: 10.1016/j.spinee.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 19.Hirabayashi H, Ebara S, Kinoshita T, Yuzawa Y, Nakamura I, Takahashi J, Kamimura M, Ohtsuka K, Takaoka K. Clinical outcome and survival after palliative surgery for spinal metastases: palliative surgery in spinal metastases. Cancer. 2003;97:476–484. doi: 10.1002/cncr.11039. [DOI] [PubMed] [Google Scholar]
- 20.Jansson KA, Bauer HC. Survival, complications and outcome in 282 patients operated for neurological deficit due to thoracic or lumbar spinal metastases. Eur Spine J. 2006;15:196–202. doi: 10.1007/s00586-004-0870-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lawson EH, Hall BL, Louie R, Ettner SL, Zingmond DS, Han L, Rapp M, Ko CY. Association between occurrence of a postoperative complication and readmission: implications for quality improvement and cost savings. Ann Surg. 2013;258:10–18. doi: 10.1097/SLA.0b013e31828e3ac3. [DOI] [PubMed] [Google Scholar]
- 22.Martin RC, 2nd, Brennan MF, Jaques DP. Quality of complication reporting in the surgical literature. Ann Surg. 2002;235:803–813. doi: 10.1097/00000658-200206000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martin RC, 2nd, Jaques DP, Brennan MF, Karpeh M. Achieving RO resection for locally advanced gastric cancer: is it worth the risk of multiorgan resection? J Am Coll Surg. 2002;194:568–577. doi: 10.1016/S1072-7515(02)01116-X. [DOI] [PubMed] [Google Scholar]
- 24.Milch CE, Salem DN, Pauker SG, Lundquist TG, Kumar S, Chen J. Voluntary electronic reporting of medical errors and adverse events: an analysis of 92,547 reports from 26 acute care hospitals. J Gen Intern Med. 2006;21:165–170. doi: 10.1111/j.1525-1497.2006.00322.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morris JA Jr, Carrillo Y, Jenkins JM, Smith PW, Bledsoe S, Pichert J, White A. Surgical adverse events, risk management, and malpractice outcome: morbidity and mortality review is not enough. Ann Surg. 2003;237:844–851; discussion 851–852. [DOI] [PMC free article] [PubMed]
- 26.Murff HJ, FitzHenry F, Matheny ME, Gentry N, Kotter KL, Crimin K, Dittus RS, Rosen AK, Elkin PL, Brown SH, Speroff T. Automated identification of postoperative complications within an electronic medical record using natural language processing. JAMA. 2011;306:848–855. doi: 10.1001/jama.2011.1204. [DOI] [PubMed] [Google Scholar]
- 27.Nunez M, Lozano L, Nunez E, Segur JM, Sastre S, Macule F, Ortega R, Suso S. Total knee replacement and health-related quality of life: factors influencing long-term outcomes. Arthritis Rheum. 2009;61:1062–1069. doi: 10.1002/art.24644. [DOI] [PubMed] [Google Scholar]
- 28.Ogura K, Yasunaga H, Horiguchi H, Fushimi K, Kawano H. What is the effect of advanced age and comorbidity on postoperative morbidity and mortality after musculoskeletal tumor surgery? Clin Orthop Relat Res. 2014;472:3971–3978. doi: 10.1007/s11999-014-3889-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Paradis AR, Stewart VT, Bayley KB, Brown A, Bennett AJ. Excess cost and length of stay associated with voluntary patient safety event reports in hospitals. Am J Med Qual. 2009;24:53–60. doi: 10.1177/1062860608327610. [DOI] [PubMed] [Google Scholar]
- 30.Patil CG, Lad SP, Santarelli J, Boakye M. National inpatient complications and outcomes after surgery for spinal metastasis from 1993-2002. Cancer. 2007;110:625–630. doi: 10.1002/cncr.22819. [DOI] [PubMed] [Google Scholar]
- 31.Paxton EW, Inacio MC, Singh JA, Love R, Bini SA, Namba RS. Are there modifiable risk factors for hospital readmission after total hip arthroplasty in a US healthcare system? Clin Orthop Relat Res. 2015;473:3446–3455. doi: 10.1007/s11999-015-4278-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rampersaud YR, Moro ER, Neary MA, White K, Lewis SJ, Massicotte EM, Fehlings MG. Intraoperative adverse events and related postoperative complications in spine surgery: implications for enhancing patient safety founded on evidence-based protocols. Spine (Phila Pa 1976). 2006;31:1503–1510. [DOI] [PubMed]
- 33.Rampersaud YR, Neary MA, White K. Spine adverse events severity system: content validation and interobserver reliability assessment. Spine (Phila Pa 1976). 2010;35:790–795. [DOI] [PubMed]
- 34.Rosenthal R, Hoffmann H, Dwan K, Clavien PA, Bucher HC. Reporting of adverse events in surgical trials: critical appraisal of current practice. World J Surg. 2015;39:80–87. doi: 10.1007/s00268-014-2776-8. [DOI] [PubMed] [Google Scholar]
- 35.Rowin EJ, Lucier D, Pauker SG, Kumar S, Chen J, Salem DN. Does error and adverse event reporting by physicians and nurses differ? Jt Comm J Qual Patient Saf. 2008;34:537–545. doi: 10.1016/S1553-7250(08)34068-9. [DOI] [PubMed] [Google Scholar]
- 36.Schectman JM, Plews-Ogan ML. Physician perception of hospital safety and barriers to incident reporting. Jt Comm J Qual Patient Saf. 2006;32:337–343. doi: 10.1016/S1553-7250(06)32043-0. [DOI] [PubMed] [Google Scholar]
- 37.Schuerer DJ, Nast PA, Harris CB, Krauss MJ, Jones RM, Boyle WA, Buchman TG, Coopersmith CM, Dunagan WC, Fraser VJ. A new safety event reporting system improves physician reporting in the surgical intensive care unit. J Am Coll Surg. 2006;202:881–887. doi: 10.1016/j.jamcollsurg.2006.02.035. [DOI] [PubMed] [Google Scholar]
- 38.Shehadi JA, Sciubba DM, Suk I, Suki D, Maldaun MV, McCutcheon IE, Nader R, Theriault R, Rhines LD, Gokaslan ZL. Surgical treatment strategies and outcome in patients with breast cancer metastatic to the spine: a review of 87 patients. Eur Spine J. 2007;16:1179–1192. doi: 10.1007/s00586-007-0357-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sink EL, Beaule PE, Sucato D, Kim YJ, Millis MB, Dayton M, Trousdale RT, Sierra RJ, Zaltz I, Schoenecker P, Monreal A, Clohisy J. Multicenter study of complications following surgical dislocation of the hip. J Bone Joint Surg Am. 2011;93:1132–1136. doi: 10.2106/JBJS.J.00794. [DOI] [PubMed] [Google Scholar]
- 40.Sink EL, Leunig M, Zaltz I, Gilbert JC, Clohisy J. Reliability of a complication classification system for orthopaedic surgery. Clin Orthop Relat Res. 2012;470:2220–2226. doi: 10.1007/s11999-012-2343-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Strasberg SM, Linehan DC, Hawkins WG. The accordion severity grading system of surgical complications. Ann Surg. 2009;250:177–186. doi: 10.1097/SLA.0b013e3181afde41. [DOI] [PubMed] [Google Scholar]
- 42.Street JT, Lenehan BJ, DiPaola CP, Boyd MD, Kwon BK, Paquette SJ, Dvorak MF, Rampersaud YR, Fisher CG. Morbidity and mortality of major adult spinal surgery: a prospective cohort analysis of 942 consecutive patients. Spine J. 2012;12:22–34. doi: 10.1016/j.spinee.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 43.Wanzel KR, Jamieson CG, Bohnen JM. Complications on a general surgery service: incidence and reporting. Can J Surg. 2000;43:113–117. [PMC free article] [PubMed] [Google Scholar]
- 44.Whitmore RG, Stephen J, Stein SC, Campbell PG, Yadla S, Harrop JS, Sharan AD, Maltenfort MG, Ratliff JK. Patient comorbidities and complications after spinal surgery: a societal-based cost analysis. Spine (Phila Pa 1976). 2012;37:1065–1071. [DOI] [PubMed]