Abstract
A main concern for women giving birth is the risk of obstetric anal sphincter injuries. In our department the incidence of sphincter injuries was around 8 % among vaginally delivering first time mothers. We aimed to halve the incidence to 4 % or less. A prospective interventional program was instituted. We implemented a hands-on technique with four elements in a bundle of care together with a certification process for all staff on the delivery ward. The incidence of episiotomies served as a balancing indicator.
The adherence to three of the four elements of the care bundle rose significantly while the all-or-nothing indicator leveled around 80 %. The median number of deliveries between cases with a sphincter injury increased from 9.5 in the baseline period to 20 during the intervention period. This corresponded with a reduction in the incidence from 7.0 % to 3.4 %. The rate of episiotomy remained low at 8.4 % in this group. By implementing the hands-on technique, we halved the risk of obstetric anal sphincter injuries. Our data suggest that further improvement may be anticipated. The study has demonstrated how implementation of a hands-on technique can be carried out within a quality improvement framework with rapid and sustainable results.
Problem
A main concern for women giving birth is the risk of obstetric anal sphincter injuries (OASIS).1 There are several potential serious long-term consequences of OASIS, like dyspareunia, perineal pain, and a risk of lifelong anal incontinence of 15 - 61 %.2 In 2010 a national quality assessment program (The Danish Quality Database of Birth) was started. One of the indicators was the incidence of OASIS in vaginally delivering nulliparous women and the standard of care was set to be 6 % or lower. In our institution around 2.800 women give birth annually from gestational week 28 + 0 including some 43 % nulliparous women. 90 midwives and 20 doctors constitute the staff together with 5 supervising midwives in charge. We refer very preterm deliveries and small groups of pregnant women with complicated medical illnesses to the University Hospital in Skejby, Aarhus. Apart from this, the cohort of delivering women is unselected.
In our institution, the incidence of OASIS was around 8 % among vaginally delivering first time mothers for several years, and previous attempts to address this were in vain.
Background
The rising rate of OASIS in the UK3 as well as in Scandinavia4 in the past decades has largely been explained by better diagnosis and demographic changes in the cohorts of delivering women.3 5 In this time period, while the obstetric community debated whether delivery of the child should be by hands-on or hands-off, a shift was noted from hands-on to hands-off among midwives in the UK6 as well as in Scandinavian countries.7 8 Recent observational studies from Norway, however, showed a reduction of OASIS from around 6 % to 3 % in vaginally delivering first time mothers when implementing a hands-on technique.9 10
Inspired by the results in Norway, we started the present study with the goal of halving the incidence of OASIS among vaginally delivering first time mothers from around 8 % to 4 % or lower using a similar technique and chose to do this within the framework of a quality improvement study.
Baseline measurement
The primary outcome indicator was the number of deliveries between cases with OASIS, which was defined as grade 3 or 4 sphincter rupture. The international classification of OASIS initially described by Abdul Sultan11 has been in use in our department for several years. Information on clinical characteristics and outcome data from the pre-intervention period was retrieved from existing electronic records. The baseline period went from January through May 2013 including 355 vaginally delivering nulliparous women. 25 women suffered from OASIS corresponding to a median of 9.5 deliveries between cases or an incidence of 7.0 %. This share was a little smaller than in previous years which may to some degree be explained by a Hawthorne effect since there was a growing concern about this particular problem.
The measurement plan was to retrieve and analyze data on the outcome, the process, and the balancing indicators monthly. The registration was planned to be collected as real-time data, i.e. on a chart immediately after each delivery by the attending midwife.
Design
The post intervention period went from June 2013 through March 2015. Our intervention comprised implementation of a bundle of care and a certification process. We decided to use a hands-on technique similar to the technique used in the Norwegian interventional studies with significant improvements. Our improvement theory was that this hand-on technique would lead to the desired lower rate of OASIS. Thus, the improvement project was not aimed at investigating how to perform the hands-on technique per se, but how to implement it in our institution. We detailed the definitions of the four elements of the bundle of care that we used for the intervention: 1) Communication settled, i.e. a shared decision with the woman about not to push when delivering the head in order to slow down the speed of delivery. Understanding this communication and the reason for it should be in place before active pushing; 2) visible brim of the perineum during the delivery of the head; 3) whole hand on the head of the child exerting a pressure on the head in order to slow down the speed of delivery; 4) perineal support when delivering the head constituting a firm support on the perineum and at the same time facilitating the naturally occurring extension of the head. See Figure 1: The hands-on technique.
Figure 1.
Hands-on technique. Original copyright, midwife Heidi Barslund-Gade, Dep Obst&Gyn, Herning, DK. Under CCBY licence, 2014.
In the first step of the certification process, all midwives and doctors in the labour ward watched a supervised power-point presentation describing the background for the project, the aim, and the means to achieve our goal. The second step included supervision of the hands-on technique on a childbirth simulator, while in the third step all midwives were supervised on the technique in three real deliveries.
The certification process started in May 2013 with two supervisor visits by two midwives from the delivery department of Hospital Vendsyssel. This department previously adopted the same hands-on technique with a significant improvement.12 They certified our group of five supervising midwives in charge in certifying others.
Adherence to each of the elements of the care bundle served as process indicators, while number of deliveries between cases with OASIS was the outcome indicator. We used the incidence of episiotomies as a balancing indicator, since concerns were raised that the use of episiotomies might rise as a consequence of the project.
We used the Anhoej rules to identify patterns of non-random variation.13
Strategy
The intervention was educational, aiming to implement the described hands-on technique in delivery, thus changing behaviour among midwives and doctors. A driver diagram describing the various primary and secondary drivers that were necessary to deal with was made.
On a registration sheet adherence to each of the four elements of the care bundle was noted after each delivery and whether the birth attendant was certified together with the gestational age and birth weight. It was noted if vacuum extraction was used (in our department forceps are rarely used), the grade of any perineal rupture, and use of episiotomy. We used several PDSA cycles in order to modify this sheet after feedback from midwives, or when we noted that clarification was needed. Process, outcome and balancing indicators were measured and analyzed during the course of the project and presented as iterative monthly feedback to midwives and doctors and management.
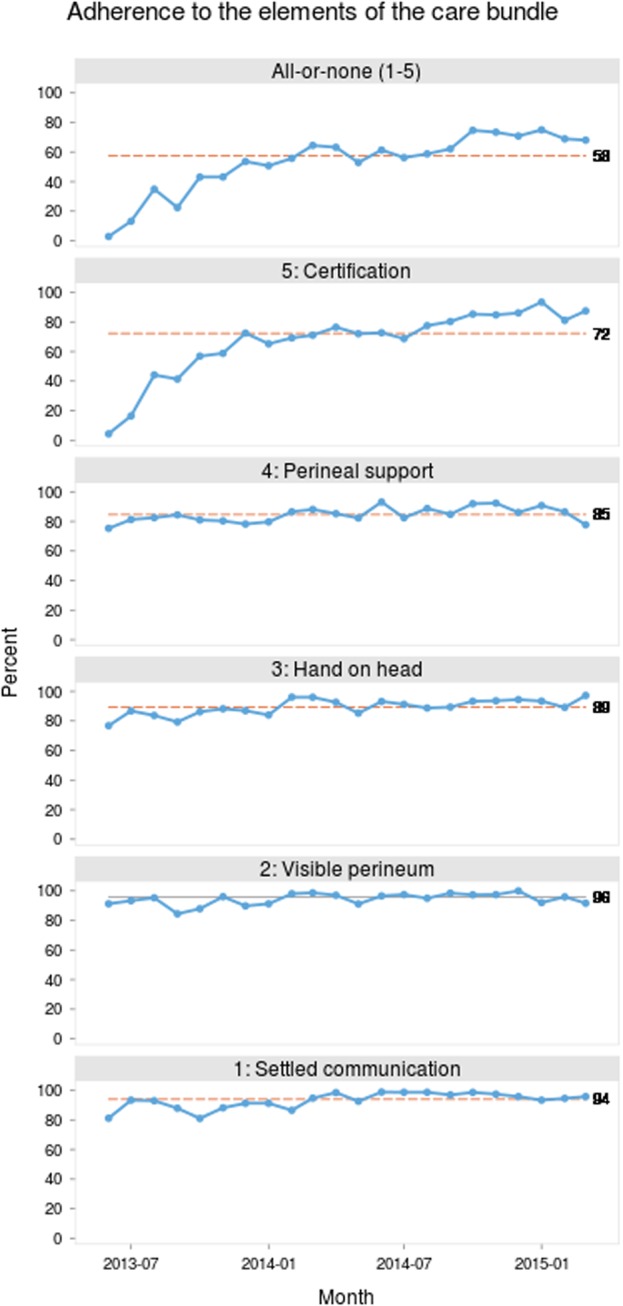
The improvement of adherence to the care bundle is displayed in Figure 2, showing run charts of the five process indicators and the all-or-nothing indicator during the intervention period. When present, non-random variation is marked by a dashed centre line. Non-random variation in the desired direction (up) is observed with settled communication, hand on the head, certification, and all-or-nothing. Thus, adherence to the new procedure increased significantly during the intervention period. Adherence to visible brim of the perineum was already high from the start.
Figure 2.

Adherence to process indicators. See text for legend. Hospitalsenheden Vest, Denmark.
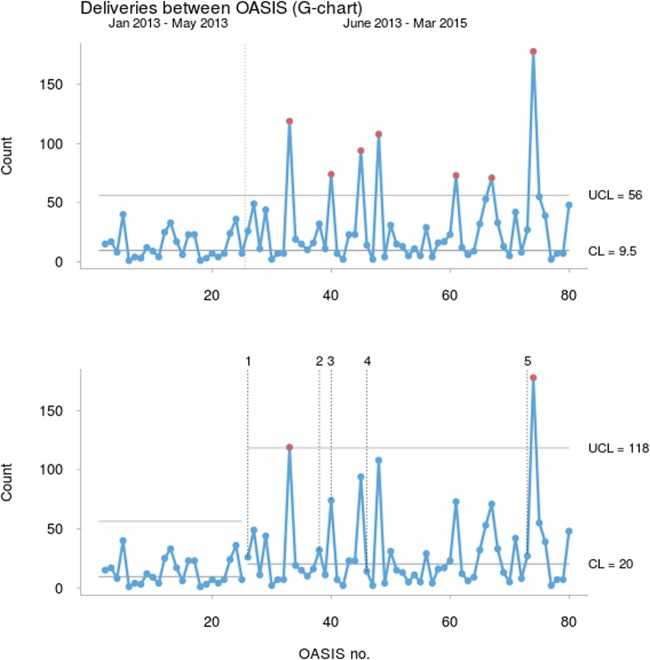
We did not use PDSA cycles in relation to our theory of improvement. Instead, several PDSA cycles based on the progress of the process indicators were used to ensure a widespread implementation of the care bundle. These cycles are described in the following paragraphs with the same numbers that are shown as annotations in Figure 3:
Figure 3.
Deliveries between cases with annotations
1: The registration chart was revised after feedback cycles from midwives and doctors from the start of the project, i.e. June 2013.
2: In October 2013, we observed that midwife students were not automatically included in the project. Also, new employees in the department and women returning from maternity leave were missed for certification. Consequently, we changed the introduction (and re-introduction) for these groups to the department.
3: By November 2013 we introduced the use of the hands-on technique in our team training program which all staff members are supposed to go through once a year or two years.
4: Primarily, the focus in the project was on the midwives and their understanding and adherence to the intervention. By February 2014 we documented confirming results from the intervention in non-operative deliveries, while at the same time, there was practically no improvement in the incidence of OASIS in operative vaginal deliveries. From this time, we established training for doctors performing a vacuum extraction on a childbirth simulator. We stressed keeping a slow progress and extending the head through introitus in order to imitate the normal process of delivery as much as possible. It was emphasized that it is often feasible to stop pulling on the extractor when the head is crowning or even remove the extractor before the head is delivered.
4: By February 2014 we noticed that the element “Communication settled” did not improve from around 80 %. It turned out that a lot of women did not know about the project before arriving on the labour ward. Thus, we began to inform about the project and its implications during antenatal classes since practically all first-time mothers attend these. Posters and handouts with information about the technique and its implications were placed in consultation rooms and discussions were initiated in order to facilitate a shared decision making about birth position and the proposed intervention.
5: By October 2014 we noticed that the all-or-none indicator had come to a standstill around 58 % without improvement for half a year. We then created a poster re-informing about the project and reminding about the care bundle.
Results
During the post intervention period 1,622 nulliparous women delivered vaginally. 55 had OASIS comprising 3.4 %. The median of deliveries between cases was 20. Outcome registration was complete in all cases, while registration charts with information of adherence to the intervention were missing in 28 deliveries (1.7 %). None of these had OASIS. They were excluded from the analysis of process indicators but included in the overall OASIS rate analysis.
The number of deliveries between cases with OASIS is displayed in the G chart in Figure 3.
Figure 3. Number of deliveries between cases with OASIS. The annotations refer to the PDSA cycles: 1: Registration chart revised; 2: Midwife students included; 3: Team training included; 4: Operative vaginal deliveries included; 4: Antenatal classes included; 5: New poster spread out. See text for further legend. Hospitalsenheden Vest, Denmark.
The top chart shows the number of deliveries without OASIS between each case of OASIS during the whole study period. The centre line (median) and the control limit are calculated from the pre intervention period. In the pre intervention period the incidence of OASIS was statistically stable showing only common cause variation with a median of 9.5 deliveries between each case. In the post intervention period, seven points fell above the upper control limit indicating special cause variation. Thus, after only 3-4 months of the intervention period the care bundle was affecting the rate of OASIS in the desired direction.
The bottom chart shows the same data with separate calculations of centre and control lines for each period. The median number of deliveries between cases with OASIS improved to 20 (using the mean, the number went from 14 to 29). The intervention period still shows special cause variation in the desired direction. These data correspond with a statistically significant decrease of the rate of OASIS from 7.0 % in the pre intervention period to 3.4 % in the post intervention period (p = 0.003; RR = 0.48; CI = 0.3-0.76).
The incidence of episiotomy in the pre intervention period in this particular group of women was 9.6 %, and during the post intervention period the incidence was 8.4 % (p = 0.46).
Lessons and limitations
Having had full support from management from the start constituted the foundation for the study, while the 5 midwives in charge together with the multidisciplinary set up strengthened internal credibility. Giving continuous feedback on process, outcome, and balancing indicators during the study period furthermore helped turning the project into a common cause for all staff members.
The only deliberate change that took place during the study period came from the intervention. In 2010 and 2011 attempts were made to reduce the incidence of OASIS in our department using discussions and a reflecting attitude among midwives. Thus, a possible Hawthorne effect may have shown prior to this project and may explain the rate of OASIS during the baseline period of 7 %.
It is well known that diagnosing OASIS is a clinical challenge14 and therefore some cases may have been overlooked. On the other hand, we addressed how to diagnose this condition in our department both for midwives and for doctors. We find it unlikely that the rate of missed diagnoses went up during the intervention period, but this aspect is definitely important when considering a project like this.
Over reporting of the use of the different elements of the care bundle may play a role, especially in cases with OASIS because of a perceived pressure for adherence to the intervention in this situation. When present, this type of bias will diminish the association between the intervention and the improvement of the outcome.
The possible presence of these two types of bias underscores an important lesson from quality improvement work, namely, that emphasis should be put on adherence to the care bundle (the process) in all situations and to a lesser degree on the outcome. Focus on the process applies for the daily work instituting the intervention, for any kind of reaction whenever there is a case of OASIS, and when giving feedback from data.
Differences in the risk profile in a cohort compared with ours may limit the generalisability when trying to implement a similar project. On the other hand, the present cohort of nulliparous women was not sorted by exclusions in any way, making the intervention results more likely to be applicable to different settings.
A great deal of enthusiasm with the project was noted in our department, not the least since positive results turned up already after 3-4 months. It may be more difficult to obtain a sustainable improvement in another setting with more resistance against the hands-on technique and in which the aspects of the Model of Improvement are not applied.
Subgroups working on a delivery ward like midwife students and newly employed should be taken into account from the start of a similar project. Likewise, certifying doctors performing operative vaginal delivery should be a part of initial plans.
From the start of the project we felt assured about our improvement theory. Hence, we did not plan to investigate the care bundle further. It is conceivable, that an even higher degree of adherence to the process indicators would have been achievable, if we had tried to roll the intervention out more gradually. On the other hand, rumours about the care bundle spread quickly inside the department, and it was unlikely to keep the specifics of the intervention to small groups.
We did not register the women's satisfaction with the intervention. The use of all components of the care bundle is naturally restricted in deliveries with alternative birth positions and in water births. The pregnant and delivering women should be informed about the possibility to significantly reduce the risk of OASIS by implementing the described hands-on technique during the last part of the delivery. Full information about the possible serious morbidity from a sphincter rupture together with implications for birth positions and handling of the last part of delivery provides a sincere ground for an informed choice and a shared decision making about implementation of the intervention.
Conclusion
The incidence of OASIS in nulliparous women was modifiable by using a hands-on technique without increasing the rate of episiotomy. Keeping the rate of OASIS low should be a paramount issue for quality improvement in any delivery ward. A sphincter rupture is a feared outcome in childbirth and may be a driver for cesarean section on maternal request even in first time mothers.1 Using the aspects of the Model of Improvement, the incidence of sphincter rupture was reduced from 7.0 % to 3.4 %, thus, resembling the results from Norway 9 10 and from the delivery department of Hospital Vendsyssel.12
Our data still show special cause variation in the desired direction (Figure 3), indicating that the new process is not stable yet and further improvement may be anticipated. The documented adherence to the intervention reached a stable and high level with an all-or-nothing application of around 80 %. The changes that were made during the project to the introduction to our department are maintained. Furthermore, we have decided to re-certify all midwives and doctors during the first two months each year. During 2015 the incidence of OASIS was 2.8 % and during the first half of 2016 it was 3.0 %.
The present study demonstrates the implementation of a hands-on technique in childbirth within a quality improvement framework with rapid and sustainable results.
Acknowledgments
We wish to thank the Danish Society for Patient Safety for valuable discussions and advice concerning study design and implementation.
We thank Associate Professor Finn Lauszus, MD, PhD for constructive discussions.
Footnotes
Declaration of interests: Nothing to declare.
Ethical approval: The study was approved by the Danish Data Protection Agency (2007-58-0010, April 2013) while approval from the local Ethics Committee was not found relevant by the committee (1-10-72-127-13, May 2013).
References
- 1.Turner CE, Young JM, Solomon MJ et al. . Vaginal delivery compared with elective caesarean section: the views of pregnant women and clinicians. BJOG 2008;115:1494–1502. DOI:10.1111/j.1471-0528.2008.01892.x [DOI] [PubMed] [Google Scholar]
- 2.Fernando RJ, Sultan AH, Kettle C et al. . Methods of repair for obstetric anal sphincter injury. Cochrane Database of Systematic Reviews 2013. DOI:10.1002/14651858.CD002866.pub3. [DOI] [PubMed] [Google Scholar]
- 3.Thiagamoorthy G, Johnson A, Thakar R et al. . National survey of perineal trauma and its subsequent management in the United Kingdom. Int Urogynecol J 2014;25:1621–1627. DOI:10.1007/s00192-014-2406-x [DOI] [PubMed] [Google Scholar]
- 4.Laine K, Rotvold W, Staff AC. Are obstetric anal sphincter ruptures preventable? - Large and consistent rupture rate variations between the Nordic countries and between delivery units in Norway. Acta Obstet Gynecol Scand 2013;92:94–100DOI:10.1111/aogs.12024. [DOI] [PubMed] [Google Scholar]
- 5.Dahlen HG, Priddis H, Thornton C. Severe perineal trauma is rising, but let us not overreact. Midwifery 2015;31:1–8. [DOI] [PubMed] [Google Scholar]
- 6.Trochez R, Waterfield M, Freeman RM. Hands on or hands off the perineum: a survey of care of the perineum in labour (HOOPS). Int Urogynecol J 2011;22:1279–1285. DOI:10.1007/s00192-011-1454-8 [DOI] [PubMed] [Google Scholar]
- 7.Samuelsson E, Ladfors L, Wennerholm UB et al. . Anal sphincter tears: prospective study of obstetric risk factors. BJOG 2000;107:926–931. [DOI] [PubMed] [Google Scholar]
- 8.Parnell C, Langhoff-Roos J, Møller H. Conduct of labor and rupture of the sphincter ani. Acta Obstet Gynecol Scand 2001;80:256–261. [DOI] [PubMed] [Google Scholar]
- 9.Hals E, Øian P, Pirhonen T et al. . A Multicenter Interventional Program to Reduce the Incidence of Anal Sphincter Tears. Obstet Gynecol 2010;116:901–908. [DOI] [PubMed] [Google Scholar]
- 10.Laine K, Skjeldestad FE, Sandvik L et al. . Incidence of obstetric anal sphincter injuries after training to protect the perineum: cohort study. BMJ Open 2012;2:e001649 DOI:10.1136/bmjopen-2012-001649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sultan AH. Obstetric perineal injury and anal incontinence. Clinical Risk 1999;5:193–196. [Google Scholar]
- 12.Leenskjold S, Høj L, Pirhonen J. Manual protection of the perineum reduces the risk of obstetric anal sphincter ruptures. Dan Med J 2015;62:A5075. [PubMed] [Google Scholar]
- 13.Anhøj J, Olesen AV. Run Charts Revisited: A Simulation Study of Run Chart Rules for Detection of Non-Random Variation in Health Care Processes. PLoS ONE 2014;9:e113825 DOI:10.1371/journal.pone.0113825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Andrews V, Sultan AH, Thakar R et al. . Occult anal sphincter injuries - myth or reality? BJOG 2006;113:195–200. DOI:10.1111/j.1471-0528.2006.00799.x [DOI] [PubMed] [Google Scholar]