Abstract
A pregnant woman aged 29 years, G1P0 at 21 weeks of gestation of a dichorionic diamniotic twin, presented with suspected deep vein thrombosis (DVT) of the left leg. Repeated (compression) ultrasonography was not diagnostic for DVT but showed reduced flow over the left external iliac vein, common femoral vein and superficial femoral vein. In pursue of a definite diagnosis, magnetic resonance direct thrombus imaging was performed showing a clear high signal in the left common iliac vein which is diagnostic for acute thrombosis in this venous segment. Phase contrast venography supported this diagnosis, showing no flow in the left common iliac vein. Treatment with anticoagulants was started. 6 months after the diagnosis, the patient is doing well and does not report signs of post-thrombotic syndrome.
Background
Pregnancy is a well known and strong risk factor for venous thromboembolism (VTE), with pregnant women having a fourfold increased risk of VTE compared with non-pregnant women.1 Considering that up to 13.9% of the maternal deaths in the UK are due to VTE,2 accurate diagnosis and adequate treatment are still of utmost clinical importance, although due to anatomical changes and the contraindication for ionising radiation, the diagnostic management of suspected VTE remains challenging today.3 We report the case of a pregnant patient with difficult to diagnose iliac vein thrombosis, in whom we applied the non-invasive magnetic resonance direct thrombus imaging (MRDTI) technique after conventional imaging tests were non-diagnostic.
Case presentation
A pregnant woman aged 29 years, G1P0 at 21 weeks of gestation of a dichorionic diamniotic twin, was referred by her general practitioner to the emergency department because of suspected deep vein thrombosis (DVT) of the left leg. She had no relevant medical history and was only taking folic acid and multivitamins as medication. Her whole left leg was swollen since 1 day. She reported no local tenderness but instead a deep pain in the left loin that had started several days before current presentation. She had not experienced respiratory symptoms or chest pain. Her family history was negative for thromboembolic events. On physical examination, her entire left leg was swollen, with a 3 cm difference in calf circumference compared with the right leg. The left leg was slightly more red coloured compared with the right leg. Peripheral pulsations were present in both legs.
Investigations
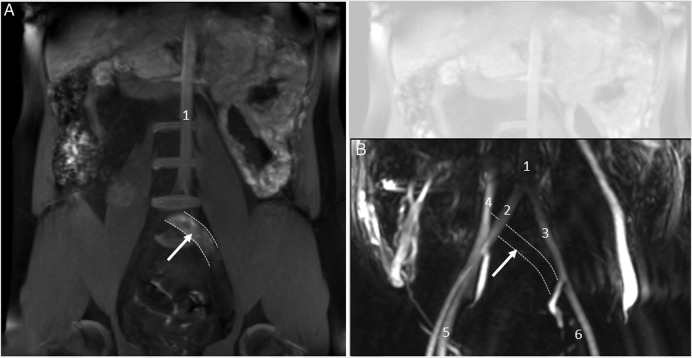
Laboratory examination showed a C reactive protein of 54 mg/L. A D-dimer test was not performed. Based on her presentation, the attending physician confirmed the suspicion of a DVT and ordered compression ultrasonography (CUS), showing full compressibility of the common femoral vein, superficial femoral vein and popliteal vein. However, additional Doppler ultrasonography revealed reduced flow over the left external iliac vein, common femoral vein and superficial femoral vein, although it was not possible to visualise a thrombus to explain this phenomenon. Because of the remaining high suspicion of iliac vein or more proximal DVT, treatment with nadroparin 15 200 U once daily was initiated and the patient was kept under close outpatient surveillance. The next day, repeated ultrasonography showed similar results. In pursue of a definite diagnosis, we subsequently performed MRDTI.4 The MRDTI sequence showed a clear high signal in the common iliac vein, distal from the crossing with the right common iliac artery, up to the bifurcation into the external iliac vein and left internal iliac vein (figure 1), confirming the presence of a fresh blood clot. MRI venography was subsequently performed. Phase contrast venography showed flow in the left external iliac vein and internal iliac vein but no flow in the left common iliac vein, which supported the diagnosis made by the MRDTI sequence.
Figure 1.
Two different MRI sequences, diagnostic for thrombosis in the left common iliac vein. (A) Magnetic resonance direct thrombus imaging, coronal view: white arrow between dashed lines indicates high-signal intensity in the left common iliac vein, indicating deep vein thrombosis directly. 1: aorta. (B) Phase contrast venography, coronal view, showing flow in the vena cava inferior (4) and right common iliac vein (5) but no flow in the left common iliac vein: should have been visible between the white dashed lines indicated by the white arrow. 1, aorta; 2: right common iliac artery; 3: left common iliac artery; 4: vena cava inferior; 5: right common iliac vein; 6: left external iliac vein.
Treatment
Consequently, anticoagulation therapy was continued and compression stockings were prescribed. Within days, her symptoms resolved completely.
Outcome and follow-up
Six weeks later, at 26 weeks plus 5 days of gestation, she presented with unexplained vaginal blood loss, CTG (cardiotocography) showed some contractions and transvaginal ultrasonography showed a lightly shortened cervix. Because of imminent preterm birth, nifidepine and betamethasone were started, and treatment with nadroparin was temporally discontinued. The next day, vaginal ultrasound showed a fully effaced cervix with 14 mm dilation and she gave birth to a premature male twin after uncomplicated vaginal delivery. The day following delivery treatment with nadroparin was restarted and continued for a period of 3 months. Both children developed an Escherichia coli sepsis with meningitis in the first week after birth, complicated by cerebral haemorrhages of which they recovered well. Currently, 6 months after the diagnosis, the patient does not report signs of post-thrombotic syndrome and the twins are doing well.
Discussion
The standard diagnostic algorithm of suspected DVT consisting of a combination of the Wells rule, D-dimer test and compression ultrasonography (CUS),5 has several limitations in pregnant women. First, because leg swelling and leg pain are common in pregnancy and often indistinguishable from symptoms of DVT, questioning and physical examination are less sensitive and cannot be relied on. Second, the Wells rule—nor any other clinical decision rule—has not been validated in pregnant patients.1 Third, the diagnostic accuracy of D-dimer tests in the diagnosis of VTE in pregnancy is hampered because of the substantial increase in D-dimer throughout gestational age.3
Fourth and most notably, 12% of all DVTs in pregnant woman are isolated pelvic vein thrombosis, compared with <1% in a non-pregnant population.6 This is caused by the compression of the left iliac vein by the gravid uterus at the point where it crosses the right iliac artery, also known as the ‘functional’ May Turner syndrome. Owing to obvious anatomical reasons, CUS examination of the pelvic veins is not possible and colour Doppler imaging of the pelvic veins may be unreliable. The latter was demonstrated in two small prospective studies in which non-pregnant patients with acute pulmonary embolism (PE) and normal bilateral CUS examination, including Doppler imaging of the iliac veins up to the inferior vena cava, were subjected to MR-venography. Isolated pelvic vein thrombosis was demonstrated in 7.1% and 29% of the study participants, respectively, despite the normal ultrasound examination.7 8 A third study that applied MR imaging in pregnant woman with CUS-proven DVT showed that the CUS examination had not picked-up the concurrent presence of pelvic vein thrombosis in 11% of patients.9 The largest diagnostic study in pregnant patients with suspected DVT to date applying a single whole-leg CUS examination reported a 3-month failure rate of up to 4.0%, which underlines the poor accuracy of current diagnostic imaging tests in this setting.10 Other established imaging modalities such as conventional venography or CT venography expose mother and fetus to ionising radiation and are therefore not recommended nor acceptable.11
An alternative MR imaging technique for the detection of acute DVT is MRDTI. This technique has reached an advanced stage of development and is close to implementation in clinical practice. The method is based on the formation of methaemoglobin in a fresh thrombus which leads to shortening of the T1 signal.4 12 It does not require contrast dye and takes about 10 min to perform. The diagnostic accuracy (sensitivity 97–100%, specificity 100%) as well as the interobserver agreement of MRDTI for DVT were reported to be excellent (κ 0.89–0.98).4 MDRTI was additionally shown to accurately and reproducibly differentiate between patients with confirmed recurrent ipsilateral DVT and those with asymptomatic residual intravascular clots,13 and is now being tested in an prospective outcome study as first-line imaging test in suspected ipsilateral DVT (ClinicalTrials.gov Identifier: NCT02262052).14 MRDTI is not contraindicated in pregnancy and may potentially be a useful test in pregnant patients with a high clinical suspicion of DVT, but normal CUS examination, as was the case in our patient. A future outcome study in pregnant patients should investigate the incremental diagnostic value of MRDTI in this clinical setting.
Because of the associated morbidity and mortality of pregnancy-associated thrombosis, more accurate diagnosis of DVT remains an important priority of future research. We present the case of a patient with suspected DVT in whom conventional diagnostic tests failed to establish a definite diagnosis. MRDTI, a non-invasive and reproducible technique with high accuracy for acute thrombosis that currently is undergoing the final steps of validation, was able to establish the diagnosis and potentially is a valuable addition to the diagnostic arsenal of imaging tests for DVT in pregnant patients.
Patient's perspective.
During my pregnancy, I had symptoms of my lower back for a longer time, but suddenly my left leg started to feel very strange. The leg was thicker than normal and looked different. The doctors told me that it might be a thrombosis in my leg, I got several tests; however, the doctors were still unsure about the thrombosis. The MRI scan did not take long and did not involve punctures. Although I was disappointed about the diagnosis, I was glad to hear the doctors had finally a definite diagnosis.
Learning points.
Venous thromboembolism (VTE) is one of the leading causes of death in pregnant women, making a proper VTE diagnosis very important for this specific patient group
Compression ultrasonography is the diagnostic imaging method of choice for diagnosing DVT in pregnant women. However, due to overlying anatomic structures, it is often very challenging to rule out thrombosis in the pelvic vein area with this test.
By directly visualising a fresh thrombus without the use of contrast dye or any ionising radiation, magnetic resonance direct thrombus imaging is a promising diagnostic test for suspected pelvic vein thrombosis in pregnant patients.
Footnotes
Contributors: CD and EK wrote the manuscript and prepared the figure. AS revised the manuscript for important intellectual content and prepared the figure. MH revised the manuscript for important intellectual content.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Chan WS, Lee A, Spencer FA et al. Predicting deep venous thrombosis in pregnancy: out in ‘LEFt’ field? Ann Intern Med 2009;151:85–92. 10.7326/0003-4819-151-2-200907210-00004 [DOI] [PubMed] [Google Scholar]
- 2.Guimicheva B, Czuprynska J, Arya R. The prevention of pregnancy-related venous thromboembolism. Br J Haematol 2015;168:163–74. 10.1111/bjh.13159 [DOI] [PubMed] [Google Scholar]
- 3.Chan WS, Chunilal S, Lee A et al. A red blood cell agglutination D-dimer test to exclude deep venous thrombosis in pregnancy. Ann Intern Med 2007;147:165–70. 10.7326/0003-4819-147-3-200708070-00005 [DOI] [PubMed] [Google Scholar]
- 4.Fraser DG, Moody AR, Morgan PS et al. Diagnosis of lower-limb deep venous thrombosis: a prospective blinded study of magnetic resonance direct thrombus imaging. Ann Intern Med 2002;136:89–98. 10.7326/0003-4819-136-2-200201150-00006 [DOI] [PubMed] [Google Scholar]
- 5.Huisman MV, Klok FA. Diagnostic management of acute deep vein thrombosis and pulmonary embolism. J Thromb Haemost 2013;11:412–22. 10.1111/jth.12124 [DOI] [PubMed] [Google Scholar]
- 6.James AH, Tapson VF, Goldhaber SZ. Thrombosis during pregnancy and the postpartum period. Am J Obstet Gynecol 2005;193:216–9. 10.1016/j.ajog.2004.11.037 [DOI] [PubMed] [Google Scholar]
- 7.Stern JB, Abehsera M, Grenet D et al. Detection of pelvic vein thrombosis by magnetic resonance angiography in patients with acute pulmonary embolism and normal lower limb compression ultrasonography. Chest 2002;122:115–21. 10.1378/chest.122.1.115 [DOI] [PubMed] [Google Scholar]
- 8.Gary T, Steidl K, Belaj K et al. Unusual deep vein thrombosis sites: magnetic resonance venography in patients with negative compression ultrasound and symptomatic pulmonary embolism. Phlebology 2014;29:25–9. 10.1258/phleb.2012.012054 [DOI] [PubMed] [Google Scholar]
- 9.Torkzad MR, Bremme K, Hellgren M et al. Magnetic resonance imaging and ultrasonography in diagnosis of pelvic vein thrombosis during pregnancy. Thromb Res 2010;126:107–12. 10.1016/j.thromres.2010.05.011 [DOI] [PubMed] [Google Scholar]
- 10.Le Gal G, Kercret G, Ben Yahmed K et al. Diagnostic value of single complete compression ultrasonography in pregnant and postpartum women with suspected deep vein thrombosis: prospective study. BMJ 2012;344:e2635 10.1136/bmj.e2635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bates SM, Jaeschke R, Stevens SM et al. Diagnosis of DVT: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012;141(2 Suppl):e351S–418S. 10.1378/chest.11-2299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saha P, Andia ME, Modarai B et al. Magnetic resonance T1 relaxation time of venous thrombus is determined by iron processing and predicts susceptibility to lysis. Circulation 2013;128:729–36. 10.1161/CIRCULATIONAHA.113.001371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tan M, Mol GC, van Rooden CJ et al. Magnetic resonance direct thrombus imaging differentiates acute recurrent ipsilateral deep vein thrombosis from residual thrombosis. Blood 2014;124:623–7. 10.1182/blood-2014-04-566380 [DOI] [PubMed] [Google Scholar]
- 14.Klok FA, Tan M, Huisman MV. Letter by Klok et al. Regarding article, ‘18F-Fluorodeoxyglucose positron emission tomography/computed tomography enables the detection of recurrent same-site deep vein thrombosis by illuminating recently formed, neutrophil-rich thrombus’. Circulation 2015;131:e530 10.1161/CIRCULATIONAHA.114.013786 [DOI] [PubMed] [Google Scholar]