Abstract
♦ Background:
Peritoneal dialysis (PD) is recommended for adults with residual kidney function and without significant comorbidities. However, peritonitis is a serious and common complication that is associated with hospitalization, pain, catheter loss, and death. This study aims to describe the beliefs, needs, and experiences of PD patients about peritonitis, to inform the training, support, and care of these patients.
♦ Methods:
Qualitative semi-structured interviews were conducted with 29 patients from 3 renal units in Australia who had previous or current experience of PD. The interviews were conducted between November 2014 and November 2015. Transcripts were analyzed thematically.
♦ Results:
We identified 4 themes: constant vigilance for prevention (conscious of vulnerability, sharing responsibility with family, demanding attention to detail, ambiguity of detecting infection, ineradicable inhabitation, jeopardizing PD success); invading harm (life-threatening, wreaking internal damage, debilitating pain, losing control and dignity); incapacitating lifestyle interference (financial strain, isolation and separation, exacerbating burden on family); and exasperation with hospitalization (dread of hospital admission, exposure to infection, gruelling follow-up schedule, exposure to harm).
♦ Conclusions:
Patients perceived that peritonitis could threaten their health, treatment modality, and lifestyle, which motivated vigilance and attention to hygiene. They felt a loss of control due to debilitating symptoms including pain and having to be hospitalized, and they were uncertain about how to monitor for signs of peritonitis. Providing patients with education about the causes and signs of peritonitis and addressing their concerns about lifestyle impact, financial impact, hospitalization, and peritonitis-related anxieties may improve treatment satisfaction and outcomes for patients requiring PD.
Keywords: Peritoneal dialysis, peritonitis, qualitative research
Although incidence rates of peritonitis have decreased substantially with technological advances in peritoneal dialysis (PD), peritonitis rates in many countries still exceed 0.4 episodes per patient-year (1,2). Worldwide, peritonitis is the direct cause of 4% of deaths in patients on PD and is a “contributing factor” in at least 16% of deaths on PD. Furthermore, peritonitis is a leading cause of hospitalization and technique failure in PD whereby patients must transfer to hemodialysis (3–10).
To minimize the risk of peritonitis, patients are required to perform an exchange following the procedure they have been taught, paying attention to aseptic technique and ensuring excellent hand hygiene. They also need to clean and care for their exit site as taught and assess the exit site regularly for any signs of infection. They need to be aware that severe constipation or diarrhea can lead to peritonitis and take steps to prevent the occurrence of constipation, and they should also be aware that certain medical procedures can lead to peritonitis and that they need to be given antibiotics with these procedures (11). All of these demands on the patient can interfere with lifestyle and cause anxiety.
A systematic review of qualitative studies of the perspectives of adults on PD found that PD can offer a sense of control, independence, self-efficacy, and freedom, but patients also reported impaired self-esteem, physical incapacitation, and reduced social functioning (12). However, there were limited data specifically about peritonitis, and comparisons between automated PD (APD) and continuous ambulatory PD (CAPD) were sparse.
This study aims to describe patients' beliefs, needs, and experiences about peritonitis in PD. An understanding of their beliefs and attitudes can inform strategies to help and empower patients in preventing peritonitis. Awareness of their concerns and needs when receiving treatment for peritonitis can inform support structures and lead to better treatment and health outcomes.
Methods
We used the Consolidated Criteria for Reporting Qualitative Health Research (COREQ) to report this study (13).
Participants and Setting
Participants were eligible for interview if they were English-speaking, over 18 years of age, able to give informed voluntary consent, and had previous or current experience with PD. Purposive sampling was used to include participants with a range of ages, gender, experiences of APD and CAPD, and peritonitis episodes. Participants were recruited from Princess Alexandra Hospital, Brisbane; Westmead Hospital, Sydney; and Monash Medical Centre, Melbourne. Ethics approval was obtained from all 3 sites.
Data Collection
We developed the interview guide after a review of the literature based on a systematic review of patients' experiences of PD and discussion among the research team (Table S1). Face-to-face interviews were performed by the primary investigator (DC) between November 2014 and November 2015, who is a researcher with training in public health and an interest in PD. Recruitment ceased once theoretical saturation was observed in the concurrent analysis, when little or no new data were obtained after 3 consecutive interviews. All interviews were recorded digitally and transcribed verbatim.
Data Analysis
The transcripts were imported into HyperRESEARCH (Version 2.8.3; Research Ware Inc., MA, USA) to facilitate thematic analysis. The principles of grounded theory were followed (i.e. the development of a theory or explanation grounded in the data collected) (14). Each transcript was reviewed line by line by DC, and meaningful segments of text were highlighted and given an appropriate code according to the concepts that had been identified inductively in the data. Similar concepts were grouped into themes. The coding was reviewed by AT, who also read the interview transcripts. A schema was developed to show conceptual relationships between the themes. The preliminary concepts were discussed among the study authors (investigator triangulation). The primary investigator revised the coding structure until it included all concepts about patient beliefs and experiences regarding peritonitis.
Results
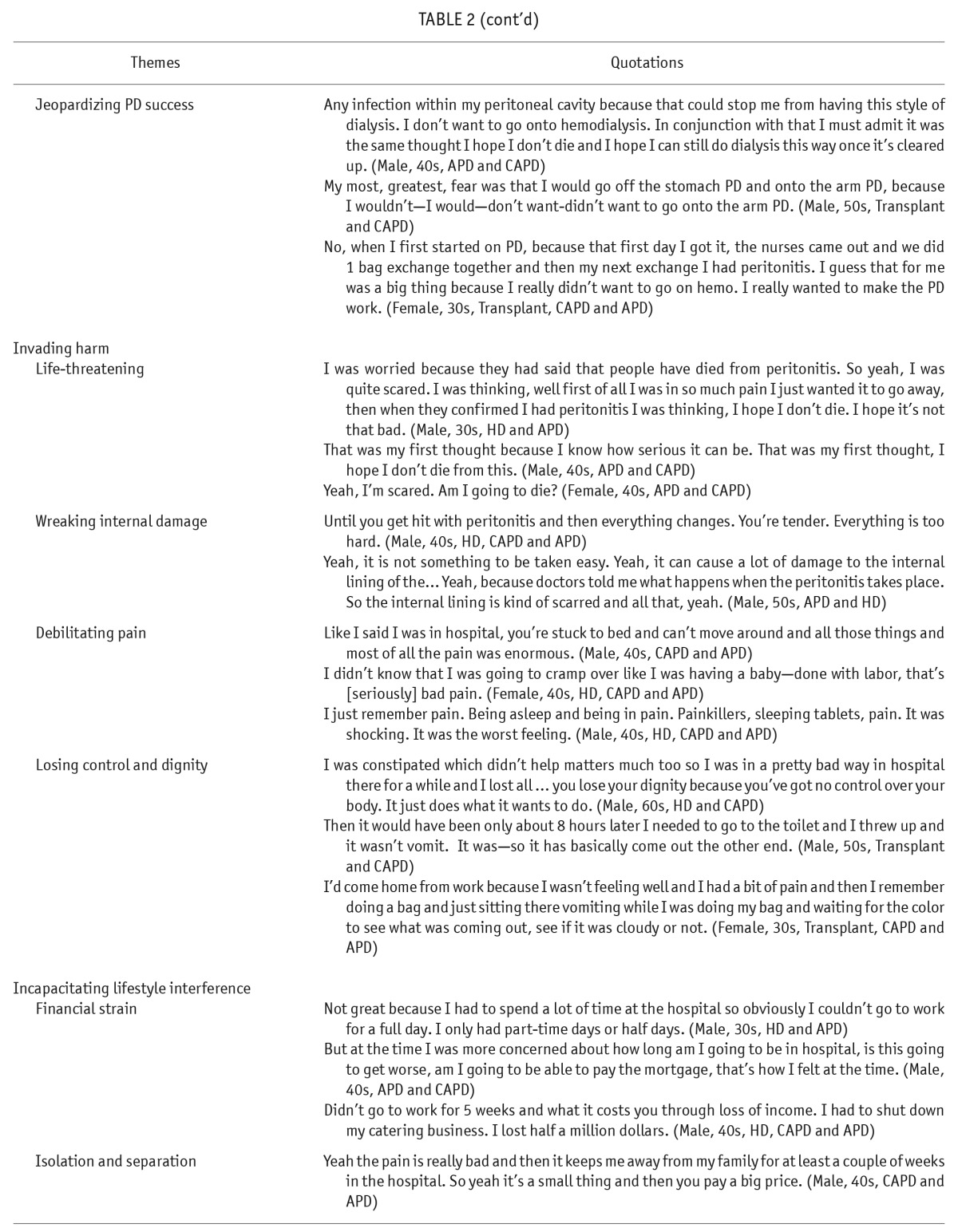
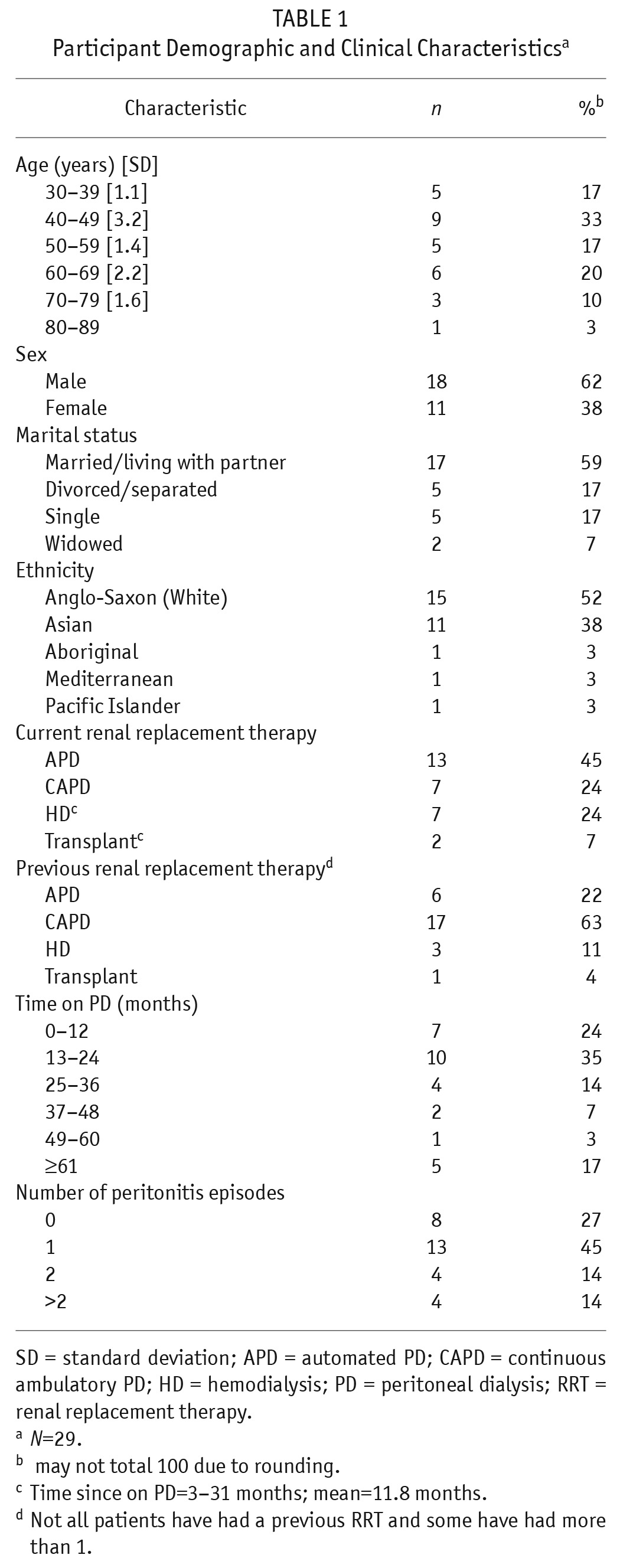
Twenty-nine patients from 3 Australian states participated (88% response rate). Non-participation (n = 4) was due to refusal or inability to set a suitable interview time after 3 attempts. The average duration of the interview which was conducted in person (n = 27) or via Skype (n = 2), was 40 minutes. The participant demographic characteristics are shown in Table 1.
TABLE 1.
Participant Demographic and Clinical Characteristicsa
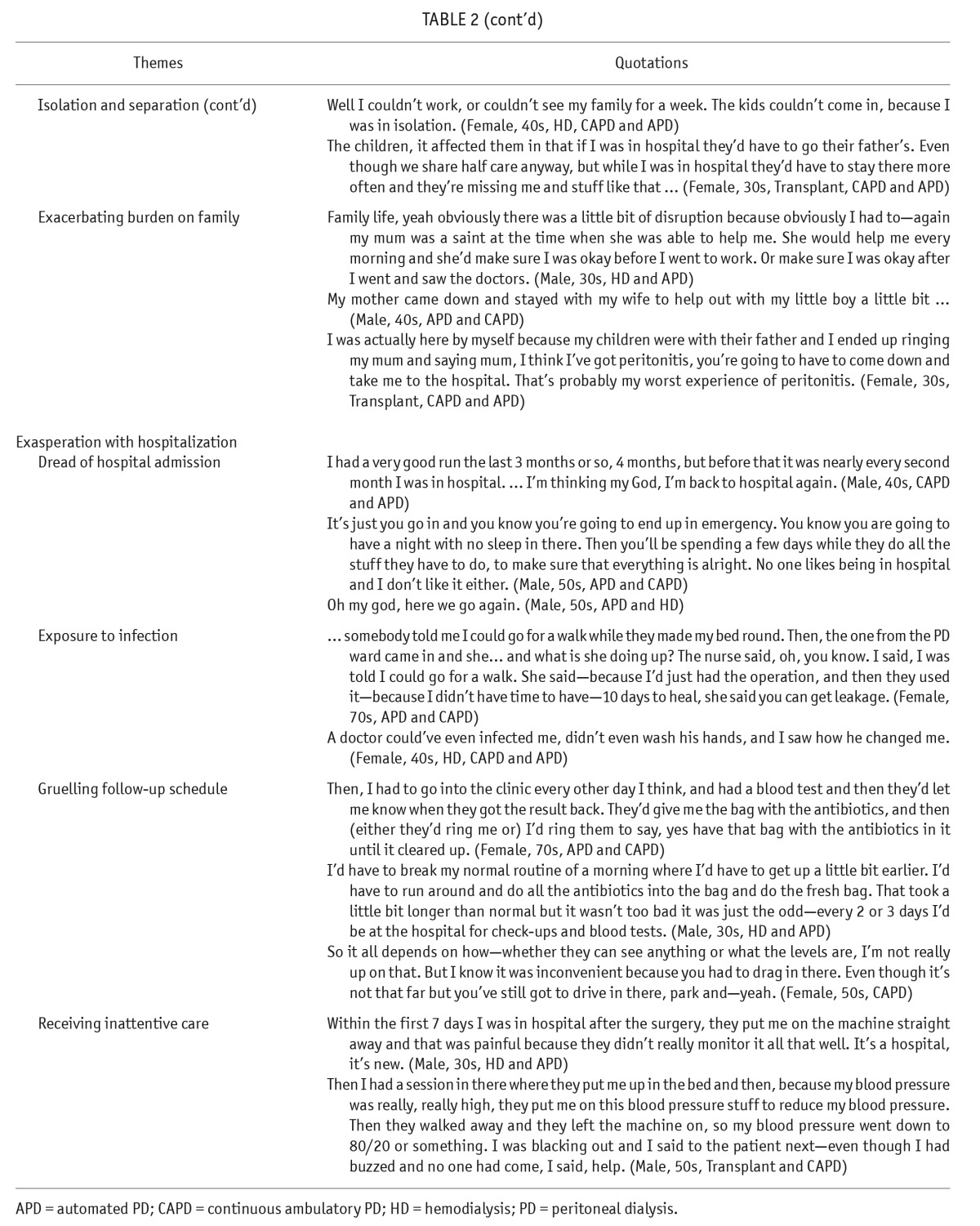
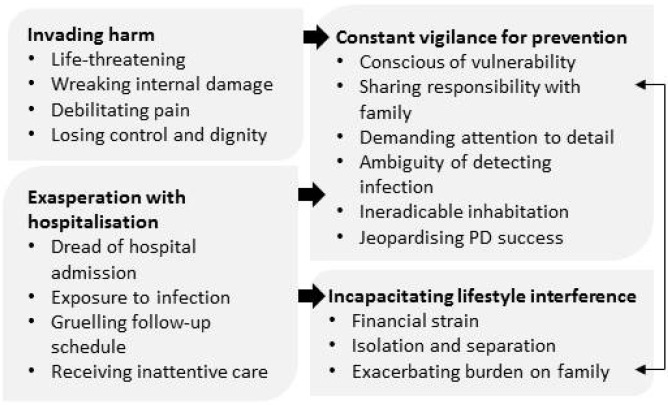
We identified 4 major themes: constant vigilance for prevention, invading harm, incapacitating lifestyle interference, and exasperation with hospitalization. The themes and related subthemes are described in the following section with illustrative quotations provided in Table 2. A thematic schema showing the patterns and relationships among themes is provided in Figure 1.
TABLE 2.
Illustrative Quotations
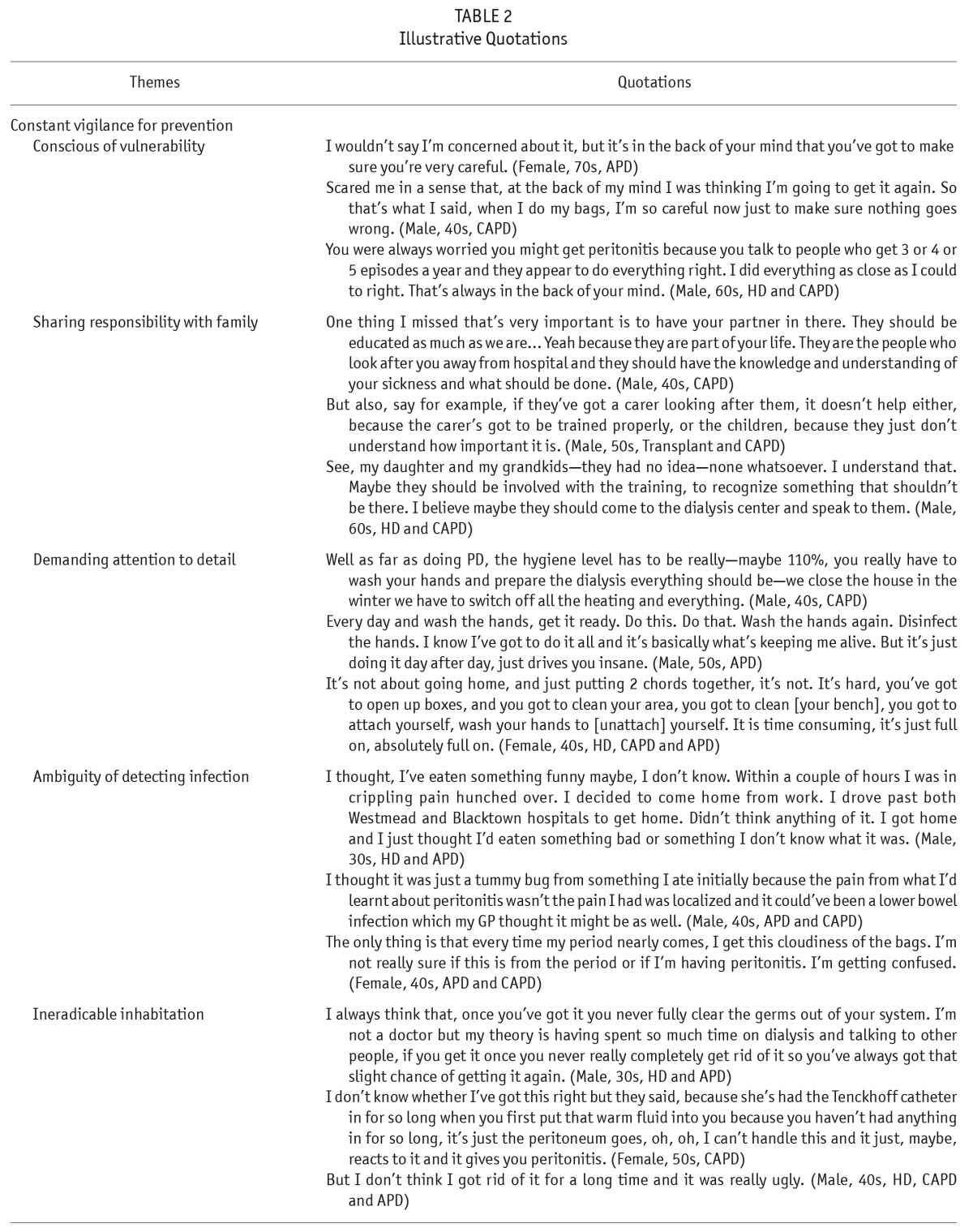
Figure 1 —
Thematic schema representing patient perspectives on the prevention and treatment of peritonitis in peritoneal dialysis.
Constant Vigilance for Prevention
Conscious of Vulnerability: Peritonitis was “always in the back of your mind” and represented a threat to participants' health and lives. Participants who had experienced peritonitis were fearful of recurrence and felt particularly susceptible during a bag exchange or when they made a mistake as “germs could get in.” Those who had not had peritonitis were “mindful” of the possibility of peritonitis because they had seen other patients with peritonitis. For some, they felt “panic” during the first few times they did an exchange.
Sharing Responsibility with Family: Some participants stressed family members had to be “educated as much as we are” so that their family would not be overwhelmed. Participants wanted to be able to depend on them for help. Others felt that their family members demonstrated a lack of care and consideration “because they just don't understand how important it is.”
Demanding Attention to Detail: The cleaning demands of doing an exchange were rigorous, such that patients felt it “just drives you insane.” They were careful to “follow all of the instructions.” Some deliberately did an exchange in a slow methodical manner, some timed how long they washed their hands for, turned off anything that would move air around the room (e.g. fan, heater, air conditioner) and closed the windows and doors before they commenced an exchange. Others checked the dates of their dialysate bags, gauze, and any other items they used. Participants were careful to not “have short-cuts” and to avoid becoming “careless or [overly] confident with their cleaning” as this could result in peritonitis. One man felt under siege and that the attention to detail required was overwhelming—“It could be anything … can't wear a fleecy shirt. A bit of fleece gets in there, you're finished.”
Ambiguity of Detecting Infection: Participants had trouble identifying the first signs of peritonitis and thought instead that they had the flu or that they had gastrointestinal problems. Some experienced only localized pain which they realized later was due to peritonitis. One participant recounted that their general practitioner diagnosed a lower bowel infection but did not suspect peritonitis. Women noticed that their bags became cloudy during ovulation and menstruation, and panicked and went to hospital.
Ineradicable Inhabitation: After experiencing peritonitis, some believed that they “never fully clear the germs” and would always be prone to peritonitis. Even after antibiotics, they believed the cause of the infection remained in their system. Others said it had taken “a long time” to get rid of the infection. Some participants who had a spontaneous infection, believed the peritonitis was caused by “a bug that just kind of happens” and that “the peritoneum … reacts to it [the fluid] and it gives you peritonitis.”
Jeopardizing PD Success: Participants wanted to remain on PD because it suited their lifestyle and offered more freedom and did not require cannulation. Aware that peritonitis could cause PD failure, patients were “worried” about being forced to go onto hemodialysis. Some hoped that they could “still do dialysis this way once [the peritonitis] cleared up.” Some had been warned that if they had 3 episodes of peritonitis, the decision could be made “to take you off peritoneal dialysis … and they will have to put a fistula in.”
Invading Harm
Life-Threatening: Some were worried that they could die from peritonitis. Others were fatalistic, saying “If you die, you die because of my problem” while some said they felt so sick at the time that they thought “I just need to die.”
Wreaking Internal Damage: Some participants anticipated that peritonitis would cause their “internal lining” to be “scarred” and “damaged.” They spoke of being “hit” with peritonitis and said that following peritonitis “everything changes” and that physically, they were “tender.”
Debilitating Pain: Although they had been told that peritonitis could be painful, participants were unprepared for the pain which they described as “enormous,” “massive,” “crippling” and like “labour pain.” They became unable to function as they were “hunched over” and “couldn't do anything” and could “hardly move” or talk. They described the pain as quickly coming on and escalating rapidly to an “unbelievable” level.
Losing Control and Dignity: When going through a peritonitis episode, unpredictable occurrences such as falling unconscious in public, being unable to get off the toilet in the ward without assistance, and vomiting in public caused participants to feel embarrassed. Participants spoke of having “no control over your body” and the humiliation of other patients in the ward “knowing what's going on.” For example, one participant who was very constipated because of peritonitis threw up feces.
Incapacitating Lifestyle Interference
Financial Strain: Having peritonitis meant that participants were unable to work or could only work part-time. For some, their partner had to take time off work. Some could not work for more than 1 month, 1 participant shut down his business, and others were concerned about being able to pay their mortgage. The accumulating cost of frequent hospital appointments to receive treatment for peritonitis also caused financial burden.
Isolation and Separation: Being in hospital meant a disruption to normal family life, and some participants were placed in isolation, so they could not interact with their family. Participants with young children worried about how others such as elderly parents were coping with caring for the children and realized their children would be “missing” them.
Exacerbating Burden on Family: Participants had to call on others such as a parent, spouse, or ex-spouse to help them when they experienced a peritonitis episode because they were too unwell to perform normal tasks. Family members helped in a variety of ways—calling the hospital for advice when the episode first started, driving the patient to hospital, bringing home-cooked food to the hospital each evening, visiting the patient each day, caring for the patient's children, and helping to organize treatment at home for those who did not have to be hospitalized.
Exasperation with Hospitalization
Dread of Hospital Admission: The thought of going to hospital “depressed” participants and was described as “a big price” to pay for making a mistake. Some participants had periods when they were in hospital “nearly every second month” and once there, they would be there for “a couple of weeks again.” They saw the hospital system as an impersonal one and that they were never consistently seen by one doctor.
Exposure to Infection: Some were concerned about the perceived lack of knowledge regarding PD among general hospital staff. For example, 1 participant had a Tenckhoff catheter inserted on an emergency basis and was told by a ward nurse post-operation that she could go for a walk but later learned from the PD nurse that this could cause leakage. Another participant who was admitted to hospital with peritonitis believed “a doctor could've even infected me—he didn't even wash his hands.”
Gruelling Follow-Up Schedule: Managing treatment for peritonitis was confronting for some as they had to inject antibiotics into a dialysis bag. Participants had to go to hospital every 2 days for about 2 weeks to have a blood test to find out if they needed to continue with the antibiotic treatment and this “took a lot of time” out of their normal routine and was “a little frustrating” and “inconvenient” but was accepted by participants as unavoidable.
Receiving Inattentive Care: Some felt they received inadequate care from hospital staff. Some experienced intense pain the first time they were hooked up to the APD machine, and blamed staff for a lack of monitoring. Another patient was given treatment for high blood pressure but staff left him unattended, which led to him blacking out and “even though I had buzzed no one had come.”
Discussion
Peritonitis was an ever-present concern for patients on PD as it meant they would be in pain, vomiting, possibly embarrassed, needing to go to hospital, calling on family or friends for help, and unable to go to work.
Some participants felt that family members should be informed about the process and demands involved in doing PD so that they could depend on their support in preventing and managing peritonitis. Patients found the cleaning routine around doing an exchange to be demanding, more so for those on CAPD compared with APD because of the need to connect and disconnect more often. When peritonitis occurred, patients experienced panic, incapacitating pain, and felt embarrassed because they lost bodily control and normal function. Those who were hospitalized expressed concerns about finances and placing extra responsibilities on family members. Participants who received out-of-hospital treatment felt burdened by frequent visits to the renal unit, the need to inject antibiotics into dialysis bags, and the costs associated with travel to and from the clinic. Many participants had difficulty identifying the symptoms of peritonitis. Changes to the management and the provision of additional support to patients could help them to cope with the challenges they encounter when they have peritonitis.
The systematic review of qualitative studies on patients' experiences of PD found that some patients regarded PD as onerous and a disruptive intrusion. However, there were limited data specifically on peritonitis (12). More recent studies on patient and family perspectives on PD have shown that patients and family members were aware of the threat of peritonitis, took measures to prevent infection, were uncertain of how to manage a crisis, and some could not recognize the symptoms of peritonitis (15). The procedures required to prevent infection were described as “daunting and time-consuming,” and peritonitis was associated with fear and uncertainty (16). Patients' fear of PD-associated peritonitis, placing a burden on family members, and lack of confidence in their ability to maintain proper PD self-care at home have been shown to be barriers to choosing PD as a dialysis modality (17). These were identified in our study. However, our study highlights that patients want family members to be better educated about PD and its requirements, some patients are unclear about the causes of peritonitis and do not believe the treatment they receive is fully effective, patients were strongly motivated to make PD work for them, they were unprepared for the level of pain they experienced and loss of bodily control. For those who could not work and especially those who were self-employed, they were worried about finances. Patients with young children were most concerned about the separation that hospitalization brought, and many patients spoke of the added responsibility that fell on family members when they had peritonitis. We also found that patients dreaded the idea of having to go to hospital, felt they were exposed to inferior treatment and possible infection when in hospital, and found the outpatient treatment schedule to be time-consuming and inconvenient.
In our study, we achieved theoretical saturation and conducted investigator triangulation to ensure that the analysis captured the range and depth of the data collected. However, there are some potential limitations. The transferability of the findings beyond Australia is uncertain but the similarity of our results with studies conducted in the UK suggests broad relevance to other settings. We did not interview non-English speaking participants to avoid cultural and linguistic misinterpretation. In addition, we did not explicitly ask participants if they would prefer hemodialysis to PD, so it is possible that our sample was biased towards remaining on PD.
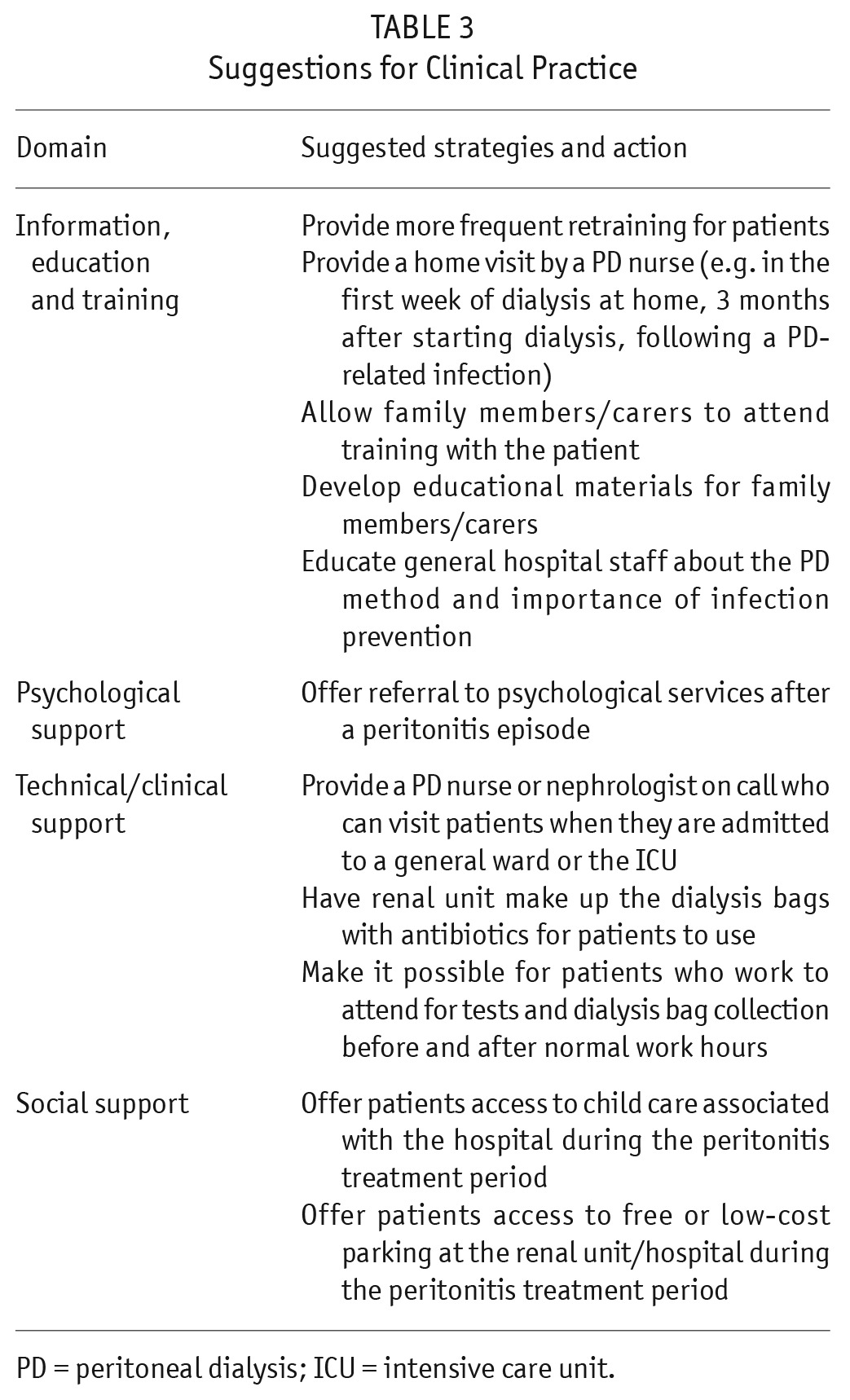
Some participants in this study could not identify the symptoms of peritonitis, and some thought the treatment they were given for peritonitis did not eradicate the cause. The International Society for Peritoneal Dialysis (ISPD) guidelines recommend that retraining occur 3 months after initial training and routinely after that (at least once/year), after hospitalization, after peritonitis or catheter infection, and after change in dexterity, vision, or mental acuity (11). More frequent retraining for patients could help clear up some of the misconceptions they have, reinforce what the symptoms of peritonitis are, and check whether the patient is performing an exchange as they were taught. A home visit by a PD nurse to see how the patient functions in their own environment has been recommended but only some of the participants in this study had received a home visit (18). The desire expressed for family members to be educated about the process of PD and the causes of peritonitis could be accommodated by allowing family members to attend training with the patient or, if this is not practical, to perhaps attend a day specifically designed for families of patients on PD.
Some participants had very mild symptoms when they experienced peritonitis because the infection was detected early. Others had a very different experience, with the peritonitis episode making a major intrusion into their life. Being unable to work for a few weeks and travel costs to and from hospital caused financial strain. Parents with young children, in particular, had to ask family and friends for help and some participants reported being disappointed with the lack of family assistance that occurred. We suggest that child care associated with the hospital be offered to patients who need to attend clinic or be hospitalized because of peritonitis and do not have anyone they can immediately call on. It would also help patients if access to free or low-cost parking at the unit/hospital could be provided during the treatment period.
We found that many participants reluctantly went to hospital when they experienced peritonitis, and the dread was intense for those patients who had repeat episodes of peritonitis. Various reasons for this response to hospitalization have been given, including the reality of the individual's mortality, dealing with an altered level of dependency, grieving for losses (self or lifestyle), and fear of recurrent problems (19). There was a perceived lack of knowledge about PD displayed by general hospital staff, and some patients felt they were potentially exposed to infection. We suggest it would be an improvement if an experienced PD nurse or physician could be on call and visit patients when they are admitted to general wards or the intensive care unit (ICU). When undergoing treatment out of hospital for peritonitis, some units gave participants the antibiotics and instructions on how to inject them into the dialysis bag. Participants said they found this process confronting and that they were not confident of doing it correctly. More practical support for antibiotic pre-administration is needed. In addition, having to go to the hospital or renal unit every 2 days for 2 weeks was time-consuming for patients and it would be an improvement if patients who are working could attend for tests and bag collection before and after normal work hours. Table 3 outlines our suggestions for clinical practice.
TABLE 3.
Suggestions for Clinical Practice
Our findings have yielded insights into the perspectives of adult PD patients about peritonitis. Further research could be conducted which explores the effect of giving patient education and retraining on an ongoing basis (e.g. every 6 months) rather than in response to an event such as hospitalization, after peritonitis, or catheter infection.
Conclusions
Patients were highly motivated to remain on PD but many found the cleaning demands and instructions around doing an exchange to be overwhelming. Some participants were unclear about the symptoms of peritonitis and others were confused about the causes of peritonitis. Peritonitis impacted participants physically, socially, and financially as it affected their ability to work and perform normal tasks. Participants wanted to avoid hospitalization, reported suboptimal care when in hospital, and, for those who were treated out of hospital for peritonitis, found the frequent trips to the renal unit or hospital to be inconvenient and time-consuming. Understanding the experiences and needs of PD patients who have had peritonitis can be used to inform strategies for patient-centered health care. Understanding the beliefs of patients about peritonitis and their knowledge of symptoms can also help inform training strategies aimed at educating patients on this topic.
Disclosures
DM has received consultancy fees, speaker's honoraria and travel assistance from Baxter Healthcare. FB is a consultant for Baxter Healthcare and Fresenius and has received travel grants from Amgen and Roche. The remaining authors have no competing financial interests to declare.
Supplementary Material
Acknowledgments
We sincerely thank all of the patients who contributed their time and energy to participate in this study. We also thank the PD nurse at each of the participating units (Laraine Aw, Richard Shipton-Smith, and Francine Lynn) who provided us with the names and contact details of patients suitable for interview.
Denise Campbell was funded by a National Health and Medical Research Council postgraduate scholarship.
Footnotes
Supplemental material available at www.pdiconnect.com
REFERENCES
- 1. Daly CD, Campbell MK, MacLeod AM, Cody DJ, Vale LD, Grant AM, et al. Do the Y-set and double-bag systems reduce the incidence of CAPD peritonitis? A systematic review of randomized controlled trials. Nephrol Dial Transplant 2001; 16(2):341–7. [DOI] [PubMed] [Google Scholar]
- 2. Piraino B. Peritonitis as a complication of peritoneal dialysis. J Am Soc Nephrol 1998; 9(10):1956–64. [DOI] [PubMed] [Google Scholar]
- 3. Fried LF, Bernardini J, Johnston JR, Piraino B. Peritonitis influences mortality in peritoneal dialysis patients. J Am Soc Nephrol 1996; 7(10):2176–82. [DOI] [PubMed] [Google Scholar]
- 4. Woodrow G, Turney JH, Brownjohn AM. Technique failure in peritoneal dialysis and its impact on patient survival. Perit Dial Int 1997; 17(4):360–4. [PubMed] [Google Scholar]
- 5. Choi P, Nemati E, Banerjee A, Preston E, Levy J, Brown E. Peritoneal dialysis catheter removal for acute peritonitis: a retrospective analysis of factors associated with catheter removal and prolonged postoperative hospitalization. Am J Kidney Dis 2004; 43(1):103–11. [DOI] [PubMed] [Google Scholar]
- 6. Johnson DW, Dent H, Hawley CM, McDonald SP, Rosman JB, Brown FG, et al. Associations of dialysis modality and infectious mortality in incident dialysis patients in Australia and New Zealand. Am J Kidney Dis 2009; 53(2):290–7. [DOI] [PubMed] [Google Scholar]
- 7. Piraino B, Bernardini J, Sorkin M. Catheter infections as a factor in the transfer of continuous ambulatory peritoneal dialysis patients to hemodialysis. Am J Kidney Dis 1989; 13(5):365–9. [DOI] [PubMed] [Google Scholar]
- 8. Canada-USA (CANUSA) Peritoneal Dialysis Study Group Adequacy of dialysis and nutrition in continuous peritoneal dialysis: association with clinical outcomes. J Am Soc Nephrol 1996; 7(2):198–207. [DOI] [PubMed] [Google Scholar]
- 9. Kawaguchi Y, Ishizaki T, Imada A, Oohira S, Kuriyama S, Nakamoto H, et al. Searching for the reasons for drop-out from peritoneal dialysis: a nationwide survey in Japan. Perit Dial Int 2003; 23(Suppl 2):S175–7. [PubMed] [Google Scholar]
- 10. Fernandes N, Bastos MG, Cassi HV, Machado NL, Ribeiro JA, Martins G, et al. The Brazilian Peritoneal Dialysis Multicenter Study (BRAZPD): characterization of the cohort. Kidney Int Suppl 2008; (108):S145–51. [DOI] [PubMed] [Google Scholar]
- 11. Piraino B, Bernardini J, Brown E, Figueiredo A, Johnson DW, Lye W-C, et al. ISPD position statement on reducing the risks of peritoneal dialysis-related infections. Perit Dial Int 2011; 31(6):614–30. [DOI] [PubMed] [Google Scholar]
- 12. Tong A, Lesmana B, Johnson D, Wong G, Campbell D, Craig J. The perspectives of adults living with peritoneal dialysis: thematic synthesis of qualitative studies. Am J Kidney Dis 2013; 61(6):873–88. [DOI] [PubMed] [Google Scholar]
- 13. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007; 19(6):349–57. [DOI] [PubMed] [Google Scholar]
- 14. Strauss A, Corbin J. Basics of qualitative research: techniques and procedures for developing grounded theory. California: Sage Publications; 1998. [Google Scholar]
- 15. Baillie J, Lankshear A. Patient and family perspectives on peritoneal dialysis at home: findings from an ethnographic study. J Clin Nurs 2015; 24(1-2):222–34. [DOI] [PubMed] [Google Scholar]
- 16. Baillie J, Lankshear A. Patients' and relatives' experiences of peritonitis when using peritoneal dialysis. J Ren Care 2015; 41(3):177–86. [DOI] [PubMed] [Google Scholar]
- 17. Tungsanga K, Kanjanabuch T, Mahatanan N, Praditpornsilp K, Avihingsanon Y, Eiam-Ong S. The status of, and obstacles to, continuous ambulatory peritoneal dialysis in Thailand. Perit Dial Int 2008; 28(Suppl 3):S53–8. [PubMed] [Google Scholar]
- 18. Bender FH, Bernardini J, Piraino B. Prevention of infectious complications in peritoneal dialysis: best demonstrated practices. Kidney Int Suppl 2006; (103):S44–54. [DOI] [PubMed] [Google Scholar]
- 19. Reactions to illness in the hospitalized adult. [Online.] Available at: https://www.nurseslearning.com/courses/nrp/nrp-1617/Section2/index.htm Accessed 15 February 2016.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.