Abstract
A 74-year-old man with multiple aortic aneurysms and shaggy aorta was simultaneously treated by conventional open repair for an abdominal aortic aneurysm and endoluminal stent grafting for a thoracic aortic aneurysm. We performed intermittent clamping of the visceral and carotid arteries under an extracorporeal circulation circuit without a blood flow pump, which lead to the avoidance of embolization in spite of the disadvantage of endoluminal stent grafting for atheromatous aorta.
Keywords: severely atheromatous aorta, multiple aortic aneurysms, endoluminal therapy
Introduction
Endoluminal therapy (ET) has been rapidly widespread as a minimally invasive procedure for aortic aneurysms. However, ET for severely atheromatous aorta is not feasible because of the high risk of embolization, which leads to cerebral infarction, renal and visceral ischemia, and paraplegia/paraparesis. Patel et al.1) reported the risk of intraoperative embolization in the ET procedure for severely atheromatous aorta; 10% incidence of renal infarction; and 5% incidence of bowel ischemia. We report a successful hybrid procedure of grafting and endoluminal stent grafting for multiple aortic aneurysms, which prevents embolization intraoperatively.
Case Report
A 74-year-old man with a history of hypertension, hyperlipidemia, atrial fibrillation, and esophageal varices was referred to our hospital with concomitant thoracic and abdominal aortic aneurysms (AAAs). Computed tomography (CT) showed a 52-mm saccular thoracic aortic aneurysm (TAA) at the distal aortic arch and a 51-mm fusiform AAA (Fig. 1). Severe atherosclerotic plaques from the descending thoracic aorta to the abdominal aorta, also known as “shaggy aorta”, and complete occlusion of the right common iliac artery were also observed (ankle brachial index on the right lower extremity; 0.62). Furthermore, both internal carotid arteries showed 50% stenosis at bifurcation.
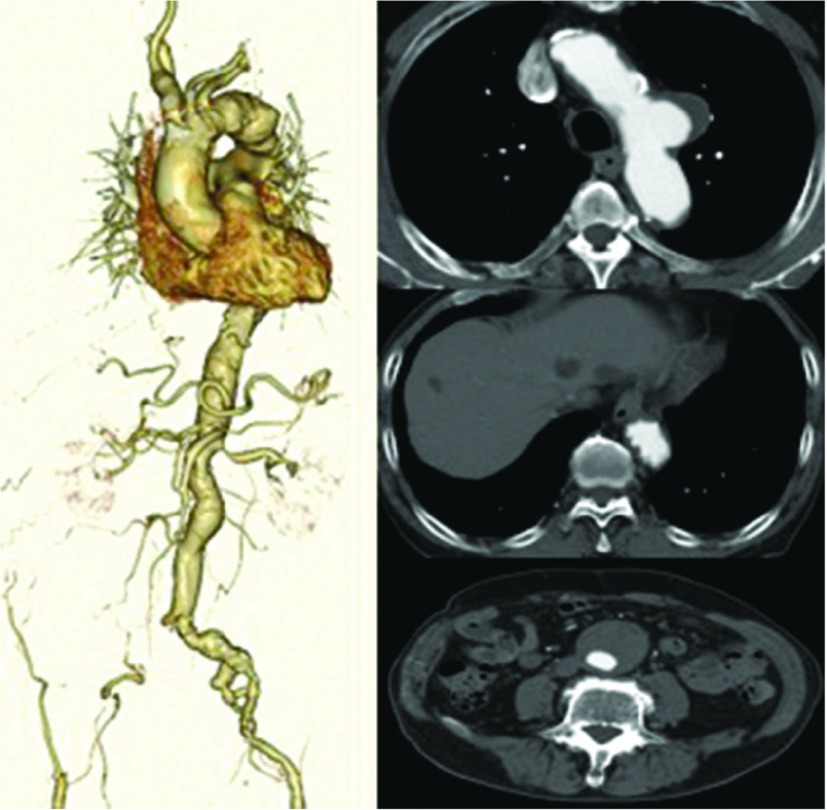
Fig. 1.
CT shows an atheroma-rich aorta with an obstruction of the right common iliac artery, a saccular aneurysm in the thoracic aorta, and a fusiform aneurysm in the abdominal aorta. CT: computed tomography
We decided to perform ET for the TAA and grafting for the AAA simultaneously. This is because the patient strongly wished for simultaneous treatment, and we had previous experience with a case of shaggy aorta that was treated by ET using extracorporeal circulation circuit (ECC).2) In addition, we judged that clamping visceral arteries directly was an advantage in laparoscopy. The strategy for intraoperative prevention of embolization was as follows: compression of the common carotid arteries which did not have atheroma confirmed by preoperative CT scan; intermittent clamping of the visceral arteries that did not have any atheroma and calcification; and similarly, clamping vascular graft of both iliac legs at the bifurcation and ECC, which was established by drainage from the graft and by perfusion to the femoral vein via a filter (FT-50, 50 ml, JMS Co., Ltd., Tokyo, Japan) to trap debris. Further spinal fluid drainage was performed preoperatively, and the intraoperative motor-evoked potential was observed for prevention of spinal cord ischemia.
The graft (InterGard K 20 × 10 mm, MAQUET Japan K.K., Tokyo, Japan) was trimmed in advance, as shown in Fig. 2. The limbs of the graft were cut in the middle to make the graft tetra-furcated, two limbs were anastomosed to the iliac arteries, another was used for ECC, and the final limb was used as an access route of ET (Fig. 3). After grafting, we began ET and clamped the visceral and limb arteries in the operative field, and the anesthesiologist compressed the carotid arteries above the skin during catheter and wire manipulation with perfusion of ECC. It took less than 2 minutes to complete most of the manipulation, and ECC remained perfuse for 30 more seconds after declamping of the vessels. Next, we inserted the Medtronic Variant Thoracic Stent Graft System (Medtronic Vascular, Santa Rosa, CA, USA) to the distal aortic arch with clamping and compressing vessels, which took 90 seconds. Furthermore, during injection and removal of all instruments, the same manipulation was performed, with an eventual total ischemic time of about 5 min. A large amount of debris was captured in the filter (Figs. 4a and 4b). During the procedure, mean blood pressure was maintained above 100 mmHg, and the hemodynamics was stable even when ECC was perfused. Postoperative contrast CT scan showed no embolization and complete exclusion of TAA (Fig. 4c). In the laboratory examinations, liver damage and elevation of creatinine kinase level were not observed. The patient walked out of the hospital independently 12 days after operation without any complications.
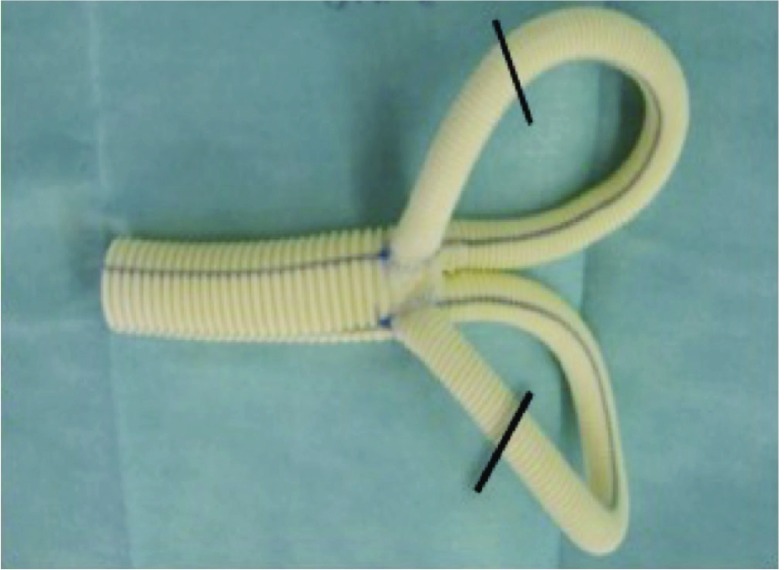
Fig. 2.
A photograph showing a graft with the end of the limb sutured to the graft body. The limbs were then cut at the lines to make a tetra-furcated graft.
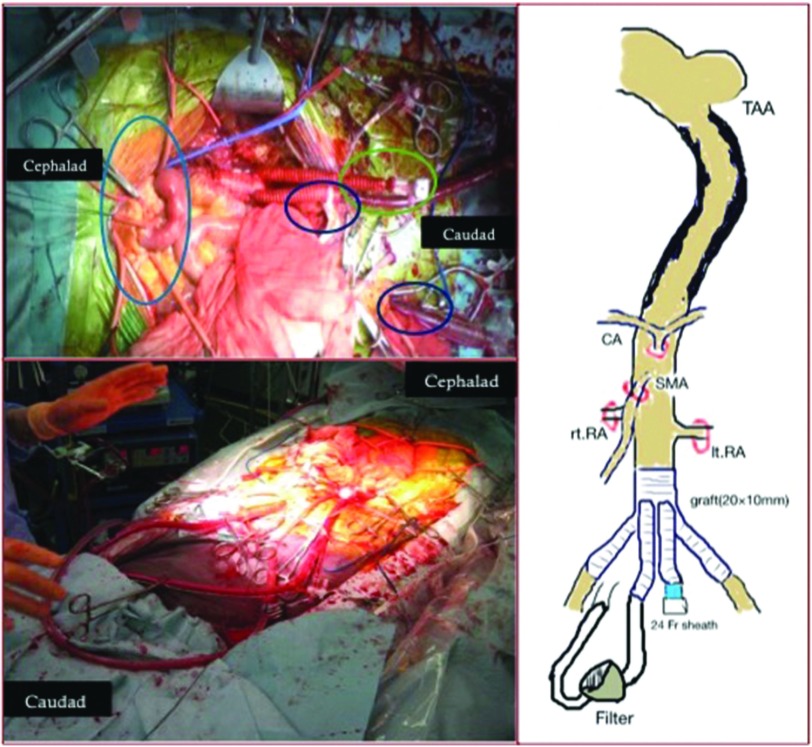
Fig. 3.
Two pictures and a schema showing the operating field after grafting of the abdominal aorta. Visceral vessels are taped with tourniquets. A sheath (24 Fr GORE DrySeal Sheath with Hydrophilic Coating, W.L. Gore & Associates, Flangstaff, AZ, USA) is inserted to a graft limb for the access route of ET, and the drainage tube is inserted to another graft limb and perfusion to the femoral vein. ET: endoluminal therapy; CA: celiac artery; SMA: superior mesenteric artery; RA: renal artery; FV: femoral vein; TAA: thoracic aortic aneurysm
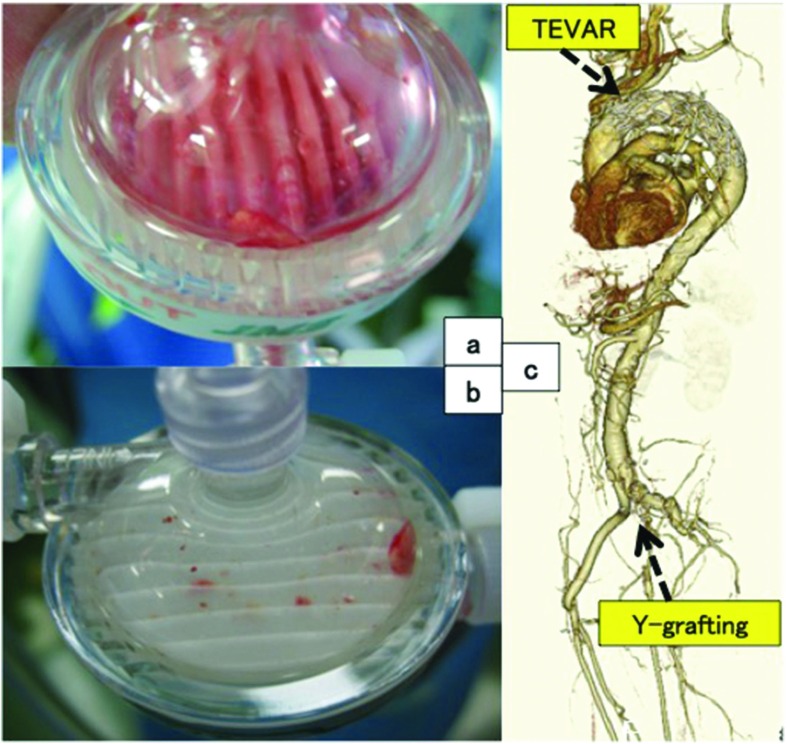
Fig. 4.
Photographs showing the large amount of debris that was captured by the filter (a) and (b). Postoperative 3D-CT showing successful Zone 2 TEVAR without any endoleak (c). 3D-CT: three-dimensional computed tomagraphy; TEVAR: thoracic endovascular aortic repair
Discussion
Castelli et al.3) reported that simultaneous ET for concomitant aneurysms is feasible, which is attractive in terms of minimal invasiveness and safety. On the other hand, it is known that ET for shaggy aorta has a high risk of stroke and bowel ischemia,1,4) and some articles have reported cases of shaggy aorta that were treated by ET using ECC or other protection devices such as an intra-aortic filter catheter against debris.5) In our institution, conventional grafting is usually considered as a standard therapy for the shaggy aorta; however, mortality and morbidity of a combined procedure of conventional TAA and AAA are still high. Furthermore, when one aneurysm is treated preferentially, there is a possibility of rupture of the other. Finally, we selected the simultaneous procedure for concomitant aneurysms with patient’s strong wish and we modified the method on the previous case that we had experienced the concomitant therapy: Thoracic endovascular aortic repair (TEVAR) for TAA and hemicolectomy for colon cancer in laparotomy.
Based on our experience of the previous case, we devised a method to secure the prevention of embolization.2) While handling wires and catheters or inserting a device, we clamped the cerebral, visceral, and lower extremity arteries; thus, most of the blood flow in the aorta circulated through the ECC with a filter, which captured a large amount of debris. A problem with this procedure, however, is that clamping carotid arteries by pressing the skin may not be a reliable method. On the other hand, other methods—for example, exposing arteries to be clamped directly or to occlude from the inside by ballooning—have equivalent risks of stroke to the above-mentioned method. In particular, the method we used was considered feasible for this case with cervical stenosis. In addition, another problem is the limitation of time period for which vessels can be clamped. We repeatedly clamped and declamped to shorten the ischemic time as much as possible, but it is possible that movement of the wire caused by a pulsatile aorta could separate debris from the aorta.
Conclusion
ET as a method for severely atheromatous aorta treatment is not recommended; however, in cases of shaggy aorta with multiple aortic aneurysms, such as in this case, a simultaneous hybrid procedure is one possible option. In particular, the method by which we performed clamping of visceral arteries reliably prevents embolization and is capable of avoidance of bowel ischemia intraoperatively.
Disclosure Statement
None.
Authors’ Contribution
Study conception: TT and ST
Investigation: TT and AK
Writing: TT
Critical review and revision: all authors
Final approval of the article: all authors
Accountability for all aspects of the work: all authors
References
- 1).Patel SD, Constantinou J, Hamilton H, et al. Editor’s choice—A shaggy aorta is associated with mesenteric embolisation in patients undergoing fenestrated endografts to treat paravisceral aortic aneurysms. Eur J Vasc Endovasc Surg 2014; 47: 374-9. [DOI] [PubMed] [Google Scholar]
- 2).Igarashi T, Takase S, Satokawa H, et al. Thoracic endovascular aortic repair with visceral arteries intermittent clamp technique for descending thoracic aortic aneurysm with shaggy aorta. Ann Vasc Surg 2013; 27: 974.e11-4. [DOI] [PubMed] [Google Scholar]
- 3).Castelli P, Caronno R, Piffaretti G, et al. Endovascular repair for concomitant multilevel aortic disease. Eur J Cardiothorac Surg 2005; 28: 478-82. [DOI] [PubMed] [Google Scholar]
- 4).Fukuda I, Daitoku K, Minakawa M, et al. Shaggy and calcified aorta: surgical implications. Gen Thorac Cardiovasc Surg 2013; 61: 301-13. [DOI] [PubMed] [Google Scholar]
- 5).Wada T, Anai H, Shuto T, et al. A new method for protection from shower embolism during TEVAR on a shaggy aorta. Gen Thorac Cardiovasc Surg 2015; 63: 105-8. [DOI] [PubMed] [Google Scholar]