Abstract
AIM
To evaluate the incidence and characteristics of kidney stones in kidney transplant recipients.
METHODS
A literature search was performed using MEDLINE, EMBASE, and Cochrane Database of Systematic Reviews from the inception of the databases through March 2016. Studies assessing the incidence of kidney stones in kidney transplant recipients were included. We applied a random-effects model to estimate the incidence of kidney stones.
RESULTS
Twenty one studies with 64416 kidney transplant patients were included in the analyses to assess the incidence of kidney stones after kidney transplantation. The estimated incidence of kidney stones was 1.0% (95%CI: 0.6%-1.4%). The mean duration to diagnosis of kidney stones after kidney transplantation was 28 ± 22 mo. The mean age of patients with kidney stones was 42 ± 7 years. Within reported studies, approximately 50% of kidney transplant recipients with kidney stones were males. 67% of kidney stones were calcium-based stones (30% mixed CaOx/CaP, 27%CaOx and 10%CaP), followed by struvite stones (20%) and uric acid stones (13%).
CONCLUSION
The estimated incidence of kidney stones in patients after kidney transplantation is 1.0%. Although calcium based stones are the most common kidney stones after transplantation, struvite stones (also known as “infection stones”) are not uncommon in kidney transplant recipients. These findings may impact the prevention and clinical management of kidney stones after kidney transplantation.
Keywords: Nephrolithiasis, Incidence, Kidney stones, Kidney transplantation, Transplantation
Core tip: The authors performed this meta-analysis to assess the incidence and characteristics of kidney stones in kidney transplant recipients. The estimated incidence of kidney stones in patients after kidney transplantation is 1.0%. Calcium based stones (CaOx and CaP) are the most common kidney stones after transplantation following by struvite stones and uric acid stones. The findings from this study may impact the management of kidney stone prevention after kidney transplantation.
INTRODUCTION
Kidney stones are one of the most common metabolic disorders and urological problems with a prevalence of 7.2%-7.7% in the adult population, and a ten-year recurrence rate of ≥ 30%[1-4]. The incidence of kidney stones is increasing especially in industrialized countries with an estimated global prevalence between 10%-15%[5-8]. Approximately 13% of men and 7% women will have a kidney stone during their lifetime[5,8].
Previous studies have shown that stone recurrence rates may be lower, when glomerular filtration rate (GFR) reduced[9,10]. Thus, patients with advanced chronic kidney disease (CKD) or end-stage kidney disease (ESRD) may encounter less stone disease[10], reported being as low as 0.68%[11]. After successful kidney transplantation, ESRD patients subsequently have significant improvement in renal function resulting in urinary excretion of metabolites that increases risk of stone disease. Studies have identified kidney stones in allograft kidney as one of the serious problems in kidney transplant recipients[12-40]. However, unlike the general population, the incidence and characteristics of kidney stones in kidney transplant recipients are not well studied. The aim of this meta-analysis was to appraise the incidence and types of kidney stones after kidney transplantation.
MATERIALS AND METHODS
Cheungpasitporn W and Thongprayoon C individually examined published studies and conference abstracts indexed in MEDLINE, EMBASE, and Cochrane Database from the inception of the databases through March 2016. The search strategy used is detailed in the supplementary material (Item 1). Further pertinent studies were retrieved by conducting a manual search using references from the articles that were reclaimed from the search strategy noted above. We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for systematic reviews and meta-analyses[41] and previously published guidelines[42,43].
The inclusion criteria were as follows: (1) randomized controlled trials or observational studies (case-control, cross-sectional, cohort studies, or case series); (2) patient population age > 18 years old; and (3) data on kidney stones in kidney transplant recipients were provided. The search was limited to English-language studies. Both published studies and conference abstracts were incorporated. Study eligibility was independently determined by the two investigators mentioned earlier. Differing decisions were settled by joint agreement.
A standardized information collection form was applied to derive the following data: The first author of each study, study design, year of publication, country where the study was conducted, number of kidney transplant recipients studied, number of patients with kidney stone, age and gender of patients with kidney stones, time of diagnosis after kidney transplantation, type of donor (Live or deceased donor), type and location of kidney stones, and period of follow-up.
Statistical analysis
MetaXL software (EpiGear International Pty Ltd)[44] was utilized for data analysis. The incidence rates (IRs) and 95%CIs of adverse effects were reported using a DerSimonian-Laird random-effects model[45]. A random-effects model was implemented due to the high likelihood of inter-study variances. The Cochran Q test was completed to assess statistical heterogeneity. The I2 statistic was added to evaluate the degree of variation across studies related to heterogeneity instead of chance. An I2 of 0%-25% represents insignificant heterogeneity, 26%-50% low heterogeneity, 51%-75% moderate heterogeneity and > 75% high heterogeneity[46]. To assess for publication bias funnel plots were used[47].
RESULTS
Our search strategy yielded 1554 articles. Of these, 1397 articles were excluded following the review of their title and abstract based on their relevance and the eligibility criteria. The remaining 157 articles underwent full-length review, and an additional 136 were excluded for failing to meet the criteria. Twenty one articles[12-29,36,38,40] met all inclusion criteria and were identified for the meta-analysis of kidney stones in kidney transplant recipients (Table 1). Supplementary Item 2 outlines our search methodology and selection process.
Table 1.
Main characteristics of the studies included in this meta-analysis
| Ref. | Country | Year | Total number | No. of patients with kidney stone | Time of diagnosis | Sex of patients with stone | Age of patients with stone | Donors | Stone location | Stone composition | Mean follow-up time |
| Cho et al[12] | United States | 1988 | 544 | 9 | Mean 14.7 mo, Median 7 mo (range 3-42 mo) | 6 male, 3 female | Mean 30 yr (range 8-65 yr) | 6 living, 3 cadaveric | 4 bladder, 3 kidney, 2 unknown | 4 calcium oxalate/calcium phosphate, 2 ammonium magnesium phosphate and carbonate appetite, 1 uric acid, 2 not studied | 5 (range 1.5-15.5) yr |
| Hayes et al[13] | United States | 1989 | 892 | 10 | Mean 13 mo (range 4-49 mo) | 7 male, 3 female | Mean 29 yr (range 17-53 yr) | 3 living, 7 cadaveric | NR | NR | NR |
| Harper et al[38] | United Kingdom | 1994 | 178 | 6 | NR | 4 male, 1 female | NR | 4 living, 1 cadaveric | NR | 1 uric acid, 2 calcium phosphate, 1 calcium oxalate, 1 Magnesium ammonium phosphate | NR |
| Shoskes et al[14] | United Kingdom | 1995 | 812 | 2 | Mean 3.5 yr (range 2-5 yr) | NR | Mean 40 yr | NR | 2 ureter | NR | At least 1 yr |
| Benoit et al[36] | France | 1996 | 1500 | 12 | NR | 7 male, 5 female | Mean 36 yr | 2 living, 10 cadaveric | 5 calyces, 6 ureter, 1 pyeloureteral junction | 4 calcium oxalate and phosphate, 2 struvite | NR |
| Del Pizzo et al[15] | United States | 1998 | 540 (445 renal transplant, 95 pancreas/renal transplant) | 4 | NR | NR | NR | NR | NR | NR | |
| Rhee et al[16] | United States | 1999 | 1813 (1730 renal transplant, 83 pancreas/renal transplant) | 8 | NR | 4 male, 4 female | Mean 51 yr (range 34-60 yr) | 2 living, 1 cadaveric, 5 pancreas/renal | 3 kidney, 1 ureter, 4 bladder | 1 uric acid, 1 calcium oxalate, 1 calcium oxalate/calcium phosphate, 1 calcium phosphate, 1 struvite stone, 3 unknown | Mean 68.6 mo (range 27-98 mo) |
| El-Mekresh et al[17] | Egypt | 2001 | 1200 | 11 | NR | NR | NR | NR | 3 kidney, 4 ureter, 4 bladder | NR | NR |
| Kim et al[18] | United States | 2001 | 849 | 15 | Mean 17.8 mo (range 3-109 mo) | 10 male, 5 female | Mean 41.5 yr (range 28-67 yr) | 8 living, 7 cadaveric | 11 bladder, 3 kidney, 1 multiple sites | 5 mixed form of calcium oxalate and calcium phosphate, 1 calcium oxalate, 3 predominant calcium phosphate, 2 struvite, 2 mixed form of struvite and calcium phosphate, 2 not studied | Mean 58 mo (range 11-149 mo) |
| Klinger et al[19] | Austria | 2002 | 1027 | 19 (4 diagnosis during transplant, 5 perioperative, 10 de novo) | For de novo: Mean 27.7 mo (range 13 to 48 mo) | 8 male, 11 female | Mean 48.1 yr (range 26-72 yr) | 1 living, 18 cadaveric | 14 kidney, 3 infundibulum, 1 distal ureter, 1 staghorn | 11 calcium oxalate, 2 uric acid, 1 calcium phosphate, 5 not studied | Mean 29 mo (range 14-48 mo) |
| Doehn et al[20] | Germany | 2002 | 1500 | 11 | NR | 5 male, 6 female | Median 50 yr | 11 cadaveric | NR | 3 uric acid, 3 calcium oxalate, 2 magnesium ammonium stone, 3 not studied | Median 4 yr |
| Streeter et al[21] | United Kingdom | 2002 | 1535 | 12 | For renal calculi: Median 150 d (range 56-1280 d); For bladder calculi: Range 8 mo - 4 yr | NR | NR | NR | 9 ureter, 3 bladder | NR | NR |
| Abbott et al[22] | United States | 2003 | 42906 | 52 | NR | NR | NR | 35 kidney, 17 ureter | NR | 1.89 ± 1.15 yr | |
| Lipke et al[23] | United States | 2004 | 500 | 7 | 9 mo (range 1.5-26 mo) | 7 female | Mean 50 yr (range 8-73 yr) | 4 living, 3 cadaveric | 7 bladder | 7 mixed between calcium oxalate and calcium phosphate | NR |
| Yigit et al[24] | Turkey | 2004 | 125 | 5 (2 preoperative, 1 early posttransplant, 2 de novo) | For de novo: Mean 6.5 mo (range 6-7 mo) | 3 male, 2 female | Mean 35.2 yr | NR | NR | 2 calcium oxalate, 1 uric acid, 2 infectious | Mean 32.4 mo |
| Challacombe et al[25] | United Kingdom | 2005 | 2085 | 21 | 3.7 (0.17-18) yr | 8 male, 13 female | Mean 41 yr (range 15-64 yr) | 3 living, 18 cadeveric | 13 kidney, 7 ureter, 1 bladder | NR | NR |
| Ferreira Cassini et al[26] | Brazil | 2012 | 1313 | 12 de novo | Range 6 mo to 13 yr | 8 males, 9 females | Mean 45.6 yr (range 32-63 yr) | 2 living, 15 cadaveric | 6 calyces, 3 renal pelvis, 3 ureter | NR | NR |
| Stravodimos et al[27] | Greece | 2012 | 1525 | 7 | Mean 3.2 (2-7) yr | NR | NR | NR | 5 kidney, 2 ureter | NR | Mean 8 yr |
| Cicerello et al[40] | Italy | 2014 | 953 | 10 | NR | 4 male, 6 female | Mean 43 yr | NR | 7 kidney, 3 ureter | NR | NR |
| Mamarelis et al[28] | Greece | 2014 | 2045 | 9 | Mean 3.1 yr (range 1-7 yr) | NR | NR | NR | 6 kidney, 3 ureter | NR | 6.6 yr (range 1-15 yr) |
| Rezaee-Zavereh et al[29] | Iran | 2015 | 574 | 25 | NR | NR | NR | NR | NR | NR | 55 ± 53 mo |
CaOx: Calcium oxalate; CaP: Calcium phosphate; NR: Not reported.
Incidence of kidney stones in kidney transplant recipients
The incidence of kidney stones after kidney transplantation within the 21 individual study ranged between 0.2% to 4.4% with an overall meta-analytical incidence of 1.0% (95%CI: 0.6%-1.4%)with evidence of a high level of heterogeneity (I2 = 93%, P < 0.001; Figure 1).
Figure 1.
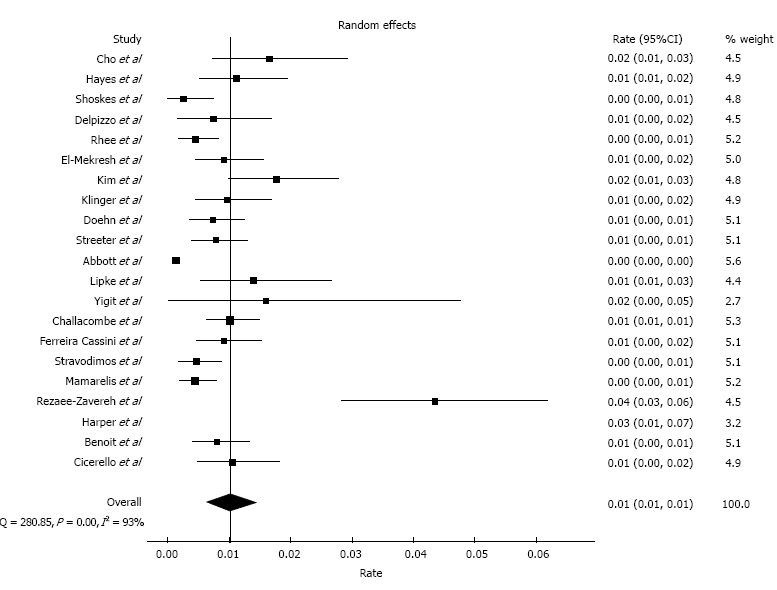
Forest plot of incidence of kidney stones in kidney transplant populations.
We performed a sensitivity analysis limited only to the studies that provided data on time of kidney stone diagnosis after kidney transplantation; the estimated incidence of kidney stones was 0.9% (95%CI: 0.7%-1.2%), and there was evidence of a high level of heterogeneity (I2 = 60%, P < 0.001; Figure 2). The mean duration to diagnosis of kidney stones after kidney transplantation was 28 ± 22 mo.
Figure 2.
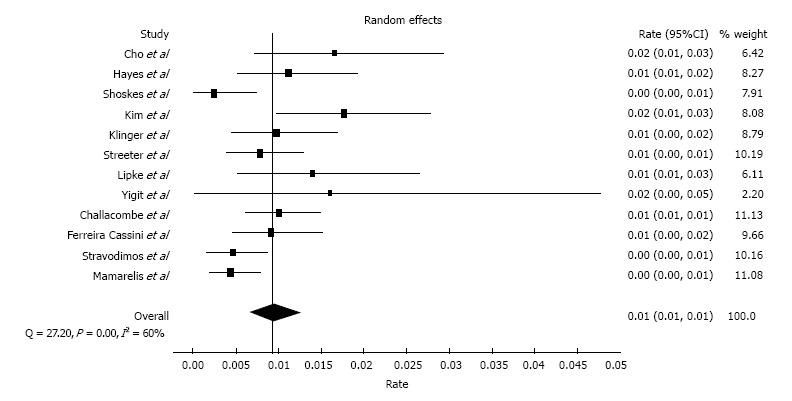
Forest plot of incidence of kidney stones in kidney transplant populations limited only to the studies that provided data on the time of kidney stone diagnosis after kidney transplantation.
Subgroup analyses by geographic information were also performed. The estimated incidences of kidney stones were 0.9% (95%CI: 0.3%-1.7%; I2 = 94%) and 0.7% (95%CI: 0.5%-0.9%; I2 = 40%) in the United States and Europe, respectively. Data on the incidence of kidney stones in kidney transplant recipients in other geographical area were limited as shown in Table 1.
Characteristics of kidney transplant recipients with kidney stones
The mean age of patients with kidney stones was 42 ± 7 years. Within reported studies (Table 1), approximately 50% of kidney transplant recipients with kidney stones were males.
Types of kidney stones in kidney transplant recipients
Sixty-seven percent of kidney stones were calcium-based stones (30% mixed CaOx/CaP, 27%CaOx and 10%CaP), followed by struvite stones (20%) and uric acid stones (13%) as shown in Table 1.
Risk factors for kidney stones in kidney transplant recipients
Despite limited data on urinary supersaturation and risk factors for kidney stones, studies reported increased risk of kidney stones in kidney transplant recipients with hyperparathyroidism, hypercalciuria, hypocitraturia, hypophosphatemia, and urinary tract infection[28,38]. Harper et al[38] found that urinary excretion of magnesium and phosphate was at the lower range for all kidney transplant recipients with kidney stones. Uncommonly, urinary outflow obstruction and foreign bodies were also found as risk factors for kidney stones in kidney transplant patients[28,48].
Allograft failure in kidney transplant recipients with kidney stones
As in general patient populations, kidney stones can also cause acute kidney injury in kidney transplant recipients[49-52]. Since kidney transplant recipients can have obstructed kidney stones without any symptom of pain[26,28], prompt diagnosis and the removal of obstructed stones are the keys to preventing renal allograft failure[18]. Rezaee-Zavareh et al[29] reported no significant association between kidney stones after transplantation and graft survival (OR = 1.04; CI: 0.71-1.54). With the prompt removal of stones, Kim et al[18] found no significant changes in renal allograft function at diagnosis and after removal of kidney stones.
Evaluation for publication bias
Funnel plot evaluating publication bias for the incidence of kidney stones in kidney transplant recipients demonstrated slight asymmetry of the graph and thus suggested the presence of publication for positive studies regarding the incidence of kidney stones.
DISCUSSION
In this study, we demonstrated that an overall incidence of kidney stones in kidney transplant recipients was 1.0%. The mean age of recipients with kidney stones was 42, and half of stone formers were males. Calcium based (CaOx and CaP) stones were the most common types of kidney stones after kidney transplantation, followed by struvite stones and then uric acid stones.
The incidence of kidney stones after kidney transplantation from our meta-analysis is much lower than reported in the general adult populations[5-8]. Although the mechanisms behind the lower incidence of kidney stones after kidney transplantation, when compared with the general population, are only speculative, there are several plausible explanations. First, with the observation that new kidney stones are usually formed in transplanted allograft kidney but not in native non-functioning kidneys, kidney transplant recipients have significantly improved but still lower GFRs than those in healthy general populations, which may be “protective” for stone disease[9,10]. Second, transplanted kidneys are from healthy donors ideally without tubulointerstitial defects, one not uncommon cause of kidney stones. Third, it is possible that kidney stones after kidney transplantation are underdiagnosed since recipients may spontaneously pass them from the transplanted kidney/ureter without pain or awareness.
Calcium based (CaOx and CaP) stones are the most common types of kidney stones in the general population as well as after kidney transplantation as demonstrated in our meta-analysis. Interestingly, struvite stones (ammonium magnesium phosphate) or “infection stones” is more common in kidney transplant recipients (20%) than in the general population (10%-15%)[53]. Since struvite stones are associated with infection with urea-splitting bacteria and the principles of treating struvite stones are different than other stones types, including removal of all stone fragments and use of antibiotics[53], this information is important for future studies targeting prevention and management of kidney stones after kidney transplantation.
There are several limitations to our study. First, there were statistical heterogeneities in the analysis of the incidence of kidney stones. The potential sources of this heterogeneity included differences in diagnostic methodology of kidney stones and follow-up duration. However, a sensitivity analysis that limited studies to those that only provided data on time of kidney stone diagnosis still showed a similar incidence rate of kidney stones, consistent with the finding of our primary analysis. Second, most included studies were conducted in developed Western countries with the majority of the subjects being Caucasian. Thus, our findings may not represent renal transplant populations from other parts of the world. Lastly, the data on urinary supersaturation and risk factors for kidney stones were limted. Although struvite stones represent an association with urinary tract infection, it is still unclear the risk factors for other stone types after kidney transplantation, and future studies are needed.
Our meta-analysis demonstrates that the estimated incidence of kidney stones in patients after kidney transplantation is 1.0%. Although calcium based stones are the most common kidney stones after transplantation, struvite stones are the second common type. These findings may impact clinical prevention and management of kidney stones in kidney transplant recipients.
COMMENTS
Background
Renal stones are one of the most prevalent metabolic disorders and urological problems. However, with reduced kidney functions, patients with advanced chronic kidney disease (CKD) or end-stage kidney disease (ESRD) may encounter less stone disease. After successful kidney transplantation, ESRD patients have significant improvement in kidney functions and may develop kidney stones in their allograft kidney.
Research frontiers
The incidence and characteristics of kidney stones in kidney transplant recipients are not well studied. It is thus necessary to assess the incidence and types of kidney stones after kidney transplantation.
Innovations and breakthroughs
In this study, the authors demonstrated that an overall incidence of kidney stones in kidney transplant recipients was 1.0%. The mean age of recipients with kidney stones was 42, and half of stone formers were males. Calcium based (CaOx and CaP) stones were the most common types of kidney stones after kidney transplantation, followed by struvite stones and then uric acid stones.
Applications
The data in this study demonstrates an estimated incidence of kidney stones in patients after kidney transplantation of 1.0%. Calcium based stones and struvite stones are common types of kidney stones after transplantation. These findings may impact the clinical management of kidney stones prevention in kidney transplant recipients.
Terminology
CaOx: Calcium oxalate; CaP: Calcium phosphate; CKD: Chronic kidney disease; GFR: Glomerular filtration rate; NR: Not reported.
Peer-review
This is a reasonable first meta-analysis of incidence of kidney stones in kidney transplant recipients. The results have potential clinical applications.
Footnotes
Conflict-of-interest statement: All authors report no conflicts-of-interest.
Data sharing statement: No additional data are available.
Manuscript source: Invited manuscript
Specialty type: Transplantation
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
Peer-review started: May 18, 2016
First decision: July 27, 2016
Article in press: October 24, 2016
P- Reviewer: Friedman EA, Shrestha BM, Watanabe T S- Editor: Kong JX L- Editor: A E- Editor: Lu YJ
References
- 1.Lieske JC, Peña de la Vega LS, Slezak JM, Bergstralh EJ, Leibson CL, Ho KL, Gettman MT. Renal stone epidemiology in Rochester, Minnesota: an update. Kidney Int. 2006;69:760–764. doi: 10.1038/sj.ki.5000150. [DOI] [PubMed] [Google Scholar]
- 2.Sakhaee K. Nephrolithiasis as a systemic disorder. Curr Opin Nephrol Hypertens. 2008;17:304–309. doi: 10.1097/MNH.0b013e3282f8b34d. [DOI] [PubMed] [Google Scholar]
- 3.Rule AD, Lieske JC, Li X, Melton LJ, Krambeck AE, Bergstralh EJ. The ROKS nomogram for predicting a second symptomatic stone episode. J Am Soc Nephrol. 2014;25:2878–2886. doi: 10.1681/ASN.2013091011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cheungpasitporn W, Erickson SB, Rule AD, Enders F, Lieske JC. Short-Term Tolvaptan Increases Water Intake and Effectively Decreases Urinary Calcium Oxalate, Calcium Phosphate and Uric Acid Supersaturations. J Urol. 2016;195:1476–1481. doi: 10.1016/j.juro.2015.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goldfarb DS. Increasing prevalence of kidney stones in the United States. Kidney Int. 2003;63:1951–1952. doi: 10.1046/j.1523-1755.2003.00942.x. [DOI] [PubMed] [Google Scholar]
- 6.Long LO, Park S. Update on nephrolithiasis management. Minerva Urol Nefrol. 2007;59:317–325. [PubMed] [Google Scholar]
- 7.López M, Hoppe B. History, epidemiology and regional diversities of urolithiasis. Pediatr Nephrol. 2010;25:49–59. doi: 10.1007/s00467-008-0960-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stamatelou KK, Francis ME, Jones CA, Nyberg LM, Curhan GC. Time trends in reported prevalence of kidney stones in the United States: 1976-1994. Kidney Int. 2003;63:1817–1823. doi: 10.1046/j.1523-1755.2003.00917.x. [DOI] [PubMed] [Google Scholar]
- 9.Marangella M, Bruno M, Cosseddu D, Manganaro M, Tricerri A, Vitale C, Linari F. Prevalence of chronic renal insufficiency in the course of idiopathic recurrent calcium stone disease: risk factors and patterns of progression. Nephron. 1990;54:302–306. doi: 10.1159/000185884. [DOI] [PubMed] [Google Scholar]
- 10.Rule AD, Krambeck AE, Lieske JC. Chronic kidney disease in kidney stone formers. Clin J Am Soc Nephrol. 2011;6:2069–2075. doi: 10.2215/CJN.10651110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hippisley-Cox J, Coupland C. Predicting the risk of chronic Kidney Disease in men and women in England and Wales: prospective derivation and external validation of the QKidney Scores. BMC Fam Pract. 2010;11:49. doi: 10.1186/1471-2296-11-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cho DK, Zackson DA, Cheigh J, Stubenbord WT, Stenzel KH. Urinary calculi in renal transplant recipients. Transplantation. 1988;45:899–902. doi: 10.1097/00007890-198805000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Hayes JM, Streem SB, Graneto D, Hodge EE, Steinmuller DR, Novick AC. Renal transplant calculi. A reevaluation of risks and management. Transplantation. 1989;47:949–952. doi: 10.1097/00007890-198906000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Shoskes DA, Hanbury D, Cranston D, Morris PJ. Urological complications in 1,000 consecutive renal transplant recipients. J Urol. 1995;153:18–21. doi: 10.1097/00005392-199501000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Del Pizzo JJ, Jacobs SC, Sklar GN. Ureteroscopic evaluation in renal transplant recipients. J Endourol. 1998;12:135–138. doi: 10.1089/end.1998.12.135. [DOI] [PubMed] [Google Scholar]
- 16.Rhee BK, Bretan PN, Stoller ML. Urolithiasis in renal and combined pancreas/renal transplant recipients. J Urol. 1999;161:1458–1462. [PubMed] [Google Scholar]
- 17.El-Mekresh M, Osman Y, Ali-El-Dein B, El-Diasty T, Ghoneim MA. Urological complications after living-donor renal transplantation. BJU Int. 2001;87:295–306. [PubMed] [Google Scholar]
- 18.Kim H, Cheigh JS, Ham HW. Urinary stones following renal transplantation. Korean J Intern Med. 2001;16:118–122. doi: 10.3904/kjim.2001.16.2.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Klingler HC, Kramer G, Lodde M, Marberger M. Urolithiasis in allograft kidneys. Urology. 2002;59:344–348. doi: 10.1016/s0090-4295(01)01575-8. [DOI] [PubMed] [Google Scholar]
- 20.Doehn C, Fornara P, Tiemer C, Fricke L, Jocham D. Renal transplant lithiasis. Transplant Proc. 2002;34:2222–2223. doi: 10.1016/s0041-1345(02)03211-6. [DOI] [PubMed] [Google Scholar]
- 21.Streeter EH, Little DM, Cranston DW, Morris PJ. The urological complications of renal transplantation: a series of 1535 patients. BJU Int. 2002;90:627–634. doi: 10.1046/j.1464-410x.2002.03004.x. [DOI] [PubMed] [Google Scholar]
- 22.Abbott KC, Schenkman N, Swanson SJ, Agodoa LY. Hospitalized nephrolithiasis after renal transplantation in the United States. Am J Transplant. 2003;3:465–470. doi: 10.1034/j.1600-6143.2003.00080.x. [DOI] [PubMed] [Google Scholar]
- 23.Lipke M, Schulsinger D, Sheynkin Y, Frischer Z, Waltzer W. Endoscopic treatment of bladder calculi in post-renal transplant patients: a 10-year experience. J Endourol. 2004;18:787–790. doi: 10.1089/end.2004.18.787. [DOI] [PubMed] [Google Scholar]
- 24.Yiğit B, Aydin C, Titiz I, Berber I, Sinanoğlu O, Altaca G. Stone disease in kidney transplantation. Transplant Proc. 2004;36:187–189. doi: 10.1016/j.transproceed.2003.11.063. [DOI] [PubMed] [Google Scholar]
- 25.Challacombe B, Dasgupta P, Tiptaft R, Glass J, Koffman G, Goldsmith D, Khan MS. Multimodal management of urolithiasis in renal transplantation. BJU Int. 2005;96:385–389. doi: 10.1111/j.1464-410X.2005.05636.x. [DOI] [PubMed] [Google Scholar]
- 26.Ferreira Cassini M, Cologna AJ, Ferreira Andrade M, Lima GJ, Medeiros Albuquerque U, Pereira Martins AC, Tucci Junior S. Lithiasis in 1,313 kidney transplants: incidence, diagnosis, and management. Transplant Proc. 2012;44:2373–2375. doi: 10.1016/j.transproceed.2012.07.052. [DOI] [PubMed] [Google Scholar]
- 27.Stravodimos KG, Adamis S, Tyritzis S, Georgios Z, Constantinides CA. Renal transplant lithiasis: analysis of our series and review of the literature. J Endourol. 2012;26:38–44. doi: 10.1089/end.2011.0049. [DOI] [PubMed] [Google Scholar]
- 28.Mamarelis G, Vernadakis S, Moris D, Altanis N, Perdikouli M, Stravodimos K, Pappas P, Zavos G. Lithiasis of the renal allograft, a rare urological complication following renal transplantation: a single-center experience of 2,045 renal transplantations. Transplant Proc. 2014;46:3203–3205. doi: 10.1016/j.transproceed.2014.09.166. [DOI] [PubMed] [Google Scholar]
- 29.Rezaee-Zavareh MS, Ajudani R, Ramezani Binabaj M, Heydari F, Einollahi B. Kidney Allograft Stone after Kidney Transplantation and its Association with Graft Survival. Int J Organ Transplant Med. 2015;6:114–118. [PMC free article] [PubMed] [Google Scholar]
- 30.Rattiazzi LC, Simmons RL, Markland C, Casali R, Kjellstrand CM, Najarian JS. Calculi complicating renal transplantation into ileal conduits. Urology. 1975;5:29–31. doi: 10.1016/0090-4295(75)90296-4. [DOI] [PubMed] [Google Scholar]
- 31.Pena DR, Fennell RS, Iravani A, Neiberger RE, Richard GA. Renal calculi in pediatric renal transplant recipients. Child Nephrol Urol. 1990;10:58–60. [PubMed] [Google Scholar]
- 32.Lancina Martín JA, García Buitrón JM, Díaz Bermúdez J, Alvarez Castelo L, Duarte Novo J, Sánchez Merino JM, Rubial Moldes M, González Martín M. [Urinary lithiasis in transplanted kidney] Arch Esp Urol. 1997;50:141–150. [PubMed] [Google Scholar]
- 33.Narayana AS, Loening S, Culp DA. Kidney stones and renal transplantation. Urology. 1978;12:61–63. doi: 10.1016/0090-4295(78)90369-2. [DOI] [PubMed] [Google Scholar]
- 34.Rosenberg JC, Arnstein AR, Ing TS, Pierce JM, Rosenberg B, Silva Y, Walt AJ. Calculi complicating a renal transplant. Am J Surg. 1975;129:326–330. doi: 10.1016/0002-9610(75)90251-2. [DOI] [PubMed] [Google Scholar]
- 35.Solà R, del Río G, Villavicencio H. Staghorn renal stone in a transplanted kidney. Urol Int. 1990;45:188–189. doi: 10.1159/000281706. [DOI] [PubMed] [Google Scholar]
- 36.Benoit G, Blanchet P, Eschwege P, Jardin A, Charpentier B. Occurrence and treatment of kidney graft lithiasis in a series of 1500 patients. Clin Transplant. 1996;10:176–180. [PubMed] [Google Scholar]
- 37.Crook TJ, Keoghane SR. Renal transplant lithiasis: rare but time-consuming. BJU Int. 2005;95:931–933. doi: 10.1111/j.1464-410X.2005.05481.x. [DOI] [PubMed] [Google Scholar]
- 38.Harper JM, Samuell CT, Hallson PC, Wood SM, Mansell MA. Risk factors for calculus formation in patients with renal transplants. Br J Urol. 1994;74:147–150. doi: 10.1111/j.1464-410x.1994.tb16576.x. [DOI] [PubMed] [Google Scholar]
- 39.Khositseth S, Gillingham KJ, Cook ME, Chavers BM. Urolithiasis after kidney transplantation in pediatric recipients: a single center report. Transplantation. 2004;78:1319–1323. doi: 10.1097/01.tp.0000139543.56886.de. [DOI] [PubMed] [Google Scholar]
- 40.Cicerello E, Merlo F, Mangano M, Cova G, Maccatrozzo L. Urolithiasis in renal transplantation: diagnosis and management. Arch Ital Urol Androl. 2014;86:257–260. doi: 10.4081/aiua.2014.4.257. [DOI] [PubMed] [Google Scholar]
- 41.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 43.STROBE statement--checklist of items that should be included in reports of observational studies (STROBE initiative) Int J Public Health. 2008;53:3–4. doi: 10.1007/s00038-007-0239-9. [DOI] [PubMed] [Google Scholar]
- 44.Barendregt JJ, Doi SA. Wilston, Australia: EpiGear International Pty Ltd; 2010. MetaXL User Guide: Version 1.0. [Google Scholar]
- 45.DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials. 2007;28:105–114. doi: 10.1016/j.cct.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 46.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Easterbrook PJ, Berlin JA, Gopalan R, Matthews DR. Publication bias in clinical research. Lancet. 1991;337:867–872. doi: 10.1016/0140-6736(91)90201-y. [DOI] [PubMed] [Google Scholar]
- 48.Verrier C, Bessede T, Hajj P, Aoubid L, Eschwege P, Benoit G. Decrease in and management of urolithiasis after kidney transplantation. J Urol. 2012;187:1651–1655. doi: 10.1016/j.juro.2011.12.060. [DOI] [PubMed] [Google Scholar]
- 49.Lusenti T, Fiorini F, Barozzi L. Obstructive uropathy and acute renal failure due to ureteral calculus in renal graft: a case report. J Ultrasound. 2009;12:128–132. doi: 10.1016/j.jus.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gómez García I, Burgos Revilla FJ, Sanz Mayayo E, Rodríguez Patrón R, Arias Fúnez F, Marcen R, Pascual J, Escudero Barrilero A. [Acute obstructive kidney failure after kidney transplantation caused by calculi transfer from donor] Arch Esp Urol. 2003;56:1047–1050. [PubMed] [Google Scholar]
- 51.Qazi YA, Ali Y, Venuto RC. Donor calculi induced acute renal failure. Ren Fail. 2003;25:315–322. doi: 10.1081/jdi-120018733. [DOI] [PubMed] [Google Scholar]
- 52.Fabbian F, Catalano C, Rizzioli E, Normanno M, Conz PA. Acute renal failure due to a calculus obstructing a transplanted kidney. Nephron. 2002;91:742–743. doi: 10.1159/000065039. [DOI] [PubMed] [Google Scholar]
- 53.Flannigan R, Choy WH, Chew B, Lange D. Renal struvite stones--pathogenesis, microbiology, and management strategies. Nat Rev Urol. 2014;11:333–341. doi: 10.1038/nrurol.2014.99. [DOI] [PubMed] [Google Scholar]


