Abstract
Background:
Conventional computed tomography (CT) images are routinely used for diagnosing patellofemoral instability and are obtained with the patient in a supine position, nonweightbearing, with the knee in full extension, and with leg muscles relaxed. A new portable extremity cone beam CT (CBCT) scanner has been developed that may allow for more accurate diagnosis, as imaging can be performed with the patient standing, the knee flexed, and with leg muscles active.
Purpose/Hypothesis:
The purpose of this study was to compare CT measurements of patellar alignment on a prototype scanner versus conventional scanner in patients with known patellar instability. The hypothesis was that the measurements obtained with the knee flexed and the patient weightbearing would be less than those obtained from the conventional CT scan.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
Twenty patients with a diagnosis of lateral patellar instability were imaged on both a conventional CT scanner and on a prototype CBCT scanner. Objective measures of patellofemoral alignment (tilt angle, congruence angle, tibial tuberosity–trochlear groove [TT-TG] offset) were assessed on images obtained from the prototype and conventional CT scans by 2 independent reviewers. Paired t tests were calculated to compare the mean measurement of patellofemoral alignment obtained from the prototype versus conventional CT. Interrater reliability was assessed using a 2-way mixed-effects model intraclass correlation coefficient (ICC) for tilt angle, congruence angle, and TT-TG offset on the prototype and conventional CT scans.
Results:
Measurements of patellofemoral alignment were significantly less when acquired by the new prototype CBCT scanner while subjects were weightbearing on a flexed knee. On the images from the prototype CBCT scan, the tilt angle averaged 18.2° ± 11.6° compared with 28.1° ± 7.1° on the conventional CT scan (P < .0001). The congruence angle was 3.0° ± 30.1° compared with 26.7° ± 18.1° on the conventional CT scan (P = .0002). Finally, the TT-TG offset distance averaged 12.3 ± 6.3 mm when measured on the CBCT scan compared with 20.1 ± 4.2 mm on the conventional CT scan (P < .0001). Good interrater reliability was found for tilt angle, congruence angle, and TT-TG offset on conventional and CBCT scans (ICC range, 0.79-0.96).
Conclusion:
In patients with patellar instability, measurements of patellofemoral alignment are reduced on images obtained from a new weightbearing extremity CBCT scanner on a flexed knee versus conventional CT in the supine position with a fully extended knee. Improvement in objective measurements of patellar alignment should lead to improved clinical and surgical care of patients with this condition.
Keywords: Weightbearing, CT scan, patella, instability
Patellar instability is a common clinical problem in orthopaedics, but the etiology is multifactorial, the evaluation complex, and the treatment remains controversial. Predisposing anatomic factors have been reported by many and are considered as components during diagnosis and treatment.10,13,20 Current methods available for imaging of the patellofemoral alignment include conventional radiographs, magnetic resonance imaging (MRI), and computed tomography (CT) scanning. CT scans are particularly useful for evaluating bone detail and to objectively measure the degree of patellar tilt, patellar subluxation, and the distance between the tibial tubercle and the center of the trochlear groove (TT-TG offset).2,10 Among the limitations of this technology are that CT scans are typically acquired in a nonweightbearing supine position, with the patient’s knee at or near full extension and the muscles relaxed.18,26,31 Degree of knee flexion and activity of the quadriceps are known to influence patellar tracking on the trochlea, but these factors are removed when images are taken with the patient supine.5,12,25 Several authors have reported that on MRI, there is a constant and significant reduction in the TT-TG offset as the knee is imaged from 0° to 90°.11,15,18,22 To our knowledge, this is the first CT study to analyze the effect of simultaneous knee flexion angle and weightbearing in symptomatic patients in a single-leg stance and compared with conventional static measurements of patellar alignment.
A new extremity cone beam CT (CBCT) scanner (Carestream Health) has been developed to allow the acquisition of portable, weightbearing, 2- and 3-dimensional (3D) CT images of the leg and other extremities.7,28,33 The Generation-3 prototype is under review by the US Food and Drug Administration (FDA) as a 510K application and can image a patient’s knee while he or she is standing, weightbearing, and with the knee in a flexed position (Figure 1).
Figure 1.

Acquisition of images in the prototype cone beam computed tomography scanner with a patient weightbearing on a flexed knee. Image reprinted with permission from Carestream Health.
This new CT technology should provide for more functional measurements of patellofemoral alignment because this position is much more relevant and places the knee in the most vulnerable position for patellar instability.31 The purpose of this study was to compare several commonly used measurements of patellofemoral alignment (tilt angle, congruence angle, and TT-TG offset) on a conventional CT scanner to the same measurements on a new prototype extremity CBCT scanner. The primary hypothesis was that measurements of patellofemoral alignment obtained from the prototype CBCT scanner will be less than those obtained by the conventional CT scanner.
Methods
Sample Selection
Twenty-five patients were evaluated and screened by 5 fellowship-trained primary care and orthopaedic sports medicine physicians. For inclusion in the study, patients aged 16 years and older who were diagnosed with acute or chronic lateral patellar instability based on conventional history, physical examination, and radiographic imaging were considered eligible and invited to participate in this study. Patients were excluded if they had a history of previous surgery on the knee, a fracture of the patellofemoral joint, a concomitant knee ligament injury, had greater than Outerbridge grade 2 chondromalacia of the patellofemoral joint, were pregnant, or could not bear weight for the CBCT scan.19 One patient had a history of previous knee surgery, and 4 patients were not interested in participating, leaving a final sample size of 20 patients who consented to the study.
Data Collection
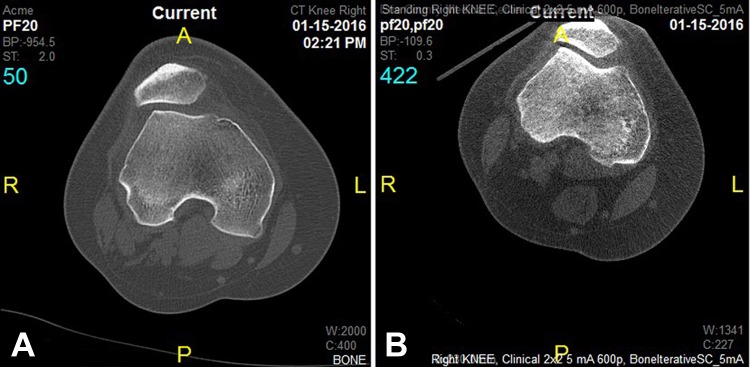
Demographic data (age, sex, race, height, weight) were extracted from patient medical records. Each patient attended 1 study visit at which time a routine conventional CT scan and an investigational prototype CT scan of their symptomatic knee was obtained by trained CT technicians at a single hospital. A conventional CT scan was acquired as part of standard of care to confirm the diagnosis, assess for etiological factors, and potentially to plan surgery. The conventional CT was performed on a Philips Brilliance 64 CT scanner (Koninklijke Philips) (rotation time, 1 s; acquisition, 128 × 0.6 mm; slice thickness, 2 × 2 mm; pitch, 0.8 mm; kV, 120-140; mA·s, 150-350; CT dose index [CTDI] (vol), 7.17-38 mGy; dose-length product [DLP], 230-1018 mGy·cm) with the patient supine, the knee in full extension, and with leg muscles relaxed. For study purposes, at baseline evaluation, the subject underwent a second CT scan of their affected knee with the prototype Generation-3 portable extremity CBCT scanner (slice thickness, 2 × 2 mm; radiation exposure, 5 mA 90 kV). The CBCT scan was obtained with the patient fully weightbearing on the involved extremity, leg muscles active, and with the knee flexed at 30° held by a fixed-angle goniometer secured to the patient by elastic wrap. The images were then reviewed on a reading station (GE PACS; GE Healthcare) by an experienced fellowship-trained musculoskeletal radiologist (rater 1) and an experienced sports fellowship–trained orthopaedic surgeon (rater 2). Representative images are shown in Figure 2.
Figure 2.
Images obtained with the (A) conventional computed tomography (CT) scan technique and (B) the cone beam CT scan technique.
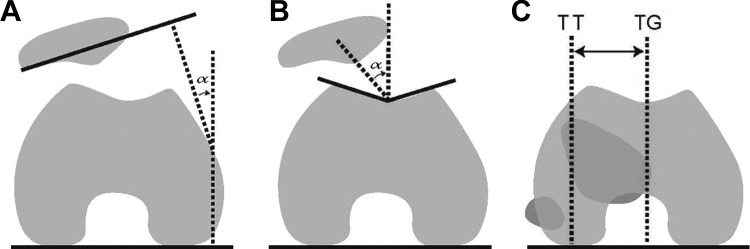
The tilt angle, congruence angle, and TT-TG offset distance were measured with the digital tools contained in the PACS viewing station, and as described in the literature and shown in Figure 3.10,17,20,21
Figure 3.
Schematic drawings of the methods used to measure (A) tilt angle, (B) congruence angle, and (C) tibial tuberosity–trochlear groove (TT-TG) offset distance on axial 2-dimensional computed tomography images.
The tilt angle is considered normal when it opens laterally and abnormal when the angle converges laterally by more than 20°.10 Merchant et al17 defined an abnormal congruence angle as more than 16° of lateral subluxation of the patella, found to be abnormal at the 95th percentile in 100 normal subjects. Many authors report 10 mm as normal for TT-TG offset in patients without any evidence of patellar instability.8,10,20 Dejour et al10 reported that a TT-TG distance of >20 mm is considered abnormal, and a 15- to 20-mm threshold is used by most as an indication for tibial tubercle transfer as a component of corrective surgery in symptomatic patients.8,11,16,20,30 Previous studies have documented excellent inter- and intrarater reliability for these types of measurements.16,18,22
Statistical Analyses
Descriptive statistics were computed for patient demographic factors including age, sex, race, weight (kg), height (m), body mass index (BMI; kg/m2), and symptomatic side. Descriptive statistics were also calculated for patellar measurements, including tilt angle, congruence angle, and TT-TG offset. Paired t tests stratified by rater were used to compare tilt angle, congruence angle, and TT-TG offset obtained from conventional versus cone beam CT scans. Interrater reliability was assessed using a 2-way mixed-effects model intraclass correlation coefficient (ICC) with corresponding 95% CI for tilt angle, congruence angle, and TT-TG offset on conventional and CBCT scans. Results were considered statistically significant when P < .05. Based on an expected correlation of at least 0.50 between the patellofemoral alignment measurements obtained from the conventional and prototype CT scanners, it was determined a priori that 20 patients were needed to obtain 80% power.29 SAS 9.4 (SAS Institute) was used for statistical analysis.
Results
Patient demographics are presented in Table 1. Mean age and BMI were 27.5 ± 10.5 years and 29.1 ± 6.4 kg/m2, respectively. The majority of the sample was female (60%), white (90%), and their right side were symptomatic (55%). Table 2 shows a comparison of patellar measurements on conventional CT versus CBCT, stratified by rater and by the average for both raters.
TABLE 1.
Patient Demographics (N = 20)a
| Age, y | 27.5 ± 10.5 |
| Sex | |
| Male | 8 (40) |
| Female | 12 (60) |
| Race | |
| White | 18 (90) |
| Black | 2 (10) |
| Weight, kgb | 84.7 ± 22.0 |
| Height, m | 1.7 ± 0.1 |
| Body mass index, kg/m2 b | 29.1 ± 6.4 |
| Symptomatic side | |
| Right | 11 (55) |
| Left | 9 (45) |
aData are reported as mean ± SD or n (%).
bOne patient’s weight was missing.
TABLE 2.
Comparison of Conventional CT Versus CBCT Patellar Measurements by Ratera
| Rater 1 | Rater 2 | Average for Both Raters | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Measurement | Conventional CT | CBCT | P Value | Conventional CT | CBCT | P Value | Conventional CT | CBCT | P Value |
| Tilt angle, deg | 28.0 ± 7.3 | 18.1 ± 12.3 | <.0001 | 28.2 ± 7.3 | 18.2 ± 11.3 | <.0001 | 28.1 ± 7.1 | 18.2 ± 11.6 | <.0001 |
| Congruence angle, deg | 22.8 ± 17.3 | 0.15 ± 31.1 | .001 | 30.7 ± 20.1 | 5.8 ± 30.8 | <.0001 | 26.7 ± 18.1 | 3.0 ± 30.1 | .0002 |
| TT-TG offset, mm | 21.4 ± 4.2 | 12.8 ± 6.3 | <.0001 | 18.9 ± 4.3 | 11.8 ± 7.6 | .001 | 20.1 ± 4.2 | 12.3 ± 6.3 | <.0001 |
aData are presented as mean ± SD. CBCT, cone beam computed tomography; CT, computed tomography; TT-TG, tibial tuberosity–trochlear groove.
For both raters, tilt angle, congruence angle, and TT-TG offset were statistically significantly decreased on cone beam versus conventional CT (P < .0001, P = .0002, and P < .0001, respectively). The interrater reliability is presented in Table 3. Good interrater reliability (ICC ≥ 0.79) was found for tilt angle, congruence angle, and TT-TG offset on conventional and CBCT scans. Intrarater reliability was not assessed.
TABLE 3.
Comparison of Conventional CT Versus CBCT Patellar Measurements Between Raters by Type of CTa
| Conventional CT | CBCT | |||||
|---|---|---|---|---|---|---|
| Measurement | Rater 1 | Rater 2 | P Value | Rater 1 | Rater 2 | P Value |
| Tilt angle, deg | 28.0 ± 7.3 | 28.2 ± 7.3 | .78 | 18.1 ± 12.3 | 18.2 ± 11.3 | .93 |
| Congruence angle, deg | 22.8 ± 17.3 | 30.7 ± 20.1 | .002 | 0.15 ± 31.1 | 5.8 ± 30.8 | .09 |
| TT-TG offset, mm | 21.4 ± 4.2 | 18.9 ± 4.3 | <.0001 | 12.8 ± 6.3 | 11.8 ± 7.6 | .46 |
aData are presented as mean ± SD. CBCT, cone beam computed tomography; CT, computed tomography; TT-TG, tibial tuberosity–trochlear groove.
Discussion
Conventional CT scanning is traditionally used to assess measures of patellofemoral alignment; however, imaging is performed with the patient in a supine position with the knee fully extended, which may not be the most clinically relevant way to acquire these measurements. A new prototype extremity CBCT scanner (Carestream Health) has been developed that allows for imaging of the patient in the weightbearing position with a flexed knee, potentially allowing for more functionally relevant measurement of patellofemoral alignment. The purpose of this study was to compare measures of patellofemoral alignment (tilt angle, congruence angle, and TT-TG offset) obtained from conventional versus prototype CT in patients diagnosed with acute or chronic patellar malalignment. Tilt angle, congruence angle, and TT-TG offset were decreased on images obtained from the prototype versus conventional CT scan.
Abnormalities in patellofemoral alignment measures, including tilt angle, congruence angle, and TT-TG offset, have been considered risk factors in patients who suffer from recurrent lateral patellar instability.2,10 Defined limits of normal for each of these measures are used by surgeons when planning corrective surgery on the patellofemoral joint.9,10,14,24 Our patient demographics are usual for a group of individuals with patellar instability, with a mean age of 27 years and a slight predilection toward female sex. Our patients had a mean tilt angle of 28°, congruence angle of 27°, and TT-TG offset distance of 20 mm when measured by traditional CT methods and verifies that our selection criteria identified a representative group of patients, that is, with radiographic confirmation of patellar instability.22,31
When imaged by a conventional CT scanning technique, the patient is relaxed, lying supine on the examination table with the knee fully extended. A potential problem with this standard method of imaging is the static nature of the imaging position in an otherwise dynamic articulation, which is affected by many forces during normal activities. A prototype CBCT scanner has been designed, with one of its unique capabilities that of being able to acquire images while the patient is standing, weightbearing, and in various positions of knee joint flexion.7,33 Since patellar instability occurs with the knee flexed and with the patient fully weightbearing, imaging in this position should produce a more “functional” representation of bone alignment. Our study shows that, in symptomatic patients, all 3 objective indices of patellofemoral alignment are significantly less than when images are acquired with the patient supine and nonweightbearing.
There is some controversy regarding whether MRI and CT measurements of patellar tilt, subluxation, and particularly, TT-TG offset are equivalent, but review of the literature reveals some studies conducted with MRI that are relevant to our results.1,6,11,15,18,20,22 Several authors have reported that with MRI there is a constant and significant reduction in the TT-TG offset as the knee is imaged from 0° to 90°.11,15,18,22 The investigation by Izadpanah et al15 is the only study that also looked at the effect of weightbearing on TT-TG offset when measured by a tilting magnet MRI. In their study, with weightbearing, the mean TT-TG offset was significantly less at both 0° and 30° of knee flexion compared with the lying position with the knee at 0° of flexion. Callaghan et al5 reported that MRIs acquired with the subject standing under natural loads exerted by body mass give a more valid view of patellofemoral alignment but noted no effect on patellar tilt. A study by Draper et al12 used real-time MRI to visualize the patellofemoral joint during dynamic knee extension from 30° to 0° during 2 conditions: upright weightbearing and supine nonweightbearing. Their results suggest that patellofemoral kinematics measured during supine, unloaded tasks do not accurately represent patellar motion during weightbearing activities. It should be noted that all of the above studies except 1 were performed on patients who were healthy, without evidence of patellofemoral alignment.22
In previous CT studies, the angle of flexion while the knee is being imaged has been shown to be a critical factor to consider when measuring the TT-TG distance.26,31 In the study by Tanaka et al,26 dynamic kinematic CT scans showed that the TT-TG offset distance increases linearly by 1 mm for every 5° of knee extension. Similarly, Williams et al31 showed that radiographic patellar tracking (ie, tilt, patellar offset, and TT-TG offset), as measured by dynamic CT scan, reveals alignment changes with knee motion and was most abnormal when the knee was in extension. In another related study, Miyanishi et al18 used rotational alignment measures other than TT-TG offset and showed that the extent of lateralization of the tibial tubercle was greater in full extension and that the change was greater in knees with patellar instability. While these studies evaluated measurements on patients who were symptomatic, the study by Williams et al31 did not measure at 0° or 30°, and that by Miyanishi et al18 did not measure TT-TG offset.
Most agree that the changes in TT-TG offset that occur with knee flexion angle are a result of the unlocking of the screw-home mechanism of the knee that occurs in early flexion and that this unlocking causes an obligatory internal rotation of the tibia in relation to the femur, and therefore, the tibial tuberosity in relation to the femoral trochlea.15,22 It seems straightforward that knee position would affect the measurement of TT-TG offset, yet no standard exists for positioning of patients for MRI or CT scan. If we pool available MRI and CT data from the literature and compare TT-TG distance obtained at full extension to knee flexion of 30° in symptomatic patients, the measurement decreases from a mean 18.6 mm to 13.3 mm, or 28%.22,26,31 If we apply the 28% reduction to our symptomatic group, TT-TG offset would be expected to decrease from 20.1 mm to 14.5 mm as an effect of knee flexion angle alone. Thus, there appears to be an additional effect from weightbearing and muscle activation of 2.2 mm, or 11%. The study by Seitlinger et al22 showed no statistically significant difference in the decrease in the TT-TG offset between symptomatic patients and healthy volunteers as a result of knee flexion. Our findings suggest that because the average nonweightbearing TT-TG distance in asymptomatic patients is 10 mm, in a normal population, the TT-TG offset distance would be approximately zero when obtained with the knee flexed and the patient weightbearing. This is intuitively reassuring, since a weightbearing TT-TG of zero would seem to effectively balance the major extensor mechanism forces across the patellofemoral joint. This is the focus of a current research project. Furthermore, for symptomatic patients, the amount of surgical correction by tibial tubercle transfer would be the exact TT-TG distance obtained when CT is acquired by the methods described here on the CBCT scanner, which would be an easy way to calculate the precise distance the tubercle needs to be transferred to centralize the patella.
In summary, a conventional CT scan, done in full extension and nonweightbearing, may overestimate the TT-TG offset and give inaccurate data to a surgeon contemplating realignment surgery. If surgery is performed, overestimation of the amount of patellar malalignment risks developing a complication from overcorrection, such as knee pain from abnormal joint loads and subsequent arthritis.23,27 For imaging of the knee joint, specifically the patellofemoral joint, the novel abilities of the prototype CBCT scanner may provide specific advantages over conventional CT.
Our study showed that the tilt angle and congruence angle are also affected by knee flexion angle and by the muscle action necessary for single-limb weightbearing, with the tilt angle decreasing 36% (28° to 18°) and the congruence angle decreasing 89% (27° to 3°) in our patients with lateral patellar instability. It is known that muscle forces, especially those of the vastus medialis obliquus, affect patellar position and likely affect measurement of patellar tilt and degree of subluxation, yet most scans are obtained without weightbearing and without quadriceps muscle activation.3,32 Few imaging studies have evaluated the effect of knee flexion angle and muscle forces on radiographic measurements of patellar tilt. The dynamic CT study by Tanaka et al26 showed a pattern of progressive decrease in patellar tilt as the knee was flexed, and this decrease correlated with changes in the TT-TG offset distance at all flexion angles. Brossmann et al4 evaluated patellofemoral joint motion from 30° of knee flexion to full extension using motion-triggered cine MRI as performed during active versus passive extension in 13 patients with confirmed patellar maltracking. They found statistically significant decreases in patellar tilt between active and passive knee extension in this group of patients. Possible causes of these effects are deepening of the trochlea distally and the effect of the quadriceps pull on the medial patellofemoral ligament and medial retinaculum.
One of the strengths of this study is that patients were imaged in a position that is functionally relevant, namely, single-leg stance on a knee flexed to 30°. This is a vulnerable position for patients predisposed to lateral patellar instability. Also, our study demonstrated good interrater reliability for all measurements of patellofemoral alignment on images obtained from conventional and prototype CT scan. One of the limitations of this study is that we looked at the influence of knee flexion and weightbearing on measurements of patellofemoral alignment in patients with a diagnosis of instability; therefore, we had no control group. We are currently enrolling healthy volunteers to be imaged per this study protocol to serve as a normal control. While other studies have shown similar influence in healthy subjects, there may be differences between the 2 groups. Some of our patients were imaged soon after a patellar instability episode, and we cannot guarantee that all patients bore full weight on the involved extremity during image acquisition. Because some instability episodes were acute, knee effusion may have been present and affected the position of the patella and therefore radiographic measurements of alignment. We also did not measure the amount of patella alta or trochlear dysplasia that may have existed in our patient group. These, as well as abnormality of femoral and tibial torsion, are factors well known to affect patellofemoral stability. Last, the muscle force used by our patients was only enough to maintain single-leg weightbearing for the duration of the CBCT, likely to have been far less than the force required for activities like running, decelerating, pivoting, and other higher energy activities where patellar instability is known to occur. We feel, however, that greater muscles forces would act to further decrease patellar tilt, congruence angle, and TT-TG distance in this situation.
Conclusion
A new extremity CBCT scanner allows for imaging while subjects are weightbearing on a flexed knee during image acquisition when the problem is that of patellar alignment. When CT is performed in this way, generally accepted measurements of patellar alignment in subjects with a clinical diagnosis of patellar instability are significantly less than those obtained on conventional CT scan.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This research was sponsored by Carestream Health via an agreement with the Research Foundation for the State of New York. J.M. and L.B. receive an unrestricted grant for research and education from Arthrex Inc.
Ethical approval for this study was obtained from the SUNY University at Buffalo Institutional Review Board (IRB #655951-3).
References
- 1. Anley CM, Morris GV, Saithna A, James SL, Snow M. Defining the role of the tibial tubercle-trochlear groove and tibial tubercle-posterior cruciate ligament distances in the work-up of patients with patellofemoral disorders. Am J Sports Med. 2015;43:1348–1353. [DOI] [PubMed] [Google Scholar]
- 2. Balcarek P, Oberthür S, Hopfensitz S, et al. Which patellae are likely to redislocate? Knee Surg Sports Traumatol Arthrosc. 2014;22:2308–2314. [DOI] [PubMed] [Google Scholar]
- 3. Biedert RM, Gruhl C. Axial computed tomography of the patellofemoral joint with and without quadriceps contraction. Arch Orthop Trauma Surg. 1997;116:77–82. [DOI] [PubMed] [Google Scholar]
- 4. Brossmann J, Muhle C, Schröder C, et al. Patellar tracking patterns during active and passive knee extension: evaluation with motion-triggered cine MR imaging. Radiology. 1993;187:205–212. [DOI] [PubMed] [Google Scholar]
- 5. Callaghan MJ, Guney H, Bailey D, et al. The effect of a patellar brace on patella position using weight bearing magnetic resonance imaging. Osteoarthritis Cartilage. 2014;22:S55. [DOI] [PubMed] [Google Scholar]
- 6. Camp CL, Stuart MJ, Krych AJ, et al. CT and MRI measurements of tibial tubercle-trochlear groove distances are not equivalent in patients with patellar instability. Am J Sports Med. 2013;41:1835–1840. [DOI] [PubMed] [Google Scholar]
- 7. Carrino JA, Al Muhit A, Zbijewski W, et al. Dedicated cone-beam CT system for extremity imaging. Radiology. 2014;270:816–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Colvin AC, West RV. Patellar instability. J Bone Joint Surg Am. 2008;90:2751–2762. [DOI] [PubMed] [Google Scholar]
- 9. Dejour D, Le Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc. 2007;15:39–46. [DOI] [PubMed] [Google Scholar]
- 10. Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19–26. [DOI] [PubMed] [Google Scholar]
- 11. Dietrich T, Betz M, Pfirrmann C, Koch P, Fucentese S. End-stage extension of the knee and its influence on tibial tuberosity–trochlear groove distance (TTTG) in asymptomatic volunteers. Knee Surg Sports Traumatol Arthrosc. 2014;22:214–218. [DOI] [PubMed] [Google Scholar]
- 12. Draper CE, Besier TF, Fredericson M, et al. Differences in patellofemoral kinematics between weight-bearing and non-weight-bearing conditions in patients with patellofemoral pain. J Orthop Res. 2011;29:312–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Escala JS, Mellado JM, Olona M, Gine J, Sauri A, Neyret P. Objective patellar instability: MR-based quantitative assessment of potentially associated anatomical features. Knee Surg Sports Traumatol Arthrosc. 2006;14:264–272. [DOI] [PubMed] [Google Scholar]
- 14. Goutallier D, Bernageau J, Lecudonnec B. The measurement of the tibial tuberosity. Patella groove distanced technique and results [in French]. Rev Chir Orthop Reparatrice Appar Mot. 1978;64:423–428. [PubMed] [Google Scholar]
- 15. Izadpanah K, Weitzel E, Vicari M, et al. Influence of knee flexion angle and weight bearing on the tibial tuberosity–trochlear groove (TTTG) distance for evaluation of patellofemoral alignment. Knee Surg Sports Traumatol Arthrosc. 2014;22:2655–2661. [DOI] [PubMed] [Google Scholar]
- 16. Koeter S, Horstmann WG, Wagenaar FC, Huysse W, Wymenga AB, Anderson PG. A new CT scan method for measuring the tibial tubercle trochlear groove distance in patellar instability. Knee. 2007;14:128–132. [DOI] [PubMed] [Google Scholar]
- 17. Merchant AC, Mercer RL, Jacobsen RH, Cool CR. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am. 1974;56:1391–1396. [PubMed] [Google Scholar]
- 18. Miyanishi K, Nagamine R, Murayama S, et al. Tibial tubercle malposition in patellar joint instability: a computed tomograpy study in full extension and at 30 degree flexion. Acta Orthop Scand. 2000;71:286–291. [DOI] [PubMed] [Google Scholar]
- 19. Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43:752–757. [DOI] [PubMed] [Google Scholar]
- 20. Schoettle PB, Zanetti M, Seifert B, Pfirrmann CWA, Fucentese SF, Romero J. The tibial tuberosity–trochlear groove distance; a comparative study between CT and MRI scanning. Knee. 2006;13:26–31. [DOI] [PubMed] [Google Scholar]
- 21. Schutzer SF, Ramsby GR, Fulkerson JP. The evaluation of patellofemoral pain using computerized tomography: a preliminary study. Clin Orthop Relat Res. 1986;204:288–293. [PubMed] [Google Scholar]
- 22. Seitlinger G, Scheurecker G, Högler R, Labey L, Innocenti B, Hofmann S. The position of the tibia tubercle in 0°-90° flexion: comparing patients with patella dislocation to healthy volunteers. Knee Surg Sports Traumatol Arthrosc. 2014;22:2396–2400. [DOI] [PubMed] [Google Scholar]
- 23. Shah JN, Howard JS, Flanigan DC, Brophy RH, Carey JL, Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40:1916–1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sherman SL, Erickson BJ, Cvetanovich GL, et al. Tibial tuberosity osteotomy: indications, techniques, and outcomes. Am J Sports Med. 2014;42:2006–2017. [DOI] [PubMed] [Google Scholar]
- 25. Tanaka M, Williams A, Elias J, Carrino J, Cosgarea A. Correlation between changes in TTTG distance and patellar position during active knee extension on dynamic kinematic CT imaging. Arthroscopy. 2014;30:e13–e14. [DOI] [PubMed] [Google Scholar]
- 26. Tanaka MJ, Elias JJ, Williams AA, Carrino JA, Cosgarea AJ. Correlation between changes in tibial tuberosity–trochlear groove distance and patellar position during active knee extension on dynamic kinematic computed tomographic imaging. Arthroscopy. 2015;31:1748–1755. [DOI] [PubMed] [Google Scholar]
- 27. Tompkins M, Arendt EA. Complications in patellofemoral surgery. Sports Med Arthrosc Rev. 2012;20:187–193. [DOI] [PubMed] [Google Scholar]
- 28. Tuominen EK, Kankare J, Koskinen SK, Mattila KT. Weight-bearing CT imaging of the lower extremity. AJR Am J Roentgenol. 2013;200:146–148. [DOI] [PubMed] [Google Scholar]
- 29. Walter SD, Eliasziw M, Donner A. Sample size and optimal designs for reliability studies. Stat Med. 1998;17:101–110. [DOI] [PubMed] [Google Scholar]
- 30. Weber AE, Nathani A, Dines JS, et al. An algorithmic approach to the management of recurrent lateral patellar dislocation. J Bone Joint Surg Am. 2016;98:417–427. [DOI] [PubMed] [Google Scholar]
- 31. Williams A, Elias J, Tanaka M, et al. Tibial tuberosity–trochlear groove distance and patellar tracking in symptomatic and asymptomatic knees in patients with unilateral patellofemoral instability. Arthroscopy. 2014;30:e15. [DOI] [PubMed] [Google Scholar]
- 32. Wunschel M, Leichtle U, Obloh C, Wulker N, Muller O. The effect of different quadriceps loading patterns on tibiofemoral joint kinematics and patellofemoral contact pressure during simulated partial weight-bearing knee flexion. Knee Surg Sports Traumatol Arthrosc. 2011;19:1099–1106. [DOI] [PubMed] [Google Scholar]
- 33. Zbijewski W, De Jean P, Prakash P, et al. A dedicated cone-beam CT system for musculoskeletal extremities imaging: design, optimization, and initial performance characterization. Med Phys. 2011;38:4700–4713. [DOI] [PMC free article] [PubMed] [Google Scholar]