Abstract
Background: Health literacy is thought to impact women's reproductive health, yet no comprehensive systematic reviews have been conducted on the topic. Our objective was to systematically identify, investigate, and summarize research on the relationship between health literacy and women's reproductive health knowledge, behaviors, and outcomes.
Methods: PRISMA guidelines were used to guide this review. English language, peer-reviewed research articles indexed in MEDLINE as of February 2015 were searched, along with study results posted on Clinicaltrials.gov. Articles were included if they (1) described original data-driven research conducted in developed countries, (2) were published in a peer-reviewed journal, (3) measured health literacy using a validated assessment, (4) reported on the relationship between health literacy and reproductive health outcomes, related knowledge, or behaviors, and (5) consisted of a study population that included reproductive age women.
Results: A total of 34 articles met eligibility criteria and were included in this review. Data were abstracted from articles by two study authors using a standardized form. Abstracted data were then reviewed and summarized in table format. Overall, health literacy was associated with reproductive health knowledge across a spectrum of topics. It was also related to certain health behaviors, such as prenatal vitamin use and breastfeeding. Its relationship with other reproductive behaviors and outcomes remains unclear.
Conclusions: Health literacy plays an important role in reproductive knowledge and may impact behaviors and outcomes. While further research is necessary, healthcare providers should utilize health literacy best practices now to promote high-quality care for patients.
Keywords: : health literacy, reproductive health, contraception, obstetrics, cancer screening, sexual behavior
Introduction
Health literacy is defined as the degree to which individuals have the “capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.”1 According to the Institute of Medicine, 90 million Americans have difficulty understanding and acting upon health information, which can negatively affect their health and well-being.1 Low, or inadequate, health literacy has been linked to numerous poor health outcomes, such as increased hospitalizations and emergency department use, poor overall health status, and higher mortality.2 Given the significant burden of low health literacy on the healthcare system, emphasis has been placed on identifying and addressing this modifiable risk factor to improve patient–provider interactions and health outcomes.
While many studies explore the relationship between health literacy and health outcomes, less attention has been focused specifically on the effects of health literacy on women's reproductive health. This is unfortunate as health literacy is likely to impact many facets of reproductive healthcare. Knowledge about contraception, safe sexual practices, healthy pregnancy and postpartum behaviors, and preventive care is important to keep women healthy and leading productive lives. Furthermore, as the demographic profile of women giving birth in the United States continues to evolve and include more women at greatest risk for limited health literacy, including non-English-speaking racial and ethnic minorities and low-income women, health literacy has been increasingly recognized as an important area of focus for women's reproductive health.3 As such, the American Congress of Obstetricians and Gynecologists (ACOG) released a Committee Opinion that highlighted the need for physicians to consider patients' health literacy skills for health promotion and clinical care activities.4
Despite a growing recognition of the importance of health literacy in reproductive health, no rigorous, systematic literature reviews have been conducted to date examining the relationship between health literacy and women's reproductive health behaviors and outcomes. Without a synthesis of the current body of research, it is difficult to understand the progress made to date and to identify gaps in research. The purpose of this study was therefore to systematically identify, investigate, and summarize research on the relationship between health literacy and reproductive health knowledge, behaviors, and outcomes in developed countries.
Materials and Methods
Sources
This systematic review was conducted according to PRISMA guidelines.5 To select articles, a search in MEDLINE was performed in February 2015 using the following terms as text words or MeSH terms: literacy OR health literacy OR numeracy OR health literacy [MeSH] AND reproduct* OR obstetric* OR gynecolog* OR maternal OR pregnan* OR contracept* OR prenatal OR postnatal OR postpartum OR preconception OR women's health OR women's health [MeSH] OR women's health services [MeSH]. A filter of English language articles only was added to the search. An additional search of studies with results posted on Clinicaltrials.gov was conducted using the search term “health literacy.”
Eligibility criteria
Articles were included in the review if they met the following eligibility criteria: (1) described original data-driven research, (2) were published in a peer-reviewed journal, (3) measured health literacy using a previously validated health literacy or numeracy assessment, (4) provided evidence on the relationship between health literacy and reproductive health outcomes or related knowledge or behaviors, and (5) consisted of a study population that included reproductive age women, defined as less than or equal to 45 years old, or included a broader age range, but focused on an issue common to reproductive age women. For the purpose of this review, reproductive health was considered to encompass any topic broadly related to obstetric and gynecological care, including (but not limited to) family planning, perinatal and postnatal care, sexual health, and screenings for gynecological cancers. Articles describing research conducted in developing countries were excluded as they generally examined the effects of illiteracy on reproductive outcomes; this was considered conceptually distinct from health literacy and therefore beyond the focus of this review. Developing countries were identified based on categorization by the U.S. Agency for International Development (USAID).6
Study selection
To select studies, one study author (M.V.) first conducted a title review of all articles, removing any that were ineligible for the review. Next, two study authors (M.V., S.C.B.) independently reviewed abstracts from remaining articles; only articles that were considered ineligible by both authors were eliminated. Last, all remaining articles underwent a full article review by two study authors. Any article receiving a discordant coding between the two authors was reviewed by a third author and a final determination of inclusion made by majority vote.
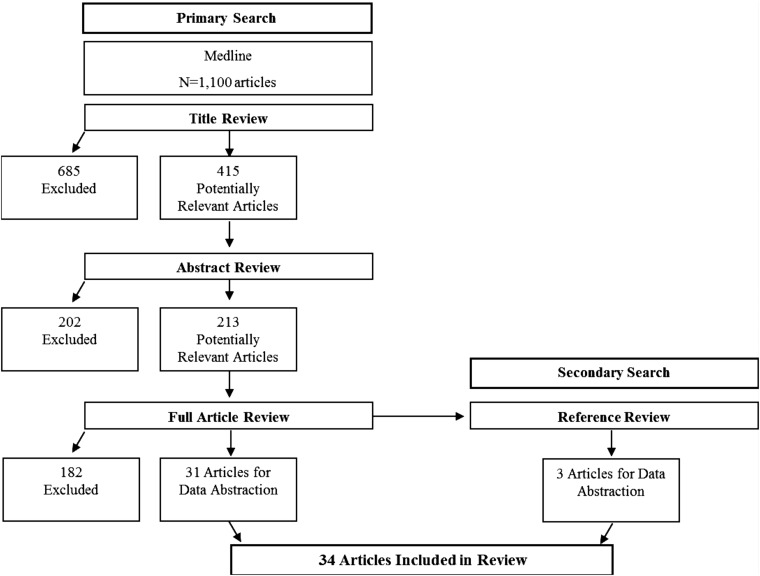
A secondary search was also performed to identify potentially eligible articles. Specifically, references for all articles that were selected for inclusion were hand-searched, along with those from commentaries and related systematic reviews identified during the primary search. Figure 1 describes the study selection process and the results from each stage of review.
FIG. 1.
Article search and review process.
Data abstraction, quality review, and analysis
Data were abstracted from selected articles by two study authors using a standardized form that captured information on study design, study population, measures utilized, and findings. Any coding discrepancies between the two authors were resolved through subsequent review. Abstracted data were then compiled, reviewed, and summarized in table format by one study author (K.K.).
Quality assessments were independently conducted for each article by two study authors. A modified version of guidelines published by the Agency for Healthcare Research and Quality (AHRQ) was used; these guidelines have been utilized in prior literature reviews conducted on health literacy and health outcomes.7–9 Specifically, reviewers were asked to consider each study in terms of its design, methodology and measurement, consideration for confounders, and use of appropriate statistical methods for analyses related to health literacy. Study quality was considered specifically within the context of our question of interest, that is, how health literacy relates to reproductive health-related knowledge, behaviors, and outcomes. Study findings were rated according to the AHRQ assessment definition of good (i.e., conclusions are very likely to be correct given degree of bias), fair (i.e., conclusions are probably correct given degree of bias), or poor (i.e., conclusions are not certain because bias is too large). Any rating discrepancies between the two study authors were resolved by a third reviewer. Quality ratings were then compiled, reviewed, and summarized in table format by one study author (K.K.) and reviewed by two authors (S.C.B., K.K.) for consistency across studies.
Results
A total of 1100 articles were returned from the primary search in MEDLINE (Fig. 1). After the title review, 415 articles remained. The abstract review eliminated 202 articles; a total of 213 abstracts were selected by one or both reviewers for full article review. After reviewing the 213 articles, 31 were selected for inclusion in the systematic review. Three additional articles were identified via reference mining procedures for a total of 34 articles. All articles included in the final review are summarized in Table 1. A total of 12 studies were identified by the search in Clinicaltrials.gov; however, none of the studies met eligibility criteria.
Table 1.
Summary of Articles Included in the Review
| Study | Design | Sample | Health literacy measure (% <adequate*) | Outcome (measure type) | Variables in adjusted analyses | Results | Quality rating |
|---|---|---|---|---|---|---|---|
| Family planning and fertility | |||||||
| Gazmararian et al.33 | Cross sectional |
N = 406 currently or recently pregnant women 19–45 years old Memphis, TN 73.2% Black; 23% White Recruited by random phone calls to Medicaid Managed Care beneficiaries |
Modified S-TOFHLA (9.6) | Contraceptive use and knowledge (questionnaire) | Age, race, and marital status | Health literacy had no association with on pregnancy intent and current use of contraception Use of LARC,† douching, and rhythm method associated with low health literacy compared with other forms of contraception Limited health literacy associated with less knowledge about timing of fertility and increased interest in obtaining more knowledge about family planning |
Fair |
| Davis et al.32 | Cross sectional |
N = 400 women 11–41 years old Louisiana 86% Black; 14% White Convenience sampling from family planning health clinic |
REALM (42) | Knowledge and correct use of oral contraceptive pills (questionnaire) | None | Low health literacy associated with decreased knowledge of the meaning, mechanism of action, and risks of oral contraception No association with correct oral contraceptive pill use or knowledge of side effects |
Poor |
| Gossett et al.30 | Cross sectional |
N = 300 women 20–50 years old Chicago, IL 47.7% Black; 33.7% White Recruited from university-based faculty and resident clinics |
REALM (13.9) | Knowledge of fertility, aging, and use of assisted reproductive technology (questionnaire) | Years of education, public insurance, previous pregnancy, and prior infertility treatment | High health literacy associated with greater knowledge about implications of aging on fertility and use of assisted reproductive technology in univariate and multivariate analyses Numeracy was not associated with the total knowledge score |
Fair |
| Yee et al.10 | Cross-sectional mixed methods |
N = 30 women, postpartum ≥18 years old Chicago, IL 63.3% Black; 36.7% Hispanic Convenience sample from academic clinic |
REALM-7 (50) | Contraception knowledge (qualitative interviews) | None | Low literacy and numeracy were associated with poor contraceptive knowledge and difficulty with contraceptive use No association with unplanned pregnancy or use of contraception at time of conception |
Poor |
| Raymond et al.34 | Cross sectional |
N = 663 women 12–50 years old 8 U.S. Cities‡ 24.6% Black; 51.4% White; 23.5% Hispanic Convenience sampling from malls and family planning clinics |
REALM (35.4) | Understanding of product labeling for OTC emergency contraceptive pill (questionnaire) | None | Low health literacy associated with being less likely to understand objectives of emergency contraception medication labeling; however, the majority of objectives (8 of 11) were understood by more than 80% of participants with low health literacy | Poor |
| Raymond et al.35 | Cross sectional |
N = 335 adolescents 12–17 years old Multiple U.S. cities Recruited from malls and family planning clinics |
REALM (42)§ | Understanding package labeling of emergency contraception | None | Low health literacy was associated with decreased understanding of indications for, timing of, and contraindications of taking emergency contraception | Poor |
| Sexual behavior, STIs, and cervical cancer screening | |||||||
| Fortenberry et al.25 | Cross sectional |
N = 1035 men and women (59% women) 12–55 years old Colorado, New York, Alabama, Indiana Recruited from clinics, community organizations, and street intercept |
REALM (35) | Screening for gonorrhea in past year (questionnaire) | Past suspicion of gonorrhea, self-inspection for gonorrhea, self-efficacy for care seeking, sex, age, education, recruitment site, health status, and insurance status | Adequate health literacy associated with an increased probability of having gonorrhea testing in the past year and decreased perception of risk of gonorrhea | Fair |
| Sharp et al.36 | Cross sectional |
N = 130 women ≥18 years old Chicago, IL 100% Black Convenience sample among patients presenting for colposcopy appointment from academic clinics and Planned Parenthood |
REALM (45) | Emotional response to abnormal pap testing and risk factors for abnormal pap testing (questionnaire, laboratory reports) | Education, knowing someone with cervical cancer, and past colposcopy | High health literacy associated with more risk factors for abnormal pap such as use of oral contraceptives and more lifetime sexual partners Low health literacy associated with greater parity and higher level of avoidance/distress related to abnormal pap results No association with time to follow-up colposcopy, history of STIs (excluding HPV), smoking, number of prior abnormal pap smears, or colposcopies |
Fair |
| Lindau et al.38 | Cross sectional |
N = 529 women ≥18 years old Chicago, IL 58% Black; 15% White; 18% Hispanic Convenience sampling from OBGYN and HIV university-based clinics |
REALM (40) | Knowledge about cervical cancer screening and follow-up; Physician perceptions of patient health literacy (questionnaire and medical record review) | Education, ethnicity, employment status, payor type, age | High health literacy associated with cervical cancer screening knowledge, care seeking, and follow-up Physicians overestimated patient health literacy 80% of the time |
Fair |
| Lindau et al.39 | Cross sectional |
N = 68 women ≥18 years old Chicago, IL 57.4% Black; 13.2% White; 23.5% Hispanic Sequential sampling of university-based Primary care and HIV OBGYN clinics |
REALM (35) | Adherence with follow-up after abnormal pap (questionnaire and medical record review) | Age, race, diagnosis of cancer or HIV, employment status, insurance status | Health literacy had no association with on-time follow-up or within 1 year of abnormal pap result There was no significant difference in the severity of abnormality by health literacy status |
Fair |
| Rutherford et al.20 | Cross sectional |
N = 505 women 16–35 years old Scotland, United Kingdom 100% White Convenience sample recruited from family planning clinics |
REALM (43.8) | Sexual health knowledge and behavior (questionnaire) | None | Low health literacy associated with earlier sexual debut, unprotected intercourse at first sexual encounter, and more sexual partners in the past 6 months Low health literacy associated with less knowledge of timing of fertility and STIs, but increased desire for more contraception knowledge No association with planned pregnancy, use of emergency contraception, and number of sexual partners in previous 4 weeks |
Poor |
| Needham et al.37 | Cross sectional |
N = 127 women 16–21 years old Texas 63.7% Black; 7.9% White; 25% Hispanic Convenience sampling from a reproductive health clinic |
REALM (37) | STI Knowledge and related behaviors (questionnaire) | Age, repeating a grade, ethnicity | Low health literacy was associated with greater difficulty understanding a Chlamydia educational brochure No difference by health literacy in reported sexual risk behaviors |
Poor |
| Pregnancy and postpartum | |||||||
| Arnold et al.44 | Cross sectional |
N = 600 pregnant women 12–45 years old Louisiana 49% Black; 51% White Convenience sampling in hospital obstetric clinics |
REALM (51.4) | Knowledge, attitudes, and use of tobacco during pregnancy; (questionnaire and urine cotinine levels) | Age, race, marital status, number of pregnancies, living with a smoker, and current smoking status | High health literacy associated with increased knowledge and concern about the health effects of smoking/secondhand smoke Health literacy was not predictive of self-reported, actual smoking practices |
Fair |
| Kaufman et al.45 | Cross Sectional |
N = 61 women, 2–12 months postpartum ≥18 years old Albuquerque, New Mexico 41% White; 39% Hispanic Recruited from public health clinic |
REALM (36) | Breastfeeding postpartum (questionnaire) | None | High health literacy was associated with exclusive breastfeeding at 2 months | Poor |
| Endres et al.24 | Cross sectional |
N = 74 pregnant women with pregestational diabetes Chicago, IL 19% Black; 55% White; 23% Hispanic English and Spanish speakers Convenience sample from university and community-based clinics |
S-TOFHLA (22) | Pregnancy preparedness (questionnaire and medical record review) | None | Low health literacy was associated with unplanned pregnancy, lack of preconception counseling, not taking preconception folic acid, and initiating prenatal care at a later gestational age Low health literacy was associated with hospitalization during pregnancy, higher birth weight, and babies categorized as large for gestational age No difference by health literacy status in hemoglobin A1c testing, preterm delivery, vaginal delivery, shoulder dystocia, or NICU admission rates. |
Poor |
| Bennett et al.11 | Cross-sectional mixed methods |
N = 202 women, immediately postpartum 15–42 years old Philadelphia, PA 100% Black Recruited from hospital-based obstetrics clinic |
REALM (16)‖ | Prenatal care (questionnaire, chart review, and qualitative data) | None | No difference by health literacy status in percentage of women with inadequate prenatal care utilization; rates of low birth weight babies, preterm delivery, or cesarean section; or in endorsed themes surrounding patient–provider communication concerns and desires during prenatal care | Poor |
| Bennett et al.23 | Cross sectional |
N = 99 pregnant women Philadelphia, PA 100% Hispanic Spanish speaking Recruited from hospital OBGYN clinic and community health centers |
S-TOFHLA (34) | Peripartum depression (CES-D) | Mexican nativity and marijuana use | Low health literacy associated with depression peripartum | Fair |
| Cho et al.43 | Cross sectional |
N = 101 pregnant women ≤40 years old Chicago, IL 57.4% Black; 11.9% White; 24.8% Hispanic recruited from hospital-based clinic |
REALM-7 (38) | Antenatal testing (questionnaire) | None | Low health literacy was associated with inadequate understanding of first and second trimester aneuploidy screening tests No difference by health literacy seen in acceptance of aneuploidy screening tests |
Poor |
| Shieh et al.42 | Cross sectional |
N = 143 pregnant, women ≥18 years old Midwest US 60.1% Black; 24.5% White; 7.7% Hispanic Convenience sampling from hospital-based prenatal clinic |
S-TOFHLA (14.7) | Pregnancy-related health information-seeking behaviors and barriers (questionnaire) | None | Low health literacy was associated with decreased knowledge of self-care in pregnancy Low health literacy was associated with less access to, and use of, the internet to obtain health information |
Poor |
| Weiss et al.15 | Cohort, longitudinal |
N = 138 women, immediately postpartum and at 6–10 weeks postpartum ≥18 years old Tuscon, AZ Recruited from academic hospital |
NVS (16.7)¶ | Postpartum depression (EPDS) | Prior history of depression, number of children living at home | Low health literacy was associated with postpartum depression (EPDS score ≥9) at 6–10 weeks postpartum in bivariate and multivariate analyses | Fair |
| You et al.46 | Cross sectional |
N = 110 pregnant women ≥18 years old; Illinois 59% Black; 5.5% White; 30% Hispanic Convenience sample recruited from a university clinic |
S-TOFHLA (9) | Knowledge of preeclampsia (questionnaire) | None | Women with adequate health literacy were more likely to score higher on a preeclampsia knowledge questionnaire No difference in ability to define preeclampsia by health literacy |
Poor |
| Shieh et al.31 | Cross sectional |
N = 143 pregnant women ≥18 years old Indiana 60.1% Black; 24.5% White; 7.7% Hispanic Convenience sampling from hospital-based prenatal clinic |
S-TOFHLA (not reported) | Pregnancy health information seeking (questionnaire) | Self-efficacy, fetal health locus of control, and nulliparity | Health literacy had no association with health information seeking Low health literacy was associated with the belief that health professionals were responsible for their baby's health |
Poor |
| Igarashi et al.22 | Cross sectional |
N = 804 women immediately postpartum Mean Age: 30 years Purposive sampling from 16 hospitals throughout Japan 29.4% of women were culturally diverse women (CDW) not originally from Japan |
REALM—Japanese version (not reported) | Quality of care during pregnancy, delivery, and postpartum (questionnaire) | Unclear | High Japanese health literacy, loneliness, and insufficient understanding were negatively associated with evaluations of maternity care quality Negative correlation between literacy level and respect in the pregnancy period and understanding in the delivery and postpartum period |
Fair |
| Duggan et al.21 | Cross sectional |
N = 404 pregnant women ≥18 years old Ireland 86% White; 13% Other |
REALM (15.3) | Beliefs about medication during pregnancy (questionnaire) | Age, education | Low health literacy associated with stronger beliefs regarding the harms of medicines as well as their overuse by providers | Fair |
| Ehrenthal et al.16 | Cohort, longitudinal |
N = 249 women with gestational diabetes and/or hypertension (N = 176 at 3 months) ≥18 years old 26.1% Black, 65.5% White Recruited from academic hospital in Delaware |
REALM-SF (8.9) | Health literacy and postpartum follow-up of medical comorbidities (questionnaire) | Not specified | Women with lower health literacy were less likely to complete follow-up testing for diabetes, but not lipid screening | Poor |
| Lupattelli et al.17 | Cross sectional |
N = 4999 pregnant women Multinational** 34.5% Western Europe; 32.5% Northern Europe; 20.9% Eastern Europe Internet based; recruited via banners and social networks |
Brief Health Literacy Screener (45.5) | Health literacy, beliefs about medication during pregnancy, and adherence (questionnaire) | Different geographic region, maternal age, education level, employment status, immigrant status, medication risk perception, and pregnancy-specific belief sum score | Low health literacy was associated with increased perception of risk and negative beliefs about medications during pregnancy High health literacy associated with use of over-the-counter and chronic medications during pregnancy Low health literacy associated with self-reported nonadherence to medication regimens in pregnancy |
Poor |
| Poorman et al.40 | Cross sectional |
N = 445 pregnant and postpartum women Atlanta, GA 92.3% Black Recruited from WIC programs |
NVS (72) | Perinatal behaviors (questionnaire) | Income, education | Low health literacy was associated with not taking a daily vitamin during pregnancy | Fair |
| Smedberg et al.19 | Cross sectional |
N = 8344 pregnant or postpartum women Multinationalπ 41.5% Western Europe; 35.6% Northern Europe; 22.9% Eastern Europe Internet based, recruited via banners and social networks |
Brief Health Literacy Screener (49.1) | Smoking in pregnancy (questionnaire) | Geographic region, maternal age, marital status, education, employment status, parity, planned pregnancy, and folic acid use | Low health literacy was associated with smoking during pregnancy Among women smoking during pregnancy, there was no difference in the amount of smoking in pregnancy by literacy status |
Poor |
| Hameen-Anttila et al.18 | Cross sectional |
N = 7092 Pregnant or postpartum women Multinational‡‡ Internet based, recruited via banners and social networks |
Brief Health Literacy Screener (44.9) | Medication use during pregnancy (questionnaire) | Age, parity, education, geographic region, taking medication for acute illness or chronic conditions, number of over-the-counter medications being used, and use of herbal medications | Low or medium health literacy was associated with needing more information about medication use in pregnancy | Poor |
| Intervention studies | |||||||
| Kakkilaya et al.12 | Randomized experiment |
N = 89 pregnant women ≥17 years old Louisiana Randomized by day of week to either counseling or counseling with the use of a visual aid 76% Black, 20% White Recruited from university hospital prenatal clinic |
REALM (59) | Knowledge regarding survival, disability, and care after very preterm birth (23 weeks) (questionnaire) | N/A | Health literacy was not predictive of change in knowledge scores related to survival and NICU stays after counseling intervention Low health literacy was associated with recall of fewer disabilities affecting very preterm infants |
Fair |
| You (2011)47 | Cross sectional |
N = 132 women 18–44 years old Secondary analysis Convenience sample of primary care patients in Chicago, IL, and Shreveport, LA 77.3% Black; 18.9% White |
REALM (57.6) | Understanding of three different types of prescription drug warning labels (questionnaire) | Age, race/ethnicity, education, and number of daily medications | Comprehension of a simplified text+icon label was higher than that of the simplified text or standard warning label. Health literacy was not predictive of comprehension of the enhanced text+icon label |
Fair |
| Boxell et al.48 | Pre–post study |
N = 451 women ≥18 years old United Kingdom 74.3% White Recruited from fundraising events and outreach events |
NVS (39) | Awareness and barriers to seeking care for gynecologic cancers (questionnaire) | Age, ethnicity, poverty level, and education | Among all women, reviewing the brochure improved awareness of ovarian and cervical cancer symptoms and reduced perceived barriers to care, but health literacy disparities remained for symptom awareness; no significant differences were found for perceived barriers | Fair |
| You et al.13 | Randomized controlled trial |
N = 120 pregnant women ≥18 years old Illinois 52% Black; 27.5% Hispanic; 10% White Recruited from a university clinic |
NVS (48.4) | Knowledge of preeclampsia (questionnaire) | None | Women viewing the patient-friendly preeclampsia tool were more knowledgeable about preeclampsia than those exposed to the ACOG pamphlet or no education at the initial assessment; this relationship did not remain at follow-up There were no differences in preeclampsia knowledge by health literacy among those who viewed the graphics-based tool |
Fair |
| Yee et al.14 | Randomized controlled trial |
N = 150 pregnant women >18 years old Chicago, IL 53.3% Black, 7.3% White, 28.0% Hispanic Recruited from a university clinic |
REALM (43.3) | Understanding of antenatal testing (questionnaire) | Electronic health literacy, prior genetic counseling, and education level | Women receiving the interactive tool had greater knowledge about antenatal testing at initial and follow-up interviews in comparison with those receiving standard care Health literacy not associated with improvement in knowledge after use of educational tool |
Good |
Adequate health literacy varies by measure used. For the purpose of this column, the definition of adequate health literacy is defined as follows and everything else was considered less than adequate: REALM: ≥9th-grade reading level (score of >60); REALM-7 or REALM-SF: seven questions correct; S-TOFHLA: score of >30 points or adequate; NVS: score of ≥4; SBSQ: score of 10–12 or high. Any variations will be documented in these footnotes.
LARC, long-acting reversible contraception, including IUD and levonorgestrel implant.
Denver, CO; Los Angeles, CA; Chicago, IL; San Antonio, TX; Philadelphia, PA; Miami, FL; Phoenix, AZ; Washington, DC.
Less than adequate health literacy in this study measured as <8th-grade reading level.
Less than adequate health literacy in this study measured as <7th-grade reading level.
Less than adequate health literacy in this study measured as NVS score of <3.
Australia, Austria, Canada, Croatia, Finland, France, Iceland, Italy, the Netherlands, Norway, Poland, Russia, Serbia, Slovenia, Sweden, Switzerland, United Kingdom, and United States.
Austria, Croatia, Finland, France, Iceland, Italy, the Netherlands, Norway, Poland, Russia, Serbia, Slovenia, Sweden, Switzerland, and the United Kingdom.
Canada, United States, South America, Australia, Croatia, Poland, Russia, Serbia, Slovenia, Finland, Iceland, Norway, Sweden, Austria, France, Italy, the Netherlands, Switzerland, and the United Kingdom.
ACOG, American Congress of Obstetricians and Gynecologists; CES-D, Center for Epidemiologic Studies–Depression Scale; EPDS, Edinburgh Postnatal Depression Scale; HPV, human papillomavirus; IUD, intrauterine device; NICU, neonatal intensive care unit; NVS, Newest Vital Sign; OTC, over-the-counter; REALM, Rapid Estimate of Adult Literacy in Medicine; SBSQ, Set of Brief Screening Questions; STI, sexually transmitted infection; S-TOFHLA, Short Test of Functional Health Literacy in Adults.
Twenty-nine (85%) of the 34 studies included were observational or cross sectional in design, with 2 studies10,11 utilizing a mixed methods design that combined qualitative focus groups with cross-sectional observational data (Table 1). There were three experimental studies that included patient randomization12–14; these studies evaluated the effects of an educational tool on knowledge of a reproductive health topic using hypothetical scenarios. Last, two longitudinal cohort studies examined health outcomes in the postpartum period.15,16
Overall, one of the included studies was given the highest quality rating of good and the rest were considered fair quality (n = 16) or poor quality (n = 17) due to suboptimal (e.g., cross-sectional) study designs, unadjusted analyses, and/or potential for bias (Table 1). It is important to note that for many studies, examining the relationship between health literacy and reproductive knowledge, behaviors, or outcomes was not the primary purpose. Therefore, authors only reported results from bivariate or unadjusted analyses for these variables, which reduced their quality rating.
Twenty-eight (82%) of the 34 studies included in the review were conducted exclusively in the United States. Of the six remaining studies, three were large, internet-based multinational studies,17–19 two were conducted in the United Kingdom,20,21 and one in Japan.22 Study samples ranged from less than 100 participants (5 total studies, the smallest consisting of 30 participants) to 8344 participants for one of the internet-based multinational studies. The majority of studies enrolled low-income women seen at university-based clinics or hospitals. Almost all included English-speaking participants only, although one study enrolled exclusively Spanish-speaking participants,23 one enrolled both Spanish- and English-speaking participants,24 and one Japanese study22 and three large, internet-based multinational studies17–19 enrolled participants in several different languages. All but one study25 had a study population that was exclusively female; most were focused on adult women.
Health literacy measurement varied across studies. Twenty-one (62%) of the 34 studies used either the original, the short form, or a translated version of the Rapid Estimate of Adult Literacy in Medicine (REALM)26 to assess patient literacy skills, while 6 studies used the Short Test of Functional Health Literacy in Adults (S-TOFHLA),27 4 studies used the Newest Vital Sign (NVS),28 and 3 studies used the Set of Brief Screening Questions (SBSQ).29 A description of these measures and how they are commonly scored is provided in Table 2. Finally, two studies used numeracy scales, in addition to one of the health literacy measures already mentioned.10,30 Two studies22,31 did not report the percentage of their sample with low health literacy.
Table 2.
Description of Commonly Used Health Literacy Measures Across Studies
| Measure | Description | Scoring |
|---|---|---|
| REALM26,a | Consists of a listing of 66 medical words that are read out loud and increase in complexity. A point is assigned to each word pronounced correctly. | Total points: 66 |
| Points are assigned to reading level: 0–18 points is 3rd grade or less; 19–44 points is 4th–6th grade; 45–60 points is 7th–8th grade; and 61–66 points is 9th grade and above | ||
| S-TOFHLA27 | This test includes reading and numeracy sections, although some chose to measure only reading. The reading portion includes two medical text passages with dropped words through the text. Participants are asked to fill in the blanks from a choice of four words. The numeracy section asks patients to respond to questions and/or prompts that require interpreting numbers. | Total points: 100 |
| 0–53 is inadequate health literacy; 54–66 is marginal health literacy; and 67–100 is adequate health literacy | ||
| NVS28 | This test consists of 6 questions that require interpreting a nutrition label for a container of ice cream. The first four questions require numeracy skills and the last two require reading comprehension. | Total points: 6 |
| 0–1 suggests high likelihood of limited health literacy; 2–3 suggests possible limited health literacy; and 4–6 suggests adequate health literacy | ||
| SBSQ29 | This screen consists of three questions: (1) How often do you have someone help you read hospital materials? (2) How confident are you filling out medical forms by yourself? (3) How often do you have problems learning about your medical condition because of difficulty understanding written information? Each response is scored from 0 to 4. | Total points: 12 |
| 0–5 is low health literacy; 6–9 is medium health literacy; and 10–12 is high health literacy |
A shortened version of the REALM (REALM-SF) was used in some studies included in this review, as well as versions in different domains (i.e., genetics) and languages (i.e., Japanese).
Outcome measurement in the studies varied considerably. The majority of studies used questionnaires or self-report to obtain information about outcomes. Medical record review was used to determine episodes of screening, follow-up after abnormal testing, obstetric outcomes, and adequacy of prenatal care. Studies were grouped broadly according to topic area and are summarized below.
Family planning and fertility
Knowledge related to contraception and fertility
Consistently, studies demonstrated that health literacy was associated with knowledge about contraception. Davis et al. examined whether knowledge regarding oral contraceptive pills was associated with health literacy among low-income women attending a family planning clinic in Louisiana.32 After viewing a standard video shown to women interested in obtaining contraception, low health literacy was associated with less knowledge regarding the meaning, mechanism of action, and risks of oral contraception. Twenty-three percent of women with a sixth-grade reading level or below could identify the purpose of contraception, compared with 54% of women with seventh- to eighth-grade reading level, or 74% of women with a ninth-grade reading level or higher (p < 0.0001).32
Similarly, two other studies found that women with low health literacy were less likely to know the time in their menstrual cycle when they were able to get pregnant. In a group of women in the United Kingdom, Rutherford et al. found that 61.5% of women with a seventh- to eighth-grade reading level knew the time in the menstrual cycle when a woman was able to get pregnant compared with 85.6% of women with a reading level equivalent to ninth grade or above (p < 0.001).20 Similarly, Gazmararian et al. found that women with low health literacy had four times the odds of not knowing when a woman could get pregnant during her menstrual cycle (odds ratio [OR] 4.54, 95% confidence interval [CI] 2.18–9.48).33 In regard to fertility and aging, Gossett et al. found that higher health literacy was associated with increased knowledge of how aging affects fertility and the need for assisted reproductive technology.30
In terms of understanding how to use contraception, Yee et al. found that women with low health literacy were more likely to identify inadequate knowledge as a barrier to taking contraception correctly.10 Two studies by Raymond et al. similarly found that low health literacy was associated with less knowledge regarding the indication for use of emergency contraception after viewing a prototype drug information label.34,35 However, in their 2002 study, Raymond et al. found that overall knowledge and understanding of the use of emergency contraception was high, with over 80% of all participants understanding 8 of 11 objectives tested.
Contraceptive use and planned pregnancies
Regarding actual contraceptive use, no relationship was found between health literacy status and use of contraception. Gazmararian et al. found no association between health literacy and report of current use of contraception,33 Rutherford et al. found that the rate of emergency contraception use was not associated with health literacy,20 and Davis et al. found no difference in correct use of contraception by health literacy in women currently using oral contraceptive pills.32 Gazmararian et al. also examined contraception choice. When asked about birth control method ever used in the past, a higher proportion of women with low health literacy were found among users of both long-term highly efficacious forms of birth control, such as an intrauterine device (17.9%) or implant (13.3%), and the less efficacious forms, such as douching (13.9%) or the rhythm method (13.7%), compared with the proportion reporting use of other methods such as the diaphragm (10.3%), medroxyprogesterone acetate (10.1%), or oral contraceptive pills (8.1%).33
There were inconsistent results regarding rates of planned pregnancy by health literacy, although almost all studies on this topic were considered of poor quality; only one was rated as fair.33 Endres et al. found that women with low health literacy were more likely to have an unplanned pregnancy compared with women with adequate health literacy (75% vs. 40%, p = 0.02).24 Lupattelli et al. similarly reported a difference in incidence of unplanned pregnancy by health literacy status. In their multinational cohort, 12.0%, 9.8%, and 8.2% of women with low, medium, and high health literacy, respectively, reported unplanned pregnancies (p < 0.05).17 Several others, however, found no difference in rate of reported unplanned pregnancy by health literacy.10,20,33
Sexual behavior, sexually transmitted infections, and cervical cancer screening
Sexual behavior and sexually transmitted infections
Four studies examined the relationship between health literacy and sexual behavior and sexually transmitted infections (STIs) and found conflicting results. Two studies were considered of fair quality and two of poor quality; there were no systematic differences in findings between studies by their quality ratings. In evaluating sexual behavior that puts women at risk of STIs, Rutherford et al. found a statistically significant, but clinically narrow, difference in onset of sexual activity by health literacy status. Women with low health literacy had a reported mean age at first intercourse of 15.5 years compared with a mean age of 15.8 years in women with high health literacy (p < 0.001).20 Women with low health literacy compared with women with high health literacy were also more likely to report unprotected intercourse with their first sexual encounter (16.3% compared with 10.2%, p < 0.05) and two or more sexual partners in the last 6 months (19% compared with 9.5%, p < 0.002).20
Conversely, Sharp et al. found that high health literacy was associated with sexual behaviors that are risk factors for abnormal pap smears (1.8 risk factors in the low health literacy group compared with 2.3 risk factors in the high health literacy group), including the use of oral contraceptive pills, a higher reported number of lifetime sexual partners, and reported initiation of sexual activity before the age of 18 years.36 A greater percentage of women with high health literacy reported more than five lifetime sexual partners compared with women with low health literacy (51.4% vs. 25.9%, p < 0.01). Forty-three percent of women with low health literacy reported four to five lifetime partners.36 There was no association between health literacy skills and age of sexual debut or history of prior STIs.36 Needham et al. found no association between health literacy and report of risk factors for STIs, including age at first intercourse, number of lifetime sexual partners, history of previous sexually transmitted illness, and use of barrier protection with last episode of intercourse.37
Rutherford et al. and Needham et al. found no differences in knowledge regarding safe sexual practices by health literacy status.20,37 However, Rutherford et al. found that women with low health literacy were less likely to know how STIs could be passed from one individual to another; they were also less likely to know how to look for and identify signs of an STI.20 In a separate study, women and men with low health literacy were more likely to perceive themselves at risk for acquiring gonorrhea, but were less likely to have obtained testing for gonorrhea in the past year.25 Women with low health literacy were also more likely to report being interested in learning more about sexual health.20
Cervical cancer screening
Three studies examined the relationship between cervical cancer screening and health literacy; all were considered of fair quality. Sharp et al. reported that the proportion of women with a prior abnormal pap smear and history of colposcopy did not vary by health literacy status. There was also no difference in severity of pap abnormalities on screening found during this study by health literacy status.36 However, women with low health literacy were less likely to follow-up after receiving abnormal pap results and were more likely to report significant distress related to the diagnosis of an abnormal pap smear.36
Lindau et al. similarly found an association with health literacy and follow-up of abnormal pap smears. Women with low health literacy compared with those with adequate health literacy were more likely to say they would not follow-up with a provider after abnormal pap smear testing (30% compared with 19%, p < 0.036). Instead they would worry, panic, do nothing, or not know what to do.38 Women with high health literacy had twice the odds of understanding the purpose of a pap smear as a screening test compared with women with inadequate health literacy (OR 2.25, 95% CI 1.05–4.80).38
A follow-up study designed to investigate this relationship further, however, found no association between health literacy and follow-up within 1 year for abnormal pap results.39 Additionally, although there were no statistically significant differences in severity of pap results by health literacy, trend data suggested a relationship. Among women with abnormal pap smears and inadequate health literacy, 29% had results that showed low-grade squamous intraepithelial lesions (LGSILs) and 55% had atypical squamous cells of unknown significance (ASCUS). Among women with abnormal pap smears and adequate health literacy, 50% had LGSIL results and 25% had ASCUS on pap smear testing.39 This was likely not statistically significant due to a small study sample size.
Pregnancy and postpartum outcomes
Prenatal care utilization and quality
Data are inconsistent as to whether there are differences in prenatal care by patient health literacy. While the quality ratings for these studies varied, there were no systematic differences in terms of findings by quality. Endres et al. evaluated prenatal care utilization among women with high-risk pregnancies due to pregestational diabetes.24 Results indicated that women with low health literacy compared with women with adequate health literacy were less likely to have received preconception counseling with an obstetric provider (13% vs. 43%, p = 0.01) and were more likely to initiate prenatal care at a later gestational age (12.8 weeks vs. 8.3 weeks, p = 0.04).24 In unadjusted analysis, Poorman et al. found that an increased proportion of women with limited health literacy reported missed prenatal care appointments compared with women with marginal and adequate health literacy (16.8% vs. 6.9% vs. 2.1%, respectively, p = 0.03).40 After controlling for income and education, this association was no longer significant.
In contrast, Bennett et al. reviewed medical records from a cohort of 202 postpartum African American women and found no difference by health literacy status in gestational age at initiation of prenatal care. Overall rates of delayed prenatal care in this sample were high, however, with 61% of women in this study initiating prenatal care after the first trimester.11 This study also did not find an association between health literacy status and adequacy of prenatal care as measured by the Adequacy of Prenatal Care Utilization Index (APNCU), a measure that combines gestational age at initiation of prenatal care and number of visits attended.41 Fifty-eight percent of women with low health literacy had inadequate prenatal care by the APNCU compared with 49% of women with high health literacy (p = 0.341).11
In several studies, perceptions of prenatal care and care quality differed by health literacy categorization. Shieh et al. reported that women with low health literacy were less likely to believe that they could have an impact on their pregnancy's outcome, instead perceiving the healthcare provider to be in control of maternal and fetal outcomes.42 A study conducted in Japan explored the relationship of health literacy among culturally diverse women and its association with reported quality of prenatal care. High health literacy was associated with less understanding, less perceived respect by the healthcare provider, and increased loneliness during and after pregnancy.22 Finally, Bennett et al. conducted four focus groups with women who had low and high health literacy skills. Regardless of health literacy status, the theme of communication and partnership between provider and patient was consistent among all focus groups. Participants agreed that it was important that providers provide information in a way that was clear and accessible. Other themes that emerged included desire for trust, continuity of care, and a close patient–physician relationship.11
Cho et al. found lower levels of understanding of aneuploidy screening options among women with limited health literacy. Pregnant women with low health literacy skills had lower average scores on the Maternal Serum Screening Knowledge (MSSK) Questionnaire compared with women with high health literacy (5.5 vs. 6.96, p < 0.01) and were more likely to have inadequate knowledge as determined by a composite MSSK score (97.3% vs. 11.1%, p < 0.01). Despite this, there was no difference by health literacy group in the rate of acceptance of first or second trimester serum screening.43
Health information seeking during pregnancy was examined in two studies by Shieh et al. One study found no difference by health literacy status in broad practices related to media that women used to obtain health information during pregnancy, including books, brochures, TV, and the internet.31 However, in a separate study, Shieh et al. found that women with low health literacy were less likely to use the internet as a source of information. Compared with women with high health literacy, pregnant women with low health literacy had less access to the internet, and among women who did have access, those with low health literacy skills were less frequent users of the internet for prenatal care information.42 Studies did not differ in terms of their quality assessment.
Prenatal medication and supplement beliefs and use
Low health literacy was associated with not taking vitamin supplements during pregnancy. Endres et al. found a lower proportion of women with low health literacy compared with women with adequate health literacy who took folic acid before pregnancy and into the first trimester (31% compared with 83% p = 0.001).24 Poorman et al. found that women with low health literacy had greater odds of not taking a prenatal vitamin during pregnancy (adjusted OR 3.6, 95% CI 1.6–8.5) in comparison with those with adequate health literacy.40
Pregnant women with low health literacy were also more likely to attribute risk to medication use in pregnancy.17,21 In Ireland, Duggan et al. demonstrated that women with low health literacy had stronger beliefs regarding the harms of medication and that medications are overused in pregnancy compared with women with high health literacy.21 In a large multinational study, Lupattelli et al. showed increased perception of risk and negative beliefs about medications and supplements in pregnancy, including herbal remedies, among women with low health literacy.17 Furthermore, these negative beliefs and perceived risks appeared to mediate the increased rate of nonadherence to medications in pregnancy reported by women with low health literacy compared with medium health literacy and high health literacy (25%, 22.5%, and 19.2%, respectively).17 In the same cohort of women, Hameen-Anttila et al. reported that women with limited health literacy skills desired greater information regarding medication use in pregnancy in comparison with women with adequate health literacy skills.18
Smoking and pregnancy
It is unclear if health literacy status impacts smoking practices in pregnancy. Arnold et al. found that high health literacy was associated with increased knowledge and concern regarding smoking and its effects on pregnancy and children in the home.44 Despite this, there was a nonsignificant trend toward a greater proportion of women with high health literacy smoking during pregnancy. Fifteen percent of women reading at or below a third-grade reading level compared with 14% reading at a fourth- to sixth-grade level, 18% of women reading at a seventh- to eighth-grade level, and 25% of women with a greater than ninth-grade reading level reported smoking during pregnancy.44
Conversely, Smedberg et al. found that low health literacy was associated with a higher proportion of smoking during pregnancy. Among women who did smoke during pregnancy, there was no difference in the amount of smoking based on health literacy status.19 Poorman et al., in unadjusted analysis, found that women with inadequate health literacy reported higher rates of smoking during pregnancy compared with women with marginal and adequate health literacy (19.8%, 15.8%, and 8.8%, respectively, p < 0.01). This difference was not significant after adjusting for income and education.40 The studies by Poorman and Arnold were considered of fair quality, while the Smedberg article was rated as poor.
Obstetric and postpartum outcomes
The effect of health literacy on obstetric outcomes has not been thoroughly evaluated. In a cohort of high-risk obstetric patients with pregestational diabetes, Endres et al. found that women with low health literacy had more frequent hospitalizations and higher birth weight babies.24 Babies of women with pregestational diabetes and low health literacy weighed ∼450 g more than babies of mothers with adequate health literacy (p = 0.001).24 However, there were no differences in other maternal and neonatal outcomes such as gestational age at delivery, percentage of women who delivered vaginally, rates of shoulder dystocia, APGAR scores, or neonatal intensive care unit admissions. Bennett et al. found no association between health literacy and obstetric outcomes, including low birth weight, preterm delivery, and cesarean section.11
Women with low health literacy were more likely to suffer from depression during pregnancy23 and at 6 weeks postpartum.15 In a cohort of pregnant Latina women, those with inadequate health literacy compared with women with adequate health literacy had twice the odds of suffering from depression during pregnancy (OR 2.39, 95% CI 1.07–5.35).23 In a separate postpartum cohort, a larger proportion of women with low health literacy met criteria for postpartum depression compared with women with high health literacy (26.1% vs. 8.8%).15 After adjusting for history of depression and number of children at home, postpartum women with low health literacy had 3.45 greater odds (95% CI 1.1–11.8) of suffering from postpartum depression compared with women with high health literacy.15
Postpartum practices were shown to vary by health literacy status across multiple studies. Health literacy was negatively associated with breastfeeding rates. Kaufman et al. found that women with low health literacy were less likely than those with adequate health literacy to report exclusively breastfeeding their infants at 2 months postpartum (23% compared with 54%, p = 0.018).45 Poorman et al. found that 30% of women with less than adequate health literacy never breastfed compared with 13% of women with adequate health literacy.45 Finally, Ehrenthal et al. found that diabetic women with low health literacy were less likely to follow-up for glucose testing postpartum.16
Interventions to improve understanding of reproductive health information
A number of studies tested interventions designed to reduce literacy-related disparities in understanding reproductive health information. Using a computer-based tool to improve prenatal screening knowledge, Yee et al. found improved patient understanding of screening methods after viewing the tool. The level of knowledge improvement did not differ by health literacy.14
Similarly, You et al. developed an educational tool with text and icons to improve preeclampsia knowledge.13 A previous study by this team found no difference in preeclampsia knowledge by health literacy in adjusted analysis, although knowledge about preeclampsia among all women in the study sample was low, with only 13% of participants able to identify signs and symptoms of this condition.46 The educational tool was shown to improve overall levels of preeclampsia knowledge among pregnant women, and no difference in understanding was found by health literacy.13 Similarly, in a study designed to improve interpretation of prescription drug warning labels by You et al., health literacy did not predict correct interpretation of an enhanced prescription drug warning label warning against medication use while pregnant.47
Kakkilaya et al. examined the effect of a visual aid on patient knowledge of the morbidity and mortality associated with birth of a very preterm infant (23 weeks gestational age). Improvement in knowledge scores did not vary by health literacy after using the aid.12
In a sample of women between the ages of 16 and 21, STI comprehension was assessed after reading an informational brochure regarding Chlamydia.37 Women with low health literacy had significantly lower knowledge scores compared with women with high health literacy after reviewing the brochure (average knowledge score of 7.54 vs. 9.08 of 10, p < 0.001).37 Boxell et al. found a larger improvement in knowledge of symptoms of gynecologic cancer in women with high health literacy compared with those with moderate or low health literacy after viewing an ovarian and cervical cancer symptom brochure.48
Discussion
Findings from this systematic review suggest that health literacy is related to reproductive health knowledge across a number of topics, including contraception, fertility, prenatal screening, and STIs. Additionally, health literacy appears to be related to certain obstetric health behaviors, such as prenatal vitamin use and exclusive breastfeeding, but its relationship with other reproductive health behaviors, such as behavioral risk factors for STIs and smoking during pregnancy, is less clear. Evidence suggests a link between health literacy and postpartum depression, but too few studies have been conducted on other obstetric and gynecologic outcomes to draw firm conclusions. Finally, the few intervention studies conducted to date have shown promising results, indicating that the use of tailored educational materials can increase understanding of reproductive health topics for patients with both limited and adequate health literacy, perhaps even reducing literacy-related disparities in reproductive health knowledge.
Several studies included in this review demonstrated that women with low health literacy are more likely to exhibit avoidance behavior when it comes to care. This includes less screening for STIs, later initiation of prenatal care, less follow-up of abnormal test results after cervical cancer screening, and less overall likelihood to seek care.24,25,36,38 This may be related to increased distress regarding results, lack of knowledge regarding risks and testing options, lack of health information seeking, poorer healthcare access, or lower level of self-efficacy. Studies in other populations have demonstrated a similar phenomenon.8,49 It is important to determine the root cause of this avoidance, whether it is health literacy or some other factor, to better engage women in preventive care and follow-up.
While this review offers insight on the relationship between health literacy and reproductive knowledge, behavior, and outcomes, it is important to note that studies included in the review had numerous limitations. Specifically, many studies had small sample sizes that were often not representative of the general population and were recruited via convenience sampling. Small sample sizes also made it harder to evaluate certain clinical outcomes such as preterm birth that are not as common. Most studies also used cross-sectional and observational study designs and even the more rigorous experimental studies generally utilized hypothetical scenarios. Measurement was highly variable and often suboptimal, with studies relying upon self-report and measures that have not been validated to assess outcomes. Last, numerous studies solely reported unadjusted analyses and did not control for known factors that impact women's health outcomes. More rigorous studies are clearly warranted to further establish the relationship between health literacy and women's reproductive health outcomes. These studies should seek to use more objective measures of clinically relevant outcomes when possible and more advanced study designs or analyses to account for potential confounding. In addition, given the changing demographics of the United States, more studies should be conducted among Hispanic and Spanish-speaking women.
This systematic review itself also has limitations. As with any systematic review, our review is limited by publication bias. We only synthesized published findings and did not search the gray literature or other sources. It is also possible that articles that should have been included were not returned with our search strategy; however, additional reference mining was performed to minimize this possibility. As this review was restricted to research conducted in the United States and other developing countries, it is possible that relevant articles from other countries were unnecessarily excluded. Additionally, there were several topics that are important to women's health areas (e.g., menopause, incontinence) that were excluded as they were believed to be less relevant to women of reproductive age. Certainly, how health literacy impacts these topics should also be explored.
Studies included in this review reported that anywhere from 9% to 78% of women had less than adequate health literacy skills (average of 46%). This wide variation likely reflects the diversity of populations that study samples were drawn from, the variety in health literacy measures used, and differences in how individuals were categorized as having adequate or inadequate health literacy. Such variability makes it difficult to make comparisons across studies and may have led to conflicting results. This challenge is present for almost all literature reviews focusing on health literacy and has been previously acknowledged to be a limitation for the field.50 Such measurement challenges highlight the need to identify the best health literacy measures available for use in this population and/or to consider the creation of new tools that effectively measure these skills in reproductive age women. Results from this review unfortunately do not offer clear guidance on which published instrument may be optimal for use among reproductive age women. Further refining, standardizing, and improving health literacy measurement will be crucial to advancing this line of research.
Despite measurement variation, findings from the studies included in this review indicate that limited health literacy is likely to be common in reproductive health practices and worthy of further attention and research. While the studies conducted to date offer insight on the relationship between health literacy and reproductive knowledge and related behaviors, more methodologically rigorous studies are needed to further investigate the association between health literacy and clinically meaningful outcomes and to further elucidate the causal mechanisms through which health literacy may affect these outcomes. Finally, more health literacy-informed interventions are needed to move beyond describing the problem of limited health literacy and into the realm of improving reproductive care and outcomes for women.
Our review suggests that health literacy plays an important role in reproductive health for women across a number of key contexts, including contraception, fertility, prenatal screening, and sexual health. Additional research is needed to fully understand these relationships, to further explore the association between health literacy and reproductive outcomes, and to evaluate interventions to reduce literacy-related disparities in reproductive health knowledge and outcomes. In the meantime, obstetricians and gynecologists should be aware of the potentially negative effects of low health literacy on reproductive health and should become more familiar with guidelines promoting clear communication and health literacy best practices for patient education and counseling.51–53 Numerous organizations, including AHRQ, the Joint Commission, and The Centers for Disease Control and Prevention, have advised healthcare providers to utilize clear communication and plain language techniques with all patients regardless of their presumed health literacy skills, thus adopting a universal precautions approach.51 This is essential as limited health literacy is likely to be prevalent in many patient populations and is not always readily recognized by healthcare providers.38,39
Acknowledgments
Dr. Kilfoyle is supported by an institutional NIH training grant (T32 HD040672-15). Dr. Bailey is supported by the UNC Center for Diabetes Translation Research to Reduce Health Disparities (P30DK093002) from the National Institute of Diabetes and Digestive and Kidney Diseases.
Author Disclosure Statement
Dr. Bailey has served as a consultant to, and received grant support from, Merck, Sharp & Dohme Corp. for work unrelated to this manuscript. Dr. Kilfoyle's spouse was employed by GlaxoSmithKline at the time that this research was performed and the manuscript was written.
References
- 1.Nielsen Bohlman L, Panzer AM, Kindig DA, eds. Health Literacy: A prescription to end confusion. Washington, DC: Institute of Medicine of the National Academies, 2004 [PubMed] [Google Scholar]
- 2.Berkman ND, Sheridan SL, Donahue KE, et al. . Health literacy interventions and outcomes: An updated systematic review. Evid Rep Technol Assess (Full Rep) 2011:1–941 [PMC free article] [PubMed] [Google Scholar]
- 3.Parker RM, Wolf MS, Kirsch I. Preparing for an Epidemic of Limited Health Literacy: Weathering the Perfect Storm. J Gen Intern Med 2008;23:1273–1276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.ACOG Committee Opinion No. 585: Health literacy. Obstet Gynecol 2014;123(2 Pt 1):380–383 [DOI] [PubMed] [Google Scholar]
- 5.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J Clin Epidemiol 2009;62:1006–1012 [DOI] [PubMed] [Google Scholar]
- 6.List of Developing Countries. USAID, 2012. Retrieved from: https://www.usaid.gov/sites/default/files/documents/1876/310maa.pdf [Google Scholar]
- 7.Berkman ND, Dewalt DA, Pignone MP, et al. . Literacy and health outcomes. Evid Rep Technol Assess (Summ) 2004:1–8 [PMC free article] [PubMed] [Google Scholar]
- 8.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: An updated systematic review. Ann Intern Med 2011;155:97–107 [DOI] [PubMed] [Google Scholar]
- 9.Kiechle ES, Bailey SC, Hedlund LA, Viera AJ, Sheridan SL. Different measures, different outcomes? A systematic review of performance-based versus self-reported measures of health literacy and numeracy. J Gen Intern Med 2015;30:1538–1546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yee LM, Simon MA. The role of health literacy and numeracy in contraceptive decision-making for urban Chicago women. J Community Health 2014;39:394–399 [DOI] [PubMed] [Google Scholar]
- 11.Bennett I, Switzer J, Aguirre A, Evans K, Barg F. ‘Breaking it down’: Patient-clinician communication and prenatal care among African American women of low and higher literacy. Ann Fam Med 2006;4:334–340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kakkilaya V, Groome LJ, Platt D, et al. . Use of a visual aid to improve counseling at the threshold of viability. Pediatrics 2011;128:e1511–e1519 [DOI] [PubMed] [Google Scholar]
- 13.You WB, Wolf MS, Bailey SC, Grobman WA. Improving patient understanding of preeclampsia: A randomized controlled trial. Am J Obstet Gynecol 2012;206:431.e431–e435 [DOI] [PubMed] [Google Scholar]
- 14.Yee LM, Wolf M, Mullen R, et al. . A randomized trial of a prenatal genetic testing interactive computerized information aid. Prenat Diagn 2014;34:552–557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weiss BD, Sheehan CP, Gushwa LL. Is low literacy a risk factor for symptoms of depression in postpartum women? J Reprod Med 2009;54:563–568 [PubMed] [Google Scholar]
- 16.Ehrenthal DB, Maiden K, Rogers S, Ball A. Postpartum healthcare after gestational diabetes and hypertension. J Womens Health (Larchmt) 2014;23:760–764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lupattelli A, Picinardi M, Einarson A, Nordeng H. Health literacy and its association with perception of teratogenic risks and health behavior during pregnancy. Patient Educ Couns 2014;96:171–178 [DOI] [PubMed] [Google Scholar]
- 18.Hameen-Anttila K, Kokki E, Lupattelli A, et al. . Factors associated with the need for information about medicines among pregnant women—a multinational internet-based survey. Res Social Adm Pharm 2015;11:297–302 [DOI] [PubMed] [Google Scholar]
- 19.Smedberg J, Lupattelli A, Mardby AC, Nordeng H. Characteristics of women who continue smoking during pregnancy: A cross-sectional study of pregnant women and new mothers in 15 European countries. BMC Pregnancy Childbirth 2014;14:213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rutherford J, Holman R, MacDonald J, Taylor A, Jarrett D, Bigrigg A. Low literacy: A hidden problem in family planning clinics. J Fam Plann Reprod Health Care 2006;32:235–240 [DOI] [PubMed] [Google Scholar]
- 21.Duggan L, McCarthy S, Curtis LM, et al. . Associations between health literacy and beliefs about medicines in an Irish obstetric population. J Health Commun 2014;19(Suppl 2):106–114 [DOI] [PubMed] [Google Scholar]
- 22.Igarashi Y, Horiuchi S, Porter SE. Immigrants' experiences of maternity care in Japan. J Community Health 2013;38:781–790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bennett IM, Culhane JF, McCollum KF, Mathew L, Elo IT. Literacy and depressive symptomatology among pregnant Latinas with limited English proficiency. Am J Orthopsychiatry 2007;77:243–248 [DOI] [PubMed] [Google Scholar]
- 24.Endres LK, Sharp LK, Haney E, Dooley SL. Health literacy and pregnancy preparedness in pregestational diabetes. Diabetes Care 2004;27:331–334 [DOI] [PubMed] [Google Scholar]
- 25.Fortenberry JD, McFarlane MM, Hennessy M, et al. . Relation of health literacy to gonorrhoea related care. Sex Transm Infect 2001;77:206–211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Davis TC, Crouch MA, Long SW, et al. . Rapid assessment of literacy levels of adult primary care patients. Fam Med 1991;23:433–435 [PubMed] [Google Scholar]
- 27.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: A new instrument for measuring patients' literacy skills. J Gen Intern Med 1995;10:537–541 [DOI] [PubMed] [Google Scholar]
- 28.Weiss BD, Mays MZ, Martz W, et al. . Quick assessment of literacy in primary care: The newest vital sign. Ann Fam Med 2005;3:514–522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med 2004;36:588–594 [PubMed] [Google Scholar]
- 30.Gossett DR, Nayak S, Bhatt S, Bailey SC. What do healthy women know about the consequences of delayed childbearing? J Health Commun 2013;18(Suppl 1):118–128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shieh C, Broome ME, Stump TE. Factors associated with health information-seeking in low-income pregnant women. Women Health 2010;50:426–442 [DOI] [PubMed] [Google Scholar]
- 32.Davis TC, Fredrickson DD, Potter L, et al. . Patient understanding and use of oral contraceptive pills in a southern public health family planning clinic. South Med J 2006;99:713–718 [DOI] [PubMed] [Google Scholar]
- 33.Gazmararian JA, Parker RM, Baker DW. Reading skills and family planning knowledge and practices in a low-income managed-care population. Obstet Gynecol 1999;93:239–244 [DOI] [PubMed] [Google Scholar]
- 34.Raymond EG, Dalebout SM, Camp SI. Comprehension of a prototype over-the-counter label for an emergency contraceptive pill product. Obstet Gynecol 2002;100:342–349 [DOI] [PubMed] [Google Scholar]
- 35.Raymond EG, L'Engle KL, Tolley EE, Ricciotti N, Arnold MV, Park S. Comprehension of a prototype emergency contraception package label by female adolescents. Contraception 2009;79:199–205 [DOI] [PubMed] [Google Scholar]
- 36.Sharp LK, Zurawski JM, Roland PY, O'Toole C, Hines J. Health literacy, cervical cancer risk factors, and distress in low-income African-American women seeking colposcopy. Ethn Dis 2002;12:541–546 [PubMed] [Google Scholar]
- 37.Needham HE, Wiemann CM, Tortolero SR, Chacko MR. Relationship between health literacy, reading comprehension, and risk for sexually transmitted infections in young women. J Adolesc Health 2010;46:506–508 [DOI] [PubMed] [Google Scholar]
- 38.Lindau ST, Tomori C, Lyons T, Langseth L, Bennett CL, Garcia P. The association of health literacy with cervical cancer prevention knowledge and health behaviors in a multiethnic cohort of women. Am J Obstet Gynecol 2002;186:938–943 [DOI] [PubMed] [Google Scholar]
- 39.Lindau ST, Basu A, Leitsch SA. Health literacy as a predictor of follow-up after an abnormal Pap smear: A prospective study. J Gen Intern Med 2006;21:829–834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Poorman E, Gazmararian J, Elon L, Parker R. Is health literacy related to health behaviors and cell phone usage patterns among the text4baby target population? Arch Public Health 2014;72:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kotelchuck M. An evaluation of the Kessner Adequacy of Prenatal Care Index and a proposed Adequacy of Prenatal Care Utilization Index. Am J Public Health 1994;84:1414–1420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shieh C, Mays R, McDaniel A, Yu J. Health literacy and its association with the use of information sources and with barriers to information seeking in clinic-based pregnant women. Health Care Women Int 2009;30:971–988 [DOI] [PubMed] [Google Scholar]
- 43.Cho RN, Plunkett BA, Wolf MS, Simon CE, Grobman WA. Health literacy and patient understanding of screening tests for aneuploidy and neural tube defects. Prenat Diagn 2007;27:463–467 [DOI] [PubMed] [Google Scholar]
- 44.Arnold CL, Davis TC, Berkel HJ, Jackson RH, Nandy I, London S. Smoking status, reading level, and knowledge of tobacco effects among low-income pregnant women. Prev Med 2001;32:313–320 [DOI] [PubMed] [Google Scholar]
- 45.Kaufman H, Skipper B, Small L, Terry T, McGrew M. Effect of literacy on breast-feeding outcomes. South Med J 2001;94:293–296 [PubMed] [Google Scholar]
- 46.You WB, Wolf M, Bailey SC, et al. . Factors associated with patient understanding of preeclampsia. Hypertens Pregnancy 2012;31:341–349 [DOI] [PubMed] [Google Scholar]
- 47.You WB, Grobman W, Davis T, et al. . Improving pregnancy drug warnings to promote patient comprehension. Am J Obstet Gynecol 2011;204:318. e1–5 [DOI] [PubMed] [Google Scholar]
- 48.Boxell EM, Smith SG, Morris M, et al. . Increasing awareness of gynecological cancer symptoms and reducing barriers to medical help seeking: Does health literacy play a role? J Health Commun 2012;17(Suppl 3):265–279 [DOI] [PubMed] [Google Scholar]
- 49.Morris NS, Field TS, Wagner JL, et al. . The association between health literacy and cancer-related attitudes, behaviors, and knowledge. J Health Commun 2013;18(Suppl 1):223–241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Haun J, Luther S, Dodd V, Donaldson P. Measurement variation across health literacy assessments: Implications for assessment selection in research and practice. J Health Commun 2012;17(Suppl 3):141–159 [DOI] [PubMed] [Google Scholar]
- 51.The Joint Commission. What did the doctor say? Improving health literacy to protect patient safety. Oakbrook Terrace, IL: The Joint Commission, 2007 [Google Scholar]
- 52.Brega AG, Barnard J, Mabachi NM, et al. . AHRQ Health Literacy Universal Precautions Toolkit, Second Edition. (Prepared by Colorado Health Outcomes Program, University of Colorado Anschutz Medical Campus under Contract No. HHSA290200710008, TO#10.) AHRQ Publication No. 15-0023-EF. Rockville, MD: Agency for Healthcare Research and Quality, January 2015 [Google Scholar]
- 53.U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. National Action Plan to Improve Health Literacy; Washington, DC, 2010 [Google Scholar]