Abstract
STUDY DESIGN
Retrospective cohort.
OBJECTIVES
The objectives of this study were (1) to examine patients’ general expectations for treatment by physical therapists and specific expectations for common interventions in patients with neck pain, and (2) to assess the extent to which the patients’ general and specific expectations for treatment, particularly spinal manipulation, affect clinical outcomes.
BACKGROUND
Patient expectations can have a profound influence on the magnitude of treatment outcome across a broad variety of patient conditions.
METHODS
We performed a secondary analysis of data from a clinical trial of interventions for neck pain. Prior to beginning treatment for neck pain, 140 patients were asked about their general expectations of benefit as well as their specific expectations for individual interventions. Next, we examined how these expectations related to the patients’ ratings of the success of treatment at 1 and 6 months after treatment.
RESULTS
Patients had positive expectations for treatment by a physical therapist, with more than 80% of patients expecting moderate relief of symptoms, prevention of disability, the ability to do more activity, and to sleep better. The manual therapy interventions of massage (87%) and manipulation (75%) had the highest proportion of patients who expected these interventions to significantly improve neck pain. These were followed by strengthening (70%) and range-of-motion (54%) exercises. Very few patients thought surgery would improve their neck pain (less than 1%). At 1 month, patients who were unsure of experiencing complete pain relief had lower odds of reporting a successful outcome than patients expecting complete relief (odds ratio [OR] = 0.33; 95% confidence interval [CI]: 0.11, 0.99). Believing that manipulation would help and not receiving manipulation lowered the odds of success (OR = 0.16; 95% CI: 0.04, 0.72) compared to believing manipulation would help and receiving manipulation. Six months after treatment, having unsure expectations for complete pain relief lowered the odds of success (OR = 0.19; 95% CI: 0.05, 0.7), whereas definitely expecting to do more exercise increased the odds of success (OR = 11.4; 95% CI: 1.7, 74.7). Regarding self-reported disability assessed with the Neck Disability Index, patients who believed manipulation would help and received manipulation reported less disability than those who did not believe manipulation would help and both received manipulation (mean difference, −3.8; 95% CI: −5.9, −1.5; P = .006) and did not receive manipulation (mean difference, −5.7; 95% CI: −9.3, −2.1; P = .014). There was also an interaction between time and the expectation for complete relief.
CONCLUSION
General expectations of benefit have a strong influence on clinical outcomes for patients with neck pain.
Keywords: cervical spine, physical therapy techniques, treatment
A recent report by the Institute of Medicine,12 Relieving Pain in America, includes many recommendations to improve care of patients with pain. Specifically, the report indicates that attention to individual patient differences is of paramount importance. Individual patient differences include a wide variety of factors known to influence the pain experience. It has been well established that health status and concomitant conditions, such as psychological factors, can influence the pain experience.10,11,15,16,20,22,23 Intrinsic biological factors, including genetics, age, and sex, are also known to influence how an individual experiences pain.8 The report also lists health beliefs, including patient preference, as an important factor for determining the choice of treatment for the management of pain.12
Patient preference is one of the pillars of evidence-based practice, alongside research evidence and clinical experience. Patient preferences are related to the outcome of treatment through at least 2 routes.3 First, patient preferences are related to outcomes through patient participation in decision making regarding treatment. Shared decision making can influence patients’ beliefs and emotions. Increasing patient participation in decision making can increase satisfaction with, and adherence to, a treatment regimen.3 In the Patient Protection and Affordable Care Act,21 passed in the United States, guidelines are provided to facilitate shared decision making among patients, healthcare professionals, and caregivers.
Second, patients’ preferences are likely intertwined with their expectations for a given treatment. That is, a patient may have a preference for a particular treatment because he or she has a specific expectation for that treatment. Thompson and Sunol19 developed a model of healthcare expectation that included predicted, ideal, and normative expectations. A predicted expectation is what the patient thinks will happen in response to treatment. For example, the patient may have a predicted expectation of a 50% reduction in pain in response to physical therapy.19 An ideal expectation is what the patient wants to happen during treatment, for example, complete pain relief. A normative expectation is what the patient thinks should occur with treatment, for example, how a healthcare provider may speak, dress, and act, as well as how the treatment should be performed.19
Expectations are unique to the individual and are developed by both past personal experiences and the experiences of family members and acquaintances.19 In addition, patient expectations can be influenced during a patient encounter by the interactions that a patient has with the healthcare provider.19 These newly formed expectations can be positive (increased expectation of benefit from an individual intervention) or negative (decreased expectation of benefit) and can potentially influence clinical outcomes. Dramatic evidence of this was demonstrated experimentally by Benedetti et al.1 These investigators injected participants with saline and told 1 group that it was a powerful painkiller. The other group was told that it was a drug that increased pain. The exact same intervention (saline injection) was associated with a significant increase in pain tolerance in the group expecting less pain and a significant decrease in pain tolerance in those told to expect more pain.1
Consequently, understanding patient expectations for interventions is an integral part of developing meaningful treatment plans that include the patient. Therefore, the purpose of this secondary analysis was 2-fold. First, we examined patient expectations for treatment effectiveness of interventions provided by a physical therapist for neck pain, then assessed specific patient expectations for treatment effectiveness of individual interventions commonly used by physical therapists to manage patients with neck pain. Evaluating these data provided information about the general expectations for treatment effectiveness held by patients prior to beginning treatment by a physical therapist. Second, we assessed the extent to which the patients’ expectations of the treatment effectiveness of spinal manipulation affected the clinical outcomes of patients enrolled in a clinical trial of a subset of interventions for patients with neck pain.
METHODS
We performed a secondary analysis of data from a randomized controlled clinical trial (NCT00504686) comparing interventions for patients with neck pain. In that study, 140 patients with a primary complaint of neck pain were randomly assigned to receive either 5 sessions of stretching and strengthening exercises (exercise group) or 2 sessions of thoracic spine manipulation and range-of-motion exercises followed by 3 sessions of stretching and strengthening exercise (manipulation and exercise group). The primary outcomes of the original study were pain and disability.7
Participants
Patients with a primary report of neck pain seen in 1 of 5 physical therapy clinics located in 4 different states across the United States (New Hampshire, Wisconsin, Colorado, Massachusetts) between July 2007 and December 2008 were screened for eligibility. Patients were eligible to participate in the primary study if they were between 18 and 60 years of age, had a primary report of neck pain with or without unilateral upper extremity symptoms, and had a Neck Disability Index (NDI) score of at least 20%. Patients were excluded if they had any of the following: serious pathologies, diagnosis of cervical spinal stenosis (as identified in the patient's medical intake form) or bilateral upper extremity symptoms, evidence of central nervous system involvement, 2 or more positive neurologic signs consistent with nerve root compression, pending legal action regarding their neck pain, or inability to adhere to the treatment and follow-up schedule. All patients provided informed consent prior to their enrollment in the study.
Expectations
General expectations for the effectiveness of treatment provided by a physical therapist were collected at the initial visit. Patients were asked a series of questions related to the results they expected from treatment. Possible responses were “definitely yes,” “yes,” “not sure,” “no,” and “definitely no,” with “not sure” as the midpoint response. Results included (1) complete relief from symptoms (pain, stiffness, swelling, numbness, weakness, instability), (2) moderate relief from symptoms (pain, stiffness, swelling, numbness, weakness, instability), (3) to do more everyday household or yard activities, (4) to sleep more comfortably, (5) to go back to my usual job, (6) to exercise and do more recreational activities, and (7) to prevent future disability.
Specific expectations for treatment effectiveness of potential individual interventions were collected at the initial visit by asking the patient to consider the following statement: “I believe [the intervention] will significantly help to improve this episode of my neck pain.” Possible responses were “definitely agree,” “agree,” “neutral,” “disagree,” and “definitely disagree,” with “neutral” as the midpoint response. These responses were used to rate 10 interventions routinely used in rehabilitation practice (definitions given to participants are shown in parentheses): aerobic exercise (ie, walking, stationary cycling, StairMaster, etc), manipulation (ie, having your neck or back “cracked”), massage, medication, modalities (ie, ultrasound, transcutaneous electrical nerve stimulation, etc), range-of-motion exercises (ie, stretching), rest, traction (lying on your back or stomach with straps, with a harness strapped on that stretches out your neck or back), strengthening exercises, and surgery.
Outcomes
The NDI is a condition-specific disability scale for patients with neck pain that consists of 10 items, including questions about pain and function, each scored from 0 to 5, with a maximum score of 50 points. The score is commonly reported as a percentage, with higher scores indicating greater perceived disability. The NDI has been reported to be a reliable and valid outcome measure for patients with neck pain.5,6
In addition, participants completed the global rating of change scale (GROC) to determine whether the intervention was successful from the participant's perspective. This served as the overall measure of how the patient viewed the outcome of his or her participation in the intervention. The GROC is a 15-point scale anchored at one end with “a very great deal worse” (−7) and at the other with “a very great deal better” (+7). The GROC is commonly used in clinical research14 and is recommended for improving the applicability of information from clinical trials to clinical practice.9 In the original trial, patients who rated themselves “a very great deal better,” “a great deal better,” or “quite a bit better” (a score of +5 or greater) were considered to have had a successful intervention. These data were analyzed based on responses at the 1-month and 6-month follow-up visits.
Analysis
First, we determined patients’ general expectations of benefit from treatment by a physical therapist, as well as their specific expectations for individual interventions. For the general expectations, the categories “definitely” and “somewhat” were collapsed, resulting in 3 categories of response for each general expectation (yes, neutral, and no). For analyses of specific expectations for an individual intervention, the categories “completely” and “somewhat” were collapsed so that there were categories for high, neutral, and low expectations of benefit from treatment. Frequencies were calculated for each category within each general expectation, and the categories were ranked. However, no inferential statistics were performed, as there were no a priori hypotheses to be tested.
Next, we examined the data from the clinical trial. First, we compared patients who did not complete the 6-month follow-up to patients who did attend the follow-up on demographic variables and general and specific expectations to determine if there were differences between these groups of participants. Then we examined how matching an intervention received by the patient with an intervention that the patient expected to produce benefit might be related to the outcomes of treatment for neck pain. For example, consider a patient who believed strongly that manipulation would be beneficial. Based on this expectation, what outcomes would that patient achieve if he or she were to be treated with exercise instead? High expectations that manipulation would benefit the patient were recoded as “believe manipulation will help,” and neutral and low expectations for manipulation were recoded as “do not believe manipulation will help.” This new variable was then cross-referenced with the assigned intervention to determine if a patient received the manipulation intervention for which he or she had “high” expectations for treatment effectiveness. This process resulted in 4 groups: believed manipulation would help and also received manipulation as part of treatment (n = 55), believed manipulation would help and did not receive manipulation (n = 52), did not believe manipulation would help and received manipulation (n = 13), and did not believe manipulation would help and did not receive manipulation (n = 13).
In the first set of analyses, we used the GROC ratings of improvement to test associations between expectations matched to intervention and perceived outcome at 1 month and at 6 months after commencing treatment. First, bivariate associations were calculated between successful outcome and each of the general expectations, as well as age, gender, disability, and average pain. Associations between categorical variables and outcome were tested by calculating chi-squares and point-biserial correlations.
We then used separate multivariate logistic regression models (1-month and 6-month outcomes) to test the association among successful outcomes (using the GROC) and the intervention received, intervention matched to specific expectation (eg, believed manipulation would help and received manipulation), and general expectations of physical therapy. Variables with significant bivariate associations (P<.05) with a successful outcome at 1 month and at 6 months were entered into each model as a block. We based this approach on not having a priori hypotheses about the variables that might be most important in predicting outcome and included these variables for exploratory reasons. Multicollinearity of variables was determined using a variance inflation factor greater than 10, and model fit was reviewed using Nagelkerke R2.
We also performed a mixed-model analysis of variance. Predictor variables were determined from bivariate Spearman correlations between general expectations and the change in disability over the 6-month period. Only the general expectation for complete relief (r = −0.252, P = .003) was associated with the change in disability. In addition, baseline pain intensity was associated with the change in disability. Therefore, the model included a repeated factor of time (baseline, 1 month, 6 months), between-subject factors of matched expectation and the expectations of complete pain relief, and baseline pain intensity as a covariate. Two-way within-by-between interactions were built for time and matched treatment, and for time and expectation for complete pain relief. Our primary interest was in the interaction terms. Self-report of disability from neck pain was the dependent variable. Missing data were estimated in the mixed-model analyses using restricted maximum likelihood ratio estimation with 100 iterations.
RESULTS
One hundred forty patients (average ± SD age, 39.9 ± 11.3 years; 69% female) were enrolled in the primary study. Seventy patients were randomly assigned to receive manipulation and exercise, and 70 patients were randomly assigned to receive exercise only. One hundred thirty-seven (98%) participants completed the assessments at 1 month and 114 (81%) participants were assessed at the 6-month follow-up. No statistical differences in demographic variables were identified between patients who responded at 6 months and those who did not (TABLE 1). The only statistical difference noted between these groups in the general expectations for physical therapy was that a greater proportion of the dropout group expected to have better sleep as a result of the interventions.
TABLE 1.
Patient Characteristics*
| Variable | All Participants (n = 140) | Did Not Complete 6-mo Follow-up (n = 26) | Completed 6-mo Follow-up (n = 114) | Comparison P Value |
|---|---|---|---|---|
| Age, y | 39.9 ± 11.3 | 41.1 ± 11.7 | 39.4 ± 11.1 | .51 |
| Gender (female), % | 69 | 62 | 72 | .35 |
| Symptom duration, d | 63.5 ± 75.2 | 73.6 ± 66.0 | 60.8 ± 55.2 | .37 |
| Neck Disability Index | 30.0 ± 7.7 | 28.5 ± 6.5 | 29.1 ± 7.9 | .66 |
| Average pain† | 4.2 ± 1.5 | 4.1 ± 2.0 | 4.2 ± 1.3 | .68 |
| Proportion reporting success at 1 mo (visit 5), % | 44 | 45 | 43 | .89 |
Values are mean ± SD unless otherwise indicated.
11-point numeric pain rating scale.
Patient Expectations
Generally, patients had positive expectations for treatment by a physical therapist, with more than 80% of patients expecting to have moderate relief of symptoms, prevention of disability, and the ability to do more activities and to sleep better. Nearly 70% of patients expected to return to their usual work, and about 60% were expecting complete relief of symptoms. These general expectations are shown in FIGURE 1.
FIGURE 1.
Participants’ general expectations of outcome from receiving interventions performed by a physical therapist. Participants responded to the statement, “What results do you expect from your treatment?” General expectations are rank ordered based on the proportion of participants indicating “yes,” which comprised “definitely yes” and “probably yes,” or those indicating “no,” which comprised “probably not” and “definitely not.” *Only 60% of participants responded to this item.
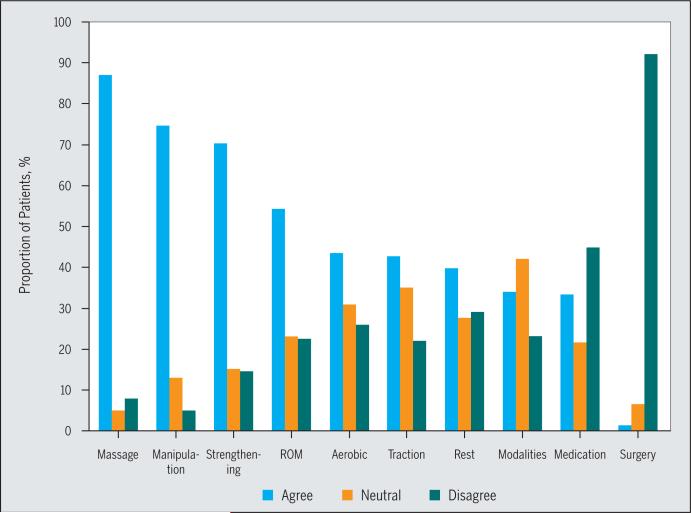
The specific expectations of significant improvement in pain for the individual interventions used by physical therapists are summarized in FIGURE 2. The manual therapy interventions of massage (87%) and manipulation (75%) had the highest proportion of patients who expected these interventions to significantly improve neck pain. These were followed by strengthening (70%) and range-of-motion (54%) exercises. Very few patients thought surgery would improve their neck pain (less than 1%).
FIGURE 2.
Participants’ specific expectations of benefit from common interventions for “this episode of neck pain.” Interventions are rank ordered based on the proportion of participants who “agreed” with the statement, “I believe [the intervention] will significantly help to improve this episode of my neck pain.” “Agree” included the collapsed categories “completely agree” and “agree.” “Disagree” included the collapsed categories “completely disagree” and “disagree.” Abbreviation: ROM, range of motion.
Effect of Expectation on Outcome: Rating of Improvement
At 1 month, 58 patients (41%) had a successful outcome using the GROC criteria. Significant unadjusted associations with outcome were found for the general expectation for complete relief and matched specific expectation for manipulation and the assigned intervention (TABLE 2), as well as with baseline disability.
TABLE 2.
General Expectations and Variables Associated With Success
| Success at 1 mo | Success at 6 mo | |||||
|---|---|---|---|---|---|---|
| χ 2 | df | P Value | χ 2 | df | P Value | |
| General expectations | ||||||
| Complete relief | 10.56 | 2 | .005 | 9.66 | 2 | .008 |
| Moderate relief | 2.96 | 2 | .228 | 3.37 | 2 | .185 |
| Do more activities | 5.26 | 2 | .072 | 2.29 | 2 | .319 |
| Sleep more | 0.51 | 2 | .773 | 0.02 | 2 | .879 |
| Exercise more | 4.89 | 2 | .087 | 10.21 | 2 | .006 |
| Prevent disability | 0.47 | 2 | .792 | 1.22 | 2 | .543 |
| Belief-group interaction* | 13.09 | 3 | .005 | 11.67 | 3 | .009 |
| Gender | 0.00 | 1 | 1.000 | 1.68 | 1 | .280 |
| R 2 | P Value | R 2 | P Value | |
|---|---|---|---|---|
| Age | −0.08 | .342 | −0.02 | .876 |
| Disability | 0.28 | .001 | 0.13 | .157 |
| Pain | 0.13 | .194 | −0.03 | .795 |
Four groups based on the specific expectations for manipulation and subsequent assignment to the intervention group: believed manipulation would help and received manipulation, believed manipulation would help and did not receive manipulation, did not believe manipulation would help and received manipulation, and did not believe manipulation would help and did not receive manipulation.
For the general expectation for complete relief, a greater proportion of participants expecting complete relief had a successful outcome (73%) compared to participants who did not expect complete relief (45%). When examining the matched variable, more participants who believed in manipulation and received it reported a successful outcome (TABLE 3). We included group assignment, the matched variable, and the general expectation for complete relief in the logistic regression model predicting success at 1 month (TABLE 4). No factor had a variance inflation factor greater than 10. The model showed significant effects for disability (Wald χ2 = 4.593, P = .032), the matched variable (Wald χ2 = 9.797, P = .020), and the general expectation for complete relief (Wald χ2 = 5.743, P = .050), but not the intervention assignment (Wald χ2 = 0.019, P = .892). Nagelkerke pseudo-R2 was 0.21. Specifically, participants who believed manipulation would help but did not receive that intervention had only 0.16 (95% CI: 0.04, 0.72) times the odds of reporting a successful outcome of those who believed manipulation would help and received manipulation. Participants who did not believe manipulation would help and received manipulation had 0.42 (95% confidence interval [CI]: 0.18, 0.97) times the odds of reporting a successful outcome of those who believed manipulation would help and received manipulation. In addition, participants who were undecided about expecting complete relief had 0.33 (95% CI: 0.11, 0.99) times the odds of reporting a successful outcome of those who expected complete relief, regardless of the intervention received.
TABLE 3.
Proportion of Patients Reporting Success*
| Success at 1 mo (n = 137) | Success at 6 mo (n = 114) | |||
|---|---|---|---|---|
| No | Yes | No | Yes | |
| BY | 40 | 60 | 21 | 79 |
| BN | 62 | 38 | 54 | 47 |
| DNBY | 77 | 23 | 36 | 64 |
| DNBN | 85 | 15 | 55 | 46 |
| Expect complete relief | ||||
| Definitely | 45 | 73 | 43 | 69 |
| Unsure | 26 | 10 | 31 | 10 |
| Definitely not | 30 | 17 | 26 | 21 |
| Expect to exercise more | ||||
| Definitely | ... | ... | 72 | 94 |
| Unsure | ... | ... | 5 | 3 |
| Definitely not | ... | ... | 23 | 3 |
Abbreviations: BN, believed manipulation would help and did not receive manipulation; BY, believed manipulation would help and received manipulation; DNBN, did not believe manipulation would help and did not receive manipulation; DNBY, did not believe manipulation would help and received manipulation.
Values are %.
TABLE 4.
Multivariate Logistic Model Predicting Perceived Improvement at 1 Month
| B | SE | P Value | Exp(B)* | |
|---|---|---|---|---|
| Intervention (reference: exercise) | 0.14 | 0.67 | .174 | 1.15 (0.67, 2.95) |
| BN† | −1.82 | 0.76 | .017 | 0.16 (0.04, 0.72) |
| DNBY† | −0.86 | 0.43 | .043 | 0.42 (0.18, 0.97) |
| DNBN† | −1.65 | 0.85 | .052 | 0.19 (0.04, 1.01) |
| Expectation for complete relief (unsure)‡ | −1.11 | 0.57 | .050 | 0.33 (0.11, 0.99) |
| Expectation for complete relief (definitely not)‡ | −0.89 | 0.48 | .066 | 0.41 (0.16, 1.06) |
| Baseline disability | 0.06 | 0.03 | .032 | 1.06 (1.01, 1.12) |
| Constant | −1.78 | 0.45 | .043 | 0.28 |
Abbreviations: BN, believed manipulation would help and did not receive manipulation; DNBN, did not believe manipulation would help and did not receive manipulation; DNBY, did not believe manipulation would help and received manipulation; Exp(B), exponentiation of the B coefficient; SE, standard error.
Values in parentheses are 95% confidence interval.
Reference group: believed manipulation would help and received manipulation.
Reference group: definitely.
Seventy of the patients who completed the 6-month follow-up (62%) experienced success. Significant unadjusted associations with success at 6 months were identified for both the general expectation for complete pain relief and the expectation to be able to exercise more, and for matched intervention (TABLE 2). We included group, both general expectations, and the matched variable in the model. No variable had a variance inflation factor greater than 10. The only significant effects were for the general expectation for complete relief (Wald χ2 = 6.223, P = .045) and the general expectation to be able to exercise more (Wald χ2 = 6.810, P = .033). The Nagelkerke pseudo-R2 was 0.37. The model is summarized in TABLE 5. In this model, a participant who was unsure of whether he or she would experience complete relief had 0.19 (95% CI: 0.04, 0.99) times the odds of reporting a successful outcome compared to someone who expected complete relief. Expecting complete relief provided no better odds than not expecting complete relief. In contrast, a participant expecting to be able to do more exercise had 11 times the odds (95% CI: 1.7, 74.6) of reporting a successful outcome compared to someone not expecting to be able to do more exercise.
TABLE 5.
Multivariate Logistic Model Predicting Perceived Improvement at 6 Months
| B | SE | P Value | Exp(B)* | |
|---|---|---|---|---|
| Intervention (reference: exercise) | 2.72 | 1.01 | .007 | 15.10 (2.10, 109.90) |
| BN† | −0.42 | 0.93 | .649 | 0.66 (0.11, 4.03) |
| DNBY† | 0.97 | 0.97 | .318 | 2.63 (0.39, 17.66) |
| DNBN†‡ | ... | ... | ... | ... |
| Expectation for complete relief (unsure)§ | −1.67 | 0.85 | .048 | 0.19 (0.04, 0.99) |
| Expectation for complete relief (definitely not)§ | 0.06 | 0.63 | .931 | 1.06 (0.31, 3.65) |
| Expectation to exercise more (unsure)§ | 2.77 | 1.46 | .058 | 15.88 (0.91, 279.11) |
| Expectation to exercise more (definitely not)§ | 2.43 | 0.96 | .011 | 11.39 (1.73, 74.56) |
| Constant | −3.18 | 1.28 | .013 | 0.04 |
Abbreviations: BN, believed manipulation would help and did not receive manipulation; DNBN, did not believe manipulation would help and did not receive manipulation; DNBY, did not believe manipulation would help and received manipulation; Exp(B), exponentiation of the B coefficient; SE, standard error.
Values in parentheses are 95% confidence interval.
Reference group: believed manipulation would help and received manipulation.
Parameter set to zero, as parameter was redundant.
Reference group: definitely.
Effect of Expectation on Outcome: Self-Report of Disability
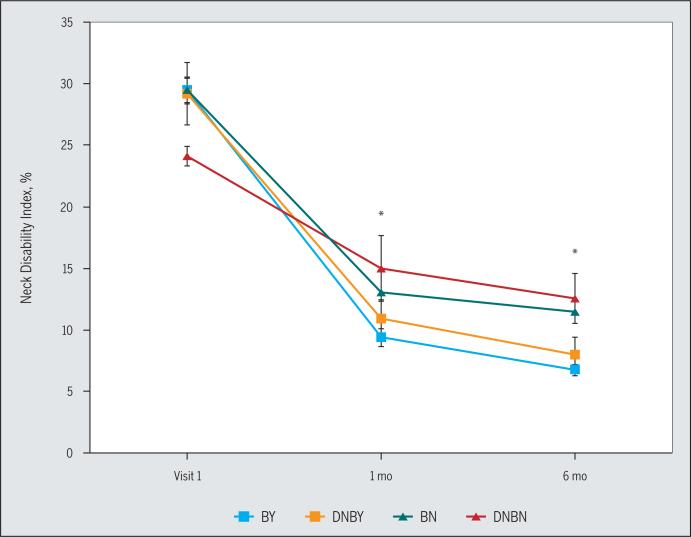
Several 2-way interactions were identified in the mixed-model analysis of variance. An interaction between time and matched variable (F3,125 = 2.628, P = .050) was noted and is shown in FIGURE 3. Further investigation of the interaction using 1-way analysis of variance at each testing session showed no statistical differences among matched groups at baseline (F3,137 = 1.91, P = .13) but differences at 1 month (F3,137 = 5.38, P = .002) and 6 months (F3,137 = 8.06, P<.001). At 1 month, participants who believed manipulation would help and received manipulation reported less disability than those who did not believe manipulation would help and both received manipulation (mean difference, −3.8; 95% CI: −5.9, −1.5) and did not receive manipulation (mean difference, −5.7; 95% CI: −9.3, −2.1). Similarly, at 6 months, participants who believed manipulation would help and received manipulation reported less disability than those who did not believe manipulation would help and both received manipulation (mean difference, −4.8; 95% CI: −7.7, −1.9) and did not receive manipulation (mean difference, −5.8; 95% CI: −10.6, −1.1).
FIGURE 3.
Interaction effect of “matched” intervention and time on self-reported disability. *BY greater than BN and DNBN (P = .001). Abbreviations: BN, believed manipulation would help and did not receive manipulation; BY, believed manipulation would help and received manipulation; DNBN, did not believe manipulation would help and did not receive manipulation; DNBY, did not believe manipulation would help and received manipulation.
There was an interaction between time and the expectation for complete relief (F2,117 = 4.036, P = .020). Here, participants who expected complete relief had greater changes in disability at 1 month (mean difference, 20.3%; 95% CI: 18.1%, 22.6%) compared to those who did not expect complete relief (mean difference, 14.1%; 95% CI: 11.1%, 17.0%). The interaction between time and baseline pain intensity was also significant (F1,125 = 22.429, P<.001).
DISCUSSION
The primary findings from these analyses were that (1) patients enrolled in a randomized clinical trial had high general expectations of treatment by a physical therapist, (2) patients expected manual therapies and exercise to be most beneficial for their episode of neck pain, (3) general expectations for pain relief had an important influence on outcome of treatment for neck pain, and (4) matching the patient's belief that manipulation would help with receiving manipulation might have added the short-term benefit of perceived success, but this benefit was lost by 6 months.
In this study, we measured general expectations for treatment in patients with neck pain. The majority of patients had high general expectations of benefit. In fact, more than three quarters of patients enrolled expected to get moderate relief from pain, to improve function, and to prevent disability. This finding is in agreement with other studies that have suggested that general expectation for the benefit of care is consistently high. Mahomed et al,17 for example, noted that 76% of patients awaiting surgery for knee or hip osteoarthritis expected “no pain at all after surgery.” One might also assume that patients seeking treatment primarily do so because they expect the treatment to be of benefit. Only when patients in our study were asked whether they expected complete relief did this differ. Approximately 24% of patients did not expect complete relief after treatment, about 18% were unsure, and less than 60% expected complete pain relief.
The second finding of this analysis was that patients seeking intervention for neck pain had specific expectations that manual therapy and exercise interventions would significantly help improve their pain more than interventions such as rest, modalities, medication, or surgery. In our previous study of specific expectations for interventions for low back pain,2 we noted that larger proportions of patients expected exercise to be beneficial for back pain (greater than 80% for stretching and strengthening) than those who expected manual therapy to be beneficial (72% for massage, 60% for manipulation). In the current study, this finding was reversed, such that more participants expected manual therapy (87% for massage, 75% for manipulation) to be effective when compared to exercise (70% for strengthening, 54% for stretching). Clinical guidelines for the management of neck pain recommend the use of manual therapy and exercise to reduce neck pain.4 This study suggests that patients seeking physical therapy for neck pain have high specific expectations for the interventions recommended by the clinical guidelines.
In the subsequent analyses, we were interested in the influence that both the general expectations and specific expectations for manipulation had on the reported outcomes of treatment. The general expectation for complete pain relief had an influence on perceived outcome (measured using the GROC) at 1-month and 6-month follow-ups and on the self-report of disability (measured using the NDI). Patients who expected complete pain relief had better odds of reporting that they were “somewhat improved,” “much improved,” or “very much improved” (success) at 1 month. At 6 months, however, a different situation existed: being unsure of whether to expect complete pain relief reduced the odds of reporting success, and expecting complete relief did not improve the odds of reporting success. The general expectation to be able to do more activities after treatment also played a role in success of treatment at 6 months. Regarding self-reported disability, participants with the expectation for complete relief had greater changes in disability over time. We interpret this combination of findings as an indication that positive expectations have a large effect on perceived improvement in the short term, whereas in the longer term and more temporally distant to the initial formulation of expectations for the treatment, the ambivalent or negative outlook had a larger effect.
Our findings in this study disagree with those of Kalauokalani et al,13 who indicated that general optimism about treatment for low back pain was not associated with changes in self-report disability. However, expectations for a specific intervention had a strong influence in that study on outcome. The participants who volunteered for that study had varied specific expectations for the interventions used; that is, some participants believed that acupuncture would be beneficial but not massage, and vice versa.
In our current study, participants who held the expectation that manipulation would help this episode of neck pain and then received manipulation as part of the intervention showed increased odds of success at 1 month compared to those who did not think that manipulation would be beneficial. This result is in agreement with a recently published study18 that demonstrated that positive expectation for benefit from manipulation is a prognostic factor in determining a favorable outcome (success) when treating patients with neck pain with manipulation to the cervical spine. In contrast, there was no statistical difference between the participants who did or did not believe that manipulation would help this episode of neck pain when considering disability. These data suggest differences in criteria used by the participant to make judgments regarding improvements in neck pain compared to the report of disability.
Our data suggest that holding a low or negative general expectation for complete pain relief before treatment affects outcomes 6 months after treatment. So, what might a practitioner do to enhance or increase expectations? The interaction between the practitioner and patient may provide the ideal opportunity to develop positive general expectations for physical therapy. Consider the education provided to the patient about prognosis and the type of therapy that will be provided. An individual with high pain-related fear, who is experiencing neck pain, may have a negative general expectation about physical therapy and anticipate a poor clinical outcome. An interaction with the physical therapist, during which education is provided to reduce pain-related fear, may result in a more optimistic expectation for improvement, with the potential for improved clinical outcomes due to a positive general expectation.
A limitation to consider in this analysis is that all participants were willing to participate in a randomized trial of interventions for neck pain. Patients who are not participants in a randomized trial may have had very different beliefs and expectations about specific interventions. In addition, we did not perform a detailed interview with participants to determine the extent to which participants were using somatic/regional judgments, for example, manipulation of the neck would provide benefit but manipulation of the thoracic spine would not. Prior work in placebo studies suggests a somatic specificity to pain-relief responses based on participant expectations for relief in one body part but not another. Consequently, there might have been participants who were expecting to have interventions applied to their neck. However, recent work by Puentedura et al18 collected very similar data on expectations regarding manipulation and neck pain. These authors found the expectation that “manipulation will help this episode of pain” to be part of a cluster of findings suggestive of favorable prognosis when the patient received cervical spine manipulation. Potentially, the combination of these findings suggests that patients may not differentiate the cervical and upper thoracic spine when considering expectations of benefit.
Additionally, there was a relatively small number of participants who did not believe in manipulation but received the intervention. However, the study was powered enough to find significant effects related to the matched variable. Another limitation of the present study is that therapist expectations or beliefs toward the interventions were not collected in the primary study.
CONCLUSION
In summary, patients with neck pain had high general expectations for physical therapy. Most patients specifically expected manual therapy and exercise to be beneficial treatments for neck pain. Patients with low general expectations for pain relief had worse outcomes at 6 months than patients who expected complete pain relief. Expectations for manipulation as a specific intervention provided during treatment increased short-term odds of success and long-term changes in disability in this study.
KEY POINTS.
FINDINGS: High general expectation of benefit from treatment was related to better short-term outcomes. Low general expectation was related to worse long-term outcomes. These findings were independent of the interventions provided.
IMPLICATIONS: Patient expectations prior to starting treatment for neck pain are important to assess when planning interventions for neck pain.
CAUTION: These data were collected from patients willing to participate in a randomized trial of interventions.
Acknowledgments
This work was supported by the Foundation for Physical Therapy and the Orthopaedic Section of the American Physical Therapy Association. Dr Bishop received support from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (K01AR054331) and Dr Bialosky received support from the K12 Rehabilitation Research Career Development Program (5K12HD055929-02).
Footnotes
LEVEL OF EVIDENCE: Prognosis, level 2b-.
The authors certify that they have no affiliations with or financial involvement in any organization or entity with a direct financial interest in the subject matter or materials discussed in the article.
REFERENCES
- 1.Benedetti F, Pollo A, Lopiano L, Lanotte M, Vighetti S, Rainero I. Conscious expectation and unconscious conditioning in analgesic, motor, and hormonal placebo/nocebo responses. J Neurosci. 2003;23:4315–4323. doi: 10.1523/JNEUROSCI.23-10-04315.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bishop MD, Bialosky JE, Cleland JA. Patient expectations of benefit from common interven tions for low back pain and effects on outcome: secondary analysis of a clinical trial of manual therapy interventions. J Man Manip Ther. 2011;19:20–25. doi: 10.1179/106698110X12804993426929. http://dx.doi.org/10.1179/106698110X12804993426929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brody H, Colloca L, Miller FG. The placebo phenomenon: implications for the ethics of shared decision-making. J Gen Intern Med. 2012;27:739–742. doi: 10.1007/s11606-011-1977-1. http://dx.doi.org/10.1007/s11606-011-1977-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Childs JD, Cleland JA, Elliott JM, et al. Neck pain: clinical practice guidelines linked to the International Classification of Functioning, Disability, and Health from the Orthopaedic Section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2008;38:A1–A34. doi: 10.2519/jospt.2008.0303. http://dx.doi.org/10.2519/jospt.2008.0303. [DOI] [PubMed] [Google Scholar]
- 5.Cleland JA, Childs JD, Whitman JM. Psycho-metric properties of the Neck Disability Index and Numeric Pain Rating Scale in patients with mechanical neck pain. Arch Phys Med Rehabil. 2008;89:69–74. doi: 10.1016/j.apmr.2007.08.126. http://dx.doi.org/10.1016/j.apmr.2007.08.126. [DOI] [PubMed] [Google Scholar]
- 6.Cleland JA, Fritz JM, Whitman JM, Palmer JA. The reliability and construct validity of the Neck Disability Index and Patient Specific Functional Scale in patients with cervical radiculopathy. Spine (Phila Pa 1976) 2006;31:598–602. doi: 10.1097/01.brs.0000201241.90914.22. http://dx.doi.org/10.1097/01.brs.0000201241.90914.22. [DOI] [PubMed] [Google Scholar]
- 7.Cleland JA, Mintken PE, Carpenter K, et al. Examination of a clinical prediction rule to identify patients with neck pain likely to benefit from thoracic spine thrust manipulation and a general cervical range of motion exercise: multi-center randomized clinical trial. Phys Ther. 2010;90:1239–1250. doi: 10.2522/ptj.20100123. http://dx.doi.org/10.2522/ptj.20100123. [DOI] [PubMed] [Google Scholar]
- 8.Diatchenko L, Nackley AG, Slade GD, Fillingim RB, Maixner W. Idiopathic pain disorders – pathways of vulnerability. Pain. 2006;123:226–230. doi: 10.1016/j.pain.2006.04.015. http://dx.doi.org/10.1016/j.pain.2006.04.015. [DOI] [PubMed] [Google Scholar]
- 9.Fischer D, Stewart AL, Bloch DA, Lorig K, Laurent D, Holman H. Capturing the patient's view of change as a clinical outcome measure. JAMA. 1999;282:1157–1162. doi: 10.1001/jama.282.12.1157. [DOI] [PubMed] [Google Scholar]
- 10.Fritz JM, George SZ. Identifying psychosocial variables in patients with acute work-related low back pain: the importance of fear-avoidance beliefs. Phys Ther. 2002;82:973–983. [PubMed] [Google Scholar]
- 11.Hirsh AT, George SZ, Bialosky JE, Robinson ME. Fear of pain, pain catastrophizing, and acute pain perception: relative prediction and timing of assessment. J Pain. 2008;9:806–812. doi: 10.1016/j.jpain.2008.03.012. http://dx.doi.org/10.1016/j.jpain.2008.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Institute of Medicine . Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. The National Academies Press; Washington, DC: 2011. [PubMed] [Google Scholar]
- 13.Kalauokalani D, Cherkin DC, Sherman KJ, Koepsell TD, Deyo RA. Lessons from a trial of acupuncture and massage for low back pain: patient expectations and treatment effects. Spine (Phila Pa 1976) 2001;26:1418–1424. doi: 10.1097/00007632-200107010-00005. [DOI] [PubMed] [Google Scholar]
- 14.Kamper SJ, Maher CG, Mackay G. Global rating of change scales: a review of strengths and weaknesses and considerations for design. J Man Manip Ther. 2009;17:163–170. doi: 10.1179/jmt.2009.17.3.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leeuw M, Goossens ME, Linton SJ, Crombez G, Boersma K, Vlaeyen JW. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med. 2007;30:77–94. doi: 10.1007/s10865-006-9085-0. http://dx.doi.org/10.1007/s10865-006-9085-0. [DOI] [PubMed] [Google Scholar]
- 16.Linton SJ. Do psychological factors increase the risk for back pain in the general population in both a cross-sectional and prospective analysis? Eur J Pain. 2005;9:355–361. doi: 10.1016/j.ejpain.2004.08.002. http://dx.doi.org/10.1016/j.ejpain.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 17.Mahomed NN, Liang MH, Cook EF, et al. The importance of patient expectations in predicting functional outcomes after total joint arthroplasty. J Rheumatol. 2002;29:1273–1279. [PubMed] [Google Scholar]
- 18.Puentedura EJ, Cleland JA, Landers MR, Mintken PE, Louw A, Fernández-de-las-Peñas C. Development of a clinical prediction rule to identify patients with neck pain likely to benefit from thrust joint manipulation to the cervical spine. J Orthop Sports Phys Ther. 2012;42:577–592. doi: 10.2519/jospt.2012.4243. http://dx.doi.org/10.2519/jospt.2012.4243. [DOI] [PubMed] [Google Scholar]
- 19.Thompson AG, Sunol R. Expectations as determinants of patient satisfaction: concepts, theory and evidence. Int J Qual Health Care. 1995;7:127–141. doi: 10.1093/intqhc/7.2.127. [DOI] [PubMed] [Google Scholar]
- 20.Turner JA, Ersek M, Kemp C. Self-efficacy for managing pain is associated with disability, depression, and pain coping among retirement community residents with chronic pain. J Pain. 2005;6:471–479. doi: 10.1016/j.jpain.2005.02.011. http://dx.doi.org/10.1016/j.jpain.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 21.United States Congress Patient Protection and Affordable Care Act: Title III, Subtitle F. Public Law. 2010:111–148. [Google Scholar]
- 22.Vlaeyen JW, Kole-Snijders AM, Boeren RG, van Eek H. Fear of movement/(re)injury in chronic low back pain and its relation to behavioral performance. Pain. 1995;62:363–372. doi: 10.1016/0304-3959(94)00279-N. [DOI] [PubMed] [Google Scholar]
- 23.Waddell G. Biopsychosocial analysis of low back pain. Baillieres Clin Rheumatol. 1992;6:523–557. doi: 10.1016/s0950-3579(05)80126-8. [DOI] [PubMed] [Google Scholar]