Abstract
AIM:
To investigate blood groups and the other possible risk factors for preeclampsia among Sudanese women.
MATERIAL AND METHODS:
A case – control study was conducted at Saad Abualila Hospital, Khartoum, Sudan during the period of July 2013 through December 2014. The cases were women with preeclampsia and healthy pregnant women were the controls.
RESULTS:
Two hundred eighty pregnant women were enrolled (140 in each arm of the study). Around one-quarter of all women (280) were primiparae (74.0, 26.4%), the majority were housewives (201, 71.7%). Seventy-nine (28.2%) were illiterate or had no informal education. Around half of the women (130, 46.4%) had O blood group. Binary logistic regression showed association between preeclampsia and lack of antenatal care (OR = 2.75, 95% CI = 1.172–6.494, P = 0.020) as well as O blood group (OR = 1.78, 95% CI = 1.088–2.934, P=0.022).
CONCLUSION:
The current study showed that women with blood group O were at higher risk of preeclampsia.
Keywords: Preeclampsia, blood groups, Sudan, pregnancy
Introduction
Preeclampsia is a common complication of pregnancy, where its incidence is approximately one tenth of births [1]. It is a major cause of increased maternal and perinatal fatality worldwide [2]. The definite aetiology of preeclampsia remains ambiguous, nevertheless, previous researchers have delineated a number of risk factors including low education, primiparity, family history of hypertension, obesity, younger or advanced maternal age, and the ethnic background [3–7].
Some biochemical and haematological factors such as serum creatinine level, serum uric acid level, anaemia were also considered as predictors of preeclampsia [8, 9]. A Proper understanding of epidemiological and clinical risk factors of preeclampsia is essential for earlier diagnoses and follow-up of women at higher risk of this disease. Most published researches on preeclampsia were carried at good resource settings with only a few exceptions [3].
Previous researchers exploring blood group in women with preeclampsia revealed different findings [10]. While some studies reported the associations of different blood groups with preeclampsia, other studies failed to reach similar conclusions [11–15]. There are an extremely high maternal mortality and morbidity in Sudan, where 4.2% out of all obstetric complications and about one fifth of maternal deaths are attributed to preeclampsia/eclampsia [16–18].
The current study was carried out to assess the possible risk factors for preeclampsia including blood groups. The data obtained is of paramount importance for the health planners, health providers, and supports the previous research on preeclampsia in Sudan [19–22].
Material and Methods
A case – control study was conducted at Saad Abualila Hospital, Khartoum, Sudan. Saad Abualila Hospital is a tertiary care hospital for women who attended the prenatal care at the hospital as well as for referrals from the other clinics and hospitals. All women with high-risk pregnancy or obstetric/medical complications are referred to the hospital. Medical files were reviewed for the women during the period of July 2013 through December 2014. A case was defined as a woman who had preeclampsia, which was defined as hypertension associated with proteinuria in a pregnant woman. Hypertension was defined as blood pressure ≥ 140 mmHg systolic or diastolic blood pressure ≥ 90 mmHg diastolic emerging after 20 weeks of gestation in a woman who was normotensive before this period. Proteinuria was defined as excretion of ≥ 300 mg of protein in 24 h urine sample or ≥ 2+ on the dipstick. A consecutive file for each case was taken as control. The controls were pregnant women presented for delivery, with blood pressure values < 139/89 mmHg and no proteinuria recorded in the pregnant health card during the antenatal visits or at the time of delivery. Women with a twin pregnancy or diabetics were excluded because these are known predictors for preeclampsia [7].
The obstetric and medical history (age, parity, education, antenatal care, weight and height) were extracted from the files. Weight and height were used to calculate the body mass index, which was expressed as weight in kg/height in m^2. Blood groups subtypes were recorded from the files of both the cases and the controls and expressed as O, A, B and AB.
A total sample size of 145 participants in each arm of the study was calculated to investigate the difference rate of the O blood group in the women with preeclampsia and the controls. We assumed the rate of O blood as 56% and 40% for preeclampsia women and the controls depending on our previous work in the same setting [22]. This rate would provide 80% power to detect a 5% difference at α = 0.05, with an assumption that complete data might not be available for 12% of participants.
Statistics
SPSS for Windows (version 16.0) was used for data analyses. Studied variables were described with means (M) and standard deviations (SD). Proportions of the studied groups were expressed in percentages (%). The difference of mean (SD) and proportion was compared between the two studied groups using T-test and χ2, respectively. Binary logistic regression analyses were performed, where preeclampsia was the dependent variable and medical/obstetrics characteristics (age, parity, and residence), blood groups (O vs. non-O blood group), BMI were the independent variables. Odds ratio and 95% CI were calculated. P < 0.05 was considered statistically significant.
Ethics
The study received ethical clearance from the Research Board at the Department of Obstetrics and Gynaecology, Faculty of Medicine, University of Khartoum, Sudan
Results
Two hundred eighty pregnant women were enrolled (140 in each arm of the study). Around one-quarter of all women (280) were primiparae (74.0, 26.4%), the majority were housewives (201, 71.7%). Seventy-nine (28.2%) were illiterate or had no informal education. Around half of these women (130, 46.4%) had O blood group.
There was no significant difference in the mean (SD) of the age, parity and BMI between women with preeclampsia and controls. Thirty-six (12.9%) and 104 (37.1) were severe and mild preeclampsia, respectively. Compared with the controls, significantly higher numbers of women with preeclampsia were illiterate and had O blood group, (Table 1, Fig. 1).
Table 1.
Comparing the obstetrics and clinical characteristics of preeclamptic and controls women at Khartoum, Sudan
| Variable | Preeclampsia (n = 140) | Controls (n = 140) | P |
|---|---|---|---|
| The mean (SD) | |||
| Age, year | 28.8 (6.2) | 28.1 (6.0) | 0.315 |
| Parity | 1.7 (2.1) | 1.7 (1.4) | 0.974 |
| Body mass index, Kg/m2 | 24.5 (3.0) | 24.4 (2.2) | 0.648 |
| Number (%) of | |||
| Education < secondary level | 38 (27.1) | 41 (29.3) | 0.410 |
| Lack of antenatal care | 35 (25) | 20 (14.3) | <0.001 |
| O | 86 (61.4) | 64 (45.7) | |
| A | 24 (17.1) | 37 (26.4) | |
| B | 27 (19.3) | 26 (18.6) | 0.007 |
| AB | 3 (2.1) | 13 (9.3) |
Figure 1.
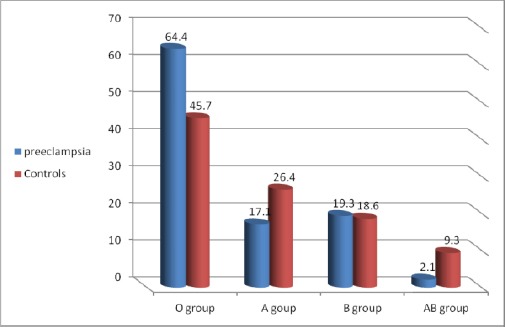
Percentage of blood group among preeclamptic and controls at Khartoum, Sudan
In binary logistic regression, women who had no antenatal care (OR = 2.75, 95%CI = 1.172–6.494, P = 0.020) and women with O blood group (OR = 1.78, 95%CI = 1.088–2.934, P = 0.022) were at higher risk of preeclampsia (Table 2).
Table 2.
Binary logistic regression of the predictors of preeclampsia, Sudan
| Variables | OR | 95%CI | P |
|---|---|---|---|
| Age, year | 1.05 | 1.001─1.113 | 0.048 |
| Parity | 0.88 | 0.739─1.050 | 0.158 |
| Education < secondary level | 1.19 | 0.647─2.203 | 0.571 |
| Lack of antenatal care | 2.75 | 1.172─6.494 | 0.020 |
| Body mass index, Kg/m^2 | 0.98 | 0.897─1.090 | 0.821 |
| O vs. none O blood group | 1.78 | 1.088─2.934 | 0.022 |
Discussion
Perhaps this is the first study investigating the association between blood groups and preeclampsia in Africa. In this study, women who had no antenatal care were more likely to develop preeclampsia than those who had an antenatal follow-up. Previously, Bilano et al. described such a finding in their secondary analysis for the world health organisation facility based, a multi-country survey [23]. An explanation for such an association is the fact that antenatal visits help to detect and treat pregnancy-induced hypertension at an early stage before the development of complications.
An important finding of the current study is the association between blood group O and preeclampsia. This goes with the previous findings, where blood group O has been reported as a risk factor for preeclampsia among 386 cases and 342 controls [24]. Likewise, blood group A has been reported as a risk factor for preeclampsia [15].
A large Swedish cohort study showed that the blood group O is rather protective against preeclampsia [14]. Interestingly, a meta-analysis conducted by Franchini et al. demonstrated that the ABO system was consistently involved in preeclampsia. According to Franchini et al., the non-O blood groups are risk factors while blood group O is protective against preeclampsia [10].
There is a great controversy about whether blood groups could have an association with preeclampsia. Scott et al. found no association between the ABO system and preeclampsia in their case-control study on a population of 46 patients [25]. However, Scott et al. study had relatively small sample size compared with the other studies that established an association between the ABO system and preeclampsia. Scott et al., results are further supported by Witsenburg et al., a report in 36 cases and 272 controls and Clark et al., findings in 4250 pregnancies, 66 of which are preeclamptic women [11, 12]. A separate population-based nested case-control study exploring 248 study cases demonstrated AB blood group as a risk factor for preeclampsia [13].
In conclusion, the current study showed that women with blood group O were at higher risk of preeclampsia.
Footnotes
Funding: This research did not receive any financial support.
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Robillard P-Y, Hulsey TC, Dekker GA, Chaouat G. Preeclampsia and human reproduction. An essay of a long term reflection. J Reprod Immunol. 2003;59(2):93–100. doi: 10.1016/s0165-0378(03)00040-8. http://dx.doi.org/10.1016/S0165-0378(03)00040-8 . [DOI] [PubMed] [Google Scholar]
- 2.Duley L. The global impact of pre-eclampsia and eclampsia. Semin Perinatol. 2009;33(3):130–7. doi: 10.1053/j.semperi.2009.02.010. http://dx.doi.org/10.1053/j.semperi.2009.02.010 . PMid: 19464502. [DOI] [PubMed] [Google Scholar]
- 3.Conde-Agudelo A, Belizan JM. Risk factors for pre-eclampsia in a large cohort of Latin American and Caribbean women. BJOG. 2000;107(1):75–83. doi: 10.1111/j.1471-0528.2000.tb11582.x. http://dx.doi.org/10.1111/j.1471-0528.2000.tb11582.x . PMid: 10645865. [DOI] [PubMed] [Google Scholar]
- 4.Lee C-J, Hsieh T-T, Chiu T-H, Chen K-C, Lo L-M, Hung T-H. Risk factors for pre-eclampsia in an Asian population. Int J Gynecol Obstet. 2000;70(3):327–33. doi: 10.1016/s0020-7292(00)00240-x. http://dx.doi.org/10.1016/S0020-7292(00)00240-X . [DOI] [PubMed] [Google Scholar]
- 5.Roberts JM, Pearson G, Cutler J, Lindheimer M. Summary of the NHLBI Working Group on research on hypertension during pregnancy. Hypertension. 2003;41(3 I):437–45. doi: 10.1161/01.HYP.0000054981.03589.E9. [DOI] [PubMed] [Google Scholar]
- 6.Sibai B, Dekker G, Kupferminc M. Pre-eclampsia. Lancet. 2005;365(9461):785–99. doi: 10.1016/S0140-6736(05)17987-2. http://dx.doi.org/10.1016/S0140-6736(05)71003-5 . [DOI] [PubMed] [Google Scholar]
- 7.Adeyinka DA, Oladimeji O, Adekanbi TI, Adeyinka FE, Falope Y, Aimakhu C. Outcome of adolescent pregnancies in southwestern Nigeria: a case-control study. J Matern Fetal Neonatal Med. 2010;23(8):785–9. doi: 10.3109/14767050903572166. http://dx.doi.org/10.3109/14767050903572166 . PMid: 20082596. [DOI] [PubMed] [Google Scholar]
- 8.Ali AA, Rayis DA, Abdallah TM, Elbashir MI, Adam I. Severe anaemia is associated with a higher risk for preeclampsia and poor perinatal outcomes in Kassala hospital, eastern Sudan. BMC Res Notes. 2011;4(1):311. doi: 10.1186/1756-0500-4-311. http://dx.doi.org/10.1186/1756-0500-4-311 . PMid: 21867566. PMCid: PMC3224576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ndayambagye EB, Nakalembe M, Kaye DK. Factors associated with persistent hypertension after puerperium among women with pre-eclampsia/eclampsia in Mulago hospital, Uganda. BMC Pregnancy Childbirth. 2010;10:12. doi: 10.1186/1471-2393-10-12. http://dx.doi.org/10.1186/1471-2393-10-12 . PMid: 20222993. PMCid: PMC2848130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Franchini M, Mengoli C, Lippi G. Relationship between ABO blood group and pregnancy complications: a systematic literature analysis. Blood Transfus. 2016;1–8 doi: 10.2450/2016.0313-15. PMid: 27483484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Witsenburg CPJ, Rosendaal FR, Middeldorp JM, Van Der Meer FJM, Scherjon SA. Factor VIII levels and the risk of pre-eclampsia, HELLP syndrome, pregnancy related hypertension and severe intrauterine growth retardation. Thromb Res. 2005;115(5):387–92. doi: 10.1016/j.thromres.2004.09.009. http://dx.doi.org/10.1016/j.thromres.2004.09.009 . PMid: 15733972. [DOI] [PubMed] [Google Scholar]
- 12.Clark P, Walker ID, Govan L, Wu O, Greer IA. The GOAL study: A prospective examination of the impact of factor V Leiden and ABO(H) blood groups on haemorrhagic and thrombotic pregnancy outcomes. Br J Haematol. 2008;140(2):236–40. doi: 10.1111/j.1365-2141.2007.06902.x. PMid: 18028481. [DOI] [PubMed] [Google Scholar]
- 13.Hiltunen LM, Laivuori H, Rautanen A, Kaaja R, Kere J, Krusius T, et al. Blood group AB and factor V Leiden as risk factors for pre-eclampsia: A population-based nested case-control study. Thromb Res. 2009;124(2):167–73. doi: 10.1016/j.thromres.2008.11.012. http://dx.doi.org/10.1016/j.thromres.2008.11.012 . PMid: 19110300. [DOI] [PubMed] [Google Scholar]
- 14.Lee BK, Zhang Z, Wikman A, Lindqvist PG, Reilly M. ABO and RhD blood groups and gestational hypertensive disorders: a population-based cohort study. BJOG. 2012 Sep;119(10):1232–7. doi: 10.1111/j.1471-0528.2012.03421.x. http://dx.doi.org/10.1111/j.1471-0528.2012.03421.x . PMid: 22734590. [DOI] [PubMed] [Google Scholar]
- 15.Phaloprakarn C, Tangjitgamol S. Maternal ABO blood group and adverse pregnancy outcomes. J Perinatol. 2013;33(2):107–11. doi: 10.1038/jp.2012.73. http://dx.doi.org/10.1038/jp.2012.73 . PMid: 22678143. [DOI] [PubMed] [Google Scholar]
- 16.Leiberman JR, Fraser D, Kasis A, Mazor M. Reduced frequency of hypertensive disorders in placenta previa. Obstet. Gynecol. 1991;77:83–86. PMid: 1984232. [PubMed] [Google Scholar]
- 17.Ali AA, Adam I. Lack of antenatal care, education, and high maternal mortality in Kassala hospital, eastern Sudan during 2005-2009. J Matern Fetal Neonatal Med. 2011. pp. 1077–8. http://dx.doi.org/10.3109/14767058.2010.545908 . PMid: 21231847. [DOI] [PubMed]
- 18.Ali AA, Okud A, Khojali A, Adam I. High incidence of obstetric complications in Kassala Hospital, Eastern Sudan. J Obstet Gynaecol (Lahore) 2012;32(2):148–9. doi: 10.3109/01443615.2011.637140. http://dx.doi.org/10.3109/01443615.2011.637140 . PMid: 22296425. [DOI] [PubMed] [Google Scholar]
- 19.Bakheit KH, Bayoumi NK, Eltom AM, Elbashir MI, Adam I. Cytokines profiles in Sudanese women with preeclampsia. Hypertens Pregnancy. 2009;28(2):224–9. doi: 10.1080/10641950802601245. http://dx.doi.org/10.1080/10641950802601245 . PMid: 19437232. [DOI] [PubMed] [Google Scholar]
- 20.Bakheit KH, Ghebremeskel K, Pol K, Elbashir MI, Adam I. Erythrocyte omega-3 and omega-6 fatty acids profile in Sudanese women with pre-eclampsia. J Obstet Gynaecol. 2010;30(2):151–4. doi: 10.3109/01443610903391005. http://dx.doi.org/10.3109/01443610903391005 . PMid: 20143974. [DOI] [PubMed] [Google Scholar]
- 21.Bakheit KH, Ghebremeskel K, Zaiger G, Elbashir MI, Adam I. Erythrocyte antioxidant enzymes and plasma antioxidant vitamins in Sudanese women with pre-eclampsia. J Obstet Gynaecol. 2010;30(2):147–50. doi: 10.3109/01443610903249448. http://dx.doi.org/10.3109/01443610903249448 . PMid: 20143973. [DOI] [PubMed] [Google Scholar]
- 22.Adam I, Elhassan EM, Mohmmed A a, Salih MM, Elbashir MI. Malaria and pre-eclampsia in an area with unstable malaria transmission in Central Sudan. Malar J. 2011;10(1):258. doi: 10.1186/1475-2875-10-258. http://dx.doi.org/10.1186/1475-2875-10-258 . PMid: 21899731. PMCid: PMC3224261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bilano VL, Ota E, Ganchimeg T, Mori R, Souza JP. Risk factors of pre-eclampsia/eclampsia and its adverse outcomes in low- and middle-income countries: a WHO secondary analysis. PLoS One. 2014 Jan;9(3):e91198. doi: 10.1371/journal.pone.0091198. http://dx.doi.org/10.1371/journal.pone.0091198 . PMid: 24657964. PMCid: PMC3962376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Amin NS, Tahir SA, Abadi NA, Kubba K. Association of blood groups with preeclamptic toxemia. Med Sci Res. 1989;17:861–2. [Google Scholar]
- 25.Scott JR, Beer AE, Stastny P. Immunogenetic factors in preeclampsia and eclampsia. Erythrocyte, histocompatibility, and Y-dependent antigens. JAMA. 1976;235(4):402–4. http://dx.doi.org/10.1001/jama.1976.03260300028025 . PMid: 54446. [PubMed] [Google Scholar]


