Abstract
BACKGROUND:
Percutaneous transcatheter closure (PTC) of patent foramen ovale (PFO) is implicated in cryptogenic stroke, transitional ischemic attack (TIA) and treatment of a migraine.
AIM:
Our goal was to present our experience in the interventional treatment of PFO, as well as to evaluate the short and mid-term results in patients with closed PFO.
MATERIAL AND METHODS:
Transcatheter closure of PFO was performed in 52 patients (67.3% women, mean age 40.7 ± 11.7 years). Patients were interviewed for subjective grading of the intensity of headaches before and after the PFO closure.
RESULTS:
During 2 years of follow-up, there was no incidence of new stroke, TIA and/or syncope. Follow-up TCD performed in 35 patients showed complete PFO closure in 20 patients (57.1%). Out of 35 patients, 22 (62.9%) reported having a migraine before the procedure with an intensity of headaches at 8.1 ± 1.9 on a scale from 1 to 10. During 2 years of follow-up, symptoms of a migraine disappeared in 4 (18.2%) and the remaining 18 patients reported the significant decrease in intensity 4.8 ± 2.04 (p = 0.0001). In addition, following PFO closure the incidence of the headaches decreased significantly (p = 0.0001).
CONCLUSIONS:
Percutaneous transcatheter closure of PFO is a safe and effective procedure showing mid-term relief of neurological symptoms in patients as well as significant reduction of migraine symptoms.
Keywords: patent foramen ovale, transcatheter closure, cerebrovascular insult, a migraine, interventional closure
Introduction
Patent foramen ovale (PFO) is a tunnel-shaped opening between the atria that helps blood circulate avoiding the lungs during intrauterine life. Most of the PFOs spontaneously close during the first year of life, but some may remain open later in life. In an autopsy study including 965 normal hearts of the general population, the prevalence of PFO was 27.3% with progressive decline as age increases (34.3% in the first three decades, 25.4% in the 4th to 8th decade, and 20.2% in the 9th and 10th decade) [1]. Until recently PFO was thought to be an anatomical variant in different people, however, more and more evidence puts into question the benign nature of this anomaly and the relative importance of the defect is being reevaluated [2-4].
Increasing medical evidence is recognising the PFO as a conduit for a paradoxical embolism resulting in cryptogenic stroke (CS) and transitory ischemic attack (TIA) [5]. There are studies suggesting the connection of PFO with a migraine with aura, orthodeoxia-platypnea and decompression illness in divers [6-8]. The pathophysiology of the neurological events associated with a paradoxical embolism may be due to the direct transfer of venous blood through the PFO into the left heart chambers during increased right heart pressure (Valsalva manoeuvre) [9]. The venous blood contains microthrombi from the lower extremities which are usually filtered through the pulmonary capillaries, “purifying” the blood returning to the left heart chambers before it enters the cerebral vasculature. During activities associated with increased right heart pressure (diving, squatting, coughing) the certain portion of this microthrombi filled blood enters the left heart via PFO and ends up in cerebral arteries causing microinfarcts. These can manifest as stroke, TIA or provoke migraine attacks [10, 11].
Up to 21% of women and 6% of men suffer from migraine attacks and 2/1000 people over 65 years will have an ischemic stroke [12]. Up to one-third of ischemic strokes are “cryptogenic” because the cause cannot be identified. A reason for this cryptogenic stroke could be a paradoxical embolism through a PFO. In younger patients with stroke, a 4-fold greater incidence of PFO has been detected compared to a stroke-free control group of the same age and sex [13]. Co-existence of PFO with certain interatrial septal abnormalities like atrial septal aneurysm (ASA) and Chiari’s network increases the risk of stroke [9, 14-17]. Systematic reviews have suggested the significant association between a migraine and stroke [18], PFO and stroke [19] as well as PFO and migraine [20, 21].
Percutaneous closure of PFO was first described as a derivative from atrial septal defect closure in 1992 [22]. While initial experiences with different devices were disappointing, in 1997 the Amplatzer PFO Occluder was introduced and the interventional technique of transcatheter PFO closure started showing promising results [23]. There are published randomised clinical trials in transcatheter closure of PFO that failed to reach the primary endpoint [23-25]. However, the RESPECT (Randomized Evaluation of Recurrent Stroke Comparing PFO Closure to Established Current Standard of Care Treatment) trial showed a 7-fold higher stroke rate in the on-PFO closure group with extremely low complication rates of the procedure. Sub-analysis showed significant reduction of stroke rate in patients with larger sized PFO and atrial septal aneurysm [26-28]. There are 3 ongoing clinical trials with a total cohort of approximately 1700 patients in France, South Korea and Canada comparing interventional and medical management of PFO.
Close analysis of all published data shows that interventional treatment of PFO is superior to medical treatment in the prevention of stroke and with the new devices and the low complication rate of the procedure one would expect greater implication of transcatheter closure technique for PFO [30].
We set out to examine our experience with PTC treatment of PFO, hypothesising that percutaneous transcatheter closure is a safe and beneficial medical intervention for preventing stroke, TIA and reducing migraine symptoms.
Material and Methods
Between 2011 and 2013, 52 patients underwent PTC of PFO. Stroke was diagnosed in 15 (28.8%), repetitive TIA in 17 (32.7%), repetitive syncope during activities that involved Valsalva manoeuvre in 10 patients (19. 2%), migraine with aura in 7 (13.5%) and without aura in 3 (5. 8%) patients.
All of the patients underwent initial diagnostic testing with TCD. We grouped the positivity of the procedure by the number of bubbles that entered cerebral vasculature after Valsalva manoeuvre. The first group was a very positive test, that is, more than 40 bubbles, the second group was with moderate positivity, from 20 to 39 bubbles, and the third group was with mildly positive transcranial Doppler test, that is, from 1 to 19 bubbles (Fig. 1).
Figure 1.
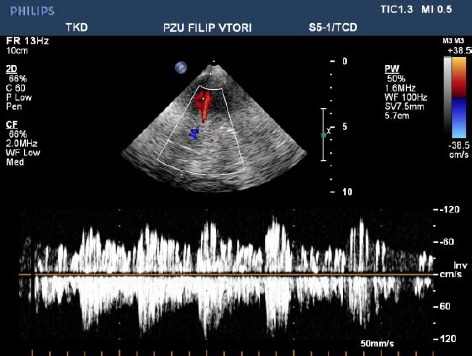
Transcranial doppler ultrasound (TCD) in a patient with large PFO (over 40 bubbles)
The patients with the moderate and severe positivity of TCD who had an indication for PFO closure were further referred for TEE using the agitated saline solution as a contrast, where the presence of PFO was validated and measurements for the size of the device were taken (Fig. 2). Most of our patients had cerebral imaging performed with brain magnetic resonance imaging (MRI) or multislice computerised tomography (MSCT).
Figure 2.

Transesophageal echocardiography (TEE) in a patient with PFO
The transcatheter closure of PFO was performed using local anaesthesia. The patients were informed of the procedure and a written consent was obtained. The PFO was crossed under fluoroscopic guidance through the femoral vein, with 5 F multipurpose catheter and hydrophilic wire, which was exchanged with stiff Amplatz wire. In large PFOs, we used balloon sizing before device implantation. We placed 4 (7.6%) Amplatzer PFO devices and 45 (86.5%) Cera Occluder (Fig. 3). In 3 (5.8%) patients, we implanted an ASD septal occluder, due to a large PFO. All of the patients received a prophylactic dose of antibiotics. Patients were placed on dual antiplatelet therapy with aspirin 100 mg daily and clopidogrel 75 mg daily for 3 months. After 3 months the clopidogrel was discontinued in all patients and aspirin therapy was maintained for an additional 3 months. Endocarditis prophylaxis was recommended for the first 6 months after the procedure. Discharge from the hospital took place one day after the transthoracic (TTE) or TEE examination.
Figure 3.

Percutaneous implantation of a PFO occluder
The patients had echocardiographic follow-up at 7 days, 1 and 6 months after the procedure. Follow-up TCD ultrasound was performed 6 and 24 months after the procedure. We performed electroencephalography (EEG) on all patients before the intervention. During the 2 year follow-up, patients were screened for neurological symptoms and events (CVI, TIA, syncope, migraine) during ambulatory visit according to the up-to-date guidelines of referent professional societies. After the 24 month follow-up period, we did a follow-up TCD, EEG and questionnaire interview for headaches in 35 patients. The remaining 17 patients were either unable or refused to come for follow up appointments and were only screened for neurological receives (TIA, stroke or syncope) according to their official clinical diagnosis by telephone interview. The thirty-five patients were interviewed for migraine severity graduation before and after the procedure. The evaluation was based on a questionnaire with a subjective grading of the intensity of headaches on a scale of 1 to 10, as well as frequency (1-10) of more than 10 attacks per month, and less than one time per month.
The study was approved by our ethics committee and participants signed informed consent documents.
Statistics
Continuous variables are expressed as mean value + SD and categorical variables as counts and percentages. Wilcoxon’s signed rank test was used to compare migraine characteristics before and after percutaneous PFO closure. All data analysis was performed using SPSS version 22.0 (IBM SPSS, Inc., Chicago, Illinois) and a p-value ≤ 0.05 was considered significant.
Results
In 52 patients an occluder was successfully placed using the PTC technique. There were two minor complications (femoral hematoma treated conservatively and hypotension in one patient). We had one patient that complained of chest pain that started 24 hours after the intervention and lasted for a month. We assigned the symptom as a possible side effect of the device implantation.
The follow-up TCD performed in 35 of the patients showed complete PFO closure in 20 (57.1%), whereas 12 patients (34.3 %) had mild (1-19 bubbles) and 3 patients (8.6 %) had moderate (20-39 bubbles) residual shunt. Over the 2 year follow-up, none of the patients had the recurrence of the neurological symptoms represented as CVI, TIA and/or syncope.
From 35 patients that were interviewed, 22 (62.9%) reported having a migraine before the procedure. Subjective grading with the questionnaire showed the average intensity of headaches to be 8.1 ± 1.9, on a scale from 1 to 10 (Table 1). Following the procedure, over a 2 year of follow-up, symptoms of a migraine ceased completely in 4 patients (18.2%) and the remaining 18 (81.8%) patients reported the significant decrease in intensity to 4.8 ± 2.0 (p = 0.0001) (Table 1). As for the frequency of headaches, before the procedure, it was graded as less than one attack per month in 3 patients (13.6%), between 1 and 10 attacks per month in 5 patients (22.7%), and more than 10 attacks per month in 14 patients (63.6%). After the procedure, frequency of headaches decreased significantly with 15 patients (88.2%) having attacks less than once per month, 1 patient (5.9%) having attacks between 1 to 10 times per month, and 1 patient (5.9%) having attacks more than 10 times per month (p = 0.0001) (Table 1).
Table 1.
Comparison of intensity and frequency of the headaches before and after PFO closure
| Before closure | After closure | p Values* | |
|---|---|---|---|
| Migraine intensity (0-10) | 8.14 ± 1.9 | 4.8 ± 2.0 | 0.0001 |
| Frequency of headaches attacks (n/%) | |||
| <1 per month | 3 (13.6%) | 15 (88.2%) | |
| 1-10 per month | 5 (22.7%) | 1 (5.9%) | 0.0001 |
| >10 per month | 14 (63.6%) | 1 (5.9%) |
Before vs. after closure.
In all patients who had EEG before the PFO closure, where findings were normal in 2 (3.8%) of the patients, 20 (38.5%) patients presented with irritative changes, 6 (11.5%) patients had changed with focal activity and paroxysmal discharge was seen in 24 (46.1%) patients. We performed follow-up EEG in 35 of the patients after 24 months of transcatheter closure of the PFO. EEG findings improved in 23 (65.7%) of the patients and in 12 (34.3%) there were no changes in the EEG after the intervention.
Discussion
Whilst CLOSURE I (Evaluation of the STARFlex Septal Closure System in Patients with a Stroke and/or Transient Ischemic Attack due to Presumed Paradoxical Embolism through a Patent Foramen Ovale) [24] as the first randomized trial published on PFO closure showed that closure with a device did not offer a greater benefit than medical therapy alone for the prevention of recurrent stroke or TIA, results of later randomized trials showed that concept of PFO closure to reduce recurrent strokes has been proven [31, 32]. The difference was subjected to mainly shorter fixed 2-year follow-up period and especially lower quality of STARFLex device used in CLOSURE I in comparison to Amplatzer devices used in later studies. The meta-analysis of Stortecky et al. included four randomised trials that included 2963 patients with 9309 patient-years. The Amplatzer device showed superiority compared to the other two devices (STF and HLX) and patients who were allocated to PFO closure with Am player were less likely to experience a stroke than patients on medical therapy [rate ratio (RR) 0.39; 95% CI: 0.17-0.84]. However, PFO closure with any of the three devices showed better probability in preventing stroke compared to medical therapy [29]. The study of Wahl et al. [25] showed that PFO closure performs better than medical treatment. In our study, there was no recurrence of CVI or TIA during a 24-month follow-up period.
The PREMIUM trial (Prospective Randomized Investigation to Evaluate Incidence of Headache Reduction in Subjects With Migraine and PFO Using the AMPLATZER PFO Occluder to Medical Management) was a randomized trial conducted in 29 centers in the United States and enrolled patients between 18 and 64 years of age who had diagnosis of migraine, ranging from 6 to 14 attacks per month, with or without aura. The patients had PFO documented with TCD and their symptoms were unresponsive to medical therapy. A total of 226 patients had the femoral puncture and while some of them received the occluder, the remaining underwent the sham procedure. Patients and neurologist were blinded to the randomization. The results of the trial did not meet the pre-specified primary endpoint of 50% reduction in migraine attack frequency in 117 patients compared to 103 who received a sham procedure and medical management. However, some secondary endpoints did achieve significance and 8.5%-11% of patients had complete migraine remission. Most of the patients who had complete remission had a migraine with aura. The conclusion of the study was that a migraine with aura might need different therapeutic approach than a migraine without aura and that maybe the key to different responses to PFO closure lies in the different anatomies of PFO and adjacent structures [33]. In our study migraine ceased completely in four patients and three of them were with a migraine with aura.
The PRIMA trial (Percutaneous Closure of PFO in Migraine with Aura) was conducted in 20 cities around the world and was prospective, randomised trial that included 107 participants with a migraine with aura who failed medical therapy. Fifty-three of them had PFO closure with Amplatzer device and 54 received medical therapy. PFO closure was associated with the mean reduction of migraine days of -2.9 compared to -1.7 for medical therapy (P = 0.17). There was numerical but not statistical significance. The responder rates were 37.5% for interventional treatment group and 14. 6% for conservative treatment group (P = 0.02). There was a complete resolution of a migraine in 10% of the interventional group compared to 0% in medical therapy group (P < 0.05). However, looking only at patients free of migraine attacks with aura the difference was pronounced with 40% in the PFO closure group and 10% in the control group (P = 0.004). In PRIMA, the reduction of migraine attacks with aura and migraine days with aura was greater than the reduction of all types of migraine attacks and days. Therefore, this unequal and greater effect on migraine with aura is likely a true effect of PFO closure. There was only one vascular major complication and one transient atrial fibrillation reported from the interventional procedure [34].
A Recent meta-analysis conducted by Kent at al. showed that among patients with PFO and cryptogenic stroke, closure reduced recurrent stroke and had statistically significant effect on the composite of stroke, TIA and death in the adjusted analysis [35].
In our study 22 out of 35 patients had migraine attacks. Ten of them went through the procedure only because of a migraine, but 12 had additional CVI, TIA or repetitive syncope. The closure of the PFO significantly reduced the intensity and the frequency of the headaches (Table 1). Four patients (18.2%) reported the complete absence of headaches, while two patients (9%) reported no change in intensity; however, they did report lower frequency of occurrence. The rest of them reported the significant reduction of intensity and frequency.
The interventional procedure of PFO closure is relatively efficient, depending on the type of the occluder used, with a very low complication rate [36-38]. In our experience, we had only two minor complications (3.8%) and no major complications. There was one case of larger hematoma due to a femoral puncture and it was treated conservatively. The second minor complication was a patient with hypotension and confusion after the procedure, which was resolved with intravenous fluids. The follow-up MSCT of the brain showed no new vascular lesions.
The limitations of our study included the use of a non-randomized sample, a small sample size and the possibility of recall bias for the patient-reported symptoms.
In conclusion, in spite of all the published data until today, we still do not have clear evidence-based recommendations for PFO closure [39, 40]. However, with the usage of new devices and recently published studies, PFO closure procedure is more beneficial than harmful. Calculations say that in young people with a life expectancy of 50 years, 2.4 PFOs need to be closed in order to prevent one stroke. The availability of new devices and the very low complication rates of the procedure suggest that perhaps we should be more proactive towards PFO screening and closure. Percutaneous transcatheter closure of PFO is a safe and effective procedure showing mid-term relief of neurological symptoms (CVI, TIA), and significant reduction of migraine symptoms. However, there is a necessity of more studies showing results of long-term follow-up.
Footnotes
Funding: This research did not receive any financial support.
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Hagen PT, Scholz DG, Edwards WD. Incidence and size of patent foramen ovale during the first 10 decades of life: an autopsy study of 965 normal hearts. Mayo Clin Proc. 1984;59(1):17–20. doi: 10.1016/s0025-6196(12)60336-x. http://dx.doi.org/10.1016/S0025-6196(12)60336-X . [DOI] [PubMed] [Google Scholar]
- 2.Seiler C. Patent foramen ovale (PFO): is there life before death in the presence of PFO? Eur J Clin Invest. 2015;45(8):875–882. doi: 10.1111/eci.12469. http://dx.doi.org/10.1111/eci.12469 . PMid: 26017145. [DOI] [PubMed] [Google Scholar]
- 3.Serena J, Jiménez-Nieto M, Silva Y, Castellanos M. Patent foramen ovale in cerebral infarction. Curr Cardiol Rev. 2010;6(3):162–174. doi: 10.2174/157340310791658794. http://dx.doi.org/10.2174/157340310791658794 . PMid: 21804775. PMCid: PMC2994108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kent DM, Thaler DE. Is patent foramen ovale a modifiable risk factor for stroke recurrence? Stroke. 2010;41(10 Suppl):S26–S30. doi: 10.1161/STROKEAHA.110.595140. http://dx.doi.org/10.1161/STROKEAHA.110.595140 . PMid: 20876498. PMCid: PMC2954503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mirzaali M, Dooley M, Wynne D, Cooter N, Lee L, Haworth P, Saha R, Gainsborough N, Hildick-Smith D. Patent foramen ovale closure following cryptogenic stroke or transient ischaemic attack: Long-term follow-up of 301 cases. Catheterization and Cardiovascular Interventions. 2015;86(6):1078–84. doi: 10.1002/ccd.26080. http://dx.doi.org/10.1002/ccd.26080 . PMid: 26105198. [DOI] [PubMed] [Google Scholar]
- 6.Rigatelli G, Dell’avvocata F, Cardaioli P, et al. Improving migraine by means of primary transcatheter patent foramen ovale closure: long-term follow-up. Am J Cardiovasc Dis. 2012;2(2):89–95. PMid: 22720197. PMCid: PMC3371619. [PMC free article] [PubMed] [Google Scholar]
- 7.Smart D, Mitchell S, Wilmshurst P, Turner M, Banham N. Joint position statement on persistent foramen ovale (PFO) and diving. South Pacific Underwater Medicine Society (SPUMS) and the United Kingdom Sports Diving Medical Committee (UKSDMC) Diving Hyperb Med. 2015;45(2):129–131. PMid: 26165538. [PubMed] [Google Scholar]
- 8.Honěk J, Šefc L, Honěk T, Šrámek M, Horváth M, Veselka J. Patent Foramen Ovale in Recreational and Professional Divers: An Important and Largely Unrecognized Problem. Can J Cardiol. 2015;31(8):1061–1066. doi: 10.1016/j.cjca.2015.03.010. http://dx.doi.org/10.1016/j.cjca.2015.03.010 . PMid: 26143138. [DOI] [PubMed] [Google Scholar]
- 9.Overell JR, Bone I, Lees KR. Interatrial septal abnormalities and stroke: a meta-analysis of case-control studies. Neurology. 2000;55(8):1172–1179. doi: 10.1212/wnl.55.8.1172. http://dx.doi.org/10.1212/WNL.55.8.1172 . PMid: 11071496. [DOI] [PubMed] [Google Scholar]
- 10.Kent DM, Dahabreh IJ, Ruthazer R, et al. Anticoagulant vs. antiplatelet therapy in patients with cryptogenic stroke and patent foramen ovale: an individual participant data meta-analysis. Eur Heart J. 2015. Jul, http://dx.doi.org/10.1093/eurheartj/ehv252 . PMid: 26141397. PMCid: PMC4568404. [DOI] [PMC free article] [PubMed]
- 11.Tobis J, Mojadidi, Khessali Levinson R, Tobis J. Visual migraine aura with or without headache: association with right to left shunt and assessment following transcutaneous closure. Clin Ophthalmol. 2012. p. 1099. http://dx.doi.org/10.2147/OPTH.S30999 . PMid: 22888208. PMCid: PMC3413347. [DOI] [PMC free article] [PubMed]
- 12.Guidetti D, Rota E, Morelli N, Immovilli P. Migraine and stroke: “vascular” comorbidity. Front Neurol. 2014;5:193. doi: 10.3389/fneur.2014.00193. http://dx.doi.org/10.3389/fneur.2014.00193 . PMid: 25339937. PMCid: PMC4189436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Manuscript A. NIH Public Access. Changes. 2012;29(6):997–1003. [Google Scholar]
- 14.Homma S, Sacco RL, Di Tullio MR, Sciacca RR, Mohr JP. Atrial anatomy in non-cardioembolic stroke patients: effect of medical therapy. J Am Coll Cardiol. 2003;42(6):1066–1072. doi: 10.1016/s0735-1097(03)00907-0. http://dx.doi.org/10.1016/S0735-1097(03)00907-0 . [DOI] [PubMed] [Google Scholar]
- 15.Fox ER, Picard MH, Chow C-M, Levine RA, Schwamm L, Kerr AJ. Interatrial septal mobility predicts larger shunts across patent foramen ovales: An analysis with transmitral Doppler scanning. Am Heart J. 2003;145(4):730–736. doi: 10.1067/mhj.2003.5. http://dx.doi.org/10.1067/mhj.2003.5 . PMid: 12679772. [DOI] [PubMed] [Google Scholar]
- 16.Davis D, Gregson J, Willeit P, Stephan B, Al-Shahi Salman R, Brayne C. Patent Foramen Ovale, Ischemic Stroke and Migraine: Systematic Review and Stratified Meta-Analysis of Association Studies. Neuroepidemiology. 2013;40(1):56–67. doi: 10.1159/000341924. http://dx.doi.org/10.1159/000341924 . PMid: 23075508. PMCid: PMC3707011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meschia JF, Bushnell C, Boden-Albala B, et al. Guidelines for the Primary Prevention of Stroke: A Statement for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2014;45(12):3754–3832. doi: 10.1161/STR.0000000000000046. http://dx.doi.org/10.1161/STR.0000000000000046 . PMid: 25355838. PMCid: PMC5020564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schürks M, Rist PM, Bigal ME, Buring JE, Lipton RB, Kurth T. Migraine and cardiovascular disease: systematic review and meta-analysis. BMJ. 2009;339:b3914. doi: 10.1136/bmj.b3914. http://dx.doi.org/10.1136/bmj.b3914 . PMid: 19861375. PMCid: PMC2768778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alsheikh-Ali AA, Thaler DE, Kent DM. Patent foramen ovale in cryptogenic stroke: incidental or pathogenic? Stroke. 2009;40(7):2349–2355. doi: 10.1161/STROKEAHA.109.547828. http://dx.doi.org/10.1161/STROKEAHA.109.547828 . PMid: 19443800. PMCid: PMC2764355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schwedt TJ, Demaerschalk BM, Dodick DW. Patent foramen ovale and migraine: a quantitative systematic review. Cephalalgia. 2008;28(5):531–540. doi: 10.1111/j.1468-2982.2008.01554.x. http://dx.doi.org/10.1111/j.1468-2982.2008.01554.x . PMid: 18355348. [DOI] [PubMed] [Google Scholar]
- 21.Wahl A, Praz F, Tai T, et al. Improvement of migraine headaches after percutaneous closure of patent foramen ovale for secondary prevention of paradoxical embolism. Heart. 2010;96(12):967–973. doi: 10.1136/hrt.2009.181156. http://dx.doi.org/10.1136/hrt.2009.181156 . PMid: 20538672. [DOI] [PubMed] [Google Scholar]
- 22.Bridges ND, Hellenbrand W, Latson L, Filiano J, Newburger JW, Lock JE. Transcatheter closure of patent foramen ovale after presumed paradoxical embolism. Circulation. 1992;86(6):1902–1908. doi: 10.1161/01.cir.86.6.1902. http://dx.doi.org/10.1161/01.CIR.86.6.1902 . PMid: 1451261. [DOI] [PubMed] [Google Scholar]
- 23.Meier B. Patent foramen ovale and closure technique with the amplatzer occluder. Scientifica 2014. 2014 doi: 10.1155/2014/129196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Furlan AJ, Reisman M, Massaro J, et al. for the CLOSURE I Investigators. Closure or medical therapy for cryptogenic stroke with patent foramen ovale. N Engl J Med. 2012;366(11):991–999. doi: 10.1056/NEJMoa1009639. http://dx.doi.org/10.1056/NEJMoa1009639 . PMid: 22417252. [DOI] [PubMed] [Google Scholar]
- 25.Meier B, Kalesan B, Mattle HP, et al. Percutaneous closure of patent foramen ovale in cryptogenic embolism. N Engl J Med. 2013;368(12):1083–1091. doi: 10.1056/NEJMoa1211716. http://dx.doi.org/10.1056/NEJMoa1211716 . PMid: 23514285. [DOI] [PubMed] [Google Scholar]
- 26.Carroll JD, Saver JL, Thaler DE, et al. Closure of patent foramen ovale versus medical therapy after cryptogenic stroke. N Engl J Med. 2013;368(12):1092–1100. doi: 10.1056/NEJMoa1301440. http://dx.doi.org/10.1056/NEJMoa1301440 . PMid: 23514286. [DOI] [PubMed] [Google Scholar]
- 27.Hammerstingl C, Bauriedel B, Stüsser C, et al. Risk and fate of residual interatrial shunting after transcatheter closure of patent foramen ovale: a long term follow up study. Eur J Med Res. 2011;16(1):13–19. doi: 10.1186/2047-783X-16-1-13. http://dx.doi.org/10.1186/2047-783X-16-1-13 . PMid: 21345765. PMCid: PMC3351944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Saver JL, Thaler DE, Smalling RW, et al. Qualifying and Outcome Strokes in the RESPECT PFO Trial: Additional Evidence of Treatment Effect Disclosure Statement of Financial Interest [Google Scholar]
- 29.Stortecky S, da Costa BR, Mattle HP, et al. Percutaneous closure of patent foramen ovale in patients with cryptogenic embolism: a network meta-analysis. Eur Heart J. 2015;36(2):120–128. doi: 10.1093/eurheartj/ehu292. http://dx.doi.org/10.1093/eurheartj/ehu292 . PMid: 25112661. [DOI] [PubMed] [Google Scholar]
- 30.Nietlispach F, Meier B. Percutaneous closure of patent foramen ovale: safe and effective but underutilized. Expert Rev Cardiovasc Ther. 2015;13(2):121–123. doi: 10.1586/14779072.2015.1000305. http://dx.doi.org/10.1586/14779072.2015.1000305 . PMid: 25556896. [DOI] [PubMed] [Google Scholar]
- 31.Tobis J, Shenoda M. Percutaneous treatment of patent foramen ovale and atrial septal defects. J Am Coll Cardiol. 2012;60(18):1722–1732. doi: 10.1016/j.jacc.2012.01.086. http://dx.doi.org/10.1016/j.jacc.2012.01.086 . PMid: 23040567. [DOI] [PubMed] [Google Scholar]
- 32.Elmariah S, Furlan AJ, Reisman M, et al. Predictors of recurrent events in patients with cryptogenic stroke and patent foramen ovale within the CLOSURE I (Evaluation of the STARFlex Septal Closure System in Patients With a Stroke and/or Transient Ischemic Attack Due to Presumed Paradoxical Embol. JACC Cardiovasc Interv. 2014;7(8):913–920. doi: 10.1016/j.jcin.2014.01.170. http://dx.doi.org/10.1016/j.jcin.2014.01.170 . PMid: 25147037. [DOI] [PubMed] [Google Scholar]
- 33.57th Annual Scientific Meeting |American Headache Society. [Accessed August 23 2015]. http://www.americanheadachesociety.org/events/57th_annual_scientific_meeting/ [DOI] [PubMed]
- 34.Mattle HP, Evers S, Hildick-Smith D, et al. Percutaneous closure of patent foramen ovale in migraine with aura, a randomized controlled trial. Eur Heart J. 2016;37:2029–36. doi: 10.1093/eurheartj/ehw027. http://dx.doi.org/10.1093/eurheartj/ehw027 . PMid: 26908949. [DOI] [PubMed] [Google Scholar]
- 35.Kent DM, Dahabreh IJ, Ruthazer R, et al. Device closure of patent foramen ovale after stroke: Pooled analysis of completed randomized trials. J Am Coll Cardiol. 2016;67(8):907–17. doi: 10.1016/j.jacc.2015.12.023. http://dx.doi.org/10.1016/j.jacc.2015.12.023 . PMid: 26916479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Meier B, Frank B, Wahl A, Diener HC. Secondary stroke prevention: Patent foramen ovale, aortic plaque, and carotid stenosis. Eur Heart J. 2012;33(6):705–713. doi: 10.1093/eurheartj/ehr443. http://dx.doi.org/10.1093/eurheartj/ehr443 . PMid: 22422912. PMCid: PMC3303713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mirzada N, Ladenvall P, Hansson PO, Eriksson P, Dellborg M. Multidisciplinary management of patent foramen ovale (PFO) and cryptogenic stroke/TIA. J Multidiscip Healthc. 2013;6:357–363. doi: 10.2147/JMDH.S46890. http://dx.doi.org/10.2147/JMDH.S46890 . PMid: 24082787. PMCid: PMC3785383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Van de Bruaene A, Stroobants D, Benit E. Percutaneous closure of inter-atrial communications (atrial septal defect and patent foramen ovale): single-centre experience and mid-term follow-up. Acta Cardiol. 2015;70(2):133–140. doi: 10.1080/ac.70.2.3073503. PMid: 26148372. [DOI] [PubMed] [Google Scholar]
- 39.Spencer F, a Lopes LC, Kennedy S, a Guyatt G. Systematic review of percutaneous closure versus medical therapy in patients with cryptogenic stroke and patent foramen ovale. BMJ Open. 2014;4(3):e004282. doi: 10.1136/bmjopen-2013-004282. http://dx.doi.org/10.1136/bmjopen-2013-004282 . PMid: 24607561. PMCid: PMC3948581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tanzi A, Onorato E, Casilli F, Anzola GP. Is the search for right-to-left shunt still worthwhile? Acta Neurol Scand. 2015 doi: 10.1111/ane.12456. PMid: 26139358. [DOI] [PubMed] [Google Scholar]


