Abstract
Bordetella pertussis, the causative agent of whooping cough, expresses many virulence factors believed to be involved in infection and disease progression. While these factors as a group are required for infection, deletion of individual virulence factor genes generally has limited effects on the ability of B. pertussis to efficiently infect the respiratory tract of mice, suggesting they may perform noncritical or redundant functions. We have recently observed that a B. pertussis strain, putatively with a mutation of a single gene, brkA, results in a severe defect in vivo. Although BrkA has been shown to be required for B. pertussis to resist complement-mediated killing in vitro, the relevance of these findings to the in vivo role of BrkA during infection has not been examined. Transducing this mutation into multiple wild-type B. pertussis strains allowed us to confirm the in vitro phenotype of reduced resistance to serum complement. All ΔbrkA mutants were increased in their sensitivity to complement in vitro, both in the presence and absence of antibodies. However, these strains differed substantially in their phenotypes in vivo. ΔbrkA mutants of recent clinical isolates were indistinguishable from wild-type strains in their efficient infection of respiratory organs, suggesting that the function of BrkA in these strains is noncritical or redundant. In contrast, multiple ΔbrkA strains derived from Tohama I were severely defective during the first week postinoculation compared to their wild-type parent. This defect was present even in complement-deficient mice, revealing a complement-independent phenotype for the ΔbrkA mutant in respiratory tract infection.
Bordetella pertussis, the causative agent of whooping cough, contains the bvgAS two-component system that controls the expression of many virulence factors, including pertussis toxin, adenylate cyclase, dermonecrotic toxin, filamentous hemagglutinin, fimbriae, pertactin, and BrkA (Bordetella resistance to serum killing) (3, 7, 28). As a group, these bvg-regulated proteins have been shown to be important factors in effective infection and disease progression. B. pertussis mutants locked in the Bvg− phase, in which the expression of multiple virulence factors is decreased, are rapidly cleared from the respiratory tracts of inoculated mice (5, 16), but deletions of single virulence factors have varying, less-severe effects on colonization, suggesting that they may perform noncritical or redundant functions (18).
To survive in the host environment, bacteria must be able to escape killing by numerous host mechanisms, including complement. The various Bordetella species have developed several different mechanisms to resist complement-mediated killing, both in the presence and absence of antibodies. The lipopolysaccharide (LPS) O antigens of Bordetella bronchiseptica and Bordetella parapertussis prevent activation of complement in naive serum (2). Deletion of the locus required for O-antigen assembly results in dramatically increased sensitivity to serum complement in vitro in both species but substantially different phenotypes in vivo; the B. parapertussis mutant was defective but the B. bronchiseptica mutant was not, indicating that in vitro complement resistance does not necessarily correlate with in vivo phenotypes (2).
B. pertussis naturally lacks O antigen, due to an insertion sequence replacing the locus required for its assembly, and is relatively sensitive to killing by naive serum in vitro, although there is a wide range of sensitivity levels observed among different isolates (2, 10, 11, 19, 24). However, even strains that are highly sensitive to serum complement in vitro efficiently infect mice, again reflecting a lack of correlation between in vitro complement sensitivity and in vivo phenotypes (2, 10). Interestingly, B. pertussis appears to have multiple alternative mechanisms to avoid antibody-mediated complement killing in vitro, including the expression of BrkA (1, 7). While BrkA has been implicated in adherence to and invasion of host cells in in vitro assays, its most well studied function is its ability to mediate resistance to human immune serum killing in vitro (6, 7, 15).
BrkA was identified in a transposon insertion screen for bvg-regulated genes (27). A strain with an insertion in the brkA gene was found to require a 10-fold-greater challenge dose to cause lethality in an infant mouse model (7, 26). The brk locus contains two divergently transcribed open reading frames (ORFs), brkA and brkB, with a putative bvgA-binding site between them. BrkA is a 103-kDa autotransporter protein, containing a 73-kDa α-domain, or passenger domain, and a 30-kDa β-domain, which acts as the transporter (20, 21, 25). It is similar in sequence to pertactin, possessing two RGD motifs, an outer membrane localization signal, and a proteolytic cleavage site.
The ΔbrkA mutant strain, RFBP2152, was generated by deleting the internal 229-bp SalI fragment of the brkA gene in B. pertussis strain BP338 and replacing it with a gentamicin resistance-OriT cassette (7). We have recently observed that RFBP2152 is severely defective in mouse lung colonization, being nearly cleared by day 3 postinoculation, whereas wild-type B. pertussis grows to greater than 106 CFU by this time point (23). Considering that BrkA is known to mediate resistance to complement killing and that B. pertussis shows substantial strain variation in serum sensitivity (23), we sought to examine the functions of BrkA in various laboratory strains and recent clinical isolates of B. pertussis. ΔbrkA mutants of four different B. pertussis strains showed increased sensitivity to serum complement in vitro, but only Tohama I derivatives were defective in vivo in the lungs of wild-type and complement-deficient mice. While the function(s) of BrkA appears to be redundant in some recent clinical isolates, these findings indicate that the in vivo function of BrkA in Tohama I-derived strains is independent of its role in complement resistance.
MATERIALS AND METHODS
Bacterial strains and growth.
Table 1 lists bacterial strains used in this study. B. pertussis strains Tohama I, BP338, RFBP2152, and GMT1 have been described elsewhere (8, 12, 16, 17, 27). B. pertussis strain 6068 is an isolate obtained in 1997 from a subject participating in the National Institutes of Health-sponsored multicenter Adult Acellular Pertussis Vaccine Efficacy Trial (APERT) conducted throughout the United States. The study subject was a 29-year-old female with a 7-day persistent cough at the time of culture. All B. pertussis strains were maintained on Bordet-Gengou (BG) agar (Difco) containing 7.5% defibrinated sheep blood (Hema Resources) and appropriate antibiotics (20 μg of gentamicin per ml for all ΔbrkA strains). Liquid culture bacteria were grown to mid-log phase in Stainer-Scholte (SS) broth containing heptakis(2,6-di-O-methyl)-β-cyclodextrin (0.1%; Sigma) and appropriate antibiotics.
TABLE 1.
Bacterial strains used in this study
| B. pertussis strain | Relevant characteristic(s) | Reference or source |
|---|---|---|
| BP338 | Wild type | 27 |
| RFBP2152 | ΔbrkA mutant of BP338, Genr | 8 |
| BP338ΔbrkA | ΔbrkA mutant of BP338, Genr | This study |
| Tohama I | Wild type | 12 |
| TohΔbrkA | ΔbrkA mutant of Tohama I, Genr | This study |
| 6068 | Wild type | 1997 clinical isolate |
| 6068ΔbrkA | ΔbrkA mutant of 6068, Genr | This study |
| GMT1 | Wild type | 16, 17 |
| GMT1ΔbrkA | ΔbrkA mutant of GMT1, Genr | This study |
Phage transduction.
RFBP2152 was grown overnight, and 5 μl of culture was added to 2.5 ml of 0.7% Top Agar at 42 to 45°C. DC3 phage (a gift from Jeff Miller's lab, University of California—Los Angeles) was added in sufficient quantity to cause confluent lysis within 2 days. Lysate was collected by adding 5 ml of SM buffer (0.1M NaCl, 0.008 M MgSO4, 0.05 M Tris-Cl [pH 7.5], 0.01% gelatin) to the plate and incubating for 3 h at 4°C. The resuspended lysate was passed through sterile syringe filters, and the titer was determined by serial dilution, with Tohama I as the test strain. The lysate was then added, at a multiplicity of infection (MOI) of 0.1 to 0.01, to 500 μl of overnight cultures of BP338, 6068, Tohama I, and GMT1 grown to mid-log phase. These mixtures were incubated for 2 h, with 200-μl aliquots taken every 30 min. The cells were spun down at 12,000 × g for 30 s, washed twice with phosphate-buffered saline (PBS), and plated on BG plates containing gentamicin. Transductants were tested for sensitivity to DC3 and confirmed by Western blot analysis.
Western blot analysis.
B. pertussis cultures were grown to an optical density at 600 nm (OD600) of 0.4 to 0.9, and 2 to 3 ml of culture was pelleted by centrifugation. The pellets were resuspended in PBS and frozen at −80°C. Samples were then diluted in sample buffer, boiled for 5 min, and run on a sodium dodecyl sulfate-10% polyacrylamide gel (14). Samples were transferred to a polyvinylidene difluoride (PVDF) membrane (Millipore Immobulon) by a semi-dry transfer at 10 V for 30 min. Blots were probed with heat-inactivated rabbit anti-BrkA antiserum (provided by Alison Weiss) diluted 1:50,000 and horseradish peroxidase-conjugated goat anti-rabbit secondary antibody diluted 1:5,000 (Sigma).
Animal experiments.
C57BL/6 mice were obtained from Jackson laboratories (Bar Harbor, Maine), and C3−/− mice, back-crossed extensively onto a C57BL/6 background, have been described elsewhere and were kind gifts of Rick Wetsel (4). All mice were breed in a Bordetella-free environment. Mice lightly sedated with isofluorane (Abbott Laboratories) were inoculated by pipetting 50 μl of PBS containing 5 × 105 bacteria onto the tip of the external nares. Groups of three or four animals were sacrificed on days 3, 7, 14, and/or 28 postinoculation. Colonization of various organs was quantified by homogenizing each tissue in PBS, plating the tissue onto BG-blood agar containing 20 μg of gentamicin per ml (for TohΔbrkA, 6068ΔbrkA, GMTΔbrkA, BP338ΔbrkA, and RFBP2152) or without antibiotic (for BP338, 6068, GMT1, and Tohama I) and by counting the number of colonies.
Antibodies.
Titers of anti-Bordetella antibodies in sera were determined by enzyme-linked immunosorbent assay (ELISA) with polyvalent anti-mouse secondary antibodies as previously described (5). Specific classes and isotypes of antibodies were determined by using appropriate anti-mouse secondary antibodies (Southern Biotechnology Associates and Pharmingen). Titers were calculated by the endpoint method, with naive mouse serum as the negative control.
Serum resistance assays.
Naïve rabbit serum was obtained from Covance Research Products, Inc., and confirmed to have undetectable levels of anti-Bordetella-specific antibodies by ELISA. Human immune serum was collected from multiple volunteers, immunized as children with whole and/or acellular vaccine. Serum aliquots were stored at −80°C. Bacteria were grown in SS broth to mid-log phase and diluted in 1× PBS or SS broth to a final concentration of 100 CFU/μl. Human immune serum and naïve rabbit serum were thawed on ice. Forty-five microliters of serum, either neat or diluted in 1× PBS to the appropriate concentration, was added on ice to 5 μl of bacteria. Controls were processed in the same manner, except that 45 μl of heat-inactivated rabbit serum diluted in PBS to a final assay concentration of 10% was used in place of the naïve complement active serum. A final concentration of approximately 500 CFU/50 μl in the indicated concentration of serum was used for all experiments. All samples were plated on BG agar plates with appropriate antibiotics and incubated for 3 to 4 days, after which CFU were enumerated. Percent survival was determined as a percentage of controls incubated in PBS. All serum assay experiments were run in triplicate and independently repeated.
RESULTS
RFBP2152 shows a severe colonization defect on day 3 postinoculation.
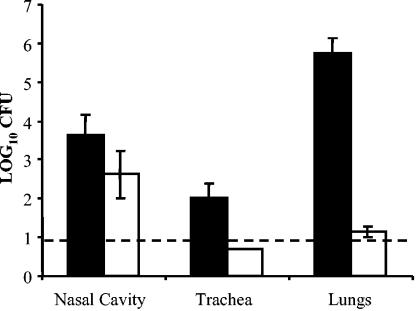
We have recently observed that RFBP2152 does not effectively colonize the respiratory tract of mice and is rapidly cleared (23, 26). The magnitude of this colonization defect is extraordinarily severe for a single virulence factor gene mutation. Such a severe colonization defect in normal adult mice has been observed only for bvgAS mutants, in which the expression of multiple virulence factors is disregulated. Normal colony morphology and growth rate indicate that RFBP2152 is not a bvg mutant. Additionally, the presence of a gentamicin resistance cassette alone cannot account for the defect, as other wild-type B. pertussis strains with a Genr insertion behave normally in vitro and in vivo (unpublished data). In order to determine that the parent strain, Tohama I derivative BP338, was not defective in vivo, groups of C57BL/6 mice were inoculated intranasally with 105 CFU of BP338 or RFBP2152 in a volume of 50 μl of PBS. The respiratory organs were harvested on day 3 postinoculation and homogenized in PBS, and the number of bacteria in the lungs, trachea, and nasal cavity was quantified. BP338 reached levels on the order of 106 CFU in the lungs, 103.5 CFU in the nasal cavity, and 102 CFU in the trachea (Fig. 1). These levels are consistent with those observed with other wildtype B. pertussis strains (13). As previously observed, RFBP2152 was severely defective in colonization of the lungs and trachea (Fig. 1) (23). The inability of RFBP2152 to colonize the lower respiratory tract is apparently not the result of a colonization defect in the parent strain. This in vivo defect is extremely severe for a single virulence factor mutation and suggests that brkA expression is critical during B. pertussis infection but does not rule out the possibility of a second site mutation acquired in the process of deriving the ΔbrkA mutant.
FIG. 1.
Colonization by wild-type B. pertussis, BP338, and the ΔbrkA mutant, RFBP2152, on day 3 postinoculation. Groups of three 4-to 6-week-old C57BL/6 mice were inoculated with 5 × 105 CFU of BP338 (solid bars) or RFBP2152 (open bars) delivered in a 50-μl volume of PBS into the nares. The number of bacteria recovered from the nasal cavity, trachea, and lungs at 3 days postinoculation is expressed as the log10 mean ± the standard error. Dashed line indicates limit of detection.
Recent clinical isolates do not require BrkA for efficient colonization of the murine respiratory tract.
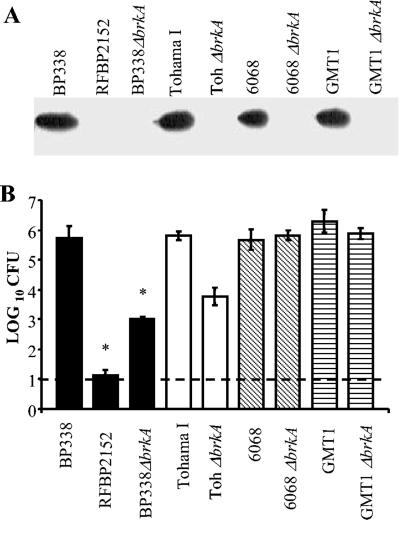
In order to determine whether the large colonization defect of RFBP2152 is due to the ΔbrkA mutation alone or additional mutations in RFBP2152, the original brkA insertion mutation was independently transduced by phage DC3 into the B. pertussis strain Tohama I and the original Tohama I-derived parent strain BP338, producing TohΔbrkA and BP338ΔbrkA, respectively. Additionally, since the serum sensitivity of B. pertussis strains varies greatly and BrkA is thought to function in resisting complement killing, we sought to investigate the function of BrkA in recent clinical isolates (strains not derived from Tohama I). Therefore, the ΔbrkA mutation was also transduced from RFBP2152 into B. pertussis strains 6068 and GMT1. Immunoblots of whole-cell lysates show that TohΔbrkA, BP338ΔbrkA, 6068ΔbrkA, and GMT1ΔbrkA lack the 73-kDa processed BrkA protein present in wild-type B. pertussis (Fig. 2A). Groups of 3 C57BL/6 mice were inoculated with 105 CFU of wild-type and ΔbrkA strains of each isolate and dissected 3 days postinoculation (Fig. 2B). All wild-type strains reached levels on the order of 106 CFU in the lungs. TohΔbrkA and RFBP2152 showed moderate (1/100 of wild-type levels) and severe (1/10,000 of wild-type levels) defects, respectively, in colonization of the lungs. Interestingly, BP338ΔbrkA showed a defect significantly different from that of RFBP2152; however, this defect was not statistically different from that seen in TohΔbrkA. Since the same ΔbrkA mutation is present in both strains, RFBP2152 and BP338ΔbrkA, and each is derived from the same parent strain, these results strongly suggest that RFBP2152 has some additional mutation resulting in a more severe in vivo defect. Interestingly, the ΔbrkA mutants of the recent clinical isolates GMT1 and 6068 efficiently colonized mouse lungs, indicating there may be differential strain-dependent requirement for BrkA-mediated functions, possibly due to a redundant mechanism in the recent clinical isolates.
FIG. 2.
(A) Western blot analysis of wild-type and ΔbrkA strains of B. pertussis. Phage transduction was performed to transfer the ΔbrkA mutation from RFBP2152 into several strains of B. pertussis. Western blot analysis was used to confirm successful transductants, verifying the presence of the 73-kDa processed BrkA protein in wild-type strains BP338, Tohama I, 6068, and GMT1 and its absence in their respective mutants, RFBP2125, BP338ΔbrkA, TohΔbrkA, 6068ΔbrkA, and GMT1ΔbrkA. (B) Colonization by wild-type and ΔbrkA mutants of B. pertussis at 3 days postinoculation. Groups of three 4-to 6-week-old C57BL/6 mice were inoculated with 5 × 105 CFU of BP338, RFBP2152, BP338ΔbrkA, Tohama I, TohΔbrkA, 6068, 6068ΔbrkA, GMT1, or GMT1ΔbrkA delivered in a 50-μl volume of PBS into the nares. The number of bacteria recovered from the lungs at 3 days postinoculation is expressed as the log10 mean ± the standard error. Key statistical differences between groups are indicated (*, P < 0.05). Dashed line indicates limit of detection.
BrkA is involved in resisting both antibody-dependent and -independent complement killing in vitro.
Since BrkA has previously been shown to have a role in resisting complement killing in vitro, it is possible that the strain-dependent severity of the in vivo colonization defect could be attributable to differential serum sensitivity of the ΔbrkA strains. Wild-type and ΔbrkA strains were assayed to determine their sensitivities to various concentrations of naïve rabbit serum (anti-Bordetella antibodies were undetectable by ELISA) for 1 h at 37°C (Fig. 3). Wild-type strains showed significant variation in their serum sensitivity. GMT1 was completely resistant to naive serum at all tested concentrations, while 6068 and Tohama I showed a steady decline in survival with increasing serum concentrations (∼50% survival at 90% serum). BP338 was much more sensitive to naïve serum, with no survival at serum concentrations of 50% and greater. All ΔbrkA mutants showed much greater sensitivity to naïve serum than their wild-type counterparts (Fig. 3). TohΔbrkA, BP338ΔbrkA, and RFBP2152 were completely killed at serum concentrations of 10% and higher. Although both 6068ΔbrkA and GMT1ΔbrkA were much more sensitive than their parental wild-type strains, they both required 50% serum to be completely killed (>99%), suggesting these recent clinical isolates may have some additional protection not shared by Tohama I derivatives. In addition, the magnitude of the defect, relative to the parental strains, was much greater for GMT1ΔbrkA than for 6068ΔbrkA, suggesting there may be additional differences between these isolates. Additional experiments performed using serum from naïve mice and B-cell-deficient mice gave similar results, indicating that killing is indeed antibody independent and not species dependent (data not shown).
FIG. 3.
Naïve serum resistance of wild-type and ΔbrkA mutant strains of B. pertussis at various concentrations of serum. In vitro grown bacteria were diluted to a concentration of 500 CFU/50 μl and treated with various concentrations of naïve rabbit serum for 1 h at 37°C. Serum resistance is expressed as the percentage of bacteria that survived ± the standard error. All samples were run in triplicate, and each strain was tested at least twice.
All of the wild-type and ΔbrkA strains were sensitive to human immune serum, even at very low concentrations (Fig. 4). None survived concentrations of 5% or higher. These results are consistent with human immune serum killing of other Bordetella subspecies, as B. parapertussis is completely killed by 1% immune serum and B. broncheseptica shows no survival at concentrations of 10% serum or higher (2). Mutants lacking BrkA were generally more sensitive at multiple concentrations, and BP338ΔbrkA, RFBP2152, 6068ΔbrkA, and TohΔbrkA were almost completely killed by serum concentrations of 0.05% and greater. These data indicate that BrkA is involved in resisting both antibody-independent and -dependent pathways of complement killing in vitro. Although B. pertussis isolates vary considerably in their sensitivities to complement, the increased sensitivity of all ΔbrkA mutants to both naïve and immune serum confirms the significance of BrkA in this phenotype.
FIG. 4.
Immune serum resistance of wild-type and ΔbrkA mutant strains of B. pertussis at various concentrations of serum. In vitro-grown bacteria were diluted to a concentration of 500 CFU/50 μl and treated with different concentrations of human immune serum for 1 h at 37°C. Serum resistance is expressed as the percentage of bacteria that survived ± the standard error. All samples were run in triplicate, and each strain was tested at least twice.
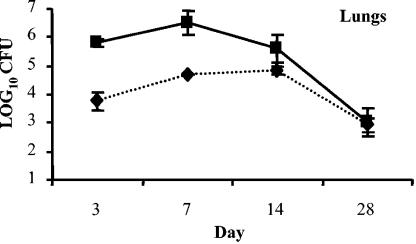
TohΔbrkA is defective early in colonization of wild-type mice.
Since the serum sensitivity assays suggest that the ΔbrkA strains are more sensitive to complement killing both in the presence and absence of antibodies, we hypothesized that the defect in colonization on day 3 postinoculation might persist throughout infection and result in earlier clearance of the bacteria from the lungs. In order to test this possibility, groups of three C57BL/6 mice were inoculated with 5 × 105 CFU of Tohama I or TohΔbrkA and sacrificed on days 3, 7, 14, and 28 days postinoculation, and numbers of bacteria in the lungs were quantified (Fig. 5). The wild-type Tohama I strain was recovered at 100-fold-higher number of CFU than the TohΔbrkA strain on days 3 and 7, though this defect was gone by day 14. ELISA (data not shown) revealed no significant differences in overall antibody production on day 28 between Tohama I and TohΔbrkA-infected mice, suggesting the lack of defect at later time points is not a result of a deficiency in antibody production. The lower number of bacteria only at early time points suggests that BrkA is required prior to substantial antibody production and indicates that resistance to antibody-mediated complement activation is not an important function of BrkA in mice.
FIG. 5.
Colonization by Tohama I and TohΔbrkA in the lungs of wild-type mice. Groups of three 4-to 6-week-old C57BL/6 mice were then inoculated with 5 × 105 CFU of Tohama I (▪) or TohΔbrkA (⧫) delivered in a 50-μl volume of PBS into the nares. The number of bacteria recovered from lungs at each indicated time postinoculation is expressed as the log10 mean ± the standard error.
The function of BrkA in vivo is independent of its role in complement resistance.
Since the severity of the early colonization defect of the Tohama I-derived ΔbrkA strains correlates with their greater susceptibility to naïve serum in vitro, we hypothesized that this colonization defect could be attributable to their greater sensitivity to antibody-independent complement killing in vivo. If this were the case, then in mice deficient in complement component 3 (C3−/− mice), the ΔbrkA strains would colonize at the same level as wild-type B. pertussis. In order to test this, groups of C3−/− mice were inoculated with 105 CFU of BP338, BP338ΔbrkA, Tohama I, or TohΔbrkA and dissected 3 days postinoculation. The lungs of C3−/− mice contained approximately 100-times-more wild-type bacteria than mutant of either background (Fig. 6). The defect of Tohama I-derived ΔbrkA strains in vivo is therefore not attributable to their increased complement sensitivity seen in vitro, since it was observed even in complement-deficient mice. These results reveal an additional, significant role for BrkA in respiratory tract colonization by Tohama I-derived strains.
FIG. 6.
Colonization of wild-type and C3-deficient mice by Tohama I-derived wild-type and ΔbrkA mutants of B. pertussis. Groups of three 4-to 6-week-old C57B1/6 and C3−/− mice were inoculated with 5 × 105 CFU of Tohama I, TohΔbrkA, BP338, or BP338ΔbrkA delivered in a 50-μl volume of PBS into the nares. The number of bacteria recovered from the lungs at 3 days postinoculation is expressed as the log10 mean ± the standard error. Statistical differences between groups are indicated (*, P < 0.05). Dashed line indicates limit of detection.
DISCUSSION
Previous studies have shown significant variance in complement sensitivity between strains of B. pertussis (23). In order to rigorously assess the role of BrkA in resisting complement-mediated killing, the same ΔbrkA mutation was introduced into several different strains. Two well studied laboratory strains, Tohama I and its nalidixic acid-resistant variant, BP338, as well as two recent clinical isolates, 6068 and GMT1, were chosen as representative strains of diverse origins with a wide range of serum sensitivities. Infection studies with wild-type strains and their respective ΔbrkA mutants showed that BrkA is required for efficient colonization of mice by Tohama I-derived strains but does not appear to have a critical role during early infection by recent clinical isolates. This is possibly the result of expression of a compensatory mechanism in both recent isolates, making the function of BrkA redundant in these strains, as has been observed for other Bordetella virulence factors (18).
While previous in vitro studies have shown BrkA to be involved in resisting antibody-dependent complement killing in vitro, our observations suggest this is not a critical function of BrkA during infection of the murine respiratory tract. The defect in colonization of Tohama I-derived ΔbrkA strains was observed on days 3 and 7, when B. pertussis-specific antibodies are undetectable, but was not observed on days 14 and thereafter, when B. pertussis-specific antibodies are readily detectable. The defect of Tohama I-derived ΔbrkA strains at early time points and the fact that B. pertussis is sensitive to antibody-independent complement killing in vitro, lead us to hypothesize that BrkA may be involved in resisting alternative pathway complement killing. Our in vitro experiments were able to confirm earlier reports that BrkA is required for serum resistance in the presence of B. pertussis-specific antibodies but also showed BrkA to be important in the absence of these antibodies (Fig. 3 and 4). Killing of B. pertussis was observed in similar assays performed with naive mouse serum and with serum from B-cell-deficient mice (μMT), confirming, respectively, that this phenotype was not dependent on the species from which the serum was obtained and that killing was independent of antibody presence. Additionally, serum from complement-deficient mice failed to kill any of these strains, indicating that complement, as opposed to antimicrobial peptides, is responsible for the reduction of CFU (data not shown). Together these data indicate that BrkA provides resistance to the antibody-dependent and -independent pathways of complement killing in vitro.
To determine whether this in vitro complement sensitivity could account for the in vivo colonization defect, complement-deficient mice were infected with Tohama I-derived strains and their ΔbrkA mutants. Interestingly, the ΔbrkA strains were still defective, compared with wild-type B. pertussis, in their ability to colonize C3−/− mice, suggesting that the critical function of BrkA in vivo is independent of its effects in resisting complement-mediated lysis. This lack of correlation between in vitro complement sensitivity and in vivo infection ability is not unprecedented (2, 10). All the B. pertussis wild-type strains colonize mice at approximately 106 CFU in the lungs on day 3 postinoculation, despite the fact that they have dramatically different sensitivities to naïve serum at what are thought to be physiologically relevant concentrations (∼10% to 20%) (22). This may be explained by the fact that B. pertussis has been shown to acquire resistance to complement-mediated killing during the first 24 h of infection, even in the absence of BrkA (23).
Previous in vitro studies have described additional putative functions of BrkA, including adherence to and invasion of host cells and resistance to killing by antimicrobial peptides (6, 7, 9). However, these experiments were performed using BP2041, the original Tn5 insertion mutation of brkA in BP338, a strain not analyzed in this study. The results of our study highlight the variability of B. pertussis strains, both in their ability to resist serum complement and in their requirement for BrkA, suggesting the need for a more in-depth examination of the function of BrkA in vitro and in vivo.
Acknowledgments
We thank Jane Pishko for critical reading and editing of the manuscript and Alison Weiss for helpful discussions and providing antibodies.
This work was supported by USDA grant 2002-35204-11684 and NIH grant AI 053075.
Editor: D. L. Burns
REFERENCES
- 1.Barnes, M. G., and A. A. Weiss. 2001. BrkA protein of Bordetella pertussis inhibits the classical pathway of complement after C1 deposition. Infect. Immun. 69:3067-3072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Burns, V. C., E. J. Pishko, A. Preston, D. J. Maskell, and E. T. Harvill. 2003. Role of Bordetella O antigen in respiratory tract infection. Infect. Immun. 71:86-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Charles, I. G., G. Dougan, D. Pickard, S. Chatfield, M. Smith, P. Novotny, P. Morrissey, and N. F. Fairweather. 1989. Molecular cloning and characterization of protective outer membrane protein P.69 from Bordetella pertussis. Proc. Natl. Acad. Sci. USA 86:3554-3558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Circolo, A., G. Garnier, W. Fukuda, X. Wang, T. Hidvegi, A. J. Szalai, D. E. Briles, J. E. Volanakis, R. A. Wetsel, and H. R. Colten. 1999. Genetic disruption of the murine complement C3 promoter region generates deficient mice with extrahepatic expression of C3 mRNA. Immunopharmacology 42:135-149. [DOI] [PubMed] [Google Scholar]
- 5.Cotter, P. A., and J. F. Miller. 1994. BvgAS-mediated signal transduction: analysis of phase-locked regulatory mutants of Bordetella bronchiseptica in a rabbit model. Infect. Immun. 62:3381-3390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ewanowich, C. A., A. R. Melton, A. A. Weiss, R. K. Sherburne, and M. S. Peppler. 1989. Invasion of HeLa 229 cells by virulent Bordetella pertussis. Infect. Immun. 57:2698-2704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fernandez, R. C., and A. A. Weiss. 1994. Cloning and sequencing of a Bordetella pertussis serum resistance locus. Infect. Immun. 62:4727-4738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fernandez, R. C., and A. A. Weiss. 1998. Serum resistance in bvg-regulated mutants of Bordetella pertussis. FEMS Microbiol. Lett. 163:57-63. [DOI] [PubMed] [Google Scholar]
- 9.Fernandez, R. C., and A. A. Weiss. 1996. Susceptibilities of Bordetella pertussis strains to antimicrobial peptides. Antimicrob. Agents. Chemother. 40:1041-1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harvill, E. T., P. A. Cotter, and J. F. Miller. 1999. Pregenomic comparative analysis between Bordetella bronchiseptica RB50 and Bordetella pertussis Tohama I in murine models of respiratory tract infection. Infect. Immun. 67:6109-6118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harvill, E. T., A. Preston, P. A. Cotter, A. G. Allen, D. J. Maskell, and J. F. Miller. 2000. Multiple roles for Bordetella lipopolysaccharide molecules during respiratory tract infection. Infect. Immun. 68:6720-6728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kasuga, T., Y. Nakase, K. Ukishima, and K. Takatsu. 1954. Studies on Haemophilus pertussis. III. Some properties of each phase of H. pertussis. Kitasato Arch. Exp. Med. 27:37-48. [PubMed] [Google Scholar]
- 13.Kirimanjeswara, G. S., P. B. Mann, and E. T. Harvill. 2003. Role of antibodies in immunity to Bordetella infections. Infect. Immun. 71:1719-1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Laemmli, U. K. 1970. Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature 227:680-685. [DOI] [PubMed] [Google Scholar]
- 15.Locht, C., R. Antoine, and F. Jacob-Dubuisson. 2001. Bordetella pertussis, molecular pathogenesis under multiple aspects. Curr. Opin. Microbiol. 4:82-89. [DOI] [PubMed] [Google Scholar]
- 16.Martinez de Tejada, G., P. A. Cotter, U. Heininger, A. Camilli, B. J. Akerley, J. J. Mekalanos, and J. F. Miller. 1998. Neither the Bvg-phase nor the vrg6 locus of Bordetella pertussis is required for respiratory infection in mice. Infect. Immun. 66:2762-2768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martinez de Tejada, G., J. F. Miller, and P. A. Cotter. 1996. Comparative analysis of the virulence control systems of Bordetella pertussis and Bordetella bronchiseptica. Mol. Microbiol. 22:895-908. [DOI] [PubMed] [Google Scholar]
- 18.Mattoo, S., A. K. Foreman-Wykert, P. A. Cotter, and J. F. Miller. 2001. Mechanisms of Bordetella pathogenesis. Front. Biosci. 6:E168-E186. [DOI] [PubMed] [Google Scholar]
- 19.McLafferty, M. A., D. R. Harcus, and E. L. Hewlett. 1988. Nucleotide sequence and characterization of a repetitive DNA element from the genome of Bordetella pertussis with characteristics of an insertion sequence. J. Gen. Microbiol. 134:2297-2306. [DOI] [PubMed] [Google Scholar]
- 20.Oliver, D. C., G. Huang, and R. C. Fernandez. 2003. Identification of secretion determinants of the Bordetella pertussis BrkA autotransporter. J. Bacteriol. 185:489-495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Passerini de Rossi, B. N., L. E. Friedman, F. L. Gonzalez Flecha, P. R. Castello, M. A. Franco, and J. P. Rossi. 1999. Indentification of Bordetella pertussis virulence-associated outer membrane proteins. FEMS Microbiol. Lett. 172:9-13. [DOI] [PubMed] [Google Scholar]
- 22.Persson, C. G. 1991. Plasma exudation in the airways: mechanisms and function. Eur. Respir. J. 4:1268-1274. [PubMed] [Google Scholar]
- 23.Pishko, E. J., D. J. Betting, C. S. Hutter, and E. T. Harvill. 2003. Bordetella pertussis acquires resistance to complement-mediated killing in vivo. Infect. Immun. 71:4936-4942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Preston, A., A. G. Allen, J. Cadisch, R. Thomas, K. Stevens, C. M. Churcher, K. L. Badcock, J. Parkhill, B. Barrell, and D. J. Maskell. 1999. Genetic basis for lipopolysaccharide O-antigen biosynthesis in bordetellae. Infect. Immun. 67:3763-3767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shannon, J. L., and R. C. Fernandez. 1999. The C-terminal domain of the Bordetella pertussis autotransporter BrkA forms a pore in lipid bilayer membranes. J. Bacteriol. 181:5838-5842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weiss, A. A., and M. S. Goodwin. 1989. Lethal infection by Bordetella pertussis mutants in the infant mouse model. Infect. Immun. 57:3757-3764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Weiss, A. A., E. Hewlett, G. A. Myers, and S. Falkow. 1983. Tn5-induced mutations affecting virulence factors of Bordetella pertussis. Infect. Immun. 42:33-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weiss, A. A., and E. L. Hewlett. 1986. Virulence factors of Bordetella pertussis. Annu. Rev. Microbiol. 40:661-686. [DOI] [PubMed] [Google Scholar]