Supplemental Digital Content is Available in the Text.
Patients with chronic widespread pain may regularly consult in primary care for regional pain without being recognized as having a generalized condition.
Keywords: Chronic widespread pain, Electronic health records, Primary care
Abstract
Chronic widespread pain (CWP) is common in the general population. It is unclear how people reporting this problem present in primary care; they may regularly consult for regional pains without being recognized as having a generalized condition. Our objectives were to determine the prevalence of people consulting in primary care for musculoskeletal conditions in different body regions on different occasions (recurrent regional pain consultation), the proportion with diagnosed generalized pain and survey-reported widespread pain, and if they have features characteristic of CWP. Phase 1 used electronic records from 12 general practices in North Staffordshire (Consultations in Primary Care Archive) from 2005 to 2009. Phase 2 used linked self-reported health and primary health care data from 8286 people aged >50 years in 8 general practices (North Staffordshire Osteoarthritis Project) between 2002 and 2005. In Phase 1, 11% of registered patients fulfilled criteria for recurrent regional pain consultation. Three-quarters had no recorded CWP-related generalized pain condition (eg, fibromyalgia). In Phase 2, 53% of recurrent regional pain consulters had survey-reported widespread pain and 88% had consulted for somatic symptoms. Self-reported general health was worse in recurrent regional pain consulters than in single-region consulters and poorest in those who also reported persistent widespread pain. Recurrent regional pain consulters are a heterogeneous group of frequent consulters sharing features with CWP (eg, somatic symptoms) but including those less severely affected. They lie on the spectrum of polysymptomatic distress characteristic of CWP and represent a group whose needs may be better met by earlier diagnosis of multisite pain.
1. Introduction
Chronic widespread pain (CWP) is characterized by long-lasting pain in multiple body regions and is associated with other physical symptoms such as fatigue, concentration problems, and psychologic distress. CWP is common, with an estimated general population point prevalence of 10%.26
In the American College of Rheumatology 1990 (ACR-1990) definition,42 CWP is the fundamental feature of fibromyalgia, defined as pain lasting ≥3 months, located axially, above and below the waist, and on both sides of the body. The updated definition (ACR-2010)41 emphasizes additional physical symptoms (eg, fatigue, waking unrefreshed) associated with fibromyalgia and placed fibromyalgia at one extreme on a spectrum of polysymptomatic distress that includes CWP.
Because of the range of symptoms experienced and a multidisciplinary approach to treatment, it has been argued that fibromyalgia and CWP should be managed in primary care.9,11,12,32,34 However, general practitioners (GPs) may not recognize fibromyalgia as a valid diagnosis,1,6,22,23 may receive inadequate formal training in fibromyalgia,1,7,22 and may have limited awareness of diagnostic criteria.6,7,22 Most UK primary care uses Read codes to summarize patient encounters within electronic records.3,35 There is no Read code for CWP, although the syndrome will be included in the forthcoming International Classification of Diseases, 11th edition.8 However, although a code does exist for fibromyalgia, the disparity between its estimated community and primary care prevalences suggests that the label of fibromyalgia is not often used in general practice.10,16 This may reflect the controversial nature of fibromyalgia and CWP, or concern about the wider implications of labeling.2 Patients fulfilling CWP criteria may instead be diagnosed and treated in primary care for individual regional pains (eg, knee pain), rather than for a generalized pain condition.33
Electronic health records (EHRs) present opportunities to study health care in large cohorts with many years of follow-up. However, using EHR data relies on the definition of robust clinical phenotypes.14 Rohrbeck et al.33 mapped the ACR-1990 CWP criteria to primary care consultation patterns for regional musculoskeletal complaints based on a select number of regional musculoskeletal pain Read codes in one general practice (Box 1). Patients identified using this recurrent regional pain consulter definition consulted for more health problems and reported worse self-reported general health, more sleep problems, and higher levels of fatigue than controls and were concluded to be potentially unrecognized as having a more generalized condition. If GPs do treat the condition presented at each consultation as a regional problem only, then early opportunities for interventions aimed at generalized pain may be missed and long-term disability exacerbated by incomplete management. A consultation-based CWP definition may prompt earlier identification of patients and more timely management. It would also allow estimates of CWP prevalence, health surveillance, and monitoring of trends over time.
Box 1. The recurrent regional pain consulter definition.33.
In a period of 5 consecutive years, a patient fulfils all of 1-4:
At least 1 consultation for a musculoskeletal complaint in the axial skeleton (neck and back);
At least 1 consultation for an upper- or lower-limb complaint;
At least 1 consultation for a regional musculoskeletal complaint in each of 3 separate years;
At least 4 consultations for regional musculoskeletal complaints during the 5-year period.
Building on earlier work,33 our objectives were to (1) determine the prevalence of recurrent regional pain consultation in primary care; (2) assess the extent to which such patients may be underrecognized as having widespread pain; and (3) determine whether they share features characteristic of CWP.
2. Methods
The study consisted of 2 phases. In Phase 1, we used routinely recorded primary care data to investigate prevalence of recurrent consultation for regional pain conditions and determined the overlap with recorded nonspecific generalized pain that may be related to fibromyalgia, to assess the extent to which widespread pain may be unrecognized in UK primary care. In Phase 2, we used linked survey and primary care consultation data to investigate whether patients with recurrent regional pain consultation have survey-reported CWP and have similar characteristics to those self-reporting CWP.
2.1. Phase 1
We used anonymized routinely collected primary care data from general practices contributing to the Consultations in Primary Care Archive (CiPCA) in North Staffordshire, United Kingdom. The North Staffordshire Research Ethics Committee gave ethical approval for the use of the CiPCA database for research (reference 03/04). In the United Kingdom, 98% of the population is registered with a National Health Service (NHS) GP,15 access to care is free, and GPs act as the entry point to all routine health care. Although North Staffordshire is more deprived than the average for England, the practices cover both affluent and deprived areas. Routine clinical data recorded by the practices are regularly audited.30 Prevalence of musculoskeletal conditions in CiPCA has been demonstrated to be similar to that of larger national primary care consultation databases17 and international databases.19 We included the 12 CiPCA practices for which there were complete data for the years 2005 to 2009, with a denominator population base of 79,796 people registered (all ages, with full registration for the 5-year study period).
We used the Read-coded consultation data for this 5-year period to identify: (1) patients fulfilling the original recurrent regional pain consultation algorithm (Box 1) based on a published list of all regional musculoskeletal morbidity codes (n = 4482)20; and (2) individuals recorded with nonspecific (ie, with no clear established underlying diagnosis) generalized pain conditions related to CWP. These included fibromyalgia, fibrositis, rheumatism, myalgia, arthralgia, and polyalgia. The code lists are available from www.keele.ac.uk/mrr. We excluded patients without complete registration; that is, those who were not registered with the same primary care practice for the full 5-year period from 2005 to 2009.
2.1.1. Analysis
We calculated the 5-year recorded prevalence of recurrent regional pain consultation, fibromyalgia, and nonspecific generalized pain and the total prevalence of recurrent regional pain consultation or generalized pain combined. We also recalculated total prevalence (of recurrent regional pain consultation or nonspecific generalized pain combined) after excluding those with specific generalized musculoskeletal diagnoses (ie, rheumatoid arthritis, systemic lupus erythematosus, polymyalgia rheumatica, ankylosing spondylitis, Sjögren's syndrome, and hypothyroidism) during the 5-year period. The denominator population was patients registered with the CiPCA practices between 2005 and 2009. We directly standardized prevalence figures using the UK general population age and sex distribution for 2009 provided by the Office for National Statistics.28
We then calculated the percentage of recurrent regional pain consulters recorded as also consulting for a nonspecific generalized pain complaint and the percentage of nonspecific pain consulters who were also recurrent regional pain consulters.
2.2. Phase 2
The Phase 2 study population was drawn from the North Staffordshire Osteoarthritis Project (NorStOP), a prospective study of pain and general health of all community-dwelling adults aged 50 years and over registered with 8 general practices.37 The North Staffordshire and Hereford and Worcester Research Ethics Committees granted ethical approval for the NorStOP project. We included those who had responded to both baseline and 3-year postal health surveys from the 3 identically recruited and measured cohorts (NorStOP 1: 2002, NorStOP 2: 2003, NorStOP 3: 2004, 2005), had consented to medical record review, and had a minimum of 5 years of medical record data available. Questionnaires were mailed with a letter from the GP practice, accompanied by a study information leaflet, and reminders were sent to nonresponders after 2 and 4 weeks. GPs checked mailing lists before mailing to exclude unsuitable patients (eg, patients with terminal illnesses or dementia). Full details of the study protocol and data collection have been published previously.37
2.2.1. Pain status
We established consultation-based pain status using linked primary care medical record data for the 5-year period starting 2 years before the baseline health questionnaire. We identified those fulfilling the recurrent regional pain consultation algorithm and those consulting for musculoskeletal problems in a single region (recorded as consulting in just one of the 3 defined body regions—axial, upper limb, or lower limb—during the 5-year study period).
Self-reported pain status was collected by postal questionnaire at baseline and 3-year follow-up. A self-completed body manikin was used to establish the location of body pain lasting for ≥1 day in the past 4 weeks. Pain diagrams have been demonstrated to be a reliable means of classifying widespread pain based on existing criteria.24 ACR-1990 widespread pain was defined as axial pain, pain in the left and right sides of the body, and pain above and below the waist.42 Because of the limitations of the self-reported data, we were unable to ascertain chronicity using the ACR-1990 definition of ≥3 months duration. Widespread pain reported at both baseline and 3 years was therefore used as a marker of “persistent” widespread pain. Self-reported widespread pain was classified into 2 categories as: (1) ACR-1990 widespread pain at baseline or 3 years; and (2) ACR-1990 widespread pain at baseline and 3 years (persistent widespread pain).
2.2.2. General health measures
Consultation-based measures were collected from medical records over the 5-year period. These were somatic symptom count, frequent attendance, and musculoskeletal and nonmusculoskeletal consultation counts.
CWP is often associated with additional symptoms such as fatigue and concentration problems. The ACR-2010 fibromyalgia definition41 emphasizes the importance of these somatic symptoms by including them in the fibromyalgia case definition. We identified the number of somatic symptoms (eg, fatigue, insomnia, and nausea) recorded for each patient over the 5-year study period. We used the symptoms itemized in the ACR-2010 fibromyalgia criteria to identify corresponding Read codes.
CWP patients have been found to consult more frequently than patients with no pain, independent of their level of psychological distress,21 suggesting that frequent attendance is a feature of CWP. Research has demonstrated an association between CWP and help-seeking behavior for health problems.13 We defined frequent attender status as being in the top 10% of consulters for nonmusculoskeletal problems over the 5-year period. Frequent attendance defined in this way is also an indirect measure of comorbidity. Nonmusculoskeletal consultations were defined as primary care contacts recorded with any Read code (including numeric chapters 0-9: history, examination, procedural and administrative codes, and chapters A-Z: diagnostic codes) except the musculoskeletal codes.20
We collected self-reported health status from baseline health questionnaire responses. General health was assessed using the 12-item short form health survey (SF-12) physical health component summary score.39 Psychological health was assessed using the anxiety and depression scores of the Hospital Anxiety and Depression Scale (HADS).43 Cognitive impairment was measured using the alertness subscale of the Sickness Impact Profile (SIP).5 Sleep was assessed by 4 questions, in which respondents were asked if they had the following sleep problems on most nights: (1) trouble falling asleep; (2) waking at night; (3) trouble staying asleep; and (4) waking up tired. A positive response to any of the 4 sleep questions was used to indicate a reported sleep problem.
2.2.3. Analysis
We descriptively compared recurrent regional pain consulters, those who consulted for pain in a single region (axial, upper limb, or lower limb), and all respondents with self-reported persistent widespread pain by age, sex, consultation-based health measures, and self-reported health measures. We then determined the positive predictive values of the recurrent regional pain consultation definition for each of the self-reported widespread pain definitions.
For the main analysis, we compared different patterns of pain consultation with self-reported persistent widespread pain status (defined as having ACR-1990 widespread pain at both baseline and 3 years), by consultation-based health measures and self-reported health measures. Specifically, we compared the following 4 mutually exclusive groups of patients: (1) recurrent regional pain consulters who also reported persistent widespread pain; (2) recurrent regional pain consulters who did not report persistent widespread pain (but may have reported widespread pain on either the baseline or the 3-year survey); (3) respondents reporting persistent widespread pain but not meeting the recurrent regional pain consulter definition; and (4) single-region consulters not reporting persistent widespread pain. For this analysis, single-region consulters not reporting persistent widespread pain were the control (reference) group.
We compared these 4 groups on frequent attendance, recording of ≥1 somatic symptoms, reporting ≥1 sleep problems on most nights, SF-12 physical component summary score, SIP cognitive impairment score, and HADS anxiety and depression scores, using logistic or linear regression as appropriate, and adjusting for age and sex.
3. Results
3.1. Phase 1
The 5-year denominator (all ages) in CiPCA was 79,796. Nine thousand one hundred seventy-two patients fulfilled the recurrent regional pain consultation criteria and 6466 patients were recorded with nonspecific generalized pain conditions.
3.1.1. Prevalence
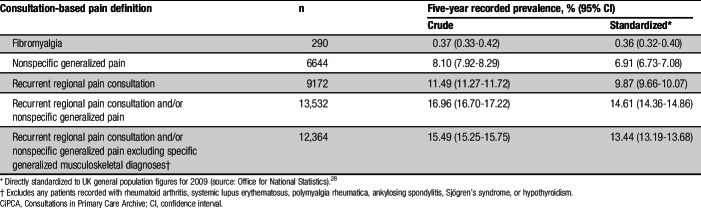
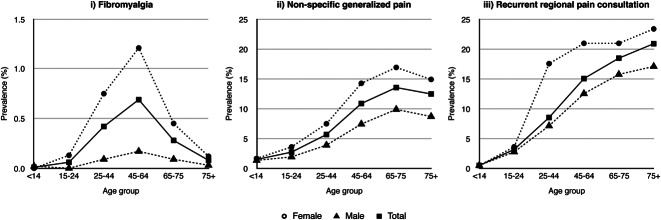
Standardized 5-year consultation prevalence ranged from 0.36% (95% confidence interval [CI]: 0.32%-0.40%) for recorded fibromyalgia to 14.61% (95% CI: 14.36%-14.86%) for the combined prevalence of recurrent regional pain consultation or a code recorded for a nonspecific generalized pain condition (Table 1). Five-year prevalence of recurrent regional pain consultation was 9.87% (95% CI: 9.66%-10.07%). The age and sex distribution of recurrent regional pain consultation was similar to those of nonspecific generalized pain conditions, except that prevalence dipped slightly for nonspecific generalized pain consultation in the highest age band but continued to increase for recurrent regional pain consultation (Fig. 1).
Table 1.
Phase 1: 5-year prevalence of recorded pain in those registered in CiPCA practices for the full 5-year period from 2005 to 2009 (all ages).
Figure 1.
Phase 1: age and sex distribution for the 5-year consultation prevalence of: (i) recorded fibromyalgia coding; (ii) recorded nonspecific generalized pain coding; and (iii) recurrent regional pain consultation for all those fully registered with the CiPCA practices from 2005 to 2009. CiPCA, Consultations in Primary Care Archive., Y-axis scale varies between (i) and (ii) and (iii).
3.1.2. Overlap of recurrent regional pain consultation with nonspecific generalized pain
Of the 6466 patients with a record of a nonspecific generalized pain condition, 290 (4%) were recorded with a specific fibromyalgia code. Thirty-three percent (2106/6466) of nonspecific generalized consulters also fulfilled the recurrent regional pain consulter definition. The recurrent regional pain consultation algorithm identified 42% (123/290) of those recorded with fibromyalgia codes. Twenty-three percent (2106/9172) of recurrent regional pain consulters had a recorded nonspecific generalized pain condition.
3.2. Phase 2
Of 26,129 eligible participants at baseline, 71% (n = 18,497) responded to the baseline health survey questionnaire. Of those consenting to follow-up and still registered with the GP (n = 11,900), 81% (n = 9665) responded to the 3-year follow-up questionnaire. Of the 9665 people responding to both the baseline and the 3-year questionnaires, 9% (n = 831) did not consent to medical record review and 6% (n = 548) had <5 years of medical record data available, leaving 8286 participants eligible for inclusion in this study (Supplementary Figure S1, available online at http://links.lww.com/PAIN/A352).
Incomplete responders (either baseline-only responders or baseline and 3-year responders without 5 years of medical record data) showed generally small differences from the study population on all baseline variables assessed (Supplementary Table S1, available online at http://links.lww.com/PAIN/A352). Nonresponders at baseline were slightly older (mean difference = 0.86 years, 95% CI: 0.53-1.18) and more likely to be male (nonresponders: 49% male; study population: 46% male, percentage difference: 3.15%, 95% CI: 1.59%-4.71%) than the study population.
Of the 8286 individuals in the study population, 85% (n = 7076) self-reported musculoskeletal pain at either baseline or 3 years. Two thousand, eight hundred three (35%) reported ACR-1990 widespread pain on one or both surveys, of whom 1190 (14% of all the study population) reported ACR-1990 widespread pain at both baseline and 3 years (persistent widespread pain).
Eighty percent (6611/8286) of the study population had at least one recorded musculoskeletal consultation in the 5-year period. Twenty-two percent (n = 1786) of the population were identified as recurrent regional pain consulters, and 24% (n = 1979) consulted for a musculoskeletal problem in only one region during the 5-year study period.
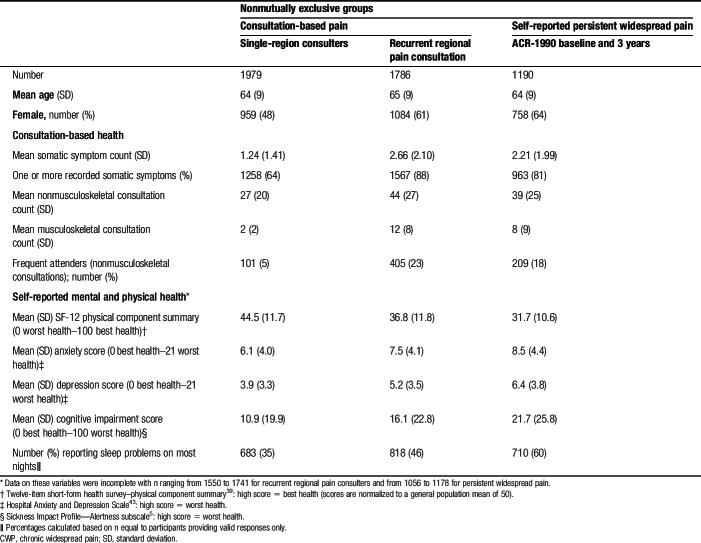
3.2.1. Patient characteristics
Descriptive statistics for participants with recurrent regional pain consultation and/or self-reported persistent widespread pain are presented in Table 2. Mean age was similar (64-65 years) across pain definitions. Sixty-four percent of patients with self-reported persistent widespread pain were female, which was similar to the figure of 61% observed in recurrent regional pain consulters. Eighty-eight percent (n = 1567) of recurrent regional pain consulters had at least one recorded consultation for a somatic symptom, compared with 81% (n = 963) of those with persistent widespread pain. In participants consulting for a single region, 48% were female, mean age was 64, and 62% (n = 1111) self-reported persistent widespread pain.
Table 2.
Phase 2: age, sex, consultation-based health, and self-reported health characteristics by single-region consulter, recurrent regional pain consulter, and self-reported CWP status (ACR-1990 at baseline and 3 years), age ≥50 years.
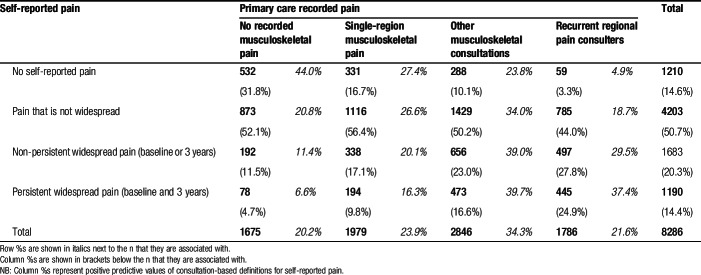
3.2.2. Agreement between consultation-based and self-reported pain status
Table 3 shows the agreement between consultation-based pain status and self-reported pain status. Virtually all recurrent regional pain consulters (97%, n = 1727) had self-reported pain. Fifty-three percent (942/1786) of recurrent regional pain consulters reported widespread pain on one or both surveys, whereas 25% (445/1786) reported persistent widespread pain at both baseline and 3 years. Patients recorded as consulting for single-region (axial, upper, or lower limb) pain reported less widespread pain than recurrent regional pain consulters—with 27% (532/1979) reporting widespread pain on one or both surveys and 10% (194/1979) reporting widespread pain at both baseline and 3 years. Recurrent regional pain consulters represented 37% (445/1190) of those reporting persistent widespread pain. However, individuals from the large group who consulted with more than single-site musculoskeletal pain but who did not meet the definition for recurrent regional pain consultation (other musculoskeletal consultations) represented 40% (473/1190) of those reporting persistent widespread pain.
Table 3.
Phase 2: overlap of consultation-based pain and self-reported pain status (n, row%, [column %]).
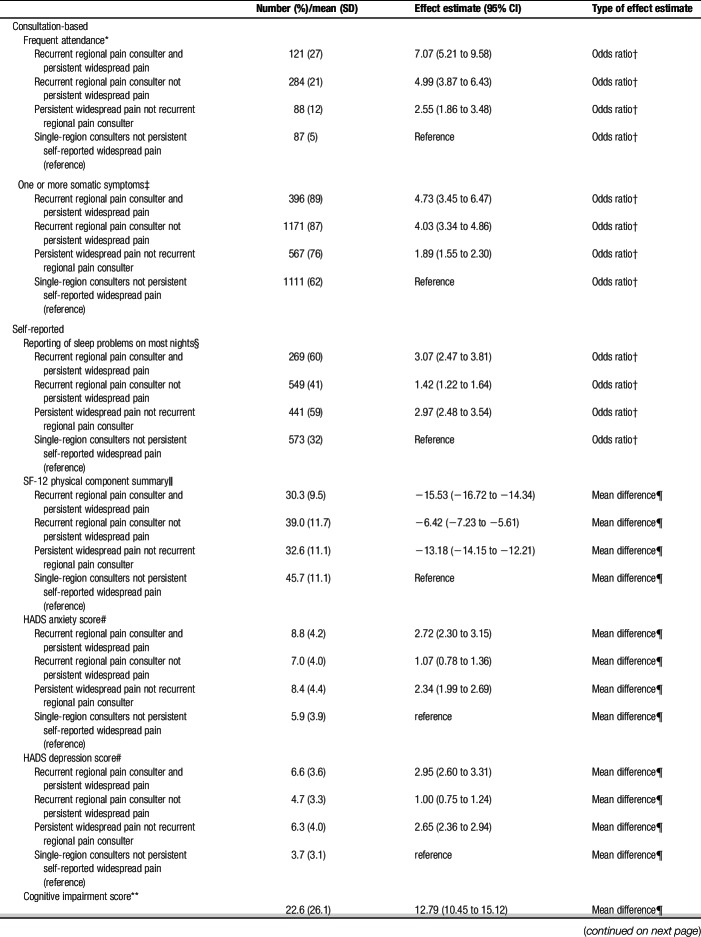
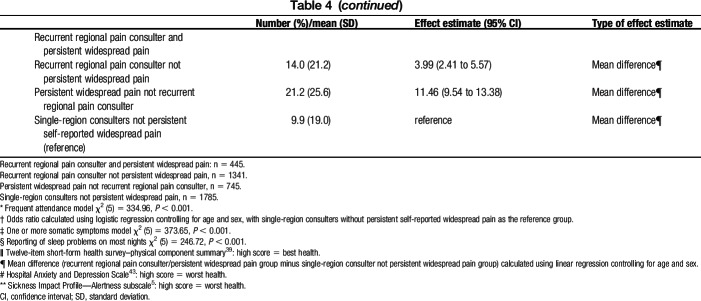
The single-region controls without self-reported persistent widespread pain had the best consultation-based and self-reported health. The 2 groups of recurrent regional pain consulters had the most severe consultation-based health on all measures, with those also reporting persistent widespread pain having the worst consultation-based health (Table 4). For example, the odds of being a frequent attender for nonmusculoskeletal conditions compared with the control group (single-region consulters) were 7.07 (95% CI: 5.21-9.58) in recurrent regional pain consulters with persistent widespread pain; 4.99 (95% CI: 3.87-6.43) in recurrent regional pain consulters without persistent widespread pain; and 2.55 (95% CI: 1.86-3.48) in those with persistent widespread pain who were not recurrent regional pain consulters.
Table 4.
Phase 2: results of logistic/linear regression analyses to compare consultation-based and self-reported health characteristics between recurrent regional pain consultation and self-reported persistent widespread pain status.
Individuals both self-reporting persistent widespread pain and identified as recurrent regional pain consulters were the most severely affected on all self-reported health measures, followed closely by those with persistent widespread pain but not fulfilling the recurrent regional pain consultation definition. Those fulfilling the recurrent regional pain consulter definition but not reporting persistent widespread pain had poorer self-reported health than the control group. For example, the odds of reporting a sleep problem compared with the control group were 3.07 (95% CI: 2.47-3.81) in recurrent regional pain consulters with persistent widespread pain; 2.97 (95% CI: 2.48-3.54) in those with persistent widespread pain but not recurrent regional pain consulters; and 1.42 (95% CI: 1.22-1.64) in recurrent regional pain consulters without persistent widespread pain.
4. Discussion
The first phase of our study determined a prevalence of recurrent regional pain consultation to primary care similar to estimates based on self-reported CWP in the general population.26 Three-quarters of recurrent regional pain consulters did not have a code recorded for generalized pain conditions related to CWP (eg, fibromyalgia). They therefore had widespread pain potentially unrecognized as such by their GP.
In the second phase, we established some overlap between consultation-based and self-reported widespread pain, with half of all recurrent regional pain consulters over a 5-year period self-reporting widespread pain at least once. However, only one-quarter reported persistent widespread pain during this period. Conversely, only a minority of all those who self-reported CWP (37%) fulfilled the recurrent regional consulter definition during the 5-year period.
There were similar patterns of poor health (eg, more somatic complaints) with recurrent regional pain consultation and self-reported CWP, although this was more marked for consultation measures of poor health in recurrent regional pain consulters and for survey measures in those with self-reported CWP.
The primary care coding prevalence of fibromyalgia was considerably lower than that predicted by community prevalence, even accounting for a proportion of patients not consulting for their symptoms. This is consistent with findings from 2 large database studies.10,16 The combined 5-year prevalence of recurrent regional pain consultation (“unrecognized” CWP) and nonspecific pain complaints (“recognized” CWP), after excluding specific generalized musculoskeletal diagnoses, was slightly higher, at 13%, than general population point prevalence estimates for CWP (10%).26 Combined with our findings from Phase 2, this indicates that prevalence of widespread pain based on consultation data may give similar prevalence estimates to general population surveys based on strict CWP criteria, but will not represent an identical group of people.
Recurrent regional pain consultation was more common in females and increased with age, consistent with that reported for CWP in the general population.26 It was associated with more somatic symptoms, self-reported sleep problems and cognitive impairment, and poorer self-reported physical and mental health than observed in those consulting only for single-region problems. These are all features consistent with CWP. Somatic symptoms are a part of the ACR-2010 definition for fibromyalgia, including fatigue and waking unrefreshed.41 Other research has also shown fibromyalgia and CWP to be associated with poor self-reported mental and physical health.38,40 Recurrent regional pain consulters were more likely to be frequent attenders, which is consistent with research linking frequent attendance to both CWP13,21,27 and medically unexplained syndromes.31,36 However, it may also be a feature of the self-fulfilling nature of a definition that requires repeated consultation, although we excluded musculoskeletal conditions from our definition of frequent attendance.
Half of recurrent regional pain consulters did not self-report widespread pain at either of the 2 survey points 3 years apart, and only a third of those self-reporting persistent widespread pain fulfilled the recurrent regional pain consulter definition. Fulfilling recurrent regional pain consultation criteria was associated with worse consultation-based health than self-reporting persistent widespread pain, whereas persistent widespread pain was associated with worse self-reported health than recurrent regional pain consultation. Rather than identifying all CWP patients who consult their GP, the recurrent regional pain consultation definition identifies a specific group of patients who may be unrecognized as having a generalized condition, and therefore, through their consultation behavior, are expressing a need that may remain unmet. This group is consequently an important one because identifying them and managing them appropriately has the potential to improve their health and reduce consultation demands.
The recurrent regional pain consulter definition represents a promising phenotype for EHR studies as it identifies patients with nonlocal pain who have higher rates of disability and health care use. However, given the disparity between self-reported CWP and recurrent regional pain consultation, it is possible we should consider other approaches to developing a consultation-based definition of CWP, based on 2 observations. First, only 7% of all those with persistent widespread pain had no record of a musculoskeletal consultation during the study period; musculoskeletal consultation thereby represents a reasonable sampling frame for identifying and managing CWP in the population. Second, single-site musculoskeletal consultation seems to represent a low-severity group (by both consultation and self-report measures). Given this, it may be that systematically seeking information about other pain sites could be a simple way to ensure that GPs consider the extent of pain in their care and management of patients and may be useful for future development of EHR-based pain phenotypes. The highest severity group—those with combined recurrent regional pain consultation and self-reported CWP—suggests that both sources of information could be useful for care and prevention.
We performed this study in 2 large samples of patients, using high-quality primary care data and validated self-report instruments. The studies were limited to one area of the United Kingdom (North Staffordshire) and the use of an older age group in Phase 2. However, sensitivity analyses using the CiPCA data (not presented) demonstrated minimal differences in the number of recorded somatic symptoms and musculoskeletal consultations between recurrent regional pain consulters from all age groups and the subgroup aged ≥45 years. Less than a third of the eligible population (ie, those invited to take part in the baseline study) was included in analyses in Phase 2, and we cannot exclude participation bias. However, we demonstrated that differences between the study sample and nonresponders and partial responders were small.
Not all patients with a problem will consult their GP for it; consequently, consultation prevalence will be lower than community population prevalence estimates. For chronic conditions, a diagnostic label for a repeatedly consulted complaint may only be coded at diagnosis.18 The use of a 5-year period to define recurrent regional pain consultation would mean it is less likely we have missed a relevant diagnosis in the Phase 1 study, but it is possible some patients were recorded with fibromyalgia or other diagnosis outside of this period.
We have attempted to define a relatively newly identified phenotype, a group of recurrent pain consulters in primary care, with a prevailing symptom of chronic musculoskeletal pain, who are potentially unrecognized by their GPs as having a generalized condition associated with somatic symptoms. We therefore had no reference standard against which to compare the recurrent regional pain consulters identified by our algorithm. However, the recurrent regional pain consultation phenotype is closely related to fibromyalgia/CWP, and these conditions have been studied extensively using the ACR-1990 definition. We were able to demonstrate that recurrent regional pain consulters share many characteristics with CWP.
We included 4482 regional musculoskeletal Read codes in the definition of recurrent regional pain consultation based on previous consensus work. However, the codes may not always indicate musculoskeletal pain (eg, unstable ankle), and the list includes codes for conditions that may not be appropriate for use in CWP, such as structural derangements (eg, meniscal tears), infections, and inflammatory arthropathies. There may be other codes with the potential to represent musculoskeletal problems. Evidence of widespread pain and somatic symptoms may also be “hidden” in the free text of the consultation.
Our study suggests that recurrent regional pain consulters represent a heterogeneous subgroup of frequent consulters, with chronic musculoskeletal problems as the prevailing symptom of their polysymptomatic distress, who may not be recognized as having a more generalized pain condition associated with somatic symptoms. They include those less severely affected, who do not necessarily fit established and strict CWP criteria, and therefore reflect an overlapping rather than identical group of persons. They nonetheless still exist on the spectrum of polysymptomatic distress characteristic of CWP and fibromyalgia.
The recurrent regional pain consulter algorithm highlights the existence of a substantial group of patients with potentially unmet needs. Treatment focused on regional pain syndromes alone may be suboptimal if the added burden of pain elsewhere in the body—and the additional characteristics associated with it (such as pain severity and propensity for long-term persistence)—is not identified and taken into account in explanation, advice, and care given to the patient.4,25
There is some underrecognition of CWP in primary care, implying a need for specific training for GPs. If some patients are not recognized as having generalized pain conditions with associated somatic symptoms, they may be inappropriately managed (as multiple episodes of regional pain). Ineffective management may lead to poor patient outcomes and contribute unnecessarily to primary care workload (continued consultation for unresolved symptoms). Screening for multisite pain in patients presenting with single-site musculoskeletal complaints may be a simple way for GPs to consider the extent of pain in their management. Future research should explore this clinically important group of chronic consulters. Although there seem to be effective treatments for patients with widespread pain, we do not yet understand how best to help those recurrently consulting for regional musculoskeletal pain. Recurrent consultation for local musculoskeletal pain offers a means of identifying a clinically relevant group of high users of primary care. Further research to investigate changes in their health over time, the financial cost of their management, and possible interventions would offer insights into long-term health outcomes, current economic burden, and management of individuals who consult with nonlocal pain complaints.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Work undertaken on this study was part of a PhD studentship funded by the Arthritis Research UK Primary Care Centre at Keele University. The NorStOP study was funded by a Programme Grant awarded by the Medical Research Council, UK (grant Code: G9900220), and funding secured from the North Staffordshire Primary Care R&D Consortium for NHS service support costs. North Staffordshire Primary Care Research Consortium and Keele University Research Institute for Primary Care and Health Sciences fund the CiPCA database. The funders had no role in the study design, collection of the data, analysis, interpretation of the study, or writing of the manuscript.
Acknowledgements
The authors thank members of the original NorStOP study teams, Keele GP Research Partnership, the informatics team at the Arthritis Research UK Primary Care Centre, and the staff at the participating general practices. The authors also thank Jens Rohrbeck for his original work on the recurrent regional pain algorithm, and Stefan Bergman and Daniëlle van der Windt for their comments on the project. K. P. Jordan had the original idea for the study. All authors were involved in the study design. K. E. Mansfield undertook the data management, did primary analysis, and wrote the first draft. All authors contributed to further drafts and approved the final manuscript. K. E. Mansfield had full access to the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The authors are unable to share individual-level data.
Appendix A. Supplemental Digital Content
Supplemental Digital Content associated with this article can be found online at http://links.lww.com/PAIN/A352.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.painjournalonline.com).
References
- [1].Arshad A, Ooi KK. Awareness and perceptions of fibromyalgia syndrome: a survey of Southeast Asian rheumatologists. J Clin Rheumatol 2007;13:59–62. [DOI] [PubMed] [Google Scholar]
- [2].Bedson J, McCarney R, Croft P. Labelling chronic illness in primary care: a good or a bad thing? Br J Gen Pract 2004;54:932–8. [PMC free article] [PubMed] [Google Scholar]
- [3].Benson T. Why general practitioners use computers and hospital doctors do not—Part 2: scalability. BMJ 2002;325:1090–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Bergman S. Management of musculoskeletal pain. Best Pract Res Clin Rheumatol 2007;21:153–66. [DOI] [PubMed] [Google Scholar]
- [5].Bergner M, Bobbitt RA, Carter WB, Gilson BS. The sickness impact profile: development and final revision of a health status measure. Med Care 1981;19:787–805. [DOI] [PubMed] [Google Scholar]
- [6].Blotman F, Thomas E, Myon E, Andre E, Caubere JP, Taïeb C. Awareness and knowledge of fibromyalgia among French rheumatologists and general practitioners. Clin Exp Rheumatol 2005;23:697–700. [PubMed] [Google Scholar]
- [7].Buskila D, Neumann L, Sibirski D, Shvartzman P. Awareness of diagnostic and clinical features of fibromyalgia among family physicians. Fam Pract 1997;14:238–41. [DOI] [PubMed] [Google Scholar]
- [8].Butler S, Landmark T, Glette M, Borchgrevink P, Woodhouse A. Chronic widespread pain—the need for a standard definition. PAIN 2015;157:1. [DOI] [PubMed] [Google Scholar]
- [9].Endresen GK. Fibromyalgia: a rheumatologic diagnosis? Rheumatol Int 2007;27:999–1004. [DOI] [PubMed] [Google Scholar]
- [10].Gallagher AM, Thomas JM, Hamilton WT, White PD. Incidence of fatigue symptoms and diagnoses presenting in UK primary care from 1990 to 2001. J R Soc Med 2004;97:571–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Ghazan-Shahi S, Towheed T, Hopman W. Should rheumatologists retain ownership of fibromyalgia? A survey of Ontario rheumatologists. Clin Rheumatol 2012;31:1177–81. [DOI] [PubMed] [Google Scholar]
- [12].Glennon P. Fibromyalgia syndrome: management in primary care. Rep Rheum Dis 2010;6:1–6. [Google Scholar]
- [13].Gupta A, Silman AJ, Ray D, Morriss R, Dickens C, Macfarlane GJ, Chiu YH, Nicholl B, McBeth J. The role of psychosocial factors in predicting the onset of chronic widespread pain: results from a prospective population-based study. Rheumatology (Oxford) 2007;46:666–71. [DOI] [PubMed] [Google Scholar]
- [14].Hripcsak G, Albers DJ. Next-generation phenotyping of electronic health records. J Am Med Inform Assoc 2013;20:117–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].HSCIC. Attribution data set GP-registered populations scaled to ONS population estimates—2011. 2012. Available at: http://www.hscic.gov.uk/catalogue/PUB05054. Accessed July 25, 2015. [Google Scholar]
- [16].Hughes G, Martinez C, Myon E, Taïeb C, Wessely S. The impact of a diagnosis of fibromyalgia on health care resource use by primary care patients in the UK: an observational study based on clinical practice. Arthritis Rheum 2006;54:177–83. [DOI] [PubMed] [Google Scholar]
- [17].Jordan K, Clarke AM, Symmons DPM, Fleming D, Porcheret M, Kadam UT, Croft P. Measuring disease prevalence: a comparison of musculoskeletal disease using four general practice consultation databases. Br J Gen Pract 2007;57:7–14. [PMC free article] [PubMed] [Google Scholar]
- [18].Jordan K, Porcheret M, Croft P. Quality of morbidity coding in general practice computerized medical records: a systematic review. Fam Pract 2004;21:396–412. [DOI] [PubMed] [Google Scholar]
- [19].Jordan KP, Jöud A, Bergknut C, Croft P, Edwards JJ, Peat G, Petersson IF, Turkiewicz A, Wilkie R, Englund M. International comparisons of the consultation prevalence of musculoskeletal conditions using population-based healthcare data from England and Sweden. Ann Rheum Dis 2014;73:212–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Jordan KP, Kadam UT, Hayward R, Porcheret M, Young C, Croft P. Annual consultation prevalence of regional musculoskeletal problems in primary care: an observational study. BMC Musculoskelet Disord 2010;11:144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Kadam UT, Thomas E, Croft PR. Is chronic widespread pain a predictor of all-cause morbidity? A 3 year prospective population based study in family practice. J Rheumatol 2005;32:1341–8. [PubMed] [Google Scholar]
- [22].Kamoun S, Elleuch M, Lay KLe, Feki H, Taïeb C, André E, Damak J. Évaluation de la connaissance de la fibromyalgie en Tunisie. Tunis Med 2010;88:703–6. [PubMed] [Google Scholar]
- [23].Kumar P, Pullar T. Perceptions of fibromyalgia among rheumatologists in Scotland. Rheumatology 2003;42:60–1. [Google Scholar]
- [24].Lacey RJ, Lewis M, Jordan K, Jinks C, Sim J. Interrater reliability of scoring of pain drawings in a self-report health survey. Spine (Phila Pa 1976) 2005;30:E455–8. [DOI] [PubMed] [Google Scholar]
- [25].Lee J, Ellis B, Price C, Baranowski AP. Chronic widespread pain, including fibromyalgia: a pathway for care developed by the British Pain Society. Br J Anaesth 2014;112:16–24. [DOI] [PubMed] [Google Scholar]
- [26].Mansfield KE, Sim J, Jordan JL, Jordan KP. A systematic review and meta-analysis of the prevalence of chronic widespread pain in the general population. PAIN 2015;157:55–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].McBeth J, Macfarlane GJ, Benjamin S, Silman AJ. Features of somatization predict the onset of chronic widespread pain: results of a large population-based study. Arthritis Rheum 2001;44:940–6. [DOI] [PubMed] [Google Scholar]
- [28].Office for National Statistics. The national statistics socio-economic classification user manual. 2005. p. 1–110. Available at: http://www.ons.gov.uk/ons/guide-method/classifications/archived-standard-classifications/soc-and-sec-archive/the-national-statistics-socio-economic-classification–user-manual.pdf. Accessed July 25, 2015. [Google Scholar]
- [29].Deleted in proof.
- [30].Porcheret M, Hughes R, Evans D, Jordan K, Whitehurst T, Ogden H, Croft P. Data quality of general practice electronic health records: the impact of a program of assessments, feedback, and training. J Am Med Inform Assoc 2004;11:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Reid S, Wessely S, Crayford T, Hotopf M. Medically unexplained symptoms in frequent attenders of secondary health care: retrospective cohort study. BMJ 2001;322:767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Reid S, Whooley D, Crayford T, Hotopf M. Medically unexplained symptoms–GPs' attitudes towards their cause and management. Fam Pract 2001;18:519–23. [DOI] [PubMed] [Google Scholar]
- [33].Rohrbeck J, Jordan K, Croft P. The frequency and characteristics of chronic widespread pain in general practice: a case-control study. Br J Gen Pract 2007;57:109–15. [PMC free article] [PubMed] [Google Scholar]
- [34].Shir Y, Fitzcharles MA. Should rheumatologists retain ownership of fibromyalgia? J Rheumatol 2009;36:667–70. [DOI] [PubMed] [Google Scholar]
- [35].Simpson CR, Anandan C, Fischbacher C, Lefevre K, Sheikh A. Will Systematized Nomenclature of Medicine-Clinical Terms improve our understanding of the disease burden posed by allergic disorders? Clin Exp Allergy 2007;37:1586–93. [DOI] [PubMed] [Google Scholar]
- [36].Smits FTM, Brouwer HJ, ter Riet G, van Weert HCP. Epidemiology of frequent attenders: a 3-year historic cohort study comparing attendance, morbidity and prescriptions of one-year and persistent frequent attenders. BMC Public Health 2009;9:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Thomas E, Wilkie R, Peat G, Hill S, Dziedzic K, Croft P. The North Staffordshire Osteoarthritis Project–NorStOP: prospective, 3-year study of the epidemiology and management of clinical osteoarthritis in a general population of older adults. BMC Musculoskelet Disord 2004;5:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Walitt B, Fitzcharles MAA, Hassett AL, Katz RS, Häuser W, Wolfe F. The longitudinal outcome of fibromyalgia: a study of 1555 patients. J Rheumatol 2011;38:2238–46. [DOI] [PubMed] [Google Scholar]
- [39].Ware J, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:220–33. [DOI] [PubMed] [Google Scholar]
- [40].Wolfe F, Brähler E, Hinz A, Häuser W. Fibromyalgia prevalence, somatic symptom reporting, and the dimensionality of polysymptomatic distress: results from a survey of the general population. Arthritis Care Res 2013;65:777–85. [DOI] [PubMed] [Google Scholar]
- [41].Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Katz RS, Mease P, Russell AS, Russell IJ, Winfield JB, Yunus MB. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res 2010;62:600–10. [DOI] [PubMed] [Google Scholar]
- [42].Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, Tugwell P, Campbell SM, Abeles M, Clark P, Fam AG, Farber SJ, Fiechtner JJ, Michael Franklin C, Gatter RA, Hamaty D, Lessard J, Lichtbroun AS, Masi AT, Mccain GA, John Reynolds W, Romano TJ, Jon Russell I, Sheon RP. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum 1990;33:160–72. [DOI] [PubMed] [Google Scholar]
- [43].Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983;67:361–70. [DOI] [PubMed] [Google Scholar]