Abstract
Setting: Socio-economically underprivileged areas in the Philippines.
Objective: To review the implementation of tuberculosis (TB) contact investigations in the urban poor areas of Manila and Quezon City.
Design: A descriptive cross-sectional study based on a review of data from household contact registries in local government unit (LGU) and non-government organisation (NGO) facilities during January–December 2012 in Manila and Quezon City. Free discussion sessions were also conducted among health-care workers.
Results: Of 6161 children and adult household contacts listed in the LGUs and 1893 in the NGOs, 17% (n = 1086) in the LGUs and 95% (n = 1800) in the NGOs were evaluated. The yield of clinically diagnosed TB among children aged <15 years was 10.2% (127/1245) in the LGUs and 8.4% (63/752) in the NGOs. The yield of isoniazid preventive therapy (IPT) for those aged <5 years was 23.1% (124/537) in the LGUs and 28.0% (78/279) in the NGOs. The NGOs produced a high yield of IPT due to a better logistical system that ensured the availability of supplies and systematic home visits.
Conclusion: Screening of household contacts in poor urban areas appears to be effective; it increased the number of children aged <15 years eligible for IPT and should be expanded as an intervention strategy for TB control in the Philippines.
Keywords: isoniazid preventive therapy, children, latent, household, TB
Abstract
Contexte : Quartiers défavorisés sur le plan socio-économique aux Philippines.
Objectif : Revoir la mise en œuvre de la recherche des contacts de tuberculose (TB) dans les zones urbaines pauvres de Manille et de Quezon City.
Schéma : Une étude descriptive transversale basée sur une revue des données des registres de contacts domiciliaires de janvier à décembre 2012 dans des unités publiques locales (LGU) et des structures d'organisations non gouvernementales (ONG) à Manille et à Quezon City. Des séances de discussion libre ont également été réalisées avec les prestataires de soins.
Résultats : Sur les 6161 contacts familiaux des LGU et les 1893 contacts des ONG (enfants et adultes) listés, 17% (1086/6161) des LGU et 95% (1800/1893) des ONG ont été évalués. Le pourcentage de TB diagnostiquées cliniquement parmi les enfants âgés de < 15 ans a été de 10,2% (127/1245) dans les LGU et de 8,4% (63/752) dans les ONG. Le pourcentage d'enfants âgés de < 5 ans mis sous traitement préventif par isoniazide (TPI) a été de 23,1% (124/537) dans les LGU et de 28,0% (78/279) dans les ONG. Les ONG ont eu une meilleure mise en œuvre du TPI grâce à un meilleur système logistique qui a assuré la disponibilité des médicaments et des visites à domicile systématiques.
Conclusion : Le dépistage des contacts familiaux dans les zones urbaines pauvres semble être efficace et il a augmenté le nombre d'enfants âgés de < 15 ans éligibles au TPI ; il devrait être étendu en tant que stratégie d'intervention pour la lutte contre la TB aux Philippines.
Abstract
Marco de referencia: Las regiones desfavorecidas desde el punto de vista socioeconómico en las Filipinas.
Objetivo: Evaluar la aplicación de la investigación de contactos de casos de tuberculosis (TB) en las zonas urbanas pobres de Manila y Ciudad Quezón.
Método: Un estudio transversal descriptivo con análisis de datos de los registros de contactos domiciliarios de enero a diciembre del 2012, en los establecimientos de las Unidades del Gobierno Local (UGL) y de Organizaciones No Gubernamentales (ONG) en Manila y Ciudad Quezón. Se realizó además una sesión abierta de conversaciones con los profesionales de salud.
Resultados: En las UGL se evaluaron 17% (1086/6161) y en los establecimientos de las ONG se investigaron 95% (1800/1893) de los contactos domiciliarios registrados (niños y adultos). El rendimiento (diagnóstico clínico) en los niños <15 años fue 10,2% (127/1245) en las UGL y 8,4% (63/752) en las ONG. El suministro del tratamiento preventivo con isoniazida en los niños de < 5 años alcanzó un 23,1% (124/537) en las UGL y un 28,0% (78/279) en las ONG. Las ONG lograron un resultado superior con respecto al tratamiento preventivo debido a su mejor organización logística, que procuraba la disponibilidad de los suministros y visitas domiciliarias sistemáticas.
Conclusión: La investigación de los contactos domiciliarios en las zonas urbanas pobres resulta eficaz y aumenta el número de niños <15 años que cumplen con los criterios para recibir el tratamiento preventivo con isoniazida. Sería conveniente ampliar la escala de esta intervención, como una estrategia de control de la TB en las Filipinas.
Tuberculosis (TB) is still a major health problem in the Philippines; it was ranked the sixth leading cause of mortality and the eighth leading cause of morbidity in the country.1 The goal of the National Tuberculosis Control Programme (NTP) was to achieve incidence, prevalence and mortality rates of 246, 414 and 23 per 100 000 population, respectively, by 2016.2 One of the strategies recommended by the World Health Organization (WHO) to find missing TB cases is through contact investigations.3,4 Contact investigations involve the systemic evaluation of contacts of known TB patients to identify TB disease or latent tuberculous infection (LTBI) and is proposed as a strategy for increasing case detection rates because contacts have a higher risk of developing the disease.4–6 In 2008, the Department of Health (DOH) guidelines for the management of TB in children in the Philippines included screening child household contacts (aged <15 years) and the provision of isoniazid preventive therapy (IPT) for children aged <5 years.7,8 The results of a project in the Philippines in 2010 showed that 589 cases were diagnosed with TB, which represents 2% of all contacts investigated through household contact investigations.9
The Research Institute of Tuberculosis/Japan Anti-Tuberculosis Association (RIT/JATA) Philippines, known as RJPI, is a local non-governmental organisation (NGO) that supports the NTP to improve access to quality TB patient care by reaching the urban poor communities of District I, Tondo, Manila, with a total population of 405 125 and Payatas, Quezon City, with a total population of 120 360.10,11 Local government unit (LGU) DOTS facilities were utilising Masterlist B, a log book in which child household contacts (aged <15 years) of registered TB cases were listed and tracked along the pathway from identification, screening and evaluation of signs and symptoms to physician assessment. Three NGO DOTS facilities, two in Tondo and one in Payatas, were conducting TB contact investigations for all household contacts, including adults, of registered TB cases, but no standard recording and reporting system was created before the RJPI began its project.
To document and develop a system of contact investigation for the NGO DOTS facilities at the project site, RJPI modified Masterlist B in 2011 with the guidance of the NTP coordinators of the Manila Health Department (MHD) and the Quezon City Health Department (QCHD). Modified Masterlist B was designed to track the pathway of all listed household contacts (both children and adults) through identification, screening, evaluation, diagnosis, initiation and completion of treatment.
This study aimed to assess the contribution of contact investigation as an intervention strategy to increase the number of children enrolled for IPT through a review of LGU and NGO facilities registries (Masterlist B) and other documents in Tondo and Payatas. The review also compared the two approaches and conducted free discussion sessions (FDS). An FDS is a simple discussion among health-care workers on the questions presented by sharing experiences, while a focus group discussion (FGD) is a more in-depth discussion guided by trained leaders, where opinions are used to guide future actions.
DESIGNS AND METHODS
This cross-sectional descriptive data review was conducted by the trained RJPI staff and a research assistant of all household contacts registered in Masterlist B and modified Masterlist B from January to December 2012 in the LGU and NGO DOTS facilities. The evaluation of household contacts was based on the following:
The contact index ratio. The ratio of the number of index cases to the number of household contacts. An index case was defined as the first diagnosed TB case in the family registered from January to December 2012 in the NTP TB register. Household contacts are persons who shared the same enclosed living space for frequent or extended periods during the day with an index case.
The proportion of evaluated household contacts among those listed in the Masterlists. Listed refers to the name of all household contacts in the Masterlists by the beginning of this study (March 2014). An evaluated household contact means that the household contact was assessed through the recognition of signs and symptoms or through diagnostic examinations up to the time when they were checked by the physician.
TB disease and IPT yield among the household contacts examined.
The treatment outcome for TB disease and for IPT of the household contact.
Other data recorded in both the Masterlists were also obtained from other NTP recording forms such as the individual treatment record, the NTP treatment card, the IPT card, the IPT register, the NTP TB register, the NTP diagnosis form and the NTP laboratory register. Any queries/discrepancies found in the logbook were immediately discussed with the staff concerned.
FDS were conducted in March 2014 with 41 participants involved in contact investigations in the LGU and NGO DOTS facilities, such as physicians, nurses, DOTS-in-charge and community health volunteers (CHVs), as recommended by the NTP coordinators. First, the status report citing the achievements of the LGU and NGO DOTS facilities' contact investigations was presented, then the participants were separated into groups of four. The NTP coordinators were assigned as facilitators to each group and the RJPI staff as documenters.
The following questions were presented to each group: 1) the current process of contact investigation, 2) gaps identified from the evaluation of household contacts, and 3) interventions undertaken to address the gaps identified during the process of contact investigation. Common answers and recommendations from the FDS were documented and discussed with the NTP coordinators.
The χ2 test was applied to compare the two categorical data sets, and a two-sided Fisher's exact test was applied if the expected number of any of the columns was <5. P < 0.05 was considered significant. Epi Info™ v. 7 (Centers for Disease Control and Prevention, Atlanta, GA, USA) was used for statistical calculation.
The research protocol was approved by the San Lazaro Hospital Research and Ethics Review Committee (Manila, Philippines) in advance of the conduct of the study. Permission was obtained from the City Health Officers of Manila and Quezon City and the organisation heads prior to the conduct of this study. Written informed consent was obtained from the health-care workers prior to participating in the FDS.
RESULTS
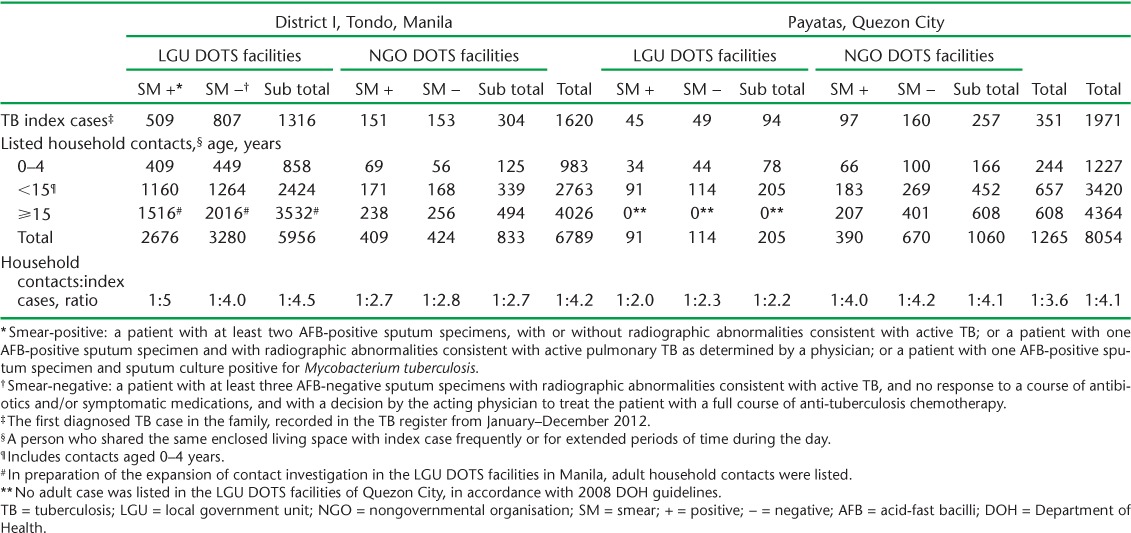
The number of household contacts listed in the LGU and the NGO DOTS facilities in Tondo and Payatas is shown in Table 1. The contact index ratio was low in the NGO DOTS facilities of Tondo compared with that of the LGU DOTS facilities (1:2.7 vs. 1:4.5), and in the LGU DOTS facilities of Payatas compared with the NGO DOTS facilities (1:2.2 vs. 1:4.1) (Table 1).
TABLE 1.
TB contact index ratio in District I, Tondo, Manila and Payatas, Quezon City, The Philippines, 2012
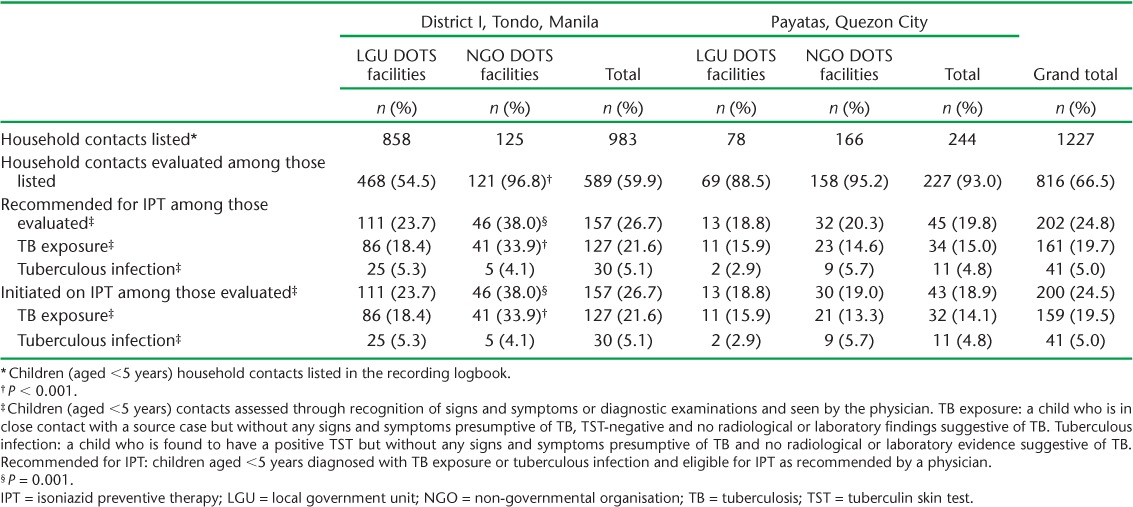
There was a low proportion of evaluated household contacts among children aged <5 years in the LGU compared to the NGO OTS facilities of Tondo (54.5% vs. 96.8%, P < 0.001) (Table 2). In Payatas, the proportion of evaluated household contacts was high in both the LGU and NGO DOTS facilities, although only 78 household contacts were listed in the LGU (Table 2). The yield of IPT diagnosis among under-fives was low in the LGU DOTS facilities compared with that of NGO DOTS facilities in Tondo (23.7% vs. 38.0%, P = 0.001), but there was no difference between the LGU and NGO DOTS facilities in Payatas (18.8% vs. 20.3%, P = 0.81, Table 2). The proportion of TB exposure was higher in the NGOs than in the LGU DOTS facilities in Tondo (33.9% vs. 18.4%, P < 0.001), and similar between the LGU and NGO DOTS facilities in Payatas (15.9% vs. 14.6%, P = 0.79, Table 2). The proportion of tuberculous infection was also similar between the LGU and NGO DOTS facilities in both Tondo and Payatas (5.3% vs. 4.1% and 2.9% vs. 5.7%, respectively, Table 2).
TABLE 2.
IPT case yield among children aged <5 years in LGU and NGO DOTS facilities of District I, Tondo, Manila and Payatas, Quezon City, The Philippines, 2012
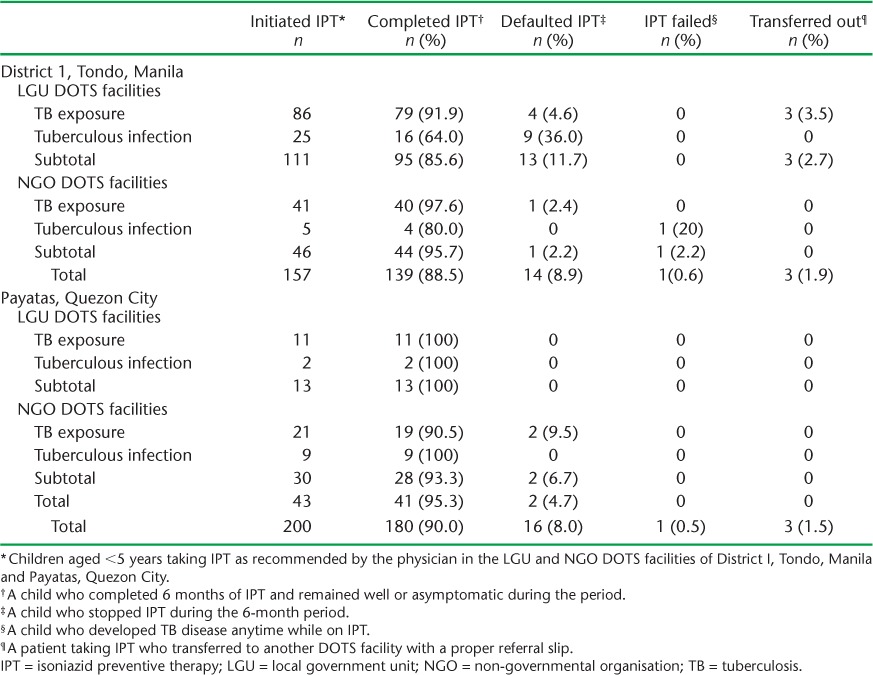
The proportion of children who completed IPT tended to be low in the LGU compared to the NGO DOTS facilities of Tondo, although the difference was not statistically significant (85.6% vs. 95.7%, P = 0.82, Table 3), and was similar in the LGU and NGO DOTS facilities in Payatas (100% vs. 93.3%, P = 0.34, Table 3).
TABLE 3.
IPT outcome of children aged <5 years in both LGU and NGO DOTS facilities in District I, Tondo, Manila and Payatas, Quezon City, The Philippines, 2012
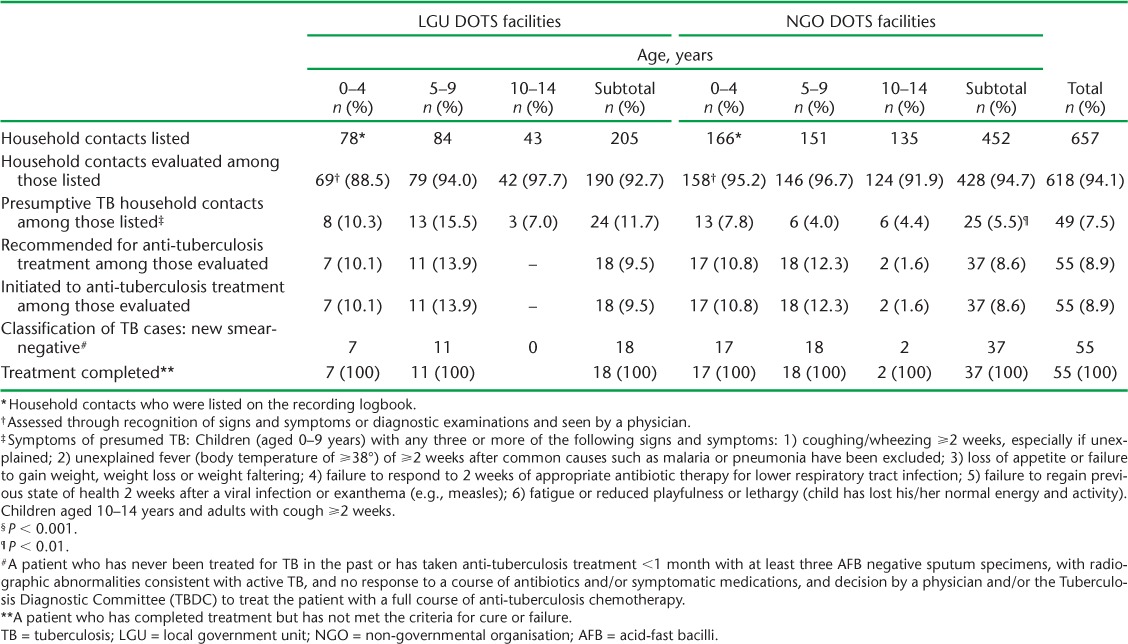
The proportion of household contacts evaluated among the listed children (aged <15 years) was higher in the NGO than the LGU DOTS facilities in Tondo (95.6% vs. 43.5%, P < 0.001, Table 4A), and similar in the LGU and NGO DOTS facilities in Payatas (92.7% vs. 94.7%, P = 0.031, Table 4B). The yield of TB disease among the children evaluated was similar between the LGU and NGO DOTS facilities in both Tondo and Payatas (10.3% vs. 8.0%, P = 0.22, Table 4A; 9.5% vs. 8.6%, P = 0.74, respectively, Table 4B). All contacts (109/109) in the LGU and 98.5% of contacts (133/135) in the NGO initiated to treatment in Tondo, while 100% (18/18) in the LGU and 100% (37/37) in the NGO were initiated on treatment in Payatas and showed a favourable outcome (defined as treatment completed) (Tables 4A and 4B). Both the LGUs and NGOs in Payatas were successful in retaining their patients on treatment.
TABLE 4A).
TB disease yield and treatment outcome among children aged <15 years in LGU and NGO DOTS facilities of District I, Tondo, Manila, The Philippines, 2012
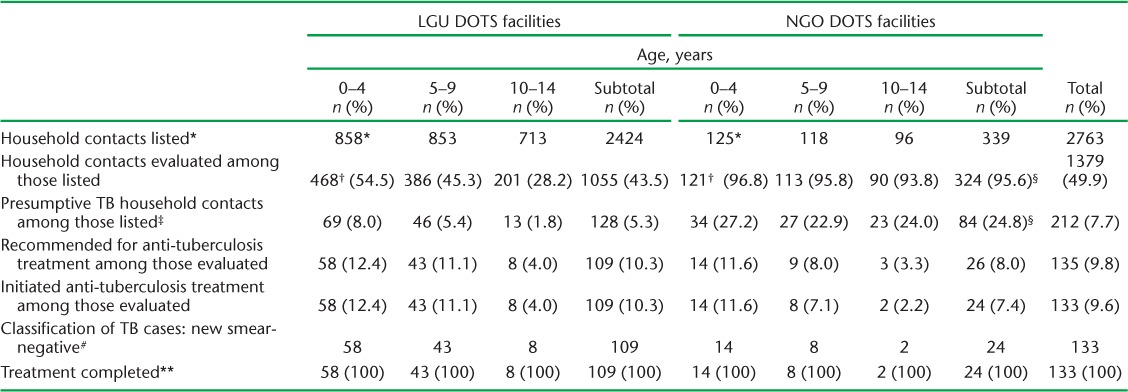
TABLE 4B).
TB disease yield and treatment outcome among children aged <15 years in LGU and NGO DOTS facilities of Payatas, Quezon City, The Philippines, 2012
The FDS revealed possible reasons for the low proportion of household contacts evaluated by physicians in the LGU DOTS facilities of Tondo: 1) only presumptive TB cases among household contacts were advised to present to the DOTS facility for evaluation; 2) children were in school; 3) mothers were too busy to take their children to the DOTS facility; 4) transportation costs; 5) erratic supplies of agents such as purified protein derivative for the tuberculin skin tests (TSTs) and anti-tuberculosis drugs for children at the DOTS facilities; 6) the manner of communicating with patients was sometimes inappropriate; 7) the health workers had no time to conduct home visits for those household contacts who did not attend the DOTS facilities. These findings were shared with the relevant partners for TB control in these areas. The NTP coordinators made a strong recommendation to train the health-care workers on the implementation of contact investigations.
The FDS concluded with the following suggestions: 1) intensify health education on TB and emphasise the importance of contact investigations to health-care workers and household contacts; 2) strict listing of all household contacts; 3) encouragement of household contacts to attend and follow-up for evaluation within 7 days of registration of an index TB case; 4) coordination of health-care workers with other agencies such as the daycare centres or schools for screening and evaluation of child household contacts; and 5) creation of a behavioural change communication seminar for health-care workers to develop and maintain communication skills and appropriate behaviour towards patients.
DISCUSSION
To our knowledge, this is the first study in the Philippines to investigate the process of implementation of contact investigation among smear-positive and smear-negative TB index cases, and to report the yield of IPT and TB disease and treatment outcomes in urban settings.
The study showed that only the LGUs in Tondo and the NGO DOTS facilities in Payatas were able to identify and list household contacts of registered TB cases, which were comparable to the average family size of 4.3–4.5 members cited in existing statistics reports in Metro Manila.12
Because of the erratic supply of diagnostics, the proportion of children aged <15 years evaluated was low, at 45.3%, in the LGU of Tondo. The study findings showed that the conduct of contact investigation was not fully implemented, as not all children exposed to TB patients were evaluated, and the IPT yield was therefore low. This finding was also observed in a study in Southern India, where household screening and IPT were not effectively implemented in the households of patients with sputum smear-positive TB, yielding a low IPT uptake.13–15 Tuberculous infection among children aged <5 years in both sites was also low, at 5.0%, compared to the study by Singh et al., which reported a rate of 33.8%,16 and a study among low- and middle-income countries, which reported rates of 24–51.2%.17–20 In the Philippines, a preliminary report by Salazar et al. revealed a high rate of LTBI, at 69.2%, among children aged 0–15 years who had contact with bacteriologically confirmed and multidrug-resistant TB index cases; the authors used a 5 mm cut-off point for TST instead of 10 mm, and the prevalence of TB disease was 3.3% for radiographically diagnosed patients and 0.65% among bacillary diagnosed patients.21 This is in contrast to our study, which revealed a high prevalence of TB in children aged <15 years in both sites, i.e., 9.5% (new smear-negative TB) among smear-positive and smear-negative index cases combined.
The implementation of contact investigation in most of the NGO DOTS facilities appears to be more comprehensive than in the LGU DOTS facilities. The NGO DOTS facilities perform the following contact investigation activities: 1) they conduct home visits before the start of treatment of the index cases to ensure the correct address of the patients, listing all household contacts (both children and adults); 2) they encourage all household contacts, including adults, to present for evaluation; 3) they follow up patients who did not present at the DOTS facility for evaluation; 4) household contacts with or without signs and symptoms also undergo chest radiography (CXR), and those who cannot pay for the diagnostic procedures are offered free or subsidised diagnostic services. Some of these activities could be undertaken by the LGU DOTS facilities to increase the proportion of evaluated household contacts and identify more IPT and TB cases. Although the TB disease yield of 1.6% among adult household contacts documented by the NGO DOTS facilities is not as high as that among children (9.8% in Tondo and 8.9% in Payatas), it is much higher than the estimated TB prevalence rate among the general population, which is 2.0 per 1000 population for smear-positive TB and 6.3% with CXR-suggestive TB, based on the 2007 national prevalence survey results.2 Our study results suggest that contact investigations would be more efficient if all children and adults were listed and evaluated alongside the TB index cases in both the LGU and NGO DOTS facilities.
As this study was undertaken in 12 DOTS facilities in Tondo and six DOTS facilities in Payatas, in Metro Manila, the interpretation of results is only applicable to these areas. The study was dependent on existing record data, which may have been affected by the rapid turnover of health-care workers in charge of the implementation of contact investigation. This could mean that important inquiries were not properly responded to by the new staff in charge. Data collection was difficult in the LGU DOTS facilities utilising Masterlist B, which did not contain items indicating treatment initiation or completion, and we had to review the NTP laboratory registers, the NTP diagnosis form, the NTP treatment cards and the IPT registers to complete data collection. Taking into account these limitations, we believe that tracking the pathway of all household contacts from identification, diagnosis and treatment initiation to the end of treatment is essential, as it provides useful information that could change the current contact investigation strategies and lead to a policy change.
In conclusion, contact investigations in most of the LGUs and other NGO DOTS facilities in the urban poor areas in Metro Manila have not yet been fully implemented for children and should be expanded further for adults, at least in the urban settings in the Philippines. Training in the step-by-step procedures on how to conduct contact investigations is necessary to improve the skills of health-care workers; consistent monitoring must be conducted to improve implementation, especially on proper recording and reporting, home visits, and regular supplies of diagnostics.
Acknowledgments
The authors would like to express their deep appreciation and gratitude to all of the staff at the LGUs and NGO DOTS facilities in District I, Tondo, Manila, and Payatas, Quezon City, for their support in conducting this research.
This study was funded in part by the ‘Tuberculosis Control Project in Socio-Economically Underprivileged Urban Area in Metro Manila, the Philippines-Stop TB para sa Lahat’ funded by the Ministry of Foreign Affairs, Tokyo, Japan; the ‘TB Control and Prevention Project in Socio-Economically Unprivileged Areas in Metro Manila, the Philippines’ under the technical cooperation for grassroots projects of the Japan International Cooperation Agency (Tokyo, Japan); the research project of the International Medical Centre of Japan, ‘A socio-medical study for facilitating effective infectious diseases control in Asia’, funded by the International Medical Cooperation Grant, the Ministry of Health, Labour and Welfare, Tokyo, Japan; and funding through the double-barred cross seal donation of the Japan Anti-Tuberculosis Association, Tokyo, Japan.
Footnotes
Conflicts of interest: none declared.
References
- 1.Philippines Department of Health. 2010 Philippine Health Statistics. Manila, Philippines: DoH; 2010. [Google Scholar]
- 2.Philippines Department of Health. Manual of procedures for the national tuberculosis control programme, Philippines. 5th ed. Manila, Philippines: DoH; 2013. [Google Scholar]
- 3.World Health Organization. Guidance for national tuberculosis programme on the management of tuberculosis in children. 1st ed. Geneva, Switzerland: WHO; 2006. WHO/HTM/TB/2006.371. [PubMed] [Google Scholar]
- 4.World Health Organization. Implementing the WHO Stop TB Strategy, a handbook for the national tuberculosis control programmes. Geneva, Switzerland: WHO; 2004. WHO/HTM/TB/2008.401. [PubMed] [Google Scholar]
- 5.Rieder H L. Contacts of TB patients in high incidence countries. Int J Tuberc Lung Dis. 2003;7(Suppl 3):S333–S336. [PubMed] [Google Scholar]
- 6.Fox G J, Bary S E, Britton W J, Marks G B. Contact investigation for tuberculosis: a systemic review and meta-analysis. Eur Respir J. 2013;41:140–156. doi: 10.1183/09031936.00070812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Philippines Department of Health. Training modules for tuberculosis in children. Manila, Philippines: DoH; 2008. [Google Scholar]
- 8.Philippines Department of Health. Revised guidelines for implementing tuberculosis control programme in children. Manila, Philippines: DoH; 2008. [Google Scholar]
- 9.World Health Organization. WHO-Canadian International Development Agency initiative in intensifying TB case detection in the Philippines: update. Geneva, Switzerland: WHO; 2012. http://www.who.int/tb/pHILIPPINESfactsheet_CIDA_oct2012.pdf?ua=1 Accessed November 2016. [Google Scholar]
- 10.Philippines Department of Health. Department Memo 2014-0008. Manila Health Department population report. Manila, Philippines: DoH; 2012. [Google Scholar]
- 11.Philippines Department of Health. Department Memo 2014-0008. Quezon City Health Department population report. Quezon City, Philippines: DoH; 2012. [Google Scholar]
- 12.Philippines Statistics Authority. Philippine National Statistics Office Report. Quezon City, Philippines: PSA; 2010. Manila Reference no. 2010–41 and Quezon City Reference no. 2002–17. [Google Scholar]
- 13.Shivaramakrishna H R, Frederick A, Shazia A et al. Isoniazid preventive treatment in children in two districts of South India: does practice follow policy? Int J Tuberc Lung Dis. 2014;18:919–924. doi: 10.5588/ijtld.14.0072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Banu Rekha V V, Jagarajamma K, Wares F et al. Contact screening and chemoprophylaxis in India's revised tuberculosis control program: a situational analysis. Int J Tuberc Lung Dis. 2009;13:1507–1512. [PubMed] [Google Scholar]
- 15.Pothukuchi M, Nagaraja S B, Kelamane S et al. Tuberculosis contact screening and isoniazid preventive therapy in South Indian District: operational issues for programmatic considerations. PLOS ONE. 2011;6:e22500. doi: 10.1371/journal.pone.0022500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Singh M, Mynak M L, Kumar L et al. Prevalence and risk factors for transmission of infection among children in household contact with adults having pulmonary tuberculosis. Arch Dis Child. 2005;90:624–628. doi: 10.1136/adc.2003.044255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morrison J, Pai M, Hopewell P C. Tuberculosis and latent TB infection in close contacts of people with pulmonary tuberculosis in low-income and middle income countries: a systemic review and meta-analysis. Lancet Infect Dis. 2008;8:359–368. doi: 10.1016/S1473-3099(08)70071-9. [DOI] [PubMed] [Google Scholar]
- 18.Triasih R, Rutherford M, Lestari T et al. Contact investigation of children exposed to tuberculosis in South East Asia: a systemic review. J Trop Med. 2012:301808. doi: 10.1155/2012/301808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sinfield R, Nyirenda M, Haves S et al. Risk factors for TB infection and disease in young childhood contacts in Malawi. Ann Trop Paediatr. 2006;26:205–213. doi: 10.1179/146532806X120291. [DOI] [PubMed] [Google Scholar]
- 20.Stapledon R, Viney K. Guidelines for tuberculosis contact tracing in Pacific Island countries and territories. Noumea, New Caledonia: Secretariat of the Pacific Community of Noumea, New Caledonia; 2010. [Google Scholar]
- 21.Salazar-Vergara R M L, Sia I G, Tupasi T E et al. Tuberculosis infection and disease in children living in hospitals of Filipino patients with tuberculosis: a preliminary report. Int J Tuberc Lung Dis. 2003;(Suppl 7):S494–S500. [PubMed] [Google Scholar]


