Abstract
Setting: Ho Chi Minh City (HCMC), Viet Nam.
Objective: To evaluate a new integrated service model for human immunodeficiency virus/acquired immune-deficiency syndrome (HIV/AIDS) care.
Design: In HCMC, co-located services, including voluntary HIV counseling and testing (VCT), HIV treatment at out-patient clinics (OPC), and methadone maintenance therapy (MMT) for persons who inject drugs, have operated under different administrative structures. In the context of decreasing international financial support, integration of these services into one administrative structure with reduced staff occurred in seven districts in HCMC between October 2013 and June 2014. We used a pre-post study design to compare service-related outcomes from routinely collected data at health facilities 6 months before and 6 months after integration.
Results: The proportion of HIV-infected persons linked from VCT to OPCs was unchanged or increased following integration. A higher percentage of patients eligible for antiretroviral therapy (ART) were started on ART. The proportion of ART patients lost to follow-up remained unchanged. The proportions of MMT patients who tested positive for heroin or other substances decreased or were unchanged.
Conclusions: VCT, OPC and MMT service delivery quality remained the same or improved during the 6 months following the integration. Expansion of the integrated model should be considered for HIV-related services.
Keywords: integrated care, human immunodeficiency virus/acquired immune-deficiency syndrome, antiretroviral treatment, methadone maintenance treatment
Abstract
Contexte : Ho Chi Minh City (HCMC), Viet Nam.
Objective : Evaluer un nouveau modèle intégré de services pour la prise en charge du virus de l'immunodéficience humaine (VIH) et syndrome de l'immunodéficience acquise (SIDA).
Schéma : A HCMC, des services installés au même endroit, incluant le test et conseil volontaire du VIH (VCT), le traitement du VIH en consultation externe (OPC) et le traitement de substitution par méthadone (MMT) pour les utilisateurs de drogues injectables, ont fonctionné sous différentes structures administratives. Dans le cadre de la réduction du soutien financier international, l'intégration de ces services dans une seule structure administrative avec un personnel réduit a eu lieu dans sept districts de HCMC entre octobre 2013 et juin 2014. Nous avons utilisé un schéma d'étude avant-après afin de comparer les résultats liés à ces services à partir de données recueillies en routine dans des structures de santé 6 mois avant et 6 mois après l'intégration.
Résultats : La proportion de patients VIH positifs envoyés du VCT vers les OPC n'a pas été modifiée ou a augmenté après l'intégration. Un pourcentage plus élevé de patients éligibles à les traitements antirétroviraux ont mis en route ce traitement. La proportion de patients sous ART perdus de vue est restée sans changement. Les proportions de patients MMT, chez qui la recherche d'héroïne ou d'autres substances a été positive, ont diminué ou sont restées inchangées.
Conclusions: La qualité des services de VCT, OPC et MMT est restée la même ou s'est améliorée pendant les 6 mois suivant l'intégration. L'expansion du modèle intégré devrait être envisagée pour les services relatifs au VIH.
Abstract
Marco de referencia: La Ciudad de Ho Chi Min.
Objetivo: Evaluar un nuevo modelo de servicios integrados de atención de la infección por el virus de la inmunodeficiencia humana (VIH) y síndrome de inmunodeficiencia adquirida (SIDA).
Método: En la Ciudad de Ho Chi Min, los servicios simultáneos de pruebas voluntarias y orientación sobre el VIH (VCT), de tratamiento en consulta externa de la infección por el VIH (OPC) y de tratamiento de mantenimiento con metadona a los consumidores de drogas inyectables (MMT) han funcionado en estructuras administrativas diferentes. En el contexto de una disminución del apoyo económico internacional, de octubre del 2013 a junio del 2014, se integraron estos servicios en una estructura administrativa única en siete distritos de la ciudad. En un estudio con análisis anterior y posterior a la intervención se compararon los resultados de estos servicios, a partir de los datos corrientes recogidos en los establecimientos de salud 6 meses antes de la integración y 6 meses después de la misma.
Resultados: Después de la integración, la proporción de personas infectadas por el VIH vinculadas por los centros de VCT a los OPC permaneció invariable o aumentó; un porcentaje más alto de pacientes aptos para recibir el tratamiento antirretrovírico (TAR) lo iniciaron; la proporción de los pacientes en TAR que se perdieron durante el seguimiento permaneció estable; y las proporciones de los pacientes que recibían MMT que obtuvieron un resultado positivo para la heroína u otras sustancias disminuyeron o no se modificaron.
Conclusión: Seis meses después de su integración, la calidad de la prestación de servicios de VCT, OPC y MMT permaneció estable o se mejoró. Se recomienda considerar la posibilidad de ampliar la escala de aplicación del modelo integrado de servicios relacionados con el VIH.
Ho Chi Minh City (HCMC), Viet Nam, has applied the Community Care and Support Centers (CCSCs) model since 2003 (unpublished). This model provides co-located services for persons at risk for or living with human immunodeficiency virus (HIV) infection, and includes harm reduction (syringe exchange for injection drug users), voluntary counseling and testing (VCT), HIV care and treatment at out-patient clinics (OPC), including antiretroviral therapy (ART), and, since 2008 at some sites, methadone maintenance therapy (MMT). CCSCs, which are under the supervision and management of the district preventive medicine centers have received support from various donors for staffing and operation costs. Although VCT, OPC and MMT services have been co-located, they have operated independently and in parallel with the district health care system in terms of personnel, budget and program activities.
Injection drug use and HIV have long been recognized as being closely related. The United Nations Office on Drugs and Crime in 2014 reported that of the 12.7 million people who inject drugs globally, approximately 1.7 million (13%) are living with HIV.1 In HCMC, the prevalence of HIV among injection drug users (IDUs) has ranged between 30% and 50% over the last 10 years.2 A simple and efficient way to provide services for patients with HIV who inject drugs has been developed and prioritized by researchers and those involved with the implementation of services.3 Services for these two conditions are not yet widely integrated, however, and little has been published on efficient ways to integrate services for ART and opioid substitution therapy.4 It has also been suggested that MMT may be a good entry point for HIV care, and that HIV treatment can be delivered effectively to persons receiving MMT.5
In the context of decreasing international financial support, the integration of VCT, OPC and MMT service delivery was considered a potentially sustainable and economical model for HIV and acquired immune deficiency syndrome (AIDS) prevention, care and treatment services. The HCMC Provincial AIDS Committee (PAC) started integrating VCT, OPC and MMT services in 2011 at some district CCSCs. A rapid assessment in one such district in 2013 found an increase in HIV testing and ART patient retention among IDUs following the integration of MMT into HIV services.6 A recent study in Viet Nam suggested that integrating MMT and ART services is cost-effective.7
Seven districts in HCMC began and completed the integration of services from October 2013 through June 2014 (Table 1). The integration of three services (VCT, OPC and MMT) occurred in four districts, while only VCT and OPC services were integrated at three sites where no co-located MMT services were offered.
TABLE 1.
Timeline of integration and data collection
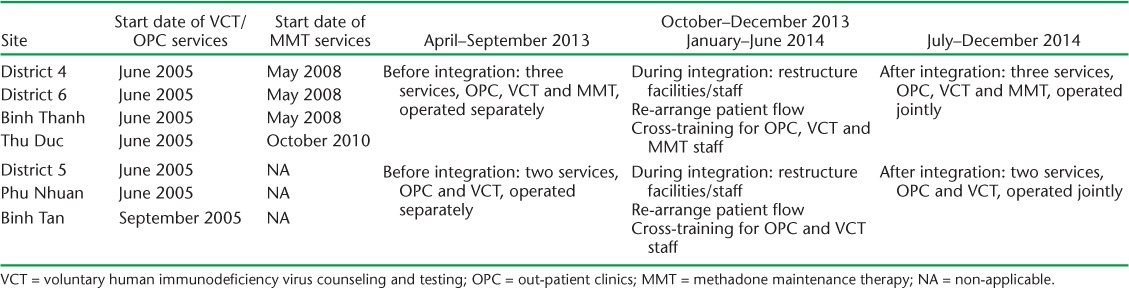
When integrated, the VCT, OPC and MMT services operate under one administrative structure, with fewer total staff and integrated patient flow. Prior to integration, 22–24 staff members at each district location offered all three HIV services at the CCSC; following integration, only 11–12 staff performed the same services (Figure, A). For the two-service districts, staff members decreased from 12–13 pre-integration to nine post-integration (Figure, B). Counselors originally trained to perform only VCT services, for example, were now providing counseling for all three types of service (Figure, A). Staff who were no longer needed under the integrated approach were transferred to other sites.
FIGURE.
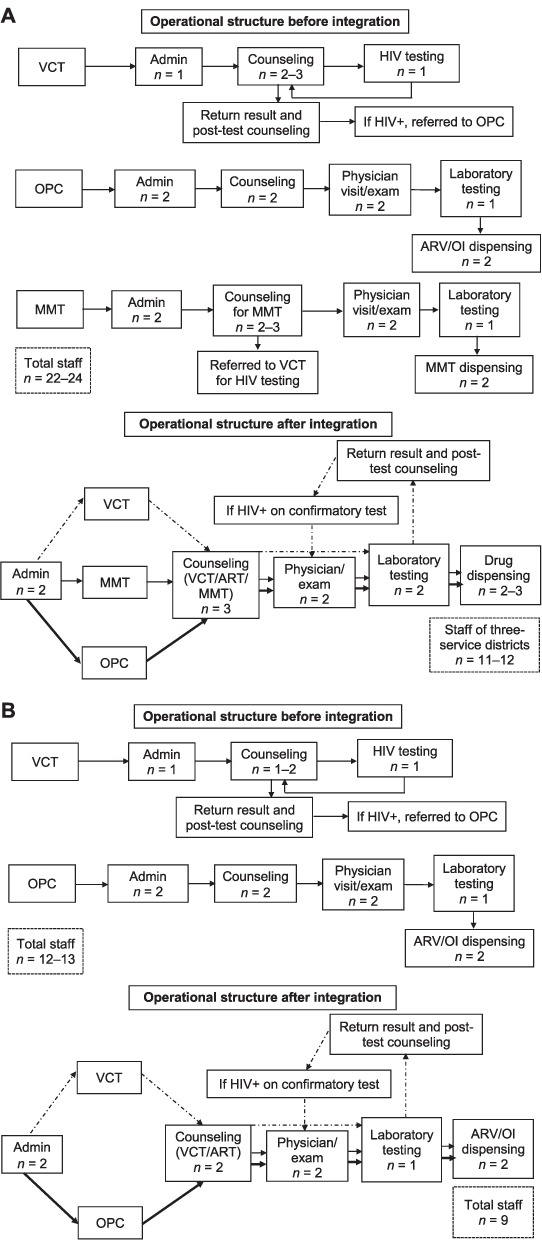
A) Operational structure of three-service sites (VCT, OPC and MMT) before and after integration. B) Operational structure of VCT and OPC services before and after integration. VCT = voluntary HIV counseling and testing; Admin = administration; HIV = human immunodeficiency virus; OPC = out-patient clinics; MMT = methadone maintenance therapy; ARV = antiretroviral drug; OI = opportunist infection; - - - = flow of VCT clients at the integrated clinic; — = flow of OPC/MMT patients at the integrated clinic; + = positive.
Patient flow was also rearranged to improve the convenience of accessing services for patients. Prior to integration, each patient entered a separate administration/reception room before being led to one of the service-specific rooms to receive VCT, HIV care and treatment or methadone. Post-integration, a patient would enter the integrated receptionist's room to complete appropriate paper work and then proceed to receive the necessary services. Integration was considered to be completed when patients could receive services from integrated staff.
The numbers of patients treated the month immediately preceding integration (September 2013) and the month immediately following integration (July 2014) at the seven surveyed clinics are as follows: pre-ART patients for each pre-integration clinic: 126, 62, 183, 190, 125, 122 and 60 (total n = 868), and pre-ART patients for each post-integration clinic: 100, 67, 134, 159, 37, 81 and 57 (total n = 635), ART patients for each pre-integration clinic: 1071, 1123, 1697, 1499, 874, 573 and 713 (total n = 7360), and ART patients for each post-integration clinic: 1141, 1161, 1706, 1588, 619, 564 and 816 (total n = 7395).
Some of the clinic management and staff were concerned that the quality of services might suffer if individual staff were required to perform multiple tasks, especially new tasks for which they may have limited knowledge and experience. We therefore sought to rapidly assess the performance of the integrated model through a comparison of selected routine indicators of service delivery and quality of three services—VCT, MMT and OPC—before and after the integration. Our purpose was to provide a quick indication of whether the quality of services remained the same, decreased, or increased following integration. This information would help guide future expansion of the integrated model.
METHODS
We used a pre-post study design to compare routinely reported programmatic data before and after integration. In four districts the VCT, OPC and MMT services were integrated; in three districts where there were no MMT services, the VCT and OPC services were integrated. Pre-integration data came from all patients who received VCT, OPC and/or MMT services in these seven districts from 1 April 2013 to 30 September 2013 (6 months prior to the start of integration). The post-integration data were taken from a cross-sectional assessment of patients receiving services and from 1 July to 31 December 2014 (6 months after integration was complete). The data were not derived from a single cohort of patients followed over time. Some clients or patients, however, may have received services during both time periods.
This assessment is based on routinely collected data from the VCT, OPC and/or MMT services; no additional data beyond those routinely collected were used in this assessment. Collection and reporting of aggregate data from these three programs was formally reviewed at the Centers for Disease Control and Prevention (Atlanta, GA, USA) and determined to be non-research, routine program activities for which informed consent was not required. For routinely reported data, staff employed at each site were responsible for collecting patient information from medical records and registers. The staff then synthesized the information collected into standardized monthly reports of aggregate data that are submitted to the PAC at the end of each month. Information from these reports were validated by PAC staff, who identified and corrected any data errors.
Among 35 current routinely collected program indicators (21 indicators for OPCs, 5 for VCT and 9 for MMT services), 15 indicators were selected for review, as we believed these indicators were most likely to be affected (either adversely or favorably) during integration. The indicators reviewed for this evaluation were: 1) the number of clients who agreed to be tested for HIV, 2) the proportion of HIV tests that were positive, 3) the number of HIV-positive clients who returned to obtain their HIV test results, 4) the proportion of those with positive test results who were successfully referred to OPCs for HIV care and treatment, 5) the proportion of ART-eligible patients who had not yet initiated ART, 6) the proportion of MMT patients who tested positive for heroin, 7) the proportion of MMT patients who tested positive for amphetamines or methamphetamines, 8) the proportion of MMT patients who tested positive for morphine, 9) the proportion of MMT patients who tested positive for benzodiazepines, 10) loss to follow-up (LTFU) of pre-ART patients, 11) the number of clients with HIV infection who died prior to receiving ART, 12) the proportion of LTFU among patients undergoing ART, 13) the number of patients who died while receiving ART, 14) the proportion of LTFU among MMT clients, and 15) the proportion of clients who died while receiving MMT. These chosen indicators might demonstrate: 1) linkages between services that could potentially be improved after integration; 2) counseling performance that might be affected, as counselors who used to perform just one job (e.g., OPC, MMT or VCT) must now be adept at performing multiple jobs, which might negatively impact performance; or 3) outcomes relating to the overall quality of services, such as the rate of eligible patients receiving treatment in a timely manner or the rate of death or LTFU. For VCT-related indicators, we selected key indicators showing program yield and VCT-OPC referral and linkage. We calculated the number and proportion of clients who agreed to be tested for HIV, the proportion of patients who returned to receive test results, and the proportion of those with positive test results who were successfully linked to an OPC for HIV care and treatment. To assess the services related to care and treatment at the OPCs, we calculated the proportion of ART-eligible patients who had not yet initiated ART and the proportions of patients who tested positive for heroin or other substances, such as amphetamines, methamphetamines, morphine or benzodiazepines, to see the trend of substance abuse while on MMT.
For pre-ART, ART and MMT patients, we calculated the rates in person-years for LTFU and death. We assumed that the number of patients reported by the end of 1 month would be the number of patients ‘at risk’ the following month. We calculated person-months by summing the number of patients from the corresponding month-end reports. As the exact date of LTFU/death or registering at the clinic in the month was not recorded, the observed follow-up time was one half month. For example, if the number of patients reported was 100 by the end of January and 120 by the end of February, the number of person-months of observation in February was 110 (100 + [120–100] * 0.5). The number of person-years was equal to the number of person-months divided by 12. The definitions for LTFU were based on the Viet Nam national guidelines: pre-ART patients who did not receive care at an OPC within 180 days; ART patients who did not receive ART for 90 consecutive days; and MMT patients who did not receive methadone for 30 consecutive days.
Differences in the proportions and rates calculated before and after integration were assessed with the χ2 test or Fisher's exact test. P < 0.05 was considered significant.
RESULTS
Most indicators for service delivery or patient outcomes that were assessed were maintained or improved following integration (Tables 2 and 3). For VCT services, the number of clients seeking VCT services increased following integration at all seven sites; the proportion of clients who agreed to be tested for HIV remained consistently high (>99%) following integration at the sites where three services were integrated, and increased slightly, from 96.5% to 99.7% (P < 0.05), at sites where two services were integrated (Table 2). The proportion of VCT patients with HIV infection successfully registered at OPCs increased following integration at the three-service sites from 70.5% before integration to 81.3% after integration (P < 0.05), while a slight non-significant decrease was noted at the two service sites, from 86.2% before integration to 75.6% after integration (P = 0.06; Table 2).
TABLE 2.
Comparison of proportions of indicators for routine activities before and after the integration of VCT, OPC and MMT, HCMC, Viet Nam
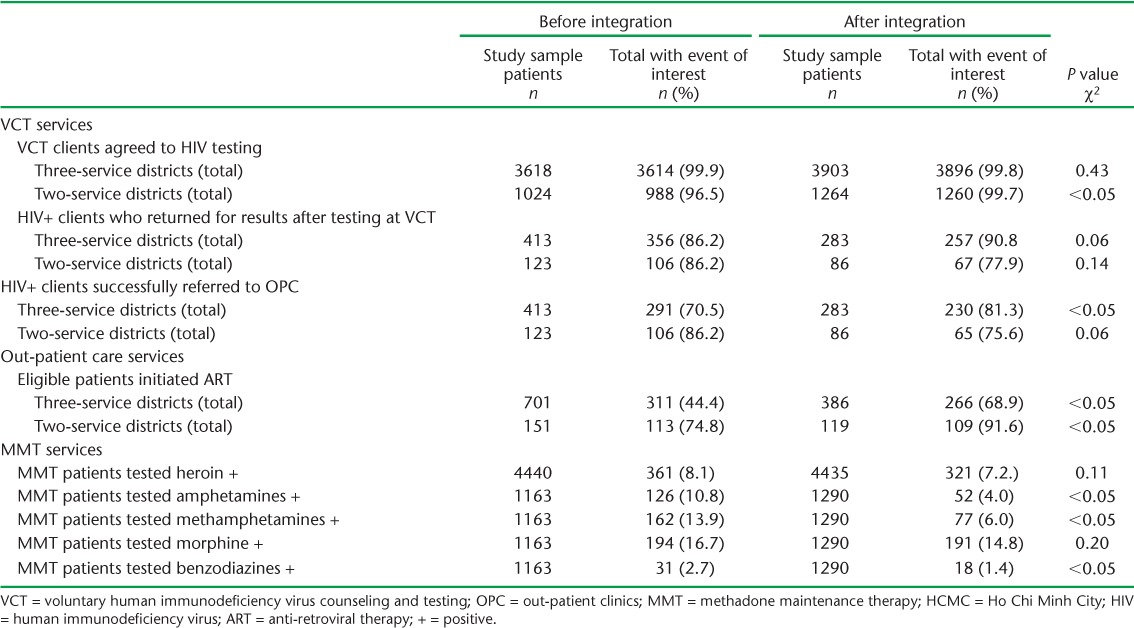
TABLE 3.
Comparison of LTFU and death rates among patients with HIV before and after the integration of voluntary testing and counseling, out-patient care and methadone maintenance therapy services before and after integration, Ho Chi Minh City, Viet Nam
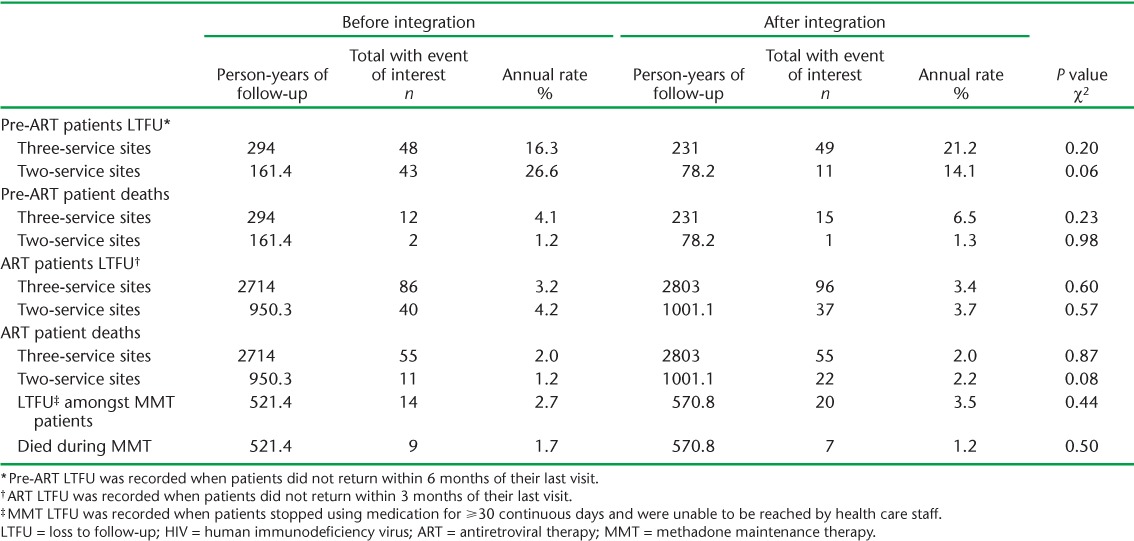
We observed a marked increase in the proportion of patients eligible for ART who initiated ART in both the three-service sites, from 44.4% before integration to 68.9% after integration (P < 0.05), and the two-service sites, from 74.8% before integration to 91.6% after integration (P < 0.05). Among pre-ART patients receiving out-patient care, the rate of LTFU did not change significantly in either the two- or three-service sites (Table 3). Similarly, we did not observe significant differences in the before and after integration rates of death among pre-ART patients (Table 3). Among ART patients, the rates of LTFU and death were both low prior to integration at all sites and did not change significantly after integration (Table 3).
Among patients receiving MMT, we observed significant decreases in the proportions of patients who tested positive for amphetamines, methamphetamines, morphine or benzodiazepines following integration. Non-significant decreases in the proportions of patients who tested positive for heroin and morphine (Table 2) were observed following integration. Among MMT patients, the rates of both LTFU and death were low prior to integration at all sites, and did not change significantly following integration (Table 3).
DISCUSSION
In this rapid assessment using routinely collected data, we observed similar outcomes among patients who received services before and after service integration in both sites with three (VCT, OPC and MMT) integrated services and sites with two (VCT and OPC) integrated services.
While there is also little available information regarding the quality of care in an integrated system relative to non-integrated services, Sullivan et al. found that the integration of buprenorphine for the treatment of opioid dependence into existing HIV clinical care was feasible and led to decreases in patients' opioid use and maintenance or improvement in biological markers for HIV.8 Other studies have suggested that the integration of ART into opioid substitution treatment services yielded comparable rates of ART retention and mortality.4,5,9 Similarly, we found that most evaluated outcomes that represent coverage, retention and mortality within the three services remained the same or improved following service integration.
The program improvements we observed should be interpreted with caution, as this was a pre-post design without a control group, limiting attributions of causality. In addition, using aggregate data limited our ability to assess the integrated system among important subpopulations. Although we did not have the resources to use an experimental study design, we believe our results are meaningful, as such ideal studies are infeasible in low-resource settings such as Viet Nam. Although some of the improvements noted might have resulted from the integration itself, improvements may also be the result of other program quality improvement activities. For example, the late initiation of ART among eligible patients was recognized prior to integration as an area in need of improvement, and PAC and OPC site staff prioritized efforts to increase early ART initiation among patients at all sites. In addition, one factor that would have a positive impact on late ART initiation is the issuance of the Ministry of Health guidelines, ‘Management, monitoring and treatment for HIV/AIDS infected or exposed people’ (Circular No. 32),10 which allowed the pre-ART counseling procedure to be flexible. Patients were not obliged to attend six sessions of counseling, which took approximately 30 days or more. Because we used routinely reported aggregate data, we were not able to examine differences in the demographics of patient populations before and after integration that may have influenced our findings, or to look specifically at the subset of patients receiving both HIV and MMT services. In addition, the CD4 cell count is believed to impact the retention rate of ART patients, as it affects patients' health. CD4 data are not included in the routinely reported apgregote data that were used for the analysis. In another study of a population of ART patients in six clinics in HCMC (of which three are among our seven surveyed clinics) from January to December 2014, however, the mean and median values of CD4 cell counts of 660 sampled ART patients were 465 cells/mm3 and 436 cells/mm3. It is reasonable to believe that patients in this study possessed similar immunologic characteristics, such as CD4 counts, as there was no difference in HIV care and treatment programs among clinics in HCMC at the time. We do not believe, therefore, that differences in CD4 counts before and after integration would have affected retention rates. Finally, it is reasonable to assume that staff become more effective and efficient in their roles as time passed, and this may also be responsible for some of the noted improvements.
Without an in-depth and time-consuming evaluation, we utilized routinely collected data to provide a quick assessment of program performance. Our analyses indicate that in the 6 months following integration of clinical services (VCT, OPC and MMT at four sites and VCT and OPC at three sites), key indicators regarding the quality of care (i.e., receipt of HIV test results), linkage from VCT to out-patient HIV care, retention and mortality, were maintained or improved. As financial resources from donors continue to decline, these results provide some indication that integration of services in the current context does not lead to a decline in the quality of care. While we did not conduct an economic evaluation of the integrated system, we believe the integrated system will prove more efficient and sustainable, as outcomes were maintained with a reduction in staff. These results have encouraged the scale-up of the integrated model throughout Ho Chi Minh City. Future programmatic evaluations should assess clinical outcomes such as CD4 changes, treatment adherence, and rates of drug resistance and viral suppression, ideally through the use of individual patient data.
Acknowledgments
The authors would like to thank the staff from all the district preventive medicine centers in Ho Chi Minh City who participated in the integration, implementation and evaluation; M Ackers for her careful review and support of this work; the Ho Chi Minh City Provincial AIDS Committee.
Footnotes
Conflicts of interest: none declared.
References
- 1.United Nations Office on Drugs and Crime. World Drug Report 2014. New York, NY, USA: UN; 2014. [Google Scholar]
- 2.Ho Chi Minh City Provincial AIDS Committee (PAC) The 2014 plan for sentinel surveillance on HIV/STI and integrated bio-behavioral survey. Internal Document. Ho Chi Minh City, Viet Nam: PAC; 2014. [Google Scholar]
- 3.UNAIDS. People who inject drugs must not be left behind. Geneva, Switzerland: UNAIDS; 2014. http://www.unaids.org/en/resources/presscentre/featurestories/2014/december/20141216_PCB_PWID Accessed November 2016. [Google Scholar]
- 4.Suthar A B, Rutherford G W, Horvath T, Doherty M C, Negussie E K. Improving antiretroviral therapy scale-up and effectiveness through service integration and decentralization. AIDS. 2014;28(Suppl 2):175–185. doi: 10.1097/QAD.0000000000000259. [DOI] [PubMed] [Google Scholar]
- 5.Achmad Y M, Istiqomah A N, Iskandar S, Wisaksana R, van Crevel R, Hidayat T. Integration of methadone maintenance treatment and HIV care for injecting drug users: a cohort study in Bandung, Indonesia. Acta Med Indones. 2009;41(Suppl 1):S23–S27. [PubMed] [Google Scholar]
- 6.Van Tieu Thi Thu Integration of methadone maintenance treatment (MMT) with HIV services to encourage HIV testing and retention in care among injection drug users. E-Poster at International Congress on AIDS in Asia and the Pacific (ICAAP) 12, Bangkok, Thailand: ICCAPP 2013.
- 7.Tran B, Ohinmaa A, Duong A et al. Cost-effectiveness of integrating methadone maintenance and antiretroviral treatment for HIV-positive drug users in Vietnam's injection-driven HIV epidemics. Drug Alcohol Depend. 2012;125:260–266. doi: 10.1016/j.drugalcdep.2012.02.021. [DOI] [PubMed] [Google Scholar]
- 8.Sullivan L, Barry D, Moore B et al. A trial of integrated buprenorphine/naloxone and HIV clinical care. Clin Infect Dis. 2006;43(Suppl 4):S184–S190. doi: 10.1086/508182. [DOI] [PubMed] [Google Scholar]
- 9.Zaller N, Gillani F S, Rich J D. A model of integrated primary care for HIV-positive patients with underlying substance use and mental illness. AIDS Care. 2007;19:1128–1133. doi: 10.1080/09540120701335196. [DOI] [PubMed] [Google Scholar]
- 10.Viet Nam Ministry of Health (MOH) Management, monitoring and treatment for HIV/AIDS infected or exposed people (Circular 32/2013/TT-BYT) Hanoi, Viet Nam: MOH; 2013. [Google Scholar]


