Abstract
Non-traumatic small bowel perforation is rare in adults but carries a high morbidity and mortality. The diagnosis is made on clinical suspicion, and the most common causes in developing countries are infectious diseases, being cytomegalovirus infection in immunocompromised patients the main etiology. We describe a patient with a recently diagnosed advanced stage HIV infection and an intestinal perforation associated with cytomegalovirus immune reconstitution inflammatory syndrome after highly active antiretroviral therapy initiation.
Keywords: Small bowel, Intestinal perforation, Non-traumatic perforation, Cytomegalovirus, IRIS
Highlights
-
•
Cytomegalovirus (CMV) is the main etiology of non-traumatic perforation of the small bowel in immunocompromised individuals.
-
•
We describe a case of CMV associated Immune reconstitution inflammatory syndrome.
-
•
To our knowledge this is the first case of small bowel perforation due to IRIS related CMV.
-
•
It is of importance for the clinician to consider CMV related IRIS as a cause of acute abdomen.
1. Introduction
Non-traumatic small bowel perforation is rare, both in the general population and in patients with HIV [1]. Immune reconstitution inflammatory syndrome (IRIS) is a condition seen in some cases of AIDS or other immunosuppressive conditions, in which the recovery of the immune system causes an exaggerated inflammatory response to a previously acquired opportunistic infection. Among its causes are cytomegalovirus infection and manifestations of IRIS. Cytomegalovirus (CMV) infection usually presents in immunocompetent patients as a mononucleosis-like syndrome which almost always is self-limiting but in immunocompromised patients it commonly causes organ-specific damage such as retinitis, polyradiculopathy, meningoencephalitis, esophagitis, and colitis. All of these can cause disability or even death if they are not treated promptly and adequately [2].
In this report we describe a case of small bowel and colon perforation due to CMV related IRIS, which is not a entity frequently thought for the clinician in the differential diagnosis of intestine perforation, highlighting the importance of consider IRIS as a cause of acute abdomen complication in the AIDS patient after the initiation of antiretroviral therapy, specially those with baseline low CD4+ count.
2. Presentation of case
The patient, a 40-year–old male who has sex with men, entered the hospital in July 2015 due to severe diffuse abdominal pain. He was diagnosed with HIV-1 two months prior with CD4+ baseline level of 54 cells/mm3. Antiretroviral regimen was started one month before admission consisting of tenofovir disoproxil fumarate, emtricitabine, and efavirenz. Also, one month before hospitalization, he was treated with oral valganciclovir because of CMV retinopathy diagnosis, manifested as a decrease in visual acuity. In this occasion on physical exploration, the patient presented abdominal pain on gentle palpation, rebound tenderness, and abdominal wall rigidity. On a CT of the abdomen splenomegaly, multiple lymphadenopathy and free fluid in the abdomen were found. On admission, blood tests showed a CMV viral load in total blood of 10 copies/mL and an undetectable HIV viral load (<20 copies/mL); the leukocyte count was 12,000 cells/μL. At the ophthalmologic exploration, chorioretinitis and macular edema were found. Subsequently, optical coherence tomography of both eyes showed a normal central retina with a central macular thickness of 264 μm, while in the left eye a diffuse macular thickening of 744 μm at the center point with the presence of intraretinal cysts in all layers of the retina was observed; this changes compatible with macular edema. No data of retinitis or cell inflammation in the vitreous cavity were found; something we would expect in a case of CMV retinitis.
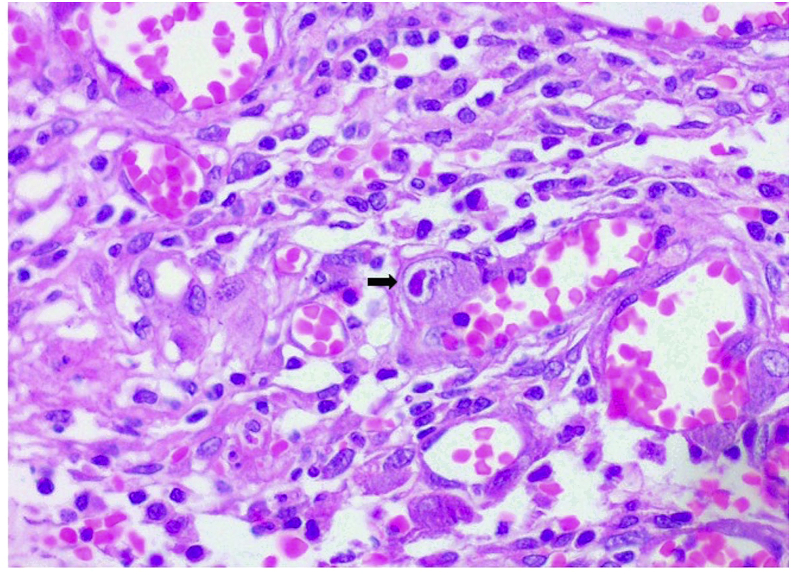
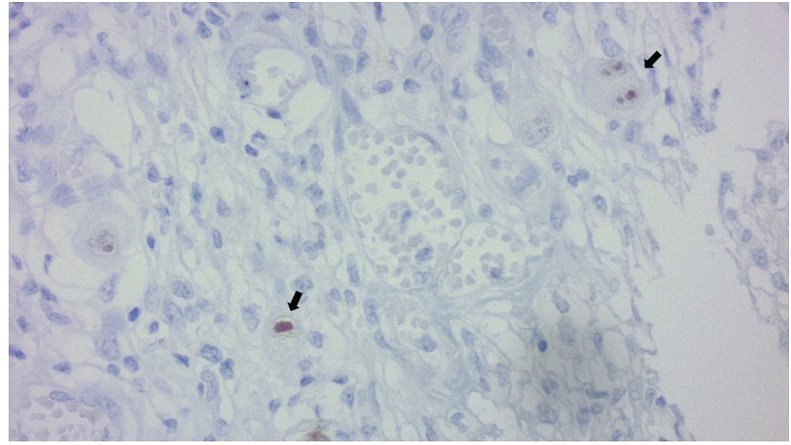
The patient was taken to the operating room and an exploratory laparotomy was performed. A perforation one meter distal to the Treitz angle in the jejunum was found, so a side-to-side anastomosis of the small bowel was performed and vancomycin, caspofungin, levofloxacin and ganciclovir were started. Acute and chronic inflammation was found in histopathological sections with cytopathic changes consisting of cells with enlarged nuclei surrounded by a clear halo (Fig. 1), these were associated to acute peritonitis and lymphoid hyperplasia of Peyer's patches. Areas of recent bleeding, ulceration, and erosion zones with granulation tissue were also seen CMV presence in the tissue was confirmed by immunohistochemistry (Fig. 2). The patient was discharged home 17 days after surgery and seven days later antiretrovirals were reinitiated and CMV treatment was switched from gancylclovir to oral valganciclovir.
Fig. 1.
Arrow indicates cytoplasmic inclusion in cytomegalovirus-infected cell.
Fig. 2.
Cytomegalovirus infected cells evidenced by immunohistochemistry.
The patient was readmitted 15 days later after sudden, severe, generalized abdominal pain. Rebound tenderness was found on exploration, therefore a new exploratory laparotomy was done finding multiple adhesions, and dissection of the colon at the splenic angle flexure. A colonic perforation without local abscesses was detected and intestinal resection, colostomy and a mucocutaneous fistula were done. A second histopathology study described a perforated wall and ulcerated colon associated with a mixed inflammatory process with a foci of granulomatous reaction and cytopathic changes suggestive of CMV. Subsequently, the patient was restarted on intravenous ganciclovir until the oral route was feasible after that, oral valganciclovir was given.
3. Discussion
Small bowel perforation in adults can result from obstruction that causes gangrene, hernia strangulation or trauma [3]. Traumatic small bowel perforation is not uncommon but can be fatal, subsequent peritonitis can lead to multi-organ failure and death unless prompt therapy is established [1]. Furthermore, perforation of the terminal ileum should be considered as a possibility in the case of dark peritonitis [4]. Non-traumatic perforation of the small intestine is rare, with an incidence of 1 case per year per 350,000 inhabitants with a mortality of 15–39%; some authors attribute this to a non-specific clinical picture resulting in a delayed diagnosis [5].
The clinical picture of small intestine perforation is non-specific [1]. Wani et al. published in 2006 a review of 79 cases. All patients had abdominal pain but only 32% presented rigidity. Also, only 57% had fever, and leukocytosis was present in 29% of cases [4]. The diagnosis was mainly clinical with imaging studies showing free gas with a low diaphragm in some cases (17–37% are evident on radiography, but generally, the cause is established after surgical treatment) [1], [3], [5].
Sometimes perforation is contained because of its retroperitoneal location, with development of an abscess, and an insidious clinical picture. This is in contrast with free perforation in which the clinical picture is more spectacular and sudden [3].
Causes of non-traumatic perforation of the small bowel can be divided into inflammatory (eg, Crohn's disease); infectious, associated with drugs such as indomethacin; congenital (Meckel's diverticulum); metabolic (homocysteinuria); vascular (granulomatous arteritis); and due to primary and secondary malignancies [3]. The most common causes in the general population in developing countries are tuberculosis and typhoid disease, while in developed countries, the main etiologies are Crohn's disease and neoplasms [1].
CMV has been found as the main etiology of non-traumatic perforation of the small intestine in immunocompromised individuals. Other infectious causes include tuberculosis, Entamoeba histolytica, and Ascaris lumbricoides [3]. The most common cause of intestinal perforation in AIDS patients is CMV infection and it is responsible for most emergency laparotomies in these patients. The main location is in the colon (53%), followed by the distal ileum (40%) and the appendix (7%) [6], [7].
The main organs involved in CMV infection in patients with HIV are the retina and the gastrointestinal system [8]. CMV was a common cause of gastrointestinal disease in patients with HIV, but after the introduction of highly active antiretroviral therapy (HAART) in 1996, there has been a dramatic decrease in its incidence; there has even been a decrease in incidence in those who fail virologic suppression with HAART. CMV infection is typically associated with CD4 levels <50 cells/μL9. In the case of intestinal perforation, larger cases series were published prior to the introduction of antiretrovirals [10], [11]. Afterwards, only case reports were found in the literature [12], [13], [14].
The pathogenesis of gastrointestinal CMV disease is believed to be submucosal vasculitis with thrombosis resulting in ischemia, thinning of the intestinal wall with subsequent perforation and gangrene [8]. Perforated intestinal ulcers caused by CMV infection in patients with HIV can usually be single or multiple [3], [7]. The diagnosis is made by histopathological analysis, especially in lesions observed macroscopically normal [7]. The gold standard for diagnosis continues to be the discovery of cytomegalic cells using H&E. Cells have Cowdry inclusions with a surrounding halo. Infection is confirmed by immunohistochemistry; both techniques have a sensitivity of 97% and a specificity of 100% [9]. Serology is of little use because localized disease can be negative, as in the case of our patient [7].
Regarding treatment, surgery involves resection and ileostomy or colostomy. Primary anastomosis is not recommended because there tend to be anastomotic complications and contamination of the peritoneal cavity with a high incidence of perforations in other sections of the intestine, postoperatively [8].
IRIS syndrome is a paradoxical condition in the patient with previously incompetent immunity that manifests as clinical worsening after the recovery of the immune system's ability to mount a vigorous inflammatory response [15]. HIV patients in advanced stages, with lower CD4+ counts at the start of antiretroviral therapy have an increased risk of developing IRIS. There is a multiple mechanisms that explain IRIS such as a quantitative restoration of immunity, an improvement in function and phenotypic expression or host genetic susceptibility to antigenic stimulus upon immune restoration [17].
In the case of IRIS associated with CMV, it is characterized as any type of ocular inflammation such as anterior uveitis, vitritis, papillitis or macular edema. It appears in about one-third of patients in whom CMV infection occurs before the start of antiretroviral treatment, with a mean time presentation of IRIS four weeks after starting therapy [16]. Appendicitis secondary to CMV immune reconstitution syndrome has been previously reported as an infrequent manifestation [2], but to our knowledge this is the first case of small intestine perforation due to CMV infection as a manifestation of IRIS.
This report is consistent with the SCARE (Consensus-based surgical case report guidelines) criteria [18].
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Sources of funding
We thank the University Hospital “Dr. Jose Eleuterio Gonzalez” of the Autonomous University of Nuevo Leon, Monterrey México for the support on the realization of this article.
Author contribution
Collection, analysis and interpretation of the data, study design, writing of the manuscript: Eva M Gutiérrez-Delgado; Collection, analysis and interpretation of the data, writing of the manuscript: Hiram Villanueva-Lozano, study design, analysis and interpretation of the data: Javier Ramos-Jiménez; interpretation of pathology results and study design: Ivett C. Miranda-Maldonado, Interpretation of Ophtalmology results and collection of the data: Miguel J. García Rojas-Acosta.
Conflicts of interest
The authors certify that they have NO affiliations with or involvement in any organization or entity with any financial interest, or non-financial interest in the subject matter or materials discussed in this manuscript.
Guarantor
Ramos-Jimenez Javier.
Head of Infectious diseases division, Hospital Universitario Dr José Eleuterio González, Universidad Autonoma de Nuevo Leon.
Gonzalitos y Madero SN, Mitras Centro. Monterrey NL, México.
Phone: +52 (81) 83485013.
E mail: javramos31@hotmail.com.
Contributor Information
Eva María Gutiérrez-Delgado, Email: evagutierrez_84@hotmail.com.
Hiram Villanueva-Lozano, Email: dr.villanueval@hotmail.com.
Miguel J. García Rojas-Acosta, Email: drgaroaretina@gmail.com.
Ivett C. Miranda-Maldonado, Email: imiranda77@hotmail.com.
Javier Ramos-Jiménez, Email: javramos31@hotmail.com.
References
- 1.Eid H.O., Hefny A.F., Joshi S., Abu-Zidan F.M. Non-traumatic perforation of the small bowel. Afr. Health Sci. 2008;8(1):36–39. [PMC free article] [PubMed] [Google Scholar]
- 2.Faldetta K.F., Kattakuzhy S., Wang H.-W., Sereti I., Sheikh V. Cytomegalovirus immune reconstitution inflammatory syndrome manifesting as acute appendicitis in an HIV-infected patient. BMC Infect. Dis. 2014;14(1):1. doi: 10.1186/1471-2334-14-313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Freeman H.J. Spontaneous free perforation of the small intestine in adults. World J. Gastroenterol. 2014;20(29):9990–9997. doi: 10.3748/wjg.v20.i29.9990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wani R.A., Parray F.Q., Bhat N.A., Wani M.A., Bhat T.H., Farzana F. Nontraumatic terminal ileal perforation. World J. Emerg. Surg. 2006;1(1):1. doi: 10.1186/1749-7922-1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kimchi N.A., Broide E., Shapiro M., Scapa E. Non-traumatic perforation of the small intestine. Report of 13 cases and review of the literature. Hepatogastroenterology. 2001;49(46):1017–1022. [PubMed] [Google Scholar]
- 6.Chui D.W., Owen R.L. AIDS and the gut. J. Gastroenterol. Hepatol. 1994;9(3):291–303. doi: 10.1111/j.1440-1746.1994.tb01729.x. [DOI] [PubMed] [Google Scholar]
- 7.Michalopoulos N., Triantafillopoulou K., Beretouli E., Laskou S., Papavramidis T.S., Pliakos I., Hytiroglou P., Papavramidis S.T. Small bowel perforation due to CMV enteritis infection in an HIV-positive patient. BMC Res. Notes. 2013;6(1):1. doi: 10.1186/1756-0500-6-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shiekh R.A., Yasmeen S., Prindiville T.P. Intestinal perforation and peritonitis in AIDS: case series and review of the literature. JK - Pract. 2004;11(4):248–256. [Google Scholar]
- 9.Baroco A.L., Oldfield E.C. Gastrointestinal cytomegalovirus disease in the immunocompromised patient. Curr. Gastroenterol. Rep. 2008;10(4):409–416. doi: 10.1007/s11894-008-0077-9. [DOI] [PubMed] [Google Scholar]
- 10.Meza A.D., Bin-Sagheer S., Zuckerman M.J., Morales C.A., Verghese A. Ileal perforation due to cytomegalovirus infection. J. Natl. Med. Assoc. 1994;86(2):145. [PMC free article] [PubMed] [Google Scholar]
- 11.Kram H.B., Shoemaker W.C. Intestinal perforation due to cytomegalovirus infection in patients with AIDS. Dis. Colon Rectum. 1990;33(12):1037–1040. doi: 10.1007/BF02139220. [DOI] [PubMed] [Google Scholar]
- 12.Ribera Irigoin R., Funes Liebana R., Poveda Gomez F., Medina Cano F., Prieto de Paula J. Perforación ileal secundaria a infección por citomegalovirus. Rev. Esp. Enf. Dig. 2005;97(1):60–61. doi: 10.4321/s1130-01082005000100009. [DOI] [PubMed] [Google Scholar]
- 13.Rodríguez R.M.J., Moreno A.M.P., Algarrada J.S., González J.M., Cartes J.M., Vacaro J.A.M. Megacolon tóxico y perforación yeyunal por citomegalovirus. Cir. Esp. 2007;82(1):44–45. doi: 10.1016/s0009-739x(07)71661-5. [DOI] [PubMed] [Google Scholar]
- 14.Shah S.K., Kreiner L.A., Walker P.A., Klein K.L., Bajwa K.S., Robinson E.K., Millas S.G., Souchon E.A., Wray C.J. Cytomegalovirus enteritis manifesting as recurrent bowel obstruction and jejunal perforation in patient with acquired immunodeficiency syndrome: rare report of survival and review of the literature. Surg. Infect. (Larchmt) 2012;13(2):121–124. doi: 10.1089/sur.2010.098. [DOI] [PubMed] [Google Scholar]
- 15.Shahani L., Hamill R.J. Therapeutics targeting inflammation in the immune reconstitution inflammatory syndrome. Transl. Res. 2016;167(1):88–103. doi: 10.1016/j.trsl.2015.07.010. [DOI] [PubMed] [Google Scholar]
- 16.Ruiz-Cruz M., Alvarado-de la Barrera C., Ablanedo-Terrazas Y., Reyes-Terán G. Proposed clinical case definition for cytomegalovirus–immune recovery retinitis. Clin. Infect. Dis. 2014;59(2):298–303. doi: 10.1093/cid/ciu291. [DOI] [PubMed] [Google Scholar]
- 17.Bosamiya S.S. The immune reconstitution inflammatory syndrome. Indian J. Dermatol. 2011;56(5):476–479. doi: 10.4103/0019-5154.87114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Agha R.A., Fowler A.J., Saeta A., Barai I., Rajmohan S., Orgill D.P., Group S.C.A.R.E. The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]