Abstract
Waterpipe tobacco usage is spreading rapidly worldwide, with reports of more youth being waterpipe users compared to adults. In many areas of the world, waterpipe usage surpasses cigarette smoking. Waterpipes and cigarettes are both mechanisms for inhalation of tobacco smoke and therefore have serious health consequences. However, because of the many differences between the two products, prevention and control strategies that have proven effective for cigarettes may not transfer readily to waterpipe. This report highlights the differences between waterpipes and cigarettes in toxicant exposure and physiologic effects, patterns of use, social norms, the extent of evidence, and the policy environment. There is little evidence to date around effective interventions for waterpipe prevention and control. The current state of evidence for intervention to curb or control waterpipe is at ground zero and critically needs attention from both scientists and policy makers. National and global efforts aimed at cigarette prevention have succeeded, particularly in developed countries. We suggest the time has come to harness what we know works for cigarette prevention and control and adapt it to tackle the growing epidemic of waterpipe tobacco use.
Keywords: waterpipe, interventions, cigarette, evidence
Introduction
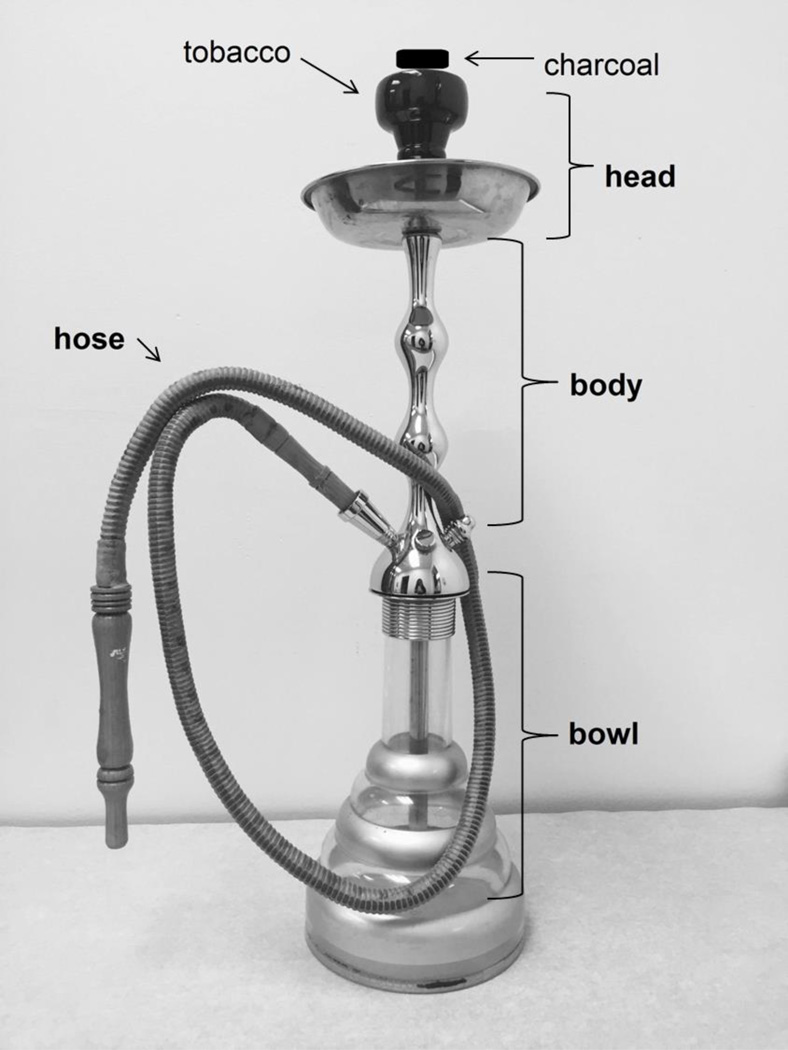
Waterpipe tobacco smoking (WTS; Maziak et al., 2004) is spreading rapidly worldwide, particularly among youth (Maziak, 2015; Maziak, Ben Taleb, et al., 2015a). A waterpipe, also known as arghile, hookah, narghile, or shisha, is composed of the head where the tobacco is placed, a body, a water bowl, a hose and a mouthpiece (Figure 1; see also Maziak et al., 2004). The instrument's design allows smoke to pass through the water or other liquid before reaching the smoker [World Health Organization (WHO), 2015a]. In many countries, WTS prevalence among youth surpasses prevalence among adults (Akl et al., 2011; Maziak, Ben Taleb et al., 2015a). In addition, WTS prevalence often exceeds cigarette smoking prevalence among youth globally (Maziak, 2011; Wareen et al., 2009; Barnett et al., 2013; Jawad, Lee and Millett, 2016). A recent analysis of Global Youth Tobacco Survey results among 13–15 year olds in 25 countries around the world has indicated rates of current WTS of over 20% in 6 countries (Jawad et al., 2016). Accumulating research indicates serious health effects associated with WTS (Bou Fakhreddine et al., 2014; El Zaatari et al., 2015; Akl et al., 2010; Jawad et al., 2013; Al Ali et al., 2013; WHO, 2015a). Clearly there is a need for urgent action to prevent and control WTS.
Figure 1.
Narguile waterpipe (shisha, hookah)
Cigarette tobacco smoking (CTS), though historically a more recent type of tobacco use, has garnered much more attention due to its relatively high prevalence worldwide and clearly documented increases in cigarette-caused dependence, disease, disability, and death (U.S. Department of Health and Human Services, 2014; WHO, 2015b). Effective interventions have been identified to prevent and control CTS at the individual, interpersonal, organizational, community, and policy level [U.S. Department of Health and Human Services (USDHHS), 2014; WHO, 2015b] culminating with the implementation of the first world health treaty in 2003: the Framework Convention on Tobacco Control (FCTC; WHO, 2003). The FCTC sets out evidence-based policy interventions to control tobacco use generally, but its specific guidelines are for the most part particular to cigarettes. For example, Article 16.3 of the FCTC states that “Each Party shall endeavor to prohibit the sale of cigarettes individually or in small packets which increase the affordability of such products to minors,” thus aiming to discourage the purchase and consumption of cigarettes among minors.
CTS and WTS are both mechanisms for inhalation of tobacco smoke and both therefore have serious health consequences. Both behaviors are a result of a variety of factors at the individual psychosocial, interpersonal, organizational, community normative, and policy levels (Fong et al., 2006; Nakkash et al., 2011; Akl et al., 2015; Jawad et al., 2015). Although previous reviews of WTS have focused on its epidemiology and determinants, and often compared aspects of those to CTS, none have addressed specifically how the differences between these two methods of tobacco use affect intervention development and implementation. Because of the many differences between the two products, CTS prevention and control strategies may not transfer readily to WTS. Instead, the interventions that have proven effective at the various ecological levels for CTS prevention and control will need to be adapted to address WTS specifically. Below we highlight the differences between CTS and WTS in toxicant exposure and physiologic effects, patterns of use, social norms, the extent of evidence, and the policy environment. We then suggest how these differences indicate the necessity for a distinctive approach to WTS prevention and control.
Toxicant Exposure & Physiological Effects
A waterpipe emits many of the same toxicants as a cigarette does and, due to the large volume of smoke inhaled in a single waterpipe use session, the amount of these toxicants in waterpipe smoke is often many times more than the amount found in the smoke of a single cigarette (Shihadeh et al., 2015). The volume of smoke is greater due to the cooler temperature of the smoke and lower draw resistance of the waterpipe: the volume from a single puff from a waterpipe can range from approximately 500 to 900 mL, compared to a volume from a single puff on a cigarette ranging from 50 to 100 mL (e.g., Cobb et al., 2011; Blank et al., 2011; Brinkman et al., 2015). Within a 45-minute WTS episode, users take 50 or more puffs, while a single cigarette is consumed in approximately 10 puffs, meaning that WTS involves inhalation of 25 or more liters of smoke, as compared to about 1 liter for a single tobacco cigarette (e.g., Cobb et al., 2011; Maziak et al., 2009; Brinkman et al., 2015).
Like cigarette smoke, waterpipe smoke contains “tar” and carbon monoxide (CO). The tar is composed of at least 82 toxicants, including carcinogenic polyaromatic hydrocarbons (PAH) and tobacco-specific nitrosamines (TSNA), as well as carbonyl compounds and volatile organic compounds that can contribute to pulmonary disease (Shihadeh et al., 2015). Intake of PAH differed between cigarette and waterpipe smokers, with the greater molecular weight PAHs being higher in waterpipe smoke, suggesting a higher risk for cancer in such smokers (Jacobs et al., 2013). Exposure to TSNA in waterpipe smokers was similar to that of pack-a-day cigarette smokers (Al Ali et al., 2015). Metabolites of both these compounds have been found in waterpipe smokers (Jacob et al., 2013, Al Ali et al., 2015).
There are also reports of higher amounts of metals and volatile organic compounds in the smoke emitted by a waterpipe relative to that of a single cigarette, and these toxicants include cobalt, chromium, nickel, cadmium, lead, and benzene, with benzene mainly released by the burning charcoal (Shihadeh et al., 2015). Heating the waterpipe tobacco (particularly the flavored ‘ma’aasel’) has also been reported to release a number of other chemical toxicants, including furanic compounds (Schubert et al., 2012a) and toxic carbonyls such as formaldehyde and acetaldehyde (Schubert et al., 2012b). Formaldehyde is a class 1 carcinogen (IARC, 2006), and acetaldehyde is classified as possibly carcinogenic to humans (IARC, 1999).
The CO in waterpipe smoke is on the order of 30 times that of a cigarette (Schubert et al., 2011). Expired breath CO levels from waterpipe smokers after a single waterpipe use episode have been reported to be, on average, 3–6 times those seen after a single cigarette (Eissenberg & Shihadeh, 2009; see also Salameh, Aoun, & Waked, 2009; Singh et al., 2011;). Nicotine is an important toxicant to examine, as it is the tobacco smoke constituent that supports compulsive use (i.e., dependence) in cigarette smokers (USDHHS, 1988) and waterpipe tobacco smokers (Aboaziza & Eissenberg, 2015). Due to the long duration of a WTS session, waterpipe users receive almost twice the nicotine in a single WTS session compared to the exposure from a single cigarette (Eissenberg & Shihadeh, 2009). In terms of nicotine exposure, daily waterpipe use is estimated to be equivalent to smoking 10 cigarettes per day (Neergaard et al., 2007). While many waterpipe smokers deny dependence and believe they can stop at any time (Afifi et al., 2013) those who desire to quit are often unsuccessful (Auf et al., 2012; Ward et al., 2005; Ward et al., 2013). At least in some users, WTS supports nicotine/tobacco dependence (Salameh et al., 2014; Kassim et al., 2014; Auf et al., 2012; Sidani et al., 2016)
As a result of exposure to all these toxicants, WTS has many of the same health risks as CTS (American Lung Association, 2007). Similar to cigarette smokers, waterpipe users are at risk to a number of diseases, including lung, stomach, and esophageal cancers, impaired pulmonary function, and cardiovascular disease, among others (Akl et al., 2010; Cobb et al., 2010; El Zaatari et al., 2015).
WTS age of initiation, use patterns and perceptual and social components
The patterns of WTS are different compared to those of CTS. Among college students in the United States, WTS is the second most popular tobacco product after cigarettes, with more than half of current waterpipe users also being non-cigarette smokers (Primack et al., 2013). In cultures where WTS has long been practiced, the age of initiation of WTS can happen at quite an early age (Alzyoud et al., 2016). Ever WTS was 44% in a national sample of 6th and 7th graders in Lebanon (Jawad et al., 2015), with higher rates of ever and current WTS compared to CTS in 7th graders in Irbid Jordan (Mzayek et al., 2012). In addition, the pattern of waterpipe smoking may differ from that of cigarette smoking; whereas cigarettes are mostly smoked daily, waterpipes are mostly smoked intermittently (Maziak et al., 2015a). Also whereas one cigarette can be smoked in minutes and often in conjunction with other activities (e.g., walking, driving), a waterpipe smoking session can last up to an hour and, due to the nature of the apparatus and the set-up required, restricts the user’s ability to perform some other activities simultaneously.
Compared to cigarettes, waterpipe use has a number of product-specific and appealing perceptual components such as the visual and tactile features of the device and its hose, the sight and smell of the voluminous smoke exhaled by the user, the fragrant smells of the tobacco itself, and the sounds produced from the bubbling water within the bowl (Nakkash et al., 2011; Ward, 2015). Traditionally, WTS is a social activity, with more than one person engaged in smoking from the same waterpipe via one or more hoses attached to the body (Blank et al., 2014). Waterpipes tend to be shared by more than one user when in the company of family members and friends, and they commonly are used in cafés or restaurants, especially amongst less-established users (Asfar et al., 2005). In these group settings in the natural environment, access to the hose may be limited when there are few waterpipes available, leading to an individual receiving fewer puffs with a longer inter-puff interval (Blank et al., 2014). On the contrary, if there is a smaller group or access to more than one waterpipe, individuals take a greater number of puffs (Blank et al, 2014). These group constraints on puffing topography may affect the nicotine and other toxicant content of the smoke and/or user exposure (Ramôa et al., 2016). Group use is thus also another salient difference between WTS and CTS, and may also need consideration in intervention development. Importantly though, group use may give way to individual use in the more dependent waterpipe smoker, potentially facilitated by personal ownership of the instrument itself (e.g., Sidani et al., 2016). Frequency and amount of WTS, location of use (public vs. private), the sharing of the waterpipe session, and the type of withdrawal symptoms experienced by smokers are all perceived to be related to dependence (Afifi et al., 2013; Sidani et al., 2016) and thus also are relevant to intervention at various levels.
Social Norms
Compared to CTS, the social norms surrounding WTS are quite different. For example, while some research has illustrated that WTS is socially acceptable, even in societies where any tobacco use among females is socially unacceptable (Akl et al., 2015; Ward et al., 2015), others have reported the negative image of women using waterpipes (Afifi et al., 2013; Khalil et al., 2013). Furthermore, regional differences also emerge regarding women using waterpipe. In Lebanon, WTS may be considered as a symbol of emancipation for women as compared to a disrespectful act to society in Egypt (Khalil et al., 2013). An important consideration is the age and marital status of the woman using a waterpipe; some consider it to be offensive if a young, single woman is using waterpipe while it is more acceptable for an older, married woman to be engaging in the same activity (Afifi et al., 2013). Family members also play an influential role in WTS initiation and continuation of use within the home and at social gatherings (Akl et al., 2015; Afifi et al., 2013). Parental figures tend to not discourage use in their children, with familial attitudes in Syria and Pakistan reported to be either neutral or positive when compared to CTS (Akl et al., 2015). Mother or father WTS has also been directly correlated with waterpipe use in youth as young as 11 years of age (Jawad et al., 2015). The apparent influence of parental smoking as well as research that has linked early initiation of WTS to higher dependency (Alzyoud et al., 2016), suggests parents as a potential target for intervention to prevent initiation. Social norms far outweigh health concerns in decision making around WTS (Afifi et al., 2013).
Policy Environment
The policy and regulatory environment of WTS does not easily mirror that of CTS. For example, while the United States Food and Drug Administration’s Center for Tobacco Products has the authority to regulate tobacco products generally, and currently regulates cigarettes, it does not regulate waterpipes and waterpipe tobacco at this time though some regulations are to come into effect in August, 2016 (FSPTCA, 2009; FDA, 2016). For example, the FDA recognizes concerns regarding the safety of waterpipe tobacco given the nicotine and carcinogens in waterpipe tobacco smoke, and the availability of waterpipe tobacco in a variety of flavors that could be appealing to youth and young adults. Thus, the FDA has included waterpipe tobacco within its regulatory scope of products subject to its tobacco control authority. Internationally, although the FCTC is intended to guide regulation of all tobacco products, policy statements on waterpipes have previously been based on evidence derived from cigarette policy effectiveness (WHO, 2014a) with a recent Framework Convention Alliance report acknowledging a number of policy challenges that differ for waterpipes. These included articles 6, 8, 11, and 13. For example, taxation of products (article 6) is an important consideration, as waterpipe tobacco is taxed at a lower rate compared to cigarettes (Jawad & Millett, 2014; Morris et al., 2012; WHO, 2014a). In addition, the actual waterpipe device and charcoal are untaxed, thus providing another target for taxation intervention. Indoor clear air legislation (article 8), with hookah bars claiming exemption (Noonan, 2010; WHO, 2014a), is another challenge and avenue to pursue in regards to policy interventions for public health protection.
Interestingly, deceitful labeling is another possible target for policy intervention. Nicotine content labelling – particular Ma’asel – seems unrelated to actual nicotine delivery (Vansickel et al., 2012). In addition, some labels misleadingly communicate that the waterpipe mouthpieces are efficient in reducing the risk of communicable disease, among other deceptive descriptors (Nakkash & Khalil, 2010). Other advertising may include such phrases as “diet shisha”, misleading consumers into false claims that waterpipe use may not only be healthy, but that it can be used to help lose weight as CTS is commonly associated with appetite control and weight loss (Audrain-McGovern & Benowitz, 2010). Deceitful labeling must be a target for intervention due to consumers’ lack of knowledge not only about the dangers of WTS previously aforementioned, but also due to false claims regarding its potential health benefits (Vansickel et al., 2012).
Extent of Supporting Evidence
Whereas the supporting evidence around the dangers of CTS and effective interventions is strong and based on over 50 years of robust research (U.S. Department of Health and Human Services, 2014; WHO, 2015b), a recent WHO document produced by the parties (countries) who are signatories to the FCTC noted: “Well documented experience with respect to WP tobacco products among the Parties is limited or non-existent. There are limited data available for Parties on consumption, manufacturing practices, advertising and promotional activities, contents, harmful effects and sociocultural factors associated with the use of WP.” (WHO, 2014b). Research gaps have been identified and span from identification of biomarkers of exposure to the influence of social practices on maintenance of use to long term health effects to indictors of dependence to effective interventions and many more (WHO, 2015a). To date, most WTS research has focused on intrapersonal and interpersonal determinants of use (Akl et al., 2015). A systematic review reported on health effects associated with WTS but the overall quality of the data included in the systematic review varied from very low to low and longitudinal studies are warranted (Akl et al., 2010). Interventions on waterpipe use reduction and cessation need to be developed and evaluated (Akl et al., 2015; Jawad et al., 2015a; Asfar et al., 2014).
Implications for WTS Interventions
What do these differences between CTS and WTS in toxicant exposure and physiologic effects, patterns of use, social norms, the extent of evidence, and the policy environment suggest in terms of the necessity for a distinctive approach to WTS prevention and control? A variety of interventions have been successful in decreasing CTS (WHO, 2016). The WHO’s M-POWER guidance document (2016) suggests effective measures to prevent tobacco use including: Monitor tobacco use and prevention policies, Protect people from tobacco smoke, Offer help to quit tobacco use, Warn about the dangers of tobacco, Enforce bans on tobacco advertising, promotion, and sponsorship, and to raise taxes on tobacco. In the text that follows, we point to how these measures may need to be adapted to WTS.
‘Warning about the dangers of tobacco smoke’ has led to reductions in CTS over time through mass media campaigns as well as school-based interventions (USDHHS, 2012; 2014). Many of the same toxicants, physiologic effects, and health consequences have been linked to WTS. One strategy then, might be crafting awareness campaigns for young people that compare WTS to CTS, pointing specifically to the similarities in toxicant exposure and tobacco-caused disease. Enlisting youth in this process likely will be critical to the success of these interventions, as they may be most aware of the messages that will resonate with their age group. In addition, the deceitful labeling must be highlighted in WTS awareness campaigns, potentially building on and adapting from past successful campaigns related to CTS (e.g., Farrelly et al., 2005; 2009). The differences in social norms between CTS and WTS also suggest the need for innovative strategies to warning about the dangers of waterpipe tobacco smoke. More specifically, raising awareness among parents may be as critical as raising awareness among youth. In some cultures, parents may be unaware of waterpipe tobacco smoking, while in others, parents may model it: both issues must be addressed as appropriate. In addition, whereas school-based interventions for CTS have indicated the critical importance of skill-building to resist peer pressure (USDHHS, 2012), such skill-building for WTS may need to tackle the more sensitive area of parent encouragement for WTS.
Warning about the dangers of CTS also includes warnings that are printed on the tobacco packs themselves. In addition to tobacco packaging, WTS includes additional features that may require labeling, including, potentially, health warnings on the apparatus itself as well as on other accessories, on the charcoal packaging, and perhaps on the doors and walls of venues where waterpipes are used (i.e., hookah cafés). This increased attention to labeling likely is necessary, as many users who frequent hookah cafés may never see tobacco/charcoal packaging. There is a small literature addressing this point, and more research clearly is needed (e.g., Islam et al., 2016; Jawad et al., 2015b; Mohammed, 2013; Nakkash et al., 2011). Text-only versus graphic warning labels have been investigated with waterpipe users using an online-questionnaire (Mohammed, 2013). Compared to text-only, graphic warnings elicited unfavorable emotional reactions, increased beliefs that WTS is harmful to their own health and also dangerous to non-users, and revealed higher quit intentions (Mohammed, 2013). Health warnings were more impactful as the warnings were large and decreased the pack branding; warnings at the point of consumption were reported to be more impactful compared to warnings at the point of sale (Jawad et al., 2015b). In the first study to test waterpipe-specific warning labels and location on the device, text-only messages and pictorial labels warning about harm to children were most effective in motivating waterpipe smokers to consider quitting, and the base, mouthpiece and stem of the apparatus were all equally noticeable locations for a warning label (Islam et al., 2016). Finding the combination of warning label content and placement that is most effective is a necessity.
With respect to ‘offer(ing) help to quit smoking’, a recent review highlighted limited knowledge of health professional students about the dangers of WTS and gaps in the education of health professional students about WTS and smoking cessation (Akl et al, 2015). Perhaps as a result, clinic based prompts – such as the 5As for CTS - to ask about WTS are lacking. Information regarding the physiological and behavioral effects of WTS should be integrated into the existing health care services. Providers should be educated on the prevalence and risks of WTS, as well as on methods of prevention and cessation. WTS’s patterns of use such as the higher prevalence in younger age groups, intermittent use, among social groups, sharing of the waterpipe, and longer use sessions – as well ability to deliver nicotine – will influence the dependence potential, and create the need for cessation interventions that potentially differ from the classical cigarette interventions (Maziak, 2011; Maziak et al., 2005). In addition, the visual, auditory and olfactory perceptual aspects of WTS are likely important to deal with in cessation interventions. To date, two cessation intervention have been tested with some success (Dogar et al., 2013; Asfar, Al Ali, Rastam, Maziak, &Ward, 2014). Both behavioral support with bupropion treatment for 7 weeks (BSS+) or behavioral support without bupropion (BSS) were effective in achieving indicated 6-month smoking abstinence among waterpipe-only smokers (Dogar et al., 2013), but were less so among cigarette smokers, thus suggesting potentially important differences in dependence (Dogar et al., 2013) linked to toxicants or patterns of use. Also, the efficacy and feasibility of a behavioral cessation program modeled on cigarette smoking cessation interventions was tested with 50 willing-to-quit adult waterpipe smokers in Syria. Both a brief (one in person session and three phone calls) or intensive (three in-person sessions and five phone calls) behavioral cessation treatment in a clinical setting were found to be effective in abstinence 3 months post quit day (Asfar, Al Ali, Rastam, Maziak, &Ward, 2014). However, process evaluation of this intervention indicated that participants requested more group sessions, and more phone calls than in person sessions. The authors suggest that this may be due to waterpipe smokers being younger and more educated than cigarette smokers. Overall, relatively few resources have been devoted to developing and testing cessation interventions that are specific to WTS, though the need for efficacious treatments is growing.
At the policy level, WTS-specific policies that protect people from waterpipe tobacco smoke (WTS clearly influences indoor air quality; Cobb et al., 2013), raise taxes on waterpipe tobacco and accessories, and enforce bans on waterpipe tobacco advertising, promotion, and sponsorship urgently are needed. These policies will need to be tracked for effectiveness. For example, there is some evidence that waterpipe tobacco may be less price elastic than cigarettes, therefore changes in taxation may not be as effective in changing behaviors (Maziak et al., 2014), although more evidence is needed regarding the behavioral economics of waterpipe. Bans on advertising will need to address deceitful labeling, as well as enticing promotions such as for the ‘diet shish (Vansickel et al., 2012; Nakkash & Khalil, 2010). The vast number of manufacturers and importers of waterpipe devices, tobacco, and assorted accessories add complexity (Jawad et al., 2015a) to policy level interventions.
All the WTS-adapted interventions suggested above are needed to change the social environment and norms conducive to WTS. Too many waterpipe users do not believe WTS is dangerous, nor do they believe they are dependent (Afifi et al., 2013; Akl et al., 2015). The social normativity of WTS being safe and not contributing to dependence leads to both initiation and sustained use. Indeed, the positive social norm around WTS may require new intervention emphases. Positive youth development approaches suggest that a key factor to reducing uptake of risk behaviors is engagement in productive use of non-school time (USDHHS, 2012). Young people often cite boredom as a reason for WTS initiation (Akl et al., 2015), particularly in relation to the socialization it provides. Enhancing options for pro-social alternative activities such as participation in clubs and sports may be an effective strategy to curb WTS, and youth themselves may be key to identifying which strategies are likely to work best.
Our ability to curb this epidemic successfully is dependent on continued research to close the gaps in knowledge. More specifically, the relationships between pharmacological, contextual, and social factors need to be explored and understood under a wide variety of cultural backgrounds (Blank et al., 2014). Exploring the interactions of waterpipe use with other types of tobacco use is warranted (Akl et al., 2010), especially as polytobacco use remains a public health problem among adolescents (USDHHS, 2012; USDHHS, 2014; Arrazola et al., 2014) and adults in the United States (Backinger et al., 2008; USDHHS, 2014) and globally among youth (Jaber et al., 2015; Jawad et al., 2016) and adults (Agaku et al., 2014). Furthermore, better validated instruments are needed to comprehend and perhaps predict dependence in waterpipe tobacco users (Aboaziza & Eissenberg, 2015; Fagerström and Eissenberg, 2012). Evaluation of the waterpipe specific interventions suggested above for their effectiveness on WTS is critical to identify best practices. In addition, establishing surveillance systems for WTS, or adding specific items on WTS to available surveillance systems including the Global Tobacco Surveillance System (GTSS; USDHHS, 1999) is necessary to monitor use and track the (hopefully) decreasing epidemic. In line with this recommendation, recently, an update to the recommendations for standardizing the measurement of waterpipe use has been suggested (Maziak et al., 2016; see also Maziak et al., 2005).
Conclusions
As noted above, there is little evidence to date around effective interventions for WTS prevention and control. The current state of evidence for intervention to curb or control WTS is at ground zero; akin to prior to the ‘cancer by the carton’ news report on the dangers of CTS of 1961 (Toch et al., 1961). National and global efforts have succeeded, particularly in developed countries, in changing social norms around CTS (USDHHS, 2012; 2014; WHO 2003; 2015b). We suggest the time has come to harness what we know works for CTS prevention and control and adapt it to tackle the epidemic of WTS.
Highlights.
Waterpipe use is spreading worldwide, surpassing cigarette use in many areas.
Waterpipes and cigarettes are forms of tobacco use and have grave health effects.
Little evidence exists of effective interventions for waterpipe prevention/control.
Cigarette and waterpipe use differ in toxicant exposure, patterns of use and norms.
These differences suggest the need to adapt not adopt cigarette interventions.
Acknowledgments
Role of Funding Sources
Drs. Lopez and Eissenberg are supported by the National Institute on Drug Abuse of the National Institutes of Health under Award Number P50DA036105 and the Center for Tobacco Products of the U.S. Food and Drug Administration. The content is solely the responsibility of the authors and does not necessarily represent the views of the NIH or the FDA.
We would like to thank reviewers for constructive comments that strengthened the manuscript.
NIH and the FDA had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Part of this paper was presented as a communication at the 16th World Conference on Tobacco or Health in Abu Dhabi, United Arab Emirates in March 2015 by RA.
Author’s disclosures
Conflict of Interest
All authors declare that they have no conflicts of interest.
Contributors
AL and MJ expanded on the presentation to develop the first draft. Subsequent drafts were edited by TEE and RAA. All authors read and have approved the final manuscript.
References
- Aboaziza E, Eissenberg T. Waterpipe tobacco smoking: what is the evidence that it supports nicotine/tobacco dependence? Tobacco Control. 2015;24:i44–i53. doi: 10.1136/tobaccocontrol-2014-051910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Afifi R, Khalil J, Fouad F, Hammal F, Jarallah Y, Abu Farhat H, Ayad M, Nakkash R. Social norms and attitudes linked to waterpipe use in the Eastern Mediterranean Region. Social Science and Medicine. 2013;98:125–134. doi: 10.1016/j.socscimed.2013.09.007. [DOI] [PubMed] [Google Scholar]
- Agaku IT, Filippidis FT, Vardavas CI, Odukoya OO, Awopegba AJ, Ayo-Yusuf OA, Connollo GN. Poly-tobacco use among adults in 44 countries during 2008–2012: evidence for an integrative and comprehensive approach in tobacco control. Drug and Alcohol Dependence. 2014;139:60–70. doi: 10.1016/j.drugalcdep.2014.03.003. [DOI] [PubMed] [Google Scholar]
- Akl EA, Gaddam S, Gunukula SK, Honeine R, Abou Jaoude P, Irani J. The effects of waterpipe tobacco smoking on health outcomes: a systematic review. International Journal of Epidemiology. 2010;39:834–857. doi: 10.1093/ije/dyq002. [DOI] [PubMed] [Google Scholar]
- Akl EA, Ward KD, Bteddini D, Khaliel R, Alexander AC, Lotfi T, Alaouie H, Afifi RA. The allure of the waterpipe: a narrative review of factors affecting the epidemic rise in waterpipe smoking among young persons globally. Tobacco Control. 2015;24:i13–i21. doi: 10.1136/tobaccocontrol-2014-051906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Ali R, Rastam S, Ibrahim I, Bazzi A, Fayad S, Shihadeh AL, Zaatari GS, Maziak W. A comparative study of systemic carcinogen exposure in waterpipe smokers, cigarette smokers and non-smokers. Tobacco Control. 2015;24:125–127. doi: 10.1136/tobaccocontrol-2013-051206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alzyoud S, Veeranki SP, Kheirallah KA, Shotar AM, Pbert L. Validation of the waterpipe tolerance questionnaire among Jordanian school-going adolescent waterpipe users. Global Journal of Health Science. 2016;8(2):198–208. doi: 10.5539/gjhs.v8n2p198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Lung Association. An Emerging Deadly Trend: Waterpipe Tobacco Use. Washington: American Lung Association; 2007. [accessed 2016 Mar 19]. [Google Scholar]
- Anjum Q, Ahmed F, Ashfaq T. Knowledge, attitude and perception of water pipe smoking (Shisha) among adolescents aged 14–19 years. Journal of the Pakistan Medical Association. 2008;58(6):312. [PubMed] [Google Scholar]
- Arrazola RA, Neff LJ, Kennedy SM, Holder-Hayes E, Jones CD Centers for Disease Control and Prevention (CDC) Tobacco use among middle and high school students--United States, 2013. Morbidity and Mortality Weekly Report. 2014;63(45):1021–1026. [PMC free article] [PubMed] [Google Scholar]
- Asfar T, Al Ali R, Rastam S, Maziak W, Ward KD. Behavioral cessation treatment of waterpipe smoking: the first pilot randomized control trial. Addictive Behaviors. 2014;39:1066–1074. doi: 10.1016/j.addbeh.2014.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asfar T, Ward KD, Eissenberg T, Maziak W. Comparison of patters of use, beliefs, and attitudes related to waterpipe between beginning and established smokers. BMC Public Health. 2005;5(19):1–9. doi: 10.1186/1471-2458-5-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Audrain-McGovern J, Benowitz NL. Cigarette smoking, nicotine, and body weight. Clin Pharmacol Ther. 2011;90(1):164–168. doi: 10.1038/clpt.2011.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auf RA, Radwan GN, Loffredo CA, El Setouhy M, Israel E, Mohamed MK. Assessment of tobacco dependence in waterpipe smokers in Egypt. Int J Tuberc Lung Dis. 2012;16(1):132–137. doi: 10.5588/ijtld.11.0457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Backinger CL, Fagan P, O’Connell ME, Grana R, Lawrence D, Bishop JA, Gibson JT. Use of other tobacco products among U.S. adult cigarette smokers: prevalence, trends and correlates. Addictive Behaviors. 2008;33(3):472–489. doi: 10.1016/j.addbeh.2007.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett TE, Smith T, He Y, et al. Evidence of emerging hookah use among university students: a cross-sectional comparison between hookah and cigarette use. BMC Public Health. 2013;13:302. doi: 10.1186/1471-2458-13-302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blank MD, Warren Brown K, Goodman RJ, Eissenberg T. An observational study of group waterpipe use in a natural environment. Nicotine and Tobacco Research. 2014;16(1):93–99. doi: 10.1093/ntr/ntt120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bou Fakhreddine HM, Kanj AN, Kanj NA. The growing epidemic of water pipe smoking: Health effects and future needs. Respiratory Medicine. 2014;108(9):1241–1253. doi: 10.1016/j.rmed.2014.07.014. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Best Practices for Comprehensive Tobacco Control Programs—2014. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Google Scholar]
- Cobb CO, Vansickel AR, Blank MD, Jentink K, Travers MJ, Eissenberg T. Indoor air quality in Virginia waterpipe cafes. Tobacco Control. 2013;22(5):338–343. doi: 10.1136/tobaccocontrol-2011-050350. Epub 2012 Mar 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobb C, Ward KD, Maziak W, Shihadeh AL, Eissenberg T. Waterpipe Tobacco Smoking: An Emerging Health Crisis in the United States. American Journal of Health Behavior. 2010;34(3):275–285. doi: 10.5993/ajhb.34.3.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dogar O, Jawad M, Shah SK, Newell JN, Kanaan M, Khan MA, Siddiqi K. Effect of cessation interventions on hookah smoking: post-hoc analysis of a cluster-randomized controlled trial. Nicotine & Tobacco Research. 2013;16(6):682–688. doi: 10.1093/ntr/ntt211. [DOI] [PubMed] [Google Scholar]
- Eissenberg T, Shihadeh A. Waterpipe tobacco and cigarette smoking: direct comparison of toxicant exposure. American Journal of Preventive Medicine. 2009;37(6):518–523. doi: 10.1016/j.amepre.2009.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Zaatari ZM, Chami HA, Zaatari GS. Health Effects associated with waterpipe smoking. Tobacco Control. 2015;24(S1):i31–i43. doi: 10.1136/tobaccocontrol-2014-051908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrelly MC, Davis KC, Haviland L, Messeri P, Healton CG. Evidence of a Dose—Response Relationship Between “truth” Antismoking Ads and Youth Smoking Prevalence. American Journal of Public Health. 2005;95(3):425–431. doi: 10.2105/AJPH.2004.049692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrelly MC, Nonnemaker J, Davis KC, Hussin A. The influence of the national truth® campaign on smoking initiation. American Journal of Preventive Medicine. 2009;36(5):379–384. doi: 10.1016/j.amepre.2009.01.019. [DOI] [PubMed] [Google Scholar]
- Fong GT, Cummings KM, Borland R, Hastings G, Hyland A, Giovino GA, Hammond D, Thompson ME. The conceptual framework of the International Tobacco Control (ITC) Policy Evaluation Project. Tobacco Control. 2006;15(Suppl III):iii3–iii11. doi: 10.1136/tc.2005.015438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Agency for Research on Cancer. IARC monographs on the evaluation of carcinogenic risks to humans, vol 71. Re-evaluation of some organic chemicals, hydrazine and hydrogen peroxide. Lyon, France: IARC; 1999. Available from: http://monographs.iarc.fr/ENG/Monographs/vol71/mono71.pdf. [PMC free article] [PubMed] [Google Scholar]
- International Agency for Research on Cancer. IARC monographs on the evaluation of carcinogenic risks to humans, vol 88. Formaldehyde, 2-Butoxyethanol and 1-tert-Butoxypropan-2-ol. Lyon, France: IARC; 2006. Available from: http://monographs.iarc.fr/ENG/Monographs/vol88/mono88.pdf. [PMC free article] [PubMed] [Google Scholar]
- Jaber R, Madhivanan P, Veledar E, Khader Y, Mzayek F, Maziak W. Waterpipe a gateway to cigarette smoking initiation among adolescents in Irbid, Jordan: a longitudinal study. International Journal of Tuberculosis and Lung Disease. 2015;19(4):481–487. doi: 10.5588/ijtld.14.0869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob P, Abu Raddaha AH, Dempsey D, Havel C, Peng M, Yu L, Benowitz NL. Comparison of Nicotine and Carcinogen Exposure with Water Pipe and Cigarette Smoking. Cancer Epidemiol Biomarkers Prev. 2013;22(5):765–772. doi: 10.1158/1055-9965.EPI-12-1422. Cancer Epidemiology, Biomarkers, and Prevention, 22(5); 765–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jawad M, Bakir A, Ali M, Grant A. Impact of waterpipe tobacco pack health warnings on waterpipe smoking attitudes: a qualitative analysis among regular users in London. BioMed Research International. 2015:745685. doi: 10.1155/2015/745865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jawad M, El Kadi L, Mugharbil S, Nakkash R. Waterpipe tobacco smoking legislation and policy enactment: a global analysis. Tobacco Control. 2015a;24:i60–i65. doi: 10.1136/tobaccocontrol-2014-051911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jawad M, Lee JT, Millett C. Waterpipe tobacco smoking prevalence and correlates in 25 Eastern Mediterranean and Eastern European countries: cross-sectional analysis of the Global Youth Tobacco Survey. Nicotine & Tobacco Research. 2016;18(4):395–402. doi: 10.1093/ntr/ntv101. [DOI] [PubMed] [Google Scholar]
- Jawad M, McEwen A, McNeill A, et al. To what extent should waterpipe tobacco smoking become a public health priority? Addiction. 2013;108(11):1873–1884. doi: 10.1111/add.12265. [DOI] [PubMed] [Google Scholar]
- Jawad M, Millett C. Impact of EU flavoured tobacco ban on waterpipe smoking. BMJ. 2014;348:g2698. doi: 10.1136/bmj.g2698. [DOI] [PubMed] [Google Scholar]
- Jawad M, Nakkash RT, Mahfoud Z, Bteddini D, Haddad P, Afifi RA. Parental smoking and exposure to environmental tobacco smoke are associated with waterpipe smoking among youth: results from a national survey in Lebanon. Public Health. 2015;129(4):370–376. doi: 10.1016/j.puhe.2015.01.011. [DOI] [PubMed] [Google Scholar]
- Kassim S, Al-Bakri A, Al'Absi M, Croucher R. Waterpipe tobacco dependence in U.K. male adult residents: a cross-sectional study. Nicotine Tob Res. 2014;16(3):316–325. doi: 10.1093/ntr/ntt148. Epub 2013 Oct 15. [DOI] [PubMed] [Google Scholar]
- Lipkus IM, Eissenberg T, Schwartz-Bloom RD, Prokhorov AV, Levy J. Affecting perceptions of harm and addiction among college waterpipe tobacco smokers. Nicotine & Tobacco Research. 2011;13(7):599–610. doi: 10.1093/ntr/ntr049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maziak W. The global epidemic of waterpipe smoking. Addictive Behaviors. 2011;36(1–2):1–5. doi: 10.1016/j.addbeh.2010.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maziak W. The waterpipe: a new way of hooking youth on tobacco. The American. Journal on Addictions. 2014;23:103–107. doi: 10.1111/j.1521-0391.2013.12073.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maziak W. Rise of waterpipe smoking. BMJ. 2015;350:h1991. doi: 10.1136/bmj.h1991. [DOI] [PubMed] [Google Scholar]
- Maziak W, Ben Taleb Z, Bahelah R, Islam F, Jaber R, Auf R, Salloum RG. The global epidemiology of waterpipe smoking. Tobacco Control. 2015a;24:i3–i12. doi: 10.1136/tobaccocontrol-2014-051903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maziak W, Eissenberg T, Ward KD. Patterns of waterpipe use and dependence: implications for intervention development. Pharmacology, Biochemistry, and Behavior. 2005;80:173–179. doi: 10.1016/j.pbb.2004.10.026. [DOI] [PubMed] [Google Scholar]
- Maziak W, Ben Taleb Z, Jawad M, Afifi R, Nakkash R, Akl EA, Ward KD, Salloum RG, Barnett TE, Primack BA, Sherman S, Cobb CO, Sutfin EL, Eissenberg E. Consensus statement on assessment of waterpipe smoking in epidemiological studies. Tobacco Control. 2016 doi: 10.1136/tobaccocontrol-2016-052958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maziak W, Jawad M, Jawad S, Ward KD, Eissenberg T, Asfar T. Interventions for waterpipe smoking cessation. Cochrane Database of Systematic Reviews. 2015b;(7) doi: 10.1002/14651858.CD005549.pub3. Art. No.: CD005549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maziak W, Nakkash R, Bahelah R, Husseini A, Fanous N, Eissenberg T. Tobacco in the Arab world: old and new epidemics amidst policy paralysis. Health Policy and Planning. 2014;29:784–794. doi: 10.1093/heapol/czt055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maziak W, Ward KD, Afifi Soweid RA, Eissenberg T. Standardizing questionnaire items for the assessment of waterpipe tobacco use in epidemiological studies. Public Health. 2005;119(5):400–404. doi: 10.1016/j.puhe.2004.08.002. [DOI] [PubMed] [Google Scholar]
- Maziak W, Ward KD, Soweid RA, Eissenberg T. Tobacco smoking using a waterpipe: a re-emerging strain in a global epidemic. Tobacco control. 2004;13(4):327–333. doi: 10.1136/tc.2004.008169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohammed HT. The Efficacy of Viewing Health Warnings on Shisha Smoking among Shisha Smokers. A Thesis presented to the University of Waterloo; Waterloo, Ontario, Canada. 2013. [Google Scholar]
- Morris DS, Fiala SC, Pawlak RP. Opportunities for policy interventions to reduce youth Hookah smoking in the United States. Preventing Chronic Disease. 2012;9:E165. doi: 10.5888/pcd9.120082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mzayek F, Khader Y, Eissenberg T, Al Ali R, Ward KD, Maziak W. Patterns of waterpipe and cigarette smoking initiation in schoolchildren: Irbid Longitudinal Smoking Study. Nicotine and Tobacco Research. 2012;14(4):448–454. doi: 10.1093/ntr/ntr234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakkash R, Khalil J. Health warning labelling practices on narghile (shisha, hookah) waterpipe tobacco products and related accessories. Tobacco Control. 2010;19:235–239. doi: 10.1136/tc.2009.031773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakkash RT, Khalil J, Afifi RA. The rise in narghile (shisha, hookah) waterpipe tobacco smoking: a qualitative study of perceptions of smokers and nonsmokers. BMC Public Health. 2011;11:315. doi: 10.1186/1471-2458-11-315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neergaard J, Pramil S, Job J, Montgomery S. Waterpipe smoking and nicotine exposure: a review of the current evidence. Nicotine and Tobacco Research. 2007;9(10):987–994. doi: 10.1080/14622200701591591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noonan D. Exemptions for hookah bars in clean indoor air legislation: a public health concern. Public Health Nursing. 2010;27(1):49–53. doi: 10.1111/j.1525-1446.2009.00826.x. [DOI] [PubMed] [Google Scholar]
- Primack BA, Shensa A, Kim KH, Carroll MV, Hoban MT, Leino EV, Eissenberg T, Dachille KH, Fine MJ. Waterpipe smoking among U.S. university students. Nicotine and Tobacco Research. 2013;15(1):29–35. doi: 10.1093/ntr/nts076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramôa CP, Shihadeh A, Salman R, Eissenberg T. Group waterpipe tobacco smoking increases smoke toxicant concentration. Nicotine and Tobacco Research. 2016;18(5):770–776. doi: 10.1093/ntr/ntv271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose-Krasnor L. The nature of social competence: a theoretical review. Social Development. 1997;6(1):111–135. [Google Scholar]
- Salameh P, Aoun Z, Waked M. Saliva cotinine and exhaled carbon monoxide in real life narghile (waterpipe) smokers: A post hoc analysis. Tobacco Use Insights. 2009;2:1–10. [Google Scholar]
- Salameh P, Salamé J, Waked M, Barbour B, Zeidan N, Baldi I. Waterpipe dependence in university students and effect of normative beliefs: a cross-sectional study. BMJ Open. 2014;4(2):e004378. doi: 10.1136/bmjopen-2013-004378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubert J, Bewersdorff J, Luch A, Schulz TG. Waterpipe smoke: A considerable source of human exposure against furanic compounds. Analytica Chimica Acta. 2012a;709:105–115. doi: 10.1016/j.aca.2011.10.012. [DOI] [PubMed] [Google Scholar]
- Schubert J, Hahn J, Dettbarn G, Seidel A, Luch A, Schulz TG. Mainstream smoke of the waterpipe: Does this environmental matrix reveal as significant source of toxic compounds? Toxicology Letters. 2011;205:279–284. doi: 10.1016/j.toxlet.2011.06.017. [DOI] [PubMed] [Google Scholar]
- Schubert J, Heinke V, Bewersdorff J, Luch A, Schulz TG. Waterpipe smoking: the role of humectants in the release of toxic carbonyl. Arch Toxicol. 2012b;86(8):1309–1316. doi: 10.1007/s00204-012-0884-5. [DOI] [PubMed] [Google Scholar]
- Shihadeh A, Saleh R. Polycyclic aromatic hydrocarbons, carbon monoxide, “tar‘, and nicotine in the mainstream smoke aerosol of the narghile water pipe. Food and Chemical Toxicology. 2005;43:655–661. doi: 10.1016/j.fct.2004.12.013. [DOI] [PubMed] [Google Scholar]
- Shihadeh A, Schubert J, Klaiany J, El Sabban M, Luch A, Saliba NA. Toxicant content, physical properties and biological activity of waterpipe tobacco smoke and its tobacco-free alternatives. Tobacco Control. 2015;24:i22–i30. doi: 10.1136/tobaccocontrol-2014-051907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh S, Soumya M, Saini A, Mittal V, Singh UV, Singh V. Breath carbon monoxide levels in different forms of smoking. Indian J Chest Dis Allied Sci. 2011;53(1):25–28. [PubMed] [Google Scholar]
- Thomas RE, McLellan J, Perera R. Effectiveness of school-based smoking prevention curricula: systematic review and metaanalysis. BMJ Open. 2015;5:e006976. doi: 10.1136/bmjopen-2014-006976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toch HH, Allen TM, Lazer W. Effects of the cancer scares: the residue of news impact. Journalism Quarterly. 1961;38:25. [Google Scholar]
- U.S. Department of Health and Human Services. The Health Consequences of Smoking: Nicotine Addiction: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Center for Health Promotion and Education, Office on Smoking and Health; 1988. [Google Scholar]
- U.S. Department of Health and Human Services. Smoking and Tobacco Use: About the GTSS. [Accessed 5 Jul 2016];1999 http://www.cdc.gov/tobacco/global/gtss/
- U.S. Department of Health and Human Services. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2012. [Google Scholar]
- U. S. Department of Health and Human Services. The Health Consequences of Smoking: 50 Years of Progress. A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. 2014. Printed with corrections. [Google Scholar]
- Vansickel AR, Shihadeh A, Eissenberg T. Waterpipe tobacco products: nicotine labelling versus nicotine delivery. Tobacco Control. 2012;21(3):377–379. doi: 10.1136/tc.2010.042416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward KD. The waterpipe: an emerging global epidemic in need of action. Tobacco Control. 2015;24:i1–i2. doi: 10.1136/tobaccocontrol-2014-052203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward KD, Siddiqi K, Ahluwalia JS, Alexander AC, Asfar T. Waterpipe tobacco smoking: the critical need for cessation treatment. Drug and Alcohol Dependence. 2015;153:14–21. doi: 10.1016/j.drugalcdep.2015.05.029. [DOI] [PubMed] [Google Scholar]
- Warren CW, Lea V, Lee J, et al. Change in tobacco use among 13–15 year olds between 1999 and 2008: Findings from the Global Youth Tobacco Survey. Global Health Promotion. 2009;16(2 suppl):38–90. doi: 10.1177/1757975909342192. [DOI] [PubMed] [Google Scholar]
- World Health Organization. WHO Framework Convention on Tobacco Control. [Accessed 20 Apr 2016];2003 http://www.who.int/fctc/text_download/en/
- World Health Organization. Framework Convention on Tobacco Control, Framework Convention Alliance Policy Briefing for COP6: Control and prevention of waterpipe tobacco products. [Accessed 15 Jun 2016];2014a http://www.fctc.org/images/stories/FCA_policy_brief_Waterpipes_B.pdf.
- World Health Organization. Conferences of the Parties to the WHO Framework Convention on Tobacco Control: Control and prevention of waterpipe tobacco products report. [Accessed 15 Jun 2016];2014b http://apps.who.int/gb/fctc/PDF/cop6/FCTC_COP6_11-en.pdf.
- World Health Organization. Advisory note: waterpipe tobacco smoking: 2nd edition. Health effects, research needs and recommended actions for regulators. [Accessed 15 Jun 2016];2015a http://apps.who.int/iris/bitstream/10665/161991/1/9789241508469_eng.pdf.
- World Health Organization. Media Centre: Tobacco Fact Sheet. [Accessed 20 Apr 2016];2015b http://www.who.int/mediacentre/factsheets/fs339/en/
- World Health Organization. Tobacco Free Initiative (TFI): MPOWER brochures and other resources. [Accessed 15 Jun 2016];2016 http://www.who.int/tobacco/mpower/publications/en/
- Zeidan RK, Rachidi S, Awada S, El Hajje A, El Bawab W, Salame J, Bejjany R, Salameh P. Carbon monoxide and respiratory symptoms in young adult passive smokers: a pilot study comparing waterpipe to cigarette. International Journal of Occupational Medicine and Environmental Health. 2014;27(4):571–582. doi: 10.2478/s13382-014-0246-z. [DOI] [PubMed] [Google Scholar]