Abstract
Women are at a higher risk for depression than are men, and this risk is especially pronounced at specific reproductive periods of vulnerability: adolescence, pregnancy, postpartum,, and the menopausal transition. Obstetrician–gynecologists are often the health care providers that women consult during these vulnerable periods, usually presenting with conditions or complaints other than depression or anxiety. Presenting symptoms are frequently known comorbidities with depression, or are risk factors for depression. Thus, by screening for depression and other mood disorders in these critical periods, in addition to screening at routine intervals such as annual examinations, obstetricians and gynecologists can play an important role in early detection, prevention, and treatment of mood disorders and their comorbid conditions. We provide a framework for depression management within busy obstetric gynecology settings using new integrated care models for mental health.
Precis
Obstetrician-gynecologists should screen and treat women for depression during routine prevention visits and at vulnerable reproductive stages; new integrated care models are recommended.
There is an urgent need to screen for, and treat, depression in obstetric gynecology settings
The United States Preventive Services Task Force (USPSTF) recently recommended depression screening for all adults with specific mention of pregnant and postpartum women.(1) This is of direct relevance to obstetrician gynecologists and comes close on the heels of the American College of Obstetricians and Gynecologists’ (ACOG)’s committee opinion recommending screening for depression and anxiety symptoms at least once during the perinatal period.(2) These recommendations are fitting as women are twice as likely to have a lifetime diagnosis of major depression as men.(3)
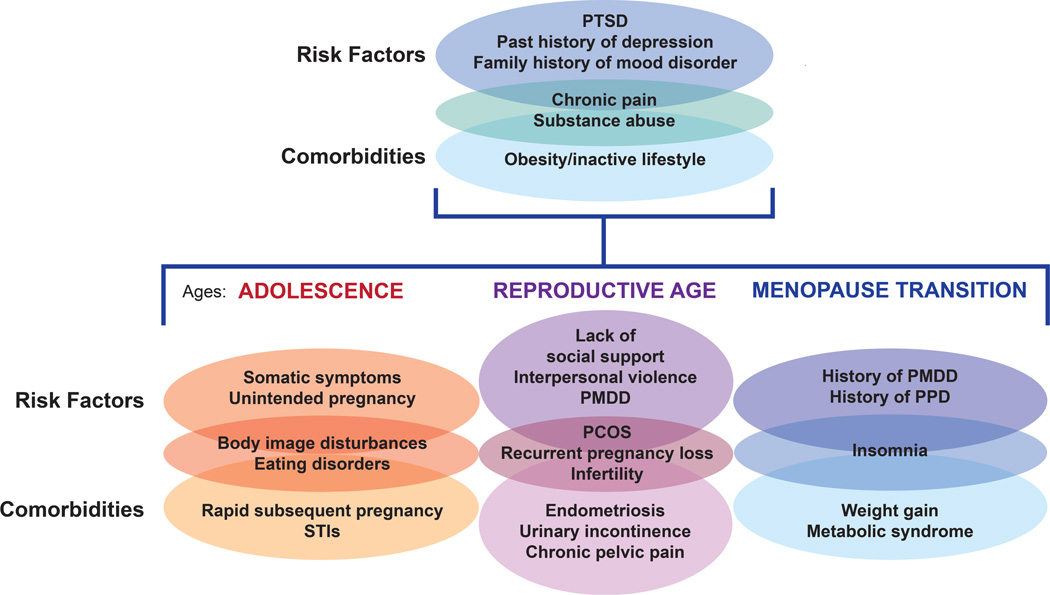
Obstetrician–gynecologists are well-placed to detect depression early and to treat before symptoms become chronic with a devastating effect on families and societies. Not only do many women consider their obstetrician–gynecologist as their primary care provider, but almost 50% of obstetrician–gynecologists also consider themselves as primary care providers.(3) In addition, several gynecologic conditions encountered by obstetrician–gynecologists e.g. endometriosis,(4) polycystic ovarian syndrome,(5) infertility, recurrent pregnancy loss,(6) and premature ovarian insufficiency,(7) are associated with depressive symptoms - either as risk factors or comorbidities (Figure 1).
Figure 1.
Risk factors and comorbidities of major depression in women across the lifespan. The top portion of the figure shows the risk factors (top sphere), comorbidities, (bottom sphere) and overlapping factors that are both risk factors and comorbidities (middle sphere) for women of all reproductive stages. The bottom portion of the figure shows these factors by reproductive stages: adolescence, cycling reproductive age women, and menopause transition. PTSD, posttraumatic stress disorder; PMDD, premenstrual dysphoric disorder; PPD, postpartum depression; PCOS, polycystic ovary syndrome; STI, sexually transmitted infection.
Screening during critical periods of vulnerability, and at routine intervals, can result in early depression detection, prevention and treatment, and can prevent associated comorbid conditions
Prevention goes hand-in-hand with early detection, as early detection and treatment can help prevent the morbidity associated with the primary disorder and comorbid conditions. Underscoring the importance of prevention, the Affordable Care Act instituted the national prevention strategy (NPS). One of 6 NPS priority areas is “mental and emotional wellbeing”. NPS emphasizes integration of early detection of mental health problems into primary care settings.(8) Preventive measures have the highest yield when delivered at routine intervals, e.g. at the annual gynecologic examination and at “critical periods” or “windows of vulnerability”- specific periods along the life course when adverse events or exposures have the greatest negative impact.(9) In women, specific reproductive stages (e.g. adolescence, pregnancy, postpartum, menopause transition) are particularly vulnerable periods when reproductive hormone levels and psychosocial circumstances are in flux. These windows of vulnerability, when appropriately identified, provide opportunities for prevention.
Several effective screening and preventive interventions for other conditions commonly treated in obstetric gynecology settings already exist: cervical and breast cancer, hypertension, sexually transmitted infections; and family planning.(10, 11) However, interventions to promote mental and emotional wellbeing are not yet systematically offered. Although obstetrician–gynecologists are aware of the importance of depression screening,(3) they may be reticent to make depression screening routine, perhaps due to lack of resources and limited clinical time allotment. Additional concerns that may arise relate to the question of necessary follow up and treatment availability for women who screen positive for depression.(12) New treatment models for depression, based in primary care(13) and obstetrics and gynecology(3, 14) clinics are relatively easy to implement, effective, and well-accepted by busy practices.
We argue that, given the high prevalence and burden of depression in women, the influence that an obstetrician–gynecologist might have by identifying and treating depression early, is substantial. This should be our new patient care paradigm. We describe the importance of depression screening and early treatment and summarize models of care that can achieve these goals in an obstetric and gynecology practice setting. Commonly used screening tools such as the 9-item Patient Health Questionnaire (PHQ-9) are integrated into many electronic health records and are easy for patients to complete in the office. Anxiety is frequently comorbid with depression, particularly in adolescence, but details are beyond the scope of this commentary. We organize our recommendations by focusing on vulnerable periods - adolescence, pregnancy, postpartum, and the menopause transition and conclude with recommendations regarding initiation of treatment. Details of our recommendations and all primary references to those recommendations can be found at www.dawncare.org.
Adolescence is a period of social transition and a high risk period for behavioral and emotional disorders
The increased risk for depression in females begins at puberty. Female adolescents are at a 2- to 3-fold higher risk of major depressive disorder (MDD) than males, and a nearly 4-fold higher risk of severe MDD.(15) Adolescents with depressive symptoms are at a higher risk of educational underachievement, unemployment, early parenthood and anxiety disorders, nicotine dependence, alcohol abuse and suicidality.(16) Thirty percent of adolescents with MDD report suicidality in the past year and 10.8% report a suicide attempt. Centers for Disease Control and Prevention data from 1999 to 2014, demonstrated suicide rates increased in both men and women of all age groups. In females, the largest increase was in adolescent girls, almost tripling in fifteen years.(17)
We recommend that obstetrician–gynecologists screen all adolescent patients for depression and anxiety. Further care coordination may be required with the pediatric provider or specialists. Knowledge of the commonly comorbid conditions in depressed adolescents (Figure 1) can guide further preventive measures. For example, assuring adequate family planning services for teens can prevent subsequent pregnancies, more common in adolescents with depression (49% of depressed adolescent mothers experienced a subsequent pregnancy within 2 years).(18) Similarly, adolescents with depression should be screened for sexually transmitted infections, substance abuse, and eating disorders.
Mood disorders in pregnant and postpartum women have tremendous public health impact due to effects on children and families, and should be treated early
Reproductive age women who are at a high risk for depression constitute the most common age group cared for by obstetrician–gynecologists. Reported rates of perinatal depression vary from 7 to 20%, (19) and untreated perinatal depression is a major public health problem, with implications not just for the mother but for the child and the family as well.(20) Screening for depression in this age group is especially important as only about 11% of those with clinically significant depression present with a chief complaint of depressive symptoms.(21) Several depression screening tools have been validated for use in this population including the Edinburgh Postnatal Depression Scale (EPDS) and the PHQ-9.(22) Obstetricians should screen at least once during the perinatal period (1, 2), perhaps arranging for closer monitoring or repeat screening in women with recognized risk factors for depression such as past or family history of depression (Figure 1).
Prevention of depression is best begun before pregnancy. At prenatal visits, attention should be paid not just to nutrition and traditional prenatal care but also to the expectant mothers’ emotional wellbeing, self-efficacy and readiness to parent. There is preliminary evidence that parenting support and anticipatory parenting guidance can prevent postpartum depression.(23) Obstetricians can play a key role in recognizing women with need for additional parenting support and refer to appropriate resources such as home visiting programs or maternity support services, available in most states.
Premenstrual dysphoric disorder (PMDD) may be a risk factor for a major depressive episode at other vulnerable periods
PMDD is a common mood disorder, observed in menstruating women, with prevalence rates of 3 – 8%.(24) The diagnosis is made based on at least 4 of 11 physical (e.g. bloating, weight gain, joint pain), and 1 of 4 behavioral (e.g. mood swings, irritability, depression, anxiety) symptoms during the luteal phase.(25) PMDD onset is in the early 20s and many of these women may never see a psychiatrist. Evidence based treatments for PMDD include luteal phase or symptom onset treatment with SSRIs,(24) rather than the continuous SSRI therapy recommended for depression. There is preliminary evidence that women with PMDD may be at elevated risk for postpartum depression and depression in the menopause transition.(26) Monitoring mood more frequently in vulnerable periods is recommended.
The late menopause transition is a time of increased risk for a major depressive episode
Mood disorders are more common in the late menopausal transition as compared with premenopausal and late postmenopausal states.(27) The late transition occurs on average 2 years before the final menstrual period, and is defined by an episode of 60 or more days of amenorrhea. Not only are the rates of new onset depressive symptoms higher in the late transition, but women with preexisting major depressive disorder are at a higher risk of recurrence during this time.(26) Risk factors and comorbidities for depression in the late transition are summarized in Figure 1. Perimenopausal women often present with atypical depressive symptoms such as increased sleep disturbances or increased weight gain and appetite(28) and obstetrician–gynecologists should account for this in their differential diagnosis.
Estrogen has been suggested as a treatment for MDD in perimenopausal women, however the evidence for this is controversial.(29) Estradiol (oral or transdermal) may have antidepressant efficacy for women in the late transition who are experiencing other menopausal symptoms, but is not effective in postmenopausal MDD treatment. There is insufficient evidence to inform the choice between estradiol monotherapy and estradiol plus an antidepressant. Similarly the ideal duration of estradiol treatment is unclear.(29) For women already on antidepressants, it is important to be aware that menopausal status, oral contraceptives and postmenopausal hormone therapy can all have an effect on antidepressant response. Rather than targeted screening, we recommend universal screening of all women presenting at midlife requesting menopausal care.
Obstetrician–gynecologists can make the diagnosis of depression and initiate treatment
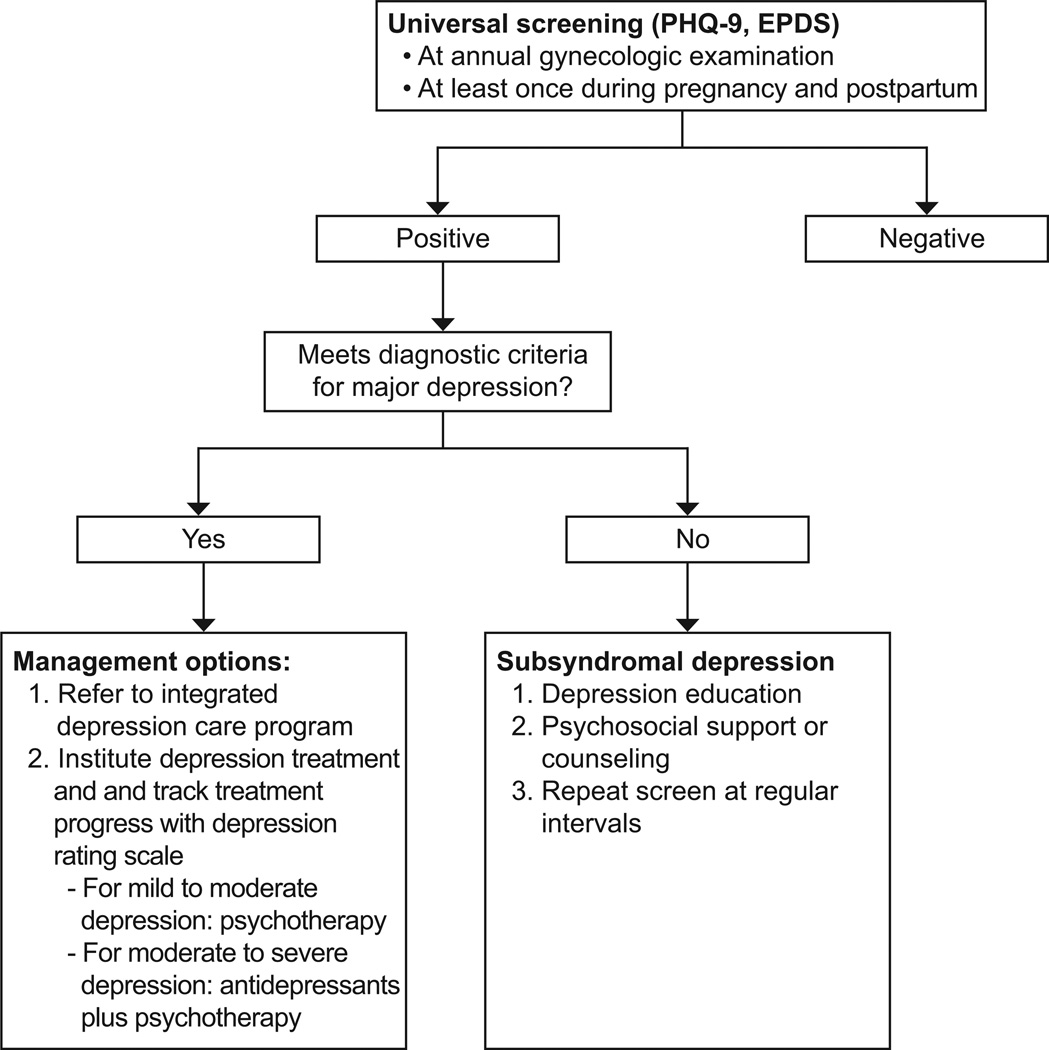
All patients who screen positive for depression do not have major depressive disorder (Box 1, Figure 2). Although subsyndromal depression can cause considerable impairment, treatment approaches differ and hence it is important to make this distinction. In all cases, attention must be paid to the suicidal ideation item in the screening questionnaire, with clinic specific procedures in place to follow up if endorsed. Adopting an integrated care model into your clinic as described below, is evidence based and can ensure high quality depression treatment while reducing physician burden.
Box 1: Diagnosis of depression.
DSM V diagnostic criteria for major depressive disorder (25)
-
Five or more of the following symptoms have been present during the same 2 week period and represent a change from previous functioning; at least one of the symptoms is either (1) depressed mood or (2) loss of interest or pleasure:
Note: Do not include symptoms that are clearly attributable to another medical condition- Depressed mood most of the day, nearly every day, as indicated by either subjective report (e.g., feels sad, empty, hopeless) or observation made by others (e.g., appears tearful). (Note: In children and adolescents, can be irritable mood.)
- Markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day (as indicated by either subjective account or observation).
- Significant weight loss when not dieting or weight gain (e.g., a change of more than 5% of body weight in a month), or decrease or increase in appetite nearly every day. (Note: In children, consider failure to make expected weight gain.)
- Insomnia or hypersomnia nearly every day.
- Psychomotor agitation or retardation nearly every day (observable by others, not merely subjective feelings of restlessness or being slowed down).
- Fatigue or loss of energy nearly every day.
- Feelings of worthlessness or excessive or inappropriate guilt (which may be delusional) nearly every day (not merely self-reproach or guilt about being sick).
- Diminished ability to think or concentrate, or indecisiveness, nearly every day (either by subjective account or as observed by others).
- Recurrent thoughts of death (not just fear of dying), recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan for committing suicide.
The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
The episode is not attributable to the physiological effects of a substance or another medical condition.
The occurrence of the major depressive episode is not better explained by schizoaffective disorder, schizophrenia, schizophreniform disorder, delusional disorder, or other specified and unspecified schizophrenia spectrum and other psychotic disorders.
-
There has never been a manic episode or a hypomanic episode.
Note: Criteria A–C represent a major depressive episode.
Reprinted with permission from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, (Copyright ©2013). American Psychiatric Association. All Rights Reserved.
Figure 2.
Depression diagnosis. Universal screening recommendations: use the 9-item Patient Health Questionnaire (PHQ-9) in busy, combined obstetrics and gynecology practices for all patients and track obstetrics patients with Edinburgh Postnatal Depression Scale (EPDS) once diagnosed. Use EPDS to screen in obstetrics practices.
Depression treatment programs integrated into busy obstetrics and gynecology practices are the wave of the future - easy to implement, extremely effective and well accepted
We strongly recommend that obstetricians and gynecologists consider implementation of a depression care model and do not attempt to screen and treat in a vacuum. Commonly implemented programs are summarized in Table 1, but this is not an exhaustive list. Key features of the programs include: on site screening, patient engagement, education, treatment, and tracking, having both behavioral and medical therapies available and psychiatric consultation. As obstetrician -gynecologist practices become more patient centered and team based these models become increasingly relevant. Paying attention to women’s mental health and emotional wellbeing has far reaching benefits, reducing both physical and social disabilities.(30) with the potential to improve outcomes for children(31) and families.(32) The extra few minutes spent on screening, counseling and coordination of care have tremendous downstream effects. Thus, obstetrician–gynecologists have a key role to play to positively influence women and their families and to make important public health contributions.
TABLE 1.
Integrated depression treatment programs in obstetric and gynecologic settings in the United States
| COLLABORATIVE CARE PROGRAMS | |||
|---|---|---|---|
| Population studied | Intervention | Outcomes | |
| DAWN(3) www.dawncare.org |
Females > 18 years in university obstetric gynecology clinics, with PHQ-9 scores ≥ 10 |
Collaborative care (engagement, problem solving therapy ±pharmacotherapy) vs usual care |
12 month outcome improved depression score – (RR = 1.74, 95%CI 1.11– 2.73) |
| MOMCare(13) | Pregnant women ≥ 18 years in FQHCs, with major depression or dysthymia. |
Collaborative care (engagement, interpersonal therapy ±pharmacotherapy) vs enhanced usual care |
Higher rates of remission (Wald's χ2 = 3.67, df = 1, P = .05) |
| MHIP Moms(33) | Pregnant or parenting women in FQHCs, with PHQ-9 scores ≥ 10 |
Collaborative care (problem solving therapy ±pharmacotherapy) |
59% of women had PHQ – 9 scores reduce by >50% |
| OTHER INTEGRATED PROGRAMS | |||
| Population studied | Intervention | Outcomes | |
| MCPAP for moms(14) |
Pregnant and postpartum women mainly in obstetric clinics, but also pediatrics and family practice |
Active outreach and engagement of obstetric providers; trainings and toolkits for providers and staff; telephone based perinatal psychiatric consultation; care coordination |
Outcome data not yet available |
| EDUCATION AND EXPEDITED REFERRAL PROGRAMS | |||
| Care manager intervention(34) |
All women ≥ 18 years of age with PHQ-9 scores ≥10;3 obstetric gynecology settings: 1) suburban office practice, 2) suburban community clinic, 3) hospital outpatient clinic. |
Care manager delivered education and referral assistance, specialty mental health appointments in same building as clinic |
Outcome data not reported |
| Nurse delivered depression feedback and referral intervention(35) |
Pregnant women in university obstetrics clinic with EPDS score ≥ 10 |
Nurse delivered, telephone based depression feedback and referral |
Modest short term increase in depression treatment use (OR 1.10, 95% CI 0.45 – 2.69) No significant change in depression outcomes |
DAWN – Depression Attention for Women Now; FQHCs – Federally Qualified Health Centers; MHIP – Mental Health Integration Program; MCPAP – Massachusetts Child Psychiatry Access Program; PHQ-9 – Patient Health Questionnaire; EPDS - Edinburgh Postnatal Depression Scale; RR- relative risk, CI - confidence interval
Acknowledgments
Disclosures and Funding:
Amritha Bhat is a postdoctoral fellow in the NIMH 537 T32 MH20021 Psychiatry-Primary Care Fellowship Program Training Grant. This work was partially funded by R01 MH085668.
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
References
- 1.Siu AL U.S. Preventive Services Task Force. Screening for depression in adults: US preventive services task force recommendation statement. JAMA. 2016;315(4):380–387. doi: 10.1001/jama.2015.18392. [DOI] [PubMed] [Google Scholar]
- 2.Committee on Obstetric Practice. The American College of Obstetricians and Gynecologists Committee Opinion no. 630. Screening for perinatal depression. Obstetrics and gynecology. 2015 May;125(5):1268–1271. doi: 10.1097/01.AOG.0000465192.34779.dc. [DOI] [PubMed] [Google Scholar]
- 3.Melville JL, Reed SD, Russo J, Croicu CA, Ludman E, LaRocco-Cockburn A, et al. Improving care for depression in obstetrics and gynecology: a randomized controlled trial. Obstetrics and gynecology. 2014 Jun;123(6):1237–1246. doi: 10.1097/AOG.0000000000000231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sepulcri RdP, do Amaral VF. Depressive symptoms, anxiety, and quality of life in women with pelvic endometriosis. European Journal of Obstetrics & Gynecology and Reproductive Biology. 2009;142(1):53–56. doi: 10.1016/j.ejogrb.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 5.Annagür BB, Kerimoglu ÖS, Tazegül A, Gündüz Ş, Gençoglu BB. Psychiatric comorbidity in women with polycystic ovary syndrome. Journal of Obstetrics and Gynaecology Research. 2015;41(8):1229–1233. doi: 10.1111/jog.12696. [DOI] [PubMed] [Google Scholar]
- 6.Bhat A, Byatt N. Infertility and Perinatal Loss: When the Bough Breaks. Current psychiatry reports. 2016;18(3):1–11. doi: 10.1007/s11920-016-0663-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khastgir G, Studd J. Hysterectomy, ovarian failure, and depression. Menopause. 1998;5(2):113–122. [PubMed] [Google Scholar]
- 8.National Prevention Council. National prevention strategy. Washington, DC: US Department of Health and Human Services, Office of the Surgeon General; 2011. [Google Scholar]
- 9.Fine A, Kotelchuck M. Rethinking MCH: The life course model as an organizing framework. US Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau; 2010. [Google Scholar]
- 10.Makuc DM, Freid VM, Kleinman JC. National trends in the use of preventive health care by women. American Journal of Public Health. 1989;79(1):21–26. doi: 10.2105/ajph.79.1.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Horton JA, Creuss DF, Pearse WH. Primary and preventive care services provided by obstetrician-gynecologists. Obstetrics & Gynecology. 1993;82(5):723–726. [PubMed] [Google Scholar]
- 12.Byatt N, Biebel K, Lundquist RS, Moore Simas TA, Debordes-Jackson G, Allison J, et al. Patient, provider, and system-level barriers and facilitators to addressing perinatal depression. Journal of Reproductive and Infant Psychology. 2012;30(5):436–449. [Google Scholar]
- 13.Grote NK, Katon WJ, Russo JE, Lohr MJ, Curran M, Galvin E, et al. Collaborative Care for perinatal depression in socioeconomically disadvantaged women: a randomized controlled trial. Depression and anxiety. 2015 doi: 10.1002/da.22405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Byatt N, Biebel K, Simas TAM, Sarvet B, Ravech M, Allison J, et al. Improving Perinatal Depression Care: The Massachusetts Child Psychiatry Access Project for Moms. General Hospital Psychiatry. doi: 10.1016/j.genhosppsych.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 15.Avenevoli S, Swendsen J, He J-P, Burstein M, Merikangas KR. Major Depression in the National Comorbidity Survey–Adolescent Supplement: Prevalence, Correlates, and Treatment. Journal of the American Academy of Child & Adolescent Psychiatry. 2015;54(1):37–44. e2. doi: 10.1016/j.jaac.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fergusson DM, Woodward LJ. Mental health, educational, and social role outcomes of adolescents with depression. Archives of general psychiatry. 2002;59(3):225–231. doi: 10.1001/archpsyc.59.3.225. [DOI] [PubMed] [Google Scholar]
- 17.Curtin SC, Warner M, Hedegaard H. Increase in suicide in the United States, 1999–2014. NCHS data brief. 2016;(241) [PubMed] [Google Scholar]
- 18.Barnet B, Liu J, DeVoe M. Double jeopardy: depressive symptoms and rapid subsequent pregnancy in adolescent mothers. Archives of Pediatrics & Adolescent Medicine. 2008;162(3):246–252. doi: 10.1001/archpediatrics.2007.60. [DOI] [PubMed] [Google Scholar]
- 19.Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: a systematic review of prevalence and incidence. Obstetrics and gynecology. 2005 Nov;106(5.1):1071–1083. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- 20.Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: a meta-analytic review. Clin Child Fam Psychol Rev. 2011 Mar;14(1):1–27. doi: 10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- 21.Cerimele JM, Vanderlip ER, Croicu CA, Melville JL, Russo J, Reed SD, et al. Presenting symptoms of women with depression in an obstetrics and gynecology setting. Obstetrics and gynecology. 2013;122(201):313. doi: 10.1097/AOG.0b013e31829999ee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhong Q-Y, Gelaye B, Rondon MB, Sánchez SE, Simon GE, Henderson DC, et al. Using the Patient Health Questionnaire (PHQ-9) and the Edinburgh Postnatal Depression Scale (EPDS) to assess suicidal ideation among pregnant women in Lima, Peru. Archives of women's mental health. 2015;18(6):783–792. doi: 10.1007/s00737-014-0481-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Werner EA, Gustafsson HC, Lee S, Feng T, Jiang N, Desai P, et al. PREPP: postpartum depression prevention through the mother–infant dyad. Archives of women's mental health. 2016;19(2):229–242. doi: 10.1007/s00737-015-0549-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hantsoo L, Epperson CN. Premenstrual Dysphoric Disorder: Epidemiology and Treatment. Current psychiatry reports. 2015 Nov;17(11):87. doi: 10.1007/s11920-015-0628-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.American Psychiatric Association. DSM 5: American Psychiatric Association. 2013. [Google Scholar]
- 26.Soares CN, Zitek B. Reproductive hormone sensitivity and risk for depression across the female life cycle: a continuum of vulnerability? Journal of psychiatry & neuroscience. 2008;33(4):331. [PMC free article] [PubMed] [Google Scholar]
- 27.Freeman EW. Associations of depression with the transition to menopause. Menopause. 2010;17(4):823–827. doi: 10.1097/gme.0b013e3181db9f8b. [DOI] [PubMed] [Google Scholar]
- 28.Burt VK, Stein K. Epidemiology of depression throughout the female life cycle. The Journal of clinical psychiatry. 2001;63:9–15. [PubMed] [Google Scholar]
- 29.Rubinow DR, Johnson SL, Schmidt PJ, Girdler S, Gaynes B. Efficacy of estradiol in perimenopausal depression: so much promise and so few answers. Depression and anxiety. 2015;32(8):539–549. doi: 10.1002/da.22391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bruce ML, Seeman TE, Merrill SS, Blazer DG. The impact of depressive symptomatology on physical disability: MacArthur Studies of Successful Aging. Am J Public Health. 1994 Nov;84(11):1796–1799. doi: 10.2105/ajph.84.11.1796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gunlicks ML, Weissman MM. Change in child psychopathology with improvement in parental depression: a systematic review. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47(4):379–389. doi: 10.1097/CHI.0b013e3181640805. [DOI] [PubMed] [Google Scholar]
- 32.Burke L. The impact of maternal depression on familial relationships. International Review of Psychiatry. 2003;15(3):243–255. doi: 10.1080/0954026031000136866. [DOI] [PubMed] [Google Scholar]
- 33.Huang H, Chan YF, Katon W, Tabb K, Sieu N, Bauer AM, et al. Variations in depression care and outcomes among high-risk mothers from different racial/ethnic groups. Fam Pract. 2012 Aug;29(4):394–400. doi: 10.1093/fampra/cmr108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Scholle SH, Haskett RF, Hanusa BH, Pincus HA, Kupfer DJ. Addressing depression in obstetrics/gynecology practice. General Hospital Psychiatry. 2003;25(2):83–90. doi: 10.1016/s0163-8343(03)00006-9. [DOI] [PubMed] [Google Scholar]
- 35.Flynn HA, O'mahen HA, Massey L, Marcus S. The impact of a brief obstetrics clinic-based intervention on treatment use for perinatal depression. Journal of Women's Health. 2006;15(10):1195–1204. doi: 10.1089/jwh.2006.15.1195. [DOI] [PubMed] [Google Scholar]