Abstract
Background
HIV and Intimate Partner Violence (IPV) are interconnected public health problems. However, few HIV prevention interventions address the unique needs of IPV survivors in shelter and none of the CDC’s best-evidence risk reduction interventions adequately explore the complex relationship between IPV and HIV risk. Although battered women’s shelters provide a safe and supportive environment for women in crisis, most do not offer HIV risk reduction services or sexual safety planning.
Methods
This study evaluated the feasibility, acceptability, and initial efficacy of a rapid HIV-testing and brief risk prevention intervention developed for residents of battered women’s shelters. The Safe Alternatives For Empowered sex for intimate partner violence (IPV) intervention (SAFE-IPV) was evaluated in an open trial (N = 98). Participants were assessed with a series of standardized interviews and self-reports at screening and three-months after leaving shelter.
Results
Few eligible participants declined SAFE-IPV and participants who received SAFE-IPV reported high levels of satisfaction. No participants in the open trial tested positive for HIV. However, participants reported significantly fewer unprotected vaginal and anal sexual occasions and increased intentions to engage in risk preventative behaviors three months after leaving shelter compared to the three months prior to shelter. Additionally, participants reported significant improvements on HIV-risk factors addressed in SAFE-IPV at three-month follow-up (i.e., reduced emotional, physical and sexual harm by abuser, posttraumatic stress symptoms, hazardous alcohol use, and drug use).
Discussion
Results extend prior research on HIV prevention with women with IPV, demonstrating the acceptability, feasibility and initial efficacy of SAFE-IPV within battered women’s shelter settings.
More than 1.2 million people in United States are currently living with HIV/AIDS, 12.8% of whom are unaware of their HIV status (Centers for Disease Control and Prevention (CDC), 2016). Further, approximately 50,000 new cases of HIV are diagnosed annually (CDC, 2016). Women account for approximately 20% of new HIV infections annually, and over 80% of new HIV infections in women are from heterosexual contact (CDC, 2015). Intimate Partner Violence (IPV) and HIV are parallel epidemics with interconnected risk factors in women (Phillips et al., 2014). IPV is highly prevalent in women, with approximately 1 in 3 women reporting rape, physical violence, and/or stalking by an intimate partner in their lifetime (Black et al., 2011).
Research has shown that IPV survivors compared to non-survivors are especially likely to engage in multiple HIV risk behaviors (e.g., coerced sexual violence by infected partner, limited skill in negotiating safe sex practices, unprotected sex, sex with risky partners, multiple sex partners, injection drug use; McCree, Koenig, Basile, Fowller, & Green, 2015; Li et al., 2014; Phillips et al., 2014). Additionally, posttraumatic stress disorder (PTSD) and substance use disorder (SUD), which are common in IPV survivors, are associated with increased HIV-risk behaviors (Cavanaugh et al., 2010; Harris et al., 2003; Phillips et al., 2014). IPV survivors also encounter distinct HIV risk factors, such as difficulty in negotiating condom use and other preventative sexual behaviors, out of fear of retaliation or being raped by their abusive partner (Li et al., 2014; Phillips et al., 2014; McCree et al., 2015).
Early knowledge of HIV status is critical to prevent transmission to others, to link HIV positive individuals to medical services that can reduce the morbidity, mortality and cost of care, and ultimately improve the quality of life of people living with HIV. However, a recent study found that almost half of women with histories of IPV have not been tested for HIV and thus do not know their HIV status (Rountree, Chen, & Bagwell, 2016). Although there is a significant need for HIV testing and preventative intervention for IPV survivors, few HIV prevention interventions incorporate tangible strategies to address IPV and none of the CDC’s best-evidence risk reduction interventions adequately explore the complex relationship between IPV and HIV risk (Prowse, Logue, Fantasia, & Sutherland, 2013).
Battered women’s shelters (BWS), a primary resource for survivors of IPV, can provide an opportune setting for HIV testing and risk prevention (Cavanaugh et al., 2016). Women in shelters have already initiated a change in their life, and BWS provide a confidential, safe, supportive, and resource rich environment where women can safely obtain test results, cope, and access treatment if HIV positive (Rountree, Goldback, Bent-Goodley, & Bagwell, 2011). However, in a study of 59 BWS, 54% did not disseminate HIV information to residents and only 17% offered testing or sexual safety planning (Rountree et al., 2011). More recently, Cavanaugh and colleagues (2016) conducted a needs assessment for HIV prevention services within BWS and found 92% of shelter staff reported that HIV interventions were never administered within shelter and only 35% reported that they provide HIV educational materials to residents. Additionally, recent research suggests that BWS staff and residents are open and supportive of integrating HIV prevention interventions within BWS (Draucker et al., 2015). Specifically, they found that the ease and promise of quick results of rapid HIV testing was acceptable to BWS staff and residents. Further, results suggest that shelters may provide a safe and opportune time for HIV testing and prevention (Draucker et. al., 2015).
Although researchers have proposed adaptations of existing evidence-based HIV prevention programs specifically for BWS (e.g., Cavanaugh et al., 2016), to date, only one HIV prevention intervention for women with IPV has been empirically evaluated (Rountree et al., 2014; Rountree & Mulraney, 2010). Rountree and colleagues developed a six-week, two-hour-per-session curriculum that focused on capacity building, sexual safety planning, and life skills (Rountree & Mulraney, 2010). Although preliminary results were promising, only 54% of the intervention group completed the program (Rountree et al., 2014). The authors suggested a shorter duration of HIV interventions to accommodate the multiple demands on IPV survivors’ lives.
The purpose of the current study was to explore the feasibility, acceptability, and initial efficacy of a rapid-HIV testing and brief (i.e., single session plus brief booster session) risk prevention intervention specifically developed for residents of BWS, “Safe Alternatives For Empowered sex for IPV” (SAFE-IPV), that focused on reducing high-risk behavior after leaving shelter. Our primary outcome was the number of unprotected vaginal or anal sexual occasions. Secondary outcomes included intentions to engage in risk-preventative behaviors, as well as other HIV-risk factors documented in the literature and addressed in the intervention (i.e., IPV, PTSD, and alcohol and drug use). Satisfaction with the intervention was also assessed. If the feasibility, acceptability, and preliminary efficacy of SAFE-IPV is supported it could serve as a model for future efforts to integrate HIV prevention interventions in BWS.
Intervention Development
Originally, the basis for SAFE-IPV was RESPECT (Metcalf et al., 2005), a 40-minute individual-level, client-focused HIV prevention intervention based in the Theory of Reasoned Action and Social Cognitive Theory. We expanded RESPECT to address the unique needs of survivors of IPV. However, after completing several focus groups ((Draucker et al., 2015) and an open trial it became clear that a core component of RESPECT (i.e., focusing on the individuals’ state of conflict and creating cognitive dissonance between her beliefs and behavior) was not well-tolerated by IPV survivors. Thus, SAFE-IPV maintained the overall structure of RESPECT (i.e., orientation to rapid HIV testing, discussion of most recent risk incident, creation of a risk reductions step or plan (RRP), provision of test results, and revision of RRP), but drew more on empowerment theory (Cattaneo & Chapman, 2010), and included several additional components (see below) to meet the unique needs of IPV survivors in shelter.
SAFE-IPV is a 90-minute intervention that focuses on the participants’ emotional safety and sexual empowerment. SAFE-IPV begins with an orientation to rapid HIV testing, including an assessment of the participants’ safety and comfort level for testing in the shelter. The rapid HIV test was administered only if both the participant and interventionist agreed it was the right decision for the participant. Following the collection of an oral specimen for HIV testing, the session turned to an assessment of the participants’ HIV risk behaviors. This discussion included education and assessment of IPV-related risks, feedback regarding their substance use and PTSD symptoms and how this may impact their risk, assessment of partner-related risks (i.e., increased risk for intravenous drug use, multiple sexual partners), and assessment of safety concerns and how they may impact risk (e.g., implications of asking abuser to wear a condom). Safety planning, including sexual safety planning, was incorporated throughout the intervention protocol.
After a thorough understanding of the participant’s primary risk factors for HIV and other sexually transmitted infections (STIs), the most recent risk incident is identified and assessed, as are recent efforts to reduce risk for HIV/STI. Rather than highlighting the cognitive dissonance between a participants’ behavior and beliefs, SAFE-IPV validates a woman’s behavior within the context of her experience of IPV and focuses on helping her identify aspects of her risk that are under her control, empowering women to identify strategies where they can take control of their sexual health. This process includes education on the female condom as a way women can take control of their sexual health and addresses safety risks that may result from asking an abusive partner to wear a condom. Additionally, participants are provided female condoms and encouraged to use them with future sexual partners. Barriers to risk reduction, including IPV, substance use, and PTSD symptoms are discussed, as are strategies to reduce those risks. Triggers to risk behaviors (i.e., an abusive incident, emotional numbing) are identified and incorporated into the development of a Risk Reduction Plan (RRP). The interventionist works collaboratively with the client to identify a RRP which includes identifying safe sources of support for the woman and often includes referrals to assist her in expanding her safe support network. After developing the RRP, the interventionist provides test results, processes those results, and adjusts the RRP and safety plan, if necessary. The session ends with provision of personalized referrals to address issues identified in session and the scheduling of a booster session.
The booster session (a brief 10-minute session during shelter stay) was implemented after completing the first nine interventions of the open trial to provide a participant with the opportunity to touch base with her counselor regarding any further referral needs, to further process their SAFE-IPV session and test results, if necessary, and ask further questions, if needed.
Methods
Participants were recruited from six regional BWS in Northeast Ohio. All research procedures were approved by the university Institutional Review Board. To further protect participants’ confidentiality, a Certificate of Confidentiality was received from the National Institutes of Health. The current study consisted of two phases: (1) the screening phase, and (2) the intervention and follow-up phase. All shelter residents were eligible for the screening phase. To protect participants’ privacy and confidentiality, we only advertised for a general study on sexual risk taking. Advertisement occurred through brochures, posted signs, and recruitment sessions during shelter house meetings. At this time, participants signed a written informed consent for the screening phase and were asked to provide permission to be contacted if their responses qualified them for future studies. The screening phase consisted of a series of in-person interviews and self-report measures as described below. All assessments occurred in a confidential and private space in shelter. Participants were invited to participate in the intervention phase if they endorsed: (1) at least one unprotected vaginal and/or anal sexual occasion (USO) with a male partner in the three months prior to shelter or a minimum of five USOs with a male partner in the six months prior to shelter, (2) IPV in the three months prior to shelter, and (3) never received an HIV diagnosis.
Participants who met inclusion criteria for the intervention phase were offered the intervention and at that time provided written informed consent for participation in the intervention and follow-up assessments. Refusal rates and reasons for refusal were recorded for all participants who declined the intervention. Participants also completed a booster session with their interventionist within two weeks of their initial session, if still in shelter. All SAFE-IPV sessions occurred in a private and confidential space within shelter.
Participants completed a follow-up assessment at three months post-shelter (3MPS) at a safe and private location of the participants’ choosing. Participants were reimbursed between $20 and $40 for assessment and booster sessions; participants were not reimbursed for participation in SAFE-IPV. All assessments were conducted by trained doctoral students in psychology, under the supervision of the first author (DJ). SAFE-IPV sessions were conducted by either (1) trained doctoral students in psychology (n = 3) or (2) trained-personnel who provide rapid HIV testing in the community (n = 2). All SAFE-IPV interventionists completed a series of 2.5-day workshops in SAFE-IPV and IPV, and a state health department training in proper administration of rapid HIV-testing. All HIV-testing was conducted within accordance to Ohio statutes.
Measures
The Timeline Followback (TLFB) was used to assess unprotected vaginal and anal sex at screening and 3MPS. The TLFB is a calendar assisted structured interview that provides a way to cue memory so that accurate recall is enhanced for event-level data. The TLFB has established reliability and validity in substance-using populations (e.g., Sobel, Sobell, Leo, & Cancilla, 1988) and has more recently been adapted to assess sexual risk-taking with excellent reliability and validity (Stein, Charuvastra, Anderson, Sobota, & Friedmann, 2002). At screening and 3MPS, a detailed, assessment of sexual behaviors and condom use was made for each of the participant’s sexual partners. Number of USOs was computed for the three months prior to shelter and for the three month period post shelter discharge.
At screening and 3MPS participants’ intentions to perform behaviors that will reduce their risk of contracting HIV (i.e., Risk Intentions) was assessed through seven self-report items previously shown to be reliable (e.g., “I will use a condom,” “I will not drink or use drugs before sex so I can be clear-headed”) (Carey et al., 1997). Participants read a detailed vignette of high-risk sexual situations and indicated how likely they are to engage in each of seven interpersonal or behavioral strategies that will reduce their risk of HIV infection on an 8-point rating scale ranging from definitely will not do to definitely will do. This measure has demonstrated excellent reliability in prior research (α’s = .90- .95; Carey et al., 1997), as well as in the current study (α = .95).
Additional secondary outcomes relevant to our target population were assessed with a series of self-report measures at screening and 3MPS. IPV was assessed with the Severity of Violence Against Women Scale (SVAWS) (Marshall, 1992). The SVAWS is a 46-item scale with three subscales that assess the frequency and severity of emotional harm (19 items), physical harm (21 items), and sexual harm (6 items) in women. The SVAWS subscales demonstrated excellent reliability in the current study (α’s = .93, .95, .88; respectively). IPV-related PTSD symptom severity was assessed with the Davidson Trauma Scale (DTS) (Davidson et al., 1997), a 17-item self-report scale that assesses the 17 DSM-IV symptoms of PTSD in the past week. The DTS has demonstrated strong reliability in prior research (α=.99; Davidson et al., 1997), as well as in the current study (α=.88). Hazardous alcohol use was assessed with the Alcohol Use Disorders Identification Test (AUDIT) (Saunders, Aasland, Babor, De La Fuente, & Grant, 1993). The AUDIT is a 10-item questionnaire that assesses hazardous and harmful alcohol consumption with established reliability, as well as sensitivity and specificity for detecting hazardous alcohol use. The AUDIT total score demonstrated good reliability in the current study (α = .86). Use of illicit drugs was assessed with items from the Risk Assessment Battery (RAB) (Metzger, Nalvaline, Woody, 2001). The RAB is a self-administered, multiple choice questionnaire with established reliability and validity that assesses drug use during the last 30 days, as well as injection and sexual risk in the last six months. For this study, a categorical variable indicating whether or not the participant endorsed any illicit drug use in the last 30 days was created.
Since SAFE-IPV adopts an empowerment approach and introduces the female condom as a potential method where women can safely take control of their STI/HIV protection, participants were asked whether they have used a female condom, as well as their intent to use a female condom (rated on a 5-point scale ranging from not at all likely to very likely) at 3MPS.
HIV status was assessed during the SAFE-IPV session via oral fluids with the OraQuick Advance® Rapid HIV-1/2 Antibody Test (OraSure Technologies, Inc, Bethlehem, PA). The OraQuick test is CLIA-waived, detects antibodies to HIV-1 and HIV-2 in 20 minutes, and has high sensitivity (86.6) and specificity (99.9; Pilcher et al., 2013). If a participant were to test positive or have unprotected sex outside of the three month window that the test can detect HIV antibodies, participants were provided with referrals to locations where they could receive confidential and free HIV testing in their community.
Intervention acceptability and satisfaction were assessed immediately after completing the SAFE-IPV session (i.e., post-intervention) and at 3MPS using the well-studied 8-item Client Satisfaction Questionnaire-Revised (CSQ-8-R) (Attkisson & Zwick, 2004). Participants rated their satisfaction with the intervention on a 4-point scale ranging from 1-quite dissatisfied to 4-very satisfied. The CSQ-8-R demonstrated sound reliability in the current study (α = .79)
Statistical Procedures
Primary and secondary continuous outcomes were analyzed according to the intent-to-treat sample, including all 98 participants who consented for SAFE-IPV. Given the occurrence of attrition at 3MPS (n = 87; 89% retention), comparisons of means of continuous outcomes at screening and 3MPS were performed with latent change scores (LCS) models in M-Plus, which allowed for direct testing of significance of mean changes (Coman et al., 2013) and use of full information maximum likelihood (FIML) to account for missing data. A McNemar’s test was used to compare the number of women who reported drug use at screening and 3MPS. Finally, descriptive statistics are reported from 3MPS regarding participants’ use, and likelihood of future use, of the female condom.
Results
Acceptability and Feasibility
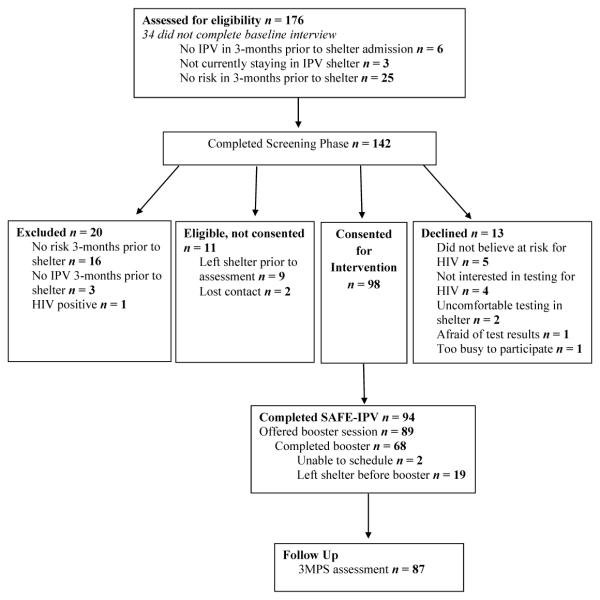
Participant flow through the study is depicted in Figure 1. Feasibility and acceptability of SAFE-IPV was assessed with eligibility and participation rates, as well as overall satisfaction with the intervention. A total of 142 shelter women completed the screening phase; 122 (85.9%) were eligible for the open trial. Of the 122, 13 (10.7%) verbally declined to participate in SAFE-IPV, 11 (9.0%) were eligible but not consented, and 98 participants consented for SAFE-IPV. Of those who consented, 94 completed the SAFE-IPV protocol. No participant who consented to SAFE-IPV and received the intervention, declined rapid HIV-testing. Satisfaction was rated high at post-intervention (N = 94) and 3MPS (N = 87), M’s = 3.84 & 3.86; SD’s = .25, .23, respectively.
Figure 1.
CONSORT diagram of participant flow through the protocol. IPV= intimate partner violence; PTSD= posttraumatic stress disorder; 3MPS = 3 months post-shelter.
Intervention Fidelity
Twenty-one randomly selected intervention sessions were rated for adherence to the SAFE-IPV protocol by study personnel trained in the intervention. Raters indicated presence or absence of 14 core components of SAFE-IPV and then rated overall adherence and competence on 7-point scales ranging from poor to excellent. On average, overall adherence was rated very good to excellent (M = 6.43, SD = .81), and competence or skill in delivery of the protocol was rated very good (M = 5.95, SD = .92).
Open Trial
No participant who completed the SAFE-IPV protocol tested positive for HIV. Demographic characteristics of the 98 participants in the open trial are found in Table 1. Data were determined to be missing completely at random (MCAR) using Little’s MCAR test, χ2 (33) = 17.90, p = .985; therefore, FIML is appropriate. Table 2 displays means, standard error, and effect sizes of primary and secondary outcomes at baseline and follow-up. Statistically significant differences were found between number of USOs at baseline and 3MPS, Wald χ2 (1) = 20.89, p< .001; intention to engage in risk-preventative behaviors, Wald χ2 (1) = 29.10, p < .001; severity of emotional, Wald χ2 (1 = 261.00, p < .001, physical, Wald χ2 (1) = 197.51, p < .001 and sexual harm, Wald χ2 (1) = 93.71, p < .001; IPV-related PTSD severity, Wald χ2 (1) = 34.39, p < .001; and hazardous alcohol use, Wald χ2 (1) = 7.35, p = .007. A significant difference was also found between the number of women who reported drug use at baseline and at 3MPS, χ2 (1) = 17.46, p < .001 (see Table 2).
Table 1.
Sample Characteristics of Open Trial (N= 98)
| Variable | ||
|---|---|---|
|
| ||
| M/n | SD/% | |
| Age | 33.10 | 10.01 |
| Race | ||
| African American | 43 | 43.9 |
| Caucasian | 49 | 50.0 |
| Biracial | 5 | 5.1 |
| American Native | 1 | 1.0 |
| Ethnicity (% Hispanic) | 11 | 11.2 |
| Highest Education Obtained | ||
| Less than high school | 21 | 21.4 |
| High school/GED | 26 | 26.5 |
| Completed some college | 39 | 39.8 |
| Graduated from college | 12 | 12.2 |
| Receiving Public Assistance | 91 | 92.9 |
| Employed | 11 | 11.2 |
| Income under 10,000/year | 94 | 95.9 |
| Lifetime STI diagnosis | 69 | 70.4 |
Note. Values are either reported as M, SD or n, %. STI = sexually transmitted infection.
Table 2.
Descriptive analyses and Effect Sizes for Primary and Secondary Outcomes (N = 98)
| Baseline | 3MPS | |||||
|---|---|---|---|---|---|---|
| M | SE | M | SE | Cohen’s D | 95% CI | |
|
|
||||||
| USO | 31.03 | 48.10 | 6.93 | 20.05 | 0.66 | −4.48 – 5.79 |
| Risk Intentions | 44.33 | 13.85 | 51.38 | 7.01 | −0.66 | −2.18 – .87 |
| SVAWS-E | 31.62 | 1.54 | 4.28 | 1.05 | 2.16 | 0.26-4.07 |
| SVAWS-P | 27.44 | 1.75 | 2.01 | 0.90 | 1.91 | −0.12-3.95 |
| SVAWS-S | 5.67 | 0.56 | 0.40 | 0.23 | 1.28 | 0.66-1.90 |
| DTS | 71.49 | 34.49 | 45.37 | 39.14 | 0.71 | −4.43 – 5.85 |
| AUDIT | 3.65 | 5.58 | 2.13 | 3.79 | 0.32 | −0.34 – 0.99 |
| Drug Use1 | 56 | 57.1 | 24 | 27.3 | 7.80 | 2.14 – 28.42 |
Note. All analyses are significant at p < .05. 3-mo PS = 3-months post shelter; USO = Unprotected Sexual Occasions; AUDIT = Alcohol Use Disorder Identification Test; SVAWS-E = Severity of Violence Against Women Scale-Emotional Harm; SVAWS-P = Severity of Violence Against Women Scale-Physical Harm; SVAWS-S = Severity of Violence Against Women Scale-Sexual Harm; DTS = Davidson Trauma Scale; 3MPS = 3-months post shelter.
Due to the categorical nature of drug use, statistics are reported as the n, %, and Odds Ratio, further, due to missing data at follow-up n = 74.
Many women (22.4%) reported that they already had used a female condom at 3MPS. Additionally, 55.1% reported that they were somewhat likely to very likely to use a female condom in the future.
Discussion
The current study extends prior HIV prevention intervention research with women with IPV (Cavanaugh et al., 2016; Draucker et al., 2015; Rountree & Mulrancy, 2010; Rountree et al., 2014), highlighting both the need for such services, as well as the feasibility in delivering such interventions within BWS settings. Consistent with the recommendations of Rountree et al. (2014), results suggest that women with IPV are more likely to engage in a brief, single-session intervention rather than a multi-session intervention given their demanding lives. SAFE-IPV appears to be feasible and acceptable to women in BWS. Only 13 participants verbally declined to participate in SAFE-IPV, with an overwhelming majority of participants eligible for SAFE-IPV participating in the intervention (80%) and most women completing the intervention (96%). Only two women indicated that they were uncomfortable with being tested for HIV within the shelter environment. No woman who participated in SAFE-IPV refused testing, even after a discussion of the emotional risk associated with receiving positive results during a period of crisis in a shelter environment. Shelter residents also reported high levels of satisfaction with the intervention. These findings further support that women perceive shelters as a safe and protective environment for HIV testing and risk prevention (Cavanaugh et al., 2016; Rountree et al., 2011).
SAFE-IPV, consistent with prior HIV prevention research with women with IPV that also focused on the inter-related risk of IPV and HIV (Rountree et al., 2014), was associated with significant gains for women. Specifically, SAFE-IPV was associated with reduced unprotected vaginal or anal sex, increased intent to engage in risk-preventative behaviors, reduced emotional, physical, and sexual IPV, PTSD symptoms, hazardous alcohol use, and drug use. Results, although promising, are preliminary and future research is needed to establish the efficacy of SAFE-IPV.
The inclusion of specific instruction on and access to the female condom appeared to be helpful to the women. The female condom provides women with an opportunity to take control of their sexual health and reduce the risk that may be associated with asking an abuser to use a condom. A majority of participants (55.1%) indicated some intent of using a female condom in the future. Although it is impossible to determine if this represents a change from pre-intervention as use of female condoms was only assessed at follow-up, these findings suggest that the female condom may be an acceptable preventative strategy with this population.
Interestingly, the primary reasons participants declined SAFE-IPV included not perceiving themselves to be at risk for HIV (n = 5) or not wanting an HIV test (n = 4). It is possible that some shelter residents do not fully understand their risk for HIV and STIs, and thus, consistent with extant recommendations (Cavanaugh et al., 2016; Rountree et al., 2011), further demonstrates the need for HIV/STI education within the shelter setting. Participants reported a large number of USOs prior to shelter (see Table 2), with an overwhelming majority of women reporting a lifetime history of at least one STI (70.4%). However, this risk did not translate into HIV positive diagnoses (i.e., no one tested positive for HIV). Most participants reported at least one unprotected sexual occasion within the last three months, when HIV antibodies may not be detectable with the OraQuick Advance® Rapid HIV-1/2 Antibody Test. Thus, future research should examine the need for ongoing HIV and STI testing in conjunction with continued prevention efforts in this high risk population.
Strengths of this study include the use of reliable and valid measures, the assessment of adherence to and competent delivery of the SAFE-IPV protocol, as well as high intervention completion and study follow-up rates. Additionally, some interventionists were community testers, supporting our ability to train such individuals in the SAFE-IPV protocol. Limitations of the study include the open trial design, and lack of a control group. Without a control group, participants’ risk behavior reduced as a result of SAFE-IPV or other factors cannot be determined. Further, results may not generalize to IPV survivors not in BWS. Additionally, a longer follow-up period than the current study is needed to assess if changes can be sustained.
Implications for Practice and Policy
Results of this research suggests that brief HIV intervention may be well suited to BWS settings. Further, high participation, completion, and satisfaction rates for SAFE-IPV in shelter women suggest that BWS present a prime opportunity for HIV prevention intervention. Despite the need for intervention, a majority of shelters do not integrate HIV and STI education, testing, and/or prevention in standard shelter services (Cavanaugh et al., 2016; Rountree et al., 2011). To improve HIV/STI-related services for IPV survivors in BWS, BWS funding sources need to recognize the need for such services in BWS and dedicate funds to address this neglected health concern.
Conclusions
Albeit preliminary, study results are promising and support the feasibility, acceptability, and initial efficacy of SAFE-IPV. Additionally, research findings highlight the need for brief HIV prevention interventions within BWS. Future research on SAFE-IPV should include a randomized design with an attention and time matched control group and a longer follow-up period.
Acknowledgements
This work was supported by NIMH grant 1R21NR013628 and the Lifespan/Tufts/Brown Center for AIDS Research P30AI42853. ClinicalTrials.gov Identifier: NCT01866046. We would like to thank Dawn Glenny, Rebecca Calahan, Myriam Kadeba, Brittany Baker, Samantha Holmes, Taylor Ceroni, Laura Pappa, Sarah Sanders, Kathleen Alto, Katherine Fedele, Vanessa Facemire, Barbara Foster, and the staff and residents of the Battered Women’s Shelter of Summit and Medina Counties, Safer Futures, Domestic Violence Project, Inc., and the Domestic Violence & Child Advocacy Center for their assistance in data collection and/or intervention support.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Descriptions
Dawn M. Johnson, Ph.D. is an Associate Professor at the University of Akron. Her research has focused on the treatment of PTSD in victims of intimate partner violence, as well as developing interventions to promote women’s sexual health and empowerment and to prevent violence against women.
Nicole L. Johnson, Ph.D. is now an Assistant Professor at Lehigh University. Her research is dedicated to the exploration and implementation of prevention programming for gender-based violence. Her professional interests include: advocacy, outreach, feminist theory/practice and mixed method research.
Patrick Palmieri, PhD, is the Director of the Center for the Treatment and Study of Traumatic Stress, Summa Health System, Akron, OH. His research and clinical interests focus on the assessment and treatment of PTSD and other trauma-related problems.
Dr. Zlotnick is Professor at the Alpert Medical School of Brown University. She is an Honorary Professor in the Department of Psychiatry and Mental Health, University of Cape Town. Dr. Zlotnick’s expertise is in intervention research for high-risk women.
Curt Beckwith, MD is Associate Professor of Medicine affiliated with The Miriam Hospital and the Alpert Medical School of Brown University. Dr. Beckwith conducts research related to the optimization of HIV testing, linkage, and retention in care among vulnerable populations.
Conflicts of Interest: Dr. Zlotnick’s husband was a consultant for Soberlink. All other authors declare that they have no conflicts of interest.
References
- Attkisson CC, Zwick R. The UCSF client satisfaction scales: I. The Cleint Satisfaction Questionnaire-8. In: Maruish ME, editor. The use of psychological testing for treatment planning and outcomes assessment. 3rd Lawrence Elbbaum Associates; hwah, NJ: 2004. [Google Scholar]
- Black MC, Basile KC, Breiding MJ, Smith SG, Walters ML, Merrick MT, Chen J, Stevens MR. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Summary Report. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; Atlanta, GA: 2011. [Google Scholar]
- Carey MP, Maisto SA, Kalichman SC, Forsyth AD, Wright EM, Johnson BT. Enhancing motivation to reduce the risk of HIV infection for economically disadvantaged urban women. Journal of Consulting and Clinical Psychology. 1997;65:531–541. doi: 10.1037//0022-006x.65.4.531. doi: 10.1037/0022-006X.65.4.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cattaneo LB, Chapman AR. The process of empowerment: A model for use in research and practice. American Psychologist. 2010;65:646–659. doi: 10.1037/a0018854. doi: 10.1037/a0018854. [DOI] [PubMed] [Google Scholar]
- Cavanaugh CE, Campbell J, Braxton N, Harvey J, Wingwood G. Adapting an evidence-based HIV-prevention intervention for women in domestic violence shelters. Psychology of Violence. 2016;6:469–477. doi: 10.1037/vio0000042. doi:10.1037/vio000042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanaugh CE, Hansen NB, Sullivan TP. HIV sexual risk behavior among low-income women experiencing intimate partner violence: The role of posttraumatic stress disorder. AIDS and Behavior. 2010;14:318–327. doi: 10.1007/s10461-009-9623-1. doi:10.1007/s10461-009-9623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention HIV in the United States: At a glance. 2015 Retrieved April 8th, 2016 from http://www.cdc.gov/hiv/statistics/overview/ ataglance.html. [Google Scholar]
- Coman EN, Picho K, McArdle JJ, Villagra V, Dierker L, Iordache E. The paired t-test as a simple latent change score model. Frontiers in Psychology. 2013;4:1–3. doi: 10.3389/fpsyg.2013.00738. doi: 10.3389/fpsyg.2013.00738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson JRT, Book SW, Colket JT, Tupler LA, Roth S, David D, Feldman ME. Assessment of a new self-rating scale for post-traumatic stress disorder. Psychological Medicine. 1997;27:153–160. doi: 10.1017/s0033291796004229. [DOI] [PubMed] [Google Scholar]
- Draucker CB, Johnson DM, Johnson-Quay NL, Kadeba MT, Mazurczyk J, Zlotnick C. Rapid HIV testing and counseling for residents in domestic violence shelters. Women & Health. 2015;55:334–352. doi: 10.1080/03630242.2014.996726. doi:10.1080/03630242.2014.996726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Marshall CM, Rees HC, Nunez A, Ezeanolue EE, Ehiri JE. Intimate partner violence and HIV infection among women: A systematic review and meta-analysis. Journal of the International AIDS Society. 2014;17:28845. doi: 10.7448/IAS.17.1.18845. doi: 10.7448/IAS.17.1.18845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris RM, Sharps PW, Allen K, Anderson EH, Soeken K, Rohatas A. The interrelationship between violence, HIV/AIDS, and drug use in incarcerated women. Journal of the Association of Nurses in AIDS Care. 2003;14:27–40. doi: 10.1177/1055329002239188. doi: 10.1177/1055329002239188. [DOI] [PubMed] [Google Scholar]
- Li Y, Marshall CM, Rees HC, Nunez A, Ezeanolue EE, Ehiri JE. Intimate partner violence and HIV infection among women: A systematic review and meta-analysis. Journal of the International AIDS Society. 2014;17:18845. doi: 10.7448/IAS.17.1.18845. doi: 10.7448/IAS.17.1.18845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall LL. Development of the severity of violence against women scales. Journal of Family Violence. 1992;7:103–121. [Google Scholar]
- McCree DYH, Koenig LJ, Basile KC, Fowler D, Green Y. Addressing the intersection of HIV and intimate partner violence among women with or at risk for HIV in the United States. Journal of Women’s Health. 2015;24:331–335. doi: 10.1089/jwh.2015.5301. doi: 10.1089/jwh.2015.5301. [DOI] [PubMed] [Google Scholar]
- Metcalf CA, Douglas JM, Malotte CK, Cross H, Dillon BA, Paul SM, Peterman TA. Relative efficacy of prevention counseling with rapid and standard HIV testing: A randomized, controlled trial (RESPECT-2) Sexually Transmitted Diseases. 2005;32:130–138. doi: 10.1097/01.olq.0000151421.97004.c0. doi: 10.1097/01.olq.0000151421.97004.c0. [DOI] [PubMed] [Google Scholar]
- Metzger DS, Nalvaline HA, Woody GE. Assessment of substance abuse: HIV risk assessment battery. In: Carson-Sewitt R, editor. Encycholopedia of Drugs, Alcohol and Addictive Behavior. 2nd Macmillan Reference; Farmington Hills, MI: 2001. [Google Scholar]
- Phillips DY, Walsh B, Bullion JW, Reid PV, Bacon K, Okoro N. The intersection of intimate partner violence and HIV in U.S. women: A review. Journal of the Association of Nurses in AIDS Care. 2014;25:S36–S49. doi: 10.1016/j.jana.2012.12.006. doi: 10.1016/j.jana.2012.12.006. [DOI] [PubMed] [Google Scholar]
- Pilcher CD, Louie B, Facente S, Keating S, Hackett J, Vallari A, et al. Performance of rapid point-of-care and laboratory tests for acute and established HIV infection in San Francisco. PLOS One. 2013;8:e80629. doi: 10.1371/journal.pone.0080629. doi:10.1371/journal.pone.0080629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prowse KM, Logue CE, Fantasia HC, Sutherland MA. Intimate partner violence and the CDC’s best-evidence HIV risk reduction interventions. Public Health Nursing. 2013;31:215–234. doi: 10.1111/phn.12076. doi: 10.1111/phn.12076. [DOI] [PubMed] [Google Scholar]
- Rountree MA, Bagwell M, Theall K, McElhaney C, Brown A. Lessons learned: Exploratory study of a HIV/AIDS prevention intervention for African American women who have experienced intimate partner violence. Journal of Health Disparities Research and Practice. 2014;7:24–46. [Google Scholar]
- Rountree MA, Chen L, Bagwell M. HIV-testing rates and testing locations among women who have experienced intimate partner violence: Data from the Centers for Disease Control Behavioral Risk Factor Surveillance System, 2006. Violence Against Women. 2016;22:399–414. doi: 10.1177/1077801215603487. doi:10.1177/1077801215603487. [DOI] [PubMed] [Google Scholar]
- Rountree MA, Goldbach J, Bent-Goodley T, Bagwell M. HIV/AIDS knowledge and prevention programming in domestic violence shelters: How are we doing? Journal of HIV/AIDS & Social Services. 2011;10:42–54. doi: 10.1080/15381501.2011.549068. [Google Scholar]
- Rountree MA, Mulraney M. HIV/AIDS risk reduction intervention for women who have experienced intimate partner violence. Clinical Social Work Journal. 2010;38:207–216. doi: 10.1007/s10615-008-0183-z. doi: 10.1007/s10615-008-0183-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, De La Fuente JR, Grant M. Developtment of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell JMB, Leo GI, Cancilla A. Reliability of a timeline method: Assessing normal drinkers’ report of recent drinking and a comparative evaluation across several populations. British Journal of Addiction. 1988;83:393–402. doi: 10.1111/j.1360-0443.1988.tb00485.x. [DOI] [PubMed] [Google Scholar]
- Stein MD, Charuvastra A, Anderson B, Sobota M, Friedmann PD. Alcohol and HIV risk taking among intravenous drug users. Addictive Behaviors. 2002;27:727–736. doi: 10.1016/s0306-4603(01)00205-2. doi: 10.1016/S0306-4603(01)00205-2. [DOI] [PubMed] [Google Scholar]