The operating room is a common site for adverse events in the hospital, which are largely related to communication breakdowns and surgical flow disruptions leading to error cycles.1-4 To reduce the rate of preventable adverse events and enhance patient safety, we present what is, to our knowledge, the first clinical use of the HUB,5 a computer-assisted system designed to support intraoperative team performance.
Methods
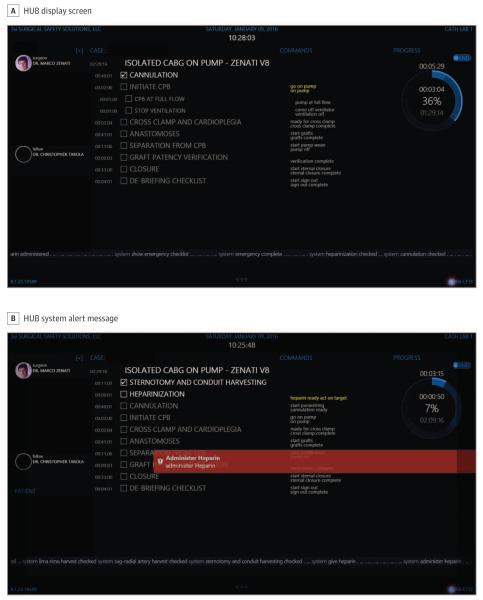
We designed a single-site, prospective pilot investigation to determine the feasibility of the HUB5 mobile workflow management system (3Si Systems LLC), which uses speech-recognition technology to support intraoperative team communication and adherence to best-practice guidelines. Based on prior audio recordings of 9 cardiac procedures, process models composed of major procedural steps were developed onto software and preloaded on the HUB preoperatively (Table). The HUB recognizes voice commands (derived from the audio recordings and specific to each team member) by key team members fitted with high-fidelity microphones (earpiece or clip-on) that correspond to procedural steps that initiate appropriate algorithms (Figure, A) or alert the team if inadvertently omitted (Figure, B).
Table.
Procedure Algorithm for Conventional Coronary Artery Bypass Grafting
| Task | Subtask | Description | Start Commanda | End Commanda,b |
|---|---|---|---|---|
| 1 | Patient in the room | “Patient in the room” | NA | |
| 2 | Preinduction checklist | “Start time-out” | NA | |
| 2.1 | Patient confirmation | NA | “Patient is confirmed” | |
| 2.2 | Preanesthesia check | NA | “Anesthesia checklist complete” |
|
| 2.3 | Perfusion check | NA | “Pump checklist complete” | |
| 2.4 | Sponge/sharps/ instrument count |
NA | “Instrument count complete” |
|
| 3 | Anesthesia induction | “Start induction” | “Induction complete” | |
| 4 | Preincision time-out | “Incision time-out” | ||
| 4.1 | Confirm patient and procedure | NA | “Site and procedure confirmed” |
|
| 4.2 | Surgeon review of operating plan | NA | “Review of operating plan” | |
| 4.3 | Anesthesia review of plan | NA | “Any anesthesia concerns?” | |
| 4.4 | Nursing review of plan | NA | “Any nursing concerns?” | |
| 4.5 | Prophylactic antibiotics | NA | “Antibiotic has been given” | |
| 5 | Sternotomy and conduit harvesting |
“Scalpel” | NA | |
| 5.1c | Sternotomy and ventilator off | “Sternal saw” | “Vent off” | |
| 5.2c | Turn ventilator on | “Vent back on” | “Vent on” | |
| 5.3 | Mammary artery harvest | NA | “LIMA retractor” | |
| 5.4 | Saphenous vein harvest | NA | “Vein ready” | |
| 6 | Epiaortic scan | NA | “Epiaortic probe” | |
| 7 | Heparinization | “Give heparin” | “Heparin given” | |
| 7.1 | Activated clotting time check | “ACT Check” | “ACT on target” | |
| 8 | Cannulation | “Let’s cannulate” | NA | |
| 8.1 | Arterial cannulation | NA | “Arterial cannula” | |
| 8.2 | Venous cannulation | NA | “Venous cannula” | |
| 8.3 | Antegrade cardioplegia | NA | “Antegrade cannula” | |
| 9c | Initiate cardiopulmonary bypass | “Start bypass” | “Full flow” | |
| 10 | Cross clamp and cardioplegia | “Cross clamp” | NA | |
| 10.1c | Turn flow down | “Flow down” | “Pump flow down” | |
| 10.2c | Cross clamp aorta | “Clamp on, flow up” | “Flow back up” | |
| 10.3c | Administer antegrade cardioplegia |
“Start antegrade” | “Cardioplegia flowing” | |
| 11 | Distal anastomoses | “Can I have the vein” | “Distals complete” | |
| 12 | Proximal anastomoses | “Side-biting clamp” | “Proximals compete” | |
| 13 | Separation from cardiopulmonary bypass |
“Wean pump” | NA | |
| 13.1c | Restart ventilation | “Restart vent” | “Vent on” | |
| 13.2c | Reduce pump flow | “Pump flow down” | “Half flow” | |
| 13.3c | Terminate bypass | “Come off pump” | “We are off pump” | |
| 13.4 | Check graft patency | “Graft check” | ||
| 13.5c | Administer protamine | “Start protamine” | “Protamine is going in” | |
| 13.6c | Discontinue pump sucker | “Stop pump suckers” | “Pump suckers off” | |
| 14 | Incision closure | “Start sternal closure” | NA | |
| 14.1 | Final instrument count | NA | “Instrument count correct” | |
| 14.2 | Check bleeding sites | NA | “Bleeding sites ok” | |
| 14.3 | Place chest tubes | NA | “Chest tubes” | |
| 14.4 | Skin closure | NA | “Skin closed” | |
| 15 | Transfer patient to intensive care |
NA | “Let’s go to ICU” |
Abbreviations: ACT, activated clotting time; ICU, intensive care unit; LIMA, left internal mammary artery; NA, not applicable.
All commands are derived from the natural operating language of the surgeons partaking in this study.
An “End Command” can both initiate and end a phase or subtask. On completion of all “Subtasks,” a “Task” is automatically ended.
Identifies a step requiring confirmation from another team member (end command expected from anesthesia or perfusion).
Figure 1. HUB System Display Screen.
A, HUB system display screen demonstrating surgical team on left (highlighted if checked in), procedural algorithm in the center (highlighted if completed), and progress bar on right. B, Example of an alert message displayed by HUB system secondary to omitted step.
Functionality of the HUB was tested between May 2015 and March 2016 during 5 procedures: minimally invasive coronary artery bypass grafting, 2 conventional coronary artery bypass graftings, aortic valve replacement/coronary artery bypass grafting, and isolated aortic valve replacement. The primary outcome measured was the qualitative ability of the HUB to distinguish commands from conversational speech. The study was approved by the Veterans Affairs Boston Healthcare System institutional review board, and all research participants provided written informed consent.
Results
The HUB system registered key surgical team members using the phrase “check-in [team member name].” Collectively, 62 major steps and 216 subtasks were tested in the procedural algorithms. All task phrases were distinguished from conversational speech and recorded appropriately by the HUB; however, 62 steps required repetition before system acknowledgment.
During the procedures, the potential for 3 errors occurred: 2 recommended surgical steps were omitted, and 1 communication loop was not closed. In each instance, the HUB appropriately displayed alerts, successfully prompting the surgical team to correct the errors.
Discussion
Surgical safety interventions often fail to account for the multidisciplinary nature of surgery. The HUB is designed to facilitate multidisciplinary team communication, recognize sentinel steps of high-consequence surgical procedures, and alert the operating room team to communication failures and procedural omissions. The feasibility test we present is encouraging and supports further intraoperative analysis of the HUB, particularly speech recognition, because standard Microsoft speech recognition software was used in this investigation and requires upgrade for a marketed system. Although false-step recognition did not occur in this investigation, future speech recognition software may use a command to prompt the system to distinguish commands directed toward the HUB from commands uttered in conversational speech. Furthermore, should an intraoperative complication occur, the HUB user can request a preloaded surgical checklist to assist with correcting the complication. This does not interfere with the procedure algorithm, although a pause function may be introduced.
Although we tested the HUB in cardiac surgery, HUB algorithms can be developed and applied across all surgical specialties. Unique algorithms can also be tailored for complex procedures involving multiple surgical teams, where communication is critical and susceptible to error. Each team member may check in and check out of the procedure at any time, provided their profile is uploaded to the system preoperatively. Although no final product cost can be estimated at this time, use of the HUB across multiple surgical specialties may reduce the additional cost per case.
Ultimately, surgical safety interventions endeavor to reduce morbidity and mortality. The logical next step is to apply the HUB to a larger series of cardiac surgical procedures to determine whether the HUB achieves this goal.
Footnotes
Author Contributions: Drs Tarola and Zenati had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Tarola, Haime, Leissner, Zenati.
Acquisition, analysis, or interpretation of data: All Authors.
Drafting of the manuscript: Tarola, Haime, Gabany, Zenati.
Critical revision of the manuscript for important intellectual content: Quin, Haime, Taylor, Leissner, Zenati.
Statistical analysis: Tarola.
Obtaining funding: Zenati.
Administrative, technical, or material support: Haime, Gabany, Taylor, Leissner, Zenati.
Study supervision: Quin, Gabany, Zenati.
Conflict of Interest Disclosures: Dr Zenati is the inventor of the original intellectual property, the HUB System, a communication management system that is licensed by Harvard University to Surgical Safety Solutions LLC. Dr Zenati additionally owns founder’s shares. No other disclosures are reported.
Additional Contributions: We thank Annette Phillips, RN, Veterans Affairs Boston Healthcare System, West Roxbury, Massachusetts, for her clerical assistance and Michael Grumbine of 3si Surgical Safety Solutions (http://www.3sisystems.com) for technical assistance in HUB operations. Neither party received financial compensation for their efforts.
References
- 1.Wahr JA, Prager RL, Abernathy JH, III, et al. American Heart Association Council on Cardiovascular Surgery and Anesthesia, Council on Cardiovascular and Stroke Nursing, and Council on Quality of Care and Outcomes Research. Patient safety in the cardiac operating room: human factors and teamwork: a scientific statement from the American Heart Association. Circulation. 2013;128(10):1139–1169. doi: 10.1161/CIR.0b013e3182a38efa. [DOI] [PubMed] [Google Scholar]
- 2.Gurses AP, Kim G, Martinez EA, et al. Identifying and categorising patient safety hazards in cardiovascular operating rooms using an interdisciplinary approach: a multisite study. BMJ Qual Saf. 2012;21(10):810–818. doi: 10.1136/bmjqs-2011-000625. [DOI] [PubMed] [Google Scholar]
- 3.Wiegmann DA, ElBardissi AW, Dearani JA, Daly RC, Sundt TM., III Disruptions in surgical flow and their relationship to surgical errors: an exploratory investigation. Surgery. 2007;142(5):658–665. doi: 10.1016/j.surg.2007.07.034. [DOI] [PubMed] [Google Scholar]
- 4.Allers JC, Hussein AA, Ahmad N, et al. Evaluation and impact of workflow interruptions during robot-assisted surgery. Urology. 2016;92:33–37. doi: 10.1016/j.urology.2016.02.040. [DOI] [PubMed] [Google Scholar]
- 5.Conboy HM, Maron JK, Christov SC, et al. Process modeling of aortic cannulation in cardiac surgery: towards a smart checklist to mitigate the risk of stroke. Presented at: MICCAI International Conference on Medical Image Computing and Computer-Assisted Intervention; Boston, MA. September 14, 2014. [Google Scholar]