Abstract
Objectives:
To investigate the degree of knowledge chiropractic fourth year interns and post-graduate chiropractic residents have in regard to concussion diagnosis and management.
Methods:
A survey modified from a study conducted by Boggild and Tator (2012), was administered to fourth year chiropractic interns and post-graduate residents via SurveyMonkey.com.
Results:
Chiropractic fourth year interns and postgraduate chiropractic specialty college residents scored 5.2 and 5.25 out of 9 respectively, which compares well with Bogglid and Tator’s reports on medical students and residents. Several knowledge gaps were identified in the sample population.
Conclusion:
The results from this survey show that the concussion knowledge among Canadian fourth year chiropractic interns and specialty college residents compares favorably with the knowledge of fourth year medical students and residents in diagnosing and managing concussions. Chiropractors appear to possess the skills and knowledge to diagnose and manage concussion equal to their medical counterparts. However, knowledge gaps regarding concussion diagnosis and management were found among chiropractic students and residents.
Keywords: concussion, chiropractic, student, resident, knowledge
Abstract
Objectifs :
Enquêter sur le niveau de connaissances en diagnostic et gestion de commotion cérébrale des stagiaires de quatrième année et des résidents de troisième cycle en chiropratique.
Méthodologie :
Une enquête modifiée d’une étude menée par Boggild et Tater (2012) a été réalisée auprès des stagiaires de quatrième année et des résidents de troisième cycle en chiropratique via SurveyMonkey.com.
Résultats :
Les stagiaires de quatrième année et les résidents du troisième cycle des collèges de spécialités en chiropratique ont obtenu respectivement 5,2 et 5,25 sur 9, ce qui se compare aux rapports de Bogglid et Tator sur les étudiants et les résidents en médecine. Plusieurs lacunes ont été identifiées dans les connaissances de la population étudiée.
Conclusion :
Les résultats de cette enquête montrent que les connaissances en diagnostic et gestion de commotion cérébrale des stagiaires de quatrième année et des résidents du troisième cycle des collèges de spécialités en chiropratique sont comparables à celles des étudiants de quatrième année et des résidents en médecine. Les chiropraticiens semblent posséder les compétences et les connaissances nécessaires pour diagnostiquer et gérer la commotion cérébrale aussi bien que leurs homologues en médecine. Toutefois, des écarts de connaissances sur le diagnostic et la gestion de commotion cérébrale ont été constatés parmi les étudiants et les résidents en chiropratique.
Keywords: commotion cérébrale, chiropratique, étudiant, résident, connaissance
Introduction
Concussions represent one of the most common types of brain injuries in sport.1 While often sustained in motor vehicle accidents, sports injuries or falls, concussions can occur at any age.1 According to discussions held at the 4th International Consensus Conference on Concussion in Sport in Zurich1, concussion is described as “a brain injury and is defined as a complex of pathological process affecting the brain, induced by biomechanical forces.” 1 The majority of concussions (80–90%) tend to resolve themselves typically in 7–10 days.1 Nevertheless, it remains pertinent for patients to be diagnosed with a concussion if present, and evaluated to determine when it is safe for them to return to certain activities.
Concussion management has evolved through the decades as research is consistently guiding mangement.1–6 Those changes include moving from the American Academy of Neurology’s 1997 practice parameters, to the 2002 Vienna guidelines, to the 2008 Zurich guidelines, and, most recently, to the 2012 Zurich guidelines, which are currently accepted as the best protocol for practitioners to take when managing a patient with a concussion1–3. Broshek et al.4 report that 56% of members of the Child Neurology Society still use the American Academy of Neurology’s 1997 parameters, whereas only 8.2% used the Zurich guidelines. Lebrun et al.5 report slightly higher figures, with 9.4% of those US physicians involved in their study using the Zurich guidelines.
Tools for managing a concussion have also changed over the years. Guskiewicz et al.6 have suggested revision to the Sport Concussion Assessment Tool 2 (SCAT2) and have introduced the SCAT3, which may provide a more complete clinical profile and comprehensive examination for the athlete with a suspected concussion. McCrory et al.1 recommend that the initial assessment of an injured athlete should involve the use of the SCAT3. Most of the examinations done at the hospital (if an athlete is taken to the emergency room) are already included in the SCAT3 assessment.
The current guidelines and tools that are available for practitioners, such as those found in the SCAT3, are not always accepted and/or implemented in the practitioner’s diagnosis and management of concussions. Lebrun et al.5 surveyed and compared American versus Canadian practicing family physicians and noted many similarities in regards to sport-related concussions. However, one notable difference involved a higher number of US physicians using outdated concussion grading scales with less than 10% of US physicians using the recent Zurich guidelines. In light of this, physicians from both countries indicated their desire for additional education regarding concussions.
Based on evidence founded by Burke et al.7, it seems as though undergraduate medical students receive a limited knowledge base regarding the diagnosis and management of patients with concussions. Of the 14 Canadian medical schools that responded to a survey (of the 17 contacted), four provided concussion-specific education, six schools offered head injury education that incorporated a concussion component, and four schools reported that there was no concussion education in their curriculum. In contrast, as shown in Boggild and Tator’s paper10, fourth year medical students and neurology residents seem to have a more comprehensive knowledge base with regards to diagnosing and managing concussion, contradicting other research.
Chiropractors receive some theoretical and practical training in concussion management with an aim to safely and competently perform physical examination, diagnosis and treatment of these conditions.8,9 The chiropractic undergraduate program in Canada provides principles of concussion management throughout all four years of the curriculum.8,9 The Graduate Studies Programs provide more chance for the chiropractic residents to learn about concussion and even manage concussions during their placements.8,9
There has been research conducted to examine the concussion knowledge of medical students and residents as well as an examination of the curriculums of various medical schools across Canada.10 In a study conducted by Boggild and Tator10 at the University of Toronto, the knowledge, awareness and attitude towards concussion management among medical students and neurology and neurosurgery residents were examined via a “25 item survey through literature review, expert review and pilot testing to assess medical trainee’s knowledge of concussion, sources of information, learning needs and educational preferences on this topic”. The survey was administered to these medical trainees via SurveyMonkey.com. Section Two of the survey consisted of nine concussion-related questions testing the students’ understanding of the condition. The fourth year medical students scored an average of 4.1 correct answers (out of nine) and the residents scored an average of 5.8 (out of nine).
Crawford11 claims that after emergency physicians, chiropractors may be the health care professionals that see the next highest amount of concussion patients. In fact, Johnson et al.12 suggest that chiropractors may actually be the first to interact with an athlete who has sustained a concussion, often because patients are seeking treatment to alleviate symptoms, commonly treated by chiropractors, associated with post-concussion syndrome.
Past studies have examined the knowledge of concussions among medical students and residents in Canada.5,7,10 However, knowledge of concussions among chiropractic students, and chiropractic residents have not yet been investigated. The purpose of this study is to assess the current knowledge in diagnosis and management of concussion among Canadian chiropractic fourth year interns and post-graduate residents.
Methods
Upon permission from the authors, a similar survey was distributed via email (linked to SurveyMonkey.com) amongst the fourth year interns and chiropractic residents at the Canadian Memorial Chiropractic College (CMCC) in the summer of 2014. A complete class list was obtained from the chiropractic college Registrar Office to avoid missing anyone within the sample. Compliance was assessed through the survey software, which immediately determined whether the participants had completed, not completed, or withdrawn themselves from the survey. The survey was composed of objectively directed questions with slight modifications from the original survey from Boggild and Tator10 to make questions more appropriately addressed to chiropractic students. (Please refer to appendix B for the modified survey) These modifications took place in Part 1 and Part 3 of the survey and will be discussed later. The study received ethics approval from a Research Ethics Board.
The demographic data collected in Section One included the following subjects: program and place of study, gender, participation in sports and recreation, and a personal history of concussion. The original survey was modified in Part 1 and Part 3 so that questions could be properly addressed to chiropractic students instead of medical students. In question 2, instead of asking which medical school students attended, students were asked “Which chiropractic college are you currently attending? If you have currently completed your chiropractic undergraduate degree, which college did you receive this at?”. Question 18 was replaced by “In your chiropractic education, how did you learn about concussions?”. The survey used in this study did not include any clerkship rotation options as this does not apply to chiropractic students. Question 23 was replaced by “On a scale of 1–10 (with 1 being ‘not at all’ and 10 being ‘very much’) are concussions something you want to learn more about as part of your chiropractic curriculum?”. All other questions were the same as those in the original survey by Boggild and Tator.10
The data involving the knowledge of concussion definitions and management considerations collected from Section Two involved nine questions to assess three areas of interest. The first three of nine questions assessed the respondent’s ability to correctly identify the definition of a concussion and to recognize that loss of consciousness is not a required symptom of concussion. The next three questions tested the respondent’s ability to correctly identify the symptoms of a concussion, the number of symptoms required to make a diagnosis of a concussion, and the mechanism of injury. The last three questions tested the respondent’s ability to recognize the steps of management, red flags that may indicate an increased risk of post-concussive sequelae, and the potential long-term sequelae of concussion. After evaluation of this section, a score from 0 to 9 was recorded for each participant. For further details, please refer to Appendices A and B.
Similar to the Boggild and Tator10 study, each question of Section Two in this survey was marked as either correct or incorrect. A score of one point was given to a correct answer and no point was given to incorrect answers. No partial points were given. If a question required a respondent to “select all that apply”, all the correct options were permitted to be selected and none of the incorrect options would be given the one point.
Descriptive statistics were used to summarize the sample and any of the variables described in the outcome measurement. When appropriate, Chi Square tests, T tests and regression analysis tests were used to assess the similarities and differences between chiropractic students (interns and residents) and medical students (fourth year students and residents) in respect to their knowledge of concussions and concussion-related clinical experience.13–15 Data that was extracted from the results of the Boggild and Tator study were compared to data generated from this study, when appropriate.10 Graphpad.com was used for statistical analysis. A two-tailed T test was used to compare the concussion knowledge scores in Part Two between chiropractic interns and fourth year medical students.13 Another two-tailed T test was used to compare scores between chiropractic residents and medical residents.13 A Yates corrected Chi Square test was used to compare lifestyle, educational background, and responses to individual questions in Part Two between chiropractic residents and interns and between chiropractic students and medical students.14 A linear regression was used to compare the chiropractic students’ self ranked knowledge about concussions and compare it with their actual concussion knowledge score in Part Two.15 All P Values less than 0.01 were considered to be statistically significant in this study.
The sample size was limited to the number of fourth year chiropractic interns and residents who completed the survey through SurveyMonkey.com.
Results
A total of 219 surveys were emailed to fourth year chiropractic interns and chiropractic residents in the chiropractic clinical sciences, chiropractic sports sciences and chiropractic diagnostic imaging programs. Thirty-six surveys were returned from fourth year chiropractic interns (19.4% response rate), two from the chiropractic clinical sciences program, six from chiropractic sports sciences program and none were returned from diagnostic imaging program (24.2% response rate for all residents). The number of surveys returned from fourth year chiropractic interns that were females and males were comparable. As for chiropractic residents, all respondents were male from the sports sciences program, and all respondents were female from the clinical sciences program (See Table 1). Three residents completed their undergraduate chiropractic education at a college outside of Canada (37.5%). The response rate of chiropractic interns (19.4%) was comparable to the response rate of medical students (23.0%), while the response rate of chiropractic residents (24.2%) was comparable to the response rate of medical residents (31.3%). However our sample size was much smaller than that of Boggild and Tator.10
Table 1.
Proportion of male and female interns and residents.
| Study Population | Sample Population | Response Rate | |
|---|---|---|---|
| Chiropractic Interns | 186 | 36 | 19.4% |
| Female | 97 | 19 | 19.6% |
| Male | 89 | 17 | 19.1% |
| All Chiropractic Residents | 33 | 8 | 24.2% |
| Female | 14 | 2 | 14.3% |
| Male | 19 | 6 | 31.6% |
| Sports Science Residents | 26 | 6 | 23% |
| Female | 9 | 0 | 0% |
| Male | 17 | 6 | 35.3% |
| Clinical Science Residents | 5 | 2 | 40% |
| Female | 3 | 2 | 67% |
| Male | 2 | 0 | 0% |
| Total Chiropractic Students and Residents | 219 | 44 | 20.1% |
| Female | 111 | 21 | 18.9% |
| Male | 108 | 23 | 21.3% |
Fourth year chiropractic interns scored an average of 5.2 out of 9 (standard deviation [SD] = 1.17, 95% confidence interval (CI) = 4.8–5.6) in Section 2: Knowledge Questions About Concussions. Chiropractic residents scored an average of 5.25 out of 9 (SD = 0.89, 95% CI = 4.6–5.9). There were no significant factors in the knowledge score of the fourth year chiropractic interns and chiropractic residents in regards to a personal history of concussion, gender or time spent participating in sports and recreation (Yates corrected Chi Square, p>0.01). In the study conducted by Boggild & Tator10, fourth year medical students received a mean score of 4.1 out of 9 in Section Two. Medical residents answered correctly significantly more of the questions on the survey than the fourth year medical students with a mean score of 5.8 out of 9 (mean = 5.8 vs. 4.1; t = 4.65; p<0.01).
A two tailed t-test comparing study groups revealed that fourth year chiropractic interns answered correctly significantly more of the questions on the survey than the graduating fourth year medical students (mean = 5.2 vs. 4.1; t=3.94; p<0.01). Chiropractic residents showed no statistically significant difference in their scores on the survey when compared to medical residents (mean = 5.25 vs. 5.80; t = 0.87; p>0.01) or to fourth year chiropractic interns (mean = 5.25 vs 5.2; t= 0.06; p>0.01).
Fifty percent of all fourth year chiropractic interns and chiropractic residents in this study did not recognize chronic traumatic encephalopathy as a possible outcome of repeated concussions, and 57% did not recognize second impact syndrome, but all chiropractic interns and residents were able to recognize that the mechanism of concussion involves a whiplash effect to the brain caused by an impact to any part of the body. Only 2.7% of fourth year chiropractic interns (1 out of 36) thought that a concussion was not a brain injury as there is no abnormality seen on structural neuroimaging. None of the chiropractic respondents answered that a period of unconsciousness was necessary for the diagnosis of a concussion. Seventy-five percent of chiropractic interns were able to correctly answer that less than one-third of all concussions involve loss of consciousness. Thirty-six percent of fourth year chiropractic interns (n=16) did not believe that every concussed individual should see a physician.
Sixty-four percent of the fourth year chiropractic interns in this study were able to correctly answer that only one symptom is required to diagnose a concussion. When the same question was asked of the chiropractic residents in this study, 50% of them (n=4) were able to correctly answer this.
Chiropractic residents were significantly more likely to have seen a concussion patient when compared to fourth year chiropractic interns (Yates corrected chi square, p<0.01). There was no statistical correlation between chiropractic trainees (both interns and residents) who had seen an acute or chronic concussion patient in the past and the number of correct concussion knowledge questions in Section Two of the survey (two tailed t-test, mean = 5.47 [have seen] vs 5.11 [have not seen], p = 0.33).
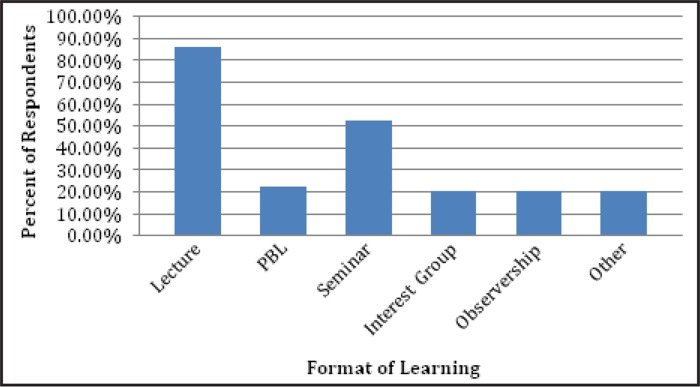
The majority of chiropractic trainees (both interns and residents) reported that they had learned about concussion in their undergraduate chiropractic education through lecture (86%) and/or seminar (52%) (see Figure 1). When chiropractic trainees were asked what resource they were most likely to use to retrieve information about concussions, 48% answered ”Pubmed” would be their preferred source, 32% answered ”Google”, 11% answered “Other”, 5% answered an “Agency Website”, 2% answered “Think-First.ca”, and 2% answered “Up-to-Date”. In terms of learning preferences, the majority (67%) responded that a seminar or workshop would be their preferred option. The second-highest learning preference option was lecture (28%), followed by informational email (2%).
Figure 1.
How chiropractic trainees learned about concussions during their undergraduate chiropractic education. PBL = Problem Based Learning.
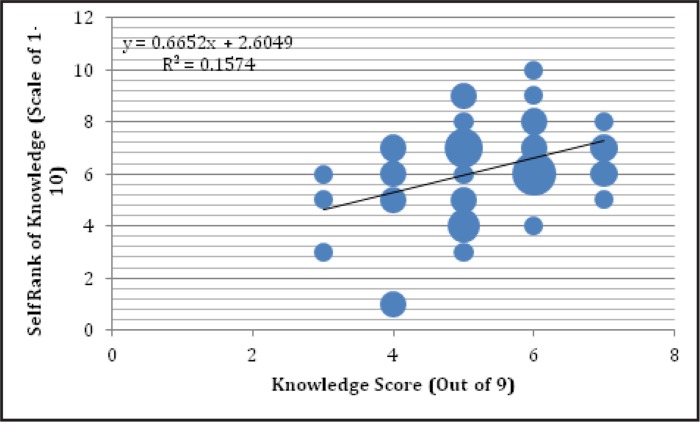
One of the questions in the survey required chiropractic trainees to self-rank their concussion knowledge on a scale of 1 to 10. This data was compared to their actual concussion knowledge scores using a bubble graph with the corresponding trend line (see Figure 2). Those that self-ranked their knowledge about concussions as poor were slightly more likely to have a lower concussion knowledge score in Part Two of the survey (linear regression, r = 0.40).
Figure 2.
Relationship between chiropractic trainees’ self-ranking of knowledge about concussions and their assessment. The area of points is proportional to the number of respondents when plotted to the same coordinate.
The chiropractic trainees in this study were also asked (in the form of an open-ended question) what challenges they feel chiropractors in general face when diagnosing and managing a concussion. The responses to these questions were organized according to theme (see Table 2).
Table 2.
Challenges faced by medical doctors and chiropractors when diagnosing and managing a concussion as reported by chiropractic interns and residents.
| Theme | Representative Quote |
|---|---|
| Appropriate plan of management | “The uncertainty surrounding the management of concussions. Treatment is often subjective, also there are so many conflicting views of the best way the manage concussions.” “The variety of ways they can present is vast, and not all concussions resolve in the same way or time frame.” |
| Continuous evolution of guidelines and protocol | “There is an abundance of information currently out in the field and it is constantly evolving and difficult to keep up with. For example: one of your questions asked about long-term consequences (including Parkinsons, CTE and dementia). Some of the recent systematic reviews are showing there is no conclusive relation between concussion and those disorders however most studies should be done to confirm this and the media plays on the few cases. Having an abundance of information can be helpful but also very confusing. Guiding our education by utilizing the best level of evidence is recommended.” “Being aware of changes in the guidelines for diagnosing and managing concussion” |
| Determining safe return to play | “Not knowing the proper protocol/return to play.” |
| Lack of knowledge about patient’s baseline testing results prior to concussion | “Baseline testing is often not done for athletes so that the SCAT become invalid.” |
| Lack of imaging findings | “Lack of physical findings on CT or MRI” |
| Subtleties of the clinical diagnosis | “The complexity of individuality. No two cases are the same: the signs and symptoms are different, the pathology, ability to heal, response to treatment.” “The main one is diagnosing one and the degree of severity.” “The consequences of missing a more severe diagnosis (e.g. intracranial bleed).” “The variability of signs and symptoms from person to person” “Separating confounding variables from the underlying cause.” |
Discussion
The objective of this study was to examine CMCC’s fourth year chiropractic interns’ and chiropractic residents’ knowledge of concussion diagnosis and management. Chiropractic fourth year interns correctly answered significantly more of the questions on the survey than the graduating fourth year medical students (mean = 5.20 vs. 4.10; t = 3.94; p<0.01). However, since our study was conducted four years after Boggild and Tator’s10, dissemination of knowledge during the intervening time may account for at least some of this difference. Chiropractic residents showed no statistically significant difference in their scores on the survey when compared to medical residents (mean = 5.25 vs. 5.80; t = 0.87; p>0.01) or to fourth year chiropractic interns (mean = 5.25 vs 5.20; t = 0.06; p>0.01). These results suggest that chiropractic students have equivalent knowledge to their medical peers, though none may have enough at graduation to engage in optimal concussion management. Concussion patients may not be the biggest population in a physician’s practice, but if chiropractors manage (or co-manage) concussed patients, it may reduce the stress on busy physicians, as 95% of family physicians see, assess, and treat concussions5.
Boggild and Tator10 reported that medical students and residents did not recognize Chronic Traumatic Encephalopathy (48%) or Second Impact Syndrome (57%) as possible outcomes of repetitive concussive injury. Chiropractic interns and residents had similar results, with half of them not recognizing chronic traumatic encephalopathy (50%) or second impact syndrome (57%) as possible consequences for individuals sustaining recurrent concussions. It is highly pertinent that a clinician be aware of these when working with concussion patients. Second Impact Syndrome (SIS) involves a second concussion occurring before the individual has recovered from their first concussion. Numerous studies have shown that even after the initial post-concussion symptoms disappear, the athlete is still extremely vulnerable, and the likelihood of re-activating symptoms hours or even days later with possible accompanying neurological deficit is highly likely.16 Marshall16 explains that it is not only return to play that can cause further damage, but even premature return to strenuous exercise can cause a prolonging of symptoms and possibly lead to a worsened outcome. Even more serious than this are the consequences of chronic concussions, which include: Post-Concussion Syndrome (PCS) and Chronic Traumatic Encephalopathy (CTE).10 It is therefore important to get an accurate diagnosis for a concussion as soon as possible.
Chiropractic interns and medical students equally identified that less than one-third of concussions involve loss of consciousness. When examining a patient, red flags such as loss of consciousness make diagnoses stand out more, but those red flags aren’t always present.10 Practitioners need to be mindful of concussions as a possible diagnosis in situations where trauma is sustained and there is no loss of consciousness.
Chiropractic interns and medical students correctly identified that only one symptom is required to diagnose a concussion or to examine a patient for a possible concussion, as only one may be present even if they do have a concussion.7
All of the chiropractic residents and interns were able to correctly recognize that the mechanism of concussion involved a whiplash effect to the brain caused by an impact to any part of the body. In comparison, 33% of fourth year medical students and 24% of neurology and neurosurgery residents believed that a direct blow to the head was necessary to sustain a concussion.10 A very small percentage of chiropractic interns (2.7%) incorrectly answered that a concussion was not a brain injury due to the absence of abnormalities seen on structural neuroimaging, whereas 1.9% of fourth year medical students incorrectly answered the same way.10 All chiropractic respondents correctly answered that a period of unconsciousness was not necessary for the diagnosis of a concussion, while 6% of fourth year medical students incorrectly answered this question.10
Boggild and Tator10 stated that 24% of respondents did not select “every concussed individual should see a physician”, whereas 36% of fourth year chiropractic interns (n=16) did not believe that every concussed individual should see a physician. It is important to emphasize that, on the survey, when asking this question to a chiropractic intern or resident, it would make sense that their first inclination would be not to select this option since chiropractors are not physicians by definition, nor do they believe that physicians are the only ones capable of managing such a condition.8 However, selecting this option was a correct answer according to Boggild and Tator10. This may act as a source of bias within the survey, which was developed for medical students. This was an oversight by the authors not to modify this question prior to administration of the survey to chiropractic population.
Question 25 in Part 3 of the survey questioned chiropractic residents and interns about what they believed the challenges faced by medical doctors and chiropractors were when diagnosing and managing a concussion. The most frequent responses to this question involved subtleties of the clinical diagnosis, and determining the appropriate plan of management for the patient. It seems that chiropractic interns and residents believe that most challenges arise due to the complexity and uniqueness of concussion cases, inconsistency in protocols used in concussion management across the board, and continuously evolving research that clinicians are not always up-to-date with.
It is important to consider the time at which this question was answered by medical students compared to chiropractic students as literature and guidelines have been subject to change over the three year since this survey had first been completed (medical students in 2011 vs chiropractic students in 2014). This in itself could mean that the participants in this study could have had greater exposure to information relating to the diagnosis and management of concussion when compared to the participants in the original study conducted by Boggild and Tator10. As such, comparing the knowledge of current chiropractic students and residents to that of medical students and residents of three years ago is not justified. In the future, such comparative studies should incorporate the chiropractic and medical students at the same time in order for a fair comparison of knowledge.
Limitations
This study has a number of limitations. One of the main limiting factors of this study was that there was limited access to the raw data from the survey conducted by Boggild and Tator10. This made it difficult to make a true comparison of results.
Another limitation considered relevant in translating these results into professional practice is the format in which knowledge was evaluated. A multiple choice answer format was used, which may be somewhat different from how a chiropractor or a medical doctor would apply their knowledge in a real life setting where decisions must be made without “recognizing” the correct answer from a list of options. Yet another limitation is that 44 Canadian chiropractic students cannot be generalized to the population of students attending all other chiropractic colleges in the world. The cumulative response rate of 21.8% is a major limitation of generalizing this study’s results to all chiropractic residents and interns. A small sample size may be another source of limit bias in this study.
Boggild and Tator10 were the first to analyze concussion knowledge among medical students and residents in Canada. However, our study is the first study which analyzes the knowledge of concussion within the chiropractic interns and residents. Evidently, the research is still in its infancy. It is imperative that more research is done to guage the knowledge chiropractic students have regarding the management of concussion. It would also be interesting to look into the knowledge of practicing chiropractors (and of other health care professionals who have not been included in this study who also manage concussion).
The survey scores of chiropractic interns and residents (5.20 and 5.25, respectively) indicate some knowledge gaps. In order to rectify this situation, we suggest incorporating more focused lecture material regarding concussion as well as hands on group learning sessions where the SCAT 3 and return to play protocols can be reviewed. This was determined with the help of question 24 of our survey, which asked, “What is your preferred format for physician learning material?” The participants of this study reported their preferred learning format was through seminar or workshop, with lecture being the second most popular choice.
Further research should examine the knowledge of concussion management among chiropractors with special interest in concussion for example among sports chiropractors.
Conclusion
The results from this survey show that knowledge about concussion among fourth year chiropractic interns and residents is comparable to the knowledge of fourth year medical students and residents in diagnosing and managing concussions. As such, this may suggest that chiropractors maybe able to play a role in diagnosis and management of concussion alongside their medical counterparts. However, knowledge gaps were found in concussion diagnosis and management among chiropractic students and residents. Hence we recommend additional lecture and workshop hours on concussion material to be added to the chiropractic undergraduate curriculum to fill knowledge gaps identified.
Appendix A. Table with Summary of Results.
| Test Question Comparison | Chiropractic Interns | Chiropractic Residents | Medical Students | Medical Residents | Statistically significant score between chiropractic Interns and 4th year Medical Students | Statistically significant score between Chiropractic Residents and Medical Residents? | Statistically significant score between Chiropractic Interns and Residents? |
| Mean Overall Test Score | 5.20 | 5.25 | 4.10 | 5.80 | Yes, t=3.94 p<0.01 |
No, t=0.87 p>0.01 |
No, t=0.06 p>0.01 |
| Which of the following are TRUE regarding concussion and loss of consciousness (LOC)? | 75% correctly identified that less than 1/3 of all concussions involve LOC. 100% correctly answered that a period of unconsciousness is not necessary for the diagnosis of concussion |
100% correctly answered that a period of unconsciousness is not necessary for the diagnosis of concussion |
66% correctly identified that less than 1/3 of all concussions involve LOC. 6% incorrectly answered that a period of consciousness is necessary for the diagnosis of concussion |
No, Yates corrected chi square p>0.01 No, Yates corrected chi square p>0.01 |
|||
| Which of the following is TRUE regarding the mechanism of concussion? | 100% correctly identified that a whiplash effect to the brain caused by an impact to any part of the body may cause a concussion | 33% incorrectly identified that a direct blow to the head was necessary to sustain a concussion | 24% incorrectly identified the same answer as medical students | Yes, Yates corrected chi square p<0.01 | No, Yates corrected chi square p>0.01 | ||
| Is a concussion a brain injury? | 2% incorrectly answered that a concussion was not a brain injury due to the absence of abnormalities on structural neuroimaging | 6% incorrectly answered that a concussion was not a brain injury due to the absence of abnormalities on structural neuroimaging | No, Yates corrected chi square p>0.01 | No, Yates corrected chi square p>0.01 | |||
| What are the long term consequences of repetitive concussive injury? | 50% of both chiropractic interns and residents did not recognize chronic traumatic encephalopathy, nor did 57% of them recognize that second impact syndrome are consequences of recurrent concussions | 48% of both medical students and residents did not recognize chronic traumatic encephalopathy, nor did 57% of them recognize that second impact syndrome are consequences of recurrent concussions | No, Yates corrected chi square p>0.01 | No, Yates corrected chi square p>0.01 | |||
| What is the appropriate management of concussion? | 42% incorrectly believed that not every concussed individual should see a physician | 24% incorrectly believed that not every concussed individual should see a physician | No, Yates corrected chi square p>0.01 | No, Yates corrected chi square p>0.01 | |||
Appendix B. Survey sent to chiropractic students in this study.
Part 1. ID questions and Sports and Recreation background
What is your gender?
Which chiropractic college are you currently attending? If you have currently completed your chiropractic undergraduate degree, which college did you receive this at?
What residency program and year are you in? (question only in survey to residents)
Have you done any of the following in the past 2 years? Mark all that apply. Thirty-one options of sports and activities given, including the option “other”
Last week, how many times did you participate in sports or physical activity? Options for 1 time to 7 times given
-
About how much time did you spend on each occasion?
Options: 1 to 15 minutes, 16 to 30 minutes, 31 to 60 minutes, More than one hour
-
In the past, have you ever suffered a concussion? You may have been “knocked out”, knocked unconscious, confused, or had your “bell rung”. You may have felt lightheaded, not known where you were, etc.
Options: Yes – once, Yes – 1–5 times, Yes – more than 5 times, No
If you answered yes to the previous question, how did your concussion(s) occur? Please select all that apply. Options: Work related, Motor Vehicle Crash, Sport or recreational activity, Fall, Other
Part 2. Knowledge questions about concussions (Answers that were considered correct are in italic)
- 9. What is the definition of concussion? Select the best answer.
- Loss of consciousness for <5 mins after an impact to the head
- A complex pathophysiological process affecting the brain, induced by traumatic biomechanical forces
- A structural brain injury caused by mild traumatic force that transiently decreases cerebral blood flow
- 10. Is a concussion a brain injury? Select the best answer.
- No, as there is no abnormality seen on standard structural neuroimaging
- No, as symptoms are only psychological in nature
- Yes, as there is a functional disturbance that cannot be seen on standard neuroimaging
- Yes, as there is structural abnormality seen on standard neuroimaging
- 11. Which one of the following is true?
- A period of unconsciousness is necessary for the diagnosis of a concussion
- Over 2/3 of all concussions involve loss of consciousness (LOC)
- 1/3 to 2/3 of all concussions involve loss of consciousness (LOC)
- Less than 1/3 of all concussions involve loss of consciousness (LOC)
-
12. Which of the following is a sign or symptom of a concussion? Select all that apply.
Options:Headache, Hemiparesis, Dizziness, Confusion, Fixed dilated pupil, Nausea and/or Vomiting, Vertigo, Amnesia, Tinnitus, Emotional or personality changes, Papilledema, Intention tremor, Fatigue, Temporary loss of consciousness, Prolonged coma
-
13. How many symptoms of a concussion are required to diagnose a concussion?
Options:One or more symptoms, three or more symptoms, five or more symptoms
- 14. Which of the following is true regarding the mechanism of concussion?
- Direct physical contact to the head is necessary to sustain a concussion
- Localized damage to the brainstem is the cause a concussion
- Localized damage to the prefrontal cortex is the cause of a concussion
- Localized damage to the hippocampus is the cause of a concussion
- A whiplash effect to the brain caused by an impact to any part of the body may cause a concussion
- 15. What is the appropriate management of concussion? Select all that apply
- Every concussed individual should see a physician
- A concussed player can return to play in the same game or practice if examined by a physician
- A stepwise increase in exercise and activity if symptomatic
- Physical rest is always recommended after a concussion
- Mental rest is always recommended after a concussion
- Signs and symptoms should be monitored for increasing severity
- Full neurological exam at initial assessment is recommended
- The standard mini mental status exam at initial assessment as an adequate cognitive test for concussion
- MRI of the brain is mandatory
- CT of the brain is mandatory
- 16. What are some “red flags” that may predict the potential for more prolonged symptoms and may influence your investigation and management of concussion? Select all that apply:
- Nosebleed
- Prolonged loss of consciousness
- Number and duration of symptoms
- Age
- Repeated concussions occurring with progressively less impact force
- Slower recovery after each successive concussion
- Repeated concussions over time
- Concussions close together in time
- Being hit on the left side of the head
- 17. What are the long term consequences of repetitive concussive injury? Select all that apply.
- Dementia
- Depression
- Headaches
- Increased risk of hemorrhagic stroke
- Death or disability with second concussion before recovery from a first concussion
- Increased risk of schizophrenia
- Prolonged fatigue
- Impairment of concentration and memory
- Parkinsonism
- Chronic traumatic encephalopathy
Part 3. Learning needs about concussions
-
18. In your undergraduate chiropractic education, how did you learn about concussions? Select all that apply.
Options: Lecture, PBL (problem based learning), Seminar, Interest Group, Shadowing/Observership, Other, Never, I can’t remember
-
19. In your residency to date, how did you learn about concussions? Select all that apply.
Options: Clinical experience, Self-study, Lecture, Never, I can’t remember, Other
- 20. To date, have you seen a patient with:
- – concussion in the acute phase? Yes, No, I don’t know (select one)
- – post-concussive syndrome? Yes, No, I don’t know (select one)
- 21. How would you self-rank your knowledge about concussions?
Inadequate Completely adequate 1 2 3 4 5 6 7 8 9 10 -
22. What resource would you most likely use to find information about concussions?
Options: Google, Wikipedia, Up-to-date, Textbook, Pubmed, an agency website, Thinkfirst.ca, other
- 23. Are concussions something you want to learn more about as part of your medical curriculum?
Not at all Very much 1 2 3 4 5 6 7 8 9 10 -
24. What is your preferred format for physician learning material?
Options: Pamphlet, letter, seminar or workshop, lecture, informational email
25. What challenges, if any, do you think physicians face when diagnosing and managing a concussion
References
- 1.McCrory P, Meeuwisse W, Aubry M, et al. Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. Br J Sports Med. 2012;47:250–258. doi: 10.1136/bjsports-2013-092313. [DOI] [PubMed] [Google Scholar]
- 2.Report of the Quality Standards Subcommittee Practice parameter: the management of concussion in sports (summary statement) Neurology. 1997;48(3):581–585. doi: 10.1212/wnl.48.3.581. [DOI] [PubMed] [Google Scholar]
- 3.Aubry M, Cantu R, Dvorak J, et al. Concussion in Sport Group Summary and agreement statement of the First International Conference on Concussion in Sport, Vienna 2001: recommendations for the improvement of safety and health of athletes who may suffer concussive injuries. Br J Sports Med. 2002;36(1):6–10. doi: 10.1136/bjsm.36.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Broshek D, Samples H, Beard J, Goodkin H. Current practices of the child neurologist in managing sports concussion. J Child Neurol. 2012;29(1):17–22. doi: 10.1177/0883073812464525. [DOI] [PubMed] [Google Scholar]
- 5.Lebrun C, Mrazik M, Prasad A, et al. Sport concussion knowledge base, clinical practices and needs for continuing medical education: a survey of family physicians and cross-border comparison. Br J Sports Med. 2012;47:54–59. doi: 10.1136/bjsports-2012-091480. [DOI] [PubMed] [Google Scholar]
- 6.Guskiewicz K, Register-Mihalik J, McCrory P, et al. Evidence-based approach to revising the SCAT2: introducing the SCAT3. Br J Sports Med. 2013;47:289–293. doi: 10.1136/bjsports-2013-092225. [DOI] [PubMed] [Google Scholar]
- 7.Burke M, Chundamala J, Tator C. Deficiencies in concussion education in canadian medical schools. Can J Neurolog Sci. 2012;39:763–766. doi: 10.1017/s0317167100015584. [DOI] [PubMed] [Google Scholar]
- 8.Program Overview. The Royal College of Chiropractic Sports Sciences (Canada) 2014. Available from: http://www.rccssc.ca/index.php/overview.
- 9.Canadian Memorial Chiropractic College Academic Calendar 2015–2016. Toronto: Canadian Memorial Chiropractic College; 2015. pp. 54–76.pp. 112–121. [Google Scholar]
- 10.Boggild M, Tator C. Concussion knowledge among medical students and neurology/neurosurgery residents. Can J Neurolog Sci. 2012;39:361–368. doi: 10.1017/s0317167100013524. [DOI] [PubMed] [Google Scholar]
- 11.Crawford M. Concussions and chiropractic. J Am Chiropr Assoc. 2011;7(9):33. [Google Scholar]
- 12.Johnson C, Green B, Nelson R, Moreau B, Nabhan D. Chiropractic and concussion in sport: a narrative review of the literature. J Chiropr Med. 2013;12:216–229. doi: 10.1016/j.jcm.2013.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stoltzfus JC. Student’s t-test for independent samples. Int J Acad Med. 2015;1:27–28. [Google Scholar]
- 14.Yates F. Contingency table involving small numbers and the χ2 test. Suppl J Royal Stat Soc. 1934;1(2):217–235. [Google Scholar]
- 15.Schneider A, Hommel G, Blettner M. Linear Regression Analysis: Part 14 of a series on evaluation of scientific publications. Deutsches Ärzteblatt Intl. 2010;107(44):776–782. doi: 10.3238/arztebl.2010.0776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marshall C. Sports-related concussion: a narrative review of the literature. J Can Chiropr Assoc. 2012;56(4):299–310. [PMC free article] [PubMed] [Google Scholar]