Abstract
Background:
Despite more than two decades since recognition of suicides by farmers in India, systematic studies comparing various risk factors are lacking. This is major hurdle for the formulation of strategies for farmers' suicide prevention.
Objective:
To identify socioeconomic and psychological risk factors and their relative contribution in suicides by farmers.
Materials and Methods:
A matched case–control psychological autopsy was done on 98 farmers' suicide victims and 98 controls in Central India.
Results:
Economic problems, psychiatric illness, and stressful life events were found to be important contributors to farmers' suicides. Important economic risk factors were procurement of debt, especially from multiple sources and for nonagricultural reasons and leasing out farms. Psychiatric illness was present significantly in higher proportion among cases than controls. Crop failure, interpersonal problems, medical illness, and marriage of female family member were significant stressful life events.
Conclusions:
There are socioeconomic and psychological risk factors for suicide by farmers which can be targets of prevention policy.
Key words: Farmers' suicide, indebtedness, risk factors, stressful life events
INTRODUCTION
Farming is one of the oldest industries in the world and often portrayed as a happy way of life. Despite this, agriculture has one of the highest rates of suicides than any industry.[1] Studies from Canada, Australia, United Kingdom (UK), and Sri Lanka have found high levels of distress and high suicide rate among farmers.[2,3,4,5] Based on proportional mortality ratios, farmers were among the top ten occupational groups with highest proportional mortality rates in the UK. In a psychological autopsy study from England, mental illness was most often judged as an important risk factor for suicide by farmers.[6] In Australia, suicide by farmers is linked with the occurrence of droughts.[3] In India, in the 10 years, between 1997 and 2006 as many as 166,304 farmers have committed suicide.[7] The farmers' suicide rate in the country in the year 2001 was 12.9 which was about one-fifth higher than the general suicide rate, which was 10.6 in that year.[8] Economic factors such as indebtedness, crop failures, and acute financial loss or responsibility (e.g., marriage in family) were significantly associated with farmers' suicides in Vidarbha region of Maharashtra and rural Punjab.[9,10] A qualitative study from Vidarbha region revealed that farmers perceived debt, addiction, environmental problems, low price for farm produce, stress, family responsibility, government apathy, etc., as the most significant reasons for farmers' suicides.[11] Studies on this issue in India so far have focused on socioeconomic and farming related risk factors. There is no controlled psychological autopsy study of farmers' suicide from India. This study was undertaken to meet this unmet need with objectives of studying socioeconomic and psychological correlates of farmers' suicide.
MATERIALS AND METHODS
A matched case–control study was conducted from July 2008 to December 2009 in wardha District, located in Vidarbha region of Maharashtra State of India, one of the worst affected regions by farmers' suicides.[9] Wardha District has an area of 6310 km2 with total cultivable area 429,600 hectare, and only one-fourth of it is under irrigation. It has a population of 1.23 million with male to female ratio of 1:0.9 and 80.5% literacy.[12] Previous studies have reported high number of suicides among farmers in the district.[13,14] Ethics Committee approval was obtained from Institute Ethics Committee for Research on Human Subjects, Mahatma Gandhi Institute of Medical Sciences, Sevagram, Wardha, India. Before participating in the study, a written informed consent was obtained in local language (Marathi) from the respondents. Data were collected by home visits.
Selection of cases
We had planned to include all 111 consecutive cases of suicides listed under farmers' suicide category in Wardha District that occurred from April 1, 2007, to March 31, 2008 (one financial year). This list was provided by office of District Magistrate Wardha, Government of Maharashtra, India on their official website.[12] Of 111 families 10 were not available on given home address and neither could be assessed on the first and nor on a second home visit. One household refused to participate in the study while two suicide victims were not farmers by occupation, so they were not included in the study. Thus, data were obtained from households of 98 suicide cases.
Selection of controls
We selected 1:1 age (+/- 2 years), sex and occupation matched living controls who were residing in the same village. They were preferably identified from the same lane where suicide (case) households were residing. Controls were not blood relatives of cases. In a situation where eligible controls could not be identified or declined to participate in the study from same lane, adjacent lanes were visited for selection of controls.
Data collection
Psychological autopsy method was used. There were 89 villages/towns spread across Wardha District where farmers in the list had committed suicides. These villages were located on map, and a team of psychiatry resident doctor and psychologist trained in psychiatric assessment visited the households. While planning the visits a minimum period of 3 months was ensured between date of suicide and date of interview for resolution of grief. After explaining the purpose of our visit, a key informant in the family was identified who was living with the subject under study and had good knowledge about his life. Whenever felt necessary information was also obtained from other persons in the family or friends when available. A semi-structured interview schedule was developed by inputs and consensus of all investigators. It was pilot tested, and relevant modifications were done to final version. Data were gathered regarding sociodemographic variables, farming practices, economic status and indebtedness, behavioral symptoms during a lifetime with special attempt to ascertain mental status in 6 months before suicide for cases. Government of India issues ration cards to its citizens. Yellow colored ration card is issued to those families with low income and is termed below poverty line (BPL) ration card. Red and white cards are issued to those above poverty line. Type of ration card was noted along with average annual income of family. History of psychoactive substance abuse was also noted. CAGE questionnaire was used to ascertain severity of alcohol abuse.[15] A detailed description was obtained whenever there were some behavioral changes, and attempt was made to ascertain diagnostic category using Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (TR) diagnostic criteria.[16] Whenever available documents of any treatment received by person were also reviewed. An overall attempt was made to get the details of mental status of the study subjects by empathetic and nonthreatening interview of informants. Family history of mental illness, suicide attempts, or completed suicide was noted. All the interview schedules and 10% of cases were reviewed by senior psychiatrist. Variables about suicide and circumstances around it like date, time, place, method of suicide, planning involved, expression of suicide ideas or suicide note, etc., were also noted. Stressful life events in prior 3 years were enquired in depth with special focus on stressors related to farming, interpersonal relations, economic difficulties, major health problems, legal issues, etc., There was also a provision to record multiple stressful life events including those not on the list prepared. Government of India provides financial aid and farming implement as ex gratia help to suicide households, details of which were also noted. Respondents were also asked if someone attempts suicide where they would take the person and whether psychiatric consultation should be done for such a person. In the end, appropriate referral services were offered to family members after ascertaining need and willingness of the person.
Statistical analysis
All the data were entered in the Microsoft Excel and analyzed by STATA/SE 14.1 statistical package (Stata Corp, 2015). Characteristics of cases and controls were described with numbers and percentages. We assessed the association of various individual risk factors of farmer suicides by univariate analysis through Mantel-Haenszel estimate of odds ratio (OR). The final model was built through multivariable conditional logistic regression analysis model with a forward stepwise procedure, the farmers' suicide being the dependent variable, and all other identified risk factors as independent variables. We omitted variables showing co-linearity from final model. The estimate of the percentage of variance in the outcome explained by the model was done by calculating pseudo R2 value. All reported P values are two-tailed, with P < 0.05 defining significance.
RESULTS
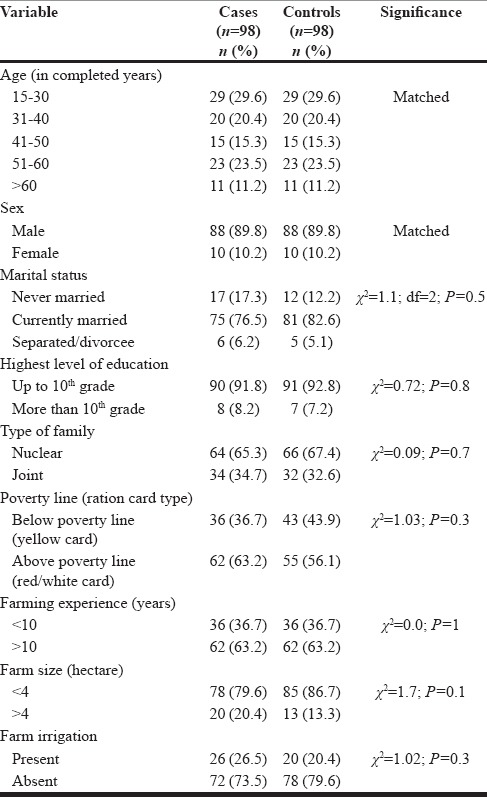
Of 111 suicide households visited, 98 could be recruited for study; thus, the response rate was 88.28%. Minimum and maximum intervals between date of suicide and date of interview were 7 months and 31 months respectively with an average of 20 months. Fifty percent of the subjects were younger than 40 years of age with male to female ratio of 8.8:1. Ninety-two percent were educated up to 10th grade, majority were married (76.5%) and resided in nuclear families (65.3%). According to ration card type, 36 (36.7%) of suicide households and 43 (43.9%) of control families were BPL. Most farmers had farming experience of more than 10 years and had small size farms (<4 hectares) without irrigation facilities [Table 1]. Case and control groups did not differ significantly on sociodemographic variables.
Table 1.
Sociodemographic and farming profile of farmers’ suicide victims and controls
Home (n = 50, 51.0%) was most common place of suicide followed by farm (n = 41, 41.8%) and other places (n = 7, 7.2%). Methods of suicide adopted were: Pesticide consumption 67 (68.37%) followed by hanging 15 (15.31%), drowning 12 (12.24%), self-immolation 3 (3.06%), and one farmer committed suicide by run over by train (1.02%). Recent change in behavior of suicide victim was noticed by 55 (56.12%) of the family members. Relatives reported that 19 (19.4%) of suicide victims had expressed suicidal ideas to family members or friends within 1 month period before suicide.
Several social and economic factors were examined for their association with farmers' suicides. In terms of social variables, two groups did not differ significantly. Compared to controls, suicide households were significantly more likely to lease out their farms, had to sell their farm land or bullocks in preceding 5 years to meet their expenses [Table 2]. Procurement of any amount of debt in the preceding 3 years four times increased risk of completed suicides by farmers while debt from multiple sources increased odds of completed suicide 28 times.
Table 2.
Univariate regression analysis of social and economic risk factors of farmer's suicides
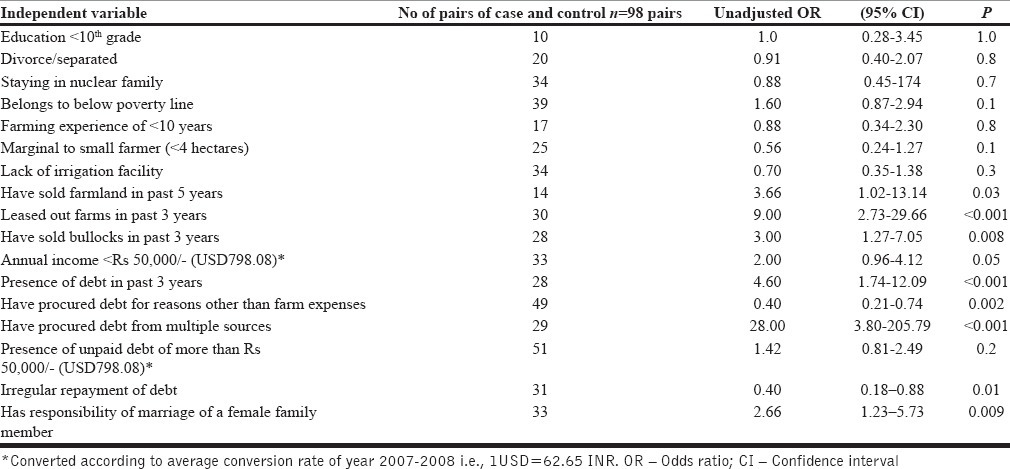
Responsibility of marriage of some female family member in the near future increased risk of completed suicides by nearly 3 times (OR = 2.66; 95% confidence interval [95% CI] =1.23–5.73).
Case and control groups did not differ significantly in terms of annual income, irregular repayment of debt, and amount of pending debt to be repaid.
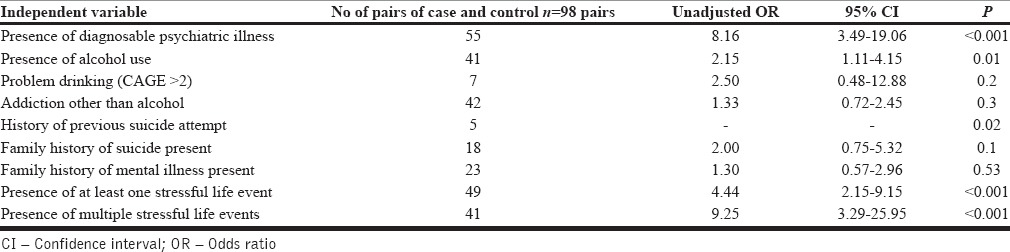
Table 3 summarizes the role of psychological factors in farmers' suicides. The presence of diagnosable psychiatric illness increased the odds of completed suicide nearly eight times (OR = 8.16; 95% CI = 3.49–19.06). Sixty percent (n = 59) of suicide victims had some diagnosable psychiatric illness, of these five had received psychiatric treatment. Common probable diagnoses in cases and controls (n = 98) respectively were depression (37 [37.7%] and 6 [6.1%]), alcohol dependence syndrome (10 [10.2%] and 8 [8.1%]), brief psychotic disorder (4 [4.0%] and 1 [1.0%], schizophrenia 3 [3.1] and 0), alcohol dependence syndrome with major depressive disorder (2 [2.0%] and 0), erectile dysfunction (1 [1.0%] and 0), alcohol-induced psychotic disorder (1 [1.0%] and 1 [1.0%]), and acute stress reaction (1 [1.0%] and 0). Use of alcohol irrespective of abuse or dependence, increased risk of suicide nearly two times (OR = 2.15; 95% CI = 1.11–4.15). There were no significant differences among two groups in terms of problem drinking based on CAGE scores, presence of other substance abuse, previous suicide attempts, and family history of mental illness or suicide. The presence of a stressful life event in the preceding year increased odds of completed suicides 4 times (OR = 4.44; 95% CI = 2.15–9.15) while presence of more than one stressful life events 9 times increased the risk of suicide (OR = 9.25; 95% CI = 3.29–25.95). Reported stressful life events among cases and controls respectively were crop failure (52 [53.06%] and 37 [37.76%]), problems in interpersonal relationships (15 [15.31] and 0), physical illness or disability (9 [9.18%] and 2 [2.04%]), marriage of sister of daughter (6 [6.12%] and 7 [7.14%]), and death of a family member (3 [3.06%] and 8 [8.16%]).
Table 3.
Univariate regression analysis of psychological risk factors of farmer's suicides
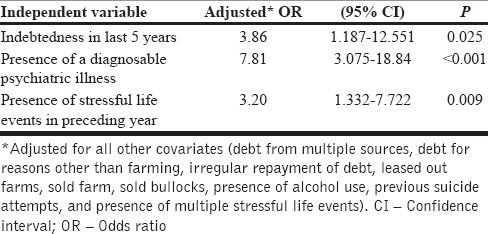
On multiple forward stepwise conditional logistic regression analysis after controlling for collinear covariates, three important risk factors emerged. These were indebtedness in preceding 5 years (OR = 3.86), presence of diagnosable psychiatric illness (OR = 7.81), and presence of stressful life events in preceding year (OR = 3.20) as described in Table 4.
Table 4.
Multivarite forward stepwise conditional logistic regression analysis model with suicide as dependent variable
Government of India provides ex gratia help to survivors of farmers' suicides either in the form of money (Rs. 100,000) or farm implements. only 45% of the suicide households had received some form of aid from the government. Perceived first point of help in a situation of suicide attempt by family member was also assessed. Of all the farmers in study (n = 196), primary health care center was perceived as first point of contact by 102 (52.04%), Civil Hospital (Government District Hospital) by 47 (23.98%), tertiary care center like medical college by 37 (18.85%), and 10 (5.10%) perceived police station as first point of help. Sixty-eight percent farmers were in favor of psychiatric consultation after suicide attempt by a person.
DISCUSSION
Case–control psychological autopsy with living persons as controls is a standard and accepted method in the study of suicides. Findings from this study highlight the multifactorial etiology of farmers' suicides. These factors often operate with cumulative effect and have complex interactions among them.[17] In this study, majority of the suicide victims were male farmers with a male to female ratio of 8.8:1. This ratio is much higher than the ratio of 1.7:1 for suicides in the general population in India.[18] High proportion of suicides among male farmers compared to females had been reported from high-income countries such as England and Wales, Australia, North America, and European countries.[3,4,19,20,21] Other similarities between findings of the present study with that of studies from high-income countries were the presence of high psychological morbidity, economic problems, and stressful life events as important risk factors for suicides by farmers. Given this, there are some important differences also. The proportion of farmers with economic difficulties and indebtedness is significantly high in the present study than that quoted in western studies. Family history of mental illness or suicides and interpersonal problems were seen less often in the present study than that reported in studies from high-income countries. Majority of farmers in India had lower annual income, and many either did not possess bullocks and livestock or had sold it.[14] This is in contradiction to findings from the UK where presence of livestock, especially pigs, was one of the important risk factors for suicides by farmers.[6] Pesticides in lethal concentrations are easily available in rural as well as urban communities in India which are the reason for pesticide consumption being most common method of suicide in country.[22] In similar lines, common methods of suicide used by farmers in the present study were pesticide poisoning followed by hanging and self-immolation while, common methods of suicide by farmers in west was by firearms, hanging, and carbon monoxide poisoning.[3,4]
Farmers, in general, have higher psychological morbidity than general population. Farmers face compounding effects of physical stressors, environmental changes, changing farm economics, lack of differentiation between professional and personal life with no customary age of retirement leading to conflicts among different generations in family.[9] A study from the UK using GHQ-12 questionnaire showed significantly higher psychological morbidity among farmers and their family members compared to nonfarmer controls.[23] One study from Australia differs in this regard where mental health problems in farmers were comparable to nonfarmer controls[24] Indebtedness has been proposed as one of the major causes of suicide by farmers in India.[11] However, there are very few controlled studies assessing role of this factor in causation of farmers' suicides. There is only one case–control study from central India, which compared indebtedness in suicide and nonsuicide households.[14] The present study found that significantly more suicide households than controls had experienced crop failure, had some additional economic liabilities, had procured debt especially debt for nonagricultural purposes and debt from multiple sources. In this study, majority of farmers (82% of all farmers interviewed) had procured debt. Most common source of debt was commercial banks, which issue “crop loan” to farmers to meet expenses during sowing season. It is hoped that providing money to spend on agriculture will help in better inputs and ultimately good yields for crops so that these debts are paid back to banks, with good profit to farmers. When there are additional or unexpected expenses like family liabilities (e.g., health, education, and festivals), marriage of female family members, etc., or loss due to crop failure occurs; farmer gets trapped into this cycle with mounting amounts of debt, causing distress.[10,14]
Psychological illnesses are important risk factors for suicide. In the present study, there was some diagnosable psychiatric illness in 60% of the farmers who completed suicide. Significant correlation between mental illness and suicide by farmers had been reported from the UK.[6] There is no prior controlled psychological autopsy study with only farmers as study group from India. There are psychological autopsy studies on suicide in general population from major cities in different parts of India such as from Bangalore, Chandigarh, and Chennai, which have reported significantly higher rate (ranging from 43% to 88%) of mental illness among suicide victims than general population controls.[16,25,26] The most common psychiatric diagnosis was depression followed by alcohol dependence and other psychiatric illnesses. Other findings from these studies replicated in present study were near similar age distribution of suicide victims, association with lower socioeconomic status and poverty and significantly higher proportion of stressful life events compared to controls. However, there are some notable differences among farmers' suicides and suicides in general population. Significantly higher proportion of farmers' suicide victims had indebtedness than reported among suicide victims in general. On the other hand, interpersonal problems, violence in family, correlation with alcohol dependence, history of suicide attempt, and family history of suicide were lesser among farmers' who had committed suicide than that found in above-mentioned psychological autopsy studies from India.
In this study, we also explored what was the perceived first source of help in situation of suicide attempt by family member. Primary health care centers and government hospitals at district place were most preferred the first source of help in an event of suicide attempt by family member. Most of these hospitals in India are not equipped with resources required to treat pesticide poisoning which is the most common method of suicide in country. Majority of respondents were in favor of seeking psychiatric consultation for a person who attempts suicide which is important point in favor of involvement of mental health professionals in prevention of farmers' suicides. These findings have important implications in devising suicide prevention strategies.
CONCLUSIONS AND IMPLICATIONS FOR SUICIDE PREVENTION
The present study emphasizes role of multiple risk factors in causation of farmers' suicides, highlights how farmers' suicides differ from suicide in general population and also throws light on perceived points of contacts in a situation of suicide attempt. Thus, suicide prevention program for farmers should be multipronged aiming at socioeconomic and psychological well-being of farmers along with provision of support in situations of stressful life events. Strategies for prevention of farmers' suicides need should have both short- and long-term interventions. Present study reveals some important risk factors which can help early identification of farmers at risk. Early identification and appropriate support to these farmers are urgently needed to prevent further suicides. Over short term, interventions targeting method of suicide can be the most effective intervention to reduce number of deaths and thus suicide rate. These include compulsory dilution of pesticides at manufacturing units to reduce lethality of pesticides before reaching market, providing lockable boxes to farmer households and educating farmers about safe use of pesticides. Similar strategy has significantly reduced suicide rate in Sri Lanka.[5] As primary and secondary health care centers are the most common perceived sources of help in case of suicide attempt, upgrading infrastructure and training of staff in management of pesticide poisoning, life support skills, etc., will help in reducing death rate from suicide significantly. Mandatory psychiatric evaluation after suicide attempt is important step in preventing future attempts. Over long term, definitive steps are needed at macro and micro level to uplift the farm economy. Considering its diversity India needs a socioculturally relevant suicide prevention program which can be incorporated into broader health, education, and other welfare programs.[16] Creating a referral network of government and private hospitals and mental health professionals, training health professionals in identifying high-risk farmers, and strategies aimed at reducing stigma attached to mental illness will go a long way in suicide prevention.
Limitations
Results of this study should be interpreted in the light of its limitations. First, this study involved only one district of India and considering geographic and cultural diversity in the country findings cannot be generalized. Recall bias on part of informants is also a limiting factor as in some cases here was long interval between suicide and date of interview of family member. This is likely to be compounded by stress and grief reaction in family members. In the absence of person in consideration, diagnoses reached upon by psychological autopsy can only a probable diagnosis.
Financial support and sponsorship
This research was funded by intramural grant by MGIMS Sevagram, which was used for travel expenses during data collection.
Conflicts of Interest
There are no conflicts of interest.
Acknowledgment
Authors are deeply thankful to Late Mrs. Manikyamba Behere for her help and support to this research project. We are thankful to all the staff in department of psychiatry for direct and indirect help. We are also thankful to Dr. Manoj Talapalliwar for statistical help. We express our gratitude towards all the family members of suicide victims and controls for participation in study.
REFERENCES
- 1.McCurdy SA, Carroll DJ. Agricultural injury. Am J Ind Med. 2000;38:463–80. doi: 10.1002/1097-0274(200010)38:4<463::aid-ajim13>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 2.Pickett W, Hartling L, Brison RJ, Guernsey JR. Fatal work-related farm injuries in Canada, 1991-1995.Canadian Agricultural Injury Surveillance Program. CMAJ. 1999;160:1843–8. [PMC free article] [PubMed] [Google Scholar]
- 3.Page AN, Fragar LJ. Suicide in Australian farming, 1988-1997. Aust N Z J Psychiatry. 2002;36:81–5. doi: 10.1046/j.1440-1614.2002.00975.x. [DOI] [PubMed] [Google Scholar]
- 4.Hawton K, Fagg J, Simkin S, Harriss L, Malmberg A, Smith D. The geographical distribution of suicides in farmers in England and Wales. Soc Psychiatry Psychiatr Epidemiol. 1999;34:122–7. doi: 10.1007/s001270050122. [DOI] [PubMed] [Google Scholar]
- 5.Hawton K, Ratnayeke L, Simkin S, Harriss L, Scott V. Evaluation of acceptability and use of lockable storage devices for pesticides in Sri Lanka that might assist in prevention of self-poisoning. BMC Public Health. 2009;9:69. doi: 10.1186/1471-2458-9-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Malmberg A, Simkin S, Hawton K. Suicide in farmers. Br J Psychiatry. 1999;175:103–5. doi: 10.1192/bjp.175.2.103. [DOI] [PubMed] [Google Scholar]
- 7.Nagaraj K. Farmers' Suicides in India: Magnitude, Trends and Partial Patterns. Madras Institute of Development Studies. 2008. [Last cited on 2009 Jul 15]. Available from: http://www.macroscan.com/anl/mar08/pdf/farmers_suicides.pdf .
- 8.National Crime Records Bureau. Accidental Deaths and Suicides in India. Ministry of Home Affairs, Government of India. 2001 [Google Scholar]
- 9.Behere PB, Bhise MC. Farmers' suicide: Across culture. Indian J Psychiatry. 2009;51:242–3. doi: 10.4103/0019-5545.58286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhalla GS, Sharma SL, Wig NN, Mehta S, Kumar P. Report Submitted to Government of Punjab by Institute for Development and Communication. Chandigarh: Himalaya Press; 1998. Suicides in Rural Punjab. [Google Scholar]
- 11.Dongre AR, Deshmukh PR. Farmers' suicides in the Vidarbha region of Maharashtra, India: A qualitative exploration of their causes. J Inj Violence Res. 2012;4:2–6. doi: 10.5249/jivr.v4i1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Office of District Magistrate. List of Farmers' Suicides in Wardha District. 2008. [Last Cited on 2008 Aug 10]. Available from: http://www.wardha.nic.in/en/htmldocs/gr/farmer-suicide.pdf .
- 13.Behere PB, Behere AP. Farmers' suicide in Vidarbha region of Maharashtra state: A myth or reality? Indian J Psychiatry. 2008;50:124–7. doi: 10.4103/0019-5545.42401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mishra S. Suicide of Farmers in Maharashtra State: Report Submitted to Government of Maharashtra State. Indira Gandhi Institute for Development Research, Mumbai. 2006. [Last cited on 2008 Sep 12]. Available from: http://www.igidr.ac.in/suicide/suicide.htm .
- 15.Mayfield D, McLeod G, Hall P. The CAGE questionnaire: Validation of a new alcoholism screening instrument. Am J Psychiatry. 1974;131:1121–3. doi: 10.1176/ajp.131.10.1121. [DOI] [PubMed] [Google Scholar]
- 16.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV TR. 4th Edition. Text Revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 17.Gururaj G, Isaac MK, Subbakrishna DK, Ranjani R. Risk factors for completed suicides: A case-control study from Bangalore, India. Inj Control Saf Promot. 2004;11:183–91. doi: 10.1080/156609704/233/289706. [DOI] [PubMed] [Google Scholar]
- 18.National Crime Records Bureau. Accidental Deaths and Suicide in India. Ministry of Home Affairs, Government of India. 2008 [Google Scholar]
- 19.Gallagher AG, Sheehy NP. Suicide in rural communities. J Community Appl Soc Psychol. 1994;4:145–55. [Google Scholar]
- 20.Gunderson P, Donner D, Nashold R, Salkowicz L, Sperry S, Wittman B. The decision to die- the epidemiology of suicide among farm residents or workers in five North Central States, 1980-88. Am J Prev Med. 1993;9:26–32. [Google Scholar]
- 21.Stallones L. Suicide mortality among Kentucky Farmers, 1979-1985. Suicide Life Threat Behav. 1990;20:156–63. [PubMed] [Google Scholar]
- 22.Vijaykumar L. Suicide and its prevention: The urgent need in India. Indian J Psychiatry. 2007;49:81–4. doi: 10.4103/0019-5545.33252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hounsome B, Edwards RT, Hounsome N, Edwards-Jones G. Psychological morbidity of farmers and non-farming population: Results from a UK survey. Community Ment Health J. 2012;48:503–10. doi: 10.1007/s10597-011-9415-8. [DOI] [PubMed] [Google Scholar]
- 24.Judd F, Jackson H, Fraser C, Murray G, Robins G, Komiti A. Understanding suicide in Australian farmers. Soc Psychiatry Psychiatr Epidemiol. 2006;41:1–10. doi: 10.1007/s00127-005-0007-1. [DOI] [PubMed] [Google Scholar]
- 25.Chavan BS, Singh GP, Kaur J, Kochar R. Psychological autopsy of 101 suicide cases from northwest region of India. Indian J Psychiatry. 2008;50:34–8. doi: 10.4103/0019-5545.39757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vijayakumar L, Rajkumar S. Are risk factors for suicide universal? A case-control study in India. Acta Psychiatr Scand. 1999;99:407–11. doi: 10.1111/j.1600-0447.1999.tb00985.x. [DOI] [PubMed] [Google Scholar]


