Abstract
Objective:
Risk factors for inpatient suicide are different from those in the general population. We examined sociodemographic and clinical variables of patients who committed suicide as an inpatient in a psychiatric hospital in India.
Methods:
Matched retrospective nested case–control design was adopted. Ten patients who died by suicide as inpatients between 2000 and 2013 were included, along with fifty controls, matched with respect to age, sex, diagnosis, and period of admission.
Results:
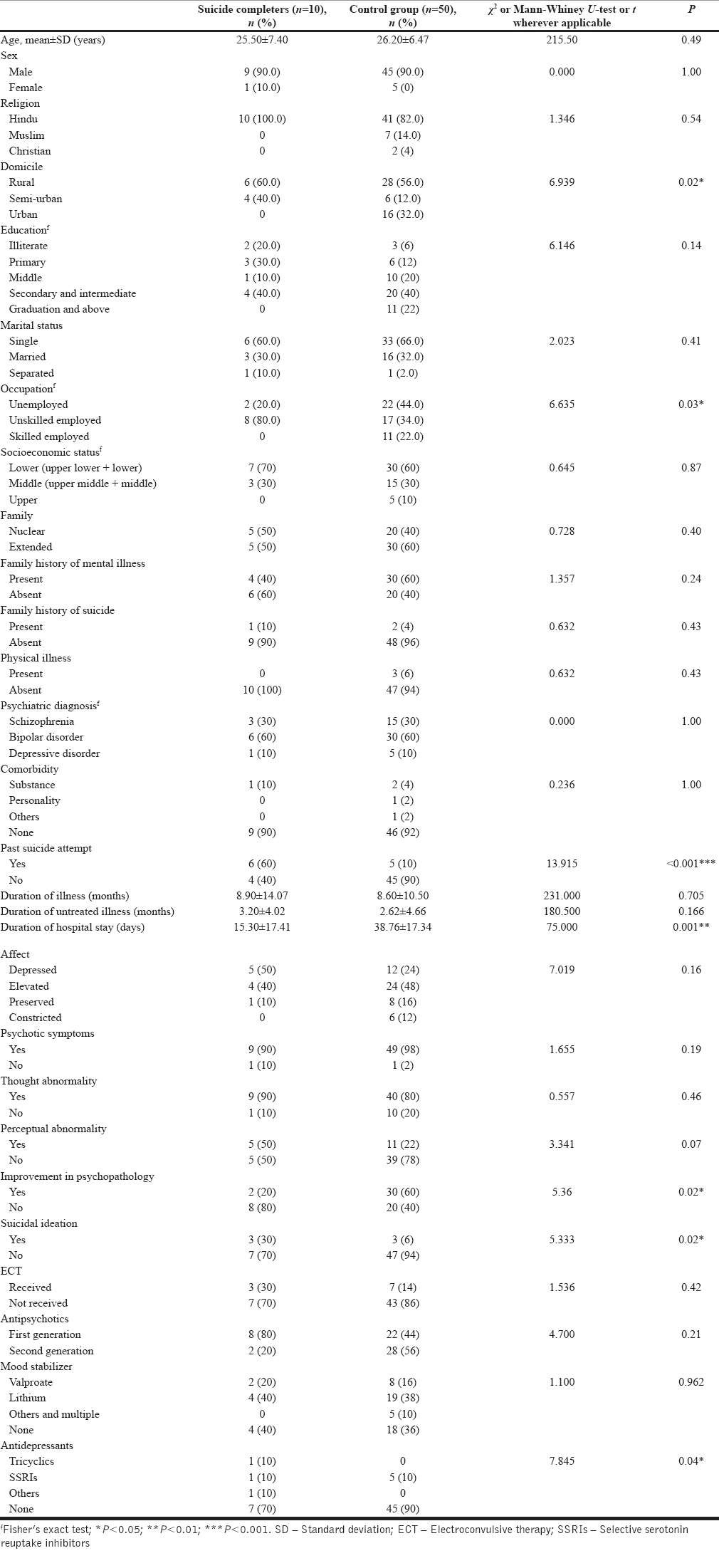
Suicide completers were mostly unskilled in occupation (P = 0.03), had a history of past suicide attempts (P < 0.001), shorter duration of hospital stay (P = 0.001), poorer improvement on psychopathology (P = 0.02), and were having more suicidal ideation (P = 0.02). Significantly more completers were receiving antidepressants (P = 0.04).
Conclusion:
This study adds to the existing sparse literature on inpatient suicides from Asia. Strength of the study was close matching between case and controls and blindedness. Limitations were retrospective design, and variations in prescription behavior and treatment decisions.
Key words: Case–control, inpatient suicide, risk factors
INTRODUCTION
Inpatient suicide is an important issue which has significant administrative, legislative, and therapeutic underpinnings.[1,2,3] It is defined by Ohemichen and Staak, as the “suicide of a patient during in-patient treatment, both inside and outside the hospital setting, e.g., during a leave, an outing, a trial discharge, or a stay in another hospital with concurrent inpatient psychiatric treatment.”[4] The rate of inpatient suicide ranges from 100 to 400 per 100,000 psychiatric admissions.[5,6,7] Research shows that approximately 25%–40% of suicide victims are in contact with psychiatric services in the year before death.[8,9] Among them, 14% receive inpatient care and 20% of them die while in the hospital.[9,10] However, suicidal behaviors are difficult to predict,[11,12] also the risk factors for suicide in inpatients are not essentially the same as the risk factors for suicide in other population groups.[7,13]
In comparison to the abundant information on inpatient suicide in the West, there is a paucity of data on inpatient suicide in Asia. Thus, the goal of the present study was to extend our previous work to identify more precisely the factors associated with inpatient suicides.
METHODS
Identification of cases and controls
This study follows an earlier study by authors on the same inpatients who had completed suicide at Central Institute of Psychiatry, Ranchi, India.[14] Instead of a 1:1 matched design, we followed a 1:5 matched nested case–control design to reduce selection bias and to enhance accuracy of the findings than our previous study.[14,15,16] This study pertains to ten suicide cases that occurred at Central Institute of Psychiatry, Ranchi, Jharkhand, India between the years from 2000 to 2013. For this study, each suicide case was matched with five living controls based on the following criteria (in descending order of importance): (1) sex, (2) diagnoses, (3) age, and (4) admission period, from the inpatient population of the institute. Period of admission was matched to minimize the influence of possible changes in clinical practice (e.g., admission policy, medication preferences, dosage strategies, prevailing prescribing guidelines, ward routines, and cultures) over time.[17,18] Thus, a living control group consisting of fifty patients was selected.
Data collection
After obtaining ethical permission, data were extracted from medical case notes by one researcher and recorded. To ensure blindedness as to the case–control status of the case notes, the senior researcher obtained the medical case notes from medical records section. The records were copied and to minimize information bias and to maintain blindness, information regarding the period after the censoring date (the date of death of the case) was also removed from the control's record. Method of chart review was followed for data collection. Data were analyzed using Statistical Package for the Social Sciences version 20.0 for windows (Armonk, NY: IBM Corp).
RESULTS
During the period from 2000 to 2013, a total number of admissions were 48,666 in our center. A total of 10 suicides were recorded during this period. Among them, 9 were males. The incidence rate of suicide was around 20 per 100,000 (0.02%) for the specified period.
Table 1 summarizes the sociodemographic, clinical, and treatment profiles between two groups.
Table 1.
Comparison of sociodemographic variables between two groups
DISCUSSION
There were few case–control studies of inpatient suicide.[7,18,19,20,21,22,23,24] A recent case–control study by Dong et al. has included inpatient suicide of 3 years' period.[24] The current study included 14 years' period for analysis of inpatient suicide which is more than most of the other studies. Another strength in our study was close matching between cases and controls. As the inpatient suicide was a relatively rare event, so we chose to multiply the number of control to five times than that of the cases, to exclude any spurious associations, those might be found with 1:1 matching in our previous study.[14] Furthermore, we tried to minimize the bias of data extraction using a data collection procedure which was blinded to one researcher who collected data.
This study found a statistically significant association between the domicile and the suicide completion. Most of the suicide completers were from the rural or semi-urban area, whereas a significant number of control group population belonged from urban areas. Although majority of the population live in the villages in this part of the country, this finding still is significant, as this has repeatedly been reproduced in various studies dealing with different populations.[25,26] The increased tendency of suicide in rural population is partly due to easy accessibility of lethal substances (such as poison in India or firearms in western countries), but the poor accessibility to mental healthcare, leading to grave psychological debility is another significant contributor,[27] which may have been reflected in the inpatient suicide also. The suicide completers were mostly unskilled in occupation. The occupation as well as domicile indicates a possible socioeconomic backwardness among the suicide completers, which may be the underlying factor for their tragic end.
Duration of hospital stay was observed to be shorter in suicide completers group. This finding indicates that the risk of suicide is much higher in the earlier part of the acute illness and inpatient stay. A number of studies have reported that the 1st week of admission is a time of particularly acute risk,[28,29] when around a quarter of suicides occur.[30,31,32] Further, the risk of suicide is declined by time since admission and discharge.[33] Our results are consistent with the findings of these earlier studies. It may be that receiving a psychiatric diagnosis that requires inpatient treatment is particularly stressful, and the experience of entering a “frightening” or “intimidating” environment may increase suicidal ideation.[34] Furthermore, symptoms of psychiatric illness are generally most severe at the time of admission, and with effective treatment, the symptoms subside thereby reducing the risk of suicide among inpatients. Further, there may be an association between being admitted and a heightened experience of stigma. If these features do contribute to risk, suicide prevention at this critical stage may be enhanced by increased support and strong therapeutic relationships, factors known to lead to positive treatment outcomes.[35] Although nature of psychopathologies across two groups did not differ significantly, improvement in psychopathology was significantly lower in suicide completers group than in control group. However, on the basis of our data, it is not possible to determine to what extent clinical improvement causally related to a reduced risk of suicide. However, our results support the general opinion regarding affective illness that clinical improvement could reduce the risk of suicide.[33,36,37] Another important finding was the past history of suicide attempts, and current suicidal ideations, which were significantly higher in suicide completers group. The suicidal thought as well as previous suicide attempts is proven risk factors for suicide,[38] both in the outpatient[39] as well as inpatient setting.[7,40] It is widely observed that suicide completers often verbalize their wish, or engage in suicidal attempt, before completion of the act, which may be an expression of the persistent “psychache” of the person, which is considered to be a core component of suicide completion.[41]
There were few drug studies on the case–control comparison of inpatient suicide. Dong et al. found no difference in treatment parameters between suicide completers and matched controls.[24] In other studies, a lower dosage of antipsychotic and fewer prescription of mood stabilizer were reported among completers group. Significantly higher proportion of controls than suicide completers across studies was on lithium.[19,23,42] However, we did not find such difference on lithium use between groups. Among antidepressants norepinephrine and specific serotonergic antidepressants (noradrenergic and specific serotonergic antidepressants) and serotonin and norepinephrine reuptake inhibitor predicted suicide risk among inpatients with affective disorder.[43] Although our study does not have any predictive value, the use of antidepressants was found to be significantly higher in suicide completers. The more extensive use of antidepressants in the suicide completers group signifies the depressed affective state in those patients before suicide. It was found that 50% of the suicidal patient's affect was depressed on the last mental status examination before the fatal act. Various studies show that depressive symptoms as well as treatment with antidepressants are associated with inpatient as well as postdischarge suicide.[44,45] Both of the findings collectively show the significant mental agony through which the suicide completers had to trudge in their final days.
One of the limitations of this study was that information is based on routine clinical assessments recorded in case record files, which were not collected for research purpose. Although the retrospective nature of this study is a drawback, the psychiatrists were “blind” to the eventuality of suicide when they made the notes in the case record files, thus eliminating the “after the event” bias. The other limitation of the current study was small sample size. Although the other studies, which had large sample size, were population-based and had included more than one mental health and general hospitals and had longer follow-up period.[20,24,46,47] Furthermore, variations in prescription behavior and treatment decisions among treating teams were not controlled.
CONCLUSION
Patients residing in the rural population, unskilled in occupation, with shorter hospital stay were more common among suicide completers in our study. In our study, early inpatient suicide appears to be in acutely ill individuals who more commonly had an affective disorder and had past history of suicide attempts, and currently active suicidal ideation. Furthermore, it is important to be aware of the risk of suicide in patients with no or little clinical improvement during inpatient treatment. Although our study was descriptive in nature due to small sample size and the ability to predict suicide accurately is limited, the comprehensive and continued assessment of individual sociodemographic and clinical factor may prevent some fatal outcome.
Financial support and sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
REFERENCES
- 1.Inpatient Suicides: Recommendations for Prevention. Washington, DC: Joint Commission on Accreditation of Healthcare Organizations; 1998. Joint Commission on Accreditation of Healthcare Organizations. [Google Scholar]
- 2.Sentinel Events in Australian Public Hospitals 2004-2005. Canberra: AIHW; 2007. Australian Institute of Health and Welfare (AIHW) and Australian Commission on Safety and Quality in Health Care (ACSQHC) (Safety and Quality of Health Care Series). [Google Scholar]
- 3.Framework 2009-2010. Process and Action for Primary Care Trusts 2009-2010. London: NPSA; 2009. National Patient Safety Agency. Never Events. [Google Scholar]
- 4.Oehmichen M, Staak M. Suicide in the psychiatric hospital. International trends and medico legal aspects. Acta Med Leg Soc (Liege) 1988;38:215–23. [PubMed] [Google Scholar]
- 5.Coakley GM, Carey TG, Owens JM. A study of psychiatric inpatient suicides. Ir J Psychiatry Med. 1996;13:102–4. [Google Scholar]
- 6.Deisenhammer EA, DeCol C, Honeder M, Hinterhuber H, Fleischhacker WW. In-patient suicide in psychiatric hospitals. Acta Psychiatr Scand. 2000;102:290–4. doi: 10.1034/j.1600-0447.2000.102004290.x. [DOI] [PubMed] [Google Scholar]
- 7.Powell J, Geddes J, Deeks J, Goldacre M, Hawton K. Suicide in psychiatric hospital in-patients. Risk factors and their predictive power. Br J Psychiatry. 2000;176:266–72. doi: 10.1192/bjp.176.3.266. [DOI] [PubMed] [Google Scholar]
- 8.Pirkis J, Burgess P. Suicide and recency of health care contacts. A systematic review. Br J Psychiatry. 1998;173:462–74. doi: 10.1192/bjp.173.6.462. [DOI] [PubMed] [Google Scholar]
- 9.Appleby L, Shaw J, Amos T, McDonnell R, Harris C, McCann K, et al. Suicide within 12 months of contact with mental health services: National clinical survey. BMJ. 1999;318:1235–9. doi: 10.1136/bmj.318.7193.1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Appleby L, Dennehy JA, Thomas CS, Faragher EB, Lewis G. Aftercare and clinical characteristics of people with mental illness who commit suicide: A case-control study. Lancet. 1999;353:1397–400. doi: 10.1016/S0140-6736(98)10014-4. [DOI] [PubMed] [Google Scholar]
- 11.Hawton K. Assessment of suicide risk. Br J Psychiatry. 1987;150:145–53. doi: 10.1192/bjp.150.2.145. [DOI] [PubMed] [Google Scholar]
- 12.Geddes J. Suicide and homicide by people with mental illness. BMJ. 1999;318:1225–6. doi: 10.1136/bmj.318.7193.1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bowers L, Banda T, Nijman H. Suicide inside: A systematic review of inpatient suicides. J Nerv Ment Dis. 2010;198:315–28. doi: 10.1097/NMD.0b013e3181da47e2. [DOI] [PubMed] [Google Scholar]
- 14.Bose S, Khanra S, Umesh S, Khess CR, Ram D. Inpatient suicide in a psychiatric hospital: Fourteen years' observation. Asian J Psychiatr. 2016;19:56–8. doi: 10.1016/j.ajp.2015.12.004. [DOI] [PubMed] [Google Scholar]
- 15.Sedgwik P. Nested case-control studies: Advantages and disadvanatages. BMJ. 2014;348:g1532. doi: 10.1136/bmj.f7707. [DOI] [PubMed] [Google Scholar]
- 16.Biesheuvel CJ, Vergouwe Y, Oudega R, Hoes AW, Grobbee DE, Moons KG. Advantages of the nested case-control design in diagnostic research. BMC Med Res Methodol. 2008;8:48. doi: 10.1186/1471-2288-8-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Appleby L, Cooper J, Amos T, Faragher B. Psychological autopsy study of suicides by people aged under 35. Br J Psychiatry. 1999;175:168–74. doi: 10.1192/bjp.175.2.168. [DOI] [PubMed] [Google Scholar]
- 18.Shah A, Ganesvaran T. Suicide among psychiatric in-patients with schizophrenia in an Australian mental hospital. Med Sci Law. 1999;39:251–9. doi: 10.1177/002580249903900311. [DOI] [PubMed] [Google Scholar]
- 19.Taiminen TJ. Effect of psychopharmacotherapy on suicide risk in psychiatric inpatients. Acta Psychiatr Scand. 1993;87:45–7. doi: 10.1111/j.1600-0447.1993.tb03328.x. [DOI] [PubMed] [Google Scholar]
- 20.Sharma V, Persad E, Kueneman K. A closer look at inpatient suicide. J Affect Disord. 1998;47:123–9. doi: 10.1016/s0165-0327(97)00131-6. [DOI] [PubMed] [Google Scholar]
- 21.Steblaj A, Tavcar R, Dernovsek MZ. Predictors of suicide in psychiatric hospital. Acta Psychiatr Scand. 1999;100:383–8. doi: 10.1111/j.1600-0447.1999.tb10882.x. [DOI] [PubMed] [Google Scholar]
- 22.King EA, Baldwin DS, Sinclair JM, Campbell MJ. The Wessex recent in-patient suicide study, 2.Case-control study of 59 in-patient suicides. Br J Psychiatry. 2001;178:537–42. doi: 10.1192/bjp.178.6.537. [DOI] [PubMed] [Google Scholar]
- 23.Gaertner I, Gilot C, Heidrich P, Gaertner HJ. A case control study on psychopharmacotherapy before suicide committed by 61 psychiatric inpatients. Pharmacopsychiatry. 2002;35:37–43. doi: 10.1055/s-2002-25027. [DOI] [PubMed] [Google Scholar]
- 24.Dong JY, Ho TP, Kan CH. A case-control study of 92 cases of in-patient suicides. J Affect Disord. 2005;87:91–9. doi: 10.1016/j.jad.2005.03.015. [DOI] [PubMed] [Google Scholar]
- 25.Yip PS, Callanan C, Yuen HP. Urban/rural and gender differentials in suicide rates: East and West. J Affect Disord. 2000;57:99–106. doi: 10.1016/s0165-0327(99)00058-0. [DOI] [PubMed] [Google Scholar]
- 26.Patel V, Ramasundarahettige C, Vijayakumar L, Thakur JS, Gajalakshmi V, Gururaj G, et al. Suicide mortality in India: A nationally representative survey. Lancet. 2012;379:2343–51. doi: 10.1016/S0140-6736(12)60606-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hirsch JK. A review of the literature on rural suicide: Risk and protective factors, incidence, and prevention. Crisis. 2006;27:189–99. doi: 10.1027/0227-5910.27.4.189. [DOI] [PubMed] [Google Scholar]
- 28.Copas JB, Robin A. Suicide in psychiatric in-patients. Br J Psychiatry. 1982;141:503–11. doi: 10.1192/bjp.141.5.503. [DOI] [PubMed] [Google Scholar]
- 29.Qin P, Nordentoft M. Suicide risk in relation to psychiatric hospitalization: Evidence based on longitudinal registers. Arch Gen Psychiatry. 2005;62:427–32. doi: 10.1001/archpsyc.62.4.427. [DOI] [PubMed] [Google Scholar]
- 30.Hunt IM, Kapur N, Webb R, Robinson J, Burns J, Turnbull P, et al. Suicide in current psychiatric in-patients: A case-control study The national confidential inquiry into suicide and homicide. Psychol Med. 2007;37:831–7. doi: 10.1017/S0033291707000104. [DOI] [PubMed] [Google Scholar]
- 31.Meehan J, Kapur N, Hunt IM, Turnbull P, Robinson J, Bickley H, et al. Suicide in mental health in-patients and within 3 months of discharge. National clinical survey. Br J Psychiatry. 2006;188:129–34. doi: 10.1192/bjp.188.2.129. [DOI] [PubMed] [Google Scholar]
- 32.Erlangsen A, Zarit SH, Tu X, Conwell Y. Suicide among older psychiatric inpatients: An evidence-based study of a high-risk group. Am J Geriatr Psychiatry. 2006;14:734–41. doi: 10.1097/01.JGP.0000225084.16636.ec. [DOI] [PubMed] [Google Scholar]
- 33.Høyer EH, Licht RW, Mortensen PB. Risk factors of suicide in inpatients and recently discharged patients with affective disorders. A case-control study. Eur Psychiatry. 2009;24:317–21. doi: 10.1016/j.eurpsy.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 34.Wood D, Pistrang N. A safe place? Service users' experiences of an acute mental health ward. J Community Appl Soc Psychol. 2004;14:16–28. [Google Scholar]
- 35.Leach MJ. Rapport: A key to treatment success. Complement Ther Clin Pract. 2005;11:262–5. doi: 10.1016/j.ctcp.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 36.Isometsa ET, Lonnqvist J. Suicide in major depression. In: Botsis JA, Soldatos CR, Stefanis CN, editors. Suicide: Biopsychosocial Approaches. Amsterdam: Elsevier; 1997. [Google Scholar]
- 37.Möller HJ. Suicide, suicidality and suicide prevention in affective disorders. Acta Psychiatr Scand. 2003;108(Suppl 418):73–80. [PubMed] [Google Scholar]
- 38.Vijayakumar L, Phillips MR, Silverman MM, Gunnell D, Carli V. Suicide. In: Patel V, Chisholm D, Dua T, Laxminarayan R, Medina-Mora ME, editors. Mental, Neurological, and Substance Use Disorders: Disease Control Priorities. 3rd ed. Vol. 4. Washington, DC: The International Bank for Reconstruction and Development/The World Bank; 2016. pp. 163–81. [PubMed] [Google Scholar]
- 39.Brown GK, Beck AT, Steer RA, Grisham JR. Risk factors for suicide in psychiatric outpatients: A 20-year prospective study. J Consult Clin Psychol. 2000;68:371–7. [PubMed] [Google Scholar]
- 40.Madsen T, Agerbo E, Mortensen PB, Nordentoft M. Predictors of psychiatric inpatient suicide: A national prospective register-based study. J Clin Psychiatry. 2012;73:144–51. doi: 10.4088/JCP.10m06473. [DOI] [PubMed] [Google Scholar]
- 41.Verrocchio MC, Carrozzino D, Marchetti D, Andreasson K, Fulcheri M, Bech P. Mental pain and suicide: A systematic review of the literature. Front Psychiatry. 2016;7:108. doi: 10.3389/fpsyt.2016.00108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Modestin J, Schwarzenbach F. Effect of psychopharmacotherapy on suicide risk in discharged psychiatric inpatients. Acta Psychiatr Scand. 1992;85:173–5. doi: 10.1111/j.1600-0447.1992.tb01464.x. [DOI] [PubMed] [Google Scholar]
- 43.Neuner T, Hübner-Liebermann B, Haen E, Hausner H, Felber W, Wittmann M. AGATE. Completed suicides in 47 psychiatric hospitals in Germany – Results from the AGATE-study. Pharmacopsychiatry. 2011;44:324–30. doi: 10.1055/s-0031-1284428. [DOI] [PubMed] [Google Scholar]
- 44.Large MM, Ryan CJ. Disturbing findings about the risk of suicide and psychiatric hospitals. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1353–5. doi: 10.1007/s00127-014-0912-2. [DOI] [PubMed] [Google Scholar]
- 45.Sakinofsky I. Preventing suicide among inpatients. Can J Psychiatry. 2014;59:131–40. doi: 10.1177/070674371405900304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vijayakumar L, Rajkumar S. Are risk factors for suicide universal? A case-control study in India. Acta Psychiatr Scand. 1999;99:407–11. doi: 10.1111/j.1600-0447.1999.tb00985.x. [DOI] [PubMed] [Google Scholar]
- 47.Hunt IM, Bickley H, Windfuhr K, Shaw J, Appleby L, Kapur N. Suicide in recently admitted psychiatric in-patients: A case-control study. J Affect Disord. 2013;144:123–8. doi: 10.1016/j.jad.2012.06.019. [DOI] [PubMed] [Google Scholar]


