Abstract
Background
General anesthesia does not block central nervous processing of auditive information. Therefore, positive suggestions even given during surgery might have the potential to encourage well-being and recovery of patients.
Aim of this review was to summarize the evidence on the efficacy of therapeutic suggestions under general anesthesia in adults undergoing surgery compared to an attention control (i.e. white noise).
Methods
We included randomized controlled trials that investigated therapeutic suggestions presented during general anesthesia to adult patients undergoing surgery or medical procedures. Outcomes on pain intensity, mental distress, recovery, use of medication, measured postoperatively within hospitalization were considered. Electronic searches were carried out in the following databases (last search February 23, 2015): MEDLINE, CENTRAL, Web of Science, PsycINFO, ProQuest Dissertations and Theses.
Results
Thirty-two eligible randomized controlled trials were included, comprising a total of 2102 patients. All studies used taped suggestions. Random effects meta-analyses revealed no effects on pain intensity (Hedges’ g = 0.04, CI 95% [−0.04; 0.12], number needed to treat [NNT] = 44.3) and mental distress (g = 0.03, CI 95% [−0.11; 0.16], NNT = 68.2). In contrast, we found small but significant positive effects on use of medication (g = 0.19, CI 95% [0.09; 0.29], NNT = 9.2) and on recovery (g = 0.14, CI 95% [0.03; 0.25], NNT = 13.0). All effects were homogeneous and robust.
Conclusions
Even though effects were small, our results provide indications that intraoperative suggestions can have the potential to reduce the need for medication and enhance recovery. Further high quality trials are needed to strengthen the promising evidence on the efficacy of therapeutic suggestions under general anesthesia for patients undergoing surgery.
Electronic supplementary material
The online version of this article (doi:10.1186/s12871-016-0292-0) contains supplementary material, which is available to authorized users.
Keywords: Therapeutic suggestions; Anesthesia, general; Efficacy, treatment; Meta-analysis
Background
Recovery from anesthesia and surgery is often hampered by side effects such as pain or postoperative nausea and vomiting (PONV), by disturbances of well-being and even complications. Pain and PONV are usually prevented and treated by medications that carry their own side effects. Other challenges such as anxiety, hopelessness and negative expectations further impair recovery and outcome [1], or lead to nocebo effects [2] which usually cannot be treated with drugs and call for non-pharmacological approaches.
Among psychological interventions to improve recovery and well-being hypnotherapeutic approaches are most effective [3]. Several meta-analyses show small to large effect sizes of therapeutic suggestions given pre- or postoperatively with or without hypnosis induction on various outcomes [3–6].
Some of the studies included suggestions presented during general anesthesia to the unconscious patient [5, 6]. In this context, suggestions are defined “as verbal or nonverbal messages that the receiver involuntarily accepts and follows” [7] and that might affect emotions, behavior and autonomous body functions. This approach is based on the consideration that anesthesia does not interrupt perception of sounds and words by the brain [8]. Intraoperative measurement of auditory evoked potentials has shown that the central auditory pathway remains intact during general anesthesia [9, 10]. Even further processing of words in the central nervous system including development of memory and appropriate responses has been demonstrated by postoperative recognition of intraoperatively presented words [11, 12], and postoperative nonverbal responses to instructions given during anesthesia [13–15]. In some cases, intraoperative awareness occurs under general anesthesia with explicit memory of the situation and of conversations [16]. In addition, the occurrence of implicit memory has been proven much more frequently [17]. Moreover, strong impact of negative intraoperative remarks on prognosis has been reported [18, 19].
One meta-analysis so far investigated the efficacy of therapeutic suggestions presented during general anesthesia to encourage well-being and recovery of surgical patients and has found mixed results [20]. Even though the effect on postoperative hospitalization was not statistically significant, the small positive effect of suggestions on patient-controlled analgesia reached statistical significance. However, these results must be interpreted with caution since a) the inclusion of non-randomized trials threatens the validity of meta-analytic results and b) the effects on patient-controlled analgesia are based on four studies only.
Hence, the present meta-analysis investigates the efficacy of therapeutic suggestions under general anesthesia on surgically relevant postoperative outcomes, i.e., pain intensity, mental distress, recovery, or the use of medication, and intraoperative outcomes, i.e., length of procedure and physiological parameters, by including randomized controlled trials only.
Methods
Objectives, inclusion criteria, and methods have been pre-specified in a review protocol [21].
Identification and selection of studies
Eligible studies were randomized controlled trials that investigated therapeutic suggestions presented during general anesthesia to adult patients undergoing surgery or medical procedures. If the intervention group received a combination of therapeutic suggestions and another psychological intervention or if therapeutic suggestions were not solely implemented intraoperatively, the study was excluded. Eligible control groups were “treatment as usual” (defined as the standard surgical care policy of the hospital) and “attention control” groups (defined as providing same amount of time and attention in addition to standard surgical care; e.g., blank tape, white noise). The included trials reported on at least one of the following outcomes measured via self- and/or observer reports: pain intensity, mental distress, recovery, use of medication, measured postoperatively within hospitalization. In addition, intraoperative outcomes, i.e., length of procedure and physiological parameters, were included (Additional file 1: Table S1).
Deviating from the protocol [21], we did not limit study inclusion to trials with a sample size of at least 20 participants in each trial arm, but rather tested this restriction in sensitivity analyses.
Electronic searches were carried out in the following databases (last search February 23, 2015): MEDLINE, CENTRAL, Web of Science, PsycINFO according to a search strategy that specified terms referring to the patient population (e.g., surg$.ti.ab.kw, General Surgery/, Anesthesia. General/), treatment (e.g., suggestion$.ti.ab.kw, Suggestion/), and study design (e.g., randomized controlled trial.pt). The search strategy was developed with consideration of validated search strategies for retrieving randomized controlled trials [22]. The MEDLINE search strategy is shown in Appendix. We adapted the strategy for the Cochrane Central Register of Controlled Trials (CENTRAL), Web of Science and PsycINFO.
In order to identify further trials, lists of references of relevant articles and previous reviews were also checked. Additionally, we screened ProQuest Dissertations and Theses Full Text Database to identify any unpublished material. One author (DJ) screened titles and abstracts of database records and retrieved full texts for eligibility assessment.
Data extraction and management
A pilot-tested data extraction form was used to collect the following information from eligible trials: characteristics of patients, intervention, control group, outcomes, bibliographic information, and effect size related data.
Data were independently extracted by two raters (DJ, JR). Inter-rater disagreement was resolved through consensus. In case of missing information, study authors were contacted. If information on effect sizes was missing and could not be retrieved, data had to be approximated using different estimation methods (e.g., estimating statistics from graphs without numerical data, setting an effect size to zero if non-significant results were mentioned without reporting statistical parameters).
Assessing the risk of bias in included studies
To assess risk of bias in the included studies, common markers of internal validity from the Cochrane Risk of Bias Tool were extracted [23]. The risk of bias assessment was conducted by two independent raters (DJ, SK) who were previously trained and blinded to extracted effect size estimates. Disagreements were resolved by discussion with one author (JR). Inter-rater agreement for the risk of bias assessment using Cohen’s kappa (κ) was excellent, κ = 0.76 [24].
Summary measures
Corrected standardized mean differences (Hedges’ g) were calculated for each assessment time-point and measurement multiplied by a small sample bias correction factor [25]. An effect size of 0.5 thus indicates that the mean of the experimental group is half a standard deviation larger than the mean of the control group. The magnitude of Hedges’ g was interpreted within the same ranges as Cohen’s d, regarding 0.20, 0.50, and 0.80 as small, medium, and large effect sizes, respectively [26]. Since such effect sizes are generally not easy to interpret in terms of clinical significance, effect sizes Hedges’ g were transformed into numbers needed to treat (NNT) [27]. For all dichotomous outcomes, Log Odds Ratios were computed and converted to Hedges’ g [28] in order to pool across different effect size formats.
If a study comprised more than one intervention group [29–31] the shared control group was divided out approximately evenly among the comparisons [32].
Data synthesis
Outcome data were meta-analyzed using a random-effects approach. The generic inverse variance method was applied with heterogeneity estimated using the DerSimonian-Laird method [33]. Statistical heterogeneity between trials was assessed with χ2 heterogeneity tests (Cochran’s Q) and I2 statistic [34]. I2 describes the percentage of the variability in effect estimates that is due to heterogeneity rather than chance, with values from 0 to 40% indicating no important heterogeneity, 30 to 60% moderate, 50 to 90% substantial, and 75 to 100% considerable heterogeneity, respectively [35].
Risk of bias across studies
In order to test for publication bias funnel plots were inspected visually and the Egger test was run [36]. Additionally, Duval & Tweedie’s trim and fill procedure was used to obtain an adjusted estimate of the treatment effect after the publication bias had been taken into account and to indicate how many missing trials have been imputed to correct for publication bias [37].
Additional analyses
We conducted sensitivity analyses in order to test the robustness of findings, examining if meta-analytic results change when excluding approximated effect sizes and when excluding small samples (n ≤ 20 per group). Moderator analyses were planned to explain statistical heterogeneity [38]. However, heterogeneity was not important (I2 < 40%). Therefore, we conducted stratified analyses in order to exploratory examine potential moderators.
All data analyses were performed using Comprehensive Meta-Analysis (CMA; Version 2.0; Biostat Inc.).
Results
Study selection
A total of 7427 records was screened and N = 32 randomized controlled trials were included in the meta-analysis. Figure 1 contains a flow chart of the study selection process.
Fig. 1.
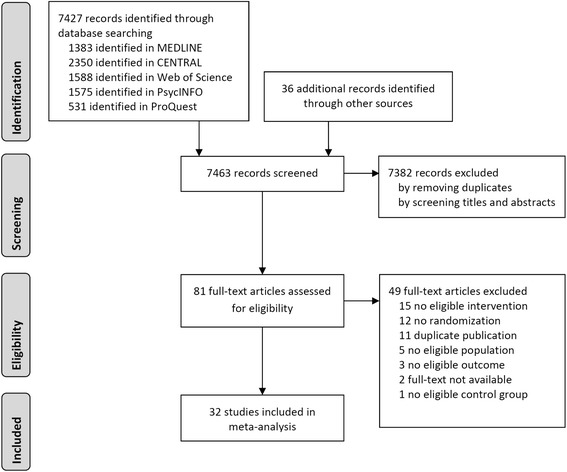
Flow chart of the study selection process
Description of included studies
Table 1 presents selected study characteristics. The majority of primary studies were published between 1986 and 2001; only one study [39] was published much earlier. Among the primary studies, there were three unpublished dissertations. One study was reported in German [40], all others were written in English. Altogether, n = 32 randomized controlled trials provided k = 37 comparisons between an intervention and a control group, incorporating a total of n = 1111 patients in intervention groups (M = 30.0, SD = 18.2) and n = 991 patients in control groups (M = 31.0, SD = 18.1). The mean age of patients in the intervention groups was 47.7 years (SD = 8.2), similarly in the control groups 47.2 years (SD = 9.4). The mean percentage of male patients was 17% (SD = 28.1) in intervention groups, and 17% (SD = 29.3) in control groups as well. This low percentage of male patients can be ascribed to a high proportion of studies including patients undergoing gynecological surgery; 16 primary studies investigated female patients only. In the majority of primary studies anesthesia was performed as “balanced anesthesia” with an opioid and an inhalational anesthetic (Table 1). In six studies, neuroleptanesthesia was used and in two studies total intravenous anesthesia (TIVA) with propofol or midazolam, respectively. Nitrous oxide was included in all except one study. In seven studies a benzodiazepine was applied for premedication. Therapeutic suggestions were presented via tape in all studies, played throughout the surgery in almost every study. Suggestion were judged as affirmative (e.g., “You will feel fine after the operation.”) in 12 intervention groups (32%), as non-affirmative (e.g., “After the operation you will not feel any nausea.”) in one (3%), and both affirmative and non-affirmative in 14 intervention groups (38%; no information reported for 10 intervention groups). In 19 intervention groups (51%), suggestion were accompanied by or alternated with soothing music or sounds. In all studies, the effects of therapeutic suggestions were compared against attention control. 18 studies (56%) used blank tapes/white noise, 7 studies (22%) offered sounds or music, and another 7 studies used spoken text (history of hospital, story of Peter Pan, parts of a cookery book) as control condition.
Table 1.
Characteristics of the included studies
| First author (publication year) | Country | Surgical procedure | Description of therapeutic suggestions a | n | Description of control group | n | Anesthesia | Outcomes |
|---|---|---|---|---|---|---|---|---|
| Bethune et al. (1993) [47] | UK | Coronary artery bypass grafting | Positive; based on text used by Evans & Richardson (1988) [48]; music at the beginning | 16 | Blank tape with musical leader | 17 | I | Mental distress (mood, anxiety) Pain intensity Recovery (nausea, mobility, general recovery) Length of procedure |
| Block et al. (1991) [15] | USA | Operation on the fallopian tubes, vertical banding gastroplasty, total abdominal hysterectomy, ovarian cystectomy, cholecystectomy, myomectomy | Smooth, rapid recovery during a short post-operative stay; no pain, nausea or vomiting; rapid return of bowel and bladder function; rapid healing and mobility; comfort; relaxation; good appetite, sleep, mood, and feeling | 109 | Blank tape | 100 | I | Medication (antiemetics, Analgesics) Length of procedure |
| Boeke et al. (1988) [49] | NL | Elective cholecystectomy | Relaxation, wellbeing, pleasant feeling in every respect, absence of nausea and vomiting, good recovery; with seaside sounds | 24 | Nonsense suggestions with seaside sounds | 26 | N | Mental distress (well-being) Pain intensity Recovery (nausea, general recovery) Length of procedure Physiological parameters (blood loss) |
| Bonke et al. (1986) [50] | NL | Biliary tract surgery | Relaxation, well-being, comfortable feelings in every respect, lack of nausea or vomiting, no difficulty with bladder function or bowel movement, rapid recovery | 31 | Monotonous low-frequency noise, resembling the sound of a vacuum cleaner | 30 | N | Mental distress (well-being, relaxation) Pain intensity Medication (analgesics) Recovery (PONV, general recovery) Length of procedure Physiological parameters (blood loss) |
| Caseley-Rondi et al. (1994) [51] | Canada | Elective total abdominal hysterectomy and/or bilateral salpingo oophorectomy | Simple and positive; alternating with Japanese melodies | 48 | Blank tape alternating with Japanese melodies | 48 | I | Mental distress (mood, anxiety) Pain intensity Medication (analgesics) Recovery (nausea, general recovery) |
| Cowan et al. (2001) [52] | USA | Bariatric surgical patients | Positive; cognitive-behavioural approach: reinforcement of information received preoperatively, encouragement of performance of recovery regimes, positive interactions with personnel, improved self-image, relaxation | 10 | Blank tape | 17 | I | Recovery (turning, coughing, breathing, mobility) |
| Dawson et al. (2001) [29] | UK | Total abdominal hysterectomy with/without bilateral salpingo oophorectomy | (1) No pain (2) No sickness (3) No sickness, no pain |
35 34 34 |
White noise | 35 | N (no N2O) | Pain intensity Medication (antiemetics, analgesics) Recovery (PONV) Length of procedure |
| De Houwer et al. (1996) [53] | Belgium | Coronary artery bypass grafting | Relaxation, fast recovery; based on Bonke et al. (1986) [50]; with background relaxing music | 19 | Blank tape | 21 | T | Mental distress (mood, anxiety) Recovery (general recovery) Length of procedure Physiological parameters (blood pressure, noradrenalin, adrenalin) |
| Eberhart et al. (1998) [54] | Germany | Thyroidectomy | Smooth postoperative recovery; relaxation, security, absence of nausea and vomiting | 36 | Blank tape | 35 | N | Medication (antiemetics, analgesics) Recovery (PONV) Length of procedure |
| Evans & Richardson (1988) [48] | UK | Total abdominal hysterectomy | Direct (no sickness, no pain), third person (operation is going very well and the patient is fine), description of normal postoperative procedures and coping advices | 19 | Blank tape | 20 | I | Mental distress (anxiety, mood) Pain intensity Recovery (PONV, pyrexia, bowel difficulties, flatulence, mobility, micturation, general recovery, complications) Length of procedure Physiological parameters (blood loss) |
| Furlong (1990) [55] | USA | Abdominal gynecological surgery | Positive | 10 | Blank tape | 9 | I | Mental distress (mood) Medication (analgesics) Length of procedure |
| Furlong & Read (1993) [56] | USA | Gynecological surgery or mastectomy | Positive; with background music | 52 | Blank tape | 56 | I | Mental distress (anxiety) Pain intensity Medication (analgesics) Recovery (PONV, mobility, bowel difficulties, micturition, wound healing) |
| Jelicic et al. (1993) [30] | NL | Cholecystectomy | (1) Affirmative (relaxation, comfort, quick healing) and non-affirmative (absence of tension, nausea); alternating with seaside sounds (2) Affirmative (3) Non-affirmative |
21 20 20 |
Irrelevant text, i.e. excerpts from a cookery book | 21 | N | Mental distress (well-being) Length of procedure Physiological parameters (blood loss) |
| Korunka et al. (1992) [40] | Austria | Hysterectomy | Positive; followed by indirect (general wellbeing, absence of pain) | 55 | Operation sounds | 53 | I | Pain intensity Medication (analgesics) Length of procedure |
| Lebovits et al. (1999) [57] | USA | Elective hernia repair | Positive postoperative course, well-being and relaxation, minimal side effects, no difficult voiding, minimal discomfort such as sore throat, muscle aches and emetic symptoms; requirement of minimal pain medication | 34 | History of hospital | 36 | T | Pain intensity Medication (analgesics) Recovery (PONV, side effects) Length of procedure |
| Liu et al. (1992) [58] | UK | Total abdominal hysterectomy | Affirmative and non-affirmative (comfort and rapid recovery; absence of pain or feelings of sickness) | 24 | History of hospital | 25 | I | Mental distress (mood) Pain intensity Medication (analgesics) Recovery (nausea, pyrexia, wound healing, mobility, flatulence) Length of procedure Physiological parameters (blood loss) |
| Liu et al. (1993) [59] | UK | Surgical repair of fractured neck of femur | Positive (relating to comfort, mobility, nausea, general recovery and discharge after surgery) | 58 | History of hospital | 61 | GA | Pain intensity Medication (analgesics, antiemetics) Recovery (ADL, mobility, pyrexia) |
| Maroof et al. (1997) [60] | Saudi Arabia | Elective abdominal hysterectomy | Positive (good progress, well-being after surgery, absence of sickness) | 25 | Blank tape | 25 | I | Medication (antiemetics) Recovery (PONV, fluid replacement) Length of procedure |
| Mastropietro (1998) [31] | USA | Open gynaecological procedures through a midline incision | (1) Synchronized with soothing music presented when stress test was positive (comfortable, relaxed intraoperative and postoperative experience) (2) Randomly presented with soothing music (comfortable, relaxed intraoperative and postoperative experience) |
24 | ||||
| McLintock (1990) [61] | UK | Elective abdominal hysterectomy by Pfannenstiel’s incision | Positive (positive progress, feelings of warmth, comfort, calmness and relaxation; absence of pain) | 30 | Blank tape | 30 | I | Pain intensity Medication (analgesics) Recovery (PONV) |
| McWilliams (1990) [62] | USA | Lumbar laminectomy surgery | Suggestions interspersed with environmental sounds | 30 | Environmental sounds alone | 30 | GA | Medication (analgesics, antiemetics) Recovery (general recovery) |
| Melzack et al. (1996) [63] | Canada | Cholecystectomy or hyterectomy | Positive; regarding the recovery process (e.g., feeling fine, mild pain only); interspersed with music | 10 | Excerpts from physiology book | 10 | I | Pain intensity Length of procedure |
| Moix et al. (1996) [64] | Spain | Abdominal hysterectomy | Affirmative (feeling of relaxation during surgery, good progress, easy and rapid recovery, rapid mobility, comfort, good appetite, digestion, micturition, sleep and mood) | 14 | Monotonous sounds | 13 | I | Pain intensity Medication (analgesics) Recovery (vomiting, pyrexia, digestion, appetite, sleep, bowel function, general recovery, micturition, complications) Length of procedure Physiological parameters (blood pressure, heart rate) |
| Münch & Zug (1990) [65] | Germany | Thyroidectomy | General (comfort and well-being), direct (relaxing and feeling well, no vomiting, no nausea, only little pain); classical music played in a modern fashion | 18 | Blank tape | 18 | N | Mental distress (well-being) Pain intensity Recovery (PONV) Length of procedure |
| Nilsson et al. (2001) [66] | Sweden | Hysterectomy | Relaxing and encouraging; music (relaxing and calming; accompanied by soothing sounds of sea waves) | 31 | Operation room sounds | 28 | I | Mental distress (well-being) Pain intensity Medication (analgesics) Recovery (nausea, fatigue, mobility) Length of procedure Physiological parameters (blood loss) |
| Oddby-Muhrbeck et al. (1995) [67] | Sweden | Elective breast surgery | Affirmative (safe atmosphere, quick recovery, feelings of hunger and thirst) | 35 | Low electronic sound set | 35 | I | Pain intensity Medication (analgesics) Recovery (PONV, general recovery) Length of procedure Physiological parameters (blood loss) |
| Pearson (1961) [39] | USA | Thyroidectomy, gastrectomy, hernia repair, hysterectomy, pelvic laparoscopy, vein stripping | In a permissive manner (relaxation and selfresponsibility of the patient for the course of recovery) | 43 | Blank tape | 38 | GA | Medication (analgesics) Recovery (general recovery) |
| Rosenberg (1992) [68] | USA | Hysterectomy, myomectomy, other gynaecological procedures, cholecystectomy | Positive (smooth, comfortable, and rapid recovery, absence of sickness and pain), procedural/ sensory information about course of surgery and recovery; imagery, recommendations for dealing with postoperative events and sensations | 33 | Blank tape | 32 | I | Mental distress (anxiety) Pain intensity Medication (analgesics, antiemetics) Recovery (mobility, pyrexia, micturation) Length of procedure |
| Steinberg et al. (1993) [69] | USA | Total abdominal hysterectomy or breast reconstruction by transverse rectus abdominus musculocutaneous reconstruction flap | Positive (relating to nausea and anxiety) | 30 | Blank tape | 30 | I | Mental distress (anxiety) Pain intensity Medication (analgesics) Recovery (PONV) |
| van der Laan et al. (1996) [70] | USA | Hysterectomy, myomectomy, gynecologic laparotomy | Nonspecific affirmative (feelings of relaxation and security) | 20 | Story of Peter Pan | 20 | I | Mental distress (anxiety) Pain intensity Medication (analgesics) Recovery (nausea) Length of procedure |
| Williams et al. (1994) [42] | UK | Major gynaecological surgery | Positive (smooth and uncomplicated progress of surgery, well-being after surgery, absence of sickness) | 22 | Blank tape | 29 | I | Medication (analgesics) Recovery (PONV, fluid replacement) Length of procedure Physiological parameters (blood loss) |
| Woo et al. (1987) [71] | USA | Hysterectomy | Positive (rapid recovery) | 7 | Ocean sounds | 7 | I | Medication (analgesics) |
NL Netherlands, I inhalation anesthesia, N neuroleptanesthesia, T intraveneous anesthesia, GA general anesthesia (not specified), PONV postoperative nausea and vomiting; a as reported in primary study
Additional file 2: Table S2 contains information on the risk of bias in included studies. Overall, the risk of bias in the included studies was mainly judged as low; no study indicated a high risk of bias in any quality item. However, due to missing information in the studies a high percentage of items was judged as unclear.
Meta-analytic results
Across all included postoperative outcomes, there was a small, but statistically significant and homogeneous effect of therapeutic suggestions compared to attention control (g = 0.13, 95% CI [0.04; 0.23], k = 37, p = .005; I2 = 0%).
When outcomes were analyzed separately, we found effects of therapeutic suggestions on pain intensity (g = 0.04, CI 95% [−0.04; 0.12], NNT = 44.3) and mental distress (g = 0.03, CI 95% [−0.11; 0.16], NNT = 68.2) to be close to zero and non-significant. However, small significant effects in favor of therapeutic suggestions appeared on medication use (g = 0.19, CI 95% [0.09; 0.29], NNT = 9.2) and on recovery (g = 0.14, CI 95% [0.03; 0.25], NNT = 13.0). Stratifying analyses on medication use and recovery with respect to outcomes, we found small, significant effects for therapeutic suggestions on PONV (g = 0.21, CI 95% [0.07; 0.36], NNT = 8.3) and analgesic use (g = 0.16, CI 95% [0.06; 0.26], NNT = 11.0). Therapeutic suggestions also revealed a small effect on antiemetic use (g = 0.22, CI 95% [−0.003; 0.45], NNT = 7.9) and on all other recovery outcomes (g = 0.11, CI 95% [−0.01; 0.24], NNT = 15.6), even though these effects were marginally significant only (Figs. 2, 3, and 4). Heterogeneity for all outcomes was not important (I2 < 40%).
Fig. 2.
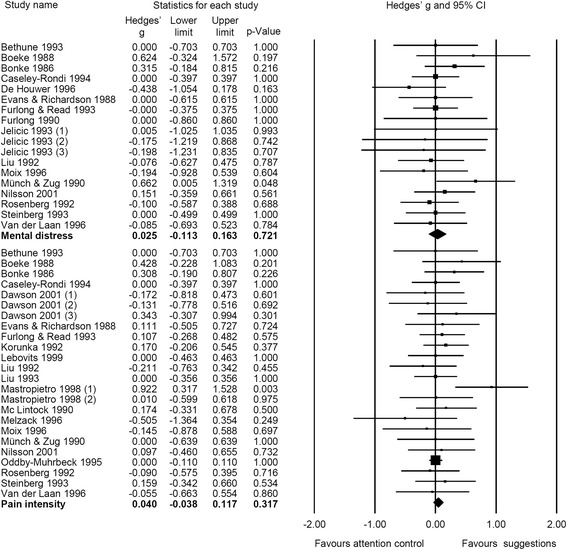
Forest plot of meta-analytic results for mental distress and pain intensity
Fig. 3.
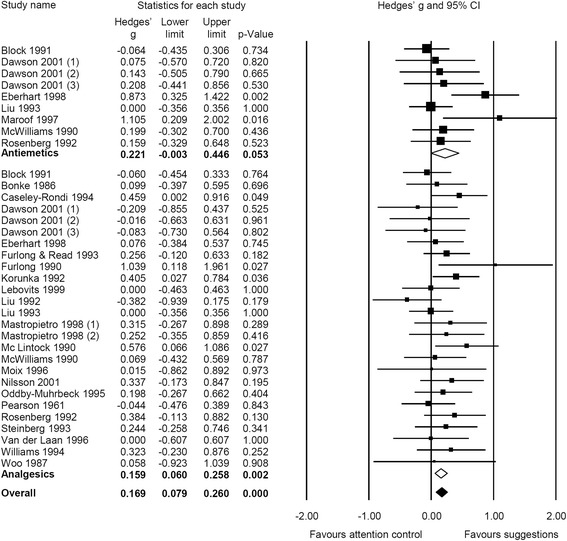
Forest plot of meta-analytic results for medication, stratified for use of antiemetics and analgesics
Fig. 4.
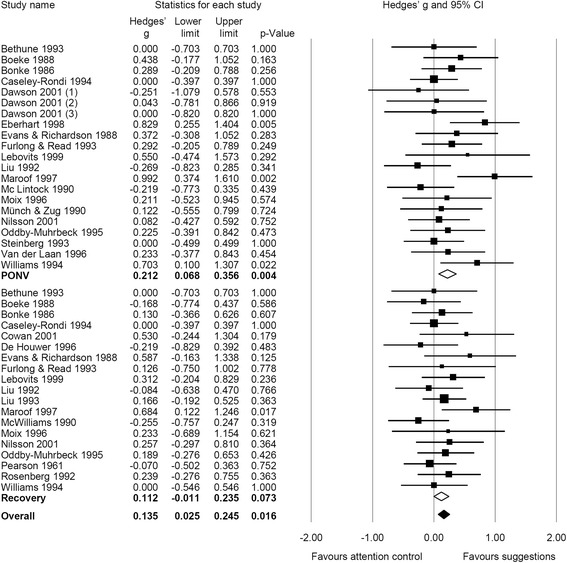
Forest plot of meta-analytic results for recovery, stratified for postoperative nausea and vomiting (PONV) and recovery (all other outcomes)
Regarding intraoperative outcomes, therapeutic suggestions revealed a small effect on physiological parameters, even though this effect was not significant (g = 0.13, CI 95% [−0.16; 0.42], k = 12, p = .389; I2 = 62%). Effects of therapeutic suggestions on length of surgical procedure (g = −0.04, CI 95% [−0.14; 0.07], k = 28, p = .499; I2 = 0%) were close to zero and non-significant.
Publication bias
A visual inspection of the funnel plot (see Additional file 3: Figure S1) gave no indication of publication bias as trials are distributed symmetrically around the pooled effect size. Egger’s test of funnel plot asymmetry did not indicate publication bias (t(35) = 0.18; p = .428), and Duval & Tweedie’s trim and fill procedure resulted in no trimmed studies. Hence, publication bias does not pose a threat to the accuracy of our meta-analytic results.
Additional analyses
We tested the robustness of effects for primary outcomes. After excluding approximated effect sizes for all outcome categories the meta-analytic result patterns (size of effect estimates and significance) did not change considerably though effect sizes were slightly larger and reached significance for recovery. Furthermore, effects were robust against the exclusion of small samples (n ≤ 20 per group) yielding effect sizes comparable in size and (non-)significance (Additional file 4: Table S3).
Since heterogeneity was not important at all (I2 < 40%), we did not run our pre-specified subgroup analyses. However, in order to get some ideas about potential moderators we exploratory conducted stratified analyses for PONV and antiemetic use since for all other postoperative outcomes results were homogeneous (I2 = 0%). Studies applying suggestions related to the absence of PONV (e.g., “no sickness”) yielded larger effects than studies without such suggestions, but this difference was not significant for both outcomes. There was no indication of an association between treatment effects and affirmativity of suggestions. Furthermore, studies using neuroleptanesthesia did not differ from those with intravenous or inhalation anesthesia.
Stratifying the analyses according to risk of bias, we only found differences with respect to handling of incomplete outcome data which were significant by trend for PONV (p = .061) with studies evaluated as low risk bias yielding smaller effects than studies judged as unclear risk of bias. Random sequence generation had no influence of treatment effects (Additional file 5: Table S4).
Discussion
The present meta-analysis aimed at evaluating the efficacy of therapeutic suggestions presented during general anesthesia to patients undergoing surgery or medical procedures. Currently, the efficacy of therapeutic suggestions applied under general anesthesia has been investigated on hospitalization and patient-controlled analgesia exclusively. Our meta-analysis expands this knowledge by adding results on pain intensity, mental distress, use of medication, and recovery.
We found small, significant positive effects of therapeutic suggestions on recovery and medication use which proved to be robust and free of publication bias. When analyzing outcomes in more detail, highest effects were found for PONV and analgesic use. Comparable results of therapeutic suggestions on the amount of morphine administered via patient-controlled analgesia were also reported in the meta-analysis of Merikle and Daneman [20]. However, there was no effect of therapeutic suggestions on pain intensity or mental distress.
One reason for the small or even zero effects might be the level of awareness. Usually, therapeutic suggestions were given during general anesthesia excluding the induction of anesthesia and emergence from anesthesia that are most sensitive to intraoperative awareness [16]. Another reason could be that when suggestions are presented via tape only, rapport and therapeutic relationship are missing, which are essential components of effective hypnosis or therapeutic suggestions [4, 8]. Accordingly, higher effect sizes of suggestions to reduce postoperative side effects spoken live compared to taped suggestions were reported [5, 6].
Since study effects were quite homogeneous, we merely ran stratified analyses on PONV and antiemetic use to get an idea about potential moderators of treatment effects. In this regard, the specificity of suggestions seems to have an influence on its efficacy since studies with specific PONV related suggestions yielded significant results on PONV, while studies with unspecific suggestions only resulted in non-significant effects. Thus, our results go along with studies demonstrating an impact of suggestion specificity on its efficacy [6].
Differences in anesthesia methods did not influence the efficacy of therapeutic suggestions, although neuroleptanesthesia is known to carry a higher risk of intraoperative awareness and lower interference with memory in comparison to balanced anesthesia with inhalational or intravenous anesthetics [16]. However, intraoperative awareness and memory are not considered a pre-requisite for effects of suggestions in unconscious patients [41, 8].
When interpreting these results the exploratory nature of the respective analyses should be considered. Although research on the impact of affirmativity and specificity of therapeutic suggestions on postoperative outcomes is available [6, 29, 30, 42] this issue has not been clarified conclusively. Studies examining the most efficacious phrasing of suggestions are still pending; an optimization of therapeutic suggestions is possible and needed.
Several limitations of the present meta-analysis are noteworthy. First, we excluded studies with children and studies where pre- or postoperative suggestions were presented in addition to those given intraoperatively. Both restrictions of inclusion might have led to smaller effects of suggestions during general anesthesia. There is some evidence of a higher level of efficacy of suggestive techniques in children [5], partly due to their higher suggestibility [43]. Moreover, meta-analytic findings have shown that suggestions are more effective when delivered at least in part prior to the medical procedure rather than solely during the medical procedure [5].
Second, the reporting quality, i.e. completeness and transparency, of the included studies was rather low making it difficult to adequately evaluate potential risks of bias. Particularly, methods of randomization and allocation concealment have been reported inadequately in the majority of studies, whereas blinding of participants, personnel, and outcome assessors was reported well. From the information on the anesthesia methods provided in the included studies no conclusion can be drawn on the precise depth of anesthesia and its impact on the results, besides that standard procedures were used without techniques to control depth, if reported, the dosage of anesthetics was reasonable, and the same procedure was used for intervention and control group. Finally, the latest available randomized controlled trial dates back to 2001.
It might be argued that insufficient anesthetic depth was more common at that time, but even modern electroencephalography (EEG)-based monitoring of anesthetic depth even could only reduce but not eliminate intraoperative awareness with recall (AWR) [44]. Current recommendations for AWR prevention include earplugs or music via earphones as an essential component. Positive suggestions should be considered as well, since being proposed for prophylaxis of posttraumatic stress disorder following AWR [45]. It has been claimed that effects of intraoperative suggestions are limited to insufficient depth of anesthesia [46], but even this pre-requisite is not absent in clinical practice today.
Conclusions
Altogether, we found at least small overall effects of therapeutic suggestions, with no significant negative effect in any primary study. Hence, therapeutic suggestions could be a conceivable way to safely improve recovery and to reduce medication. In the light of the quite low effort and costs of implementation and use of suggestions it might be efficient to present suggestions under general anesthesia in clinical practice.
So far the evidence on the efficacy of therapeutic suggestions applied under general anesthesia has been summarized with respect to hospitalization and patient-controlled analgesia exclusively [20]. Our meta-analysis expands this knowledge by adding results on mental distress, pain intensity, medication, and recovery. With solely including randomized trials the internal validity of the findings should have been increased.
However, we cannot make clinical recommendations since the quality of evidence supporting the beneficial effects of therapeutic suggestions was rated as unclear in a considerable number of included trials, particularly with regard to selection bias and reporting bias. Moreover, there is a lack of respective publications after 2001. We encourage the proliferation of studies with a high methodological and reporting quality to strengthen the promising evidence for the efficacy of therapeutic suggestions presented during general anesthesia for patients undergoing surgery.
Acknowledgements
Not applicable.
Funding
This work was supported by the German Federal Ministry of Education and Research [grant number FKZ 01KG1016] and the Milton H. Erickson Foundation, Germany. The funding bodies were not involved in the design of the study, in the collection, analysis, and interpretation of data and in writing the manuscript.
Availability of data and material
All data generated and analyzed during this study are included in the supplementary information files (Additional file 6).
Authors’ contributions
JR and SK: drafted protocol, developed a search strategy, searched for studies, obtained copies of studies, selected which studies to include, extracted data from studies, drafted the final write-up of the review. DJ: searched for studies, obtained copies of studies, selected which studies to include, extracted data from studies, carried out the analysis, co-authored sections of the review. NZ: extracted data from studies, co-authored sections of the review. EH: interpreted the analysis, co-authored sections of the review. All authors read and approved the final version of the manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Abbreviations
- AWR
Awareness with recall
- CENTRAL
Cochrane Central Register of Controlled Trials
- EEG
Electroencephalography
- NNT
Number needed to treat
- PONV
Postoperative nausea and vomiting
- TIVA
Total intravenous anesthesia
Appendix
Full electronic search strategy for PubMed (MEDLINE)
#1 suggestion$.ti.ab.kw
#2 Suggestion/
#3 hypno$.ti.ab.kw
#4 Hypnosis/
#5 Hypnosis. Anesthetic/
#6 Persuasive Communication/
#7 auditory information$.ti.ab.kw
#8 Intraoperative Care/ px [Psychology]
#9 1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8
#10 exp Surgical Procedures. Operative/
#11 anesth$.ti.ab.kw
#12 anaesth$.ti.ab.kw
#13 Anesthesia/
#14 Anesthesia. General/
#15 Balanced Anesthesia/
#16 narcot$.ti.ab.kw
#17 narcosis.ti.ab.kw
#18 surg$.ti.ab.kw
#19 General Surgery/
#20 operat$.ti.ab.kw
#21 intraoperat$.ti.ab.kw
#22 intra-operat$.ti.ab.kw
#23 Intraoperative Period/
#24 intrasurg$.ti.ab.kw
#25 intra-surg$.ti.ab.kw
#26 medical procedure$.ti.ab.kw
#27 10 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16 OR 17 OR 18 OR 19 OR 20 OR 21 OR 22 OR 23 OR 24 OR 25 OR 26
#28 randomized controlled trial.pt
#29 controlled clinical trial.pt
#30 randomized.ab
#31 placebo.ab
#32 randomly.ab
#33 trial.ti.
#34 28 OR 29 OR 30 OR 31 OR 32 OR 33
#38 9 AND 27 AND 34
Additional files
Measures of outcomes. (DOCX 15 kb)
Risk of bias in individual studies. (DOCX 17 kb)
Funnel plot of Hedges’ g against its standard error for all outcomes. (TIF 302 kb)
Results of sensitivity analyses for the exclusion of approximated effect sizes and effect sizes which were set to zero, and for the exclusion of small samples. (DOCX 18 kb)
Results of subgroup analyses for PONV and antiemetic use. (DOCX 20 kb)
Data with descriptive and effect size related information. (XLSX 60.6 kb)
Contributor Information
Jenny Rosendahl, Phone: +49 3641 935482, Email: jenny.rosendahl@med.uni-jena.de.
Susan Koranyi, Email: susan.koranyi@medizin.uni-leipzig.de.
Davina Jacob, Email: davinajacob@yahoo.de.
Nina Zech, Email: nina.zech@klinik.uni-regensburg.de.
Ernil Hansen, Email: nina.zech@klinik.uni-regensburg.de.
References
- 1.Eaker E, Pinsky J, Castelli WP. Myocardial infarction and coronary death among women: psychosocial predictors from a 20- year follow-up of women in the Framingham Study. Am J Epidemiol. 1992;135:854–64. doi: 10.1093/oxfordjournals.aje.a116381. [DOI] [PubMed] [Google Scholar]
- 2.Häuser W, Hansen E, Enck P. Nocebo phenoma in medicine: their relevance in everyday clinical practice. Dtsch Arztebl Int. 2012;109:459–65. doi: 10.3238/arztebl.2012.0459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tefikow S, Barth J, Maichrowitz S, Beelmann A, Strauss B, Rosendahl J. Efficacy of hypnosis in adults undergoing surgery or medical procedures: a meta-analysis of randomized controlled trials. Clin Psychol Rev. 2013;33:623–36. doi: 10.1016/j.cpr.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 4.Montgomery GH, David D, Winkel G, Silverstein JH, Bovbjerg DH. The effectiveness of adjunctive hypnosis with surgical patients: a meta-analysis. Anesth Analg. 2002;94:1639–45. doi: 10.1097/00000539-200206000-00052. [DOI] [PubMed] [Google Scholar]
- 5.Schnur JB, Kafer I, Marcus C, Montgomery GH. Hypnosis to manage distress related to medical procedures: a meta-analysis. Contemp Hypn. 2008;25:114–28. doi: 10.1002/ch.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kekecs Z, Nagy T, Varga K. The effectiveness of suggestive techniques in reducing postoperative side effects: a meta-analysis of randomized controlled trials. Anesth Analg. 2014;119:1407–19. doi: 10.1213/ANE.0000000000000466. [DOI] [PubMed] [Google Scholar]
- 7.Varga K. Suggestive techniques connected to medical interventions. Interv Med Appl Sci. 2013;5:95–100. doi: 10.1556/IMAS.5.2013.3.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ghoneim MM, Block RI. Learning and consciousness during general anesthesia. Anesthesiology. 1992;76:279–305. doi: 10.1097/00000542-199205000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Clark DL, Rosner BS. Neurophysiologic effects of general anesthesia. Anesthesiology. 1973;38:564–82. doi: 10.1097/00000542-197306000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Madler C, Keller I, Schwender D, Pöppel E. Sensory information processing during general anaesthesia: effect of isoflurane on auditory evoked neuronal oscillations. Br J Anaesth. 1991;66:81–7. doi: 10.1093/bja/66.1.81. [DOI] [PubMed] [Google Scholar]
- 11.Millar K, Watkinson N. Recognition of words presented during general anaesthesia. Ergonomics. 1983;26:585–94. doi: 10.1080/00140138308963377. [DOI] [PubMed] [Google Scholar]
- 12.Schwender D, Kaiser A, Klasing S, Peter K, Pöppel E. Midlatency auditory evoked potentials and explicit and implicit memory in patients undergoing cardiac surgery. Anesthesiology. 1994;80:493–501. doi: 10.1097/00000542-199403000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Bennett HL, Davis HS, Giannini AJ. Non-verbal response to intraoperative conversation. Br J Anaesth. 1985;57:174–9. doi: 10.1093/bja/57.2.174. [DOI] [PubMed] [Google Scholar]
- 14.Goldmann L, Shah MV, Helden MW. Memory of cardiac anaesthesia: psychological sequelae in cardiac patients of intraoperative suggestion and operating room conversation. Anaesthesia. 1987;42:596–603. doi: 10.1111/j.1365-2044.1987.tb03082.x. [DOI] [PubMed] [Google Scholar]
- 15.Block RI, Ghoneim MM, Sum Ping ST, Ali MA. Efficacy of therapeutic suggestions for improved postoperative recovery presented during general anesthesia. Anesthesiology. 1991;75:746–55. doi: 10.1097/00000542-199111000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Mashour GA, Avidan MS. Intraoperative awareness: controversies and non-controversies. Br J Anaesth. 2015;115(suppl 1):i20–6. doi: 10.1093/bja/aev034. [DOI] [PubMed] [Google Scholar]
- 17.Sanders RD, Tononi G, Laureys S, Sleigh JW. Unresponsiveness ≠ unconsciousness. Anesthesiology. 2012;116:946–59. doi: 10.1097/ALN.0b013e318249d0a7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cheek DB. Surgical memory and reaction to careless conversation. Am J Clin Hypn. 1964;6:237–40. doi: 10.1080/00029157.1964.10402350. [DOI] [PubMed] [Google Scholar]
- 19.Levinson BW. States of awareness during general anaesthesia. Brit J Anaesth. 1965;37:544–6. doi: 10.1093/bja/37.7.544. [DOI] [PubMed] [Google Scholar]
- 20.Merikle PM, Daneman M. Memory for unconsciously perceived events: evidence from anesthetized patients. Conscious Cogn. 1996;5:525–41. doi: 10.1006/ccog.1996.0031. [DOI] [PubMed] [Google Scholar]
- 21.Jacob D, Tefikow S, Rosendahl J. Efficacy of therapeutic suggestions in adults undergoing surgery or medical procedures under general anaesthesia: a systematic review and meta-analysis of randomized controlled trials. PROSPERO 2013:CRD42013003963. http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42013003963 [Assessed 18 Mar 2015].
- 22.Lefebvre C, Manheimer E, & Glanville J. Searching for studies. In: Higgins JPT, Green S, eds. Cochrane handbook for systematic reviews of interventions version 5.1.0 (updated March 2011). The Cochrane Collaboration; 2011. Available from http://www.handbook.cochrane.org [Assessed 27 Apr 2015].
- 23.Higgins JPT, Altman DG, Sterne JAC. Assessing risk of bias in included studies. In: Higgins JPT, Green S, eds. Cochrane handbook for systematic reviews of interventions version 5.1.0 (updated March 2011). The Cochrane Collaboration; 2011. Available from http://http://www.cochrane-handbook.org [Assessed 23 July 2014].
- 24.Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994;6:284–90. doi: 10.1037/1040-3590.6.4.284. [DOI] [Google Scholar]
- 25.Hedges LV, Olkin I. Statistical methods for meta-analysis. New York: Academic; 1985. [Google Scholar]
- 26.Cohen J. A power primer. Psychol Bull. 1992;112:155–9. doi: 10.1037/0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 27.Kraemer HC, Kupfer DJ. Size of treatment effects and their importance to clinical research and practice. Biol Psychiatry. 2006;59:990–6. doi: 10.1016/j.biopsych.2005.09.014. [DOI] [PubMed] [Google Scholar]
- 28.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. Chichester: Wiley & Sons; 2009. [Google Scholar]
- 29.Dawson PR, Van Hamel C, Wilkinson D, Warwick P, O’Connor M. Patient-controlled analgesia and intra-operative suggestion. Anaesthesia. 2001;56:65–9. doi: 10.1046/j.1365-2044.2001.01763-5.x. [DOI] [PubMed] [Google Scholar]
- 30.Jelicic M, Bonke B, Millar K. Effect of different therapeutic suggestions presented during anaesthesia on post-operative course. Eur J Anaesthesiol. 1993;10:343–7. [PubMed] [Google Scholar]
- 31.Mastropietro CA. Development and testing of a middle range theory of assessment and intervention for pain and awareness during anesthesia: efficacy of timing of a therapeutic suggestion for surgical pain relief [dissertation] Cleveland: Case Western Reserve University; 1998. p. 205. [Google Scholar]
- 32.Higgins JPT, Deeks JJ, Altman DG. Special topics in statistics. In: Higgins JPT, Green S, eds. Cochrane handbook for systematic reviews of interventions version 5.1.0 (updated March 2011). The Cochrane Collaboration; 2011. Available from http://www.handbook.cochrane.org [Assessed 27 Apr 2015].
- 33.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 34.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Br Med J. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Deeks JJ, Higgins JPT, Altmann DG. Analysing data and undertaking meta-analyses. In: Higgins JPT, Green S, eds. Cochrane handbook for systematic reviews of interventions version 5.1.0 (updated March 2011). The Cochrane Collaboration; 2011. Available from http://www.handbook.cochrane.org [Assessed 24 Apr 2015].
- 36.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Br Med J. 1997;315:629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–63. doi: 10.1111/j.0006-341X.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 38.Thompson SG, Higgins JPT. How should meta-regression analyses be undertaken and interpreted. Stat Med. 2002;21:1559–73. doi: 10.1002/sim.1187. [DOI] [PubMed] [Google Scholar]
- 39.Pearson RE. Response to suggestions given under general anesthesia. Am J Clin Hypn. 1961;4:106–14. doi: 10.1080/00029157.1961.10401876. [DOI] [Google Scholar]
- 40.Korunka C, Guttmann G, Schleinitz D, Hilpert M, Haas R, Fitzal S. Die Auswirkung von Suggestionen und Musik während Vollnarkose auf postoperative Befindlichkeit [The effects of suggestions and music presented during general anaesthesia on postoperative well-being] Z Klin Psychol. 1992;21:272–85. [Google Scholar]
- 41.Kihlstrom JF, Cork RC. Consciousness and anesthesia. In: Schneider S, Velmans M, editors. The Blackwell Companion to Consciousness. Chichester: Wiley; 2007. p. 628–39.
- 42.Williams AR, Hind M, Sweeney BP, Fisher R. The incidence and severity of postoperative nausea and vomiting in patients exposed to positive intra-operative suggestions. Anaesthesia. 1994;49:340–2. doi: 10.1111/j.1365-2044.1994.tb14190.x. [DOI] [PubMed] [Google Scholar]
- 43.London P, Cooper LM. Norms of hypnotic susceptibility in children. Develop Psychol. 1969;1:113–24. doi: 10.1037/h0027002. [DOI] [Google Scholar]
- 44.Palanca BJ, Mashour GA, Avidan MS. Processed electroencephalogram in depth of anesthesia monitoring. Curr Opin Anaesthesiol. 2009;22:553–9. doi: 10.1097/ACO.0b013e3283304032. [DOI] [PubMed] [Google Scholar]
- 45.Bejenke CJ. Intraoperative awareness. In: Cyna A, Andrew MI, Tan SGM, Smith AF, editors. Handbook of communication in anaesthesia and critical care. Oxford: Oxford University Press; 2010. pp. 175–85. [Google Scholar]
- 46.Kerssens C, Ouchi T, Sebel PS. No evidence of memory function during anesthesia with propofol or isoflurane with close control of hypnotic state. Anesthesiology. 2005;102:57–62. doi: 10.1097/00000542-200501000-00012. [DOI] [PubMed] [Google Scholar]
- 47.Bethune DW, Ghosh S, Walker IA, Carter A, Kerr L, Sharples L. Intraoperative positive therapeutic suggestions improve immediate postoperative recovery following cardiac surgery. In: Sebel PS, Bonke B, Winograd E, editors. Memory and awareness in anesthesia. Englewood Cliffs: Prentice-Hall; 1993. pp. 154–61. [Google Scholar]
- 48.Evans C, Richardson PH. Improved recovery and reduced postoperative stay after therapeutic suggestions during general anaesthesia. Lancet. 1988;2:491–3. doi: 10.1016/S0140-6736(88)90131-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Boeke S, Bonke B, Bouwhuis-Hoogerwerf ML, Bovill JG, Zwaveling A. Effects of sounds presented during general anaesthesia on postoperative course. Br J Anaesth. 1988;60:697–702. doi: 10.1093/bja/60.6.697. [DOI] [PubMed] [Google Scholar]
- 50.Bonke B, Schmitz PIM, Verhage F, Zwaveling A. Clinical study of so- called unconscious perception during general anaesthesia. Br J Anaesth. 1986;58:957–64. doi: 10.1093/bja/58.9.957. [DOI] [PubMed] [Google Scholar]
- 51.Caseley-Rondi G, Merikle PM, Bowers KS. Unconscious cognition in the context of general anesthesia. Conscious Cogn. 1994;3:166–95. doi: 10.1006/ccog.1994.1011. [DOI] [Google Scholar]
- 52.Cowan GS, Buffington CK, Cowan GS, Hathaway D. Assessment of the effects of a taped cognitive behavior message on postoperative complications (therapeutic suggestions under anesthesia) Obes Surg. 2001;11:589–93. doi: 10.1381/09608920160556779. [DOI] [PubMed] [Google Scholar]
- 53.De Houwer J, Demeyere R, Verhamme B, Eelen P. Intra- and post-operative effects of information presented during CABG surgery with sufentanil anaesthesia. In: Bonke B, Bovill JG, Moerman N, editors. Memory and awareness in anesthesia III. Assen: Van Gorcum; 1996. pp. 243–55. [Google Scholar]
- 54.Eberhart LHJ, Döring HJ, Holzrichter P, Roscher R, Seeling W. Therapeutic suggestions given during neurolept-anaesthesia decrease post-operative nausea and vomiting. Eur J Anaesthesiol. 1998;15:446–52. doi: 10.1097/00003643-199807000-00010. [DOI] [PubMed] [Google Scholar]
- 55.Furlong M. Positive suggestions presented during anaesthesia. In: Bonke B, Fitch W, Millar K, editors. Memory and awareness in anaesthesia. Lisse: Swets & Zeitlinger Publishers; 1990. pp. 170–5. [Google Scholar]
- 56.Furlong M, Read C. Therapeutic suggestions during general anesthesia. In: Sebel PS, Bonke B, Winograd E, editors. Memory and awareness in anesthesia. Englewood Cliffs: Prentice-Hall; 1993. pp. 166–75. [Google Scholar]
- 57.Lebovits AH, Twersky R, McEwan B. Intraoperative therapeutic suggestions in day-case surgery: are there benefits for postoperative outcome. Br J Anaesth. 1999;82:861–6. doi: 10.1093/bja/82.6.861. [DOI] [PubMed] [Google Scholar]
- 58.Liu WHD, Standen PJ, Aitkenhead AR. Therapeutic suggestions during general anaesthesia in patients undergoing hysterectomy. Br J Anaesth. 1992;68:277–81. doi: 10.1093/bja/68.3.277. [DOI] [PubMed] [Google Scholar]
- 59.Liu WDH, Standen PJ, Aitkenhead AR. The influence of intraoperative therapeutic suggestions on postoperative recovery after surgical repair of fractured neck of femur. In: Sebel PS, Bonke B, Winograd E, editors. Memory and awareness in anesthesia. Englewood Cliffs: Prentice-Hall; 1993. pp. 162–5. [Google Scholar]
- 60.Maroof M, Ahmed SM, Khan RM, Bano SJ, Haque AW. Intra-operative suggestions reduce incidence of post hysterectomy emesis. J Pak Med Assoc. 1997;47:202–4. [PubMed] [Google Scholar]
- 61.McLintock TTC, Aitken H, Downie CFA, Kenny GNC. Postoperative analgesic requirements in patients exposed to positive intraoperative suggestions. Br Med J. 1990;301:788–90. doi: 10.1136/bmj.301.6755.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.McWilliams JL. Using hypnotic suggestions to reduce postoperative nausea and pain following lumbar laminectomies [dissertation] Mississippi State: Mississippi State University; 1990. p. 102. [Google Scholar]
- 63.Melzack R, Germain M, Belanger E, Fuchs PN, Swick R. Positive intrasurgical suggestion fails to affect postsurgical pain. J Pain Symptom Manage. 1996;11:103–7. doi: 10.1016/0885-3924(95)00157-3. [DOI] [PubMed] [Google Scholar]
- 64.Moix J, Bayés R, Burrel L, Casas JM. Effects of intraoperative suggestions on intra- and postoperative variables: Preliminary report. In: Bonke B, Bovill JG, Moerman N, editors. Memory and awareness in anaesthesia III. Assen: Van Gorcum; 1996. pp. 227–34. [Google Scholar]
- 65.Münch F, Zug H-D. Do intraoperative suggestions prevent nausea and vomiting in thyroidectomy-patients? An experimental study. In: Bonke B, Fitch W, Millar K, editors. Memory and awareness in anaesthesia. Lisse: Swets & Zeitlinger Publishers; 1990. pp. 185–8. [Google Scholar]
- 66.Nilsson U, Rawal N, Unestahl LE, Zetterberg C, Unosson M. Improved recovery after music and therapeutic suggestions during general anaesthesia: a double-blind randomised controlled trial. Acta Anaesthesiol Scand. 2001;45:812–7. doi: 10.1034/j.1399-6576.2001.045007812.x. [DOI] [PubMed] [Google Scholar]
- 67.Oddby-Muhrbeck E, Jakobsson J, Enquist B. Implicit processing and therapeutic suggestion during balanced anaesthesia. Acta Anaesthesiol Scand. 1995;39:333–7. doi: 10.1111/j.1399-6576.1995.tb04072.x. [DOI] [PubMed] [Google Scholar]
- 68.Rosenberg JI. Postoperative recovery and cost-benefit of an audiotape played to patients under general anesthesia [dissertation] Washington, DC: The George Washington University; 1992. p. 225. [Google Scholar]
- 69.Steinberg ME, Hord AH, Reed B, Sebel PS. Study of the effect of intra- operative suggestion on postoperative analgesia and well-being. In: Sebel PS, Bonke B, Winograd E, editors. Memory and awareness in anesthesia. Englewood Cliffs: Prentice-Hall; 1993. pp. 205–8. [Google Scholar]
- 70.van der Laan WH, van Leeuwen BL, Sebel PS, Winograd E, Baumann P, Bonke B. Therapeutic suggestion has no effect on postoperative morphine requirements. Anesth Analg. 1996;82:148–52. doi: 10.1097/00000539-199601000-00027. [DOI] [PubMed] [Google Scholar]
- 71.Woo R, Seltzer JL, Marr A. The lack of response to suggestion under controlled surgical anesthesia. Acta Anaesthesiol Scand. 1987;31:567–71. doi: 10.1111/j.1399-6576.1987.tb02622.x. [DOI] [PubMed] [Google Scholar]


