Abstract
Background
Men who have sex with men (MSM) are at high risk of HIV and sexually transmitted infections (STIs) in China and globally. Engaging in commercial sex put them at even greater risk. This study estimated the prevalence of HIV/STIs among three subgroups of MSM: MSM who sold sex (MSM-selling), MSM who bought sex (MSM-buying), and non-commercial MSM (NC-MSM) and evaluated the relationship between commercial sex and HIV/STIs.
Methods
We conducted a cross-sectional survey among MSM in six Chinese cities (Shenyang, Ji’nan, Changsha, Zhengzhou, Nanjing, and Kunming) from 2012 to 2013. Data on socio-demographics and sexual behaviors were collected. Serological tests were conducted to detect HIV, syphilis, and human simplex virus type 2 (HSV-2).
Results
Of 3717 MSM, 6.8% were engaged in commercial sex. The overall prevalence of HIV, syphilis and HSV-2 infections was 11.1, 8.8 and 12.1%, respectively. MSM-selling had higher prevalence of HIV (13.4%), syphilis (12.1%) and HSV-2 (17.9%) than NC-MSM (10.9, 8.7 and 11.9% for HIV, syphilis and HSV-2, respectively), though the differences are not statistically significant. Among MSM-selling, HIV prevalence was significantly higher for those who found sex partners via Internet than those did not (19.4% vs. 8.1%, P = 0.04). Compared to NC-MSM, MSM-selling were more likely to use recreation drugs (59.3% vs. 26.3%), have unprotected anal intercourse (77.9% vs. 61.7%), and have ≥10 male sex partners (46.2% vs. 6.2%) in the past 6 months (each P < 0.05).
Conclusions
All three subgroups of MSM in six large Chinese cities have high prevalence of HIV/STIs. Those who sell sex only have a particularly high risk of acquiring and transmitting disease, and therefore, they should be considered as a priority group in HIV/STIs surveillance and intervention programs.
Electronic supplementary material
The online version of this article (doi:10.1186/s12879-016-2130-x) contains supplementary material, which is available to authorized users.
Keywords: Men who have sex with men, Commercial sex, HIV, Sexually transmitted infection China
Background
Men who have sex with men (MSM) are at a high risk of HIV infection around the world [1]. The pooled data from seven low- and middle-income Asian countries including China showed that MSM were 18.7 times more likely to have HIV infection than other reproductive-age men [2]. The risk factors associated with HIV infection among MSM include both biological and behavioral factors such as unprotected anal intercourse (UAI), substance abuse, and co-infection with other sexually transmitted infections (STIs) like syphilis and herpes simplex virus type 2 (HSV-2) [1, 3–6]. Co-infection of HIV and other STIs are prevalent among Chinese MSM [7]. Co-infection of ulcerative STIs such as syphilis and HSV-2 is of particular concern, as these STIs can increase the likelihood of HIV transmission.
Many Chinese MSM engaged in both homosexual and heterosexual activities, and some engaged in the commercial sex [8]. MSM who sell sex to men for money or goods (MSM-selling), have been found to be at higher risks of HIV and other STIs due to multiple sexual partners and high frequency of UAI [9, 10]. One study in Chengdu in southwest China showed that MSM-selling were 6.4 times more likely to have HIV infection than other MSM [11]. However, data are inconsistent. For example, a study in Shenzhen in south China found lower HIV prevalence among MSM-selling (4.6%) than other MSM (7.0%; P = 0.03) [12].
Along with the inconsistent data on HIV risk among MSM-selling, there are few studies among Chinese MSM who buy sex (MSM-buying). The risk of HIV/STIs has never been compared among MSM-selling, MSM-buying, and MSM who did not engage in commercial sex (NC-MSM). Such a comparison could enrich the understanding of China’s HIV epidemic and provide evidence for public health worker and policy makers to develop specific HIV intervention strategies. The aim of this study was to estimate the prevalence of HIV, syphilis and HSV-2 infections among MSM-selling, MSM-buying and NC-MSM, and assess the relationship between commercial sex engagement (either selling or buying sex) and HIV/STIs among Chinese MSM.
Methods
Study participants
From June 2012 to June 2013, a cross-sectional study was conducted among MSM who were living in six large Chinese cities: Shenyang, Ji’nan, Changsha, Zhengzhou, Nanjing and Kunming. These large cities represent different geographical locations, social and economic development, and HIV epidemics across China. MSM participants were recruited using multiple approaches, including advertising on gay websites and online chat rooms, outreach to gay-gathering venues (e.g., gay bars, parks, public bathhouses), and peer referrals. Subjects were eligible if they were male, 18 years or older, able to provide informed consent, and self-reported ever having sex with other men. The sample size of recruited MSM in each city was estimated based on a two-sided Z test, by using an alpha(α) of 0.05, a statistical analysis power of 90%, a HIV prevalence of 10%, and an estimate rate difference(d0) of 0.04, a sample size of 641 MSM in each city was needed.
Questionnaire interview
Each participant completed a face-to-face interview with trained interviewers to collect the following information: (1) socio-demographics, including age, marital status, residency, ethnicity, education, and occupation etc.; (2) HIV/AIDS knowledge; (3) sexual and illicit drug use behaviors, including sexual orientation, sexual debut, number of sexual partners in the past 6 months, UAI, venues for seeking male sexual partners, and recreational drug use, etc.; and (4) experiences of buying or selling sex with other male partners in the past 6 months (Additional file 1). To minimize the interviewer bias, a uniform study protocol was used, and all the interviewers were trained for conducting the survey.
Laboratory testing
A blood sample was collected from each participant for testing antibodies to HIV, syphilis and HSV-2. HIV-1 antibody was detected by enzyme-linked immunosorbent assay [ELISA] (Vironostika® HIV-1Microelisa System; bioMerieux, Durham, NC, USA), and positive tests were confirmed by Western blot test (HIV Blot 2.2 WBTM, Genelabs Diagnostics, Singapore). Rapid plasma reagin (RPR) test (RPR, Shanghai Kehua Biotechnology Ltd, Shanghai, China) was used to screen syphilis and positive tests were confirmed by the Treponema pallidum particle assay (TPPA) test (TPPA, Hainan Huamei Biomedicine Co, LTD, Haikou, China). Subjects with both RPR and TPPA positive testing results were considered currently infected syphilis. HSV-2 infection was determined using ELISA (HerpeSelect-2®, Focus Diagnostics, Cypress, CA, USA).
Statistical analysis
Student t-tests were used to calculate means ± standard deviations (SD) for continuous variables and Pearson’s Chi-square test or Fisher’s exact test were used for comparing proportions (%) for categorical variables. Specifically, we compared demographic and behavioral characteristics and HIV/STI prevalence among three groups of MSM (MSM-selling, MSM-buying and NC-MSM). Univariate logistic regression analyses were performed to screen factors associated with HIV, syphilis and HSV-2 infections, respectively, and those factors which were significant at P < 0.05 and suggested as possible risk factors in the literature were included in multivariate logistic regression models with HIV, syphilis and HSV-2 infection as a dependent variable, separately. As the number of participants with missing data in any key variables was <10% of the total sample size, and the potential bias due to list-wise deletion in the multivariable analysis was unlikely to be significant, we did not impute the missing values using methods like the multiple imputation by chained equations. A significant level was defined as P < 0.05 for two-sided testing. All statistical analyses were performed using Statistical Analysis System software (SAS 9.2 for Windows; SAS Institute Inc., NC, USA).
Ethic, consent and permissions
The study protocol and informed consent form were reviewed and approved by the institutional review board of the First Affiliated Hospital of China Medical University (2011). Study details were explained clearly for each participant and written informed consent was obtained prior to the survey.
Results
Demographic characteristics
A total of 3749 MSM were invited for this study, of whom 10 declined (0.3%) and 20 were ineligible due to age <18 years. Of 3719 eligible MSM participants, 2 did not answer the question about commercial sex. Therefore, 3717 participants (99.9%) were included in the analyses, with 100% of participants having HIV and syphilis outcomes and 91.2% (n = 3389) having HSV-2 testing results (Fig. 1).
Fig. 1.
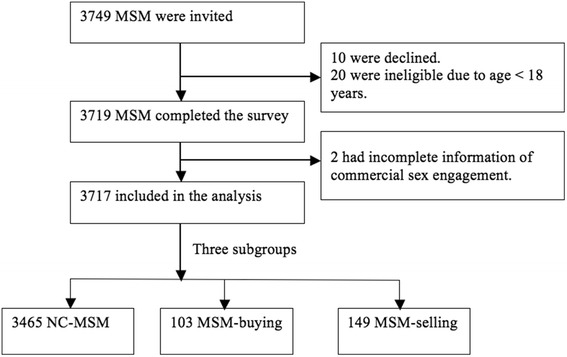
Flowchart of participant selection
About 6.8% of MSM participants reported being ever engaged in commercial sex in past 6 months, including 149 MSM-selling (4.0%) and 103 MSM-buying (2.8%). The median age of all participants was 26 years (IQR: 23–33 years), and the majority were single (76%), of Han ethnics (93%) and had lived in the study cities for over 6 months. About 57% had received college education or above and 14.8% were students (Table 1).
Table 1.
Demographics and HIV, syphilis and HSV-2 prevalence by commercial sex engagement among 3717 MSM in six Chinese cities
| Characteristic | Total | NC-MSM | MSM-buying | MSM-selling | P-value* |
|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | ||
| Overall | 3717 (100.0) | 3465 (93.2) | 103 (2.8) | 149 (4.0) | _ |
| HIV positive | 411 (11.1) | 378 (10.9) | 13 (12.6) | 20 (13.4) | 0.554 |
| Syphilis positive | 327 (8.8) | 302 (8.7) | 7 (6.8) | 18 (12.1) | 0.285 |
| HSV-2 positive | 409 (12.1) | 380 (11.9) | 12 (14.1) | 17 (17.5) | 0.202 |
| Age (median, IQR, in years) | 26 (23–33) | 26 (23–33) | 28 (24–34) | 23 (21–28) | <0.001 |
| Han majority | 3447 (92.7) | 3237 (93.4) | 87 (84.5) | 123 (82.6) | <0.001 |
| Married with females | 893 (24.0) | 846 (24.4) | 33 (32.0) | 14(9.4) | <0.001 |
| Living in the study city ≤6 mo. | 261 (8.6) | 239 (8.2) | 5 (7.6) | 17 (29.3) | <0.001 |
| Student, in school | 548 (14.8) | 530 (15.3) | 8 (7.8) | 10 (6.8) | <0.001 |
| Education: College or above | 2128 (57.3) | 2048 (59.1) | 52 (50.5) | 28 (18.8) | <0.001 |
| Seeking male sexual partners via internet | 2560 (69.0) | 2439 (70.5) | 59 (57.3) | 62 (41.9) | <0.001 |
| Seeking male partners locally or in other cities | |||||
| Locally | 2461 (72.3) | 2377 (73.8) | 43 (52.4) | 41 (41.0) | <0.001 |
| In other cities | 516 (15.2) | 452 (14.0) | 25 (30.5) | 39 (39.0) | |
| Neither | 427 (12.5) | 393 (12.2) | 14 (17.1) | 20 (20.0) | |
| Number of MSM partners in past 6 months | |||||
| 0–2 | 2315 (63.2) | 2250 (65.5) | 37 (39.0) | 28 (21.5) | <0.001 |
| 3–9 | 1052 (28.7) | 973 (28.3) | 37 (39.0) | 42 (32.3) | |
| ≥10 | 294 (8.0) | 213 (6.2) | 21 (22.1) | 60 (46.2) | |
| Use of any recreational drugs in past 6 months | 886 (27.5) | 804 (26.3) | 31 (40.3) | 51 (59.3) | <0.001 |
| UAI in past 6 months | 2320 (62.4) | 2136 (61.7) | 68 (66.0) | 116 (77.9) | <0.001 |
| Predominant role in anal sex | |||||
| Equal | 1228 (33.9) | 1136 (33.4) | 31 (31.6) | 61 (49.2) | 0.001 |
| Insertive | 1180 (32.5) | 1122 (33.0) | 36 (36.7) | 22 (17.4) | |
| Receptive | 1219 (33.6) | 1147 (33.7) | 31 (31.6) | 41 (33.1) | |
| Having sex with female, in past 6 months | 675 (18.2) | 613 (17.7) | 34 (22.8) | 28 (27.2) | 0.016 |
HSV-2 human herpes virus type 2, UAI Unprotected anal intercourse, IQR interquartile range
*Chi-square test
Overall, MSM-selling were younger, less likely to be married and more likely to living in the study cities for only 6 months or less, and had lower education level than both MSM-buying and NC-MSM. Fewer student MSM were found in the subgroups of MSM-buying or MSM-selling than NC-MSM (each P < 0.001).
Prevalence of HIV, syphilis and HSV-2
The overall prevalence of HIV, syphilis and HSV-2 infection was 11.1, 8.8 and 12.1%, respectively (Table 1). MSM-selling had higher HIV prevalence than NC-MSM and MSM-buying (13.4% vs. 10.9% vs. 12.6%, p = 0.55). MSM-selling also had higher prevalence of syphilis and HSV-2 (12.1 and 17.5%, respectively) than the other the two groups though the difference was not statistically significant (P > 0.05).
When the prevalence of HIV was broken down by seeking male sex partners online, among MSM-selling the prevalence of HIV infection was significantly higher for those seeking sex partners online than those seeking male sex partners offline 19.4% (95% CI, 10.4–31.4%) vs. 8.1% (95% CI, 3.3–16.1%), P = 0.04, Fig. 2a). Among NC-MSM, those who seek male partners online had significantly lower prevalence of syphilis/HSV-2 infection than NC-MSM seeking male sex partners offline with syphilis prevalence of 7.3% (95% CI, 6.3–8.5%) vs. 11.9% (95% CI, 9.9–14.0%, P < 0.01, Fig. 2b) and HSV-2 prevalence of 10.2% (95% CI, 9.0–11.6%) vs. 15.8% (95% CI, 13.4–18.3%, P < 0.01, Fig. 2c).
Fig. 2.
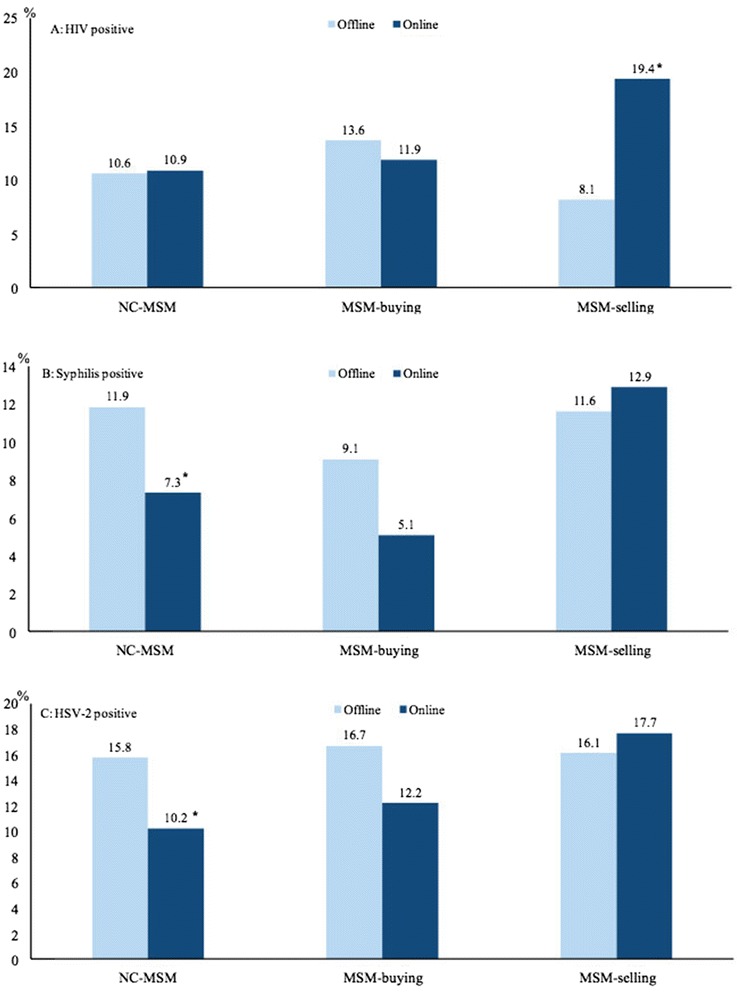
The prevalence of HIV (a), syphilis (b), and HSV-2 (c) among MSM seeking male sex partners online by commercial sex engagement (HSV-2 = human herpes virus type 2; *chi-square test, p < 0.05)
Sexual behavior of participants
Almost 70% of participants reported seeking male sexual partners online, 72% had sought male partners in local cities and 18.2% had sex with females in the past 6 months (Table 1). Over 62% were engaged in UAI, 27.5% used recreational drugs and 36.8% had 3 or more male sex partners in past 6 months.
Fewer MSM-selling reported seeking male sex partners online than NC-MSM (41.9% vs. 70.5%). More MSM-selling had ≥10 male sex partners, used recreational drugs, were engaged in UAI, and had sex with a female in the past 6 months.
Factors associated with HIV, syphilis and HSV-2 infection
The unadjusted odds of having HIV was 1.2 (95% CI, 0.7–2.1) and 1.3 (95% CI, 0.8–2.1) for MSM-buying and MSM-selling, in comparison to NC-MSM (Table 2). Engagement in commercial sex was not independently associated with HIV/STIs after adjusted for socio-demographics, co-infections and risk behaviors. In the multivariable model, the prevalence of HIV was significantly associated with several socio-demographic factors (shorter length of residency, non-student occupation, and lower educational level), sexual behaviors (multiple sexual partners, use of drugs, UAI and predominantly reception anal sex), and biological co-factors (co-infection with syphilis or HSV-2) (Table 2).
Table 2.
Factors associated with HIV infection among 3717 Chinese MSM
| Characteristic | No. of MSM HIV positive (%) | Crude OR (95% CI) | P-value | AOR (95% CI) | P-value |
|---|---|---|---|---|---|
| Commercial sex | |||||
| NC-MSM | 378 (10.9) | Ref. | 0.55 | Ref. | 0.88 |
| MSM-buying | 13 (12.6) | 1.2 (0.7–2.1) | 1.1 (0.5–2.5) | ||
| MSM-selling | 20 (13.4) | 1.3 (0.8–2.1) | 1.2 (0.5–2.6) | ||
| Syphilis positive | |||||
| No | 333 (9.8) | Ref. | <0.001 | Ref. | <0.001 |
| Yes | 78 (23.9) | 2.9 (2.2–3.8) | 2.0 (1.4–2.8) | ||
| HSV-2 positive | |||||
| No | 275 (9.2) | Ref. | <0.001 | Ref. | <0.001 |
| Yes | 88 (21.5) | 2.7 (2.1–3.5) | 2.3 (1.7–3.1) | ||
| Age (per year) | 1.0 (1.0–1.1) | 0.001 | 1.0 (0.9–1.0) | 0.24 | |
| Married to a woman | |||||
| No | 293 (10.4) | Ref. | 0.018 | Ref. | 0.18 |
| Yes | 118 (13.2) | 1.3 (1.0–1.7) | 1.2 (0.9–1.6) | ||
| Time living in the study city | |||||
| >6 months | 317 (11.4) | Ref. | 0.023 | Ref. | 0.031 |
| ≤6 months | 42 (16.1) | 1.5 (1.1–2.1) | 1.5 (1.0–2.2) | ||
| Student | |||||
| No | 376 (11.9) | Ref. | <0.001 | Ref. | 0.002 |
| Yes | 35 (6.4) | 0.5 (0.4–0.7) | 0.5 (0.3–0.8) | ||
| Education | |||||
| College or above | 210 (9.9) | Ref. | 0.008 | Ref. | 0.15 |
| High school or below | 201 (12.6) | 1.3 (1.1–1.6) | 1.2 (0.9–1.5) | ||
| Seeking partners online | |||||
| No | 121 (10.5) | Ref. | 0.6 | Ref. | 0.72 |
| Yes | 284 (11.1) | 1.1 (0.8–1.3) | 1.1 (0.8–1.4) | ||
| Number of male sex partners in past 6 months | |||||
| 0–2 | 220 (9.5) | Ref. | <0.001 | Ref. | 0.023 |
| 3–9 | 147 (14.0) | 1.5 (1.2–1.9) | 1.4 (1.1–1.8) | ||
| ≥10 | 34 (11.6) | 1.2 (0.8–1.8) | 1.1 (0.7–1.7) | ||
| Drug use in past 6 months | |||||
| No | 237 (10.1) | Ref. | <0.001 | Ref. | <0.001 |
| Yes | 144 (16.3) | 1.7 (1.4–2.1) | 1.7 (1.3–2.2) | ||
| UAI in past 6 months | |||||
| No | 123 (8.8) | Ref. | <0.001 | Ref. | 0.001 |
| Yes | 288 (12.4) | 1.5 (1.2–1.8) | 1.5 (1.2–1.9) | ||
| Predominant anal sex position | |||||
| Receptive | 265 (12.8) | Ref. | <0.001 | Ref. | 0.014 |
| Insertive | 139 (9.0) | 0.7 (0.5–0.8) | 0.7 (0.6–0.9) | ||
The risks of current syphilis infection were similar to those of HIV infection, with a few differences (Table 3). In multivariable analysis, syphilis was associated with HIV and/or HSV-2 infections, older age, more sex partners, drug use, and UAI. The length of city residency and predominant receptive anal sex position were not significant for syphilis infection. For HSV-2 infection, co-infections with HIV and/or syphilis, non-students, lower educational status, and not seeking partners online were significantly associated (Table 4).
Table 3.
Factors associated with syphilis infection among 3717 Chinese MSM
| Characteristic | No. of MSM syphilis positive (%) | Crude OR (95% CI) | P-value | AOR (95% CI) | P-value |
|---|---|---|---|---|---|
| Commercial sex | |||||
| NC-MSM | 302 (8.7) | Ref. | 0.28 | Ref. | 0.262 |
| MSM-buying | 7 (6.8) | 0.8 (0.4–1.7) | 0.5 (0.2–1.4) | ||
| MSM-selling | 18 (12.1) | 1.4 (0.9–2.4) | 1.5 (0.7–3.3) | ||
| HIV positive | |||||
| No | 249 (7.5) | Ref. | <0.001 | Ref. | <0.001 |
| Yes | 78 (19.0) | 2.9 (2.2–3.8) | 2.0 (1.5–2.8) | ||
| HSV-2 positive | |||||
| No | 208 (7.0) | Ref. | <0.001 | Ref. | <0.001 |
| Yes | 81 (19.8) | 3.3 (2.5–4.4) | 2.7 (2.0–3.7) | ||
| Age (per year) | 1.0 (1.0–1.1) | 0.001 | 1.0 (1.0–1.1) | 0.002 | |
| Married to a woman | |||||
| No | 222 (7.9) | Ref. | <0.001 | Ref. | 0.45 |
| Yes | 105 (11.8) | 1.6 (1.2–2.0) | 0.9 (0.6–1.2) | ||
| Time living in the study city | |||||
| >6 months | 244 (8.7) | Ref. | 0.31 | _ | _ |
| ≤6 months | 18 (6.9) | 0.8 (0.5–1.3) | |||
| Student | |||||
| No | 305 (9.6) | Ref. | <0.001 | Ref. | 0.170 |
| Yes | 22 (4) | 0.4 (0.3–0.6) | 0.7 (0.4–1.2) | ||
| Education | |||||
| College or above | 145 (6.8) | Ref. | <0.001 | Ref. | 0.080 |
| High school or below | 182 (11.5) | 1.8 (1.4–2.2) | 1.3 (1.0–1.7) | ||
| Seeking partners online | |||||
| No | 135 (11.7) | Ref. | <0.001 | Ref. | 0.082 |
| Yes | 190 (7.4) | 0.6 (0.5–0.8) | 0.8 (0.6–1.0) | ||
| Number of male sex partners in past 6 months | |||||
| 0–2 | 175 (7.6) | Ref. | 0.002 | Ref. | 0.002 |
| 3–9 | 113 (10.7) | 1.5 (1.1–1.9) | 1.5 (1.1–1.9) | ||
| ≥10 | 35 (11.9) | 1.7 (1.1–2.4) | 1.5 (1.0–2.5) | ||
| Drug use in past 6 months | |||||
| No | 182 (7.8) | Ref. | 0.024 | Ref. | 0.007 |
| Yes | 91 (10.3) | 1.4 (1.0–1.8) | 1.5 (1.1–2.0) | ||
| UAI in past 6 months | |||||
| No | 102 (7.3) | Ref. | 0.013 | Ref. | 0.038 |
| Yes | 225 (9.7) | 1.4 (1.1–1.7) | 1.3 (1.0–1.8) | ||
| Predominant position in anal sex | |||||
| Receptive | 265 (12.8) | Ref. | 0.23 | _ | _ |
| Insertive | 139 (9.0) | 0.9 (0.7–1.1) | |||
Table 4.
Factors associated with HSV-2 infection among 3389 Chinese MSM
| Characteristic | No. of MSM HSV-2 positive (%) | Crude OR (95% CI) | P-value | AOR (95% CI) | P-value |
|---|---|---|---|---|---|
| Commercial sex | |||||
| NC-MSM | 380 (11.8) | Ref. | 0.20 | Ref. | 0.52 |
| MSM-buying | 12 (14.1) | 1.2 (0.7–2.3) | 1.5 (0.7–2.9) | ||
| MSM-selling | 17 (17.5) | 1.6 (0.9–2.7) | 1.2 (0.5–2.6) | ||
| HIV positive | |||||
| No | 88 (24.2) | Ref. | <0.001 | Ref. | <0.001 |
| Yes | 321 (10.6) | 2.7 (2.1–3.5) | 2.3 ((1.8–3.1) | ||
| Syphilis positive | |||||
| No | 81 (28) | Ref. | <0.001 | Ref. | <0.001 |
| Yes | 328 (10.6) | 3.3 (2.5–4.4) | 2.7 (2.0–3.7) | ||
| Age (per year) | 1.1 (1.0–1.1) | <0.001 | 1.0 (1.0–1.1) | <0.001 | |
| Married to a woman | |||||
| No | 266 (10.4) | Ref. | <0.001 | Ref. | 0.61 |
| Yes | 143 (17) | 1.8 (1.4–2.2) | 0.9 (0.7–1.2) | ||
| Time living in the study city | |||||
| >6 months | 333 (11.9) | Ref. | 0.88 | _ | _ |
| ≤6 months | 32 (12.3) | 1.0 (0.7–1.5) | |||
| Student | |||||
| No | 391 (13.6) | Ref. | <0.001 | Ref. | <0.001 |
| Yes | 18 (3.5) | 0.2 (0.1–0.4) | 0.4 (0.2–0.7) | ||
| Education | |||||
| College or above | 194 (9.8) | Ref. | <0.001 | Ref. | 0.37 |
| High school or below | 215 (15.3) | 1.7 (1.4–2.1) | 1.1 (0.9–1.4) | ||
| Seeking partners online | |||||
| No | 159 (15.8) | Ref. | <0.001 | Ref. | 0.28 |
| Yes | 247 (10.4) | 0.6 (0.5–0.8) | 0.9 (0.7–1.1) | ||
| Number of male sex partners in past 6 months | |||||
| 0–2 | 236 (11.1) | Ref. | 0.12 | Ref. | 0.27 |
| 3–9 | 129 (13.3) | 1.2 (1.0–1.5) | 1.2 (0.9–1.5) | ||
| ≥10 | 36 (14.2) | 1.3 (0.9–1.9) | 1.3 (0.8–1.9) | ||
| Drug use in past 6 months | |||||
| No | 278 (11.9) | Ref. | 0.88 | Ref. | 0.64 |
| Yes | 93 (11.7) | 1.0 (0.8–1.3) | 1.1 (0.8–1.4) | ||
| UAI in past 6 months | |||||
| No | 154 (11.6) | Ref. | 0.54 | Ref. | 0.19 |
| Yes | 255 (12.3) | 1.1 (0.9–1.3) | 0.9 (0.7–1.1) | ||
| Predominant anal sex position | |||||
| Receptive | 134 (11.6) | Ref. | 0.35 | _ | _ |
| Insertive | 127 (11.6) | 0.9 (0.7–1.1) | |||
Discussion
Our study showed that HIV, syphilis and HSV-2 infections were prevalent in all of three subpopulations of MSM (MSM-selling, MSM-buying and NC-MSM) in China. However, among MSM-selling, HIV prevalence was significantly higher for those seeking sex partners online than those seeking sex partners offline. To our knowledge, these findings were scarcely reported before. Additionally, MSM-selling reported to have risk sexual behaviors more frequently than other two groups.
In this cross-sectional study, the rates of HIV (11.1%) and HSV-2 (12.1%) among MSM overall were comparable to another study in multiple cities [13], which reported 10% of HIV infection and 16% of HSV-2 infection among MSM. But the overall HIV prevalence was more than 2-fold higher than that in a national survey across 61 cities during 2008–2009 (4.9%), and the overall syphilis rate (8.8%) was lower than that of national survey (12%) [14]. The prevalence of HIV/STIs varied by geographical distributions across China [14, 15], which was in agreement with our findings in these six cities. To investigate the association between the prevalence of STIs and commercial sex activities, the advantages of using pooled data from multiple sites include is to while having heterogeneity associated with regions.
Compared to MSM without commercial sex, the prevalence of HIV/STIs is usually higher among MSM sex workers [11, 16, 17]. Our findings also demonstrated this trend that MSM with commercial sex had higher HIV/STIs prevalence than those without commercial sex, as suggested in other study [18], though the prevalence of HIV, syphilis and HSV-2 was not significant different among MSM-selling, MSM-buying and NC-MSM. One noticeable characteristic of MSM-selling in the current study was that they were significantly younger than MSM-buying or NC-MSM. Hence, shorter HIV exposure period may decrease their cumulative HIV acquiring risk.
It is usually assumed that female commercial sex workers play a bridging role for HIV heterosexual transmission [19]. Our study results enriched the understanding between commercial sexual activity and HIV transmission risk. We revealed that MSM-selling may contribute to both hetero- and homo- sexual transmission, which has special public health significance in China. We found that a larger number of MSM-selling had sex with females in past 6 months and the prevalence of HIV/STIs was also significantly higher among married MSM. Additionally, more MSM-selling and MSM-buying reported looking for male sex partners in other cities than NC-MSM. Given the facts that almost one-third of MSM-selling lived in study cities for ≤6 months and that short local residency was significantly related to HIV infection, domestic migration and commercial sex activities in other cities might potentially facilitate the transmission of HIV among MSM across geographical locations [20]. These findings indicated the potential bridges of HIV infection across sexes, from MSM to general female population, and then possibly to children [21].
HIV prevalence among MSM was significantly associated with co-infections with syphilis and/or HSV-2, as expected [13, 14, 22]. Genital ulcers can facilitate HIV transmission by breaching protective mucosal barriers and recruiting susceptible immune cells (e.g., CD4 T-helper cells, macrophages) to the site of infection [23], and can also create portals of entry for HIV to access susceptible cells. Another potential explanation is that HIV shares the same sexual risk factors with these STIs.
We found that MSM-selling were significantly different from MSM-buying and NC-MSM regarding socio-demographics and sexual behaviors. As well as being younger, MSM-selling were less educated, more likely to be unmarried, and highly migratory. Compared to NC-MSM, more MSM-selling had ≥10 male sex partners (46%), had sex with females (27%), used recreational drugs (59%) and had UAI (78%) in past 6 months. The profiles of characteristics among MSM-selling in this study were similar to findings in other studies on MSM sex workers [20, 24]. We can prudently suggest that the prevalence of HIV/STIs among MSM-selling in our study may rise higher than NC-MSM and MSM-buying (median ages 23 vs. 26 vs. 28 years old, respectively) after given it 3 or 5 more years of HIV exposure period, since they also had highest prevalence of syphilis and HSV-2 which were significantly associated with HIV as mentioned before.
Usually MSM seeking sexual partners via internet were involved in comparatively higher HIV risk behavior such as recreational drug use, multiple partners and unprotected anal sex [25]. A study which reviewed HIV surveillance data from 33 U.S. states between 1999 and 2008 claimed that a major online personals ad site, craigslist®, accounted for a 16% increase in HIV infection [26]. The studies from China had different results. In a prospective cohort study in China, the HIV incidence was similar between MSM who sought male sex partners online and those offline (8.6% vs 7.4%, p = 0.6) [27]. A meta-analysis that investigated the relationship between the prevalence of HIV/syphilis and the types of venues seeking male sex partners found that men seeking sex via sauna were 2.27 and 1.61 times more likely to have HIV and syphilis infection than men seeking partners online, respectively [14]. Wu et al. [21] suggested that MSM seeking male sex partners online are relatively younger, better-educated, less engagement in UAI, less involvement in commercial sex, and have more HIV knowledge. These characteristics might explain the lower prevalence of HIV/syphilis among MSM seeking male sex partners online in China.
Among all MSM participants, we found that seeking male sex partners online was not significantly related to HIV infection, but significantly related to syphilis and HSV-2 infection as a protective factor, even after adjusted for other variables. These findings were in agreement with previous studies [14, 27]. However, these results must be interpreted with some cautions. We further compared the prevalence of HIV/STI infection between MSM seeking male partners online and those offline for the three MSM subpopulations separately. Among MSM-selling, we observed that MSM seeking male sex partners online had significantly higher HIV prevalence than those seeking sex offline. The significantly lower prevalence of syphilis and HSV-2 among MSM seeking male partners online was only observed among NC-MSM, not among MSM-buying or MSM-selling. These results echoed our finding that MSM-selling is a significantly different subgroup from NC-MSM and MSM-buying. MSM-selling had higher prevalence of unprotected anal intercourse and recreational drug use. As suggested by Zhao et al., sexual risk behaviors among MSM may be influenced by venue-specific characteristics [28]. MSM-selling might use different websites to seek male sex partners and have different perception of online seeking, which might increase their HIV risk or facilitate HIV/STIs transmission. We lacked the statistical power to investigate the interaction effect of seeking male sex partners online and commercial sex activities on HIV/STI infections.
The strengths of our study include large sample size, diverse geography, and multiple recruitment venues. This study also has limitations. First, behavioral data were collected via interviewer-administered questionnaire survey, which might lead to underreporting of commercial sex due to stigma. We took several measures to minimize this information bias, including providing standardized trainings for all interviewers, not collecting any personal identifiable information from participants, and explaining to participants about the study purpose and anonymity nature prior to conducting the interviews. Second, the number of MSM with commercial sex experience was moderate, which limited the statistical power for MSM subgroup comparisons. Third, while the refusal rate in our study was low, we cannot assess the proportion of MSM who heard about the study but did not come for eligibility screening. Last, since our study sample represents MSM in urban China only, we cannot generalize findings to rural or small township residents. We speculate that MSM in rural or small town venues may have more clandestine social networks with stronger local stigma against homosexuality, with attendant differences in sexual behaviors and HIV/STI prevalence. As our study is the first study comparing the risk of HIV/STIs among Chinese MSM with different commercial sex activities, the findings provide valuable information for HIV/STI prevention interventions among these high-risk subgroups.
Conclusions
The high prevalence of risky sexual behaviors among MSM-selling may not only promote HIV acquiring and transmission risk in this specific subpopulation, but also in other MSM subpopulations and general population. Moreover, the subgroup of MSM-selling who sought male sex partners online had higher HIV prevalence. The increasing use of internet in China may influence MSM preferences in venues seeking male sex partners. All MSM in China, especially those MSM-selling subgroups seeking sex partners online, should be considered as a key population, to be given highest priority in disease surveillance and intervention programs.
Acknowledgements
The authors thank staff at Yunnan Provincial CDC, Henan Provincial CDC, Jiangsu Provincial CDC, Shandong Provincial CDC, Hunan Provincial CDC for their help with participant enrollment, laboratory tests and other project activities.
Funding
This study was supported by the Mega-projects of national science research for the 12th 5-Year Plan (2012ZX10001-006), China-Gates Foundation Cooperation Programme (2012), Innovation Team Development Programme of The Ministry of Education (2012), and Liaoning Educational Department project (LZ2014038). The preparation of this manuscript was also partially supported by U.S. National Institute of Health grant (R01AI094562).
Availability of data and materials
The data supporting the conclusions of this article will be available from Professor Shang upon request.
Authors’ contributions
JJX, HS, SHV, and HZQ: designed the conceived the research, JJX, QHH, YQY, ZXC, JZ, XXH, LL, ZW, JHF, XC, HJY, YJJ, WQG, CGZ: collected the data, CGZ, QHH, YQY, ZXC, JZ, XXH, LL: analyzed the data, CGZ, JJX and SHV: drafted the manuscript, ZW, JHF, XC, HJY, YJJ, and WQG: revised and interpreted the data. All authors edited and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study protocol and informed consent form were reviewed and approved by the institutional review board of the First Affiliated Hospital of China Medical University. Study details were explained clearly for each participant and written informed consent was obtained prior to the survey.
Abbreviations
- ELISA
Enzyme-linked immunosorbent assay
- HIV
Human immunodeficiency virus
- HSV-2
Herpes simplex virus type 2
- MSM
Men who have sex with men
- MSM-buying
MSM who buy sex
- MSM-selling
MSM who sell sex to men for money or goods
- NC-MSM
MSM who did not engage in commercial sex
- RPR
Rapid plasma reagin
- SAS
Statistical Analysis System
- SD
Standard deviations
- STIs
Transmitted infections
- TPPA
Treponema pallidum particle assay
- UAI
Unprotected anal intercourse
Additional file
Questionnair and Related Questions_Commercial Sex and Sexual behavior Survey among MSM in Big Cities of China. (PDF 82 kb)
Contributor Information
Cunge Zheng, Email: zcgwjx@gmail.com.
Jun-jie Xu, Email: xjjcmu@163.com.
Qing-hai Hu, Email: qinghaihucn@gmail.com.
Yan-qiu Yu, Email: yuyanqiu0710@163.com.
Zhen-xing Chu, Email: laochu323@163.com.
Jing Zhang, Email: zhangjing1985zj@163.com.
Xiao-xu Han, Email: xxhan@yeah.net.
Lin Lu, Email: lulin@yncdc.cn.
Zhe Wang, Email: wangzhe@hncdc.com.cn.
Ji-hua Fu, Email: fujihua@163.com.
Xi Chen, Email: chenxi161@sohu.com.
Hong-jing Yan, Email: yanhj@jscdc.cn.
Yong-jun Jiang, Email: jiangjun55555@163.com.
Wen-qing Geng, Email: windygeng@163.com.
Sten H. Vermund, Email: sten.vermund@vanderbilt.edu
Han-Zhu Qian, Phone: (86 24) 8328-2634, Email: han-zhu.qian@vanderbilt.edu.
Hong Shang, Phone: (86 24) 8328-2634, Email: hongshang100@hotmail.com.
References
- 1.van Griensven F, de Lind van Wijngaarden JW, Baral S, Grulich A. The global epidemic of HIV infection among men who have sex with men. Curr Opin HIV AIDS. 2009;4(4):300–307. doi: 10.1097/COH.0b013e32832c3bb3. [DOI] [PubMed] [Google Scholar]
- 2.Baral S, Sifakis F, Cleghorn F, Beyrer C. Elevated risk for HIV infection among men who have sex with men in low- and middle-income countries 2000–2006: a systematic review. PLoS Med. 2007;4(12):e339. doi: 10.1371/journal.pmed.0040339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chow EP, Wilson DP, Zhang J, Jing J, Zhang L. Human immunodeficiency virus prevalence is increasing among men who have sex with men in China: findings from a review and meta-analysis. Sex Transm Dis. 2011;38(9):845–857. doi: 10.1097/OLQ.0b013e31821a4f43. [DOI] [PubMed] [Google Scholar]
- 4.Fan S, Lu H, Ma X, Sun Y, He X, Li C, et al. Behavioral and serologic survey of men who have sex with men in Beijing, China: implication for HIV intervention. AIDS Patient Care STDS. 2012;26(3):148–155. doi: 10.1089/apc.2011.0277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zetola NM, Klausner JD. Syphilis and HIV infection: an update. Clin. Infect Dis. 2007;44(9):1222–1228. doi: 10.1086/513427. [DOI] [PubMed] [Google Scholar]
- 6.Beyrer C, Baral SD, van Griensven F, Goodreau SM, Chariyalertsak S, Wirtz AL, et al. Global epidemiology of HIV infection in men who have sex with men. Lancet. 2012;380(9839):367–377. doi: 10.1016/S0140-6736(12)60821-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xu J, Han X, Reilly KH, Shang H. New features of the HIV epidemic among men who have sex with men in China. Emerg Microbes Infect. 2013;2(7):e45. doi: 10.1038/emi.2013.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chow EP, Iu KI, Fu X, Wilson DP, Zhang L. HIV and sexually transmissible infections among money boys in China: a data synthesis and meta-analysis. PloS One. 2012;7(11):e48025. doi: 10.1371/journal.pone.0048025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith MD, Seal DW. Sexual Behavior, Mental Health, Substance Use, and HIV Risk Among Agency-Based Male Escorts in a Small U.S. City. Int J Sex Health. 2008;19(4):27–39. doi: 10.1300/J514v19n04_04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chemnasiri T, Netwong T, Visarutratana S, Varangrat A, Li A, Phanuphak P, et al. Inconsistent condom use among young men who have sex with men, male sex workers, and transgenders in Thailand. AIDS Educ Prev. 2010;22(2):100–109. doi: 10.1521/aeap.2010.22.2.100. [DOI] [PubMed] [Google Scholar]
- 11.Feng Y, Wu Z, Detels R, Qin G, Liu L, Wang X, et al. HIV/STD prevalence among men who have sex with men in Chengdu, China and associated risk factors for HIV infection. J Acquir Immune Defic Syndr. 2010;53(Suppl 1):S74–S80. doi: 10.1097/QAI.0b013e3181c7dd16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhao J, Cai WD, Gan YX, Zhang Y, Yang ZR, Cheng JQ, et al. A comparison of HIV infection and related risk factors between money boys and noncommercial men who have sex with men in Shenzhen, China. Sex Trans Dis. 2012;39(12):942–948. doi: 10.1097/OLQ.0b013e31826f356f. [DOI] [PubMed] [Google Scholar]
- 13.Yin YP, Chen SC, Wang HC, Wei WH, Wang QQ, Liang GJ, et al. Prevalence and risk factors of HSV-2 infection and HSV-2/HIV coinfection in men who have sex with men in China: a multisite cross-sectional study. Sex Trans Dis. 2012;39(5):354–358. doi: 10.1097/OLQ.0b013e318244aef0. [DOI] [PubMed] [Google Scholar]
- 14.Lau JT, Zhao JK, Wu XB, Gu J, Hao C. Gay saunas and the risks of HIV and syphilis transmissions in China--results of a meta-analysis. J Sex Med. 2013;10(3):642–652. doi: 10.1111/j.1743-6109.2012.02956.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.China MoHotPsRo. 2015 China AIDS Response Progress Report. Available at: http://www.unaids.org/sites/default/files/country/documents/CHN_narrative_report_2015.pdf. Accessed 20 Dec 2016.
- 16.Narayanan P, Das A, Morineau G, Prabhakar P, Deshpande GR, Gangakhedkar R, et al. An exploration of elevated HIV and STI risk among male sex workers from India. BMC Public Health. 2013;13(1):1059. doi: 10.1186/1471-2458-13-1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xu HL, Jia MH, Min XD, Zhang RZ, Yu CJ, Wang J, et al. Factors influencing HIV infection in men who have sex with men in China. Asian J Androl. 2013;15(4):545–549. doi: 10.1038/aja.2013.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Luo Y, Zhu C, Chen S, Geng Q, Fu R, Li X, et al. Risk factors for HIV and syphilis infection among male sex workers who have sex with men: a cross-sectional study in Hangzhou, China, 2011. BMJ Open. 2015;5(4):e006791. doi: 10.1136/bmjopen-2014-006791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dore GJ, Brown T, Tarantola D, Kaldor JM. HIV and AIDS in the Asia-Pacific region: an epidemiological overview. AIDS. 1998;12(Suppl B):S1–S10. [PubMed] [Google Scholar]
- 20.Chow EP, Lau JT, Zhuang X, Zhang X, Wang Y, Zhang L. HIV prevalence trends, risky behaviours, and governmental and community responses to the epidemic among men who have sex with men in China. BioMed Res Int. 2014;2014:607261. doi: 10.1155/2014/607261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu Z, Xu J, Liu E, Mao Y, Xiao Y, Sun X, et al. HIV and Syphilis Prevalence Among Men Who Have Sex With Men: A Cross-Sectional Survey of 61 Cities in China. Clin Infect Dis. 2013. Epub 2013/04/13. [DOI] [PMC free article] [PubMed]
- 22.Xiao Y, Ding X, Li C, Liu J, Sun J, Jia Y. Prevalence and correlates of HIV and syphilis infections among men who have sex with men in Chongqing Municipality, China. Sex Trans Dis. 2009;36(10):647–656. doi: 10.1097/OLQ.0b013e3181aac23d. [DOI] [PubMed] [Google Scholar]
- 23.Ward H, Ronn M. Contribution of sexually transmitted infections to the sexual transmission of HIV. Curr Opin HIV AIDS. 2010;5(4):305–310. doi: 10.1097/COH.0b013e32833a8844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tang W, Mahapatra T, Liu F, Fu G, Yang B, Tucker JD, et al. Burden of HIV and Syphilis: A Comparative Evaluation between Male Sex Workers and Non-Sex-Worker Men Who Have Sex with Men in Urban China. PloS One. 2015;10(5):e0126604. doi: 10.1371/journal.pone.0126604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.White JM, Mimiaga MJ, Reisner SL, Mayer KH. HIV sexual risk behavior among black men who meet other men on the internet for sex. J Urban Health. 2013;90(3):464–481. doi: 10.1007/s11524-012-9701-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chan J, Ghose A. Internet’s Dirty Secret: Assessing the Impact of Online Intermediaries on HIV Transmission. MIS Quarterly. 2013;38(4):955-76. Available at: http://www.krannert.purdue.edu/academics/MIS/workshop/2014/jason.pdf. Accessed 20 Dec 2016.
- 27.Li D, Li S, Liu Y, Gao Y, Yu M, Yang X, et al. HIV incidence among men who have sex with men in Beijing: a prospective cohort study. BMJ Open. 2012;2(6). Epub 2012/11/21. [DOI] [PMC free article] [PubMed]
- 28.Zhao J, Chen L, Cai WD, Tan JG, Tan W, Zheng CL, et al. HIV infection and sexual behaviors among non-commercial men who have sex with men at different venues. Arch Sex Behav. 2014;43(4):801–809. doi: 10.1007/s10508-013-0167-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supporting the conclusions of this article will be available from Professor Shang upon request.


