By the end of the 1980s and early 1990s a major shift occurred in the choice of pharmacologic therapy for hypertension. Many physicians stopped prescribing diuretics for older patients with hypertension in favour of angiotensin-converting- enzyme (ACE) inhibitors and calcium-channel blockers (CCBs), particularly in diabetic patients and patients at high risk of illness or death from cardiovascular disease. Clinicians worried about the adverse effects associated with diuretics (e.g., hyperglycemia) and embraced the purported anti-atherosclerotic and cardiovascular protective effects of these newer drugs despite the tenuous evidence for these claims. By the mid 1990s ACE inhibitors moved up to be the recommended treatment of hypertension in high-risk and diabetic patients, and CCBs lost favour because of results from small, largely observational studies that suggested increased rates of myocardial infarction, gastrointestinal bleeding and cancer associated with their use.
Given the lack of evidence at the time, we started the ALLHAT study in the early 1990s to compare the incidence of fatal and nonfatal myocardial infarction among patients randomly assigned to take a CCB (amlodipine), an ACE inhibitor (lisinopril) or a thiazide diuretic (chlorthalidone) for their hypertension. In addition to hypertension, study patients also had at least 1 other risk factor for coronary artery disease (CAD). Over 30 000 patients completed the study, which also allowed a comparison of other predefined clinical outcomes in various population subgroups (e.g., black patients v. non-black patients, and patients with diabetes v. those without diabetes). The following highlights key messages based on the results of the ALLHAT study that clinicians can immediately apply to their practices.
First and foremost, the lowering of blood pressure, and not the drug used to achieve this, remains the key variable in preventing future cardiovascular events. Contrary to other large studies that have reported benefits associated with ACE inhibitors (HOPE and EUROPA trials), we found no improvement in clinical outcomes that was independent of blood pressure lowering in patients who took lisinopril. This was true for all non-black patients, including those at high risk for cardiovascular events (those with diabetes or CAD at baseline). Among black patients, those who received lisinopril had higher blood pressure (by 4–5 mm Hg), and higher rates of cardiovascular events (19%), than those in the chlorthalidone arm. Why the different findings from those of other studies? Previous results were probably explained by modest, yet important (from a population viewpoint) improvements in blood pressure control. Moreover, our findings are consistent with overviews of clinical trials1,2 demonstrating that the reduction in risk of future cardiovascular events is proportional to the reduction in blood pressure and not the drug used to achieve it.
The development of congestive heart failure (CHF) was an important secondary outcome in our study. We found that rates of CHF were higher among patients who received either amlodipine or lisinopril than among those given chlorthalidone. Considering the (surprisingly) high rates of CHF in ALLHAT and that the diagnosis of CHF relied on individual clinical judgement rather than on a formal adjudication committee, concerns have been raised about overdiagnosis of CHF in ALLHAT.3 However, a post-hoc validation study confirmed the large majority of diagnoses of CHF that necessitated hospital care or resulted in death.4,5 A conservative interpretation would be that dihydropyridines such as amlodipine have a neutral effect (i.e., they do not improve or worsen CHF), whereas diuretics and, to a lesser extent, ACE inhibitors help to delay the onset of symptoms.
As for adverse events, CCBs were not associated with increased rates of gastrointestinal bleeding, the highest rate occurring among patients taking lisinopril. Furthermore, CCBs were not associated with increased rates of cardiac events or cancer. We observed a small increase in fasting blood glucose levels of 0.2 mmol/L6 and therefore modestly higher rates of new-onset diabetes in the chlorthalidone group compared with the ACE inhibitor and CCB groups. However, this difference may reflect an earlier diagnosis (by 1–3 years) in the chlorthalidone group rather than a true difference in rates and unlikely would affect outcomes in older patients with hypertension.
We also gleaned information about general practice patterns from the ALLHAT baseline data. Most patients at the start of the study had poor blood pressure control: more than 90% were receiving treatment, but in only 27% of them was blood pressure control actually achieved. Control rates gradually improved during the study and were over 65% by the end of the study.6 In Canada, control rates improved from 22% to 75%. The gradual increase in overall control rates was paralleled by a slowly increasing number of additional drugs prescribed (Fig. 1). Therefore, a key lesson learned was that most hypertensive patients require more than 1 medication for blood pressure control.
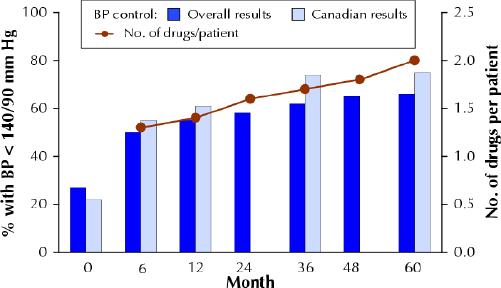
Fig. 1: Blood pressure (BP) control rates during the ALLHAT study. Bars represent proportion of participants who achieved target BP (< 140/90 mm Hg) among those attending follow-up visits. Line represents mean number of antihypertensive drugs prescribed per patient.
Based on current information, physicians should consider once again thiazide diuretics an essential component of antihypertensive treatment for most older patients. There are very few reasons (e.g., gout, allergic reaction) for not starting antihypertensive therapy with a thiazide diuretic and then adding a CCB or ACE inhibitor, or both, for blood pressure control. Although hydrochlorothiazide (HCTZ) is the more commonly used thiazide diuretic, chlorthalidone is 1.5 to 2 times as potent and has a longer duration of action. If HCTZ is used, it may be started at a dose of 12.5 mg/d and increased to 25 mg/d as tolerated; in some patients (e.g., those with obesity or decreased renal function), up to 50 mg/d may be required.
Accountability for blood pressure control
We know that blood pressure control can be achieved in most older hypertensive patients. In our study, physicians received regular report cards on control rates among their patients and feedback on how to improve blood pressure control. This probably helped to overcome the reluctance of many physicians to prescribe more than 1 antihypertensive medication to their patients. Given that this strategy was effective within the confines of this community-based clinical trial, perhaps one of the most important lessons learned was that evaluation of physicians' performance may be necessary to achieve better population-based blood pressure control. Low control rates reflect poor prevention efforts by the health care system, are unnecessary and lead to substantial premature cardiovascular disease and death.
Issuing yearly guidelines and recommending CME per se make only a marginal difference in actual practice. To make an immediate and substantial impact, standards of care should be established7 and a process for evaluating the performance of individual health care providers developed. The evaluation process could start immediately with audits of physicians' charts; in the future, this will be greatly facilitated once electronic medical records become standardized and common.
Information on quality of care and blood pressure control rates should be made available to the public. A person with hypertension has the right to know the quality of care provided by his or her physician relative to the care received by others. One may debate whether differences in quality of care also should be reflected in physicians' remunerations, as is being implemented in the United Kingdom.
Frans H.H. Leenen Principal Investigator for ALLHAT Region 9 (Canada) University of Ottawa Heart Institute Ottawa, Ont.
References
- 1.Turnbull F; Blood Pressure Lowering Treatment Trialists' Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet 2003;362: 1527-35. [DOI] [PubMed]
- 2.Staessen JA, Wang JG, Thijs L. Cardiovascular prevention and blood pressure reduction: a quantitative overview updated until 1 March 2003. J Hypertens 2003;21:1055-76. [DOI] [PubMed]
- 3.Messerli FH. ALLHAT, or the soft science of the secondary end point. Ann Intern Med 2003;139:777-80. [DOI] [PubMed]
- 4.Piller LB, Davis BR, Cutler JA, Cushman WC, Wright JT Jr, Williamson JD, et al. Validation of heart failure events in the antihypertensive and lipid lowering treatment to prevent heart attack trial (ALLHAT): participants assigned to doxazosin and chlorthalidone. Curr Control Trials Cardiovasc Med 2002;3:10-19. [DOI] [PMC free article] [PubMed]
- 5.Davis BR, Furberg CD, Wright JT, Cutler JA, Whelton P, for the ALLHAT Collaborative Research Group. ALLHAT: Setting the record straight. Ann Intern Med 2004;141: 39-46. [DOI] [PubMed]
- 6.ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) [published errata in JAMA 2003; 289(2):178 and 2004; 291 (18): 2196]. JAMA 2002;288: 2981-97. [DOI] [PubMed]
- 7.Asch SM, Kerr EA, Lapuerta P, Law A, McGlynn EA. A new approach for measuring quality of care for women with hypertension. Arch Intern Med 2001; 161: 1329-35. [DOI] [PubMed]


