Abstract
Background
This study aimed at identifying preoperative predictors of patient-reported outcomes after total knee arthroplasty (TKA) and at investigating their association with the outcomes over time.
Methods
We used data from 2080 patients from the Knee Arthroplasty Trial who received primary TKA in the United Kingdom between July 1999 and January 2003. The primary outcome measure was the Oxford knee score (OKS) collected annually over 10 years after TKA. Preoperative predictors included a range of patient characteristics and clinical conditions. Mixed-effects linear regression model analysis of repeated measurements was used to identify predictors of overall OKS, and pain and function subscale scores over 10 years, separately.
Results
Worse preoperative OKS, worse mental well-being, body mass index greater than 35 kg/m2, living in the most deprived areas, higher American Society of Anesthesiologists grade, presence of comorbidities, and history of previous knee surgery were associated with worse overall OKS over 10 years after surgery. The same predictors were identified for pain and function subscale scores, and for both long-term (10 years) and short-to-medium-term outcomes (1 and 5 years). However, fitted models explained more variations in function and shorter-term outcomes than in pain and longer-term outcomes, respectively.
Conclusion
The same predictors were identified for pain and functional outcomes over both short-to-medium term and long term after TKA. Within the factors identified, functional and shorter-term outcomes were more predictable than pain and longer-term outcomes, respectively. Regardless of their preoperative characteristics, on average, patients achieved substantial improvement in pain over time, although improvement for function was less prominent.
Keywords: epidemiology, osteoarthritis, knee arthroplasty, patient-reported outcome, Oxford knee score
Total knee arthroplasty (TKA) is a commonly performed and effective surgical intervention to relieve pain and restore function in severely damaged knee joints. As the burden of knee arthritis keeps increasing, the number of TKAs performed is reported to be increasing every year [1]. However, variation in postoperative outcomes has been observed among patients, with up to 20% of patients dissatisfied with their outcomes [2]. It is important, therefore, for both clinicians and patients to understand the prognosis of surgery on an individual basis so as to decide whether to undergo TKA and whether it is necessary to enhance treatment protocols. In recent years, patient-reported outcome measures (PROMs) have been widely used to assess clinical outcomes from patients’ perspective, which is believed to better reflect patients’ health status and quality of life 3, 4, 5.
A range of potential predictors of PROMs after TKA have been identified within the literature, including preoperative level of pain and function 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, age 6, 7, 8, 12, 13, 16, 17, 18, 19, 20, sex 6, 8, 9, 13, 16, 19, 21, body mass index (BMI) 13, 15, 18, 20, comorbidities 6, 7, 8, 9, 12, 13, 14, 15, 20, 22, preoperative mental health 9, 10, 12, 18, 20, 22, and surgeon volume [22]. Most of these studies had a follow-up less than 5 years after TKA. Very few studies examined the effect of predictors over time [23]. Several studies suggested that predictors of pain were not necessarily the same as function 11, 13, 18, 19, 22, 24, 25. It should be noted, however, that these studies distinguished pain and function based on the wording of questions without formal statistical validation.
Using data from the Knee Arthroplasty Trial (KAT) 26, 27 which included patients receiving TKAs in the United Kingdom, this study aimed at the following: (1) identifying preoperative predictors of PROMs as measured by the Oxford knee score (OKS) over 10 years after primary TKA, with pain and function analyzed separately and (2) investigating their effect over short-to-medium-term outcomes.
Materials and Methods
The study used data from the KAT, a pragmatic, multicenter, randomized, controlled trial 26, 27 (International Standard Randomized Trial No. ISRCTN45837371). From July 1999 to January 2003, a total of 2352 patients across 34 centers in the United Kingdom were randomly allocated to primary knee arthroplasty with metal-backed tibial component or not; patellar resurfacing or not; mobile bearing or not; or, TKA or unicompartmental arthroplasty.
Outcome Variables
The primary outcome measure was the OKS [28] completed by patients at baseline (preoperative), at 1 year after operation, and annually thereafter by postal questionnaire. The OKS is a validated questionnaire specifically developed to assess patient’s pain and function status after knee arthroplasty. It comprises 12 questions, each with 5 responses on a Likert scale. Each question is scored from 0 (most severe pain or most limited function) to 4 (no pain or no function limitation). An overall OKS is created by summing the scores for each question, ranging from 0 (the worst outcome) to 48 (the best outcome) [29]. OKS pain and function subscale scores were calculated according to Harris et al [30]: the function subscale score was obtained by summing the scores for OKS questions 2, 3, 7, 11, and 12 (ranging from 0 to 20) and the pain subscale score by summing scores for the other 7 questions (ranging from 0 to 28). Higher subscale scores indicate better function or less pain. Patients were censored for follow-up if they died or received revision surgery within 10 years after the primary TKA.
Predictor Variables
Patient characteristics including age at operation (<60, 60-70, 70-80, or 80+ years), sex, marital status (married or living alone), and BMI (<25, 25-30, 30-35, or >35 kg/m2) were collected by local research nurses using patient entry questionnaires and routine medical database [27]. The Index of Multiple Deprivation 2004 was used as a measure of social deprivation [31]. Residential postcodes of patients at randomization were linked to the Lower Layer Super Output Areas. A higher score indicates higher rate of deprivation in that area. The Index of Multiple Deprivation 2004 was analyzed using quintiles in this study.
Preoperative mental well-being was assessed using the 12-Item Short Form Health Survey Mental Component Summary (SF-12 MCS) [32], with higher scores indicating better mental well-being. In the analysis, SF-12 MCS score was categorized into 2 groups: <50 and 50+. This was based on the sample distribution in this study (the mean of preoperative SF-12 MCS was 49.9) and also on previous studies [33].
Preoperative clinical conditions included diagnosis of arthritis (osteoarthritis or rheumatoid arthritis), joints affected (one knee, both knees, or general), presence of comorbidities, history of previous surgery, and the American Society of Anesthesiologists (ASA) grade. ASA grading system is a standard assessment of the patient’s general physical health before surgery [34]. In the KAT study, the range of ASA grade is from 1 (fit and healthy) to 4 (symptomatic with severe restriction on daily activities). Grades 3 and 4 were collapsed into 1 group to ensure a sufficient number of patients.
Statistical Methods
STATA 13.0 (Statacorp, College Station, TX) was used for all statistical analyses. Complete case analysis can be biased [35]. Moreover, missing data in several variables often lead to a substantial loss of observations, reducing the power and precision of estimates. Multiple imputation has been proposed to overcome this problem [36]. In this study, multiple imputation by chained equations procedures in STATA were used [37]. We included all predictor variables as described above and the outcome variable in each imputation process. For each analysis (at 1 year, over 5 years, and over 10 years), a total of 200 imputed datasets were created separately. The statistically significant level was set at .05.
Predictors of Overall OKS, and Pain and Function Subscale Scores Over Time
To identify predictors of continuous outcomes over 10 years, multilevel, mixed-effects linear regression with an unstructured variance-covariance matrix was conducted to take into account of clustering on the same patient. For each predictor variable as described previously, a univariable model adjusting for preoperative OKS was performed. Variables with P < .20 in the univariable models were included in the multivariable model. Age at operation, sex, preoperative OKS, and year of follow-up were included as a priori predictors. Fractional polynomial regression modelling was used to explore evidence of nonlinear relationships for continuous variables. An interaction term was fitted between the predictor variable and year of follow-up to see whether the effect of predictors depended on time. The same process was repeated for overall OKS , and pain and function subscale scores, respectively. To better understand the effect of predictor variables over medium-term and short-term outcomes, we repeated the above process for OKS outcomes over 5 years and at 1 year after TKA.
Changes in Overall OKS, and Pain and Function Subscale Scores over 10-Year Time, Stratified by Identified Predictors
For analyses over 10 years, after the final model was built, the outcome was expanded to include both baseline OKS (year 0) and follow-up OKS (year 1 through to year 10) and an interaction term was fitted between predictors that have been identified as statistically significant and year of follow-up. Average marginal effects were obtained to show the adjusted mean OKS over time across categories of important predictors. The same process was repeated for overall OKS, and OKS pain and function subscale scores, respectively.
Results
Description of the Study Sample
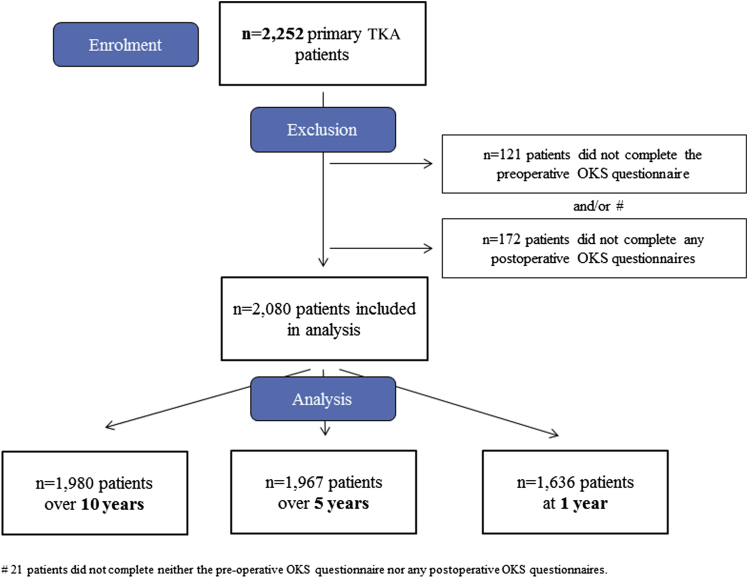
One hundred patients were excluded from this study because they received unicompartmental knee arthroplasty, withdrew from the trial before surgery, or died before the first follow-up of the trial. Of the remaining 2252 patients receiving TKA, 75.8% of patients completed the OKS at 1 year and 41.6% responded at 10 years after TKA (254 [11.3%] patients died within 10 years and 101 [4.5%] patients received revision surgery during follow-up). Patients were included for analysis if they completed the preoperative and at least 1 postoperative OKS questionnaire during follow-up, which included 1980 (87.9%) for analyses over 10 years, 1967 (87.3%) over 5 years, and 1636 (72.6%) at 1 year (Fig. 1). A comparison of the patients who were included and excluded from analysis over 10 years is described in Supplementary Table 1. Patients included tended to be younger, had better preoperative OKS, had better mental well-being, and had lower ASA grading system. They were also more likely to have a history of previous knee surgery or present with comorbidities.
Fig. 1.
A flow diagram of patients included and excluded for each analysis. TKA, total knee arthroplasty; OKS, Oxford knee score.
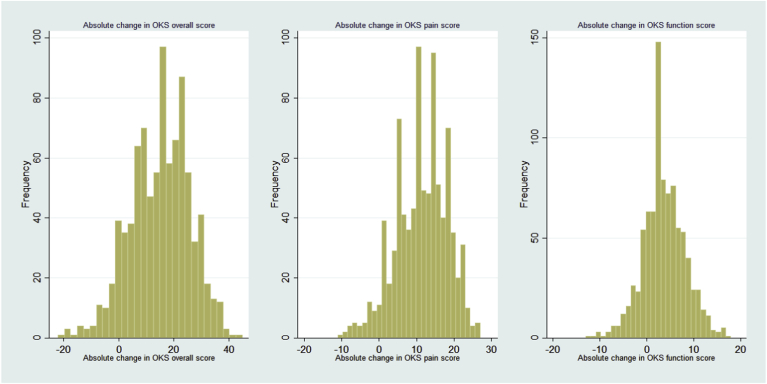
The mean preoperative overall OKS was 18.2 ± 7.5 (mean ± standard deviation), with a pain subscale score of 9.5 ± 4.6 and function subscale score of 8.5 ± 3.5. Histograms of the absolute difference between year 10 and preoperative OKS (Supplementary Fig. 1) suggested that whereas a small number of patients received no improvement or got worse at 10 years after TKA, the majority achieved improvement in overall OKS, as well as pain and function subscale scores.
Supplementary Fig. 1.
Distribution of absolute differences in overall Oxford knee score (OKS), and pain and function subscale scores between baseline and 10-year follow-up after primary total knee arthroplasty.
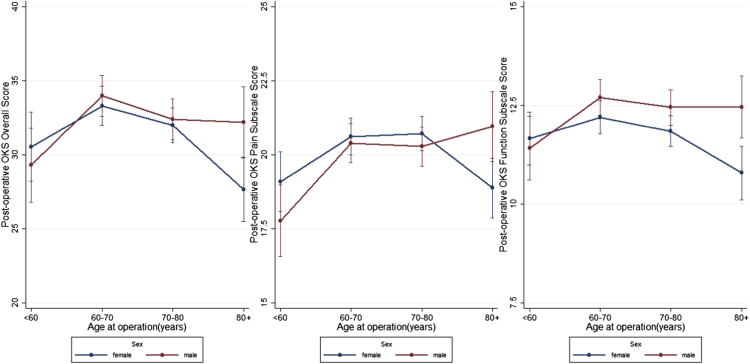
Predictors of OKS Over Time After TKA
A number of variables were identified as statistically significant predictors of postoperative OKS over 10 years after TKA (Table 1, Table 2, Table 3, last column). Better baseline scores were associated with better postoperative scores over 10 years, while worse mental well-being (SF-12 MCS < 50), BMI > 35 kg/m2, living in more deprived areas, higher ASA grade, presence of comorbidities, and history of previous knee surgery were associated with worse outcomes. A statistically significant interaction was found between age at the time of operation and sex (Supplementary Fig. 2). For women, patients aged younger than 60 or older than 80 at the time of operation presented worse outcomes over 10 years, while for men, only those younger than 60 showed statistically significantly worse outcomes. For patients younger than 60, women had better outcome while for those older than 80, men did better. There was also strong evidence that all OKS decreased over time, with an average annual decrease of 0.3 points for overall scores, and 0.2 points for both pain and function subscale scores. Predictors and their direction of effect were the same for both pain and functional outcomes, whereas difference was observed in the R2 statistic. The final model of overall OKS explained 14.5% of variability in outcome, whereas the model for function explained 20.7% and pain only 10.1%. No significant interaction was found between predictors and year of follow-up. For outcomes over 5 years and at 1 year, the same predictors were identified but the fitted models explained slightly more of the variability in each outcome measure (Table 1, Table 2, Table 3, first column for outcomes at 1 year and second column for outcomes over 5 years).
Table 1.
Multivariable Analysis of Overall OKS at 1 Year, and over 5 and 10 Years After TKA.
| Variables | At 1 y (n = 1636) |
Over 5 y (n = 1967) |
Over 10 y (n = 1980) |
|---|---|---|---|
| Multivariablea Coefficient (95% CI) |
Multivariablea Coefficient (95% CI) |
Multivariablea Coefficient (95% CI) |
|
| R2 = 18.76% | R2 = 15.62% | R2 = 14.51% | |
| Patient characteristics | |||
| Sex | |||
| Female | 0 | 0 | 0 |
| Male | 0.44 (−1.05, 1.92) | 0.33 (−0.96, 1.61) | 0.31 (−0.96, 1.58) |
| Age at operation (y) | |||
| <60 | −0.86 (−3.18, 1.46) | −2.09 (−3.89, −0.30)∗ | −1.96 (−3.73, −0.20)∗ |
| 60-70 | 0 | 0 | 0 |
| 70-80 | 0.74 (−0.59, 2.08) | 0.07 (−1.11, 1.25) | −0.28 (−1.45, 0.88) |
| 80+ | −2.75 (−4.98, −0.51)∗ | −2.92 (−4.73, −1.10)∗∗ | −3.23 (−5.03, −1.42)∗∗∗ |
| Sex#age at operationb | |||
| Male#age < 60 | −4.29 (−7.80, −0.78)∗ | −1.90 (−4.63, 0.83) | −1.94 (−4.64, 0.76) |
| Male#age 60-70 | −0.53 (−2.48, 1.41) | −0.10 (−1.83, 1.62) | −0.15 (−1.86, 1.55) |
| Male#age 80+ | 2.74 (−0.36, 5.84)† | 3.57 (0.90, 6.23)∗∗ | 3.42 (0.76, 6.08)∗ |
| Marital status | |||
| Married | 0 | 0 | 0 |
| Living alone | −0.48 (−1.48, 0.52) | −0.65 (−1.52, 0.21)† | −0.72 (−1.59, 0.15)† |
| BMI (kg/m2) | |||
| <25 | 0 | 0 | 0 |
| 25-30 | −0.33 (−1.55, 0.90) | −0.36 (−1.45, 0.73) | −0.36 (−1.40, 0.69) |
| 30-35 | −1.84 (−3.23, −0.46)∗∗ | −0.95 (−2.11, 0.21)† | −0.92 (−2.06, 0.21)† |
| >35 | −1.97 (−3.62, −0.32)∗ | −1.67 (−3.07, −0.27)∗ | −1.79 (−3.12, −0.46)∗∗ |
| IMD 2004 quintiles | |||
| 1st (most deprived) | 0 | 0 | 0 |
| 2nd | 1.22 (−0.82, 3.25) | 0.39 (−0.53, 1.32) | 0.39 (−0.28, 1.05) |
| 3rd | 2.38 (0.47, 4.29)∗ | 1.08 (0.19, 1.98)∗ | 0.82 (0.21, 1.43)∗∗ |
| 4th | 2.70 (0.86, 4.53)∗∗ | 1.07 (0.17, 1.97)∗ | 0.96 (0.35, 1.58)∗∗ |
| 5th (most affluent) | 1.97 (0.04, 3.91)∗ | 1.08 (0.15, 2.02)∗ | 0.94 (0.26, 1.61)∗∗ |
| Preoperative patient-reported health status | |||
| Preop overall OKS | 0.35 (0.29, 0.42)∗∗∗ | 0.39 (0.34, 0.45)∗∗∗ | 0.41 (0.35, 0.46)∗∗∗ |
| Preop SF-12 MCS | |||
| <50 | 0 | 0 | 0 |
| 50+ | 1.65 (−0.70, 2.61)∗∗ | 1.77 (0.96, 2.57)∗∗∗ | 1.61 (0.81, 2.40)∗∗∗ |
| Preoperative clinical conditions | |||
| ASA grade | |||
| Fit and healthy | 0 | 0 | 0 |
| Asymptomatic | −1.04 (−2.25, 0.17)† | −0.81 (−1.83, 0.21)† | −0.66 (−1.60, 0.28) |
| Symptomatic | −2.69 (−4.25, −1.13)∗∗ | −2.19 (−3.43, −0.95)∗∗ | −1.91 (−3.07, −0.75)∗∗ |
| Previous knee surgery | |||
| No | 0 | 0 | 0 |
| Yes | −1.78 (−2.72, −0.84)∗∗∗ | −1.24 (−2.07, −0.42)∗∗ | −1.17 (−1.98, −0.36)∗∗ |
| Comorbidities | |||
| No | 0 | 0 | 0 |
| Yes | −3.00 (−4.35, −1.65)∗∗∗ | −2.37 (−3.50, −1.24)∗∗∗ | −2.24 (−3.36, −1.12)∗∗∗ |
| Year of follow-up | −0.16 (−0.25, −0.06)∗∗ | −0.33 (−0.38, −0.27)∗∗∗ | |
Coefficient: the regression coefficient represents the difference in outcome compared with the reference group. A positive value indicates that the group has better postoperative pain/function.
OKS, Oxford knee score; TKA, total knee arthroplasty; CI, confidence interval; IMD, Index of Multiple Deprivation; BMI, body mass index; SF-12 MCS, 12-item Short-Form Health Survey Mental Component Summary; ASA, American Society of Anesthesiologists.
∗∗∗<.001; ∗∗<.01; ∗<.05; †<.20.
In the multivariable models, all variables are mutually adjusted and an interaction term between age and sex was included.
Interaction between sex and age at operation.
Table 2.
Multivariable Analysis of OKS Pain Subscale Score at 1 Year, and Over 5 and 10 Years After TKA.
| Variables | At 1 y (n = 1636) |
Over 5 y (n = 1967) |
Over 10 y (n = 1980) |
|---|---|---|---|
| Multivariable Coefficient (95% CI)a |
Multivariable Coefficient (95% CI)a |
Multivariable Coefficient (95% CI)a |
|
| R2 = 14.85% | R2 = 10.89% | R2 = 10.10% | |
| Patient characteristics | |||
| Sex | |||
| Female | 0 | 0 | 0 |
| Male | −0.29 (−1.23, 0.65) | −0.23 (−1.03, 0.57) | −0.22 (−1.01, 0.56) |
| Age at operation (y) | |||
| <60 | −0.78 (−2.29, 0.73) | −1.53 (−2.65, −0.40)∗∗ | −1.52 (−2.63, −0.42)∗∗ |
| 60-70 | 0 | 0 | 0 |
| 70-80 | 0.54 (−0.31, 1.39) | 0.27 (−0.47, 1.01) | 0.11 (−0.62, 0.83) |
| 80+ | −1.50 (−2.94, −0.07)∗ | −1.61 (−2.75, −0.48)∗∗ | −1.74 (−2.86, −0.61)∗∗ |
| Sex#age at operationb | |||
| Male#age <60 | −2.38 (−4.67, −0.09)∗ | −1.06 (−2.77, 0.64) | −1.10 (−2.78, 0.58) |
| Male#age 60-70 | −0.21 (−1.45, 1.03) | −0.11 (−1.19, 0.96) | −0.22 (−1.28, 0.84) |
| Male#age 80+ | 1.92 (−0.04, 3.88)† | 2.44 (0.77, 4.11)∗∗ | 2.30 (0.64, 3.96)∗∗ |
| Marital status | |||
| Married | 0 | 0 | 0 |
| Living alone | −0.38 (−1.01, 0.25) | −0.43 (−0.97, 0.11)† | −0.46 (−1.00, 0.07)† |
| BMI (kg/m2) | |||
| <25 | 0 | 0 | 0 |
| 25-30 | −0.33 (−1.10, 0.44) | −0.28 (−0.96, 0.40) | −0.27 (−0.92, 0.39) |
| 30-35 | −1.28 (−2.17, −0.39)∗∗ | −0.63 (−1.35, 0.09)† | −0.60 (−1.29, 0.08)† |
| >35 | −1.25 (−2.31, −0.19)∗ | −1.00 (−1.86, −0.14)∗ | −1.11 (−1.93, −0.28)∗∗ |
| IMD 2004 quintiles | |||
| 1st (most deprived) | 0 | 0 | 0 |
| 2nd | 0.75 (−0.54, 2.04) | 0.26 (−0.35, 0.86) | 0.25 (−0.20, 0.70) |
| 3rd | 1.49 (0.30, 2.69)∗ | 0.74 (0.14, 1.35)∗ | 0.55 (0.13, 0.97)∗ |
| 4th | 1.60 (0.43, 2.77)∗∗ | 0.71 (0.11, 1.31)∗ | 0.63 (0.21, 1.05)∗∗ |
| 5th (most affluent) | 1.18 (−0.06, 2.42)† | 0.72 (0.11, 1.34)∗ | 0.62 (0.17, 1.06)∗∗ |
| Preoperative patient-reported health status | |||
| Preop OKS pain score | 0.29 (0.22, 0.36)∗∗∗ | 0.30 (0.24, 0.35)∗∗∗ | 0.31 (0.26, 0.37)∗∗∗ |
| Preop SF-12 MCS | |||
| <50 | 0 | 0 | 0 |
| 50+ | 1.11 (0.51, 1.72)∗∗∗ | 1.26 (0.76, 1.76)∗∗∗ | 1.16 (0.68, 1.65)∗∗∗ |
| Preoperative clinical conditions | |||
| ASA grade | |||
| Fit and healthy | 0 | 0 | 0 |
| Asymptomatic | −0.56 (−1.33, 0.21)† | −0.41 (−1.05, 0.23) | −0.35 (−0.94, 0.25) |
| Symptomatic | −1.60 (−2.60, −0.60)∗∗ | −1.33 (−2.11, −0.55)∗∗ | −1.17 (−1.90, −0.44)∗∗ |
| Previous knee surgery | |||
| No | 0 | 0 | 0 |
| Yes | −1.20 (−1.79, −0.59)∗∗∗ | −0.81 (−1.33, −0.30)∗∗ | −0.75 (−1.25, −0.25)∗∗ |
| Comorbidities | |||
| No | 0 | 0 | 0 |
| Yes | −1.73 (−2.61, −0.85)∗∗∗ | −1.34 (−2.04, −0.63)∗∗∗ | −1.29 (−1.99, −0.60)∗∗∗ |
| Year of follow-up | −0.04 (−0.10, 0.03) | −0.15 (−0.19, −0.12)∗∗∗ | |
Coefficient: the regression coefficient represents the difference in outcome compared with the reference group. A positive value indicates that the group has better postoperative pain/function.
OKS, Oxford knee score; TKA, total knee arthroplasty; CI, confidence interval; IMD, Index of Multiple Deprivation; BMI, body mass index; SF-12 MCS, 12-item Short-Form Health Survey Mental Component Summary; ASA, American Society of Anesthesiologists.
∗∗∗<.001; ∗∗<.01; ∗<.05; †<.20.
In the multivariable models, all variables are mutually adjusted and an interaction term between age and sex was included.
Interaction between sex and age at operation.
Table 3.
Multivariable Analysis of OKS Function Subscale Score at 1 Year, and Over 5 and 10 Years After TKA.
| Variables | At 1 y (n = 1636) |
Over 5 y (n = 1967) |
Over 10 y (n = 1980) |
|---|---|---|---|
| Multivariable Coefficient (95% CI)a |
Multivariable Coefficient (95% CI)a |
Multivariable Coefficient (95% CI)a |
|
| R2 = 23.76% | R2 = 22.30% | R2 = 20.72% | |
| Patient characteristics | |||
| Sex | |||
| Female | 0 | 0 | 0 |
| Male | 0.66 (0.04, 1.28)∗ | 0.49 (−0.05, 1.03)† | 0.49 (−0.05, 1.02)† |
| Age at operation (y) | |||
| <60 | −0.13 (−1.07, 0.80) | −0.65 (−1.40, 0.09)† | −0.53 (−1.26, 0.21) |
| 60-70 | 0 | 0 | 0 |
| 70-80 | 0.24 (−0.33, 0.81) | −0.16 (−0.66, 0.33) | −0.35 (−0.84, 0.13) |
| 80+ | −1.20 (−2.13, −0.27)∗ | −1.24 (−2.00, −0.49)∗∗ | −1.42 (−2.18, −0.67)∗∗∗ |
| Sex#age at operationb | |||
| Male#age <60 | −1.84 (−3.24, −0.44)∗ | −0.74 (−1.88, 0.39) | −0.76 (−1.89, 0.36) |
| Male#age 60-70 | −0.29 (−1.11, 0.52) | 0.07 (−0.64, 0.79) | 0.11 (−0.60, 0.82) |
| Male#age 80+ | 0.91 (−0.42, 2.24) | 1.22 (0.11, 2.33)∗ | 1.20 (0.09, 2.30)∗ |
| Marital status | |||
| Married | 0 | 0 | 0 |
| Living alone | −0.11 (−0.53, 0.31) | −0.23 (−0.59, 0.14) | −0.26 (−0.63, 0.10) |
| BMI (kg/m2) | |||
| <25 | 0 | 0 | 0 |
| 25-30 | 0.02 (−0.51, 0.55) | −0.08 (−0.54, 0.38) | −0.09 (−0.54, 0.36) |
| 30-35 | −0.55 (−1.14, 0.04)† | −0.32 (−0.82, 0.17) | −0.34 (−0.84, 0.16) |
| >35 | −0.75 (−1.44, −0.06)∗ | −0.73 (−1.32, 0.14)∗ | −0.75 (−1.33, −0.17)∗ |
| IMD 2004 quintiles | |||
| 1st (most deprived) | 0 | 0 | 0 |
| 2nd | 0.50 (−0.34, 1.33) | 0.16 (−0.22, 0.54) | 0.15 (−0.13, 0.44) |
| 3rd | 0.92 (0.12, 1.72)∗ | 0.40 (0.04, 0.77)∗ | 0.31 (0.05, 0.57)∗ |
| 4th | 1.13 (0.37, 1.89)∗∗ | 0.42 (0.04, 0.79)∗ | 0.38 (0.12, 0.64)∗∗ |
| 5th (most affluent) | 0.84 (0.05, 1.62)∗ | 0.42 (0.04, 0.80)∗ | 0.36 (0.08, 0.64)∗ |
| Preoperative patient-reported health status | |||
| Preop OKS function score | 0.40 (0.34, 0.47)∗∗∗ | 0.46 (0.41, 0.51)∗∗∗ | 0.47 (0.42, 0.52)∗∗∗ |
| Preop SF-12 MCS | |||
| <50 | 0 | 0 | 0 |
| 50+ | 0.57 (0.17, 0.97)∗∗ | 0.59 (0.25, 0.93)∗∗ | 0.54 (0.20, 0.88)∗∗ |
| Preoperative clinical conditions | |||
| ASA grade | |||
| Fit and healthy | 0 | 0 | 0 |
| Asymptomatic | −0.46 (−0.97, 0.05)† | −0.39 (−0.82, 0.03)† | −0.32 (−0.72, 0.08)† |
| Symptomatic | −1.05 (−1.70, −0.40)∗∗ | −0.87 (−1.39, −0.35)∗∗ | −0.77 (−1.27, −0.28)∗∗ |
| Previous knee surgery | |||
| No | 0 | 0 | 0 |
| Yes | −0.58 (−0.97, −0.19)∗∗ | −0.43 (−0.77, −0.08)∗ | −0.42 (−0.76, −0.08)∗ |
| Comorbidities | |||
| No | 0 | 0 | 0 |
| Yes | −1.24 (−1.77, −0.70)∗∗∗ | −1.03 (−1.50, −0.57)∗∗∗ | −0.96 (−1.43, −0.50)∗∗∗ |
| Year of follow-up | −0.11 (−0.15, −0.07)∗∗∗ | −0.17 (−0.20, −0.15)∗∗∗ | |
Coefficient: the regression coefficient represents the difference in outcome compared with the reference group. A positive value indicates that the group has better postoperative pain/function.
OKS, Oxford knee score; TKA, total knee arthroplasty; CI, confidence interval; IMD, Index of Multiple Deprivation; BMI, body mass index; SF-12 MCS, 12-item Short-Form Health Survey Mental Component Summary; ASA, American Society of Anesthesiologists.
∗∗∗<.001; ∗∗<.01; ∗<.05; †<.20.
In the multivariable models, all variables are mutually adjusted and an interaction term between age and sex was included.
Interaction between sex and age at operation.
Supplementary Fig. 2.
Marginal effect (95% confidence interval) of age-groups on postoperative OKS divided by sex and controlling for preoperative variables retained into the final regression model.
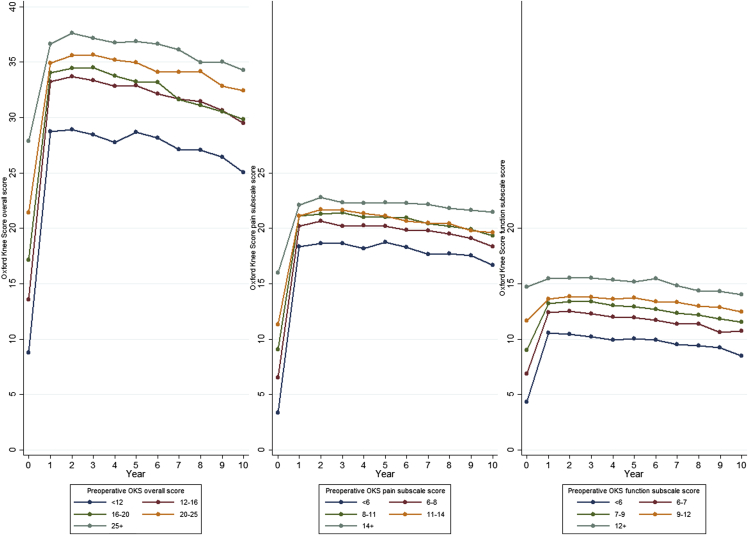
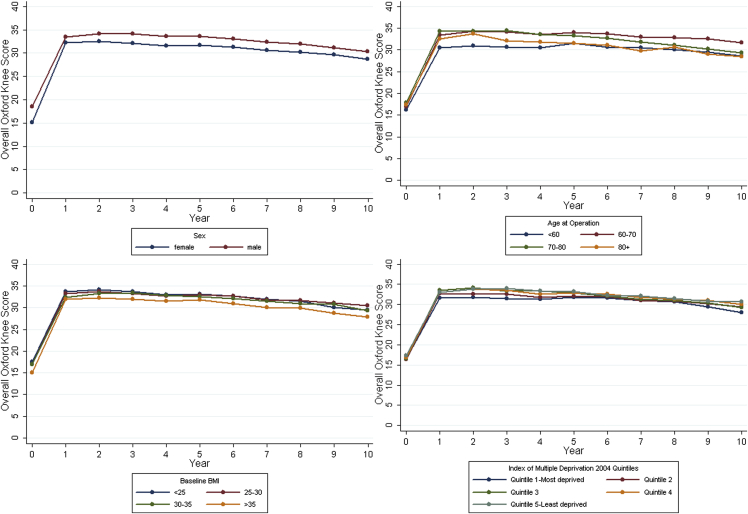
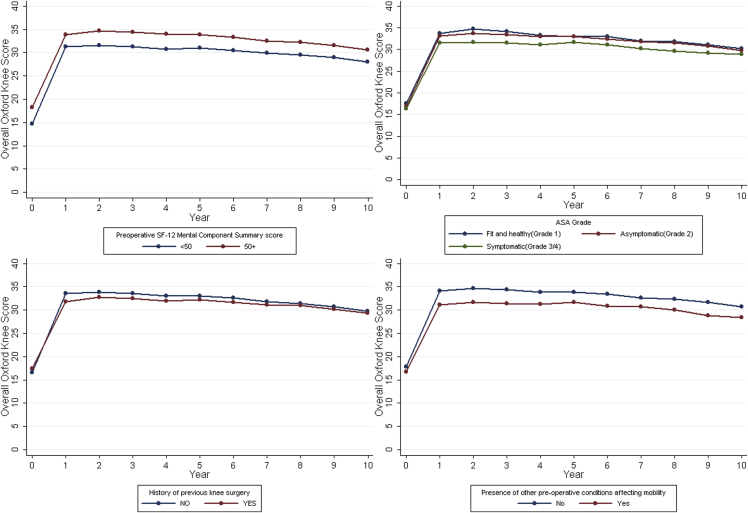
Changes in OKS Over Time, Stratified by Important Predictors
Fig. 2, Fig. 3, Fig. 4 describe the change in outcomes over time stratified by predictors identified. The graphs highlighted again that the effect of predictors on pain and functional outcomes remained almost unchanged over time. They also demonstrated that despite the small size of difference in the attained postoperative outcomes among patients with different preoperative characteristics, on average, these patients achieved substantial improvement in pain from preoperative level regardless of which group they belong to. For functional outcomes, on average, the improvement was less prominent especially for patients whose preoperative function score was among the highest quintile.
Fig. 2.
Distribution of absolute differences in overall OKS, and pain and function subscale scores between baseline and 10-year follow-up after primary TKA.
Fig. 3.
Change in overall OKS over 10 years after primary TKA, stratified by preoperative patient characteristics and controlled for variables retained into the final regression model. The best possible score for overall OKS, and pain and function subscale scores is 48, 28, and 20, respectively. BMI, body mass index.
Fig. 4.
Change in overall OKS over 10 years after primary TKA, stratified by preoperative health status and controlled for variables retained into the final regression model. The best possible score for overall OKS, and pain and function subscale score is 48, 28, and 20, respectively. ASA, American Society of Anesthesiologists.
Discussion
Main Findings
Using a large prospective cohort of patients receiving primary TKA in the United Kingdom, we identified a number of statistically significant predictors of patient-reported pain and functional outcomes as measured by the OKS over 10 years after operation. Worse preoperative OKS, worse mental well-being (SF-12 MCS < 50), BMI > 35 kg/m2, living in the most deprived areas, higher ASA grade, presence of comorbidities, and history of previous knee surgery were associated with worse postoperative outcome. A statistically significant interaction was found between sex and age at the time of operation. Predictors and their direction of effect were the same for both pain and functional outcomes, and for both short-term and medium-term results. Within the predictors identified, functional outcome was more predictable than pain, and shorter-term outcomes more predictable than longer-term outcomes. There was a slight yet statistically significant decrease in postoperative OKS over time.
What Is Already Known?
In line with previous studies, we found that worse baseline scores, living in the most deprived areas, history of previous knee surgery, presence of comorbidities, and worse mental well-being were associated with worse short-term and long-term OKS. The association between age and postoperative PROMs is inconclusive in the literature, with some indicating no relationship [7], while others showing that older age is related to poorer outcomes 11, 12, 13, 19, 38. Most previous studies analyzed age by fitting a linear relationship with the outcome. In this study, a nonlinear relationship was evident and the effect varied by sex. For patients younger than 60, women had better outcome while for those older than 80, men did better. Possible explanation might be that daily activities are more physically demanding for younger male patients, while older female patients might have more disabling conditions or experience more pain.
Several studies suggested that predictors of pain were not necessarily the same as function 11, 13, 18, 19, 22, 24, 25. One of them used OKS as the outcome measure [11]. In that study, the authors extracted pain and function subscale scores based on face validity (ie, the wording of questions) and looked at outcomes 6 months after TKA. In this study, we extracted subscale scores according to Harris et al [30] who distinguished pain and function scores using formal factor analysis. Different from what they have found, the same predictors were identified for both pain and function outcomes in this study.
Fitted models explained more variability in functional outcome than in pain over 10 years (20.7% vs 10.1%). It is possible that unmeasured predictors might explain a greater proportion of pain variability such as expectations of surgery. Some suggested that greater expectation of surgical outcome independently predicted greater pain relief but not for function [39]. Several studies also demonstrated that pain catastrophizing scale, the extent of a patient's negative or exaggerated orientation to pain, was a strong predictor of pain outcome after TKA 24, 40. It is also possible that the way information is measured on predictors is not detailed enough to capture the variability in their relation to pain. Previous studies suggested some patients might experience chronic pain after TKA despite the lack of noxious stimuli, which might be due to a dysfunction of pain modulation in the central nervous system, known as central sensitization [41]. The proportion of outcome variability explained by fitted models also decreased over time, which might be due to that some other unknown or unmeasured factors start to play an increasing role in the variability of outcomes.
Although our results showed statistically significant difference in attained postoperative OKS relating to preoperative patient and clinical characteristics, the size of effect for all identified variables is small. Moreover, regardless of their preoperative characteristics, on average, patients still achieved substantial improvement in pain and benefited from surgery over a long term. Improvement in function was less prominent, especially for patients with the highest quintile of preoperative function subscale scores. This might be explained by a ceiling effect or that TKA is less effective in restoring function compared to relieving pain.
What This Study Adds?
Within this study, we have identified a number of preoperative predictors of attained postoperative PROMs over a long term after TKA. Predictors were the same for both pain and functional outcomes, and for both short-to-medium-term and long-term results. Within the variables collected, functional outcome was more predictable than pain and shorter-term outcomes more predictable than longer-term outcomes. Changes in outcomes over time revealed that regardless of their preoperative characteristics, on average, patients benefited from TKA and improved substantially in pain over 10 years, although the improvement was less prominent in functional outcomes.
Strengths and Limitations
The strengths of this project include the following. (1) Relatively large cohort; a total of 1980 patients were included in the multivariable analysis over 10 years. (2) Long-term follow-up; repeated measurements of OKS were examined over 10 years after TKA. (3) The inclusion of a wide range of predictor variables; this made it possible to identify predictor variables more comprehensively and to minimize residual confounding. (4) Pain and functional outcomes analyzed separately; this is important to inform patients of their specific outcomes that can be expected.
Limitations include that other potential predictor variables suggested by previous studies, for example, patient expectations [39] and surgeon volume [22], were not measured in this project. The medical conditions of the involved knee joint were not examined either. Response bias is also possible as those included for analysis tended to be younger and healthier. Patients who were recruited in the KAT study might also have different characteristics from those declining to participate or not eligible and thus limit the generalizability of this study. However, the sample of patients included for analysis (mean age of 70 years with 56.4% females) is similar to all patients treated by the National Health Service (NHS) in 2005-2006 (mean age of 70 years with 57.7% females) [42], suggesting that our sample is fairly representative of the general population in the United Kingdom.
Conclusion
The same predictors were identified for pain and functional outcomes over both short-to-medium-term and long-term after primary TKA. Functional outcome and shorter-term outcomes were more predictable than pain and longer-term outcomes, respectively. Regardless of their preoperative characteristics, on average, patients still benefited from surgery and improved substantially in pain, although the improvement in function was less prominent.
Acknowledgment
We would like to acknowledge all the patients and professionals who participated in data collection within the KAT study.
Footnotes
One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to http://dx.doi.org/10.1016/j.arth.2016.06.009.
This manuscript received support from the Arthritis Research UK Centre for Sport, Exercise and Osteoarthritis. The Knee Arthroplasty Trial was funded by the National Institute for Health Research (NIHR) Health Technology Assessment Programme (project number 95/10/01), with additional funding for research support in clinical centers provided by Howmedica Osteonics; Zimmer; Johnson & Johnson DePuy; Corin Medical; Smith & Nephew Healthcare; Biomet Merck; and Wright Cremascoli. The authors conducted the research independently of all funding organizations. The funders had no role in the collection, analysis or interpretation of data, writing of the manuscript, or the decision to publish.
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.arth.2016.06.009.
Appendix A. Supplementary Data
Supplementary Table 1.
Descriptive Statistics and Comparison of Those Who Were Included, and Not, Into the Analysis.
| Variables | Missing | Overall (N = 2252) | Inclusion Into Analysis |
||
|---|---|---|---|---|---|
| Included (n = 1980) | Excluded (n = 272) | P Value | |||
| Preop overall OKS (mean, SD) | 121 (5.4%) | 18.0 (7.5) | 18.2 (7.5) | 15.2 (7.3) | <.001 |
| Postop overall OKS (median, IQR) | |||||
| 1 y | 544 (24.2%) | 36 (28, 42) | 36 (28, 42) | 34 (25, 42) | .35 |
| 2 y | 683 (30.3%) | 38 (28, 43) | 38 (28, 43) | 38 (28, 42) | .78 |
| 3 y | 603 (26.8%) | 37 (28, 43) | 37 (28, 43) | 38 (30, 44) | .48 |
| 4 y | 608 (27.0%) | 37 (27, 43) | 36 (27, 43) | 39 (29, 44) | .23 |
| 5 y | 690 (30.6%) | 37 (28, 43) | 37 (28, 43) | 39 (28, 44) | .30 |
| 6 y | 838 (37.2%) | 37 (28, 43) | 37 (28, 43) | 39 (31, 43) | .34 |
| 7 y | 912 (40.5%) | 37 (27, 43) | 37 (27, 43) | 37 (30, 42) | .77 |
| 8 y | 989 (43.9%) | 36 (27, 43) | 36 (27, 43) | 37 (28, 41) | .78 |
| 9 y | 1105 (49.1%) | 36 (27, 43) | 36 (27, 43) | 36 (29, 42) | .53 |
| 10 y | 1316 (58.4%) | 36 (26, 43) | 36 (26, 43) | 35 (27, 42) | .68 |
| Patient characteristics | |||||
| Sex, n (%) | 0 | ||||
| Female | 1271 (56.4%) | 1116 (56.4%) | 155 (57.0%) | .85 | |
| Male | 981 (43.6%) | 864 (43.6%) | 117 (43.0%) | ||
| Marital status, n (%) | 38 (1.7%) | ||||
| Married | 1458 (65.8%) | 1305 (66.3%) | 153 (62.5%) | .23 | |
| Alone | 756 (34.2%) | 664 (33.7%) | 92 (38.5%) | ||
| Age, y (mean, SD) | 0 | 71 (8) | 70 (8) | 72 (9) | .004 |
| BMI, kg/m2 | 106 (4.7%) | .98 | |||
| <25 | 366 (17.1%) | 327 (17.1%) | 39 (17.0%) | ||
| 25-30 | 878 (40.9%) | 781 (40.8%) | 97 (42.2%) | ||
| 30-35 | 597 (27.8%) | 534 (27.9%) | 63 (27.4%) | ||
| >35 | 305 (14.2%) | 274 (14.3%) | 31 (13.5%) | ||
| IMD 2004 quintiles | 819 (36.4%) | .53a | |||
| 1st (most deprived) | 210 (14.6%) | 179 (14.4%) | 31 (16.6%) | ||
| 2nd | 255 (17.8%) | 227 (18.2%) | 28 (15.0%) | ||
| 3rd | 343 (23.9%) | 304 (24.4%) | 39 (20.9%) | ||
| 4th | 349 (24.4%) | 299 (24.0%) | 50 (26.7%) | ||
| 5th (most affluent) | 276(19.3%) | 237 (19.0%) | 39 (20.9%) | ||
| Preoperative mental well-being | |||||
| Preop SF-12 MCS | 148 (6.6%) | .01 | |||
| 1024 (48.7%) | 916 (47.8%) | 108 (57.5%) | |||
| 1080 (51.3%) | 1000 (52.2%) | 80 (42.5%) | |||
| Preoperative clinical conditions | |||||
| Diagnosis, n (%) | 42 (1.9%) | ||||
| OA | 2102 (95.1%) | 1871 (95.2%) | 231 (94.7%) | .74 | |
| RA | 108 (4.9%) | 95 (4.8%) | 13 (5.3%) | ||
| Joint affected, n (%) | 42 (1.9%) | ||||
| One knee | 569 (25.8%) | 515 (26.2%) | 54 (22.1%) | .18 | |
| Both knees | 874 (39.5%) | 765 (38.9%) | 109 (44.7%) | ||
| General | 767 (34.7%) | 686 (34.9%) | 81 (33.2%) | ||
| ASA grade, n (%) | 111 (4.9%) | ||||
| Grade 1 | 366 (17.1%) | 332 (17.5%) | 34 (14.1%) | .002 | |
| Grade 2 | 1320 (61.7%) | 1185 (62.4%) | 135 (56.0%) | ||
| Grade 3-4 | 455 (21.3%) | 383 (20.2%) | 72 (39.9%) | ||
| Previous knee surgery, n (%) | 42 (1.9%) | ||||
| No | 1420 (64.3%) | 1246 (63.4%) | 174 (71.3%) | .02 | |
| Yes | 790 (36.7%) | 720 (36.6%) | 70 (28.7%) | ||
| Previous contralateral TKA, n (%) | 42 (1.9%) | ||||
| No | 1916 (86.7%) | 1705 (86.7%) | 211 (86.5%) | .91 | |
| Yes | 294 (13.3%) | 261 (13.3%) | 33 (13.5%) | ||
| Comorbidities, n (%) | 49 (1.9%) | ||||
| No | 1882 (85.4%) | 1688 (86.0%) | 194 (81.2%) | .05 | |
| Yes | 321 (14.6%) | 276 (14.0%) | 45 (18.8%) | ||
The t tests were used for continuous variables and χ2 tests for categorical variables.
OKS, Oxford knee score; SD, standard deviation; BMI, body mass index; Preop, preoperative; Postop, postoperative; SF-12 MCS, 12-item Short-Form Health Survey Mental Component Summary; IMD, Index of Multiple Deprivation; IQR, interquartile range; OA, osteoarthritis; RA, rheumatoid arthritis; ASA, American Society of Anesthesiologists; TKA, total knee arthroplasty.
t test based on log transformation of IMD 2004.
Appendix A. Supplementary Data
References
- 1.National Joint Registry for England and Wales . NJR Center; Hertfordshire, England: 2012. 9th Annual Report 2012. [Google Scholar]
- 2.Beswick A.D., Wylde V., Gooberman-Hill R. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open. 2012;2(1):e000435. doi: 10.1136/bmjopen-2011-000435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ghanem E., Pawasarat I., Lindsay A. Limitations of the Knee Society Score in evaluating outcomes following revision total knee arthroplasty. J Bone Jt Surg Am. 2010;92(14):2445. doi: 10.2106/JBJS.I.00252. [DOI] [PubMed] [Google Scholar]
- 4.Carr A.J., Robertsson O., Graves S. Knee replacement. Lancet. 2012;379(9823):1331. doi: 10.1016/S0140-6736(11)60752-6. [DOI] [PubMed] [Google Scholar]
- 5.Black N. Patient reported outcome measures could help transform healthcare. BMJ. 2013;346:f167. doi: 10.1136/bmj.f167. [DOI] [PubMed] [Google Scholar]
- 6.Baker P.N., Deehan D.J., Lees D. The effect of surgical factors on early patient-reported outcome measures (PROMS) following total knee replacement. J Bone Joint Surg Br. 2012;94(8):1058. doi: 10.1302/0301-620X.94B8.28786. [DOI] [PubMed] [Google Scholar]
- 7.Fortin P.R., Clarke A.E., Joseph L. Outcomes of total hip and knee replacement: preoperative functional status predicts outcomes at six months after surgery. Arthritis Rheum. 1999;42(8):1722. doi: 10.1002/1529-0131(199908)42:8<1722::AID-ANR22>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 8.Jones C.A., Voaklander D.C., Johnston D.W. The effect of age on pain, function, and quality of life after total hip and knee arthroplasty. Arch Intern Med. 2001;161(3):454. doi: 10.1001/archinte.161.3.454. [DOI] [PubMed] [Google Scholar]
- 9.Clement N.D., Jenkins P.J., MacDonald D. Socioeconomic status affects the Oxford knee score and short-form 12 score following total knee replacement. Bone Joint J. 2013;95-B(1):52. doi: 10.1302/0301-620X.95B1.29749. [DOI] [PubMed] [Google Scholar]
- 10.Clement N.D., MacDonald D., Simpson A.H. Total knee replacement in patients with concomitant back pain results in a worse functional outcome and a lower rate of satisfaction. Bone Joint J. 2013;95-B(12):1632. doi: 10.1302/0301-620X.95B12.31684. [DOI] [PubMed] [Google Scholar]
- 11.Judge A., Arden N.K., Cooper C. Predictors of outcomes of total knee replacement surgery. Rheumatology (Oxford) 2012;51(10):1804. doi: 10.1093/rheumatology/kes075. [DOI] [PubMed] [Google Scholar]
- 12.Escobar A., Quintana J.M., Bilbao A. Effect of patient characteristics on reported outcomes after total knee replacement. Rheumatology (Oxford) 2007;46(1):112. doi: 10.1093/rheumatology/kel184. [DOI] [PubMed] [Google Scholar]
- 13.Dowsey M.M., Nikpour M., Choong P.F. Outcomes following large joint arthroplasty: does socio-economic status matter? BMC Musculoskelet Disord. 2014;15:148. doi: 10.1186/1471-2474-15-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lingard E.A., Katz J.N., Wright E.A. Predicting the outcome of total knee arthroplasty. J Bone Jt Surg Am. 2004;86-A(10):2179. doi: 10.2106/00004623-200410000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Rajgopal V., Bourne R.B., Chesworth B.M. The impact of morbid obesity on patient outcomes after total knee arthroplasty. J Arthroplasty. 2008;23(6):795. doi: 10.1016/j.arth.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 16.Singh J.A., Gabriel S., Lewallen D. The impact of gender, age, and preoperative pain severity on pain after TKA. Clin Orthop Relat Res. 2008;466(11):2717. doi: 10.1007/s11999-008-0399-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCalden R.W., Robert C.E., Howard J.L. Comparison of outcomes and survivorship between patients of different age groups following TKA. J Arthroplasty. 2013;28(8 Suppl):83. doi: 10.1016/j.arth.2013.03.034. [DOI] [PubMed] [Google Scholar]
- 18.Franklin P.D., Li W., Ayers D.C. The Chitranjan Ranawat Award: functional outcome after total knee replacement varies with patient attributes. Clin Orthop Relat Res. 2008;466(11):2597. doi: 10.1007/s11999-008-0428-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lopez-Olivo M.A., Landon G.C., Siff S.J. Psychosocial determinants of outcomes in knee replacement. Ann Rheum Dis. 2011;70(10):1775. doi: 10.1136/ard.2010.146423. [DOI] [PubMed] [Google Scholar]
- 20.Gandhi R., Dhotar H., Razak F. Predicting the longer term outcomes of total knee arthroplasty. Knee. 2010;17(1):15. doi: 10.1016/j.knee.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 21.Ritter M.A., Wing J.T., Berend M.E. The clinical effect of gender on outcome of total knee arthroplasty. J Arthroplasty. 2008;23(3):331. doi: 10.1016/j.arth.2007.10.031. [DOI] [PubMed] [Google Scholar]
- 22.Katz J.N., Mahomed N.N., Baron J.A. Association of hospital and surgeon procedure volume with patient-centered outcomes of total knee replacement in a population-based cohort of patients age 65 years and older. Arthritis Rheum. 2007;56(2):568. doi: 10.1002/art.22333. [DOI] [PubMed] [Google Scholar]
- 23.Williams D.P., Blakey C.M., Hadfield S.G. Long-term trends in the Oxford knee score following total knee replacement. Bone Jt J. 2013;95-B(1):45. doi: 10.1302/0301-620X.95B1.28573. [DOI] [PubMed] [Google Scholar]
- 24.Riddle D.L., Wade J.B., Jiranek W.A. Preoperative pain catastrophizing predicts pain outcome after knee arthroplasty. Clin Orthop. 2010;468(3):798. doi: 10.1007/s11999-009-0963-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lingard E.A., Riddle D.L. Impact of psychological distress on pain and function following knee arthroplasty. J Bone Joint Surg Am. 2007;89(6):1161. doi: 10.2106/JBJS.F.00914. [DOI] [PubMed] [Google Scholar]
- 26.Group KATT. Johnston L., MacLennan G., McCormack K. The Knee Arthroplasty Trial (KAT) design features, baseline characteristics, and two-year functional outcomes after alternative approaches to knee replacement. J Bone Jt Surg Am. 2009;91(1):134. doi: 10.2106/JBJS.G.01074. [DOI] [PubMed] [Google Scholar]
- 27.Murray D.W., MacLennan G.S., Breeman S. A randomised controlled trial of the clinical effectiveness and cost-effectiveness of different knee prostheses: the Knee Arthroplasty Trial (KAT) Health Technol Assess. 2014;18(19):1. doi: 10.3310/hta18190. vii-viii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dawson J., Fitzpatrick R., Murray D. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br. 1998;80-B:63. doi: 10.1302/0301-620x.80b1.7859. [DOI] [PubMed] [Google Scholar]
- 29.Murray D.W., Fitzpatrick R., Rogers K. The use of the Oxford hip and knee scores. J Bone Joint Surg Br. 2007;89-B:1010. doi: 10.1302/0301-620X.89B8.19424. [DOI] [PubMed] [Google Scholar]
- 30.Harris K., Dawson J., Doll H. Can pain and function be distinguished in the Oxford Knee Score in a meaningful way? An exploratory and confirmatory factor analysis. Qual Life Res. 2013;22(9):2561. doi: 10.1007/s11136-013-0393-x. [DOI] [PubMed] [Google Scholar]
- 31.Noble M., Wright G., Dibben C. Neighbourhood Renewal Unit; London: 2004. The English Indices of Deprivation 2004 (revised) Report to the Office of the Deputy Prime Minister. [Google Scholar]
- 32.Ware J., Jr., Kosinski M., Keller S.D. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 33.Ayers D.C., Franklin P.D., Trief P.M. Psychological attributes of preoperative total joint replacement patients: implications for optimal physical outcome. J Arthroplasty. 2004;19(7 Suppl 2):125. doi: 10.1016/j.arth.2004.06.019. [DOI] [PubMed] [Google Scholar]
- 34.Daabiss M. American Society of Anaesthesiologists physical status classification. Indian J Anaesth. 2011;55(2):111. doi: 10.4103/0019-5049.79879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rubin D.B. Inference and missing data. Biometrika. 1976;63(3):581. [Google Scholar]
- 36.Sterne J.A., White I.R., Carlin J.B. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338:b2393. doi: 10.1136/bmj.b2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Royston P. Multiple imputation of missing values: update of ice. Stata J. 2005;5:527. [Google Scholar]
- 38.Kane R.L., Saleh K.J., Wilt T.J. The functional outcomes of total knee arthroplasty. J Bone Jt Surg Am. 2005;87(8):1719. doi: 10.2106/JBJS.D.02714. [DOI] [PubMed] [Google Scholar]
- 39.Gandhi R., Davey J.R., Mahomed N. Patient expectations predict greater pain relief with joint arthroplasty. J Arthroplasty. 2009;24(5):716. doi: 10.1016/j.arth.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 40.Forsythe M.E., Dunbar M.J., Hennigar A.W. Prospective relation between catastrophizing and residual pain following knee arthroplasty two-year follow-up. Pain Res Manag. 2008;13(4):335. doi: 10.1155/2008/730951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wylde V., Dieppe P., Hewlett S. Total knee replacement: is it really an effective procedure for all? Knee. 2007;14(6):417. doi: 10.1016/j.knee.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 42.Browne J., Jamieson L., Lewsey J. London School of Hygiene and Tropical Medicine; London: 2007. Patient reported outcome measures (PROMs) in elective surgery, Report to the Department of Health. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.