Abstract
Objective
The relationship between respiratory tuberculosis (RT) and incident fragility fracture and osteoporosis/fragility fracture in the general population is not well determined; therefore, we conducted a nationwide cohort study to investigate this relationship.
Methods
We used the National Health Insurance Research Database of Taiwan to identify 6612 newly diagnosed patients with RT (RT cohort) and 13220 patients without RT (non-RT cohort) from 1999 to 2005. The mean durations of follow-up were (6.73 ± 4.00 years, 8.11 ± 3.24 years) in the (RT cohort, non- RT cohort); respectively. The occurrence of incident fragility fracture and osteoporosis/fragility fracture were followed up until the end of 2011. The adjusted hazard ratios (aHRs) and 95% confidence intervals (CIs) and 98% CIs of incident fragility fracture and osteoporosis/fragility fracture were estimated using the multivariable Cox proportional hazard model after adjusting for age, sex, occupation, drug use, and comorbidities.
Results
A Cox proportional hazards regression analysis was performed and showed the aHRs of [incident fragility fracture; osteoporosis/fragility fracture] were [1.69 (95% CI = 1.26–2.28, 98% CI = 1.18–2.44); 1.42 (95% CI = 1.25–1.61, 98% CI = 1.21–1.65)] between the RT and non-RT cohorts. Regarding the sex, the aHRs of the [incident fragility fracture; osteoporosis / fragility fracture] were [1.57 (98% CI = 1.10–2.23, 98% CI = 1.02–2.41); 1.15 (95% CI = 0.97–1.36, 98% CI = 0.94–1.41)] in the men. The aHRs of the RT cohort without oral steroid use in the [incident fragility fracture; osteoporosis / fragility fracture] were [1.87 (95% CI = 1.20–2.90, 98% CI = 1.09–3.19); 1.41 (95% CI = 1.19–1.67, 98% CI = 1.14–1.74)].
Conclusion
The RT associated with the incident fragility fracture, either in men or absence of oral steroid use.
Introduction
Osteoporosis is the most common type of bone disease [1] and is a major public health problem [2]. Osteoporosis increases the risk of breaking a bone [3]. Approximately 50% of women older than 50 years were predicted to fracture their hip, wrist, or vertebra (bone of the spine) during their lifetime. Studies have reported that one out of 4 osteoporotic hip fractures resulted in long-term nursing home care, and half of these patients are unable to walk without assistance and have a 24% increased risk of death within one year [4,5].
Parathyroid hormone (PTH) stimulates osteoblasts, which increase the production of receptor activator of nuclear factor kappa-B ligand (RANKL) [6]. Hematopoietic cell precursors stimulated by macrophage colony-stimulating factor (M-CSF) facilitate osteoclast production that expresses RANK [6]. Osteoblasts also produce a decoy receptor called osteoprotegerin (OPG) that binds to RANKL and prevents RANKL and RANK interaction [7]. Estradiol increases the production of OPG to diminish bone resorption. Glucocorticoids stimulate RANKL expression and inhibit OPG synthesis by osteoblasts to enhance osteoclast proliferation and differentiation, leading to bone resorption [8].
Patient profiles at a bone health and osteoporosis prevention service center in Ireland revealed that only 13% of patients did not present with comorbidities [9]. Osteoporosis has been reported to be associated with hyperlipidemia, hypertension, diabetes, ischemic heart disease, end-stage renal disease [10], and liver cirrhosis [11]. Infections such as hepatitis C virus (HCV) infection are also risk factors of osteoporosis [11]. Osteoporotic changes [12] in tuberculosis arthritis were observed in previous report [13]. However, the respiratory tuberculosis (RT) intervention associated with bone fracture among patients with or without comorbidities is not found in literature.
Methods and Materials
Study population
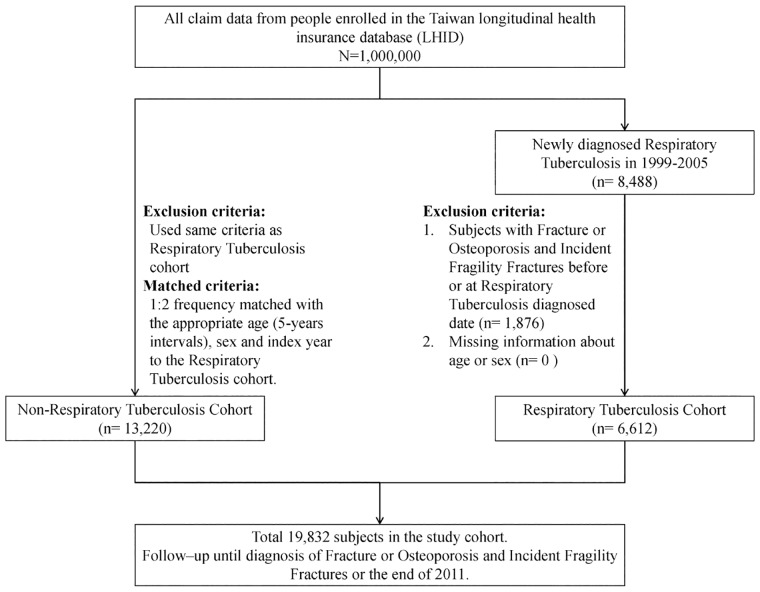
The patient selection process used in our study is illustrated in Fig 1. We conducted a retrospective population-based cohort study to investigate the association between RT and risk of incident bone fracture and osteoporosis / fragility fracture. The diagnosis and treatment of the RT is under the strict control of the Centers for Disease Control in Taiwan for avoiding pulmonary tuberculosis (PTB) transmission [14]. The coding of the RT is after the consensus of the chest physician, infection specialist and the well-trained coder. The RT cohort follow up by the public nurse and chest physician or infection specialist. During the study period (1999–2005), we identified newly diagnosed patients with RT (ICD-9-CM 011–012) as the RT cohort, and the initial date of RT diagnosis served as their index date. We randomly selected comparison participants (individuals without RT) from the LHID as the non-RT cohort and frequency-matched the participants by age and sex at a ratio of 1:2. The index date of the non-RT cohort was randomly assigned a month and day with the same year as the matched cases. We excluded individuals with missing data such as date of birth, sex, and known history of osteoporosis / fragility fracture before the baseline from the study.
Fig 1. Flow chart of the selection of study participants.
Outcome and comorbidities measurement
The primary endpoint of our study was the occurrence of fragility fracture (ICD-9-CM 733.1). The secondary endpoint was osteoporosis /fragility fracture (pathology fractures; ICD-9-CM 733.0, 733.1) [15–17]. All participants were followed up from the index date to the date when the participants stopped claiming insurance and showing signs of incident fragility fracture, osteoporosis / fragility fracture or until December 31, 2011.
Comorbidities were defined as the patient having used medical services for hyperlipidemia (ICD-9-CM 272), hypertension (ICD-9-CM 401–405), diabetes (ICD-9-CM 250), pneumonia (ICD-9-CM 480–488), liver cirrhosis (ICD-9-CM 571), ischemia heart disease (IHD, ICD-9-CM 410–414), end-stage renal disease (ESRD, ICD-9-CM 585), hyperparathyroidism (ICD-9-CM 252.0), celiac disease (ICD-9-CM 579.0), Crohn’s disease (ICD-9-CM 555.0, 555.1, 555.2, and 555.9), alcohol-related illness (ICD-9-CM 291, 303, 305, 571.0, 571.1, 571.2, 571.3, and 790.3), stroke (ICD-9-CM 430–438), chronic obstructive pulmonary disease (COPD; ICD-9-CM 490–496), and lower body weight (ICD-9-CM 783.2) before the end date [18]. We also investigated drug effects and collected the history of oral steroid, bisphosphonates, hormone replacement therapy (HRT), vitamin D supplements, and aromatase inhibitors prescription before the end date. The oral steroid users was defined subjects had ever used the oral steroid at least one month [19]. Besides, the bisphosphonates, HRT, vitamin D supplements, and aromatase inhibitors were considered for adjustment, when subjects ever used for one dose before the study end date.
Ethics statement
The NHIRD encrypts patient personal information to protect privacy and provides researchers with anonymous identification numbers associated with relevant claims information, including sex, date of birth, medical services received, and prescriptions. Therefore, patient consent is not required to access the NHIRD. This study was approved to fulfill the condition for exemption by the Institutional Review Board (IRB) of China Medical University (CMUH104-REC2-115). The IRB also specifically waived the consent requirement.
Statistical analysis
We presented the mean and standard deviation (SD) for age and percentages for sex, age groups, occupation, comorbidities, and each type of drug used. We used the chi-squared test and Student’s t-test to assess the differences in the distribution between the RT and non-RT cohorts. The incidence–density of fragility fracture, osteoporosis / incident fragility fracture were calculated as the number of patients with incident fragility fracture, osteoporosis / fragility fracture divided by the sum of person–years (per 1000 person–years). We also measured the cumulative incidence curves of incident fragility fracture, osteoporosis / fragility fracture for both cohorts by using the Kaplan–Meier method. We used the log-rank test to assess the different incidence curves. We demonstrated the incidence–density between the RT and non-RT cohorts after stratifying the data on the basis of sex, age, occupation, comorbidities, oral steroid used, follow-up period (<2 and ≥2 years), and oral steroid use. The incidence rate ratio (IRR) of incident fragility fracture, osteoporosis / fragility fractures for these variables between the two cohorts was assessed using the Poisson regression model. The multivariable Cox proportional hazards model was used to estimate hazard ratios (HRs) and 95% and 98% confidence intervals (CIs) for the risk of incident fragility fracture, osteoporosis /fragility fracture between the two cohorts. The Bonferroni adjustment was used in multiple comparisons.
All the statistical analyses were performed using the SAS 9.4 statistical package (SAS Institute Inc., NC, USA). We used the R software (R Foundation for Statistical Computing, Vienna, Austria) to plot the cumulative incidence of both cohorts. A p-value < 0.05 and (p-value < 0.02) was considered significant in the 2-tailed tests performed this study.
Results
This study included 6612 patients with RT and 13220 normal controls from 1999 to 2005 (Table 1). The frequency-matched cohorts demonstrated a similar age and sex distribution (p-value > 0.05), in which 69.7% were men and 43.5% were ≧65 years old. Except for hypertension, celiac disease and Chron’s disease, the percentage of comorbidities in the RT cohort was greater than that in the non-RT cohort. RT cohort used the oral steroid (51.5%) or bisphosphonates (1.53%) was more common than comparison cohort.
Table 1. Comparison of demographics and comorbidity between with and without respiratory tuberculosis cohorts.
| Respiratory tuberculosis | |||||
|---|---|---|---|---|---|
| No (N = 13220) | Yes (N = 6612) | ||||
| n | % | n | % | p-value | |
| Sex | 0.99 | ||||
| Women | 4008 | 30.3 | 2004 | 30.3 | |
| Men | 9212 | 69.7 | 4608 | 69.7 | |
| Age, year | 0.99 | ||||
| <35 | 2274 | 17.2 | 1137 | 17.2 | |
| 35–65 | 5196 | 39.3 | 2598 | 39.3 | |
| ≥65 | 5750 | 43.5 | 2877 | 43.5 | |
| Mean (SD)# | 56.7 | 20.2 | 56.9 | 20.3 | 0.64 |
| Occupation | <0.001 | ||||
| White collar | 5685 | 43.0 | 2468 | 37.3 | |
| Blue collar | 4839 | 36.6 | 2641 | 39.9 | |
| Others | 2696 | 20.4 | 1503 | 22.7 | |
| Comorbidity | |||||
| Hyperlipidemia | 3439 | 26.0 | 1576 | 23.8 | <0.001 |
| Hypertension | 6446 | 48.8 | 3283 | 49.7 | 0.24 |
| Diabetes | 2909 | 22.0 | 1793 | 27.1 | <0.001 |
| Pneumonia | 4712 | 35.6 | 4019 | 60.8 | <0.001 |
| Live cirrhosis | 3565 | 27.0 | 2376 | 35.9 | <0.001 |
| IHD | 3597 | 27.2 | 2038 | 30.8 | <0.001 |
| Stroke | 3319 | 25.1 | 1806 | 27.3 | <0.001 |
| COPD | 5793 | 43.8 | 4982 | 75.4 | <0.001 |
| ESRD | 183 | 1.38 | 170 | 2.57 | <0.001 |
| Alcohol-related illness | 374 | 2.83 | 447 | 6.76 | <0.001 |
| Hyperparathyroidism | 12 | 0.09 | 18 | 0.27 | 0.002 |
| Celiac disease | 0 | 0.00 | 1 | 0.02 | - |
| Chron’s disease | 236 | 1.79 | 133 | 2.01 | 0.27 |
| Lower body weight | 323 | 2.44 | 286 | 4.33 | <0.001 |
| Treatment | |||||
| Oral steroid | 4340 | 32.8 | 3402 | 51.5 | <0.001 |
| Bisphosphonates | 76 | 0.57 | 101 | 1.53 | <0.001 |
| HRT | 1218 | 9.21 | 651 | 9.85 | 0.15 |
| Vitamin D supplements | 21 | 0.16 | 12 | 0.18 | 0.71 |
| Aromatase inhibitors | 13 | 0.10 | 10 | 0.15 | 0.30 |
Chi-square test; # Student’s t-test; White collar: civil services, institution workers, enterprise, business and industrial administration personnel; Blue collar: farmers, fishermen, vendors, and industrial laborers; Others: retired, unemployed, and low-income populations; HRT, Hormone Replacement Therapy; IHD, ischemia heart disease; COPD, chronic obstructive pulmonary disease; ESRD, end-stage renal disease
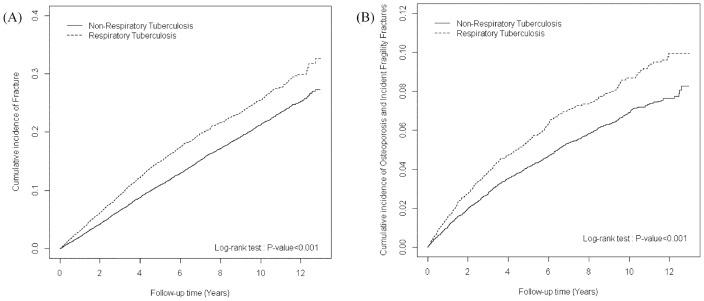
The cumulative incidence of incident fragility fracture (Fig 2A, log-rank P < 0.001) were significantly higher for patients in the RT cohort than for participants without RT. During the 44517 and 107232 person-years follow-up, the overall incidence density of fragility fractures was 1.69-fold significantly higher in RT patients than in the non-RT cohort (2.02 vs 1.11 per 1000 person-y), with an adjusted HR = 1.69 (95% CI = 1.26–2.28; 98% CI = 1.18–2.44) (Table 2). Stratified by sex, men with RT had a 57% increased fragility fracture risk compared to the non-RT cohort. The RT cohort was significantly associated with a higher risk of fragility fracture compared with the non-RT cohort for aged of 65–75 years (adjusted HR = 1.76, 95% CI = 1.12–2.75; 98% CI = 1.02–3.03) and ≧75 years (adjusted HR = 1.94, 95% CI = 1.18–3.19; 98% CI = 1.06–3.56). The adjusted HR of fragility fracture was higher in RT cohort regardless of white collar (adjusted HR = 2.19, 95% CI = 1.21–3.97; 98% CI = 1.06–4.52). The risk of fragility fracture was observed in patients with comorbidities (adjusted HR = 1.90, 95% CI = 1.43–2.52; 98% CI = 1.34–2.68) in the RT cohort than in the non-RT cohort. Stratified by oral steroid, RT patients with oral steroid or without oral steroid had an increased fragility fracture risk compared to the non-RT cohort. The adjusted HR of fragility fracture was significantly higher in the more than two follow-up year (adjusted HR = 1.67, 95% CI = 1.16–2.40; 98% CI = 1.07–2.59).
Fig 2. The cumulative incidence of incident bone fracture (A) and osteoporosis / fragility fracture (B) between non-respiratory tuberculosis cohort (solid line) and respiratory tuberculosis cohort (dashed line).
Table 2. Incidence and adjusted hazard ratio of Incident fragility fractures stratified by sex, age, comorbidity, oral steroid used and follow-up time between with and without respiratory tuberculosis cohorts.
| Respiratory tuberculosis | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| No | Yes | Compared to non-respiratory tuberculosis | |||||||
| Variables | Event | PY | Rate | Event | PY | Rate | IRR (95% CI) | Adjusted HR† (95% CI) | Adjusted HR† (98% CI) |
| Overall | 119 | 107232 | 1.11 | 90 | 44517 | 2.02 | 1.82(1.66, 2.00)*** | 1.69(1.26, 2.28)*** | 1.69(1.18, 2.44)** |
| Sex | |||||||||
| Women | 46 | 33713 | 1.36 | 25 | 15002 | 1.67 | 1.22(1.02, 1.46)*** | 0.98(0.58, 1.65) | 0.98(0.52, 1.85) |
| Men | 73 | 73519 | 0.99 | 65 | 29515 | 2.20 | 2.22(1.98, 2.48)*** | 1.57(1.10, 2.23)** | 1.57(1.02, 2.41)** |
| P for interaction | 0.06 | ||||||||
| Age, year | |||||||||
| <65 | 21 | 67869 | 0.31 | 17 | 30751 | 0.55 | 1.79(1.56, 2.05)*** | 0.98(0.49, 1.98) | 0.98(0.42, 2.30) |
| 65–75 | 51 | 23387 | 2.18 | 42 | 8699 | 4.83 | 2.21(1.84, 2.66)*** | 1.76(1.12, 2.75)** | 1.76(1.02, 3.03)** |
| ≥75 | 47 | 15976 | 2.94 | 31 | 5066 | 6.12 | 2.08(1.72, 2.52)*** | 1.94(1.18, 3.19)** | 1.94(1.06, 3.56)** |
| P for interaction | 0.92 | ||||||||
| Occupation | |||||||||
| White collar | 29 | 48453 | 0.60 | 24 | 18665 | 1.29 | 2.15(1.84, 2.50)*** | 2.19(1.21, 3.97)** | 2.19(1.06, 4.52)** |
| Blue collar | 59 | 38758 | 1.52 | 37 | 16878 | 2.19 | 1.44(1.23, 1.68)*** | 1.37(0.88, 2.13) | 1.37(0.80, 2.35) |
| Others | 31 | 20021 | 1.55 | 29 | 8974 | 3.23 | 2.09(1.72, 2.54)*** | 1.76(1.01, 3.06)* | 1.76(0.90, 3.45) |
| P for interaction | 0.99 | ||||||||
| Comorbidity | |||||||||
| No | 4 | 24565 | 0.16 | 1 | 3705 | 0.27 | 1.66(1.19, 2.30)*** | 2.97(0.31, 28.4) | 2.97(0.19, 46.4) |
| Yes | 115 | 82667 | 1.39 | 89 | 40812 | 2.18 | 1.57(1.42, 1.74)*** | 1.90(1.43, 2.52)*** | 1.90(1.34, 2.68)** |
| P for interaction | 0.60 | ||||||||
| Oral steroid | |||||||||
| No | 64 | 73083 | 0.88 | 34 | 23253 | 1.46 | 1.22(1.09, 1.37)*** | 1.82(1.16, 2.87)** | 1.82(1.05, 3.17)** |
| Yes | 55 | 34149 | 1.61 | 56 | 21264 | 2.63 | 1.38(1.22, 1.55)*** | 1.63(1.10, 2.42)** | 1.63(1.01, 2.64)** |
| P for interaction | 0.52 | ||||||||
| Follow-up, year | |||||||||
| <2 | 35 | 25420 | 1.38 | 31 | 11455 | 2.71 | 1.97(1.77, 2.18)*** | 1.78(1.05, 2.99)* | 1.78(0.94, 3.36) |
| ≥2 | 84 | 81813 | 1.03 | 59 | 33062 | 1.78 | 1.74(1.57, 1.92)*** | 1.67(1.16, 2.40)** | 1.67(1.07, 2.59)** |
PY: person-year; Rate: incidence rate (per 1,000 person-years); IRR: incidence rate ratio; Adjusted HR†: multiple analysis including age, sex, occupation, drug of oral steroid, bisphosphonates, hormone replacement therapy (HRT), vitamin D supplements, and aromatase inhibitors and each comorbidity [including hyperlipidemia, hypertension, diabetes, pneumonia, live cirrhosis, ischemia heart disease (IHD), stroke, chronic obstructive pulmonary disease (COPD), end-stage renal disease (ESRD), alcohol-related illness, hyperparathyroidism, celiac disease, Chron’s disease, and lower body weight];
*p<0.05,
**p<0.02,
***p<0.001
The overall incidence of osteoporosis / fragility fracture was 9.61 per 1000 person–years and 7.29 per 1000 person–years in the RT and non-RT cohorts, respectively (Table 3). Fig 2B shows that the cumulative incidence of osteoporosis / fragility fracture was higher in the RT cohort than in the non-RT cohort (log-rank test < 0.001) at the end of the follow-up period. After adjustment for age, sex, drug use and comorbidities, the RT cohort was observed to be at a significantly higher risk of osteoporosis / fragility fracture compared with the non-RT cohort (adjusted HR = 1.42, 95% CI = 1.25–1.61; 98% CI = 1.21–1.65). The risk of osteoporosis was presented 1.36-fold (95% CI = 1.18–1.56; 98% CI = 1.14–1.61) in RT cohort. The RT cohort (except patients aged <65 years) was significantly associated with a higher risk of osteoporosis / fragility fracture compared with the non-RT cohort, particularly at the age of 65–75 years and ≧75 years. The adjusted HR of osteoporosis / fragility fracture was higher in RT cohort regardless of white collar (adjusted HR = 1.57, 95% CI = 1.24–1.99; 98% CI = 1.18–2.10), and others (adjusted HR = 1.72, 95% CI = 1.34–2.22; 98% CI = 1.27–2.34).
Table 3. Incidence and adjusted hazard ratio of osteoporosis / fragility fracture stratified by sex, age, comorbidity, oral steroid used and follow-up time between with and without respiratory tuberculosis cohorts.
| Respiratory tuberculosis | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| No | Yes | Compared to non-respiratory tuberculosis | |||||||
| Variables | Event | PY | Rate | Event | PY | Rate | IRR (95% CI) | Adjusted HR† (95% CI) | Adjusted HR† (98% CI) |
| Overall | 782 | 107232 | 7.29 | 428 | 44517 | 9.61 | 1.32(1.21, 1.43)*** | 1.42(1.25, 1.61)*** | 1.42(1.21, 1.65)** |
| Osteoporosis (ICD-9-CM: 7330) | 663 | 6.18 | 338 | 7.59 | 1.23(1.12, 1.34)*** | 1.36(1.18, 1.56)*** | 1.36(1.14, 1.61)** | ||
| Sex | |||||||||
| Women | 354 | 33713 | 10.5 | 189 | 15002 | 12.6 | 1.20(1.04, 1.39)* | 1.11(0.92, 1.34) | 1.11(0.89, 1.40) |
| Men | 428 | 73519 | 5.82 | 239 | 29515 | 8.10 | 1.39(1.26, 1.54)*** | 1.15(0.97, 1.36) | 1.15(0.94, 1.41) |
| P for interaction | 0.34 | ||||||||
| Age, year | |||||||||
| <65 | 210 | 67869 | 3.09 | 129 | 30751 | 4.19 | 1.36(1.21, 1.52)*** | 1.03(0.81, 1.30) | 1.03(0.77, 1.37) |
| 65–75 | 284 | 23387 | 12.1 | 169 | 8699 | 19.4 | 1.60(1.37, 1.87)*** | 1.50(1.22, 1.85)*** | 1.50(1.17, 1.93)** |
| ≥75 | 288 | 15976 | 18.0 | 130 | 5066 | 25.7 | 1.42(1.21, 1.68)*** | 1.49(1.19, 1.86)*** | 1.49(1.14, 1.96)** |
| P for interaction | 0.74 | ||||||||
| Occupation | |||||||||
| White collar | 236 | 48453 | 4.87 | 121 | 18665 | 6.48 | 1.33(1.16, 1.52)*** | 1.57(1.24, 1.99)*** | 1.57(1.18, 2.10)** |
| Blue collar | 359 | 38758 | 9.26 | 184 | 16878 | 10.9 | 1.18(1.03, 1.34)* | 1.16(0.95, 1.40) | 1.16(0.92, 1.46) |
| Others | 187 | 20021 | 9.34 | 123 | 8974 | 13.7 | 1.47(1.24, 1.74)*** | 1.72(1.34, 2.22)*** | 1.72(1.27, 2.34)** |
| P for interaction | 0.48 | ||||||||
| Comorbidity | |||||||||
| No | 62 | 24565 | 2.52 | 5 | 3705 | 1.35 | 0.53(0.35, 0.82)** | 1.11(0.44, 2.81) | 1.11(0.36, 3.43) |
| Yes | 720 | 82667 | 8.71 | 423 | 40812 | 10.4 | 1.19(1.09, 1.30)*** | 1.48(1.31, 1.68)*** | 1.48(1.28, 1.72)** |
| P for interaction | 0.38 | ||||||||
| Oral steroid | |||||||||
| No | 516 | 73083 | 7.06 | 200 | 23253 | 8.60 | 1.22(1.09, 1.37)*** | 1.40(1.17, 1.67)*** | 1.40(1.13, 1.73)** |
| Yes | 266 | 34149 | 7.79 | 228 | 21264 | 10.7 | 1.38(1.22, 1.55)*** | 1.46(1.21, 1.76)*** | 1.46(1.16, 1.83)** |
| P for interaction | 0.73 | ||||||||
| Follow-up, year | |||||||||
| <2 | 257 | 25419 | 10.1 | 162 | 11455 | 14.1 | 1.40(1.28, 1.53)*** | 1.59(1.28, 1.97)*** | 1.28(1.08, 1.52)** |
| ≥2 | 525 | 81813 | 6.42 | 266 | 33062 | 8.05 | 1.25(1.15, 1.37)*** | 1.33(1.14, 1.57)*** | 1.67(1.07, 2.59)** |
PY: person-year; Rate: incidence rate (per 1,000 person-years); IRR: incidence rate ratio; Adjusted HR†: multiple analysis including age, sex, occupation, drug of oral steroid, bisphosphonates, hormone replacement therapy (HRT), vitamin D supplements, and aromatase inhibitors and each comorbidity [including hyperlipidemia, hypertension, diabetes, pneumonia, live cirrhosis, ischemia heart disease (IHD), stroke, chronic obstructive pulmonary disease (COPD), end-stage renal disease (ESRD), alcohol-related illness, hyperparathyroidism, celiac disease, Chron’s disease, and lower body weight];
*p<0.05,
**p<0.02,
***p<0.001
The statistically significant increased risk of osteoporosis / fragility fracture was observed in patients with comorbidities (adjusted HR = 1.48, 95% CI = 1.31–1.68; 98% CI = 1.28–1.72) in the RT cohort. The RT cohort without oral steroid use was at a 1.40-fold increased risk of osteoporosis / fragility fracture compared with the non-RT cohort without oral steroid use (adjusted HR = 1.40, 95% CI = 1.17–1.67; 98% CI = 1.13–1.73), and the RT cohort was at a 1.46-fold increased osteoporosis / fragility fracture risk compared with the non-RT cohort with oral steroid use (adjusted HR = 1.46, 95% CI = 1.21–1.76; 98% CI = 1.16–1.83). The adjusted HR of osteoporosis / fragility fracture was significantly higher in the first two follow-up year (adjusted HR = 1.59, 95% CI = 1.28–1.97; 98% CI = 1.08–1.52) and in later on (adjusted HR = 1.33, 95% CI = 1.14–1.57; 98% CI = 1.07–2.59).
The incidence rate of fragility fracture was higher for those with comorbidities of hypertension, diabetes, pneumonia, live cirrhosis, and IHD in both cohorts (Table 4). The risk of fragility fracture was higher among patients without hypertension (adjusted HR = 2.81, 95% CI = 1.44–5.51) than patients with hypertension (adjusted HR = 1.52, 95% CI = 0.97–2.36) (P for interaction = 0.02).
Table 4. Incidence and adjusted hazard ratio of fragility fracture stratified by different comorbidity in respiratory tuberculosis and non-respiratory tuberculosis groups.
| Respiratory tuberculosis | Compared to without respiratory tuberculosis | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| No | Yes | ||||||||
| Variables | Event | PY | Rate | Event | PY | Rate | IRR (95% CI) | Adjusted HR† (95% CI) | Adjusted HR† (98% CI) |
| Hyperlipidemia | |||||||||
| No | 90 | 78246 | 1.15 | 66 | 32997 | 2.00 | 1.77(1.59, 1.96)*** | 1.73(1.22, 2.46)** | 1.73(1.13, 2.66)** |
| Yes | 29 | 28986 | 1.00 | 24 | 11520 | 2.08 | 2.11(1.77, 2.52)*** | 2.17(1.22, 3.86)** | 2.17(1.08, 4.37)** |
| P for interaction | 0.52 | ||||||||
| Hypertension | |||||||||
| No | 31 | 57441 | 0.54 | 37 | 24315 | 1.52 | 2.86(2.50, 3.27)*** | 2.81(1.62, 4.89)*** | 2.81(1.44, 5.51)** |
| Yes | 88 | 49792 | 1.77 | 53 | 20202 | 2.62 | 1.51(1.33, 1.71)*** | 1.52(1.05, 2.18)* | 1.52(0.97, 2.36) |
| P for interaction | 0.02 | ||||||||
| Diabetes | |||||||||
| No | 85 | 84771 | 1.00 | 66 | 33583 | 1.97 | 1.99(1.79, 2.20)*** | 1.86(1.30, 2.66)*** | 1.86(1.21, 2.87)** |
| Yes | 34 | 22462 | 1.51 | 24 | 10934 | 2.19 | 1.49(1.25, 1.78)*** | 1.69(0.97, 2.95) | 1.69(0.85, 3.33) |
| P for interaction | 0.31 | ||||||||
| Pneumonia | |||||||||
| No | 52 | 70796 | 0.73 | 26 | 19286 | 1.35 | 1.87(1.64, 2.14)*** | 2.25(1.36, 3.72)** | 2.25(1.22, 4.15)** |
| Yes | 67 | 36436 | 1.84 | 64 | 25231 | 2.54 | 1.40(1.23, 1.59)*** | 1.62(1.13, 2.34)** | 1.62(1.04, 2.53)** |
| P for interaction | 0.22 | ||||||||
| Live cirrhosis | |||||||||
| No | 81 | 78405 | 1.03 | 59 | 27834 | 2.12 | 2.08(1.86, 2.32)*** | 1.89(1.31, 2.74)*** | 1.89(1.21, 2.96)** |
| Yes | 38 | 28828 | 1.32 | 31 | 16683 | 1.86 | 1.44(1.23, 1.70)*** | 1.66(0.99, 2.78) | 1.66(0.88, 3.11) |
| P for interaction | 0.38 | ||||||||
| IHD | |||||||||
| No | 70 | 80293 | 0.87 | 51 | 32385 | 1.57 | 1.84(1.65, 2.05)*** | 1.98(1.32, 2.96)** | 1.98(1.21, 3.24)** |
| Yes | 49 | 26939 | 1.82 | 39 | 12132 | 3.21 | 1.79(1.53, 2.11)*** | 1.66(1.06, 2.59)* | 1.66(0.96, 2.86) |
| P for interaction | 0.71 | ||||||||
| ESRD | |||||||||
| No | 119 | 105958 | 1.12 | 89 | 43658 | 2.04 | 1.85(1.69, 2.02)*** | 1.80(1.33, 2.43)*** | 1.80(1.25, 2.59)** |
| Yes | 0 | 1274 | 0 | 1 | 859 | 1.16 | - | - | - |
| P for interaction | 0.97 | ||||||||
| Alcohol-related illness | |||||||||
| No | 118 | 104094 | 1.13 | 83 | 41430 | 2 | 1.79(1.63, 1.96)*** | 1.72(1.27, 2.34)*** | 1.72(1.19, 2.50)** |
| Yes | 1 | 3138 | 0.32 | 7 | 3086 | 2.27 | 7.67(4.11, 14.3)*** | 8.67(0.84, 80.1) | 8.67(0.50, 149.9) |
| P for interaction | 0.11 | ||||||||
| Hyperparathyroidism | |||||||||
| No | 118 | 107120 | 1.1 | 90 | 44375 | 2.03 | 1.87(1.71, 2.05)*** | 1.83(1.36, 2.47)*** | 1.83(1.27, 2.64)** |
| Yes | 1 | 112 | 8.95 | 0 | 142 | 0 | - | - | - |
| P for interaction | 0.96 | ||||||||
| Celiac disease | |||||||||
| No | 119 | 107232 | 1.11 | 90 | 44505 | 2.02 | 1.85(1.69, 2.03)*** | 1.81(1.35, 2.45)*** | 1.81(1.26, 2.61)** |
| Yes | 0 | 0 | - | 0 | 12 | 0 | - | - | - |
| P for interaction | - | ||||||||
| Chron’s disease | |||||||||
| No | 115 | 105230 | 1.09 | 88 | 43519 | 2.02 | 1.88(1.72, 2.06)*** | 1.88(1.39, 2.54)*** | 1.88(1.30, 2.71)** |
| Yes | 4 | 2002 | 2.00 | 2 | 997 | 2.01 | 1.00(0.53, 1.87) | 0.12(0.01, 3.18) | 0.12(0.002, 6.50) |
| P for interaction | 0.38 | ||||||||
| Lower body weight | |||||||||
| No | 115 | 104556 | 1.10 | 85 | 42491 | 2.00 | 1.85(1.69, 2.03)*** | 1.83(1.35, 2.48)*** | 1.83(1.26, 2.65)** |
| Yes | 4 | 2676 | 1.49 | 5 | 2026 | 2.47 | 1.62(0.99, 2.66) | 1.70(0.33, 8.70) | 1.70(0.23, 12.4) |
| P for interaction | 0.97 | ||||||||
PY: person-year; Rate: incidence rate (per 1,000 person-years); IRR: incidence rate ratio; Adjusted HR†: multiple analysis including age, sex, occupation, drug of oral steroid, bisphosphonates, hormone replacement therapy (HRT), vitamin D supplements, and aromatase inhibitors and each comorbidity [including hyperlipidemia, hypertension, diabetes, pneumonia, live cirrhosis, ischemia heart disease (IHD), stroke, chronic obstructive pulmonary disease (COPD), end-stage renal disease (ESRD), alcohol-related illness, hyperparathyroidism, celiac disease, Chron’s disease, and lower body weight];
**p<0.02,
***p<0.001
Table 5 shows the osteoporosis / fragility fracture risk between the RT and non-RT cohorts stratified by different comorbidities. Our results consistently showed that the RT cohort was significantly associated with an increased risk of osteoporosis / fragility fracture compared with the non-RT cohort in the presence of different comorbidities, such as hyperlipidemia, hypertension, diabetes, pneumonia, live cirrhosis, and IHD. The RT cohort without lower body weight have the higher risk of osteoporosis / fragility fracture (adjusted HR = 1.41, 95% CI = 1.24–1.60; 98% CI = 1.20–1.65), compared with the non-RT cohort also.
Table 5. Incidence and adjusted hazard ratio of osteoporosis / fragility fracture stratified by different comorbidity in respiratory tuberculosis and non-respiratory tuberculosis groups.
| Respiratory tuberculosis | Compared to without respiratory tuberculosis | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| No | Yes | ||||||||
| Variables | Event | PY | Rate | Event | PY | Rate | IRR (95% CI) | Adjusted HR† (95% CI) | Adjusted HR† (98% CI) |
| Hyperlipidemia | |||||||||
| No | 533 | 78246 | 6.81 | 295 | 32997 | 8.94 | 1.31(1.19, 1.45)*** | 1.42(1.21, 1.66)*** | 1.42(1.17, 1.72)** |
| Yes | 249 | 28986 | 8.59 | 133 | 11520 | 11.5 | 1.34(1.15, 1.57)*** | 1.43(1.14, 1.79)** | 1.43(1.09, 1.88)** |
| P for interaction | 0.72 | ||||||||
| Hypertension | |||||||||
| No | 259 | 57441 | 4.51 | 168 | 24315 | 6.91 | 1.53(1.36, 1.73) | 1.50(1.21, 1.87)*** | 1.50(1.15, 1.96)**** |
| Yes | 523 | 49792 | 10.5 | 260 | 20202 | 12.9 | 1.23(1.10, 1.37)*** | 1.34(1.15, 1.58)*** | 1.34(1.11, 1.63)** |
| P for interaction | 0.048 | ||||||||
| Diabetes | |||||||||
| No | 584 | 84771 | 6.89 | 297 | 33583 | 8.84 | 1.28(1.17, 1.41)*** | 1.39(1.20, 1.63)*** | 1.39(1.16, 1.68)** |
| Yes | 198 | 22462 | 8.82 | 131 | 10934 | 12 | 1.36(1.16, 1.59)*** | 1.42(1.12, 1.80)** | 1.42(1.07, 1.89)** |
| P for interaction | 0.71 | ||||||||
| Pneumonia | |||||||||
| No | 452 | 70796 | 6.38 | 159 | 19286 | 8.24 | 1.29(1.14, 1.46)*** | 1.52(1.26, 1.84)*** | 1.52(1.20, 1.92)** |
| Yes | 330 | 36436 | 9.06 | 269 | 25231 | 10.7 | 1.18(1.05, 1.32)** | 1.33(1.12, 1.58)** | 1.33(1.08, 1.64)** |
| P for interaction | 0.19 | ||||||||
| Live cirrhosis | |||||||||
| No | 541 | 78405 | 6.9 | 261 | 27834 | 9.38 | 1.36(1.23, 1.50)*** | 1.43(1.22, 1.68)*** | 1.43(1.18, 1.74)** |
| Yes | 241 | 28828 | 8.36 | 167 | 16683 | 10 | 1.20(1.04, 1.38)* | 1.37(1.11, 1.69)** | 1.37(1.06, 1.77)** |
| P for interaction | 0.87 | ||||||||
| IHD | |||||||||
| No | 465 | 80293 | 5.79 | 251 | 32385 | 7.75 | 1.34(1.21, 1.48)*** | 1.51(1.27, 1.79)*** | 1.51(1.23, 1.86)** |
| Yes | 317 | 26939 | 11.8 | 177 | 12132 | 14.6 | 1.24(1.08, 1.43)** | 1.30(1.07, 1.58)** | 1.30(1.02, 1.64)** |
| P for interaction | 0.26 | ||||||||
| ESRD | |||||||||
| No | 777 | 105958 | 7.33 | 419 | 43658 | 9.6 | 1.31(1.20, 1.42)*** | 1.40(1.23, 1.60)*** | 1.40(1.20, 1.64)** |
| Yes | 5 | 1274 | 3.92 | 9 | 859 | 10.5 | 2.67(1.46, 4.88)** | 2.24(0.56, 8.98) | 2.24(0.41, 12.2) |
| P for interaction | 0.13 | ||||||||
| Alcohol-related illness | |||||||||
| No | 769 | 104094 | 7.39 | 410 | 41430 | 9.9 | 1.34(1.23, 1.46)*** | 1.40(1.23, 1.59)*** | 1.40(1.19, 1.64)** |
| Yes | 13 | 3138 | 4.14 | 18 | 3086 | 5.83 | 1.41(0.96, 2.07) | 2.61(1.14, 5.95)* | 2.61(0.96, 7.12) |
| P for interaction | 0.35 | ||||||||
| Hyperparathyroidism | |||||||||
| No | 780 | 107120 | 7.28 | 427 | 44375 | 9.62 | 1.32(1.22, 1.43)*** | 1.42(1.25, 1.61)*** | 1.42(1.21, 1.66)** |
| Yes | 2 | 112 | 17.9 | 1 | 142 | 7.06 | 0.39(0.07, 2.35) | - | - |
| P for interaction | 0.29 | ||||||||
| Celiac disease | |||||||||
| No | 782 | 107232 | 7.29 | 428 | 44505 | 9.62 | 1.32(1.22, 1.43)*** | 1.42(1.25, 1.61)*** | 1.42(1.21, 1.65)** |
| Yes | 0 | 0 | - | 0 | 11.7 | 0 | - | - | |
| P for interaction | - | ||||||||
| Chron’s disease | |||||||||
| No | 766 | 105230 | 7.28 | 420 | 43519 | 9.65 | 1.33(1.22, 1.44)*** | 1.42(1.25, 1.62)*** | 1.42(1.22, 1.67)** |
| Yes | 16 | 2002 | 7.99 | 8 | 997 | 8.02 | 1.00(0.56, 1.80) | 0.85(0.31, 2.33) | 0.85(0.25, 2.90) |
| P for interaction | 0.41 | ||||||||
| Lower body weight | |||||||||
| No | 768 | 104556 | 7.35 | 413 | 42491 | 9.72 | 1.32(1.22, 1.44)*** | 1.41(1.24, 1.60)*** | 1.41(1.20, 1.65)** |
| Yes | 14 | 2676 | 5.23 | 15 | 2026 | 7.4 | 1.42(0.91, 2.19) | 2.03(0.86, 4.82) | 2.03(0.71, 5.82) |
| P for interaction | 0.74 | ||||||||
PY: person-year; Rate: incidence rate (per 1,000 person-years); IRR: incidence rate ratio; Adjusted HR†: multiple analysis including age, sex, occupation, drug of oral steroid, bisphosphonates, hormone replacement therapy (HRT), vitamin D supplements, and aromatase inhibitors and each comorbidity [including hyperlipidemia, hypertension, diabetes, pneumonia, live cirrhosis, ischemia heart disease (IHD), stroke, chronic obstructive pulmonary disease (COPD), end-stage renal disease (ESRD), alcohol-related illness, hyperparathyroidism, celiac disease, Chron’s disease, and lower body weight];
*p<0.05,
**p<0.02,
***p<0.001
The RT cohort without oral steroid use was at a 1.87-fold increased risk of fragility fractures (adjusted HR = 1.87, 95% CI = 1.20–2.90; 98% CI = 1.09–3.19) compared with the non-RT cohort (Table 6). The RT cohort using oral steroid demonstrated a statistically significant increased risk of fragility fractures in men (adjusted HR = 1.89, 95% CI = 1.19–3.00; 98% CI = 1.07–3.32). Similar results were observed for osteoporosis / fragility fracture.
Table 6. Adjusted hazard ratio of fragility fractures and osteoporosis / fragility fracture found the associated with respiratory tuberculosis and drugs.
| Event | PY | Rate | Adjusted HR† (95% CI) | Adjusted HR† (98% CI) | |
|---|---|---|---|---|---|
| Fragility fractures | |||||
| Overall | |||||
| Without respiratory tuberculosis | 119 | 107232 | 1.11 | 1.00 | 1.00 |
| With respiratory tuberculosis | |||||
| Without oral steroid | 34 | 23253 | 1.46 | 1.87(1.20, 2.90)** | 1.87(1.09, 3.19)** |
| With oral steroid | 56 | 21264 | 2.63 | 1.58(1.08, 2.31)* | 1.58(0.99, 2.51) |
| Men | |||||
| Without respiratory tuberculosis | 73 | 73519 | 0.99 | 1.00 | 1.00 |
| With respiratory tuberculosis | |||||
| Without oral steroid | 25 | 14837 | 1.68 | 2.26(1.32, 3.85)** | 2.26(1.18, 4.33)** |
| With oral steroid | 40 | 14678 | 2.73 | 1.89(1.19, 3.00)** | 1.89(1.07, 3.32)** |
| Women | |||||
| Without respiratory tuberculosis | 46 | 33713 | 1.36 | 1.00 | 1.00 |
| With respiratory tuberculosis | |||||
| Without oral steroid | 9 | 8416 | 1.07 | 1.25(0.56, 2.77) | 1.25(0.47, 3.29) |
| With oral steroid | 16 | 6586 | 2.43 | 1.09(0.55, 2.15) | 1.09(0.47, 2.49) |
| Osteoporosis /fragility fractures | |||||
| Overall | |||||
| Without respiratory tuberculosis | 782 | 107232 | 7.29 | 1.00 | 1.00 |
| With respiratory tuberculosis | |||||
| Without oral steroid | 200 | 23253 | 8.60 | 1.41(1.19, 1.67)*** | 1.41(1.14, 1.74)** |
| With oral steroid | 228 | 21264 | 10.7 | 1.42(1.19, 1.70)*** | 1.42(1.14, 1.77)** |
| Men | |||||
| Without respiratory tuberculosis | 428 | 73519 | 5.82 | 1.00 | 1.00 |
| With respiratory tuberculosis | |||||
| Without oral steroid | 107 | 14837 | 7.21 | 1.56(1.23, 1.98)*** | 1.56(1.17, 2.09)** |
| With oral steroid | 132 | 14678 | 8.99 | 1.43(1.13, 1.81)** | 1.43(1.08, 1.90)** |
| Women | |||||
| Without respiratory tuberculosis | 354 | 33712 | 10.5 | 1.00 | 1.00 |
| With respiratory tuberculosis | |||||
| Without oral steroid | 93 | 8416 | 11.1 | 1.25(0.98, 1.61) | 1.25(0.92, 1.70) |
| With oral steroid | 96 | 6586 | 14.6 | 1.42(1.07, 1.89)* | 1.42(1.00, 2.01) |
PY, person-year; Rate, incidence rate (per 1,000 person-years); Adjusted HR†: multiple analysis including occupation, drug of oral steroid, bisphosphonates, hormone replacement therapy (HRT), vitamin D supplements, and aromatase inhibitors and each comorbidity [such as hyperlipidemia, hypertension, diabetes, pneumonia, live cirrhosis, ischemia heart disease (IHD), stroke, chronic obstructive pulmonary disease (COPD), end-stage renal disease (ESRD), alcohol-related illness, hyperparathyroidism, celiac disease, crohn disease, and lower body weight];
*p<0.05,
**p<0.02,
***p<0.001
Discussion
A published meta-analysis including 167 studies evaluated the risk factors for a low bone marrow density (BMD)-related fracture in men and women, and reported age (>70 years), low body weight [body mass index (BMI) <20 to 25 kg/m2], weight loss (>10%), physical inactivity, prolonged corticosteroid use, and previous osteoporotic fracture as high risk factors [20]. An additional 102 studies assessed 15 other proposed risk factors but provided insufficient evidence in support of a male population [20]. This study suggested that the incidence of fragility fracture (adjusted HR = 1.69), osteoporosis / fragility fracture (adjusted HR = 1.42) in the RT cohort is higher than in the non-RT cohort, irrespective of age, sex, steroids use and comorbidities.
Respiratory tuberculosis is one of the diseases characterized granuloma formation which was controlled by cellular immune reactions, interferon-gamma (INF-gamma) which mediate inflammatory reactions increased in the tuberculosis [21]. Expression levels of IFN-gamma have a positive correlation to bone fracture [22]. The cytokine IFN-gamma stimulates neopterin release. High levels of neopterin were associated with increased hip fracture risk [23]. These previous finding imply that the RT associated with the bone fracture, even without comorbidities or steroid use. Holloway et al. study in 3 to 5% of active cases of tuberculosis [24] with bone fracture (e.g. compression fracture) in accordance with our study [25]. However, these hypothesis warrant further research.
Vitamin D deficiency and a low calcium intake were risk factors for osteoporosis observed in men. A study conducted by Ho-Pham et al suggested that vitamin D deficiency was also reported to be a risk factor for tuberculosis in men but not in women [26]. The dual effect of vitamin D deficiency on RT and osteoporosis may confound the association between RT and bone fracture. These factors support the higher risk of the fragility fracture (adjusted HR = 1.57, P for interaction = 0.06) observed in a male population than in female belonging to the RT cohort. Dehydroepiandrosterone (DHEA) and testosterone levels were profoundly reduced in the RT cohort along with a modest increase in cortisol and estradiol levels [27]. The low DHEA increased the RANAL activity owing to the decrease of the ratio of OPG / RANKL mRNA in osteoblasts [28], the high cortisol inhibit the OPG activity, thus resulting in the osteoporosis [8]. Wang NB et al, they found the osteoporosis with low BMD in the PTB patients also [29]. BMD changes were more marked in patients with RT than in those of the same age group with other chronic lung diseases agree this finding also [30]. The osteoporosis contribute to the bone fracture. Therefore, the adjusted HR of the RT cohort for fragility fracture was higher than that of the non-RT cohort, particularly in men (for men, adjusted HR = 1.57, p <0.001; for women, adjusted HR = 0.98; p>0.05).
Vitamin D deficiency was common in both underweight and normal-weight patients, but an association between vitamin D deficiency and reduced femur neck T scores was indicated only in the underweight patients with RT [31]. The median 25(OH)D level increased after tuberculosis treatment. In Taiwan, patients with RT receive antituberculosis (anti-TB) treatment [16] or anti-TB with a short-term low dose steroid may increase the BMI of patients with RT and malnutrition [32]. The BMD of Taiwanese women shows a positive relationship to body weight and BMI in the femoral neck fracture group [33]. Similarly, patients with inhaled steroid use [34] may have the less incidence of the osteoporosis [35]. Therefore, RT cohort with steroid use and anti-TB drug may have an increased BMI [35], 25(OH)D level [31], and BMD [35]; these may explain the RT cohort with the lower body weight reveal no significant risk of the incident fragility fracture (aHR = 1.70, p value >0.05) or osteoporosis / fragility fracture (aHR = 2.03, p value >0.05). These hypotheses warrant research.
The Nanjundaiah et al. report, Lewis rats by injection of heat-killed M. tuberculosis H37Ra (Mtb). The antigen-presenting cells (APCs) took up the microbial antigens. APCs process antigens and then present these Mtb to antigen-specific T cells. These antigen-primed T cells then migrate into the joints, and release proinflammatory cytokines (osteopontin, tumor necrosis factor-α, interleukin) locally leading to arthritic inflammation. These cytokines also stimulate the production of RANKL/MCSF, which activates osteoclasts producing cathepsin K (Cat K) and matrix metalloproteases (MMPs) resulting in bone damage such as osteoporosis [36]. Similarly, sinomenine could attenuate osteoclast formation and Mtb-induced bone loss by mediating RANKL signaling pathways in Li et al study support the RT presenting as systemic inflammation and contribute to the osteoporosis in our study [37].
Women who lived in institutions and had osteoporosis, RT, and cardiac diseases (hypertension) were at risk of a contralateral hip fracture after the initial hip fracture [38]. Activity restriction led to an increased bone resorption in hospitalized women, which possibly affected the risk of osteopenia and osteoporosis [39]. In our study, the patients with the hypertension (aHR = 1.34, p value <0.05) and IHD (aHR = 1.30, p value <0.05) were association with the osteoporosis / fragility fracture in RT cohort. Meanwhile, women in the RT cohort with the oral steroid use are at an increased risk of osteoporosis / fragility fracture (aHR = 1.42, 95% CI; p value <0.05) than the non-RT cohort. These finding in line with previous study. Yet, this result need the random control trial for confirmation.
Previous studies have reported that metabolic-syndrome-related diseases such as hyperlipidemia, hypertension, diabetes, ischemic heart diseases, ESRD [10], and liver cirrhosis [11] were more common in patients with osteoporotic fracture. This study also demonstrated that metabolic diseases increased the risk of bone fracture, osteoporosis / fragility fracture. Meanwhile, alcohol-related illness were associated with the bone fractures, osteoporosis / fragility fracture in RT cohort also. Previous studies have rarely reported pneumonia as a risk factor of osteoporosis. In this study, we observed that both acute pneumonia (viral and bacterial) and chronic respiratory infectious diseases (RT) increased the risk of fragility fracture (aHR = 1.69), osteoporosis / fragility fracture (aHR = 1.42).
Respiratory infections were frequently observed in elderly patients with malnutrition. The combined effect of malnutrition, respiratory infection, and physical inactivity contributes to osteoporosis / incident fragility fracture [40]. In our study, we found that a higher incidence of bone fracture, osteoporosis / fragility fracture among the frequently hospitalized patients with RT even without low body weight, or without steroid use; compared with patients without RT. This study increases physicians awareness of incident bone fracture associated with RT.
Limitations
Several limitations must be considered when interpreting these findings. The NHIRD does not provide detailed lifestyle information such as smoking, BMI, and physical activity, which were potential confounding factors in this study. However, anti-TB treatment and lifestyle modification of patients with RT may implicate these factors in accelerated bone fracture or osteoporosis / fragility fracture observed in RT. Additionally, information on osteoporosis severity scales such as disease activity, functional impairment, and physical damage may lead to underdiagnosis of this metabolic syndrome. Insufficient drug data such as oral antidiabetic drugs to adjust for the outcomes of interest could be another limitation. The evidence derived from this retrospective cohort study is generally of lower methodological evidence than that from randomized controlled trials because a retrospective cohort study is subject to many biases due to lack of the necessary adjustments for possible confounding factors (such as lack of the important data like serum levels OPG, RANKL, osteoclast activity markers and bone formation markers; and individual data of the histological or densitometric changes in bone). The Nanjundaiah and Li et al. study were experimental study in animals. Therefore, further investigation with a prospective and randomized controlled study design to reveal the cause-effect between RT and bone fracture or osteoporosis / fragility fracture would be worthwhile. In addition, lack of BMD data to do the optimal diagnosis of osteoporosis in the NHIRD is the study limitation. However, NHIRD covers a highly representative sample of Taiwan’s general population because the reimbursement policy is universal and operated by a single-buyer, the government in Taiwan. All insurance claims should be scrutinized by medical reimbursement specialists and peer review according to the standard diagnosed criteria in the study. If these doctors or hospitals make wrong diagnoses or coding, they will be punished with a lot of penalties. Therefore, the diagnoses of osteoporosis based on ICD-9 codes in this study were highly reliable. In addition, fracture reported here is based on ICD codes, not X-ray report. We can’t distinguish between atraumatic and traumatic fractures. Meanwhile, Underlying causes of pathological fractures include osteoporosis, metastatic bone tumor, osteomyelitis, Paget’s disease, disuse atrophy, hyperparathyroidism, and nutritional or congenital disorders [Coding for Fractures: For The Record Vol. 20 No. 24 P. 28 (Great Valley Publishing Co., Inc)]. After we did analyses, we didn’t find the coding of the [ICD-9-CM -198.5, Secondary malignant neoplasm of bone and bone marrow; ICD-9-CM—170.9, Malignant neoplasm of bone and articular cartilage, site unspecified; ICD-9-CM-731.0, Osteitis deformans without mention of bone tumor] in the RT cohort. The impact of these confounding factors on the fragility fractures needs further investigation. Finally, when performing several tests, increasing the family-wise error rate (FWER, the probability of rejecting at least one null hypothesis erroneously). In statistics, FWER is the probability of making one or more false discoveries, or typeΙerrors when performing multiple hypotheses tests. The Bonferroni adjustment will always provide strong control of the family-wise error rate [41]. If the number of comparisons in the test becomes large, the test may become too conservative and no longer allows us to find anything significant [42].
Strength
The nationwide population-based longitudinal cohort study used to investigate the risk factors of incident bone fracture, osteoporosis / fragility fracture in an Asian population with RT was the strength of this study. We investigated drug effects such as oral steroid of the impact on the osteoporosis. We have replaced the smoking history data with the comorbidity which were associated with smoking such as IHD, stroke and COPD for adjustment. Meanwhile the life style such as drinking (alcohol-related disease) and patients received anti-osteoporosis drugs were included for analysis also. Furthermore, the study included participants from the general population representative of a true population, thereby improving the generalizability of our results. Even the BMD unavailable in this study; the policy of diagnosis of the osteoporosis is well established in Taiwan [43]. The coding the osteoporosis under the “guideline for the prevention and treatment of osteoporosis in Taiwan” at most healthcare system [44]. This multidisciplinary system may avoid the diagnosis bias.
Conclusion
The Respiratory tuberculosis associated with the incident fragility fracture, either in men or absence of oral steroid use
Supporting Information
(DOC)
Abbreviations
- aHR
adjusted hazard ratio
- APCs
antigen-presenting cells
- Cat K
cathepsin K
- CI
confidence interval
- HCV
hepatitis C virus
- HRT
hormone replacement therapy
- INF-gamma
interferon-gamma
- LHID 2000
Longitudinal Health Insurance Database 2000
- MMPs
matrix metalloproteases
- Mtb
M. tuberculosis
- NHIRD
National Health Insurance Research Database
- NHI
National Health Insurance
- NHRI
National Health Research Institutes
- OPG
osteoprotegerin
- PTB
pulmonary tuberculosis
- PTH
Parathyroid hormone
- RANKL
receptor activator of nuclear factor kappa-B ligand
- RT
respiratory tuberculosis
Data Availability
All data and related metadata were deposited in an appropriate public repository. The data on the study population that were obtained from the NHIRD (http://w3.nhri.org.tw/nhird/date_01.html) are maintained in the NHIRD (http://nhird.nhri.org.tw/). The NHRI is a nonprofit foundation established by the government.
Funding Statement
This study is supported in part by Taiwan Ministry of Health and Welfare Clinical Trial and Research Center of Excellence (MOHW105-TDU-B-212-133019), China Medical University Hospital, Academia Sinica Taiwan Biobank Stroke Biosignature Project (BM10501010037), NRPB Stroke Clinical Trial Consortium (MOST 104-2325-B-039 -005), Tseng-Lien Lin Foundation, Taichung, Taiwan, Taiwan Brain Disease Foundation, Taipei, Taiwan, and Katsuzo and Kiyo Aoshima Memorial Funds, Japan; and CMU under the Aim for Top University Plan of the Ministry of Education, Taiwan. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. No additional external funding received for this study.
References
- 1.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res. 2007;22: 465–475. 10.1359/jbmr.061113 [DOI] [PubMed] [Google Scholar]
- 2.Shriraam V, Mahadevan S, Anitharani M, Selvavinayagam, Sathiyasekaran B. National health programs in the field of endocrinology and metabolism—Miles to go. Indian J Endocrinol Metab. 2014;18: 7–12. 10.4103/2230-8210.126521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sale JE, Beaton D, Bogoch E. Secondary prevention after an osteoporosis-related fracture: an overview. Clin Geriatr Med. 2014;30: 317–332. 10.1016/j.cger.2014.01.009 [DOI] [PubMed] [Google Scholar]
- 4.Osteoporosis. Information from your family doctor. Am Fam Physician. 2009;79: 201–202. [PubMed] [Google Scholar]
- 5.Hodgson SF, Watts NB, Bilezikian JP, Clarke BL, Gray TK, Harris DW, et al. American Association of Clinical Endocrinologists medical guidelines for clinical practice for the prevention and treatment of postmenopausal osteoporosis: 2001 edition, with selected updates for 2003. Endocr Pract. 2003;9: 544–564. 10.4158/EP.9.6.544 [DOI] [PubMed] [Google Scholar]
- 6.Trouvin AP, Goeb V. Receptor activator of nuclear factor-kappaB ligand and osteoprotegerin: maintaining the balance to prevent bone loss. Clin Interv Aging. 2010;5: 345–354. 10.2147/CIA.S10153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sambrook P, Cooper C. Osteoporosis. Lancet. 2006;367: 2010–2018. 10.1016/S0140-6736(06)68891-0 [DOI] [PubMed] [Google Scholar]
- 8.Romas E. Clinical applications of RANK-ligand inhibition. Intern Med J. 2009;39: 110–116. 10.1111/j.1445-5994.2008.01732.x [DOI] [PubMed] [Google Scholar]
- 9.McGowan B, Bennett K, Marry J, Walsh JB, Casey MC. Patient profile in a bone health and osteoporosis prevention service in Ireland. Ir J Med Sci. 2012;181: 511–515. 10.1007/s11845-012-0806-9 [DOI] [PubMed] [Google Scholar]
- 10.Lai SW, Liao KF, Lai HC, Tsai PY, Lin CL, Chen PC, et al. Risk of major osteoporotic fracture after cardiovascular disease: a population-based cohort study in Taiwan. J Epidemiol. 2013;23: 109–114. 10.2188/jea.JE20120071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dong HV, Cortes YI, Shiau S, Yin MT. Osteoporosis and fractures in HIV/hepatitis C virus coinfection: a systematic review and meta-analysis. AIDS. 2014;28:2119–31. 10.1097/QAD.0000000000000363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pattamapaspong N, Muttarak M, Sivasomboon C. Tuberculosis arthritis and tenosynovitis. Semin Musculoskelet Radiol. 2011;15: 459–469. 10.1055/s-0031-1293492 [DOI] [PubMed] [Google Scholar]
- 13.Spiegel DA, Singh GK, Banskota AK. Tuberculosis of the Musculoskeletal System. Techniques in Orthopaedics. 2005;20: 167–178. [Google Scholar]
- 14.Yen YF, Yen MY, Lin YP, Shih HC, Li LH, Chou P, et al. Directly observed therapy reduces tuberculosis-specific mortality: a population-based follow-up study in Taipei, Taiwan. PLoS ONE. 2013;8: e79644 10.1371/journal.pone.0079644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pietri M, Lucarini S. The orthopaedic treatment of fragility fractures. Clin Cases Miner Bone Metab. 2007;4: 108–116. [PMC free article] [PubMed] [Google Scholar]
- 16.Curtis JR, Taylor AJ, Matthews RS, Ray MN, Becker DJ, Gary LC, et al. "Pathologic" fractures: should these be included in epidemiologic studies of osteoporotic fractures? Osteoporos Int. 2009;20: 1969–1972. 10.1007/s00198-009-0840-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang Y, Du F, Ye W, Chen Y, Li J, Zhang J, et al. Inpatient cost of treating osteoporotic fractures in mainland China: a descriptive analysis. Clinicoecon Outcomes Res. 2015;7: 205–212. 10.2147/CEOR.S77175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yeh CC, Wang HH, Chou YC, Hu CJ, Chou WH, Chen TL, et al. High risk of gastrointestinal hemorrhage in patients with epilepsy: a nationwide cohort study. Mayo Clin Proc. 2013;88: 1091–1098. 10.1016/j.mayocp.2013.06.024 [DOI] [PubMed] [Google Scholar]
- 19.Evans DJ. The use of adjunctive corticosteroids in the treatment of pericardial, pleural and meningeal tuberculosis: do they improve outcome? Respir Med. 2008;102: 793–800. 10.1016/j.rmed.2008.01.018 [DOI] [PubMed] [Google Scholar]
- 20.Liu H, Paige NM, Goldzweig CL, Wong E, Zhou A, Suttorp MJ, et al. Screening for osteoporosis in men: a systematic review for an American College of Physicians guideline. Ann Intern Med. 2008;148: 685–701. [DOI] [PubMed] [Google Scholar]
- 21.Kim M, Ahn JH, Moon HS, Park SH, Song JS. The Changes of Serum Level of Tumor Necrosis Factor-Alpha, Gamma-Interferon and Soluble-Intercellular Adhesion Molecule-1 Relating to the Progression and Treatment of Patients with Pulmonary Tuberculosis. Tuberc Respir Dis. 1998;45: 1167–1177. [Google Scholar]
- 22.Chen H, Cheng C, Li M, Gao S, Li S, Sun H. Expression of TNF-alpha, IFN-gamma, TGF-beta, and IL-4 in the spinal tuberculous focus and its impact on the disease. Cell Biochem Biophys. 2014;70: 1759–1764. 10.1007/s12013-014-0125-z [DOI] [PubMed] [Google Scholar]
- 23.Apalset EM, Gjesdal CG, Ueland PM, Øyen J, Meyer K, Midttun Ø, et al. Interferon gamma (IFN-gamma)-mediated inflammation and the kynurenine pathway in relation to risk of hip fractures: the Hordaland Health Study. Osteoporos Int. 2014;25: 2067–2075. 10.1007/s00198-014-2720-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Holloway KL, Henneberg RJ, de Barros Lopes M, Henneberg M. Evolution of human tuberculosis: a systematic review and meta-analysis of paleopathological evidence. Homo. 2011;62: 402–458. 10.1016/j.jchb.2011.10.001 [DOI] [PubMed] [Google Scholar]
- 25.Holloway KL, Link K, Ruhli F, Henneberg M. Skeletal lesions in human tuberculosis may sometimes heal: an aid to palaeopathological diagnoses. PLoS ONE. 2013;8: e62798 10.1371/journal.pone.0062798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ho-Pham LT, Nguyen ND, Nguyen TT, Nguyen DH, Bui PK, Nguyen VN, et al. Association between vitamin D insufficiency and tuberculosis in a Vietnamese population. BMC Infect Dis. 2010;10: 306 10.1186/1471-2334-10-306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rey AD, Mahuad CV, Bozza VV, Bogue C, Farroni MA, Bay ML, et al. Endocrine and cytokine responses in humans with pulmonary tuberculosis. Brain Behav Immun. 2007;l21: 171–179. [DOI] [PubMed] [Google Scholar]
- 28.Wang YD, Wang L, Li DJ, Wang WJ. Dehydroepiandrosterone inhibited the bone resorption through the upregulation of OPG/RANKL. Cell Mol Immunol. 2006;3: 41–45. [PubMed] [Google Scholar]
- 29.Wang NB, Wang HX, Gao JX. Therapeutic effect of exercise therapy on bone mineral density and low back pain in pulmonary tuberculosis patients with osteoporosis. Chinese Journal of Clinical Rehabilitation. 2005;9: 176–177. [Google Scholar]
- 30.Savula MM, Kravchenko NS, Slivka IuI. [Bone mineral density in some lung diseases]. Probl Tuberk Bolezn Legk. 2004;45–47. [PubMed] [Google Scholar]
- 31.Førli L, Halse J, Haug E, Bjørtuft Ø, Vatn M, Kofstad J, et al. Vitamin D deficiency, bone mineral density and weight in patients with advanced pulmonary disease. J Intern Med. 2004;256: 56–62. 10.1111/j.1365-2796.2004.01337.x [DOI] [PubMed] [Google Scholar]
- 32.Dooley DP, Carpenter JL, Rademacher S. Adjunctive corticosteroid therapy for tuberculosis: a critical reappraisal of the literature. Clin Infect Dis. 1997;25: 872–887. [DOI] [PubMed] [Google Scholar]
- 33.Yang TS, Chen YR, Chen YJ, Chang CY, Ng HT. Osteoporosis: prevalence in Taiwanese women. Osteoporos Int. 2004;15: 345–347. 10.1007/s00198-003-1509-x [DOI] [PubMed] [Google Scholar]
- 34.Liu SF, Kuo HC, Liu GH, Ho SC, Chang HC, Huang HT, et al. Inhaled corticosteroids can reduce osteoporosis in female patients with COPD. Int J Chron Obstruct Pulmon Dis. 2016;11: 1607–1614. 10.2147/COPD.S106054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yanik B, Ayrim A, Ozol D, Koktener A, Gokmen D. Influence of obesity on bone mineral density in postmenopausal asthma patients undergoing treatment with inhaled corticosteroids. Clinics (Sao Paulo). 2009;64: 313–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nanjundaiah SM, Astry B, Moudgil KD. Mediators of inflammation-induced bone damage in arthritis and their control by herbal products. Evid Based Complement Alternat Med. 2013;2013: 518094 10.1155/2013/518094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li X, He L, Hu Y, Duan H, Li X, Tan S, et al. Sinomenine suppresses osteoclast formation and Mycobacterium tuberculosis H37Ra-induced bone loss by modulating RANKL signaling pathways. PLoS ONE. 2013;8: e74274 10.1371/journal.pone.0074274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liu S, Zhu Y, Chen W, Sun T, Cheng J, Zhang Y. Risk factors for the second contralateral hip fracture in elderly patients: a systematic review and meta-analysis. Clin Rehabil. 2015;29:285–94. 10.1177/0269215514542358 [DOI] [PubMed] [Google Scholar]
- 39.Vanderspank D, Bernier SM, Sopper MM, Watson P, Mottola MF. Activity restriction increases deoxypyridinoline excretion in hospitalized high-risk pregnant women. Biol Res Nurs. 2014;16: 7–15. 10.1177/1099800412463120 [DOI] [PubMed] [Google Scholar]
- 40.Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster JY, et al. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2013;24: 23–57. 10.1007/s00198-012-2074-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Armstrong RA. When to use the Bonferroni correction. Ophthalmic Physiol Opt. 2014;34: 502–508. 10.1111/opo.12131 [DOI] [PubMed] [Google Scholar]
- 42.Perneger TV. What’s wrong with Bonferroni adjustments. BMJ. 1998;316: 1236–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hwang JS, Chan DC, Chen JF, Cheng TT, Wu CH, Soong YK, et al. Clinical practice guidelines for the prevention and treatment of osteoporosis in Taiwan: summary. J Bone Miner Metab. 2014;32: 10–16. 10.1007/s00774-013-0495-0 [DOI] [PubMed] [Google Scholar]
- 44.Yeh MC, Weng SF, Shen YC, Chou CW, Yang CY, Wang JJ, et al. Increased Risk of Sudden Sensorineural Hearing Loss in Patients With Osteoporosis: A Population-based, Propensity Score-matched, Longitudinal Follow-Up Study. J Clin Endocrinol Metab. 2015;100: 2413–2419. 10.1210/jc.2014-4316 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
Data Availability Statement
All data and related metadata were deposited in an appropriate public repository. The data on the study population that were obtained from the NHIRD (http://w3.nhri.org.tw/nhird/date_01.html) are maintained in the NHIRD (http://nhird.nhri.org.tw/). The NHRI is a nonprofit foundation established by the government.