Abstract
Transforming growth factor-beta (TGF-β) is a multi-functional cytokine implicated in the control of cell growth and differentiation. TGF-β signals through a complex of TGF-β receptors 1 and 2 (TGFβR1 and TGFβR2) that phosphorylate and activate Smad2/3 transcription factors driving transcription of the Smad-target genes. The Na+/K+-ATPase is an integral plasma membrane protein critical for maintaining the electro-chemical gradient of Na+ and K+ in the cell. We found that inhibition of the Na+/K+ ATPase by ouabain results in a dramatic decrease in the expression of TGFβR2 in human lung fibrobalsts (HLF) at the mRNA and protein levels. This was accompanied by inhibition of TGF-β-induced Smad phosphorylation and the expression of TGF-β target genes, such as fibronectin and smooth muscle alpha-actin. Inhibition of Na+/K+ ATPase by an alternative approach (removal of extracellular potassium) had a similar effect in HLF. Finally, treatment of lung alveolar epithelial cells (A549) with ouabain also resulted in the downregulation of TGFβR2, the inhibition of TGF-β-induced Smad phosphorylation and of the expression of mesenchymal markers, vimentin and fibronectin. Together, these data demonstrate a critical role of Na+/K+-ATPase in the control of TGFβR2 expression, TGF-β signaling and cell responses to TGF-β.
Introduction
Transforming growth factor-β (TGF-β) is a multi-functional cytokine implicated in regulation of epithelial cell growth [1–3], differentiation of smooth muscle cells [4], myofibroblast transformation [5–7], epithelial-to-mesenchymal transition [8,9] and other cellular processes. TGF-β signals through a receptor kinase complex, consisting of TGF-β receptor type I (TGFβR1) and TGF-β receptor type II (TGFβR2). Upon binding of TGF-β to the receptor complex, TGFβR2 phosphorylates and activates TGFβR1, which in turn phosphorylates SMAD2/3 transcription factors. The phosphorylated SMAD2/3 heterodimerize with SMAD4, translocate to the nucleus and bind to SMAD binding elements (SBE) in target genes to initiate SMAD-dependent gene transcription [10].
The TGF-β signaling pathway is a highly regulated process. There is evidence to support internalization of the TGF-β receptors via clathrin coated pits or lipids rafts plays a role in modulating TGF-β-induced signaling. Endocytosis of TGF-β receptors by clathrin-coated pits to phosphatidylinositol-3 phosphate enriched early endosome, allows for the recruitment of SARA (the SMAD anchor for receptor activation) via the FYVE domain, to mediate Smad phosphorylation [11]. Blocking of clathrin-mediated endocytosis is sufficient to inhibit TGF-β signaling [12]. On the other hand, endocytosis by lipid rafts is associated with decreased signaling by increasing TGF-β receptor degradation. Disruption of lipid rafts by nystatin decreased receptor turnover and therefore enhanced TGF-β signaling [13]. Thus, lipid rafts may play a dual role in TGF-β receptor signaling and receptor downregulation.
The Na+/K+ ATPase (sodium pump) is an integral plasma membrane protein required for maintaining the electro-chemical gradient of Na+ and K+ in the cell. The pump is made up of the catalytic alpha subunit and the regulatory beta subunit. The alpha subunit hydrolyzes ATP to pump 3Na+ ions out of the cell and 2K+ ions into the cell against their concentration gradient. The beta subunit stabilizes the enzyme [14–16] and acts as a molecular chaperone to assist in the transport and insertion of the alpha subunit to the plasma membrane [17]. A family of drugs known as cardiac glycosides, including digoxin and ouabain, bind to the catalytic alpha subunit and are pharmacological inhibitors of the Na+/K+ ATPase [18]. Digoxin, isolated from Digitalis lanata [19], has been used for treatment of congestive heart failure and cardiac arrhythmias [20]. Ouabain, isolated from Strophanthus gratus [21], is the most commonly used cardiac glycoside for in vitro studies due to its high water solubility. Inhibition of Na+/K+ ATPase by cardiac glycosides leads to an increase in the intracellular Na+/K+ ratio and depolarization of cells, resulting in the activation of reverse mode of Na+/Ca2+ exchanger and of voltage-gated Ca2+ channels, respectively, both leading to an increase in the intracellular Ca2+ concentrations [22].
Recent studies have suggested that cardiac glycosides, through binding to Na+/K+-ATPase, can also affect cell growth signaling pathways. It was shown initially that ouabain and marinobufagenin induced proliferation of vascular smooth muscle cells [23]. Subsequently, it was demonstrated that ouabain stimulated Src / epidermal growth factor receptor (EGFR) signaling leading to the activation of extracellular signal regulated proteins kinases (ERK1/2) and of phosphatidylinositol-3-kinase (PI3K) in various cell types [24–26]. It was reported that at least some of these effects of ouabain (i.e. activation of ERK1/2, but not of PI3K) are mediated through a direct interaction and activation of Src by ouabain-bound Na+/K+ ATPase [27–29]. Interestingly, the signaling role of Na+/K+ ATPase was reported to be associated with caveolae, where significant amounts of Src, EGFR, ERK1/2 and α1/2-subuntis of Na+/K+-ATPase have been detected [30,31]. However, this signaling role of caveolae seems to be dissociated from the Na+/K+ pump activity and from regulation of cardiac contractility by Na+/K+ ATPase [32–34].
In this study, we show for the first time that inhibition of the Na+/K+ ATPase leads to substantial downregulation of TGFβR2 expression at mRNA and protein levels resulting in the inhibition of TGF-β signaling and cellular responses, and this effect is likely mediated through inhibition of the Na+/K+ pump activity of Na+/K+-ATPase.
Materials and Methods
Primary Culture of Human Lung Fibroblasts
Human lung fibroblasts were cultured as described previously [6,7]. Briefly, human lung parenchyma was minced to ∼1-mm3 pieces, washed, and plated on 10-cm plates in growth medium containing Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 10% FBS, L-glutamine, and antibiotics. The medium was changed every two days. After ∼2 weeks, the explanted and amplified fibroblasts were cleared from the tissue pieces, trypsinized, and further amplified as passage 1. For experiments, cells were grown in 12-well plates at a density of 1 × 105 cells per well in growth medium for 24 hours, starved in DMEM containing sterile bovine serum albumin at 0.1% (DMEM/BSA) for 24 hours, and treated with desired drugs or with DMEM/BSA containing or lacking potassium chloride (5mM) for desired times.
Reverse Transcription-quantitative Real-time PCR
RNA STAT-60 (TEL-Test) was used to isolate total RNA following the manufacturer's protocol. RNA was randomly primed and reverse transcribed using the iScript cDNA synthesis kit (Bio-Rad, Hercules, USA) according to the manufacturer's protocols. Real-time PCR analysis was performed using iTaq SYBR Green Supermix with ROX (Bio-Rad) in a MyIQ single-color real-time PCR detection system (Bio-Rad), The TGFΒR2 primers were: GGAGTTTCCTGTTTCCCCCG (forward) and ATGTCTCAGTGGATGGGCAG (reverse). The 18s primers were: GATTAAGTCCCTGCCCTTTG (forward) and GTTCACCTACGGAAACCTTG (reverse).
Western Blotting
Cells were lysed in urea buffer containing 8 M deionized urea, 1% SDS, 10% glycerol, 60mM Tris-HCl pH 6.8, 0.02% pyronin Y, and 5% β-mercaptoethanol. Lysates were sonicated for 5 s. Samples were then subjected to polyacrylamide gel electrophoresis and Western blotting with desired primary antibodies and corresponding horseradish peroxidase (HRP)-conjugated secondary antibodies, and developed by chemiluminescence reaction (Pierce). Digital chemiluminescent images below the saturation level were obtained with a LAS-4000 analyzer, and the light intensity was quantified using Multi Gauge software (Fujifilm).
Reagents
Dulbecco’s Modified Eagle Medium was from Thermofisher, catalog number 11960044. L-glutamine was from Thermofisher, catalog # 25030081. Antibiotic-Antimycotic was from Thermofisher, catalog # 15240062. Ouabain octahydrate was from Sigma-Aldrich, CAS # 11018-89-6. TGF-β was from EMD Millipore, catalog # GF111 (Billerica, MA). Pharmaceutical grade bleomycin (BLEOmycin) was from TEVA (lot#: 31314497B). iScript cDNA Synthesis (catalog # 1708891) and iTaq SYBR Green Supermix (catalog # 1725121) were from Bio-Rad. Antibodies for Western blotting against SM α-actin (catalog # A5228-200ul), β-actin (catalog # A5441-.2ML), and α-tubulin (catalog # T6074-200ul) were from Sigma-Aldrich; collagen-1 was from Cedarlane laboratories (catalog # CL50111AP-1), and transforming growth factor-beta type 2 receptor antibodies were from Santa Cruz (catalog # SC-400)
Statistical Analysis
Quantitative data from three independent experiments were analyzed by Student's T-test. Values of p < 0.05 were considered statistically significant.
Results
Inhibition of the Na+/K+ ATPase Downregulates the mRNA and Protein Expression of TGFβR2
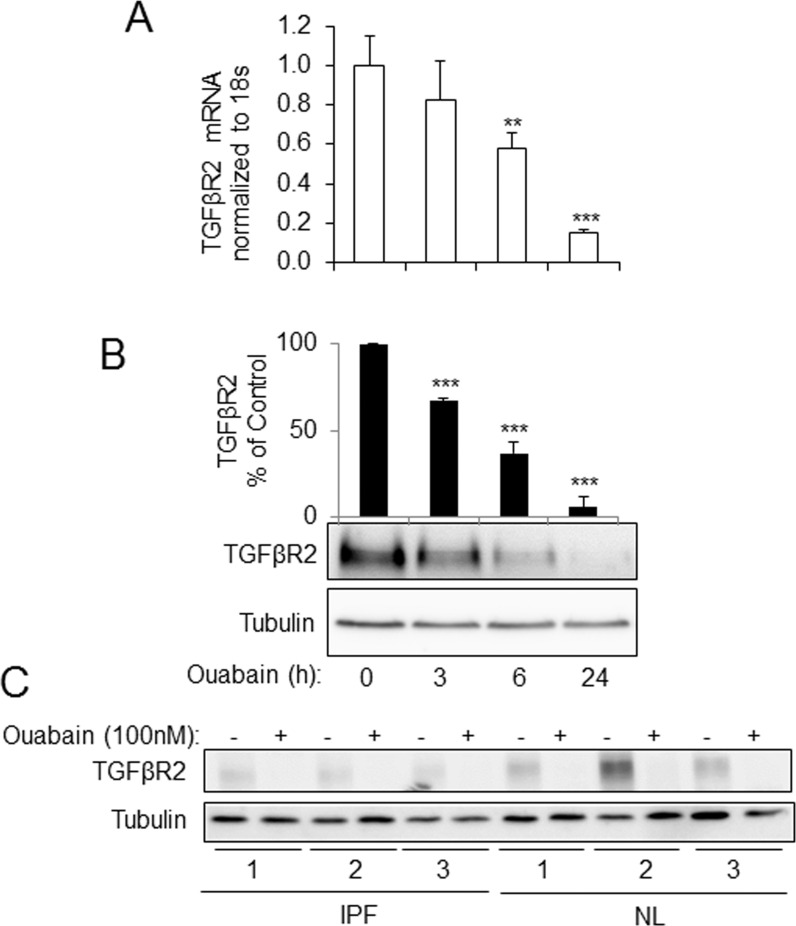
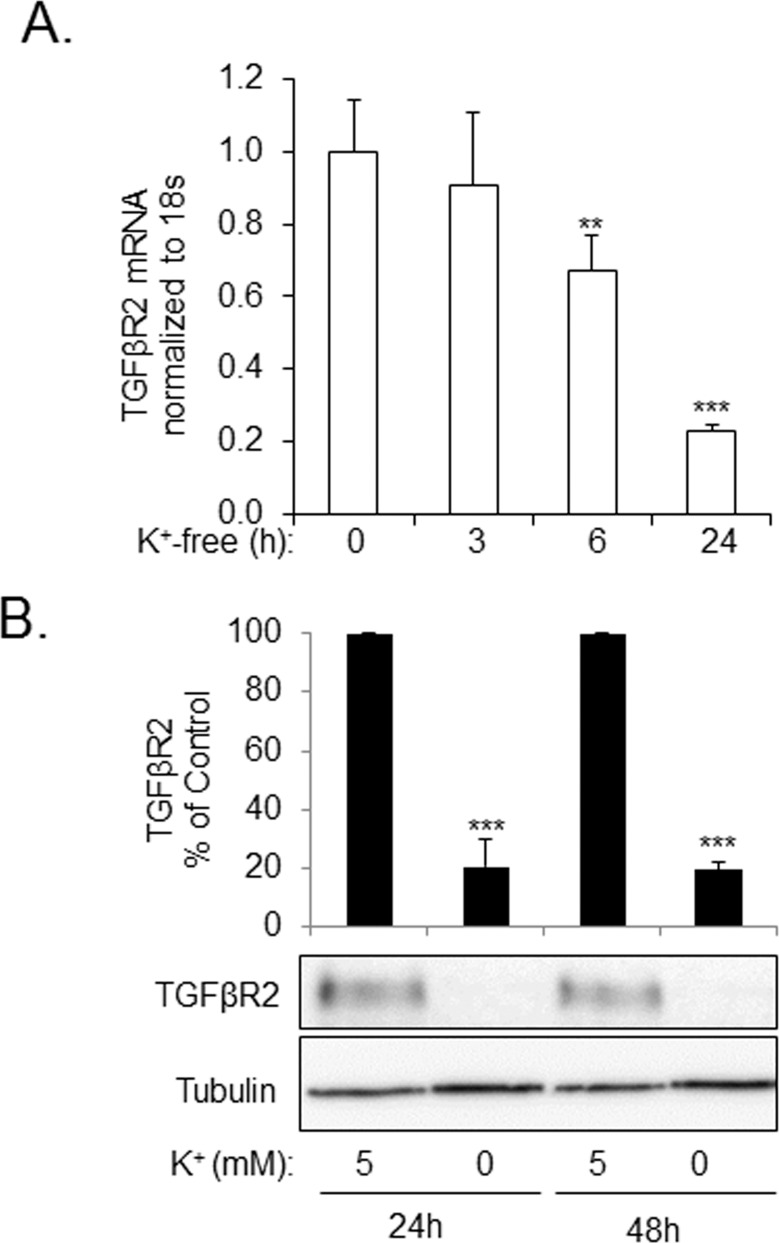
Fig 1 shows that treatment of human lung fibroblasts (HLFs) with 100 nM ouabain resulted in a time-dependent downregulation of TGFβR2 mRNA (Fig 1A) and protein (Fig 1B) levels, as assessed by real time qPCR and Western blotting, respectively. The inhibitory effect of ouabain on TGFβR2 expression was further examined using primary HLF cultures isolated from lungs of six individuals—three with idiopathic pulmonary fibrosis (IPF) and three with non-fibrotic lungs (NL). As shown in Fig 1C, while variable expression of TGFβR2 between the HLF cultures was observed, 100 nM ouabain substantially reduced TGFβR2 expression in all six HLF cultures. In order to determine whether the downregulation of TGFβR2 by ouabain was due to the inhibition Na+/K+ ATPase, we used an alternative approach for inhibition of Na+/K+ ATPase through a removal of extracellular potassium. As shown in Fig 2, incubation of HLFs in a potassium-free medium resulted in a sustained inhibition of the expression of TGFβR2 mRNA and protein as compared to the medium containing 5 mM KCl.
Fig 1. Ouabain down-regulates TGFβR2 mRNA and protein levels in human lung fibroblasts (HLF).
Serum-starved HLF were treated with 100 nM ouabain for 3, 6, and 24 hours. Cells were analyzed by real-time qPCR for TGFβR2 mRNA levels (A) and by Western blotting for TGFβR2 protein levels (B). Shown are the representative images and the quantitative analysis of ECL (mean±SD) from at least three independent experiments (RLU, relative light units). **p < 0.005, ***p < 0.0005. C. HLF isolated and cultured from IPF and non-IPF (NL) lungs were treated with or without 100 nM ouabain. Cells lysates were analyzed for TGFβR2 or tubulin protein expression by Western blotting.
Fig 2. Inhibition of Na+/K+ ATPase by potassium free media results in the down-regulation of TGFβR2 mRNA and protein levels in human lung fibroblasts (HLF).
A. HLFs were placed in potassium free media for 3, 6, and 24 hours, and then analyzed for TGFβR2 mRNA levels via real time qPCR. B. HLFs were treated with media containing either 5 mM KCl or 0 mM KCl for 24 or 48 hours. Cell extracts were examined by Western blotting for TGFβR2 expression or tubulin. Shown are the representative images and the quantitative analysis of ECL (mean±SD) from at least three independent experiments (RLU, relative light units). **p < 0.005, ***p < 0.0005.
Downregulation of TGFβR2 Through Inhibition of the Na+/K+-ATPase Results in Decreased Cellular Responses to TGF-β
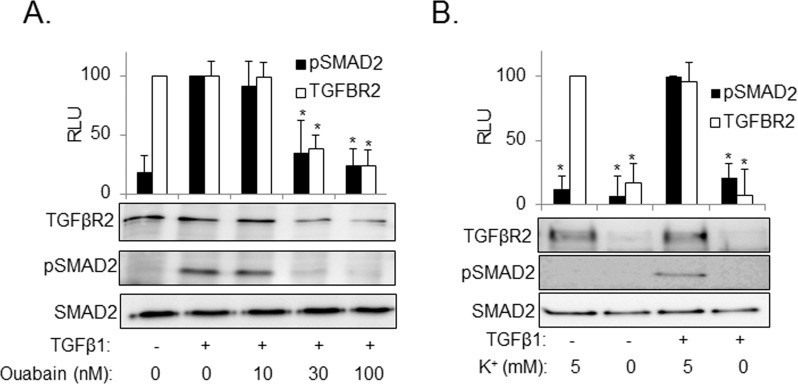
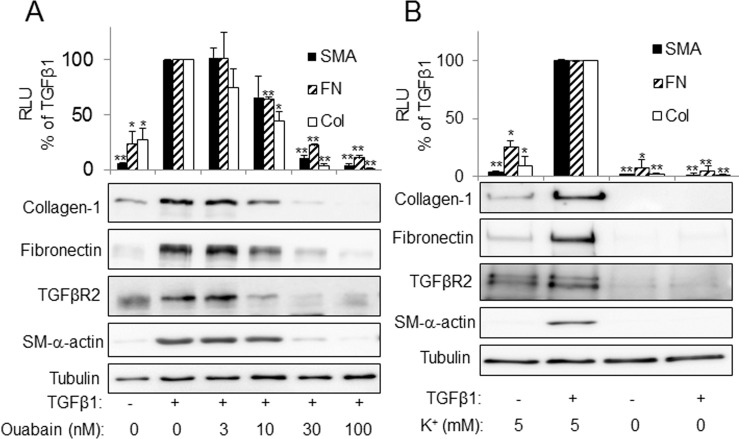
To determine whether downregulation of TGFβR2 through inhibition of Na+/K+-ATPase translates to the functional cell responses to TGF-β, we treated HLFs with TGF-β in the presence or absence of ouabain. As shown in Fig 3, TGF-β-induced phosphorylation of Smad2 was inhibited by ouabain (Fig 3A) or through incubation in potassium-free media (Fig 3B). Furthermore, ouabain or removal of extracellular potassium blocked TGF-β-induced expression of TGF-β-target genes such as fibronectin or α-smooth muscle actin (α-SMA) (Fig 4), without affecting the levels of tubulin or caveolin-1 (S1 Fig).
Fig 3. Inhibition of the Na,K-ATPase by potassium free media or by ouabain blocks TGFβ1-induced SMAD2 phosphorylation.
HLF were pretreated with ouabain at 10, 30,100 nM (A) or placed in media containing 5 mM KCl or 0 mM KCl (B) for 24 hours. Cells were then stimulated with 1ng/ml of TGFβ1 for 1 hour. Cell lysates were analyzed by Western blotting with desired antibodies as indicated. Shown are the representative images and the quantitative analysis of ECL (mean±SD) from at least three independent experiments (RLU, relative light units). *, p < 0.05.
Fig 4. Inhibition of the Na,K-ATPase by potassium free media and ouabain blocks TGFβ1-induced myofibroblast differentiation.
HLF were treated with increasing doses of ouabain (A) or placed in media containing 5 mM KCl or 0 mM KCl (B) and stimulated with or without 1 ng/ml of TGFβ1 for 24 hours. Cell lysates were then analyzed by Western blotting with desired antibodies as indicated. Shown are the representative images and the quantitative analysis of ECL (mean±SD) from at least three independent experiments (RLU, relative light units). *p < 0.005, **p < 0.0005.
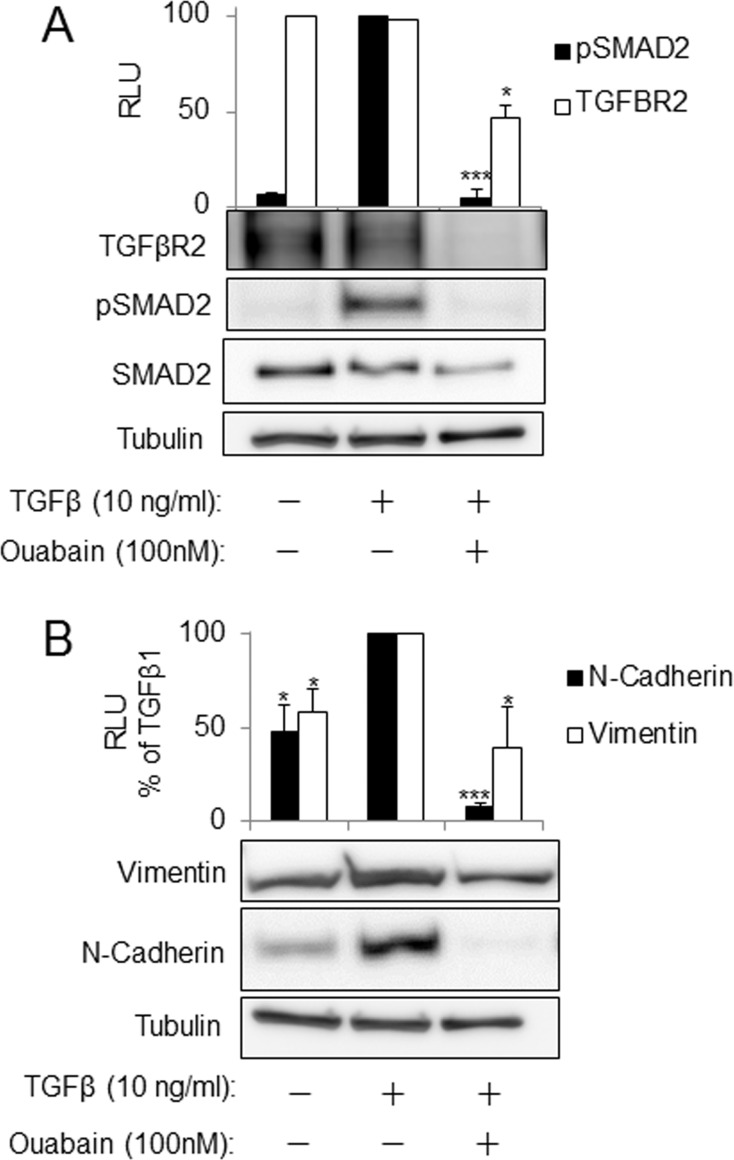
To determine whether the inhibitory effects of ouabain on TGFβR2 expression that we observed in fibroblasts could be generalized to other cells, we treated human alveolar epithelial cells (A549) with TGF-β in the presence and absence of ouabain. Fig 5 demonstrates that treatment of A549 cells with ouabain inhibits TGFβR2 expression, TGF-β-induced Smad2 phosphorylation and the expression of TGF-β target genes, vimentin and N-cadherin.
Fig 5. Downregulation of TGFβR2 by ouabain is accompanied by inhibition of TGFβ1-induced SMAD2 phosphorylation and of the expression of mesenchymal markers in A549 cells.
Serum starved A549 cells were pretreated with increasing doses of ouabain for 24 hours followed by stimulation with 10ng/ml of TGFβ1 for 1 hour (A) or simultaneously treated with ouabain and TGFβ1 for 48 hours (B). Cell lysates were then analyzed by Western blotting with desired antibodies as indicated. Shown are the representative images and the quantitative analysis of ECL (mean±SD) from at least three independent experiments (RLU, relative light units). *, p < 0.05, **p < 0.005, ***p < 0.0005.
Discussion
Cardiac glycosides have been used extensively for the treatment of cardiac arrhythmias and heart failure due to their positive inotropic effects. Inhibition of the Na+/K+ ATPase and the resultant increase in intracellular Ca2+ concentration in cardiac myocytes is considered a major mechanism for the therapeutic effects of cardiac glycosides. Our study for the first time demonstrates that inhibition of Na+/K+ ATPase by two independent approaches (ouabain and K+-free media) downregulates TGFβR2 mRNA and protein levels in human lung fibroblasts and alveolar epithelial (A549) cells, resulting in the loss of TGFβ-induced signaling (SMAD2 phosphorylation) and functional responses to TGF-β (myofibroblast differentiation and EMT).
At this time, the precise mechanism by which ouabain downregulates the expression of TGFβR2 is not clear. It is well established that binding of ouabain to Na+/K+ ATPase results in the inhibition of its pump activity. In our experiments, the depletion of extracellular potassium, an alternative approach of inhibiting the Na+/K+ ATPase, resulted in effects similar to ouabain treatment on TGFβR2 expression, TGF-β-induced Smad2 phosphorylation and gene expression. This suggests that the effects of ouabain are likely mediated by inhibition of the Na+/K+ -ATPase pump activity. On the other hand, increasing evidence suggests that cardiac glycosides may promote cell growth signaling through Src, EGFR, ERK and PI3K in caveolae [23–31]. Even though these caveolae-mediated signaling events may be dissociated from the pump activity of Na+/K+ ATPase [32–34], it is possible that these signaling events may also contribute to the downregulation of TGFβR2 expression by ouabain. Understanding the mechanism by which cardiac glycosides downregulate TGFβR2 expression is our current goal.
Myofibroblast differentiation and possibly EMT are thought to represent critical processes in wound healing and pathogenesis of fibrosis during congestive heart failure [35–37], secondary or idiopathic pulmonary fibrosis [38–41], advanced kidney disease [42–44], scleroderma [45,46], and liver cirrhosis [47,48]. Importantly, TGF-β levels are upregulated in fibrotic organs; and TGF-β signaling is thought to be critical for the development of fibrosis [49,50]. Thus, it is conceivable that if cardiac glycosides decrease the expression of TGFβR2 and TGF-β signaling in vivo they may have potential as anti-fibrotic agents.
In addition to treatment of heart disease, recent studies may suggest that cardiac glycosides may be re-purposed for treatment of other diseases, such as cancer [51,52]. The first observation of possible anti-cancer effects of cardiac glycosides was noted in 1979 by Dr. Stenkvist [53]. He noticed that tumor cells in breast cancer patients taking cardiac glycosides showed more benign characteristics as compared to patients not taking cardiac glycosides [53]. Moreover, patients with breast cancer taking digitalis were ~10 times less likely to have recurring cancer within 5 years after mastectomy, suggesting that cardiac glycosides may play a role in modulating aggressiveness of the tumor [54]. A 20-year follow-up study showed that 6% as compared to 34% patients died from breast cancer when on digitalis compared to those not on digitalis [55]. Given our new data and the reported role of TGF-β in stroma development and metastasis [56–58], it is plausible that cardiac glycosides may have anti-cancer activity through downregulation of TGFβR2 in relevant cells. However, while multiple studies have demonstrated the anti-proliferative [24,59] and pro-apoptotic effects [60,61] of cardiac glycosides on various cancer cells in vitro, the effect of cardiac glycosides in the in vivo models of cancer has not been rigorously assessed.
On the other hand, our findings may also warn about potential adverse effects of cardiac glycosides (in addition to overall toxicity). TGF-β signaling is required for efficient wound healing [62,63]; hence, if cardiac glycosides attenuate the expression of TGFβR2 in vivo, one would predict that cardiac glycosides would be harmful during the external or internal injury. Further, it is now established that TGF-β regulates T cell function through driving differentiation of regulatory Treg cells and inhibition of T-helper cells [64,65]. Thus, inhibition of TGF-β signaling by cardiac glycosides may potentially lead to increased T cell responses and enhanced inflammation.
The caveat in addressing the discussed above potential benefits and limitations of cardiac glycosides is behind the fact that in rodents (which are largely used as animal models of disease in experimental research), α1 subunit of Na+/K+-ATPase is insensitive to therapeutic doses of cardiac glycosides [66]. Therefore, wild type rodents may not be used for assessing the therapeutic effect of cardiac glycosides in organs/cells expressing α1-Na+/K+-ATPase. The resistance to cardiac glycosides is caused by a substitution of Gln111 and Asn122 of human α1-subunit for Arg and Asp, respectively, in rodents. Based on this, Lingrel and co-workers have generated a mouse with knock-in of ouabain-sensitive α1 isoform of Na+/K+-ATPase and have used it to delineate the role of α1 in blood pressure regulation, cardiac and skeletal muscle contraction and renal salt handling [67].
Ethical Aspects of the Proposed Research
Human subjects
This study largely used primary cultures of human pulmonary fibroblasts (HPF) established from human lungs rejected for transplantation through the Regional Organ Bank of Illinois (ROBI) / Gift of Hope Network. No IRB protocol is required for using ROBI lungs from deceased individuals. The IPF-HLF were isolated and cultured from lungs of de-identified IPF patients shortly after lung transplantation at the University of Chicago under the IRB protocol #14514A.
Supporting Information
Serum starved HLF were treated with or without 1 ng / ml TGFβ1 and / or 30 nM ouabain for 24 hours. Cells were lysed and analyzed by Western blotting with desired antibodies.
(PPTX)
Acknowledgments
Research reported in this publication was supported by the National Institutes of Health Award 1R56HL127395 (N.O.D) and National Center For Advancing Translational Sciences of the National Institutes of Health under Award UL1TR000430 (N.O.D). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This study was also supported by American Heart Association Predoctoral Fellowship Award 14PRE18360017 (J.L.), the Russian Foundation for Fundamental Research (14-04-31705 and 15-04- 385 00101) and the Russian Scientific Foundation #14-15-0006. (O.A.A., S.N.O.).
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
Research reported in this publication was supported by the National Institutes of Health Award 1R56HL127395 (N.O.D.) and National Center For Advancing Translational Sciences of the National Institutes of Health under Award UL1TR000430 (N.O.D.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This study was also supported by American Heart Association Predoctoral Fellowship Award 14PRE18360017 (J.L.), the Russian Foundation for Fundamental Research (14-04-31705 and 15-04- 385 00101) and the Russian Scientific Foundation #14-15-0006. (O.A.A., S.N.O.).
References
- 1.Barnard JA, Beauchamp RD, Coffey RJ, Moses HL. Regulation of intestinal epithelial cell growth by transforming growth factor type beta. Proc Natl Acad Sci U S A. 1989. March;86(5):1578–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boyd FT, Massagué J. Transforming growth factor-beta inhibition of epithelial cell proliferation linked to the expression of a 53-kDa membrane receptor. J Biol Chem. 1989. February 5;264(4):2272–8. [PubMed] [Google Scholar]
- 3.Moses HL. TGF-beta regulation of epithelial cell proliferation. Mol Reprod Dev. 1992. June;32(2):179–84. 10.1002/mrd.1080320215 [DOI] [PubMed] [Google Scholar]
- 4.Mack CP. Signaling Mechanisms That Regulate Smooth Muscle Cell Differentiation. Arterioscler Thromb Vasc Biol. 2011. July;31(7):1495–505. 10.1161/ATVBAHA.110.221135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Desmoulière A, Geinoz A, Gabbiani F, Gabbiani G. Transforming growth factor-beta 1 induces alpha-smooth muscle actin expression in granulation tissue myofibroblasts and in quiescent and growing cultured fibroblasts. J Cell Biol. 1993. July;122(1):103–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kach J, Sandbo N, La J, Denner D, Reed EB, Akimova O, et al. Antifibrotic effects of noscapine through activation of prostaglandin E2 receptors and protein kinase A. J Biol Chem. 2014. March 14;289(11):7505–13. 10.1074/jbc.M113.546812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kach J, Sandbo N, Sethakorn N, Williams J, Reed EB, La J, et al. Regulation of myofibroblast differentiation and bleomycin-induced pulmonary fibrosis by adrenomedullin. Am J Physiol Lung Cell Mol Physiol. 2013. June 1;304(11):L757–764. 10.1152/ajplung.00262.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu J, Lamouille S, Derynck R. TGF-beta-induced epithelial to mesenchymal transition. Cell Res. 2009. February;19(2):156–72. 10.1038/cr.2009.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kasai H, Allen JT, Mason RM, Kamimura T, Zhang Z. TGF-β1 induces human alveolar epithelial to mesenchymal cell transition (EMT). Respir Res. 2005;6(1):56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Feng X-H, Derynck R. Specificity and versatility in tgf-beta signaling through Smads. Annu Rev Cell Dev Biol. 2005;21:659–93. 10.1146/annurev.cellbio.21.022404.142018 [DOI] [PubMed] [Google Scholar]
- 11.Chen Y-G. Endocytic regulation of TGF-beta signaling. Cell Res. 2009. January;19(1):58–70. 10.1038/cr.2008.315 [DOI] [PubMed] [Google Scholar]
- 12.Penheiter SG, Mitchell H, Garamszegi N, Edens M, Jules J. E. Doré J, Leof EB. Internalization-Dependent and -Independent Requirements for Transforming Growth Factor β Receptor Signaling via the Smad Pathway. Mol Cell Biol. 2002. July 1;22(13):4750–9. 10.1128/MCB.22.13.4750-4759.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Di Guglielmo GM, Le Roy C, Goodfellow AF, Wrana JL. Distinct endocytic pathways regulate TGF-beta receptor signalling and turnover. Nat Cell Biol. 2003. May;5(5):410–21. 10.1038/ncb975 [DOI] [PubMed] [Google Scholar]
- 14.Geering K, Theulaz I, Verrey F, Häuptle MT, Rossier BC. A role for the beta-subunit in the expression of functional Na+-K+-ATPase in Xenopus oocytes. Am J Physiol. 1989. November;257(5 Pt 1):C851–858. [DOI] [PubMed] [Google Scholar]
- 15.Ackermann U, Geering K. Mutual dependence of Na,K-ATPase alpha- and beta-subunits for correct posttranslational processing and intracellular transport. FEBS Lett. 1990. August 20;269(1):105–8. [DOI] [PubMed] [Google Scholar]
- 16.Geering K, Beggah A, Good P, Girardet S, Roy S, Schaer D, et al. Oligomerization and maturation of Na,K-ATPase: functional interaction of the cytoplasmic NH2 terminus of the beta subunit with the alpha subunit. J Cell Biol. 1996. June;133(6):1193–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Geering K. The functional role of beta subunits in oligomeric P-type ATPases. J Bioenerg Biomembr. 2001. October;33(5):425–38. [DOI] [PubMed] [Google Scholar]
- 18.Solomon AK, Gill TJ, Gold GL. THE KINETICS OF CARDIAC GLYCOSIDE INHIBITION OF POTASSIUM TRANSPORT IN HUMAN ERYTHROCYTES. J Gen Physiol. 1956. November 20;40(2):327–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Orosz F, Nuridsány M, Ovádi J. Isolation and quantitative determination of some cardioactive glycosides from Digitalis lanata by high-performance liquid chromatography. Anal Biochem. 1986. July;156(1):171–5. [DOI] [PubMed] [Google Scholar]
- 20.Rahimtoola SH, Tak T. The use of digitalis in heart failure. Curr Probl Cardiol. 1996. December 1;21(12):781–853. [DOI] [PubMed] [Google Scholar]
- 21.Pubchem. ouabain | C29H44O12—PubChem [Internet]. 2016 [cited 2016 Jun 25]. Available from: https://pubchem.ncbi.nlm.nih.gov/compound/ouabain#section=Protein-Binding
- 22.Blaustein MP, Lederer WJ. Sodium/calcium exchange: its physiological implications. Physiol Rev. 1999. July;79(3):763–854. [DOI] [PubMed] [Google Scholar]
- 23.Abramowitz J, Dai C, Hirschi KK, Dmitrieva RI, Doris PA, Liu L, et al. Ouabain- and marinobufagenin-induced proliferation of human umbilical vein smooth muscle cells and a rat vascular smooth muscle cell line, A7r5. Circulation. 2003. December 16;108(24):3048–53. 10.1161/01.CIR.0000101919.00548.86 [DOI] [PubMed] [Google Scholar]
- 24.Kometiani P, Liu L, Askari A. Digitalis-Induced Signaling by Na+/K+-ATPase in Human Breast Cancer Cells. Mol Pharmacol. 2005. March 1;67(3):929–36. 10.1124/mol.104.007302 [DOI] [PubMed] [Google Scholar]
- 25.Tian J, Cai T, Yuan Z, Wang H, Liu L, Haas M, et al. Binding of Src to Na+/K+-ATPase Forms a Functional Signaling Complex. Mol Biol Cell. 2006. January;17(1):317–26. 10.1091/mbc.E05-08-0735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu L, Zhao X, Pierre SV, Askari A. Association of PI3K-Akt signaling pathway with digitalis-induced hypertrophy of cardiac myocytes. Am J Physiol—Cell Physiol. 2007. November 1;293(5):C1489–97. 10.1152/ajpcell.00158.2007 [DOI] [PubMed] [Google Scholar]
- 27.Ye Q, Li Z, Tian J, Xie JX, Liu L, Xie Z. Identification of a potential receptor that couples ion transport to protein kinase activity. J Biol Chem. 2011. February 25;286(8):6225–32. 10.1074/jbc.M110.202051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li Z, Cai T, Tian J, Xie JX, Zhao X, Liu L, et al. NaKtide, a Na/K-ATPase-derived peptide Src inhibitor, antagonizes ouabain-activated signal transduction in cultured cells. J Biol Chem. 2009. July 31;284(31):21066–76. 10.1074/jbc.M109.013821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wu J, Akkuratov EE, Bai Y, Gaskill CM, Askari A, Liu L. Cell Signaling Associated with Na+/K+-ATPase: Activation of Phosphatidylinositide 3-Kinase IA/Akt by Ouabain Is Independent of Src. Biochemistry (Mosc). 2013. December 17;52(50):9059–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu L, Mohammadi K, Aynafshar B, Wang H, Li D, Liu J, et al. Role of caveolae in signal-transducing function of cardiac Na+/K+-ATPase. Am J Physiol Cell Physiol. 2003. June;284(6):C1550–1560. 10.1152/ajpcell.00555.2002 [DOI] [PubMed] [Google Scholar]
- 31.Liu L, Abramowitz J, Askari A, Allen JC. Role of caveolae in ouabain-induced proliferation of cultured vascular smooth muscle cells of the synthetic phenotype. Am J Physiol Heart Circ Physiol. 2004. November;287(5):H2173–2182. 10.1152/ajpheart.00352.2004 [DOI] [PubMed] [Google Scholar]
- 32.Liang M, Tian J, Liu L, Pierre S, Liu J, Shapiro J, et al. Identification of a pool of non-pumping Na/K-ATPase. J Biol Chem. 2007. April 6;282(14):10585–93. 10.1074/jbc.M609181200 [DOI] [PubMed] [Google Scholar]
- 33.Quintas LEM, Pierre SV, Liu L, Bai Y, Liu X, Xie Z-J. Alterations of Na+/K+-ATPase function in caveolin-1 knockout cardiac fibroblasts. J Mol Cell Cardiol. 2010. September;49(3):525–31. 10.1016/j.yjmcc.2010.04.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bai Y, Wu J, Li D, Morgan EE, Liu J, Zhao X, et al. Differential roles of caveolin-1 in ouabain-induced Na+/K+-ATPase cardiac signaling and contractility. Physiol Genomics. 2016. August 12;physiolgenomics.00042.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brown RD, Ambler SK, Mitchell MD, Long CS. THE CARDIAC FIBROBLAST: Therapeutic Target in Myocardial Remodeling and Failure. Annu Rev Pharmacol Toxicol. 2005;45(1):657–87. [DOI] [PubMed] [Google Scholar]
- 36.Fan D, Takawale A, Lee J, Kassiri Z. Cardiac fibroblasts, fibrosis and extracellular matrix remodeling in heart disease. Fibrogenesis Tissue Repair. 2012. September 3;5:15 10.1186/1755-1536-5-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cucoranu I, Clempus R, Dikalova A, Phelan PJ, Ariyan S, Dikalov S, et al. NAD(P)H Oxidase 4 Mediates Transforming Growth Factor-β1–Induced Differentiation of Cardiac Fibroblasts Into Myofibroblasts. Circ Res. 2005. October 28;97(9):900–7. 10.1161/01.RES.0000187457.24338.3D [DOI] [PubMed] [Google Scholar]
- 38.Phan SH. The myofibroblast in pulmonary fibrosis. Chest. 2002. December;122(6 Suppl):286S–289S. [DOI] [PubMed] [Google Scholar]
- 39.Hinz B, Phan SH, Thannickal VJ, Galli A, Bochaton-Piallat M- L, Gabbiani G. The myofibroblast: one function, multiple origins. Am J Pathol. 2007. June;170(6):1807–16. 10.2353/ajpath.2007.070112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sandbo N, Lau A, Kach J, Ngam C, Yau D, Dulin NO. Delayed stress fiber formation mediates pulmonary myofibroblast differentiation in response to TGF-β. Am J Physiol Lung Cell Mol Physiol. 2011. November;301(5):L656–666. 10.1152/ajplung.00166.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sandbo N, Kregel S, Taurin S, Bhorade S, Dulin NO. Critical role of serum response factor in pulmonary myofibroblast differentiation induced by TGF-beta. Am J Respir Cell Mol Biol. 2009. September;41(3):332–8. 10.1165/rcmb.2008-0288OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Strutz F, Zeisberg M. Renal Fibroblasts and Myofibroblasts in Chronic Kidney Disease. J Am Soc Nephrol. 2006. November 1;17(11):2992–8. 10.1681/ASN.2006050420 [DOI] [PubMed] [Google Scholar]
- 43.Meran S, Steadman R. Fibroblasts and myofibroblasts in renal fibrosis. Int J Exp Pathol. 2011. June;92(3):158–67. 10.1111/j.1365-2613.2011.00764.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Iwano M, Plieth D, Danoff TM, Xue C, Okada H, Neilson EG. Evidence that fibroblasts derive from epithelium during tissue fibrosis. J Clin Invest. 2002. August;110(3):341–50. 10.1172/JCI15518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Varga J, Abraham D. Systemic sclerosis: a prototypic multisystem fibrotic disorder. J Clin Invest. 2007. March 1;117(3):557–67. 10.1172/JCI31139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wynn TA. Common and unique mechanisms regulate fibrosis in various fibroproliferative diseases. J Clin Invest. 2007. March 1;117(3):524–9. 10.1172/JCI31487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lee S-J, Kim K-H, Park K-K. Mechanisms of fibrogenesis in liver cirrhosis: The molecular aspects of epithelial-mesenchymal transition. World J Hepatol. 2014. April 27;6(4):207–16. 10.4254/wjh.v6.i4.207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schuppan D, Afdhal NH. Liver cirrhosis. The Lancet. 2008. March 14;371(9615):838–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pohlers D, Brenmoehl J, Löffler I, Müller CK, Leipner C, Schultze-Mosgau S, et al. TGF-β and fibrosis in different organs—molecular pathway imprints. Biochim Biophys Acta BBA—Mol Basis Dis. 2009. August;1792(8):746–56. [DOI] [PubMed] [Google Scholar]
- 50.Biernacka A, Dobaczewski M, Frangogiannis NG. TGF-β signaling in fibrosis. Growth Factors Chur Switz. 2011. October;29(5):196–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Slingerland M, Cerella C, Guchelaar HJ, Diederich M, Gelderblom H. Cardiac glycosides in cancer therapy: from preclinical investigations towards clinical trials. Invest New Drugs. 2013. August;31(4):1087–94. 10.1007/s10637-013-9984-1 [DOI] [PubMed] [Google Scholar]
- 52.Menger L, Vacchelli E, Kepp O, Eggermont A, Tartour E, Zitvogel L, et al. Trial watch: Cardiac glycosides and cancer therapy. Oncoimmunology. 2013. February 1;2(2):e23082 10.4161/onci.23082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Stenkvist B, Bengtsson E, Eriksson O, Holmquist J, Nordin B, Westman-Naeser S. Cardiac glycosides and breast cancer. Lancet Lond Engl. 1979. March 10;1(8115):563. [DOI] [PubMed] [Google Scholar]
- 54.Stenkvist B, Bengtsson E, Dahlqvist B, Eriksson O, Jarkrans T, Nordin B. Cardiac glycosides and breast cancer, revisited. N Engl J Med. 1982. February 25;306(8):484. [PubMed] [Google Scholar]
- 55.Stenkvist B. Is digitalis a therapy for breast carcinoma? Oncol Rep. 1999. June;6(3):493–6. [PubMed] [Google Scholar]
- 56.Pickup M, Novitskiy S, Moses HL. The roles of TGFβ in the tumour microenvironment. Nat Rev Cancer. 2013. November;13(11):788–99. 10.1038/nrc3603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Padua D, Massagué J. Roles of TGFbeta in metastasis. Cell Res. 2009. January;19(1):89–102. 10.1038/cr.2008.316 [DOI] [PubMed] [Google Scholar]
- 58.Jakowlew SB. Transforming growth factor-beta in cancer and metastasis. Cancer Metastasis Rev. 2006. September;25(3):435–57. 10.1007/s10555-006-9006-2 [DOI] [PubMed] [Google Scholar]
- 59.Lin S-Y, Chang H-H, Lai Y-H, Lin C-H, Chen M-H, Chang G-C, et al. Digoxin Suppresses Tumor Malignancy through Inhibiting Multiple Src-Related Signaling Pathways in Non-Small Cell Lung Cancer. PloS One. 2015;10(5):e0123305 10.1371/journal.pone.0123305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Frese S, Frese-Schaper M, Andres A-C, Miescher D, Zumkehr B, Schmid RA. Cardiac Glycosides Initiate Apo2L/TRAIL-Induced Apoptosis in Non–Small Cell Lung Cancer Cells by Up-regulation of Death Receptors 4 and 5. Cancer Res. 2006. June 1;66(11):5867–74. 10.1158/0008-5472.CAN-05-3544 [DOI] [PubMed] [Google Scholar]
- 61.Cardiac Glycosides Stimulate Ca2+ Increases and Apoptosis in Androgen-independent, Metastatic Human Prostate Adenocarcinoma Cells | Cancer Research [Internet]. [cited 2016 Aug 5]. Available from: http://cancerres.aacrjournals.org/content/60/14/3807.short [PubMed]
- 62.Mustoe TA, Pierce GF, Thomason A, Gramates P, Sporn MB, Deuel TF. Accelerated healing of incisional wounds in rats induced by transforming growth factor-beta. Science. 1987. September 11;237(4820):1333–6. [DOI] [PubMed] [Google Scholar]
- 63.Montesano R, Orci L. Transforming growth factor beta stimulates collagen-matrix contraction by fibroblasts: implications for wound healing. Proc Natl Acad Sci. 1988. July 1;85(13):4894–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bridoux F, Badou A, Saoudi A, Bernard I, Druet E, Pasquier R, et al. Transforming growth factor beta (TGF-beta)-dependent inhibition of T helper cell 2 (Th2)-induced autoimmunity by self-major histocompatibility complex (MHC) class II-specific, regulatory CD4(+) T cell lines. J Exp Med. 1997. May 19;185(10):1769–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Li MO, Flavell RA. TGF-beta: a master of all T cell trades. Cell. 2008. August 8;134(3):392–404. 10.1016/j.cell.2008.07.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Schoner W, Scheiner-Bobis G. Endogenous and exogenous cardiac glycosides: their roles in hypertension, salt metabolism, and cell growth. Am J Physiol Cell Physiol. 2007. August;293(2):C509–536. 10.1152/ajpcell.00098.2007 [DOI] [PubMed] [Google Scholar]
- 67.Lingrel JB. The physiological significance of the cardiotonic steroid/ouabain-binding site of the Na,K-ATPase. Annu Rev Physiol. 2010;72:395–412. 10.1146/annurev-physiol-021909-135725 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Serum starved HLF were treated with or without 1 ng / ml TGFβ1 and / or 30 nM ouabain for 24 hours. Cells were lysed and analyzed by Western blotting with desired antibodies.
(PPTX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.