Abstract
Objective
To estimate the global and national burden of emergency conditions, and compare them to emergency care utilization rates.
Methods
We coded all 291 Global Burden of Disease 2010 conditions into three categories to estimate emergency burden: conditions that, if not addressed within hours to days of onset, commonly lead to serious disability or death; conditions with common acute decompensations that lead to serious disability or death; and non-emergencies. Emergency care utilization rates were obtained from a systematic literature review on emergency care facilities in low- and middle-income countries (LMICs), supplemented by national health system reports.
Findings
All 15 leading causes of death and DALYs globally were conditions with potential emergent manifestations. We identified 41 facility-based reports in 23 countries, 12 of which were in LMICs; data for 17 additional countries were obtained from national or regional reports on emergency utilization. Burden of emergency conditions was the highest in low-income countries, with median DALYs of 47,728 per 100,000 population (IQR 45,253-50,085) in low-income, 25,186 (IQR 21,982-40,480) in middle-income, and 15,691 (IQR 14,649-16,382) in high-income countries. Patterns were similar using deaths to measure burden and excluding acute decompensations from the definition of emergency conditions. Conversely, emergency utilization rates were the lowest in low-income countries, with median 8 visits per 1,000 population (IQR 6-10), 78 (IQR 25-197) in middle-income, and 264 (IQR 177-341) in high-income countries.
Conclusion
Despite higher burden of emergency conditions, emergency utilization rates are substantially lower in LMICs, likely due to limited access to emergency care.
Keywords: global health, emergency department utilisation, emergency care systems, access to care
Introduction
Emergency conditions are thought to make up a large part of the global burden of disease, [1–3] and high-quality emergency care has the potential to address and prevent a substantial portion of death and disability around the world. [4–6] There is increasing recognition that emergency care delivery is an essential part of health systems, [7–9] and this has been reflected in the dramatic rise in emergency department (ED) patient volumes over the last few decades in many parts of the world.[10] However, outside of a handful of high-income countries (HICs) with well-established emergency care systems, there is a dearth of information about the burden of emergency conditions, or how frequently patients seek emergency care.[2, 9, 11]
The unpredictable and time-sensitive nature of emergencies means that it is often more difficult to capture data on emergency care than care delivered in other settings. These constraints are particularly heightened in low- and middle- income countries (LMICs).[9, 11] Even where data are collected, systematic analysis is difficult because emergency care is frequently delivered across a variety of settings, including clinics and outpatient departments,[2, 7, 12] and formal EDs may not exist, even in some HICs.[12] This lack of basic information about emergency care delivery and the burden of emergency conditions has stalled attempts to understand and improve emergency care, particularly in LMICs.[11
A better understanding of the burden of emergency conditions and how it compares to emergency care utilization could allow for more effective policy making, resource allocation, and health system planning.[1, 2, 4, 13] Here we perform a descriptive analysis to characterize the global and national burden of emergency conditions, synthesize existing information on the current status of emergency care utilization around the world, and highlight the potential role of emergency care delivery in alleviating global morbidity and mortality.
Methods
Burden of emergency conditions
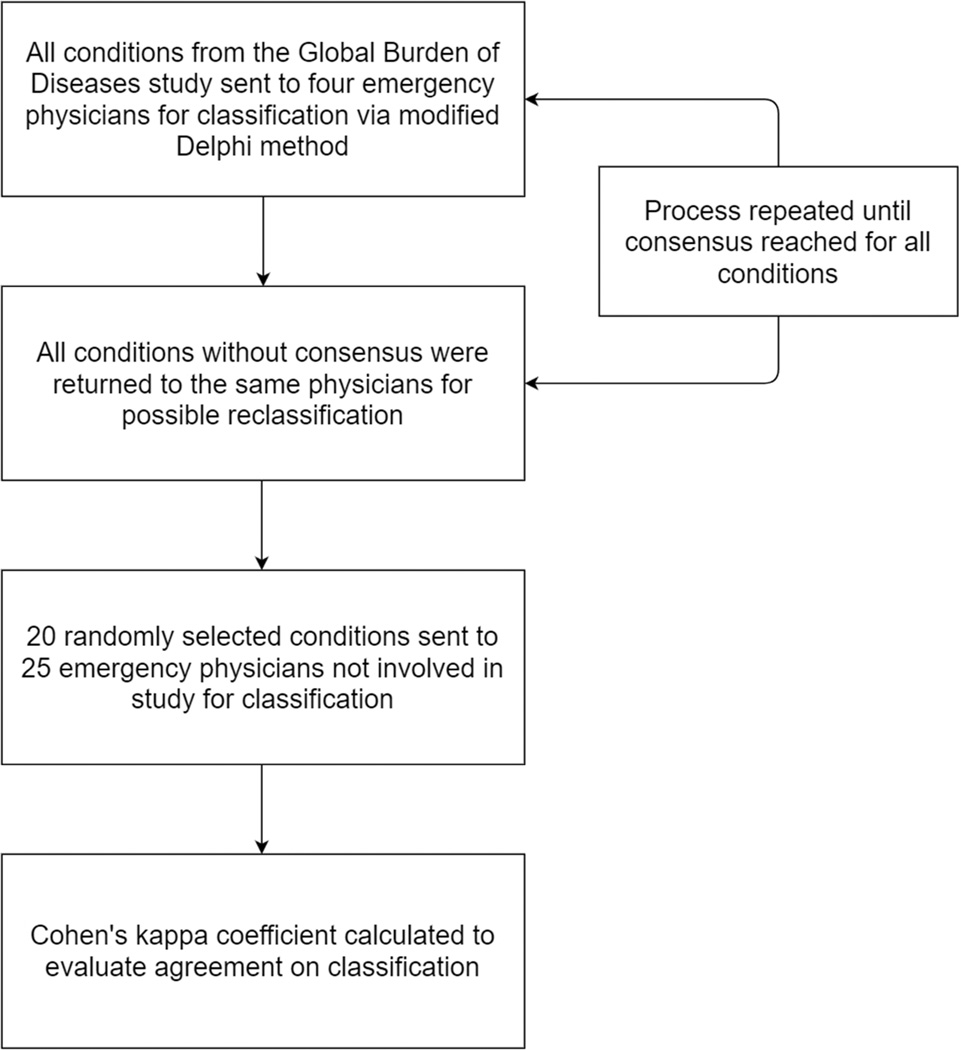
To determine the burden of emergency conditions, we used data from the 2010 Global Burden of Disease (GBD) study.[14] Building on legal definitions of emergency care, we defined emergency conditions as ones that, if not diagnosed and treated within hours to days of onset, often lead to serious physical or mental disability or death.[15, 16] We then used modified Delphi process to classify each of the 291 conditions catalogued in the GBD study into three disease categories: 1) conditions that, if not diagnosed and treated within hours to days of onset, commonly lead to serious physical or mental disability or death (e.g., lower respiratory infections, trauma), 2) conditions with trajectories that can involve acute decompensation, that lead many patients to experience serious physical or mental disability or death (e.g., diabetes mellitus, HIV/AIDS), and 3) non-emergency conditions (e.g., osteoarthritis, dementia).[2] Four physician researchers first independently classified each condition into one of the three categories. Conditions without consensus were then highlighted and sent back to the same physicians for possible reclassification. This process was repeated until all differences were reconciled. In order to externally validate the classification, a randomly selected list of 20 conditions was given to 25 additional emergency physicians from various regions and income groups who were not involved in the study. Cohen’s kappa coefficient was calculated to assess each rater’s agreement with the classification resulting from the modified Delphi process (Figure 1).[17, 18] A full list of the disease classification is found in the online supplement. The first two categories were defined as “emergency conditions,” and these conditions were further classified as communicable or non-communicable conditions. We calculated the global burden of emergency conditions by summing data on global rates of deaths and disability-adjusted life-years (DALYs) for each condition. Age-standardized death and DALY rates reported by the GBD study were used to allow for comparisons of populations with different age profiles. We performed similar calculations to determine the burden of emergency conditions at the national level for the 187 countries with available GBD data. Death and DALY rates were assumed to be zero for 10 region-specific conditions (e.g., Chagas, yellow fever) when no data were available.
Figure 1.
Flowchart of the modified Delphi classification and external validation processes
Rates of emergency utilization
To estimate rates of emergency utilization in LMICs, we extracted data from a systematic literature review that recorded data on patient volumes and catchment populations of individual emergency care facilities in 139 countries classified by the World Bank as low- and middle-income.[20, 21] Emergency utilization rate was defined as number of visits per 1,000 population to facilities providing emergency care. We selected reports that documented both facility volume and catchment population, and specified that it was the only facility serving the catchment area, and used the data to calculate single-facility emergency utilization rates. Since the existing systematic review only identified facilities in LMICs, we applied similar methods to the 75 World Bank high-income countries to obtain additional emergency utilization rates. Literature searches were started on 8/12/2013 and concluded on 7/18/2014. Additional details of the literature review are described elsewhere.[21]
We further supplemented single-facility emergency utilization rates with national emergency utilization rates reported in nation-wide surveys of emergency facilities and official statistics from national health systems where available. The first 100 results from a search using the terms [country name] + emergency department on Google and Google Scholar for all countries were screened for relevant information. We restricted the search to reports published after 1990 but did not restrict by language, provided the resource was searchable with English search terms. Some reports directly provided national emergency utilization rates, while others provided only data on the number of emergency visits. For the latter, we obtained the national population for the year when data collection was completed from the United Nations Statistics Division.[19] Where national data were unavailable, we used data from large sub-regions. For countries with multiple reports, overall national emergency utilization rates were averaged using inverse-variance weighting.
Analysis: comparison of burden of emergency conditions to emergency utilization rates
We compared national burden of emergency condition to national emergency utilization rates via two-way plots. As a sensitivity analysis, three different definitions of emergency conditions were explored for each country using age-standardized death and DALY rates. The first estimate included death and DALY rates from only conditions that commonly lead to serious disability or death if not treated within hours to days of onset, the second included only conditions commonly associated with acute decompensations that lead to serious disability or death, and the third included conditions in both of the two aforementioned categories. Countries that did not have GBD data were excluded from the study.[14]
Results
Consensus on classification of all 291 GBD conditions was reached after four rounds of discussions and reclassifications among the four physician researchers via the modified Delphi process. At the end of the process, agreement was unanimous on all conditions. Median kappa statistic for 20 randomly selected conditions was 0.70 (IQR 0.63-0.84), or “substantial agreement” as usually defined, when classified by 25 external emergency physicians from 12 countries, who were not involved in the study (9 physicians from low-income countries (LICs), 3 from middle-income countries (MICs), and 13 from HICs).[22
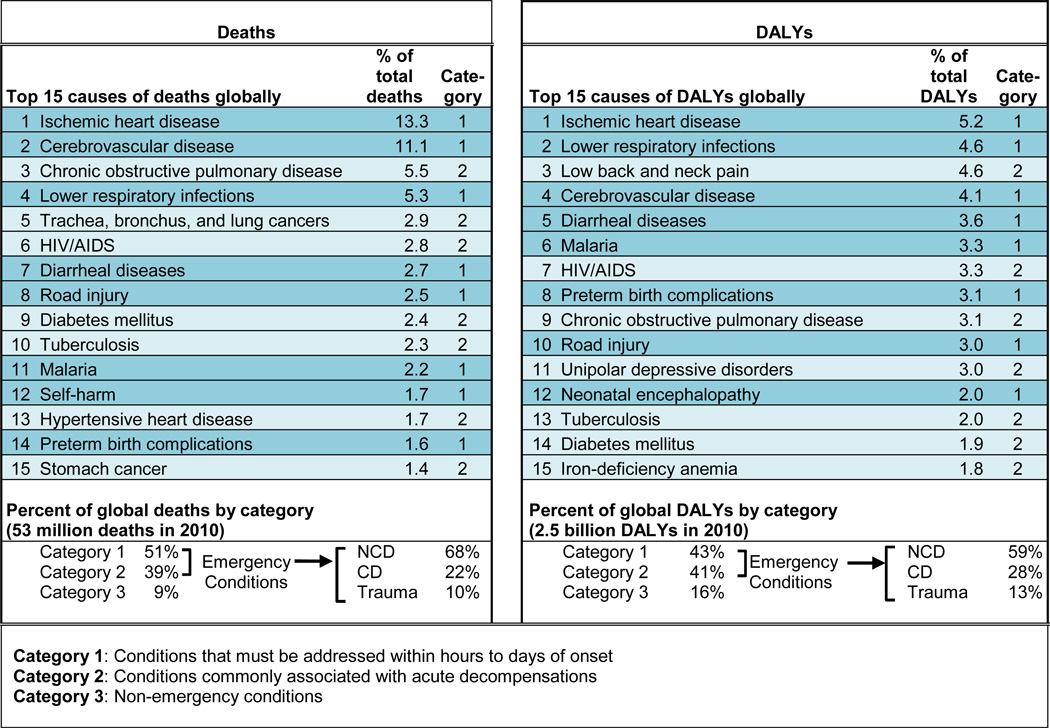
Table 1 lists the leading global causes of death and DALYs. Ischemic heart disease, cerebrovascular diseases, and lower respiratory infections were the top global causes that commonly lead to serious disability or death if not treated within hours to days of onset. Chronic obstructive pulmonary disease, low back and neck pain, and HIV/AIDS were examples of conditions commonly associated with acute decompensations that lead to serious disability or death. All 15 leading global causes of death and DALYs were conditions with potential emergent manifestations. 90% of deaths and 84% of DALYs around the world were due to emergency conditions, driven in nearly equal part by conditions that must be addressed within hours to days of onset and conditions with common acute decompensations. Of the DALYs attributable to emergency conditions globally, 59% was caused by non-communicable diseases (NCDs), with communicable diseases (CDs) and trauma representing 28% and 13%. The breakdown of the burden attributable to each of the disease categories is summarized in Table 1.
Table 1.
Global leading causes of deaths and disability-adjusted life years (DALYs) and distribution of deaths and DALYs
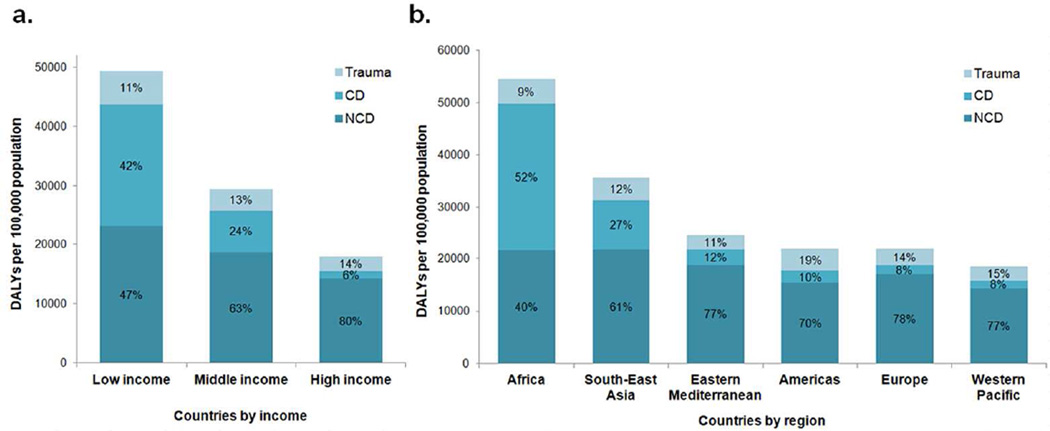
The amount of emergency conditions and the proportions of NCDs and CDs amongst emergency conditions varied considerably by income level and region. By income level, LICs had the highest burden of emergency conditions, with nearly triple the burden of emergency conditions in HICs (Figure 2a). The proportion of emergency condition deaths and DALYs from NCDs and CDs were nearly equal in LICs, where as in HICs, NCDs made up 83% of deaths and 80% of DALYs, with CDs representing only 7% and 6% of deaths and DALYs from emergency conditions (Figure 2a). By WHO regions, Africa and South-East Asia had the highest burden of emergency conditions (Figure 2b), with over 3 times the burden of lowest burden regions. Except Africa and South-East Asia that had markedly higher proportions of CDs, rates of emergency condition deaths and DALYs from NCDs and traumas were roughly the same across all other regions (Figure 2b).
Figure 2.
DALYs per 100,000 population attributable to emergency conditions, by etiology: separated by income level (a) and region (b). Distribution of deaths was similar. Abbreviations: non-communicable diseases (NCDs), communicable-diseases (CDs), disability-adjusted life years (DALYs).
Table 2 summarizes the sources of emergency utilization data identified for this study. We identified 78 reports in 40 countries that provided data on emergency utilization rates. Systematic literature review yielded 28 reports from 12 LMICs that included patient volume and catchment population of emergency facilities; a similar search identified 20 single-facility reports from HICs. Thirty additional national and regional reports provided emergency utilization data on 18 HICs; only 6 LMICs had national or regional data. Four World Bank high-income economies (Andorra, Bermuda, Curaçao, and Hong Kong) were excluded due to lack of corresponding GBD data.[14
Table 2.
Summary of the emergency utilization data sources, national emergency utilization rates, and rates of deaths and disability-adjusted life years (DALYs) from emergency conditions
| Country | Reports | Publication year |
National emergency utilization rates per 1,000 |
Death from emergency conditions per 100,000 |
DALYs from emergency conditions per 100,000 |
|---|---|---|---|---|---|
| Low and middle income (15) | 28 | 1999–2014 | |||
| Brazil | □□□ | 2005–2011 | 232 | 601 | 23,872 |
| Cameroon | □ | 2011–2011 | 4 | 1,167 | 55,066 |
| China | ◘□ | 2012–2012 | 123 | 562 | 18,876 |
| Ethiopia | □ | 2014–2014 | 8 | 1,154 | 47,728 |
| Kenya | □□ | 2007–2011 | 3 | 933 | 42,779 |
| Mexico | □ | 1999–1999 | 18 | 542 | 20,149 |
| Morocco | ■ | 2003–2003 | 101 | 615 | 26,501 |
| Nigeria | ◘□□□□ | 2002–2013 | 0.7 | 1,076 | 56,202 |
| Romania | □ | 2009–2009 | 27 | 668 | 22,862 |
| South Africa | □□□ | 2008–2010 | 53 | 1,168 | 55,358 |
| St. Vincent and the Grenadines | ■■ | 2003–2014 | 254 | 663 | 27,228 |
| Sudan | □ | 2014–2014 | 55 | 705 | 35,618 |
| Tunisia | ■ | 2001–2001 | 250 | 495 | 20,191 |
| Turkey | ◘□ | 2003–2014 | 185 | 573 | 22,579 |
| Uganda | □□ | 2012–2012 | 11 | 1,191 | 52,441 |
| High income (25) | 50 | 2001–2014 | |||
| Australia | ■ | 2013–2013 | 291 | 330 | 14,308 |
| Brunei | □□ | 2011–2013 | 331 | 531 | 17,889 |
| Canada | ■◘◘ | 2001–2011 | 341 | 360 | 15,156 |
| Denmark | ■■ | 2011–2012 | 185 | 445 | 17,141 |
| Finland | ■ | 2011–2011 | 194 | 369 | 16,382 |
| Germany | ■□ | 2011–2014 | 143 | 384 | 15,624 |
| Greece | □ | 2004–2004 | 406 | 419 | 15,691 |
| Iceland | □□ | 2012–2012 | 177 | 311 | 13,767 |
| Ireland | ■ | 2009–2009 | 264 | 398 | 15,836 |
| Israel | ■□ | 2012–2012 | 371 | 354 | 14,590 |
| Italy | ■ | 2011–2011 | 498 | 344 | 14,395 |
| Kuwait | □ | 2008–2008 | 286 | 470 | 19,315 |
| Netherlands | ■■ | 2011–2012 | 127 | 357 | 15,351 |
| New Zealand | ■ | 2010–2010 | 229 | 353 | 15,408 |
| Norway | □ | 2013–2013 | 78 | 367 | 16,301 |
| Saudi Arabia | ■ | 2011–2011 | 591 | 495 | 20,427 |
| Singapore | ■ | 2012–2012 | 182 | 404 | 14,784 |
| Slovenia | ■ | 2012–2012 | 207 | 422 | 16,374 |
| Spain | ■■◘□□□ | 2008–2013 | 543 | 328 | 13,818 |
| Sweden | □□□□ | 2013–2013 | 105 | 349 | 14,649 |
| Switzerland | ■□□□ | 2002–2014 | 81 | 325 | 13,990 |
| Taiwan | ■ | 2014–2014 | 294 | 441 | 16,346 |
| Trinidad and Tobago | □ | 2004–2004 | 174 | 802 | 28,961 |
| United Kingdom | ■■■ | 2011–2013 | 315 | 389 | 15,974 |
| United States | ■■■■■ | 2001–2011 | 407 | 438 | 17,166 |
| Total 40 | 78 | 1999–2014 |
Each diamond represents a single report; data from national health system report or survey (■); city or regional report or survey (◘); single facility data (□).
Across the 40 countries with data on emergency utilization, median death rates from emergency conditions were 1,154 (IQR 1043-1172), 639 (IQR 570-798), and 384 (IQR 353-438) per 100,000 population for low-, middle-, and high-income countries, respectively. Median DALYs attributable to emergency conditions were 47,728 (IQR 45,253-50,085), 25,186 (IQR 21,982-40,408), and 15,691 (IQR 14,649-16,382) per 100,000 population for low-, middle-, and high-income countries, respectively.
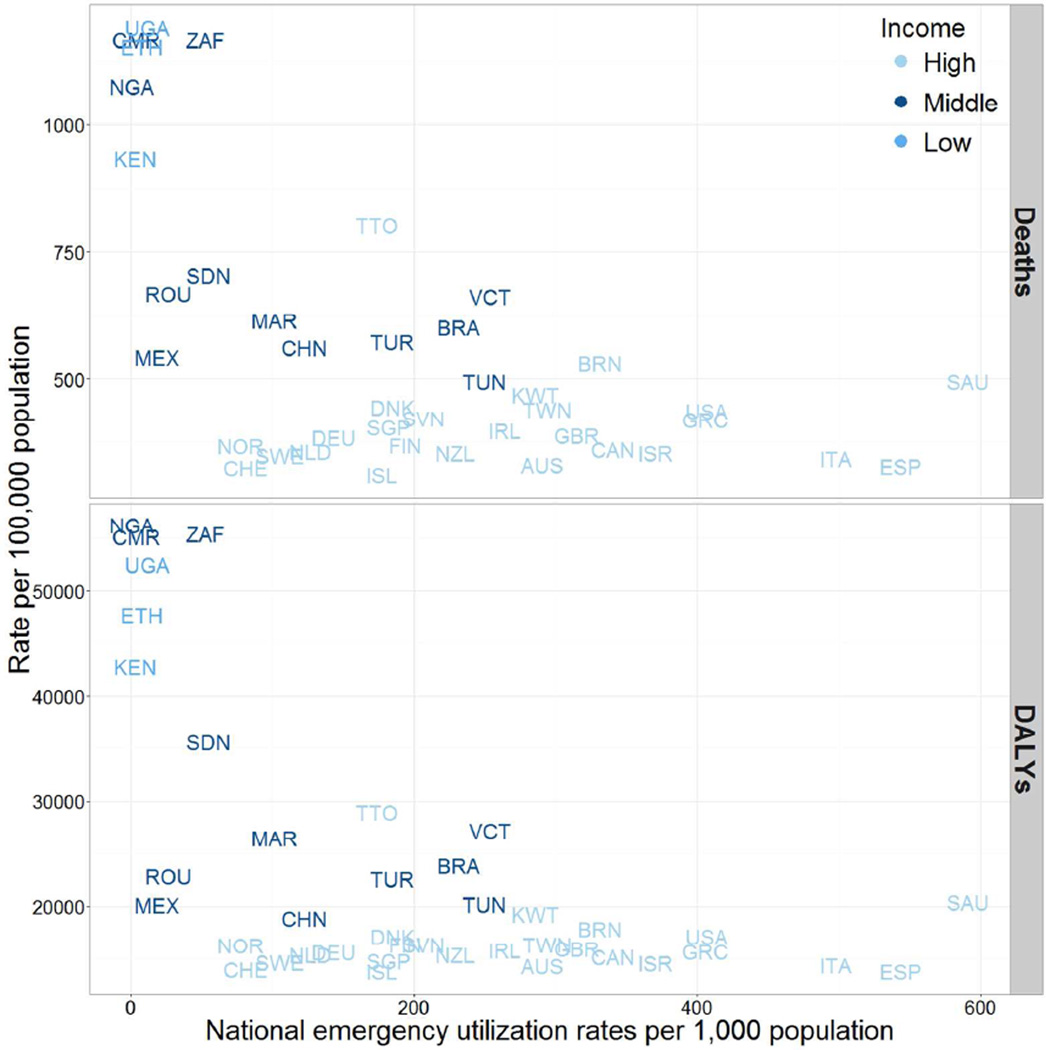
Emergency utilization rates spanned a wide range across the world, from the highest rate in Saudi Arabia, a HIC (591 visits per 1,000 population), to the lowest rate in Nigeria, a MIC (0.7 visits per 1,000 population). The median emergency utilization rate of HICs was 33-fold greater than that of LICs and over 3-fold greater than that of MICs. Median emergency utilization rates for the 40 countries were 8 (IQR 6- 10), 78 (IQR 25-197), and 264 (IQR 177-341) per 1,000 population for low-, middle-, and high-income countries, respectively. Compared to HICs (lowest in Norway at 78 to highest in Saudi Arabia at 591) and MICs (lowest in Nigeria at 0.7 to highest in St. Vincent and Grenadines at 254), there was less variation in emergency utilization rates in LICs, where the rates were consistently low (lowest in Kenya at 3 to highest in Uganda at 11).
Figure 3 compares national emergency utilization rates to deaths and DALYs from emergency conditions. Emergency utilization rates were the lowest in LMICs, which had the highest burden of emergency conditions. These observations were true whether deaths or DALYs were used to measure burden, and whether conditions commonly associated with acute decompensations were included in the calculations (Figure 3).
Figure 3.
Comparison of national emergency utilization rates with burden of emergency conditions, as measured by deaths and DALYs per 100,000 population.
Discussion
To our knowledge, this is the first report to systematically compare the burden of emergency conditions to the frequency of emergency care utilization around the world. It is also the first to characterize the breakdown of the types of emergency conditions in various income groups or geographic regions. Our classification of GBD conditions as emergency or non-emergency resulted in “substantial” agreement among emergency physicians from various income groups and geographic regions.[22] This represents an early step towards reaching a consensus on the classification of emergency conditions. We found that the rates of deaths and DALYs from emergency conditions were markedly higher in LMICs compared to HICs, driven in equal proportion by NCDs as CDs. This finding is consistent with limited data from prior reports on the importance of emergency care in LMICs: for example, a WHO report shows that all 10 leading causes of death in LMICs are emergency conditions, with majority being conditions that could lead to serious disability or death if not addressed in hours to days of onset, whereas the 10 leading causes in HICs include more non-emergencies and chronic conditions with common acute decompensations (e.g., Alzheimer's, cancers).[23] Our estimation that 90% of global causes of death and 84% of global causes of DALYs are amenable to emergency care was higher than previous estimates from over a decade ago.[23, 24] This hints at the growing burden of emergency conditions and the potential role for emergency care in reducing the global burden of disease.
This study also highlights the paucity of data on emergency service utilization around the world, particularly in LMICs. While we were able to obtain several official reports of national emergency utilization rates, there was limited country-level data, even in HICs with well-developed emergency care systems. Despite a prior systematic review and extensive literature search, we were only able to identify 78 reports in 40 countries—representing a third of HICs and less than 10% of LMICs—that provided insight into how frequently patients seek emergency care. Nonetheless, given how little we currently know, this dataset offers an initial window into how emergency care is utilized around the world.
Where we did locate data, we identified several characteristics and associations. The most striking of which is that while emergency utilization rates varied considerably amongst HICs with similar burden of emergency conditions, LMICs consistently had substantially lower rates of emergency utilization, despite higher burden of diseases. The large variation within income groups may be due to the known heterogeneity in models of emergency care delivery or in the maturity of emergency care systems around the world.[12] The lower rates of utilization in LMICs are likely driven by the lack of access to emergency facilities and limited availability of emergency care. Notably, MICs with lower burden of emergency conditions demonstrated emergency utilization rates similar to those of HICs, but middle-countries with the highest burden of emergency conditions conversely had emergency utilization rates that were comparable to or lower than those of LICs. This finding suggests that how frequently patients access emergency care is likely more strongly associated with a country's burden of diseases than its gross national income.
Limitations
The primary limitation of this study was the widespread lack of reliable data on emergency utilization, not only in LMICs, where emergency care is often delivered outside of formal EDs, but also in HICs. Even in HICs with well-developed emergency care systems, data on emergency care utilization were sparse. This may be due to the fact that emergency medicine is a recent or nonexistent medical specialty in some HICs, or that EDs play a limited role in health care delivery: some emergency care systems emphasize pre-hospital care and alternative ways of accessing emergency diagnosis and intervention.[12] Lack of data may have biased our results in two ways. First, in LMICs, we often relied on single-facility reports to estimate national emergency utilization rates since these were often the only data available. If these data were biased upward or downward—either of which would be plausible—it would have affected our assessment of the relationship between emergency conditions and utilization across income levels. Single facility estimates also presume static demographic trends. Second, many of these facilities in LMICs were large and urban, with very few data on the rural facilities that may deliver a large proportion of emergency care in LMICs. This would have biased our estimates of emergency utilization rates in LMICs downward.
Another limitation relates to the search strategy used to identify single-facility reports. Although we employed a methodical search strategy on Google and Google Scholar using the term "emergency department", relevant reports that used alternative terminology or were not in English may have potentially been omitted. Emergency care in many countries are delivered in a number of settings outside of a formal ED, and this study only captures visits to facilities explicitly providing emergency care. Therefore, our results likely only describe a fraction of how emergency care is utilized around the world, and is unlikely to be a precise representation of the global emergency care landscape. Future efforts to obtain official data from governments and major healthcare providers may address these limitations. In estimating the burden of emergency conditions, the assumption that deaths and DALYs were zero for the 10 region-specific conditions when no data were reported may have resulted in an underestimation. Finally, while deaths and DALYs are commonly used to quantify burden of disease, there are inherent limitations in representing complex realities using aggregate measurements.
Conclusions
Despite these limitations, our findings shed some light on the global burden of emergency conditions and how emergency care is currently utilized around the world. Emergency facilities in LMICs serve large patient populations with high levels of critical illnesses and mortality in populations with higher burden of emergency conditions, yet the current rates of emergency utilization are exceedingly low when compared to those of HICs.[21] A substantial proportion of the world's leading causes of deaths and DALYs have the potential to be addressed in an emergency care setting, and these results suggest that emergency care can no longer be considered a non-essential luxury, especially as LMICs experience the mounting "double burden" of communicable and noncommunicable diseases.[25] Emergency medicine has the potential to play an integral and vital role in global health. Prioritizing and broadening access to high-quality emergency care in LMICs and dedicating more resources to strengthening emergency care research could have a powerful impact on the global burden of disease.
Supplementary Material
Key messages.
What is already known on this subject?
High quality emergency care has the potential to address and prevent a substantial portion of death and disability around the world.
Little is known about the burden of emergency conditions or how frequently patients seek medical care, particularly in low- and middle-income countries.
No previous study has compared the burden of emergency conditions to the frequency of emergency care utilization or characterized the breakdown of the types of emergency conditions in various income groups and geographic regions.
What might this study add?
There is a paucity of data on emergency care utilization in both high- and low-income countries around the world, and where there were data, low income countries had higher burden of emergency conditions and lower rates of emergency care utilization.
Our estimation that a substantial portion of the global morbidity and mortality can be attributed to emergency conditions highlights the potentially powerful role for emergency care in reducing the global burden of disease.
Acknowledgments
Funding
None
Abbreviations
- CDs
Communicable diseases
- DALYs
Disability-adjusted life years
- ED
Emergency department
- HICs
High-income countries
- IQR
Interquartile range
- LICs
Low-income countries
- LMICs
Low- and middle- income countries
- MICs
Middle-income countries
- NCDs
Non-communicable diseases
Footnotes
Contributorship
All authors participated in the conception and design of the study. CYC and ZO designed the study. CYC and SA performed the data collection. CYC performed the data analysis and drafted and revised the manuscript. TAR, CAC, ZO provided guidance and edited the manuscript. ZO provided methodological oversight. All authors participated in the critical revisions of the manuscript for important intellectual content and approved the final manuscript.
Competing Interests
None
Contributor Information
Cindy Y. Chang, Harvard Affiliated Emergency Medicine Residency Program, Brigham and Women’s Hospital and Massachusetts General Hospital, Boston, Massachusetts, USA.
Samer Abujaber, Department of Emergency Medicine, Brigham and Women’s Hospital, Boston, Massachusetts, USA.
Teri A. Reynolds, Department for the Management of Noncommunicable Diseases, Disability, Violence and Injury, Prevention, World Health Organization, Geneva, Switzerland.
Carlos A. Camargo, Jr, Department of Emergency Medicine, Massachusetts General Hospital, Boston, Massachusetts, USA.
Ziad Obermeyer, Department of Emergency Medicine, Harvard Medical School, Boston, Massachusetts, USA.
References
- 1.Anderson PD, Suter RE, Mulligan T, et al. World Health Assembly Resolution 60.22 and Its Importance as a Health Care Policy Tool for Improving Emergency Care Access and Availability Globally. Ann Emerg Med. 2012;60 doi: 10.1016/j.annemergmed.2011.10.018. 35-44.e3. [DOI] [PubMed] [Google Scholar]
- 2.Hsia R, Razzak J, Tsai AC, et al. Placing emergency care on the global agenda. Ann Emerg Med. 2010;56:142–149. doi: 10.1016/j.annemergmed.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 3.Razzak JA, Kellermann AL. Emergency medical care in developing countries: is it worthwhile? Bull World Health Organ. 2002;80:900–905. [PMC free article] [PubMed] [Google Scholar]
- 4.Hirshon JM, Risko N, Calvello EJ, et al. Health systems and services: the role of acute care. Bull World Health Organ. 2013;91:386–388. doi: 10.2471/BLT.12.112664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Calvello E, Reynolds T, Hirshon JM, et al. Emergency care in sub-Saharan Africa: Results of a consensus conference. Afr J Emerg Med. 2013;3:42–48. [Google Scholar]
- 6.Kobusingye OC, Hyder AA, Bishai D, et al. Emergency medical systems in low- and middle-income countries: recommendations for action. Bull World Health Organ. 2005;83:626–631. [PMC free article] [PubMed] [Google Scholar]
- 7.Reynolds TA, Calvello EJB, Broccoli MC, et al. AFEM consensus conference 2013 summary: Emergency care in Africa - Where are we now? Afr J Emerg Med. 2014;4:158–163. [Google Scholar]
- 8.Hsia RY, Mbembati NA, Macfarlane S, et al. Access to emergency and surgical care in sub-Saharan Africa: the infrastructure gap. Health Policy Plan. 2012;27:234–244. doi: 10.1093/heapol/czr023. [DOI] [PubMed] [Google Scholar]
- 9.Moresky RT, Bisanzo M, Rubenstein BL, et al. A Research Agenda for Acute Care Services Delivery in Low- and Middle-income Countries. Acad Emerg Med. 2013;20:1264–1271. doi: 10.1111/acem.12259. [DOI] [PubMed] [Google Scholar]
- 10.Pines JM, Hilton JA, Weber EJ, et al. International perspectives on emergency department crowding. Acad Emerg Med Off J Soc Acad Emerg Med. 2011;18:1358–1370. doi: 10.1111/j.1553-2712.2011.01235.x. [DOI] [PubMed] [Google Scholar]
- 11.Reynolds TA, Bisanzo M, Dworkis D, et al. Research Priorities for Data Collection and Management Within Global Acute and Emergency Care Systems. Acad Emerg Med. 2013;20:1246–1250. doi: 10.1111/acem.12261. [DOI] [PubMed] [Google Scholar]
- 12.Steptoe AP, Corel B, Sullivan AF, et al. Characterizing emergency departments to improve understanding of emergency care systems. Int J Emerg Med. 2011;4:42. doi: 10.1186/1865-1380-4-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Risko N, Calvello EJ, de Ramirez SS, et al. Including emergency and acute care as a global health priority. Int J Emerg Med. 2011;4:75. doi: 10.1186/1865-1380-4-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Institute for Health Metrics and Evaluation. Global Burden of Disease Study 2010 (GBD 2010) Results by Cause 1990–2010 - Country Level. 2013 http://ghdx.healthdata.org/ihme_data.
- 15.American College of Emergecy Physicians. EMTALA Fact Sheet. http://www.acep.org/News-Mediatop-banner/EMTALA/
- 16.American Medical Association. Medicaid - Definition of Emergency Medical Condition and Emergency Medical Services. http://www.acep.org/uploadedFiles/ACEP/advocacy/state/medicaidreimb/AMA-StateMedicaidLawDefinitionsofEmergencyMedicalCondition.pdf.
- 17.Fleiss JL. Measuring nominal scale agreement among many raters. Psychol Bull. 1971;76:378–382. [Google Scholar]
- 18.Cohen J. A Coefficient of Agreement for Nominal Scales. Educ Psychol Meas. 1960;20:37–46. [Google Scholar]
- 19.United Nations Statistics Division. Demographic Yearbook. http://unstats.un.org/unsd/demographic/products/dyb/dybcensusdata.htm.
- 20.World Bank. Country and Lending Groups | Data. http://data.worldbank.org/about/country-and-lending-groups.
- 21.Obermeyer Z, Abujaber S, Makar M, et al. Emergency care in 59 low- and middle-income countries: a systematic review. Bull World Health Organ. 2015;93:577–586. doi: 10.2471/BLT.14.148338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Landis JR, Koch GG. The Measurement of Observer Agreement for Categorical Data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 23.World Health Organization. WHO | The top 10 causes of death. WHO. http://www.who.int/mediacentre/factsheets/fs310/en/
- 24.Jamison DT, Breman JG, Measham AR, et al., editors. Disease Control Priorities in Developing Countries. 2nd. Washington (DC): World Bank; 2006. [PubMed] [Google Scholar]
- 25.World Health Organization. The World Health Report 1999. Geneva: World Health Organization; 1999. Chapter 2: The Double Burden: Emerging Epidemics and Persistent Problems. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.