Abstract
Foreign body (FB) aspiration into the airway is lees common in adults than children. Nevertheless its incidence does not decrease through time. We present clinical relevant aspects of airway FBs on the basis of a selective review of pertinent literature retrieved by a search in the PubMed database. The most common aspirated FBs by adults are organics, especially fragments of bones and seeds. Symptoms usually are cough, chocking and dyspnea. Right localization, especially bronchus intermedius and right lower lobe, is more frequent. Chest radiography can be normal in up to 20% of the cases and FBs can be detected in 26% of the patients. FBs can safely remove in the majority of patients under flexible bronchoscopy. Surgical treatment must be reserved for cases in which bronchoscope fails or there are irreversible bronchial or lung complications.
Keywords: Bronchoaspiration, foreign body (FB), fibrobronchoscopy, rigid bronchoscopy
Introduction
Aspiration of a foreign body (FB) is a potentially life-threatening emergency and 75% of cases occur in children younger than 3 years of age (1-3). However, FB aspiration does happen in adults and elderly people as well (4). The estimated incidence in these age groups is not well known, but in literature is around 0.2% to 0.33% of all performed bronchoscopies (5-9).
The first published case of endoscopic extraction occurred on March 1897, when a German farmer experienced dyspnea, cough and hemoptysis after aspirating a pork bone. Using a modified Mikulicz-Rosenheim esophagoscope (a rigid tube illuminated with a mirror) and rigid forceps, Gustav Killian removed the splinter from de right main bronchus (10). Currently, both rigid and flexible bronchoscopes are performed for this indication depending on the age of the patient and the nature of the FB (5).
The aim of this review is to describe the clinical, radiological and endoscopic characteristics of adult patients with FB bronchoaspiration.
Methods
In order to compile this review article we conducted a selective literature search in PubMed (last accessed on 30 August 2016). A total of 125 manuscripts matched our search term “airway FB and adult NOT child NOT case report”. Restricting the search to include only articles in English or Spanish reduced the number of matches to 95 articles. After excluding articles with case reports, with children or with fewer than 10 patients, we were left with 12 publications.
Because data from randomized studies are lacking, we based our article exclusively on retrospective publications, reviews, and recommendations from medical specialty societies in patients older than 14 years old.
The analysed variables were: age, sex, clinical picture, risk factors for aspiration, type of FB, radiographic findings and information concerning the FB removal (type of bronchoscopy and surgical requirement).
Clinical presentation
Taking account all the selected papers, the mean age of patients with FB aspiration is 48 years with a range of 16 to 99 years. In all series, male sex is more frequent with a ratio 1.5:1.
The classical triad of cough, dyspnea, and cyanosis occurs in only a small percentage of patients (11). A non-asphyxiating FB may be asymptomatic, especially in elderly people. Many of these objects are wedged distally and patients often do not recall the choking episode, the aspiration, or any precipitating event (4). Thus, FB aspiration is commonly misdiagnosed. In some cases the delay in establishing the correct diagnosis and initiating the appropriate treatment after aspiration can be long periods of time, for months to years (6). Moreover, they often result from fortuitous discovery when fibrobronchoscopy is performed to evaluate a chronic cough, hemoptysis, or a slow resolution of pneumonia (7). In the analysed series the longest time between the bronchoaspiration and FB removal was 30 years (12). The most common symptoms of a nonasphyxiating FB reported were: cough (66.1%), choking (27%), dyspnea (26.6%), fever (22.2%) and hemoptysis (17.2%).
We have found that few papers report risk factors present in patients with airway FB. Nevertheless we think that it is an important fact because it helps us to understand the mechanism of bronchoaspiration and sometimes the type of FB aspirated (6). The most frequent risk factors are older age, abuse of sedative medications, neurological disorders, mental retardation, trauma with loss of consciousness, dental care, alcoholism and tracheostomy cannula handling (6,8,13).
FB aspiration in adult patients is more frequently in the right bronchial tree, this could be explained by a more direct pathway of the right main stem bronchus whereas in children right and left bronchial trees present an equal distribution (14,15). Analyzing all series, we have checked that FBs were more frequently in the right bronchial tree versus left bronchial tree (71.5% vs. 22.8%) and only 5.7% were in the trachea. Lodgement was more common in intermediaries bronchus (27%) and right lower lobe (33%).
Radiological findings
With regard to radiological findings, the standard posteroanterior or lateral chest X-ray is performed in almost all of the patients with suspected FB aspiration. There are few papers reporting the use of computed tomography (CT) to diagnose a FB aspiration (for example, 35% of the cases in the paper published by Hsu; they explain that CT was useful to plan the airway intervention) (8). It is striking the paper published by Lin et al. (4). They performed CT in 96% of the patients. This fact can be explained because they studied a geriatric series and symptoms were nonspecific.
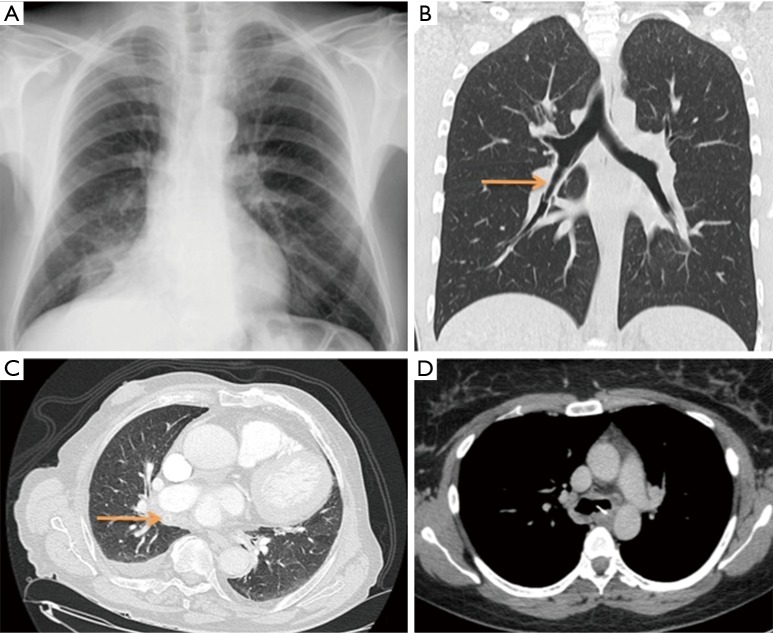
Radiopaque FBs such as seen in Figure 1 may be visualized in 26% of the cases. Metallic FBs are easily identified with great accuracy but they have a low frequency. In up to 20% of cases with suspected airway FB the chest X-ray can be normal. This fact should not obviate bronchoscopic evaluation in a clinical setting where the suspicion for airway FB aspiration is high (16). Delayed complications due to FB aspirations can result in recurrent pneumonia, obstructive emphysema, bronchial stenosis, bronchiectasis, pneumothorax, pneumomediastinum, recurrent hemoptysis, pleural effusion, empyema or bronchopleural fistula (17,18). Analysing all series, we observed the followed radiological findings: consolidation (43%), bronchiectasis (5%), and atelectasis (15%). Other signs like empyema, lung abscess, hyperinflation or pleural effusion were occasional (Figure 1A,C).
Figure 1.
Radiological images showing complications and/or different radiopaque foreign bodies. (A) Posteroanterior chest radiograph. We can observe a consolidation in the medium lobe caused by chicken bone; (B) coronal image of CT. Arrow is showing a Bic cap lodged in the bronchus intermedius; (C) axial image of CT. Right pleural effusion and a cherry pit indicated by arrow; (D) axial image of CT. We can observe a deer bone lodged in left main bronchus. CT, computed tomography.
Categorizing foreign bodies
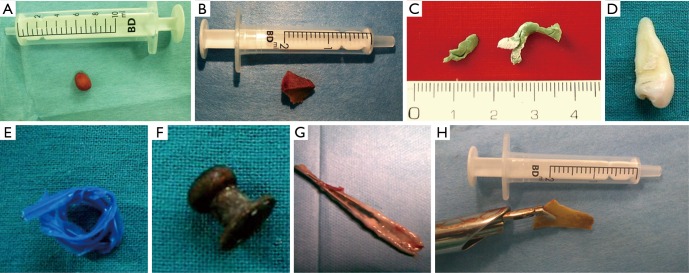
Airway FBs can be classified into organic and inorganic substances (17). After analysing all papers, it seems sensible to relate FBs with the risk factors presented in patients. Thus, organic FBs group includes bone fragments (specially chicken), fishbones, pieces of vegetables or fruits (for example pit cherries or bone plumps) and seeds (melon, sunflower). These FBs are more frequent in older patients and alcoholism abuse (6). Inorganic FBs comprehend pins, screws, rivets or plastic devices. They are typical in young people that accidentally aspirate small plastic or metal objects that had been introduced into the mouth as entertainment. Inorganic group also includes teeth (prevalent in craneoencephalic traumatisms), tablets or hypodermic needles (typical in IV drug addiction). We also could include an iatrogenic subgroup that comprehends pieces of voice prosthesis, tracheostomy cleaning brushes or dental bridges (Figure 2).
Figure 2.
Different FBs removed by flexible or rigid bronchoscope. (A) Cherry pit from an older patient; (B) fragment of a pork bone; (C) bronchial mold made from synthetic material used to make a dental prosthesis; (D) a dental piece removed from a patient with craneoencephalic traumatism; (E) plastic device used to close some bags with manufactured products; (F) a rivet; (G) hair clip removed from a patient with tracheostomy; (H) deer bone lodged for two years in the airway. FB, foreign body.
The most common group of FBs was the organic (47%; range 26–62%). In this group, the fragments of bones with a 20% stood out, followed by seeds (17%). Inorganic FBs counted 41% (range, 35–62%). The most frequent were tooth (10%) and metallic FBs (8%). In the iatrogenic subgroup any FB stands out of other representing a minimum percentage in each series.
FB removal
Although the rigid bronchoscope is still considered as the safest instrument in most pediatric centers to FB removal (11), most of the studies included in this review, considered the flexible bronchoscope as the initial and preferred method of choice to treat the adult airway (Table 1).
Table 1. Cases series of airway FB removal.
| First author, year (reference) | Patients (n) | Method used for FB removal [n (%)] | Surgery [n (%)] |
|---|---|---|---|
| Limper, 1990 (19) | 60 | 14 (23.3%) flexible bronchoscope; 37 (61.6%) rigid bronchoscope; 6 (10%) both | 3 (5%) |
| Lan, 1994, (20) | 47 | 41 (87.2%) flexible bronchoscope; 5 (10.6%) lost follow-up and spontaneous expulsion | 1 (2.1%) |
| Chen, 1997 (12) | 43 | 32 (74%) flexible bronchoscope; 2 (4.6%) rigid bronchoscope; 3 (7.5%) no dates | 6 (13.9%) |
| Doñado, 1998 (13) | 56 | 54 (96.4%) flexible bronchoscope; 2 (3.5%) rigid bronchoscope | 1 (1.7%) |
| Debeljak, 1999 (5) | 62 | 42 (68%) flexible bronchoscope; 4 (6%) rigid bronchoscope; 16 (26%) both | 1 (1.6%) |
| Swanson, 2004 (16) | 65 | 58 (89%) flexible bronchoscope; 2 (3.07%) rigid bronchoscope; 4 (6.3%) both | 1 (1.56%) |
| Ramos, 2009 (6) | 32 | 24 (75%) flexible bronchoscope; 4 (12.5%) rigid bronchoscope; 2 (6.3%) both; 2 (6.3%) spontaneous expulsion | 5 (15.6%) |
| Mise, 2009 (7) | 86 | 86 (100%) flexible bronchoscope | 1 (1.16%) |
| Rodrigues, 2012 (21) | 40 | 34 (85%) flexible bronchoscope; 6 (15%) rigid bronchoscope | 1 (2.5%) |
| Lin, 20014 (4) | 43 | 43 (100%) flexible bronchoscope | 0 |
| Sehgal, 2015 (9) | 49 | 45 (91.8%) flexible bronchoscope; 2 (4.08%) rigid bronchoscope; 2 (4.08%) lost follow-up | 0 |
| Hsu, 2015 (8) | 80 | 48 (60%) flexible bronchoscope; 32 (40%) rigid bronchoscope | 0 |
FB, foreign body.
Flexible bronchoscopy is a relatively easy and safe procedure in experienced hands. With the use of a flexible bronchoscopy under local anesthesia to visualize airway, removal of a FB can be attempted and avoids the added cost, risk, and morbidity of a secondary invasive procedure such as rigid bronchoscopy under general anaesthesia (22,23).
In our analysis, most of FBs were retrieved with flexible bronchoscopy, with a pooled success rate of 79.1%. Open surgical procedures were required for only 3.76% of the patients. In some series, surgery was necessary in more than 10% of the cases (6,12). Usually, these patients had residual lesions following inflammatory process (6).
Du Rand et al. removed FBs using a rigid bronchoscopy in 60% of the cases (22). However, in other papers like the reported by Hsu, the majority of FB removed by rigid bronchoscopy could not otherwise be done with flexible bronchoscopy. This is due to the fact that FBs were stents and its retrieval was only possible with rigid bronchoscopy (8).
The most useful instruments for FB removal are shark-tooth forceps, alligator forceps or wire basket (2,5,8). In some cases suction is enough to resolve the problem. Complications during bronchoscopy are very rare. Bleeding is the most frequent (1% of the cases). With regard to bronchoscopic findings due to FB impaction, the most common lesion is granulation tissue (43% of cases) and mucosal inflammation (28%).
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Yalçin S, Karnak I, Ciftci AO, et al. Foreign body ingestion in children: an analysis of pediatric surgical practice. Pediatr Surg Int 2007;23:755-61. 10.1007/s00383-007-1958-y [DOI] [PubMed] [Google Scholar]
- 2.Zhijun C, Fugao Z, Niankai Z, et al. Therapeutic experience from 1428 patients with pediatric tracheobronchial foreign body. J Pediatr Surg 2008;43:718-21. 10.1016/j.jpedsurg.2007.10.010 [DOI] [PubMed] [Google Scholar]
- 3.Salih AM, Alfaki M, Alam-Elhuda DM. Airway foreign bodies: A critical review for a common pediatric emergency. World J Emerg Med 2016;7:5-12. 10.5847/wjem.j.1920-8642.2016.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lin L, Lv L, Wang Y, et al. The clinical features of foreign body aspiration into the lower airway in geriatric patients. Clin Interv Aging 2014;9:1613-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Debeljak A, Sorli J, Music E, et al. Bronchoscopic removal of foreign bodies in adults: experience with 62 patients from 1974-1998. Eur Respir J 1999;14:792-5. 10.1034/j.1399-3003.1999.14d11.x [DOI] [PubMed] [Google Scholar]
- 6.Ramos MB, Fernández-Villar A, Rivo JE, et al. Extraction of airway foreign bodies in adults: experience from 1987-2008. Interact Cardiovasc Thorac Surg 2009;9:402-5. 10.1510/icvts.2009.207332 [DOI] [PubMed] [Google Scholar]
- 7.Mise K, Jurcev Savicevic A, Pavlov N, et al. Removal of tracheobronchial foreign bodies in adults using flexible bronchoscopy: experience 1995-2006. Surg Endosc 2009;23:1360-4. 10.1007/s00464-008-0181-9 [DOI] [PubMed] [Google Scholar]
- 8.Hsu AA. Endoscopic intervention of lower airway foreign matter in adults-a different perspective. J Thorac Dis 2015;7:1870-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sehgal IS, Dhooria S, Ram B, et al. Foreign Body Inhalation in the Adult Population: Experience of 25,998 Bronchoscopies and Systematic Review of the Literature. Respir Care 2015;60:1438-48. 10.4187/respcare.03976 [DOI] [PubMed] [Google Scholar]
- 10.Killian G. Meeting of the Society of Physicians of Freiburg, Freiburg. 1897, Dec 17. Munchen Med Wschr 1898;45:378. [Google Scholar]
- 11.Acharya K. Rigid Bronchoscopy in Airway Foreign Bodies: Value of the Clinical and Radiological Signs. Int Arch Otorhinolaryngol 2016;20:196-201. 10.1055/s-0036-1584293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen CH, Lai CL, Tsai TT, et al. Foreign body aspiration into the lower airway in Chinese adults. Chest 1997;112:129-33. 10.1378/chest.112.1.129 [DOI] [PubMed] [Google Scholar]
- 13.Donado Uña JR, de Miguel Poch E, Casado López ME, et al. Fiber optic bronchoscopy in extraction of tracheo-bronchial foreign bodies in adults. Arch Bronconeumol 1998;34:76-81. [DOI] [PubMed] [Google Scholar]
- 14.Oğuzkaya F, Akçali Y, Kahraman C, et al. Tracheobronchial foreign body aspirations in childhood: a 10-year experience. Eur J Cardiothorac Surg 1998;14:388-92. 10.1016/S1010-7940(98)00205-X [DOI] [PubMed] [Google Scholar]
- 15.Brkić F, Delibegović-Dedić S, Hajdarović D. Bronchoscopic removal of foreign bodies from children in Bosnia and Herzegovina: experience with 230 patients. Int J Pediatr Otorhinolaryngol 2001;60:193-6. 10.1016/S0165-5876(01)00531-6 [DOI] [PubMed] [Google Scholar]
- 16.Swanson KL. Airway foreign bodies: what's new? Semin Respir Crit Care Med 2004;25:405-11. 10.1055/s-2004-832713 [DOI] [PubMed] [Google Scholar]
- 17.Rafanan AL, Mehta AC. Adult airway foreign body removal. What's new? Clin Chest Med 2001;22:319-30. 10.1016/S0272-5231(05)70046-0 [DOI] [PubMed] [Google Scholar]
- 18.Zissin R, Shapiro-Feinberg M, Rozenman J, et al. CT findings of the chest in adults with aspirated foreign bodies. Eur Radiol 2001;11:606-11. 10.1007/s003300000619 [DOI] [PubMed] [Google Scholar]
- 19.Limper AH, Prakash UB. Tracheobronchial foreign bodies in adults. Ann Intern Med 1990;112:604-9. 10.7326/0003-4819-112-8-604 [DOI] [PubMed] [Google Scholar]
- 20.Lan RS. Non-asphyxiating tracheobronchial foreign bodies in adults. Eur Respir J 1994;7:510-4. 10.1183/09031936.94.07030510 [DOI] [PubMed] [Google Scholar]
- 21.Rodrigues AJ, Oliveira EQ, Scordamaglio PR, et al. Flexible bronchoscopy as the first-choice method of removing foreign bodies from the airways of adults. J Bras Pneumol 2012;38:315-20. 10.1590/S1806-37132012000300006 [DOI] [PubMed] [Google Scholar]
- 22.Du Rand IA, Blaikley J, Booton R, et al. British Thoracic Society guideline for diagnostic flexible bronchoscopy in adults: accredited by NICE. Thorax 2013;68 Suppl 1:i1-i44. 10.1136/thoraxjnl-2013-203618 [DOI] [PubMed] [Google Scholar]
- 23.Dikensoy O, Usalan C, Filiz A. Foreign body aspiration: clinical utility of flexible bronchoscopy. Postgrad Med J 2002;78:399-403. 10.1136/pmj.78.921.399 [DOI] [PMC free article] [PubMed] [Google Scholar]