Abstract
Self-efficacy, defined as the confidence one has in the ability to perform a behavior or specific task, has been introduced as a crucial motivational factor for successfully carrying out social and everyday living skills (Bandura, 1977, 1997). Few studies have assessed its role in functioning in schizophrenia. The current study was designed to investigate whether degree of illness insight determined whether self-efficacy was a mediator of the relationship between two key illness features, negative symptoms and cognition, and functional skills. Sixty-nine individuals with schizophrenia were administered measures of self-efficacy, cognition, symptoms, insight and performance-based measure of everyday living and social skill. Results revealed that self-efficacy was only linked to measures of functional skills when illness insight was intact. There was evidence of moderation of confounding effects such that when self-efficacy was controlled, the relationship between negative symptoms and measures of everyday life skills became non-significant, but only when illness insight was intact. These findings emphasize the importance of including illness insight in models of the role of self-efficacy in functioning in schizophrenia.
Keywords: schizophrenia, self-efficacy, cognition, negative symptoms, insight
1. Introduction
While contemporary pharmacologic strategies are effective at managing positive symptoms, they have had little impact on poor vocational, social and educational outcome that is a defining feature of schizophrenia (DSM-IV; APA, 1994). Thus, understanding determinants of poor outcome in the disorder has become a central goal of study for the development of efficacious treatments. A wealth of studies conducted over the past 20 years has supported a link between cognitive skills (e.g., attention, memory, and problem-solving) and functional status for patients with schizophrenia, whether measured cross-sectionally or longitudinally, and whether functioning is measured by third-party assessments of community function, measures of performance-based social and daily-living skill measures, or the ability to benefit from rehabilitation programs. Current estimates suggest that 20–60% of variance in functioning is explained by cognitive deficits (e.g., Green et al., 2000; Green et al., 2004).
Similarly, negative symptoms, including blunted affect, social withdrawal, and alogia, have also been linked moderately to a variety of indices of functional status including third-party ratings of community function (e.g., Kurtz et al., 2005) as well as performance-based measures of social (Patterson et al., 2001) and everyday living (Patterson et al., 2001) skills. Most recent analyses from the CATIE trial (Rabinowitz et al., 2012; n=1447) suggest that improvements in negative symptoms are more strongly linked to improvements in function than other symptom types, even when functioning items that might be linked to ratings of negative symptoms (method variance) are removed. Recent research has sought to expand on previous studies by understanding how cognition and negative symptoms are linked to function in schizophrenia, and whether other illness variables may mediate these relationships. For example, measures of social cognition, the cognitive operations involved in perceiving, understanding and interpreting our social world have been increasingly viewed as mediating the relationship between cognitive skills and outcome (see Schmidt et al., 2011, for a review), and thus have been increasingly attended to as a potential target for treatment.
Self-efficacy, defined as the confidence one has in their ability to perform a behavior or specific task, has been introduced as a crucial motivational factor for successfully carrying out social and everyday living skills (Bandura, 1977, 1997). Few studies have assessed its role in functioning in schizophrenia. Pratt et al., (2008) in a cross-sectional study of 85 patients with schizophrenia or schizoaffective disorder, tested a model in which a measure of self-efficacy was assessed as a mediator of the relationship between cognition, negative symptoms and premorbid functioning and a measure of psychosocial status (an average of two indices of third-party rated function). Results revealed that while measures of self-efficacy were modestly related to function and negative symptoms and premorbid function, there was no evidence that self-efficacy mediated links between other illness domains and functional status. Instead, there was evidence that negative symptoms mediated the relationship of self-efficacy and function. The authors concluded that negative symptoms, rather than self-efficacy should be the target of novel behavioral and pharmacologic treatments that have as a goal enhancing function in schizophrenia. The authors noted that impaired insight in their sample may have impacted the ability of clients to render the type of appraisal of self-efficacy evident in healthy populations.
In a more recent study, Cardenas et al. (2012) explored whether self-efficacy levels bridged the capacity-to-functioning gap in which a person with schizophrenia is able to demonstrate the capacity for completing daily life tasks, but fails to successfully accomplish these tasks in everyday life. In a sample of 97 middle-aged and older people with schizophrenia or schizoaffective disorder, results revealed a relationship between functional capacity and actual community daily functioning in patients with high self-efficacy (those who believed that they could carry these behaviors out successfully in the community); however, this relationship was not significant in patients with low self-efficacy. These findings suggest that the construct of self-efficacy may help explain why some individuals with schizophrenia have the capacity to function well in the community but remain unable to translate these skills into achieved levels of community function. Thus, studies to date in schizophrenia support the role of motivational factors such as self-efficacy in bridging the gap between everyday life skills demonstrated in the clinic and skills employed in the community, but show less of a role in influencing functioning in the disorder when compared to other key illness domains.
The current study was designed to investigate whether self-efficacy either serves, or doesn’t serve as a mediator of the relationship of key illness features, negative symptoms and cognition, and two performance-based measures of functional skills, a measure of performance of everyday living skills and a measure of social skill, depending upon the level of illness insight. The study was motivated by the assumption that accurate insight into illness is a necessary precondition for forming accurate appraisals about one’s ability to carry out behaviors necessary for functioning and that individuals with poor illness insight would also show poor insight into one’s own functioning and the effectiveness of one’s behaviors. We also hypothesized that performance-based assessments of skills would be less influenced by factors external to the disease that might influence the ability to perform behaviors in vivo even when belief in successful performance of those behaviors is high, (e.g., opportunity to engage in social interactions secondary to living in a an isolated area, limited opportunity to engage in recreational activities because of limited financial resources), and thus might provide a better index of the relationship of key illness domains, beliefs about skills and performance of those skills. We predicted: (1) illness insight would moderate the relationship of self-efficacy with functional status in domains of everyday living and social skills; patients with good illness insight would show a stronger relationship between self-efficacy and function than patients with poor insight, and (2) only in patients with strong illness insight, and not in those with poor insight, self-efficacy would mediate the relationship of key illness domains such as negative symptoms and cognition and measures of everyday living and social skills (moderated mediation).
2. Methods
2.1 Participants
Sixty-nine patients who met the criteria for schizophrenia or schizoaffective disorder, according to the DSM-IV (APA, 1994) participated. Diagnosis was confirmed via the Structured Clinical Interview for DSM-IV (First et al., 1995). Exclusion criteria for all potential participants were: (a) known neurological disease, (b) developmental disability, (c) current substance abuse, (d) mental retardation as evidenced by a history of services, or (e) lack of fluency in English. All participants provided written informed consent forms and all procedures were in accordance with institutional review procedures. Recruitment for the study was ongoing over a five-year period (2007–2012) and participants were recruited from one of three sites: outpatient clinics at The Institute of Living in Hartford, CT. (n=56), Inter-Community Mental Health Group in East Hartford, CT (n=10), or an inpatient unit at Cedar Crest Mental Health Center, Newington, CT. (n=3). Data for this study were collected at entry to an ongoing parent study of the combined effects of cognitive remediation and social skills training on a variety of proximal and distal treatment outcome measures in schizophrenia (e.g., Kurtz et al., 2007). Demographic and clinical characteristics of the sample are presented in Table 1.
Table 1.
Demographic and clinical characteristics (n=62–68)
| Variable | Mean (SD; range) |
|---|---|
|
| |
| Age | 31.4 (11.5; 18–57) |
|
| |
| Sex (% male) | 73.5 |
|
| |
| Education (years) | 12.0 (2.2; 6–16) |
|
| |
| Illness Duration (years) | 10.6 (9.8; 0.3–37) |
|
| |
| Age Onset (years) | 22 (6.3; 13–46) |
|
| |
| PANSS Positive Subscale Score | 17.3 (5.3; 9–30) |
|
| |
| PANSS Negative Subscale Score | 19.3 (5.7; 9–35) |
|
| |
| Antipsychotic Medication | Percentage (%) treated |
|
| |
| Atypical: | |
| Risperidone | 23.0 |
| Clozapine | 14.9 |
| Quetiapine | 14.9 |
| Olanzipine | 13.8 |
| Aripiprazole | 12.6 |
| Paliperidone | 3.5 |
| Ziprasidone | 3.5 |
|
| |
| Typical: | |
| Haloperidol | 6.9 |
| Perphenazine | 4.6 |
2.2 Assessment Measures
2.2.1 Self-Efficacy
The Revised Self-Efficacy Scale (SES, McDermott, 1995) designed specifically for use with people with schizophrenia, was used to assess the participants’ confidence in their abilities to control symptoms associated with their illness in order to perform specific tasks or behaviors. The ratings are based on a 100-point scale, in which a rating of “0” indicates no confidence, and a rating of “100” indicates total confidence in one’s ability to complete the task or behavior. The scale consists of fifty-seven items that are divided into three subscales, each consisting of nineteen items. The subscales measure confidence in one’s ability to perform social behaviors and to manage positive and negative symptoms, as well as an overall self-efficacy score, representing a mean score of the three subscales. The scale has demonstrated strong evidence of reliability and evidence of construct validity (McDermott, 1995; Pratt et al., 2008).
2.2.2 Insight into Illness
Insight into illness was measured from the PANSS, “Lack of Judgment and Insight (G12)”. This item is rated on a seven-point scale with a “1” indicating no impaired awareness or understanding of one’s own psychiatric condition and life situation and a “7” indicating extreme impairment, an emphatic denial of past and present psychiatric illness.
2.2.3 Cognitive Assessment
All participants were administered a neuropsychological test battery including the Digit Span and the Digit Symbol subtests from the Wechsler Adult Intelligence Scale-III or IV (WAIS-III and IV; Wechsler, 1997; 2008), the California Verbal Learning Test-II (Delis et al., 2000), and the Penn Conditional Exclusion Test (PCET; Kurtz et al., 2004). For the CVLT-II, performance on trials 1 through 5 was selected as the independent measure. For the PCET, the total number of errors was selected for analysis. Age-corrected scaled scores were selected for WAIS subtests. Measures were selected based on their relationships with functional status in previous studies of schizophrenia (e.g., Green et al., 2000; 2004) and are a representative subgroup of the six separable factors underlying cognition in schizophrenia and consistent with the domains of MATRICS (e.g., Nuechterlein et al., 2004). Cognitive testing and scoring were supervised by a doctoral-level psychologist.
2.2.4 Symptoms
The Positive and Negative Syndrome Scale (PANSS; Kay et al., 1987) was used to assess symptoms. This measure is a semi-structured interview that generates ratings of signs and symptoms on thirty 7-point Likert scale items. The subscale for total negative symptoms was selected as an independent measure. Symptom raters of this study maintained inter-rater reliability, and all raters were trained to a criterion reliability of 0.7 intraclass correlation coefficient for four independent, consecutive ratings.
2.2.5 Measure of ADLs
The brief version of the UCSD Performance-based Skills Assessment (UPSA-B; Patterson et al., 2001; Mausbach et al., 2007) was used to assess the participants’ abilities to perform certain everyday living tasks. The original version of the UPSA comprised five domains of functioning; in this brief form of the assessment, participants are asked to role-play skills in finances, including tasks such as writing a check, and communicative skills, with tasks such as dialing for help in an emergency and rescheduling an appointment with a doctor. Participants received a score ranging from zero to twenty, with higher scores representing better functional capacity. Performance on the UPSA-B is effective at predicting whether persons with schizophrenia are living independently in the community and employed (Mausbach et al., 2011).
2.2.6 Social Skill Measure
The Social Skill Performance Assessment (SSPA; Patterson et al., 2001) uses role-play scenarios, which model real-world situations, to measure functional social skills. The first role-play scenario involves greeting a new neighbor, while the second scenario involves effectively convincing a landlord to fix a leak as soon as possible. The scenario is rated on a five-point Likert scale based on a variety of dimensions of the social skill including interest/disinterest, fluency, clarity, focus, affect, overall conversation/argument, social appropriateness, grooming, negotiation ability, and submissive-persistent.
2.2.7 Data Analysis
The Statistical Package for the Social Sciences (SPSS 19.0) was used for statistical analyses. Pearson’s product-moment correlations were calculated between SES, ratings of illness insight, cognitive variables, negative symptom severity, and performance-based measures of ADLs and social skill to assess the relatedness of these constructs. SES subscales with strongest observed relationships to function were selected for subsequent analysis. To assess hypothesis 1, simultaneous regression models were tested entering insight, self-efficacy ratings and the interaction of insight and self-efficacy for each of the two outcome measures (UPSA-B and SSPA) to allow us to test the moderating effects of insight on the relationship of self-efficacy to function. Significant interactions were interpreted using methods outlined by Aiken and West (1991). Simple slope coefficients were calculated for the relation of self-efficacy to functional capacity at low (−1 SD), medium (mean) and high (+1 SD) levels of illness insight (Aiken & West, 1991). To test the second hypothesis of whether self-efficacy mediated functioning only in patients with good illness insight, we applied a moderated mediation model, to assess whether insight ratings moderated the relationship between cognitive deficits, negative symptoms, self-efficacy and functioning. Thus, at high levels of insight we would expect that, according to the methods of Baron and Kenny (1986): (a) measures of cognition and negative symptoms would be related to performance-based measures of both everyday life (UPSA-B) and social (SSPA) skill, (b) self-efficacy measures would be performance-based measures of both everyday life (UPSA-B) and social (SSPA) skill, (c) self-efficacy would be related to elementary cognitive function and negative symptoms, and (d) when self-efficacy was controlled for statistically, the relationship between cognition and negative symptoms and performance-based ADL and social skills would be reduced or removed. We then confirmed these findings with formal assessment of a conditional indirect effect (e.g., Muller et al., 2005; Preacher et al., 2007). For this analysis, the “Process” macro for SPSS 19 was used (Hayes, A. F. 2012), which implements a conditional path analysis model; the macro is available at the following site, http://www.afhayes.com/spss-sas-and-mplus-macros-and-code.html. In this analysis, the indirect effect was calculated by using a conditional indirect effect with a biased-corrected 95% bootstrap confidence interval. Participants with missing values for variables of a certain analysis were excluded from that specific analysis. The moderated mediation model we tested is presented in graphic form in Figure 1. All analyses were two-tailed and alpha was set at .05.
Figure 1.
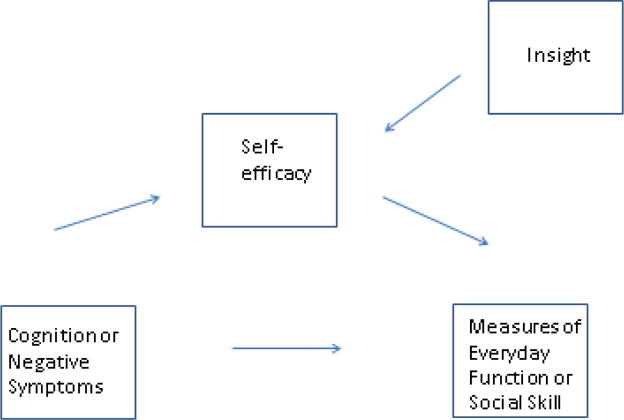
Graphic depiction of the moderated mediation model tested in the current study.
3. Results
3.1 Relationship of Study Variables
Correlations between standardized neurocognitive assessment scores, negative symptom ratings, scores from the three subscales of the Self-Efficacy Scale, illness insight ratings and scores from the two performance-based functioning measures are presented in Table 2. Neurocognitive measures of digit span were related to both UPSA-B (r=.50) and SSPA (r=.27) while Digit Symbol Coding was linked to SSPA (r=.30). Negative symptoms were linked to both UPSA-B (r=−.36) and SSPA (r=−.54). Relationships between self-efficacy ratings and everyday life and social skill were non-significant.
Table 2.
Intercorrelations of variables (n=62–69)
| Symptoms | Self-efficacy Scores | Cognitive Variables | Functional Measures | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Insight | Negative Symptoms | Positive | Negative | Social | Average | Digit Span | Coding | CVLT-II | PCET errors | UPSA-B | SSPA | |
|
Symptoms: Insight Negative Symptoms |
||||||||||||
| 0.301* | ||||||||||||
|
Self-efficacy: Positive Negative Social Average |
0.104 | −0.121 | ||||||||||
| 0.276* | −0.105 | 0.719** | ||||||||||
| 0.130 | −0.166 | 0.630** | 0.785** | |||||||||
| .179 | −.134 | .889** | .923** | .882** | ||||||||
|
Cognitive Variables: Digit Span Coding CVLT PCET errors |
−0.188 | −0.311* | 0.117 | −0.102 | −0.035 | .002 | ||||||
| 0.030 | −0.121 | −0.047 | −0.091 | −0.061 | −.069 | 0.78 | ||||||
| −0.016 | 0.002 | 0.019 | −0.218 | −0.234 | −.148 | 0.292* | 0.259* | |||||
| 0.077 | 0.034 | −0.171 | −0.028 | −0.055 | −.106 | −0.200 | 0.074 | −0.299* | ||||
|
Functional Measures UPSA-B SSPA |
−0.175 | −0.375** | 0.215 | −0.030 | −0.030 | .058 | 0.511** | 0.050 | 0.061 | −0.087 | ||
| −0.229 | −0.554** | 0.017 | −0.052 | 0.059 | −.011 | 0.274* | 0.302* | 0.105 | 0.128 | 0.445** | ||
3.2 Moderating effects of insight on the relationship of self-efficacy on everyday life and social skill
Results from the simultaneous regression analysis testing the moderating effects of illness insight on the relationship of self-efficacy to performance-based functioning was significant for both everyday life (t=−2.55; p<.05) and social skill (t=−2.09; p<.05; see Table 3). These interactions were plotted in Figures 2 and 3 using the simple slopes method described by Aiken and West (1991). For the patient group showing high levels of insight, scores of the self-efficacy positive subscale were related to UPSA-B scores (B=.061; p=.012), but this relationship did not exist for patients showing mean or low levels of insight (B=.023; p=.145; B=−.014, p=.562, respectively). Self-efficacy social subscale was significantly related to SSPA scores at high levels of insight (B=.014; p=.019) but not at mean and low levels of illness insight (B=.002, p=.684; B=−.011, p=.123, respectively).
Table 3.
Multiple regressions for the prediction of outcome by insight, the negative or positive subcategory of self-efficacy, and the interaction of insight and self-efficacy (n=52–66)
| Measure | Step 1 | Step 2 | Step 3 | F-value | R2 |
|---|---|---|---|---|---|
|
SSPA Insight |
−.229 p = .106 |
−.254 p = .082 |
1.207 p = .046 |
2.715 p = .106 |
.052 |
| Social SE | .115 p = .427 |
.991 p = .010 |
1.668 p = .199 |
.065 | |
| Insight × Social SE | −1.891 p = .014 |
3.415 p = .025 |
.179 |
| Measure | Step 1 | Step 2 | Step 3 | F-value | R2 |
|---|---|---|---|---|---|
|
UPSA-B Insight |
−.180 p = .154 |
−.200 p = .113 |
.620 p = .136 |
2.087 p = .154 |
.033 |
| Positive SE | .187 p = .138 |
.789 p = .014 |
2.192 p =.120 |
.067 | |
| Insight × Positive SE | −1.096 p = .041 |
2.996 p = .048 |
.130 |
Figure 2.
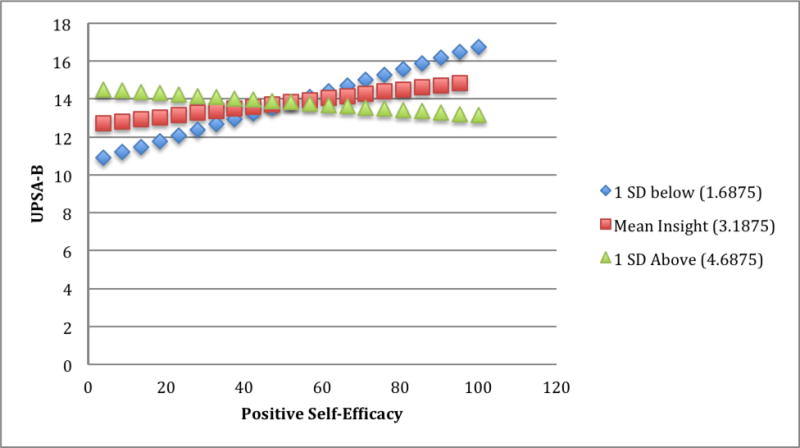
The moderating effect of insight on the relationship between the positive subcategory of the Self-Efficacy Scale and the UPSA-B (n = 66). Note: UPSA-B=UCSD Performance-Based Skills Assessment, Brief version.
Figure 3.
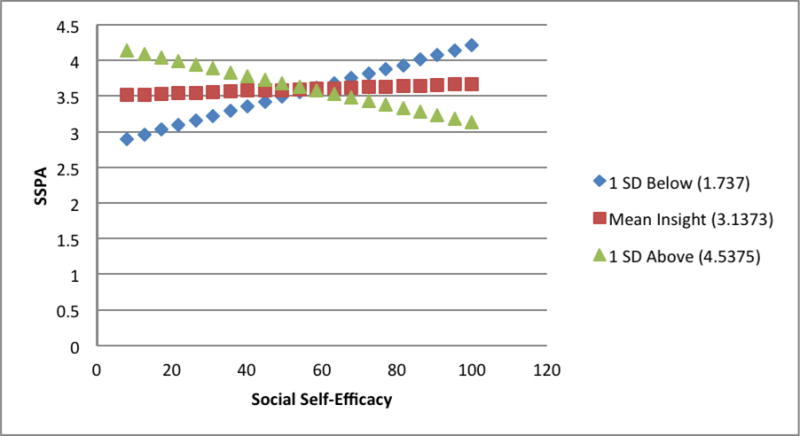
The moderating effect of insight on the relationship between the social subcategory of the Self-Efficacy Scale and the SSPA (n = 52). Note: SSPA=Social-Skill Performance Assessment.
3.3 Moderated Mediation
Subgroup analysis using a median split of insight scores showed the requisite relationships between negative symptoms and UPSA-B (r=−.43), self-efficacy and UPSA-B (r=.51) and but not negative symptoms and self-efficacy (p>.22). Thus, true moderated mediation was not supported. The standardized beta value for negative symptoms was significant (beta=−.41, t=−2.49, p=.021) with a regression model including negative symptoms only; but non-significant (negative symptom standardized beta=−.35, t=−1.84, p=.079) for a model with negative symptoms and self-efficacy measures. Taken together these findings suggest moderation of a confounding effect of self-efficacy on the relationship between negative symptoms and everyday life skills. Analysis of the model described in Figure 1 showed that measures of self-efficacy when controlled reduced the relationship of negative symptom ratings to a performance-based measure of functional status (UPSA-B) to non-significance when insight was high; however, the coefficient of the indirect effect was not significant (effect=−.02; 95% CI:−.10/.02). All other model coefficients were non-significant and no other subgroup regression analyses revealed evidence of moderated mediation or moderation of confounding effects. Prerequisite relationships were not evident for any of the cognitive measures and functioning or negative symptoms and performance-based social skills in the high-insight subsample, and consequently no tests for mediation were conducted for those measures.
4. Discussion
This is the first study, to our knowledge, to assess the relative roles of insight, self-efficacy, negative symptoms, cognition and performance-based functional status (ADL and social skill) in schizophrenia. The results of the current study revealed two interesting findings. First, and consistent with hypotheses, insight was found to moderate the relationship between self-efficacy and performance-based measures of both ADLs and social skill. At high levels of illness insight, self-appraisals regarding the ability to carry out key social and ADL activities were linked to objective measures of functional status; however, at lower levels of illness insight, when presumably self-appraisals regarding life skills were likely less accurate, measures of self-efficacy had little relationship to performance-based measures of function. These findings provide an explanation for why self-efficacy beliefs, which have been shown to play a significant role in achievement outcomes in healthy populations (e.g., academic expectations and subsequent performance and career choice; Bandura et al., 2001), have been shown to play less of a role in mediating the effects of key illness features such as cognition, negative symptoms and function, in at least some studies of schizophrenia (Pratt et al., 2008).
Second, we found limited evidence for moderation of confounding effects of illness features, self-efficacy and ADL skill. More specifically, there was evidence that the relationship of negative symptoms to a performance-based measure of ADL skill was rendered non-significant when self-efficacy for managing symptoms was controlled, but only at high levels of illness insight; thus, the influences of symptoms such as amotivation and alogia on functional skills are shared through the impact of a client’s appraisal of their ability to manage their symptoms (self-efficacy) when illness insight is intact. These findings suggest that targeted treatment of self-efficacy beliefs in patients with high illness insight could play a crucial role in improving outcome for those patients. These findings also suggest that self-efficacy beliefs may play a differential role in mediating important illness features (negative symptoms as opposed to cognitive skills) and functioning.
It is important to note that the current findings are inconsistent of those of Grant and Beck (2009), who found that a measure of defeatist beliefs mediated the relationship of cognition and function in their sample of outpatients with schizophrenia, using a battery of neurocognitive measures highly similar to those selected for the current study. The use of two performance-based measure of functioning in the current study versus a third-party rating of subjective report of function in the previous study, may provide a partial explanation for this discrepancy and may suggest that attention to the type of measurement and domain of functioning in schizophrenia in future studies may help elucidate the role of self-efficacy beliefs in different aspects of outcome in schizophrenia.
Self-efficacy theory in its original formulation posits that the role of self-efficacy beliefs in motivation is domain specific, such that confidence in the ability to perform a specific task, such as running a 4.5-minute mile, influences the degree of effort expended to achieve that specific goal. More recent theoretical models have suggested that self-efficacy beliefs can be more general with beliefs about the ability to perform well in a domain more broadly (academic achievement) linked as tightly to specific outcomes as beliefs about these specific outcomes themselves (Eccles & Wigfield, 2002). In the current paper we took an exploratory approach, utilizing those self-efficacy beliefs that were most closely tied to functioning in a correlation analysis for further investigation. While relationships between self-efficacy and function were very modest and non-significant in the overall sample, when insight was controlled for, beliefs about social skill were linked to a functioning measure focused on social skill, while self-efficacy beliefs about the ability to manage positive symptoms, a set of beliefs less tightly linked conceptually to our selected outcome (UPSA-B), was found to be related to daily functioning skills. These findings suggest that in schizophrenia the relationship between self-efficacy beliefs and specific functional skills are not always domain specific, and self-efficacy beliefs related to symptom management more generally may link to some aspects of function most strongly in individuals with high insight.
Several limitations to the current study should be noted. First, items from the self-efficacy scale selected for the current study were not isomorphic with our skills used to assess function, such as writing a check or negotiating a house repair with a landlord. It is possible that self-efficacy beliefs would play a larger role in mediating outcome if belief assessments were more closely tuned to the specific skills measured as part of outcome in this study. Related to this concern, failure to find a mediating role between self-efficacy beliefs, cognition and functioning could be related to the fact that only two items on the measures of self-efficacy selected for this study (the RSES) measure self-efficacy with respect to cognitive function. Second, the current study is cross-sectional and is limited in its ability to suggest causal relationships between the psychological, symptom and function constructs measured in this study. We note one recent study that has linked self-efficacy beliefs measured at study entry to both a learning effect and the durability of that learning effect after completing a math learning program, even after accounting for differences in method of instruction, baseline arithmetic ability and task interest (Choi et al., 2010; Choi & Medalia, 2010). Third, our sample consisted of stabilized, chronic patient samples and it remains unclear to what extent these findings apply to patients in more acute or earlier stages of illness.
Acknowledgments
This work was supported by grants K08 MH-69888 from the National Institute of Mental Health (NIMH), and a Young Investigator Award from the National Alliance for Research on Schizophrenia and Depression (Kurtz) and a Howard Hughes Medical Institute Undergraduate Summer Research Fellowship (Olfson).
Role of funding source
The funding sources for this study had no role in the study design, collection, analysis or interpretation of the data, the writing of the report and in the decision to submit the manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
All authors declare they have no conflicts of interest.
Contributors
Matthew M. Kurtz, Ph.D., was responsible for initial conceptualization and design of the study (along with RO), oversaw all data collection, conducted portions of the statistical analyses, helped formulate the data analytic plan, and co-wrote the manuscript.
Rachel Olfson, was responsible for design of the study (along with MMK), conducted portions of the statistical analyses and co-wrote the manuscript.
Jennifer Rose, PhD, helped formulate the data analytic plan, provided models for testing indirect mediation effects and edited the data analytic portions of the manuscript.
References
- American Psychiatric Association. DSM-IV: Diagnostic and Statistical Manual of Mental Disorders. Fourth. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Bandura A. Self-efficacy: Towards a unifying theory of behavioral change. Psychological Review. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: The Exercise of Control. New York: Freeman; 1997. [Google Scholar]
- Bandura A, Barbaranelli C, Caprara GV, Pastorelli C. Self-efficacy beliefs as shapers of children’s aspirations and career trajectories. Child Development. 2001;72:187–206. doi: 10.1111/1467-8624.00273. [DOI] [PubMed] [Google Scholar]
- Cardenas V, Abel S, Bowie CR, Tiznado D, Depp CA, Patterson TL, Jeste DV, Mausbach BT. When functional capacity and real-world functioning converge: the role of self-efficacy. Schizophrenia Bulletin. 2012 doi: 10.1093/schbul/sbs004. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi J, Fiszdon J, Medalia A. Expectancy-value theory in a persistence of a learning effects in schizophrenia: role of task value and perceived competency. Schizophrenia Bulletin. 2010;36:957–965. doi: 10.1093/schbul/sbq078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi J, Medalia A. Intrinsic motivation and learning in a schizophrenia-spectrum sample. Schizophrenia Research. 2010;118:12–19. doi: 10.1016/j.schres.2009.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delis DC, Kramer JH, Kaplan E, Ober BA. CVLT-II. The Psychological Corporation; New York: 2000. [Google Scholar]
- Eccles JS, Wigfield A. Motivational beliefs values and goals. Annual Review of Psychology. 2002;53:109–132. doi: 10.1146/annurev.psych.53.100901.135153. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders—Patient Edition (SCID-I/P, Version 2.0) Biometrics Research Department, New York State Psychiatric Institute; New York: 1995. [Google Scholar]
- Grant PM, Beck AT. Defeatist beliefs as a mediator of cognitive impairment, negative symptoms and functioning in schizophrenia. Schizophrenia Bulletin. 2009;35:798–806. doi: 10.1093/schbul/sbn008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green MF, Kern RS, Braff D, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: Are we measuring the right stuff? Schizophrenia Bulletin. 2000;26(1):119–136. doi: 10.1093/oxfordjournals.schbul.a033430. [DOI] [PubMed] [Google Scholar]
- Green MF, Kern RS, Heaton RK. Longitudinal studies of cognition and functional outcome schizophrenia: implications for MATRICS. Schizophrenia Research. 2004;72(1):41–51. doi: 10.1016/j.schres.2004.09.009. [DOI] [PubMed] [Google Scholar]
- Hayes AF. PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling [White paper] 2012 Retrieved from http://www.afhayes.com/public/process2012.pdf.
- Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale for schizophrenia. Schizophrenia Bulletin. 1987;13:261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- Kurtz MM, Moberg PJ, Ragland JD, Gur RC, Gur RE. Symptoms versus neurocognitive test performance as predictors of functional status; A 1- and 4-year prospective study. Schizophrenia Bulletin. 2005;31:167–174. doi: 10.1093/schbul/sbi004. [DOI] [PubMed] [Google Scholar]
- Kurtz MM, Ragland JD, Moberg PJ, Gur RC. The Penn Conditional Exclusion Test: a new measure of executive-function with alternate forms of repeat administration. Archives of Clinical Neuropsychology. 2004;19(2):191–201. doi: 10.1016/S0887-6177(03)00003-9. [DOI] [PubMed] [Google Scholar]
- Mausbach BT, Depp CA, Bowie CR. Sensitivity and specificity of the UCSD Performance-based Skills Assessment (UPSA-B) for identifying functional milestones in schizophrenia. Schozophr Res. 2011;132:165–170. doi: 10.1016/j.schres.2011.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mausbach BT, Harvey PD, Goldman SR, Jeste DV, Patterson TL. Development of a brief scale of everyday functioning in persons with serrious mental illness. Schizophr Bull. 2007;33:1364–1372. doi: 10.1093/schbul/sbm014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mausbach BT, Depp CA, Cardenas V, Jeste DV, Patterson TL. Relationship between functional capacity and community responsibility in patients with schizophrenia: differences between independent and assisted living sittings. Community Mental Health J. 2008;44:385–391. doi: 10.1007/s10597-008-9141-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDermott BE. Development of an instrument for assessing self-efficacy in schizophrenic spectrum disorders. J Clin Psychol. 1986;51:320–331. [PubMed] [Google Scholar]
- Muller D, Yzerbyt VY, Judd CM. When moderation is mediated and mediation is moderated. Journal of Personality and Social Psychology. 2005;89:852–863. doi: 10.1037/0022-3514.89.6.852. [DOI] [PubMed] [Google Scholar]
- Nuechterlein KH, Barch DM, Gold JM, Goldberg TE, Green MF, Heaton RK. Identification of separable factors in schizophrenia. Schizophrenia Research. 2004;72:29–39. doi: 10.1016/j.schres.2004.09.007. [DOI] [PubMed] [Google Scholar]
- Patterson TL, Goldman S, McKibbin CL, Hughs R, Jeste DV. UCSD Performance-Based Skills Assessment: Development of a new measure of everyday functioning for severely mental ill adults. Schizophr Bull 2001. 2001;27:235–245. doi: 10.1093/oxfordjournals.schbul.a006870. [DOI] [PubMed] [Google Scholar]
- Patterson TL, Moscona S, McKibbin CL, Favidson K, Jeste DV. Social skills performance assessment among older patients with schizophrenia. Schizophr Bull. 2001;21(2):269–281. doi: 10.1016/s0920-9964(00)00109-2. [DOI] [PubMed] [Google Scholar]
- Pratt SI, Mueser KT, Smith TE, Lu W. Self-efficacy and psychosocial functioning in schizophrenia: A meditational analysis. Schizophrenia Research. 2005;78:187–197. doi: 10.1016/j.schres.2005.02.014. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Rucker DD, Hayes AF. Assessing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate Behavioral Research. 2007;42:185–227. doi: 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- Rabinowitz J, Levine SZ, Garibaldi G, Bugarski-Kirola D, Berardo CG, Kapur S. Negative symptoms have greater impact than positive symptoms on functioning: analysis of CATIE data. Schizophrenia Research. 2012;37:147–150. doi: 10.1016/j.schres.2012.01.015. [DOI] [PubMed] [Google Scholar]
- Schmidt SJ, Mueller DR, Roder V. Social cognition as a mediator variable between neurocognition and functional outcome: empirical review and new results by structural equation modeling. Schizophrenia Bulletin. 2011;37:S41–54. doi: 10.1093/schbul/sbr079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolman AW, Kurtz MM. Neurocognitive predictors of objective and subjective quality of life in individuals with schizophrenia: a meta-analytic investigation. Schizophrenia Bulletin. 2012;38:304–315. doi: 10.1093/schbul/sbq077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventura J, Hellemann GS, Thames AD, Koellner V, Nuechterlein K. Symptoms as mediators of the relationship between neurocognition and functional outcome in schizophrenia: A meta-analysis. Schizophrenia Research. 2009;113:189–199. doi: 10.1016/j.schres.2009.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. WAIS-III Manual. The Psychological Corporation; New York: 1997. [Google Scholar]
- Wechsler D. WAIS-IV Manual. The Psychological Corporation; New York: 2008. [Google Scholar]


