Abstract
Limited funding for medical technology, low levels of education and poor infrastructure for delivering and maintaining technology severely limit medical decision support in low- and middle-income countries. Perinatal and maternal mortality is of particular concern with millions dying every year from potentially treatable conditions.
Guatemala has one of the worst maternal mortality ratios, the highest incidence of intrauterine growth restriction (IUGR), and one of the lowest gross national incomes per capita within Latin America. To address the lack of decision support in rural Guatemala, a smartphone-based system is proposed including peripheral sensors, such as a handheld Doppler for the identification of fetal compromise.
Designed for use by illiterate birth attendants, the system uses pictograms, audio guidance, local and cloud processing, SMS alerts and voice calling. The initial prototype was evaluated on 22 women in highland Guatemala. Results were fed back into the refinement of the system, currently undergoing RCT evaluation.
A. Introduction and background
While advances in medical care have reduced mortality rates across the globe, perinatal mortality has decreased at a significantly slower pace. This is particularly true of low- and middle-income countries (LMICs), which contribute by far the largest proportion of both perinatal and maternal deaths annually. Perinatal mortality includes both fetal death in utero (stillbirth) and neonatal death in the first seven days of life. Figure 1 illustrates the prenatal development stages, including a definition of the perinatal period.
Fig. 1.
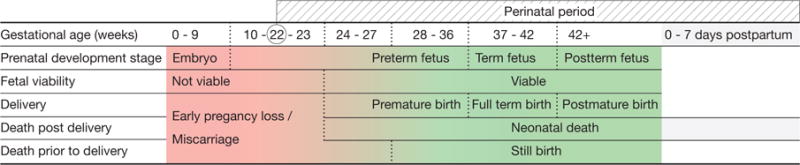
The prenatal development stages, including commonly used definitions for fetal and early neonatal death, and the perinatal period [1].
Maternal and child health has long been recognised as a key concern by the international development and healthcare community, as reflected in two of the eight United Nation’s Millennium Development Goals (MDGs) [2], which were formulated in 2000 to drastically reduce maternal and child mortality by 2015. Significant progress could be reported in lowering especially child mortality rates over the past 15 years, however targets have not been met with a substantial disparity pertaining between lower resource settings and developed regions, as well as rural and urban areas. The recent report on MDG outcomes [3] estimated maternal mortality to be 14 times higher in developing regions with only half of pregnant women receiving the recommended number of antenatal visits. Furthermore only 56% of births are attended by skilled healthcare workers in rural communities, as compared to 87% in urban areas.
By far the slowest decline in mortality rates was observed for in utero deaths and neonates in their first days of life [4], [5]. Global mortality estimates for 2009 were 2.6 million stillbirths and 2.8 million early neonatal deaths (within the first week of life) among 133 million babies born alive each year [1]. Birth remains an event of extreme risk accounting for 40% of perinatal and maternal deaths (of a total of over 287 000 worldwide [1]). Figure 2 summarises recent global estimates of maternal and perinatal mortality rates, assigned to the respective stages of pregnancy and the post-partum period. Close to 99% of those deaths occur in developing countries [1]. Estimates especially in the perinatal period are prone to inaccuracy due to discrepancies in death records at country and regional levels alike [6]. However, estimates do highlight that risk is prevalent along the continuum of pregnancy and the post-partum period, which has often been neglected.
Fig. 2.
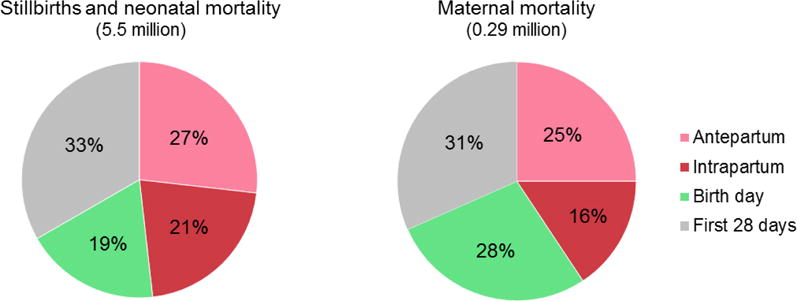
Maternal, fetal and early neonatal mortality rates as estimated globally, adapted from [4]. The majority of both maternal and perinatal deaths (close to 99%) occur in developing regions [1]. Perinatal estimates in particular are susceptible to error given discrepancies in death records [6], nevertheless they emphasise the high risk prevalent along the continuum of pregnancy and the often neglected post-partum period.
The little attention that has been given to perinatal compared to child (under 5) and maternal mortality may to some extent be attributed to these substantial discrepancies in registration practices of birth and death including disagreement in definitions of terms such as ‘stillbirth’ [4], [6]. This has resulted in a lack of reliable data to act upon. Relevant data required to effectively address perinatal risk includes harmonised records of fetal and neonatal deaths, information on where deaths occur geographically and with respect to location (in a healthcare facility or at home), in which stage of pregnancy they occur, and their causes if known [7].
In developed regions the steep reduction of perinatal deaths in the past century is commonly attributed to the advances in skilled birth support, medical technologies and specialised healthcare infrastructure [6]. All of those are often amiss in low-resource and particularly rural regions. Interdependent factors, such as a lack of skilled medical personnel, sparse coverage of specialised care in remote areas or the cost of healthcare provision all play a role in the slow progress. Among the main direct and indirect causes of perinatal death reported in 2015 were preterm birth (16%), intrapartum related complications (11%) and sepsis (7%) [5]. The largest risk factor, however, for over 80% of neonatal deaths is low birth weight [4]. Babies with low birth weight are either born pre-term, small-for-gestational age (SGA), or both. Some term SGA babies are considered constitutionally small and might develop normally, others are affected by intra-uterine growth restriction (IUGR), a pathological slow-down in growth preventing the fetus from reaching its full growth potential. The IUGR prevalence has been estimated at 11%, six times higher than in developed regions [8], [9]. Small-sized babies are equally at substantial risk of post-neonatal mortality and a high morbidity rate in later life [4].
To alleviate the burden of perinatal mortality, improving birth outcomes and registration have been named as high priorities in the post-2015 development agenda [4], [6], [10], and a particular focus has been suggested on low-birth weight and a reduction in fetal growth-restriction [4], [8].
One approach to contribute to the prevention of avoidable deaths and disabilities is accessible perinatal screening of mother and baby, and appropriate medical referral.
Fetal wellbeing is most commonly assessed by monitoring of the fetal heart rhythm [11], with clinicians aiming to identify non-reassuring fetal status to initiate an appropriate and timely intervention [12]. A low-cost method to record this signal is by hand-held (1D) Doppler, a modality widely used by healthcare professionals (primarily midwives) world-wide. Several consumer models have recently entered the market, offering mothers-to-be a device to listen to the fetal heart beat at home. The clinical utility of such devices for personal use is debatable as those monitors typically do not offer any form of analysis. However, this development means that extremely low-cost transducers, which can easily be adapted to connect to recording and processing devices such as smart phones, are available for purchase. This has motivated the use of such transducers and the testing of its appropriateness for risk screening in low-resource environments. The objective of the mHealth perinatal monitoring system is to enable the recording of fetal cardiac activity onto a mobile phone for further processing and fetal risk assessment. In its wider context the system was also conceived at a platform for a more comprehensive maternal-fetal health assessment. The prototype therefore includes not only a Doppler sensor, but also a pulse oximeter interfacing with the smart phone (see figure 3 for the prototype in use).
Fig. 3.
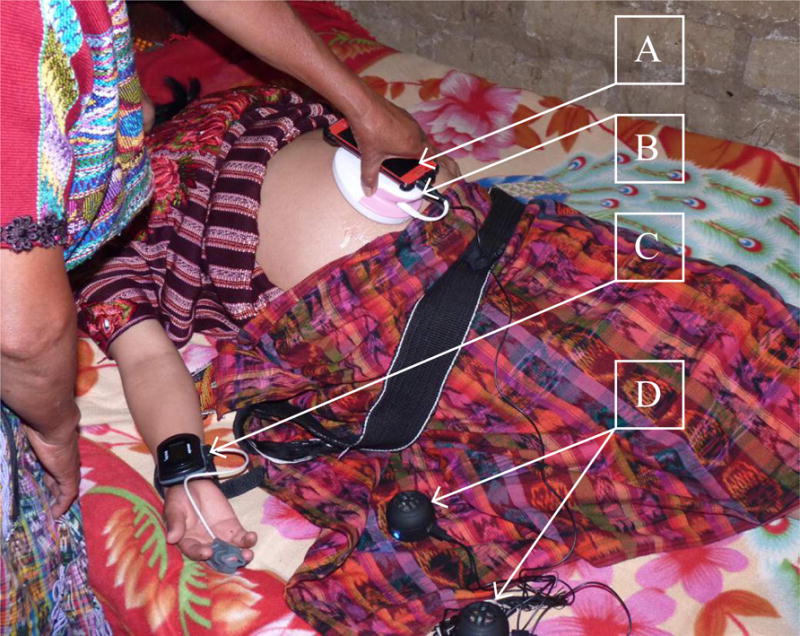
Traditional birth attendant with prototype equipment for recording fetal heart activity in a remote village in the Guatemalan highlands. The separate components: A: Smart phone, B: Low-cost 1D Doppler, C: Pulse oximeter D: Speakers to enable both healthcare worker and patient to listen to the fetal cardiac signal.
In order to achieve set Millennium Development Goals (MDGs) [2] and further improve maternal and perinatal health it has been acknowledged that information and communication technologies (ICTs) have an increasingly important role to play [13]. The rapidly increasing coverage of smart mobile devices not only in developed regions, but to an astonishing extent in the world’s rural communities and settings where other technologies remain scarce, and ICTs’ promising potential in healthcare delivery, have spurred the development of mHealth solutions [14]. Key challenges of perinatal mHealth solutions for lower resource environments include not only cost, but also the socio-cultural context and the formal or informal healthcare systems in place. It has been highlighted that, for a successful implementation of mHealth initiatives, their integration into the existing infrastructure, supporting and complementing resources available is crucial [15]. This includes working with frontline community healthcare workers to ensure ownership and committed participation [13].
The successful development of any healthcare intervention requires the early involvement of existing care providers and relevant stakeholders. The non-governmental organisation Wuqu’ Kawoq — Maya Health Alliance1 was established in 2007 to provide healthcare solutions for Guatemala’s poor, under-served and mostly indigenous communities. Wuqu’ Kawoq has a well established midwife program aiming to empower traditional birth attendants to improve care delivery for expectant mothers and newborns in their communities. Wuqu’ Kawoq was therefore chosen as an excellent partner in the effort to develop and evaluate the appropriateness of anticipated mHealth perinatal monitoring concept presented in this article.
Guatemala is likewise an excellent case study for the complexity of the health system problems that underlie high perinatal morbidity and mortality. Health statistics for 2013 estimated 49% of all births to occur in the community as supposed to facilities with only 52% attended by a skilled healthcare worker; the percentage of low birth weight babies (<2500 g) is high at 11% and the estimated adjusted maternal mortality ratio of 140 (maternal deaths per 100 000 live births) is among the highest in Central America [16] (see figure 4 for population and health statistics). Guatemala has not met MDG4 or MDG5 by the end of 2015.
Fig. 4.

The most recent (2013) population [18] and health statistics [17] for the Chimaltenango region in Guatemala, Wuqu’ Kawoq’s primary area of care provision.
In comparison, most developed nations have reported maternal mortality ratios of 10 or less [7] and a low birth weight percentage of under 7% [16]. The relationship between gross national income per capita (GNI) and low birth weight as well as neonatal mortality is shown in figure 5. A significant discrepancy persists in skilled birth attendance between urban (77%) and rural (37%) communities as well as the poorest and richest 20% of the population (20% and 95% respectively) [16].
Fig. 5.
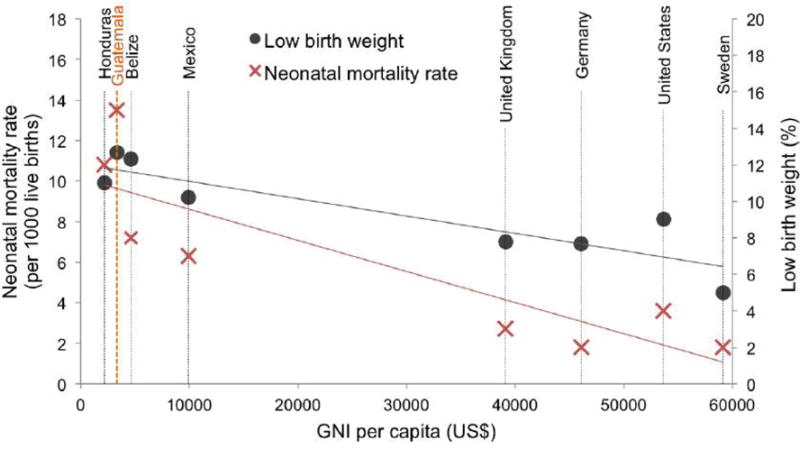
The percentage of low birth weight (<2500g) and the rate of neonatal mortality plotted against the gross national income per capita, comparing Guatemala with its neighbouring countries and examples of developed nations. The 2013 country statistics used to produce this graph can be found in [16].
In 2010 Guatemala introduced policies to promote maternal and neonatal health requiring authorities to provide basic services for women throughout pregnancy and the neonatal period, and initiatives such as obstetrics and paediatric residency programs to increase the availability of skilled staff [17]. In a recent study [17] researchers analysed the progress in reducing maternal, fetal and neonatal mortality rates in the Guatemalan state of Chimaltenango, which is Wuqu’ Kawoq’s primary area of service delivery. They found maternal mortality lowered from 134 per 100 000 live births in 2010 to 113 in 2013, both stillbirth and perinatal rates significantly decreased from 22.0 per 1000 births to 16.7 and from 43.9 to 31.6 respectively. Notable were the differences in outcomes for facility and home deliveries, illustrated in figure 6. Whereas perinatal mortality could be reduced by 41.4% in facilities, it only reduced by 21.4% for home births over the same period. The same applies to stillbirths with a reduction of 39.0% and only 17.6% respectively.
Fig. 6.
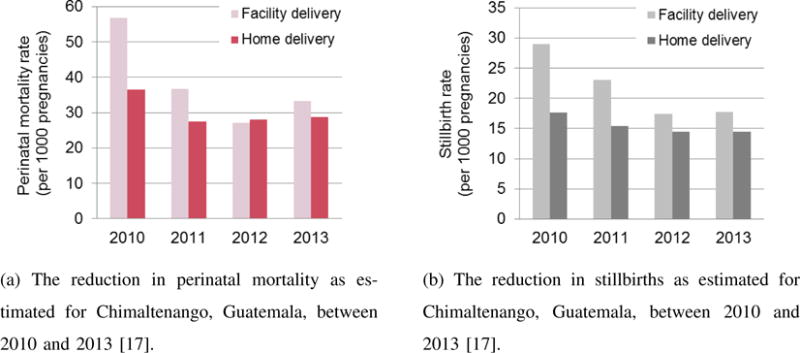
Both perinatal mortality (a) and stillbirths (b) decreased with between 2010 and 2013, coinciding with policy changes to improve access to obstetric care [17]. Whereas mortality could be reduced significantly in healthcare facilities, a slower decrease was noted for home births.
Given the discrepancy in mortality reduction dependent on birth location, researchers have advocated to phase-out community deliveries led by traditional birth attendants [17], which account for at least 59% of births in rural areas of Guatemala [19]. Birth attendants however, known as ‘comadronas’, are an integral part of indigenous communities, not only as providers of reproductive care but also as trusted leaders [17]. This may be one of the reasons why expecting women in the rural highlands often choose delivery at home attended by a traditional birth attendant over delivery at a healthcare facility [17], [20]. Equally important are cultural differences, language barriers and high illiteracy rates that deter Mayan mothers from accessing the formal healthcare system. An alternative approach taken by Wuqu’ Kawoq is to integrate comadronas into the care delivery model. This approach includes culturally appropriate training to traditional birth attendants and education for women in their own language addressing skill and knowledge gaps, to support solutions that empower comadronas to assess perinatal risk early reducing delays in advice seeking, and to include comadronas into the referral process strengthening the linkage to formal healthcare services.
I. The iterative design process
To test the feasibility and ultimately the potential impact of the mHealth intervention proposed in this article, the early involvement of target user communities is essential. The non-profit organisation Wuqu’ Kawoq works closely with traditional birth attendants as part of their programme delivering primary healthcare in an under-served rural and predominantly indigenous region of Guatemala. The development of the mHealth application and overall healthcare intervention was designed as an iterative process and is being executed in collaboration with Wuqu’ Kawoq’s medical staff, their extensive network of comadronas and their patients.
The development process including all stages completed or in progress is summarised in figure 7. The first prototype was piloted with comadronas in order to assess the acceptability of such intervention by both healthcare worker and patient, and to evaluate the usability and technical feasibility of such system. Based on collected insights and by closely working with Wuqu’ Kawoq’s team and traditional birth attendants, the mobile application was extended in its functionality and an appropriate user interface developed. Both feasibility testing and system refinement are discussed in this article. The project is currently entering its evaluation phase. A proof of concept study has been designed and is supported by a National Institutes of Health (NIH) grant to assess the impact of the mobile application and overall healthcare intervention. An overview of this study concludes this article.
Fig. 7.
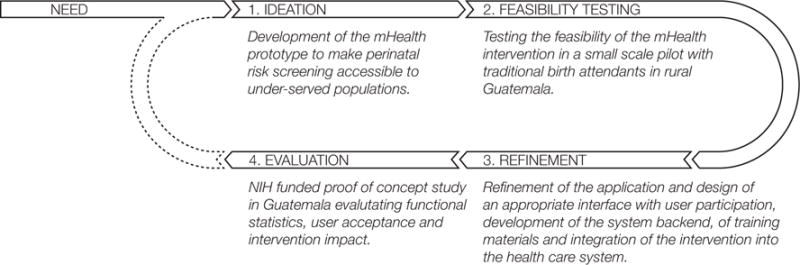
The iterative design process followed in the development of the mHealth perinatal monitoring intervention.
II. Feasibility testing
The feasibility assessment was designed to evaluate whether frontline healthcare workers could operate the study equipment (1D fetal Doppler, pulse oximeter and recording application) and record signals successfully using a smart phone. The feasibility study also set out to gauge user need and to assess the acceptability by both healthcare provider and patient to inform subsequent system refinement and the proof-of-concept pilot, as well as to determine training requirements. The study protocol titled “Preliminary evaluation of a mobile health perinatal monitoring system” was approved by the Wuqu’ Kawoq Institutional Review Board (WK-2014-003). Patient consent was recorded by an accompanying research physician or health centre personnel not directly involved in the respective patient’s antenatal care provision.
A. Data collection
Recording staff included nine healthcare workers drawn from the Wuqu’ Kawoq network of perinatal care providers: four traditional birth attendants (TBAs), two physicians (PH), one nurse (N), one healthcare worker (HCW) specialising in women’s health and one health promoter (HP) (Participant information is summarised in table I). They were instructed to attach the pulse oximeter to the mother’s wrist and index finger, start the recording application, locate the fetal heart beat with the Doppler (using ultrasound gel for better contact with the skin) and to record the cardiac activity for a minimum of ten minutes. They were then asked to save the recording, switch off and remove all devices (see figure 3). An alternative set-up was trialled with staff that had some degree of experience in the use of fetal Doppler. Those staff were asked to position the Doppler probe on the abdomen with an elastic belt and start recording thereafter. This was to assess the option of continuous monitoring for advanced cardiac signal analysis, such as screening for IUGR risk. If necessary, researchers provided guidance during the recording. Participants were given headphones or speakers to listen to the fetal cardiac activity while recording. No analysis of the fetal cardiac signal was provided at this stage of the investigation. Recording staff were accompanied to their antenatal consultations over a three week period. A total of 22 pregnant women were enrolled with an average age of 26 years (Range: 16 to 37 years), carrying a fetus with an average gestational age of 27 weeks 3 days (Range: 6 weeks 5 days to 39 weeks 6 days). All pregnancies were singleton pregnancies with no known fetal complications. Recordings were collected during five home visits and in four different community health centres, where 25 unique staff-patient interactions were observed (three women were recorded twice by different staff) and 28 recording attempts. The average recording length was 11 minutes and 10 seconds (±3m49s).
TABLE I.
Participants were Wuqu’ Kawoq staff and healthcare workers recruited from Wuqu’ Kawoq’s network with varying levels of education and experience working in perinatal care. The total number of patients recorded by each participant was dependent on their current patient load. Recordings were observed and classified into instances requiring no support, minimum support (verbal) or extensive support (hands-on) support by study staff.
| Participants* | PH01 | PH02 | N01 | HCW01 | TBA01 | TBA02 | TBA03 | TBA04 | HP01 |
|---|---|---|---|---|---|---|---|---|---|
| Experience (yrs) | 2 | 3 | 1 | 15 | 15 | 25 | <1 | 25 | <1 |
|
| |||||||||
| NRecordings | 6 | 5 | 5 | 2 | 1 | 2 | 1 | 2 | 1 |
| NRec no support | 2 | 3 | 2 | 1 | 0 | 0 | 0 | 0 | 0 |
| NRec min support | 4 | 2 | 3 | 1 | 0 | 0 | 0 | 0 | 1 |
| NRec ext support | 0 | 0 | 0 | 0 | 1 | 2 | 1 | 2 | 0 |
PH = Physician, N = Nurse, HCW = Healthcare worker, TBA = Traditional birth attendant, HP = Health promoter
The number of participating staff and birth attendants was considered acceptable to keep logistics manageable at this stage of the development process whilst covering varying degrees of medical training and experience in the use of mobile and monitoring technologies. The number of patients enrolled was governed by the participants’ work load and the objective to include a representative range of patient age and location (remote and more accessible villages).
B. Evaluation tools
To evaluate whether Wuqu’ Kawoq’s antenatal care providers could successfully handle the study equipment for physiological signal capture, both qualitative and quantitative research tools were employed, assessing data quality and implementation realities. Participating staff were invited to provide feedback rating the potential utility of such a system in their practice and the ease-of-use of the individual system components on a Likert scale. Each visit and recording procedure was also observed in detail by an accompanying researcher to gain insights into the work environment of the target users, their routine consultations and in particular their interaction with the study equipment. Further quantitative metrics collected were the success rate of recording all signals onto the phone concurrently and the success rate of staff identifying fetal heart sounds. The quality of Doppler recordings was furthermore reviewed using signal quality metrics developed by the authors. The reader is referred to Stroux al. [21], [22] for specific details of these metrics.
C. Feasibility testing outcomes
1) Device use
Five out of the nine staff required no or minimal support (occasional oral instructions or reminders) when setting up the prototype system (attaching pulse oximeter, switching on Doppler probe and starting the recording application). In only 21% of the recording instances (consultations) additional instructions had to be provided when starting the Doppler probe, and in 24% when attaching and starting the pulse oximeter. Navigating the smart phone application to start recording proved more difficult, required guidance in 40% of all cases. In total, 25 recordings were successfully started. In 16 cases staff located fetal cardiac activity with ease, in seven with some difficulty, while in two recordings no heart sounds could be found (this was however anticipated, as the gestational ages were 6 weeks 5 days and 10 weeks respectively). In 48% of all cases the fetal cardiac signal could be well maintained over the duration of the recording. A number of participants were not aware whether they had recorded cardiac activity from the placenta or the fetal heart directly. Similarly two participants seemed to not notice maternal interference and did not attempt to find a clearer signal. Several participants appeared not to be conscious of the differences in signal quality and the clarity in heart sound that could be achieved.
Seven out of the nine staff could end the procedure with ease. There was no difference in the number of sessions requiring support in navigating the app (saving the signals) and those requiring help switching off and removing the devices. In summary, eight recordings required no intervention, eleven minimal guidance (i.e. oral instructions), whereas six demanded hands-on support (i.e. entering the patient ID into the smart phone). Required levels of support are summarised in table I. Staff participants with experience in handling similar devices were generally more at ease. This was particularly true for operating the smart phone but also applied to the use of the Doppler probe. The five out of nine participants who were familiar with operating smart phones, were all staff with a higher educational level or of younger age. In total, participating staff collected 24 successful recordings (all signals recorded for desired length of time), in three instances a second recording attempt was required as the pulse oximeter communication had timed out (the application was started before the pulse oximeter), one recording failed as it was accidentally saved and the application exited too early. All staff managed to identify and record fetal heart activity, only two recordings did not contain any heart sounds, however this was expected due to the gestational age of the fetuses (<12 weeks). Four out of nine staff participants appeared to be capable of handling all devices in the system with the very basic training provided by the researchers.
2) Staff and patient response
All pregnant women approached for participation agreed to be enrolled. Neither staff nor patients voiced concerns over the use of the study equipment prior, during or after recording. All recording staff appeared comfortable using the study devices on their patients, and, even if unfamiliar with their use, applied them with confidence and no noticeable hesitation. The six staff who provided written feedback found all system components easy to operate and independently agreed on the potential benefit of such system.
3) Doppler signal quality assessment
The signal quality of the fetal cardiac recordings was assessed using a logistic regression based classifier developed as part of this project. In addition to the signal’s quality index (SQI) assigned by the algorithm, signal segments were regarded as poor if the heart rate computed by autocorrelation was out of a rhythm’s normal range (110–180 bpm [23]). SQI and heart rate were computed for 3.75 epochs at 0.33 Hz sampling frequency. An example recording including assigned quality score is shown in figure 8.
Fig. 8.
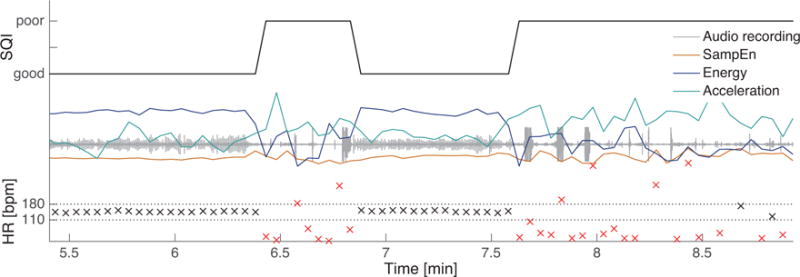
An example showing an original recording segment, the computed quality features (the signal’s sample entropy, energy and concurrently recorded phone acceleration), the associated heart rate, and assigned quality score.
Of the 4 hours and 16 minutes recorded (probe in contact with abdomen) 41% were found to be of good and 59% to be of poor (including intermediate) quality. The number of years working in antenatal care showed not to be positively correlated with an increase in the quality of data collected. On the contrary, quality appeared to decrease for longer serving staff, which may be attributed to their age and lack of exposure to technology of similar kind (figure 9). The percentage of high quality data was greater for staff informally trained in their profession compared to university educated participants. Doppler signals collected by lay midwives and healthcare workers (N recordings = 9) contained 47% good and 53% poor quality, signals recorded by the nurse and clinicians (N recordings = 13) 37% and 63% respectively. Figure 10 however illustrates how gestational age influences the ease with which good quality data can be collected. The proportion of good quality data in the signal increases substantially towards the third trimester of gestation. The difference in the proportion of high quality recordings between informally and formally educated participants can likely be attributed to the greater number of early gestation patients recorded by the latter group.
Fig. 9.
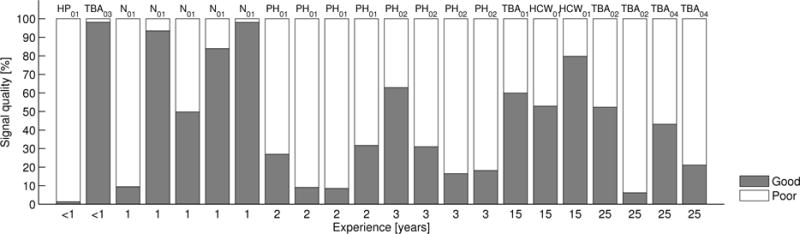
The proportion of good and poor quality in recordings sorted according to the staff’s experience in antenatal care. (PH = Physician, N = Nurse, HCW = Healthcare worker, TBA = Traditional birth attendant, HP = Health promoter)
Fig. 10.
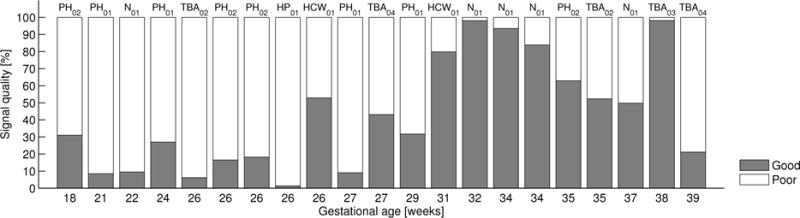
The proportion of good and poor quality in recordings sorted according to gestational age. (PH = Physician, N = Nurse, HCW = Healthcare worker, TBA = Traditional birth attendant, HP = Health promoter)
The percentages of signal quality are comparable to those of data collected by healthcare professionals in the UK using the same prototype (N patients = 17) [21], [22]. Applying the SQI algorithm, 55% of the total dataset was classified as poor, 45% as of good quality. The algorithm may be considered conservative as signal segments labelled ‘poor’ can contain data of intermediate quality, which may explain the rather low percentage of good quality signal. What is important to note however is that there is no significant discrepancy between data collected in the hospital environment compared to data recorded in the field.
D. Discussion
Three key areas for successful fetal cardiac signal recording have emerged, the ability to operate the equipment provided, the clinical knowledge to identify and to target the best possible signal, and the degree of willingness to employ such technology. The technology-related difficulties participants experienced were largely related to the participants’ educational level (including a very high illiteracy rate amongst traditional birth attendants) and experience in handling similar equipment. As the instructions provided by the study team prior to the recording sessions were minimal and did not consider the various skill levels of the participants, several of the observed challenges could to some extent be attributed to a lack of appropriate training and guidance material.
It is noteworthy that despite only rudimentary instructions, all participants were able to successfully locate the fetal cardiac signal and complete a recording.
Participants with formal clinical education (physicians and nurse) who had used 1D Doppler at least occasionally in their practice had the ability not only to operate the device but also to understand the cardiac signal obtained, its origin, its susceptibility to maternal interference and the varying degrees of quality. Participants not trained in the use of similar devices, however, quickly developed a grasp of the technology and were able to successfully handle most recording steps with the limited instructions provided. Even though differences between formal and informally trained healthcare providers in the ease of handling devices were apparent, the educational level did not appear to impact the quality of data collected.
Observation confirmed that 1D Doppler can be operated with minimal training only, suggesting that wider dissemination is possible. To record good quality data early on in gestation appeared difficult to both groups and will require additional training in locating, identifying and maintaining an adequate signal.
Participating staff, independent of education or experience level, were generally comfortable using the study equipment on their patients and demonstrated a high degree of confidence. Similarly all patients agreed to participate and appeared at ease throughout the recordings. These observations allow for the assumption of a well-functioning doctor/healthcare worker-patient relationship, considered essential for high quality healthcare delivery.
E. Conclusion and system implications
All participants were able to record and to identify fetal heart sounds with only six recordings (out of 25) requiring hands-on support of study staff. The high rate of successful recordings, with only minimal instructions provided prior to each patient encounter, in combination with the positive participant feedback, were encouraging indicators that the introduction and adoption of such equipment in the communities visited is feasible.
Several areas for improvement were identified during the feasibility testing. The familiarity with the technology and the clinical understanding of the physiological signals and their characteristics, the system’s usability and ultimately signal quality, could all be improved by a combination of educational measures such as training and training manuals, an appropriate application interface and built-in guidance on the phone with real time quality feedback.
The implementation of signal analysis capabilities, such as the discrimination of maternal from fetal cardiac signal by comparing the pulse oximeter to the ultrasound measure, would provide real time quality improvement and reduce false readings. (This is particularly important, since a pregnant woman can have an elevated heart rate, which may seem like a normal fetal heart rate and mask any abnormalities. Conversely, a low maternal heart rate might lead to a false alarm if mistaken for the fetus.) In addition, user feedback throughout the intervention, such as the acknowledgement of successful recordings, may prevent unnecessary loss of data. In the next section, improvements and their implementation are discussed.
III. System refinement and intervention design
The perinatal monitoring system is anticipated to be used primarily by front-line birth attendants who are typically informally educated in their profession, often illiterate and currently do not use monitoring technology in their practice. By bringing together engineers2, physicians3, public health specialists and medical anthropologists4, and working with the local network of healthcare workers, the aim was to create a system suited to the existing healthcare infrastructure and appropriate to the needs of the local population. The system was designed with the ultimate goal of becoming an intuitive tool for data collection, improving the diagnostic capabilities of practicing midwives and assisting with timely and accurate referral. Towards this goal three areas of system refinement and system extension were identified for the next stage of development:
-
Mobile application
Continuum of care: Extension of the application from prenatal assessment only, to the inclusion of intrapartum and postnatal health checks.
Comprehensive health checks: Inclusion of maternal blood pressure measurements and checks for pregnancy-related complications into the application work flow.
User interface (UI): The design of a user-centred mobile application interface, to be inclusive of an illiterate user group.
Signal analysis: Implementation of heart rate analysis including discrimination between the maternal and fetal rhythm.
Emergency response: Implementation of logic to trigger calls to higher level care staff in case of detected emergencies.
-
Integration into medical records
Data consolidation: Automated upload of recorded signals, patient and health information to Wuqu’ Kawoq’s medical record system, openMRS, a globally adopted open source electronic medical record (EMR) system.
-
User training and education
User manuals: The development of on-phone user manuals, inclusive of an illiterate user group.
User training: The development of training sessions, which will teach participants in the application of all devices and the appropriate clinical knowledge to enable the recording of good quality physiological signals and the assessment of complications. (The development of the training material will not be covered in this article.)
A. Mobile application design
As outlined above, the mobile application was significantly extended in its functionality. This included comprehensive health checks antenatally, during birth and postnatally, on-phone signal analysis and emergency communication. A flow diagram illustrating the application’s additional functionality is shown in figure 11.
Fig. 11.
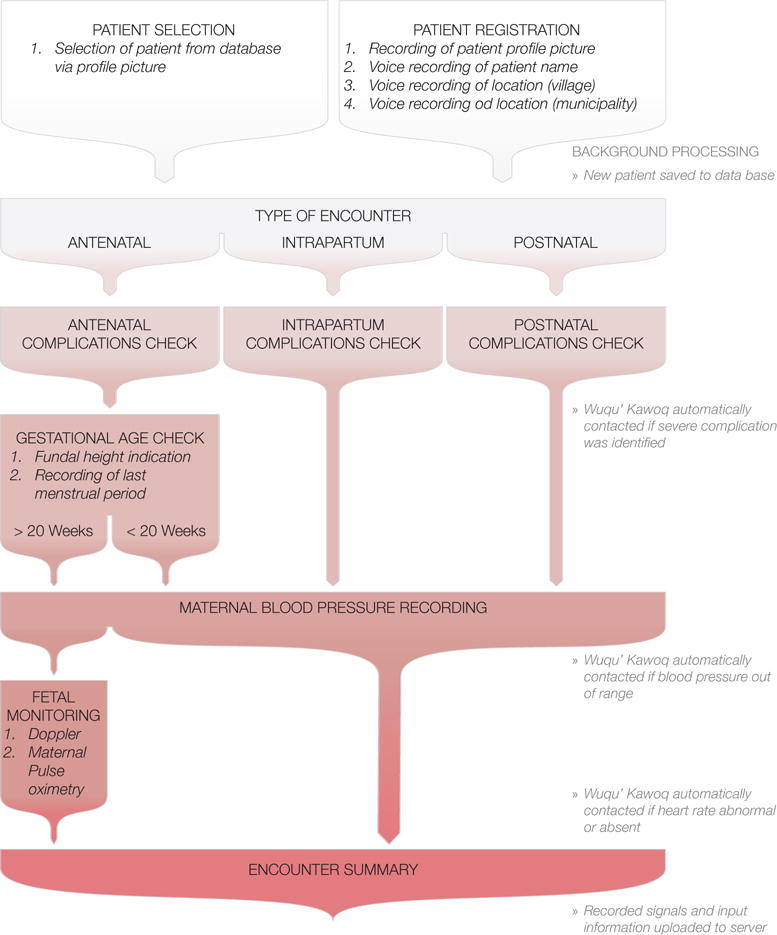
Flow diagram summarising the application steps the user is guided through during a patient visit. The application combines patient registration, guidance on and recording of pregnancy related complications and the recording of physiological signals to assess maternal and fetal wellbeing. The encounter summary and recorded signals are uploaded to Wuqu’ Kawoq’s central patient records.
1) User interface
The feasibility study revealed the limited familiarity with smart phones and confirmed the high illiteracy rate especially amongst traditional birth attendants of older age. To be maximally inclusive the application interface was therefore adapted using a combination of audio and visual instructions only, replacing any written content. Likewise the mechanism to record patient information manually was changed to voice and image capture, eliminating the need for written input. As a result, each screen presents an illustration serving as a visual clue to prompt a certain action. The illustration is accompanied by an audio playback button which provides additional audio instructions to the midwife, if required. Illustrations were drawn based on the specific use context and care was taken to guarantee their cultural relevance. All audio instructions were recorded by Wuqu’ Kawoq staff in collaboration with birth attendants in the local Mayan dialect Kaqchikel. To ensure the quality of the information being collected, midwives are asked to confirm each input, presented back to them visually or aurally (via a tick mark button), before progressing through the application. Three example application screens are shown in figure 12.
Fig. 12.
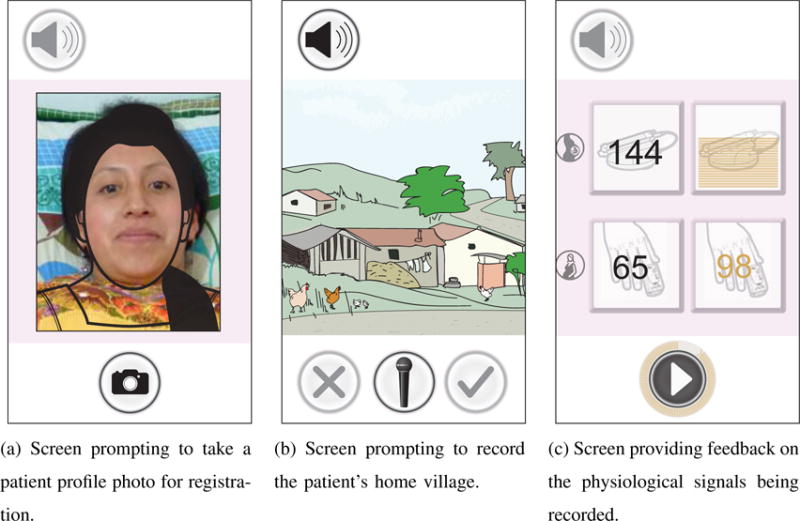
Example screens of the mobile perinatal monitoring application. (a) Patient registration: In order to register a new patient the birth attendants is prompted to take a patient profile picture, guided by a positioning frame. (b) Location information: The image provides a visual clue about the information to be collected, the loudspeaker button plays audio instructions if required, and the microphone button voice records the name of the patient’s home village provided by the midwife or patient. (c) The physiological measurements are displayed real time to indicate successful recording. Signals are recorded for 30 minutes, the time elapsed is visualised by a progress wheel. Interface illustrations were produced for the specific use context, ©Lisa Stroux 2015, released under the creative commons license attribution 4.0 international (CC BY 4.0)
2) Emergency response
To provide support to birth attendants and to initiate immediate higher level care intervention if required, the application alerts a clinician on duty should a complication be detected. A single number is programmed into the application which uses a dynamic call forwarding system to ensure the on-call doctor is always reached. Complication detection occurs in a twofold manner. Firstly the application guides the birth attendant through a number of pregnancy related complications. If abnormalities are present, those will be confirmed on the phone by the birth attendant. As with all other instructions, guidance through symptom assessment is audio and pictogram based. All visit-specific complications and the alerts they trigger are summarised in table II.
TABLE II.
The list of complications the birth attendant is guided through dependent on the type of visit. The identification of severe complications (in red) automatically triggers an emergency phone call to the clinician on duty. If there is no signal it alerts the user to it and queues an emergency SMS which can often get through as soon as even a weak or transient signal is detected. All complications are summarised at the end of the consultation and are sent via SMS to the Wuqu’ Kawoq medical record (See figure 13 for an illustration of the application’s data transfer backend.)
| Prenatal | Delivery | Postnatal |
|---|---|---|
| Seizures | Membrane rupture without labour | Seizures |
| Haemorrhage | Prolonged labour | Postpartum haemorrhage |
| Membrane rupture | Multiple pregnancy | Difficult breathing |
| Abdominal pain | Inadequate fetal position | Abdominal pain |
| Difficult breathing | Placenta praevia | Fever |
| Blurred vision | Umbilical cord around neck | Blurred vision |
| Fever | Haemorrhage | Headache |
| Edema | Placental retention | Difficult breathing (new born) |
| Headache | Previous C-section | Fever (new born) |
| Difficult breathing | Cold baby | |
| Abdominal pain | Very little baby | |
| Blurred vision | Difficult breastfeeding | |
| Fever | Umbilical infection | |
| Headache | Jaundice | |
| Edema |
Secondly, the physiological signals recorded (1D fetal Doppler, maternal pulse, maternal oxygen saturation and blood pressure) may be indicative of an underlying fetal or maternal pathology. In addition to fetal heart rate abnormalities, indicative of fetal distress, maternal blood pressure and oxygenation levels are reviewed with the primary aim of detecting pre-eclampsia [24]–[26]. The logic triggering an alert given the requisite heart rate, oxygen saturation and blood pressure is outlined in table III.
TABLE III.
The logic implemented to alert clinicians if maternal and fetal heart rate, maternal oxygen saturation and maternal blood pressure readings are abnormal. Readings that require urgent attention trigger an automated call at the end of the encounter, all other measurements are included in the encounter summary SMS to inform medical staff. Blood pressure readings are currently transmitted as photo and are therefore addressed when reviewed by medical staff after data upload; optical character recognition is being implemented for the next iteration to convert the image into numeric values automatically triggering the appropriate alert. There are currently no Bluetooth enabled blood pressure monitors approved for use in pregnancy (for the detection of pre-eclampsia).
| Measurement | Logic | Detection trigger | Indication |
|---|---|---|---|
| Heart rate [bpm] | Maternal HR ≤ 60 | SMS alert | Maternal bradycardia |
| Maternal HR ≥ 100 | SMS alert | Maternal tachycardia | |
| Fetal HR ≤ 120 | Call | Fetal bradycardia [27] | |
| Fetal HR ≥ 160 | Call | Fetal tachycardia [27] | |
|
| |||
| Oxygen saturation [%] | Oxygen ≤ 90 | Call | Maternal hypoxemia [28] |
|
| |||
| Blood pressure [mmHg] | Systolic ≤ 70 | Current: Addressed at data review | Low blood pressure |
| Future: Call | |||
| Systolic ≥ 140, diastolic ≥ 90 | Current: Addressed at data review | Mild hypertension [29] | |
| Future: SMS alert | |||
| Systolic ≥ 155, diastolic ≥ 105 | Current: Addressed at data review | Severe hypertension [29] | |
| Future: Call | |||
B. Backend infrastructure
Patient information is transmitted via voice, short message service (SMS), mobile data service (GPRS) and wireless network access (WIFI). A diagram summarising the backend infrastructure is shown in figure 13. To ensure an immediate higher level healthcare response, the phone automatically connects to the clinician on call for remote consultation if severe complications are identified (see section III-A2 and tables II and III).
Fig. 13.
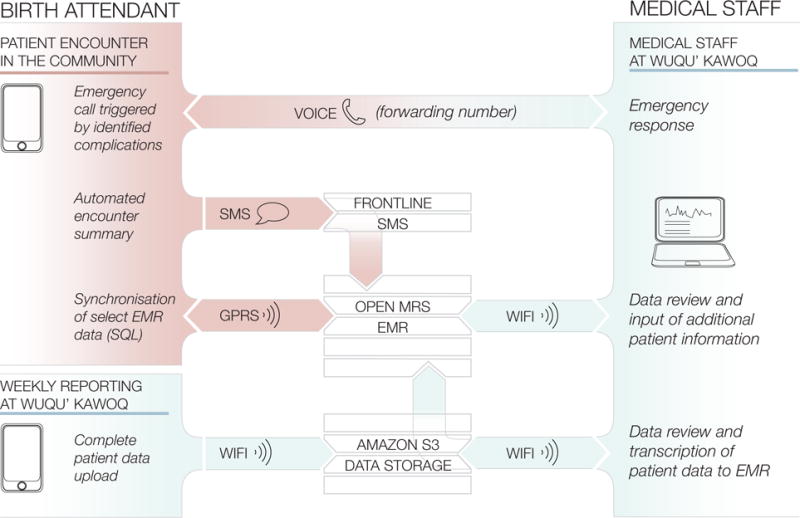
The backend infrastructure of the perinatal mobile application. Patient information is communicated via voice, text and data services dependent on urgency and connectivity. All patient information is ultimately collated in Wuqu’ Kawoq’s central electronic medical record system.
Once a patient assessment is completed, the application sends a text message via the SMS management software FrontlineSMS5 to the OpenMRS6 electronic medical record (EMR). The SMS contains coded patient information providing a summary of the patient encounter. A subset of data, such as blood pressure readings or gestational age recorded, are uploaded to the EMR when in range of GPRS transmission. This is a two-way process to ensure synchronised patient data on phone and server.
The complete set of collected patient data, including all raw signal files such as Doppler and pulse oximetry recordings, is uploaded once a week via WiFi to the data storage service Amazon S37. Wuqu’ Kawoq medical staff can review data on Amazon S3, transcribe information from Amazon S3 to the central EMR, check for missing data between data bases and review and complement patient information in the EMR.
C. User manuals
To train midwives in the use of the equipment and to allow for a review of how to apply all devices during a patient encounter, pictogram based manuals were developed and implemented on the phone. All pictograms were drawn based on photos depicting each action required when taking blood pressure, recording the fetal cardiac Doppler signal and the maternal pulse and oxygen levels. Photos were staged with the help of Wuqu’ Kawoq staff to ensure they were familiar and culturally appropriate. Before each recording action requiring the use of a sensor, the midwife has the opportunity to remind herself of the correct procedure in a step-by-step manner.
IV. System evaluation
The mHealth system described in this article is now being evaluated as part of the NIH funded study titled Mobile Health Intervention to Improve Perinatal Continuum of Care in Guatemala. The study was approved by the Wuqu’ Kawoq and Emory University institutional review boards (Wuqu’ Kawoq IRB approval number: WK-2015-001, Emory University protocol record: IRB00076231) to ensure compliance with ethical standards.
The study was designed as a step-wedge randomised control trial involving 50 traditional birth attendants in the department of Chimaltenango, and an overall enrolment of approximately 500 pregnant women and their newborns over the duration of 12 months. Initially, 25 midwives have been randomly assigned to receive the study equipment (mobile phone, 1D Doppler, pulse oximeter and automated blood pressure cuff) at the start of the project8. The remaining 25 have been provided with laminated decision support cards which mimic the logic of the phone application and use the same pictograms as are included in the mobile phone app. Each birth attendant received the same conceptual training for using the cards as the 25 midwives that receive training on the mHealth system. Equal training time was allotted to both arms of the study. In order to establish a study baseline (such as referral rates) the remaining 25 will receive the equipment with a delay of 6 months, at which point both arms of the study will be trained (or retained) in the use of the equipment. Recruitment and training is currently being performed by dedicated Wuqu’ Kawoq staff.
A. Expected study outcomes
Two primary outcomes are anticipated in this proof-of-concept study: an increased appropriate antenatal referral rate and an increase in timely evaluation of neonates, conducted by birth attendants at delivery and by higher level care staff where indicated after initial assessment. The data being collected through the mHealth-EMR system will furthermore allow for the analysis of the system’s technical efficacy and process evaluation. Clinical measures such as maternal, fetal and neonatal mortality and morbidity will also be collected, however, the study is not powered sufficiently to translate those into authoritative indicators. Participating birth attendants will be tested following training provided to assess the amount of clinical knowledge and tech-literacy gained.
Post-intervention interviews with the 50 birth attendants will be conducted to further understand their attitudes toward the mHealth-EMR system, perceptions of self-efficacy while using the system, and input for further implementation. Direct observation will also give additional insight into the ease-of-use of the system. The key process outcomes and health indicators that will be extracted from the EMR, from interviews and observation are summarised in table IV.
TABLE IV.
List of study indicators collected and anticipated outcomes analysed during the mHealth system evaluation period.
| Study indicators and outcomes |
|
|
|
|
|
|
|
|
|
TBA = Traditional birth attendant
V. Conclusion
The initial user testing provided a positive indication that introducing monitoring technology into the practice of traditional birth attendants is indeed feasible. This led to the system’s extension and refinement as described in this article, working closely with Wuqu’ Kawoq staff and representative local birth attendants. The approach of including frontline healthcare workers in the design process shows promise to not only create a system able to address healthcare shortages prevalent in the region, but a system that relates to the cultural context, maximising the chances of successful implementation and ultimately adoption.
The proof-of-concept evaluation study under way will test those assumptions and is expected to uncover additional improvements required, with respect to technology, process and usability. The mHealth intervention presented in this article takes the approach of integrating traditional birth attendants into formal care delivery. This acknowledges traditional birth attendants as a valuable part of the community, as opposed to side-stepping their services in order to achieve higher levels of facility-based care. The study will show whether this alternative approach will in fact lead to improvements in early risk detection and adequate referrals as anticipated.
At present, no reliable data covering the region of Chimaltenango is available on causes of maternal and fetal compromise, the latter of which is particularly scare. Frequent and meaningful monitoring reaching families in remote areas, together with centralised record keeping as made possible with the system described, is expected to create a richer knowledge base enabling the design of studies adequately powered to investigate the health impact of such intervention. Similarly there is no information available on referral rates to higher level care facilities initiated by traditional birth attendants. The study will establish a baseline of the birth attendants’ abilities to adequately refer with training on the assessment of complications only, and allow for comparison with referral rates by birth attendants equipped with the monitoring application and devices. The physiological signals together with other health metrics collected during the study period will support further algorithm development towards the reliable detection of pre-eclampsia, fetal distress and IUGR.
Great care has been taken to tailor the presented application interface and mHealth intervention to the specific social and cultural realities and infrastructural challenges of Guatemala and the Chimaltenango region in particular. The core components of the system including its back end and decision support are however directly transferable, and the approach to UI design and intervention implementation easily replicable, suggesting that use in other low-resource contexts is viable.
Although we will not discuss any sustainability model in detail, we note that the projected cost of the entire system (after replacing with a low cost pulse oximeter) could be sub US$50 and therefore purchased by midwives and easily amortised over the cost of many pregnancies. In order to keep the costs of the software as low as possible we will release all source code for the project under an open source license and the images developed for the app will be released under the creative commons license attribution 4.0 international (CC BY 4.0). Integration across the fractured landscape of EMRs and service providers means scaling our system on a national level may be problematic, but optimism can be found in the adoption of OpenMRS by multiple countries and organisations across the planet. By open sourcing the code, increased interoperability and a lowering of costs is perhaps far more likely.
Acknowledgments
LS acknowledges the support of the RCUK Digital Economy Programme grant number EP/G036861/1 (Oxford Centre for Doctoral Training in Healthcare Innovation) and of the Oxford Centre for Affordable Healthcare Technology. GC, PR and RHC acknowledge the support of the National Institutes of Health, the Fogarty International Center and the Eunice Kennedy Shriver National Institute of Child Health and Human Development, grant number 1R21HD084114-01 (“Mobile Health Intervention to Improve Perinatal Continuum of Care in Guatemala”). Generous sponsorship was also received from ARM through the Centre for Affordable Healthcare Technology at Kellogg College, Oxford.
Footnotes
Wuqu’ Kawoq — Maya Health Alliance, 2 calle 5–43 zona 1, Santiago Sacatepquez, Guatemala 03006, Central America. Web URL: www.wuqukawoq.org
Department of Engineering Science, University of Oxford, Oxford, UK and Department of Biomedical Informatics, Emory University, & Department of Biomedical Engineering, Georgia Institute of Technology, Atlanta, US
Maya Health Alliance Wuqu’ Kawoq, Guatemala and Harvard Medical School Boston, US
Department of Anthropology and Public Health, Agnes Scott College, Atlanta, US
FrontlineSMS is an open source desktop software that enables two-way communication to mobile handsets. Website URL: http://www.frontlinesms.com
OpenMRS is an open source software platform, which enables the design of customised medical record systems. Website URL: http://openmrs.org
Part of the Amazon Web Services (AWS), Amazon Simple Storage Service (S3) is a web-based data storage service. Website URL: https://aws.amazon.com/s3
Randomisation was constrained to balance both travel time to Wuqu’ Kawoq headquarters and age of traditional birth attendants. Participants were randomised by village to reduce interaction between arms and potential envy.
References
- 1.Maternal and perinatal health. World Health Organisation. [Online]. Available: http://www.who.int/maternal_child_adolescent/topics/maternal/maternal_perinatal/en/
- 2.Milennium Development Goals. United Nations. [Online]. Available: http://www.un.org/millenniumgoals/
- 3.The Millennium Development Goals report 2015. United Nations; [Online]. Available: http://www.un.org/millenniumgoals. [Google Scholar]
- 4.Lawn JE, Blencowe H, Oza S, You D, Lee ACC, Waiswa P, Lalli M, Bhutta Z, Barros AJD, Christian P, Mathers C, Cousens SN. Every newborn: progress, priorities, and potential beyond survival. Lancet. 2014 Jul;384(9938):189–205. doi: 10.1016/S0140-6736(14)60496-7. [DOI] [PubMed] [Google Scholar]
- 5.Tech Rep. UNICEF, World Health Organization, the World Bank Group and the United Nations; 2015. Levels & trends in child mortality. [Google Scholar]
- 6.Woods R. Long-term trends in fetal mortality: implications for developing countries. Bull World Health Organ. 2008 Jun;86(6):460–466. doi: 10.2471/BLT.07.043471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goldenberg RL, McClure EM. Maternal, fetal and neonatal mortality: lessons learned from historical changes in high income countries and their potential application to low-income countries. Maternal Health, Neonatology and Perinatology. 2015;1(1):1–10. doi: 10.1186/s40748-014-0004-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Black RE, Allen LH, Bhutta ZA, Caulfield LE, De Onis M, Ezzati M, Mathers C, Rivera J. Maternal and child undernutrition: global and regional exposures and health consequences. The lancet. 2008;371(9608):243–260. doi: 10.1016/S0140-6736(07)61690-0. [DOI] [PubMed] [Google Scholar]
- 9.de Onis M, Blssner M, Villar J. Levels and patterns of intrauterine growth retardation in developing countries. Eur J Clin Nutr. 1998 Jan;52(Suppl 1):S5–15. [PubMed] [Google Scholar]
- 10.Transforming our world: the 2030 Agenda for Sustainable Development. United Nations; [Online]. Available: https://sustainabledevelopment.un.org/post2015/transformingourworld. [Google Scholar]
- 11.Peters M, Crowe J, Piri JF, Quartero H, Hayes-Gill B, James D, Stinstra J, Shakespeare S. Monitoring the fetal heart non-invasively: a review of methods. J Perinat Med. 2001;29(5):408–416. doi: 10.1515/JPM.2001.057. [DOI] [PubMed] [Google Scholar]
- 12.Ayres-de Campos D, Bernardes J. Twenty-five years after the FIGO guidelines for the use of fetal monitoring: Time for a simplified approach? International Journal of Gynecology & Obstetrics. 2010;110(1):1–6. doi: 10.1016/j.ijgo.2010.03.011. [DOI] [PubMed] [Google Scholar]
- 13.Tech Rep. Online, World Health Organization (WHO) and the International Telecommunication Union (ITU); 2014. ehealth and innovation in women’s and children’s health: A baseline review. [Google Scholar]
- 14.Tamrat T, Kachnowski S. Special delivery: An analysis of mhealth in maternal and newborn health programs and their outcomes around the world. Maternal and Child Health Journal. 2012;16(5):1092–1101. doi: 10.1007/s10995-011-0836-3. [DOI] [PubMed] [Google Scholar]
- 15.Labrique AB, Vasudevan L, Kochi E, Fabricant R, Mehl G. mhealth innovations as health system strengthening tools: 12 common applications and a visual framework. Global Health: Science and Practice. 2013;1(2):160–171. doi: 10.9745/GHSP-D-13-00031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.UNICEF. State of the world’s children 2015 country statistical information. 2015 [Online]. Available: http://www.unicef.org/infobycountry/guatemala_statistics.html.
- 17.Garces A, Mcclure EM, Hambidge K, Krebs NF, Figueroa L, Aguilar M, Moore JL, Goldenberg RL. Trends in perinatal deaths from 2010 to 2013 in the Guatemalan Western Highlands. Reprod Health. 2015 Jun;12(Suppl 2):S14. doi: 10.1186/1742-4755-12-S2-S14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Caracterizacin departamental: Chimaltenango 2013. Instituto Nacional de Estadstica (INE); [Online]. Available: http://www.ine.gob.gt/sistema/uploads/2015/07/20/uYeKswXf9BHOJHZZZ7f7eR8CaMWVXnzg.pdf. [Google Scholar]
- 19.Walsh LV. Beliefs and rituals in traditional birth attendant practice in guatemala. J Transcult Nurs. 2006 Apr;17(2):148–154. doi: 10.1177/1043659605285412. [DOI] [PubMed] [Google Scholar]
- 20.Kestler E, Walker D, Bonvecchio A, Senz de Tejada S, Donner A. A matched pair cluster randomized implementation trail to measure the effectiveness of an intervention package aiming to decrease perinatal mortality and increase institution-based obstetric care among indigenous women in Guatemala: study protocol. BMC Pregnancy and Childbirth. 2013;13(1) doi: 10.1186/1471-2393-13-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stroux L, Clifford GD. 2014 Tech4Dev International Conference UNESCO Chair in Technologies for Development: What is Essential? EPFL; Lausanne, Switzerland: 2014. The Importance of Biomedical Signal Quality Classification for Successful mHealth Implementation. [Google Scholar]
- 22.Stroux L. A Perinatal Monitoring System for Low Resource Settings. D.Phil., University of Oxford; 2016. [Google Scholar]
- 23.Hornberger LK, Sahn DJ. Rhythm abnormalities of the fetus. Heart. 2007 Oct;93(10):1294–1300. doi: 10.1136/hrt.2005.069369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sibai B, Dekker G, Kupferminc M. Pre-eclampsia. The Lancet. 2005;365(9461):785–799. doi: 10.1016/S0140-6736(05)17987-2. [DOI] [PubMed] [Google Scholar]
- 25.Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-eclampsia. The Lancet. 2010;376(9741):631–644. doi: 10.1016/S0140-6736(10)60279-6. [DOI] [PubMed] [Google Scholar]
- 26.Millman AL, Payne B, Qu Z, Douglas MJ, Hutcheon JA, Lee T, Magee LA, Walley KR, von Dadelszen P. Oxygen saturation as a predictor of adverse maternal outcomes in women with preeclampsia. J Obstet Gynaecol Can. 2011 Jul;33(7):705–714. doi: 10.1016/S1701-2163(16)34955-6. [DOI] [PubMed] [Google Scholar]
- 27.Pildner von Steinburg S, Boulesteix A, Lederer C, Grunow S, Schiermeier S, Hatzmann W, Schneider KM, Daumer M. What is the normal fetal heart rate? PeerJ. 2013 May;1:e82. doi: 10.7717/peerj.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McAuliffe F, Kametas N, Krampl E, Ernsting J, Nicolaides K. Blood gases in pregnancy at sea level and at high altitude. BJOG. 2001 Sep;108(9):980–985. doi: 10.1111/j.1471-0528.2001.00225.x. [DOI] [PubMed] [Google Scholar]
- 29.NICE. Hypertension in pregnancy: diagnosis and management. clinical guideline. 2010 Aug; Online. [Online]. Available: http://www.nice.org.uk/guidance/cg107.


