Abstract
Introduction
Young workers (aged 15–24) suffer disproportionately from workplace injuries, with a nonfatal injury rate estimated to be two times higher than among workers age 25 or over. These workers make up approximately 9% of the U.S. workforce and studies have shown that nearly 80% of high school students work at some point during high school. Although young worker injuries are a pressing public health problem, the critical knowledge and skills needed to prepare youth for safe and healthy work are missing from most frameworks used to prepare the emerging U.S. workforce.
Methods
A framework of foundational workplace safety and health knowledge and skills (the NIOSH 8 Core Competencies)was developed based on the Health Belief Model (HBM).
Results
The proposed NIOSH Core Competencies utilize the HBM to provide a framework for foundational workplace safety and health knowledge and skills. An examination of how these competencies and the HBM apply to actions that workers take to protect themselves is provided. The social and physical environments that influence these actions are also discussed.
Conclusions
The NIOSH 8 Core Competencies, grounded in one of the most widely used health behavior theories, fill a critical gap in preparing the emerging U.S. workforce to be cognizant of workplace risks.
Practical applications
Integration of the NIOSH 8 Core Competencies into school curricula is one way to ensure that every young person has the foundational workplace safety and health knowledge and skills to participate in, and benefit from, safe and healthy work. National Safety Council and Elsevier Ltd. All rights reserved.
Keywords: Young workers, Life skills, Career readiness, Health Belief Model, Workplace safety and health
1. Introduction
In the United States, the Occupational Safety and Health (OSH) Act of 1970 requires employers to provide employees with a safe and healthy workplace, free of recognized hazards (“Occupational Safety and Health Act”, 1970). Despite vast improvements in occupational safety and health since the enactment of the OSH Act, work-related injuries, illness, and fatalities remain a persistent and pressing public health problem (Smith & DeJoy, 2012). Every day in the United States, more than 12 workers die on the job (US Bureau of Labor Statistics [BLS], 2015). Furthermore, according to estimates from the Survey of Occupational Injuries and Illnesses (SOII) conducted by the BLS, employers reported more than 3 million nonfatal injuries and illnesses to workers in private industry and 746,000 in state and local government in 2013 (BLS, 2014a). Workplace incidents cause significant physical, financial, and emotional hardship for businesses, workers, their families, and communities (Adams et al., 2002; Boden, Biddle, & Spieler, 2001; Brown, Shannon, Mustard, & McDonough, 2007; Dembe, 2001; Safe Work Australia, 2012). Based on 2007 U.S. data, the estimated direct medical costs ($67 billion) and indirect costs ($183 billion) of occupational injuries and illnesses were found to be at least as large as the cost of cancer (Leigh, 2011).
For numerous developmental and environmental reasons, younger workers (aged 15–24 years3) suffer disproportionately from workplace injuries (Centers for Disease Control and Prevention [CDC], 2010). Approximately 21.3 million individuals under 25 years of age were in the workforce in 2014, representing 8.6% of the total U.S. workforce (BLS, 2014b). Studies have shown that nearly 80% of high school students in the U.S. work at some point while still in school (BLS, 2005; Castillo & Lewko, 2013; Runyan, Schulman, & Scholl, 2012). During the 10-year period 1998–2007, an estimated 7.9 million nonfatal injuries to young workers were treated in U.S. hospital emergency departments (EDs) (CDC, 2010). The nonfatal injury rate was 5.0 ED-treated injuries per 100 full-time equivalent (FTE) workers, approximately two times higher than among workers age 25 or over (CDC, 2010). One study estimated that work-related injuries for youth up to age 19 accounted for an annual, total cost of $5 billion, or 3.9% of all workplace injury costs in the United States (Miller &Waehrer, 1998).
Given the high burden of workplace injuries and illnesses suffered by young workers, occupational safety education and training for this vulnerable population is imperative (Chin et al., 2010). Most of the current frameworks to teach work-readiness skills to the emerging workforce do not include the knowledge of and abilities for safe and healthy work. The nature and organization of work is evolving and young workers can expect to change jobs and employers many times during their working lives. These shifts will result in an increased likelihood of encountering new or different hazards or risk scenarios, suggesting the importance of an ongoing application of foundational occupational safety and health knowledge (Schulte, Stephenson, Okun, Palassis, & Biddle, 2005).
The intention of this article is to introduce a framework of core competencies for workplace safety and health. This theoretical framework—grounded in the Health Belief Model—delineates the foundational workplace safety and health knowledge and skills that young workers need and that serve as the basis for subsequent workplace safety and health learning. A brief review of the literature is provided for selected factors contributing to the higher rates of job-related injuries among young workers (when compared to their adult peers). Next, a theoretical framework for foundational workplace safety and health knowledge and skills (the NIOSH 8 Core Competencies) is introduced. Finally, avenues for future research and intervention are discussed, including the integration of the NIOSH competencies into school curricula to prepare youth to participate in, and benefit from, safe, healthy, and productive workplaces.
1.1. Factors that contribute to young worker injuries
The inverse relationship between age and non-fatal work injuries is a consistent association found in occupational safety and health research (Breslin & Smith, 2013; Laflamme & Menckel, 1995; Salminen, 2004). As new workers, adolescents are likely to be inexperienced and unfamiliar with many of the tasks required of them. Furthermore, adolescents’ unique characteristics such as their size, sleep requirements, musculoskeletal and endocrinal development, and cognitive and emotional maturity (National Institute for Occupational Safety and Health, 1997; Institute of Medicine, 1998; Sudhinaraset & Blum, 2010)may predispose them to workplace injuries (Runyan & Zakocs, 2000). Adolescent sensation seeking—the desire to pursue novel and intense experiences and sensations—and adolescent risk taking, especially when in the company of other young people, are commonly observed phenomena among developing youth (Spear, 2000; Steinberg, 2005, 2011). Moreover, when adolescents experience an absence of negative consequences when they engage in risky behavior, feelings of invulnerability may increase (Reyna& Farley, 2006). Adolescents’ orientation toward risk may predispose them to job-related injury (Sudhinaraset & Blum, 2010) and their most positive traits—energy, enthusiasm, and a need for increased challenge and responsibility—can increase their likelihood of taking on tasks they are not prepared to do safely.
The literature pertaining to the epidemiology of adolescent work-related injuries is limited when compared to that for adult workers (Steers, Elliott, Nemiro, Ditman, & Oskamp, 1996); nevertheless, a substantial evidence base has been built over the past two decades that identifies both individual factors, including minority status (Mardis & Pratt, 2003; Miller & Waehrer, 1998; New Zealand Department of Labour, 2007), socioeconomic status (Rauscher & Myers, 2008), and work-based risk factors, such as the fast pace of work (Breslin, Day, et al., 2007; Evensen, Schulman, Runyan, Zakocs, & Dunn, 2000; Frone, 1998; Zakocs, Runyan, Schulman, Dunn, & Evensen, 1998), inadequate supervision and training (Knight, Castillo, & Layne, 1995; Lewko, Runyan, Tremblay, Staley, & Volpe, 2010; Runyan & Zakocs, 2000; Runyan et al., 2007; Zakocs et al., 1998), equipment use (Breslin, Polzer, MacEachen, Morrongiello, & Shannon, 2007; Evensen et al., 2000; Frone, 1998; Knight et al., 1995; Mardis & Pratt, 2003; Parker, Carl, French, & Martin, 1994), working late, and working with cash and customers (Miller & Waehrer, 1998; NIOSH, 2003; Richardson & Windau, 2003; Runyan, Schulman, & Hoffman, 2003), that increase the risk for job-related injuries among adolescents (Breslin, Day, et al., 2007; Laberge & Ledoux, 2011; Rauscher & Runyan, 2013). Lack of job-related knowledge, skills, and training; and lack of job control also contribute to heightened risk among younger workers, who might be less likely to recognize hazards, less likely to speak up regarding safety issues (Breslin, Polzer, et al., 2007; Tucker & Turner, 2013; Zakocs et al., 1998), and less aware of their legal rights as workers (NIOSH, 2003).
1.2. Missing life skills and competencies for life
The terms “21st century skills,” “work-readiness skills,” “job-readiness skills,” and “employability skills,” have become watchwords in education, business, and government. Numerous frameworks articulate the skills, knowledge, and abilities for a skilled worker in the modern economy (Partnership for 21st Century Skills, 2009; The Conference Board, Partnership for 21st Century Skills, Corporate Voices for Working Families, & Society for Human Resource Management, 2006; U.S. Department of Labor, 2008). However, as previously noted, workplace safety and health is currently missing from many, if not most, of the current frameworks to prepare the future American workforce. Young people frequently enter the labor force lacking even the most basic workplace safety and health knowledge and skills needed to be cognizant of the safety and health challenges and hazards they may face. The benefits of incorporating foundational workplace health and safety knowledge and skills into education and training frameworks for youth are believed to include increased job/career knowledge, safer work activities, increased competence when dealing with occupational situations, and reduced incidence of job-related injuries and illnesses (Schulte et al., 2005).
In general, foundational skills in and for the context of work are considered the fundamental, portable skills needed for training and workplace success (ACT, 2013). These skills, which include reading for information, applied mathematics, problem solving, critical thinking, managing personal and interpersonal relationships, and communication, are fundamental in that they serve as a basis for supporting more advanced skill development, and they are portable because, rather than being job specific, they can be applied across a wide variety of occupations (ACT, 2013; Lankard, 1990; Partnership for 21st Century Skills, 2009; Saterfiel & McLarty, 1995; Symonds, Schwartz, & Ferguson, 2011; The Conference Board et al., 2006). In short, foundational skills are the fundamental, portable skills necessary for conveying and receiving information critical to training and workplace success (ACT, 2013). Having foundational skills is important as general competency “leavens” subsequent learning and practical experience (Darche & Stam, 2012).
Foundational skills for workplace safety and health are situated within the larger context of “work readiness” skills, which are generally thought of as “life skills” with a strong work focus. Life skills in turn are abilities that allow individuals to adapt to the challenges of everyday life (World Health Organization [WHO], 1997). Life skills are not in themselves behaviors but rather are abilities to behave in certain ways given the motivation, and given the scope to do so within an individual’s social, cultural, and environmental constraints (WHO, 1997).
1.3. Influence of environment on individual health actions
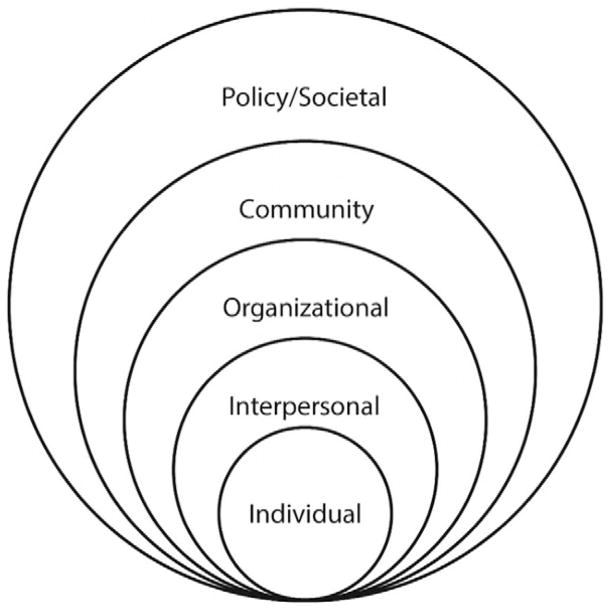
Historically there has been tension between injury prevention programs that use “active” (i.e. behavioral) strategies and those that use “passive” (i.e. structural) strategies (Gielen & Girasek, 2001). Active approaches are based on the premise that people are able to take an active role in protecting themselves, despite the hazards and other factors in their environments. These approaches have raised concerns about “blaming the victim” for their workplace injuries and illnesses (Frederick & Lessin, 2000; Gielen & Sleet, 2003). However, as Gielen and Sleet note, although structural interventions might appear straight-forward, environmental changes require human adaptation (Gielen & Sleet, 2003). This view is consistent with social ecological models of behavioral influences (see Fig. 1) (Bronfenbrenner, 1979; McLeroy, Bibeau, Steckler, & Glanz, 1988; Stokols, Pelletier, & Fielding, 1996) in which individual behavior models are situated, and must be considered, within a larger context of intrapersonal, interpersonal, organizational, community, and public policy dimensions. The basic premise of social ecological models is that providing individuals with the skills and motivation to change behaviors cannot be effective if environments are not supportive of change (Sallis, Owen, & Fisher, 2008). Hanson et al. have noted that because safety has both personal and environmental dimensions, it is in essence an ecological concept (2005). Their “injury iceberg” portrays individuals as “the tip” of a multi-level system in which they interact with both their physical and social environments. To reduce an individual’s risk of injury requires systematically addressing the factors “hidden below the waterline,” that influence individual behavior and choices (Hanson, Hanson, Vardon, et al., 2005). Therefore, injury prevention efforts are most effective when they are situated within an ecological framework that considers simultaneously individual and sociocultural factors (Sleet, Ballesteros, & Borse, 2010). Given the interactive aspect of individual and organizational factors in the workplace, it should be understood that even well-designed efforts to influence hazard-related beliefs and attitudes of workers may fail if the environment (including organization of work, management and safety culture) is nonsupportive (DeJoy, 1996).
Fig. 1.
Social ecological model (Sallis et al., 2008).
2. Methods
Foundational workplace safety and health skills are missing from most work readiness frameworks. To address this gap, the National Institute for Occupational Safety and Health (NIOSH) and its partners developed—through an iterative process during the revision of the NIOSH Youth@Work: Talking Safety curriculum—a framework of eight foundational workplace safety and health competencies. The NIOSH 8 Core Competencies were developed to prepare young workers to be cognizant of workplace risks and controls, and be able to participate in promoting safe and healthy workplaces. The framework for the 8 Core Competencies is based on the Health Belief Model (HBM), one of the most widely used theories in health behavior research and practice (Hochbaum, 1958; Janz & Becker, 1984; Rosenstock, 1974). The HBM is frequently used as a theoretical underpinning for research on adolescent health promotion (Bond, Aiken, & Somerville, 1992; Brown, DiClemente, & Reynolds, 1991; Eisen, Zellman, & McAlister, 1985) The development of the NIOSH 8 Core Competencies was informed by results of prior, formative research, conducted under a cooperative agreement with NIOSH (Miara, Gallagher, Bush, & Dewey, 2003) and is based in part on activities included in precursor curricula developed by partners in Massachusetts and California (NIOSH, 1999). This earlier curricula, based on the Health Belief Model, served as the initial building blocks for the NIOSH Talking Safety curriculum and the 8 Core Competencies.
The NIOSH 8 Core Competencies were articulated based on the six key constructs of the HBM—perceived susceptibility; perceived severity; perceived benefits of taking action; perceived barriers to taking action; cues to action; and self-efficacy. A theoretical approach was used to allow for the linking of subsequent educational interventions using the NIOSH competencies with behavioral change and, ultimately, with positive health outcomes.
3. Results
The NIOSH 8 Core Competencies include the following:
Recognize that, while work has benefits, all workers can be injured, become sick, or even be killed on the job. Workers need to know how workplace risks can affect their lives and their families.
Recognize that work-related injuries and illnesses are predictable and can be prevented.
Identify hazards at work, evaluate the risks, and predict how workers can be injured or made sick.
Recognize how to prevent injury and illness. Describe the best ways to address workplace hazards and apply these concepts to specific workplace problems.
Identify emergencies at work and decide on the best ways to address them.
Recognize that employers are responsible for, and workers have the right to, safe and healthy work. Workers also have the responsibility for keeping themselves and coworkers safe.
Find resources that help keep workers safe and healthy on the job.
Demonstrate how workers can communicate with others—including people in authority roles—to ask questions or report problems or concerns when they feel unsafe or threatened.
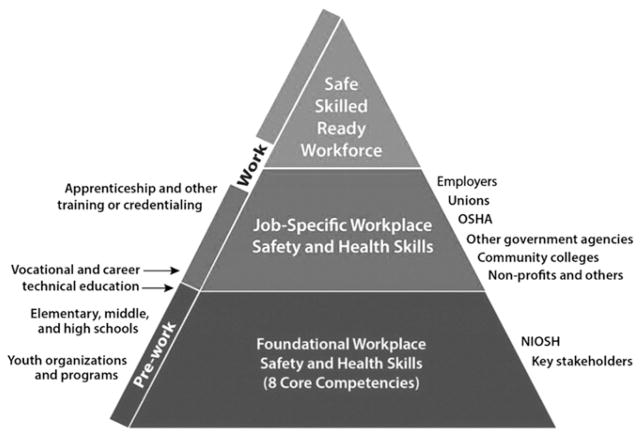
The 8 Core Competencies are not specific to any individual vocation or trade; rather they apply to all occupations and industries, and are supportive of job-specific skills gained through apprenticeships and career technical and vocational training programs, as well as on-the-job training. The competencies are not meant to preclude or replace any subsequent workplace safety and health training, rather they form the bottom of the pyramid shown in Fig. 2, and serve as the basis for future job-specific safety and health learning. The competencies are portable, in that they could apply across occupations and industries, and also transferable, meaning that they enable an individual to select, adapt, and apply knowledge, skills, and abilities to different situations, across different social contexts, and across different cognitive domains (Bridges, 1993).
Fig. 2.
The NIOSH 8 Core Competencies are foundational workplace safety and health skills.
The Health Belief Model is based the premise that for any behavior change to succeed, individuals must: 1) feel threatened (perceived susceptibility and severity); 2) believe that change of a specific kind will result in a beneficial outcome at an acceptable cost (perceived benefit and barriers); and, 3) feel themselves competent (self-efficacious) to take the necessary action and to overcome perceived barriers. Table 1 maps the NIOSH 8 Core Competencies to Health Belief Model (HBM) constructs, and the discussion that follows provides an explanation of this alignment.
Table 1.
NIOSH core competencies alignment with health belief model.
| Concept | Definition | NIOSH eight core competencies |
|---|---|---|
| Perceived susceptibility | Belief about the chances of experiencing a risk or getting a condition or disease | (1) Recognize that, while work has benefits, all workers can be injured, become sick, or even be killed on the job. Workers need to know how workplace risks can affect their lives and their families. |
| Perceived severity | Belief about seriousness of a condition and its sequelae | (1) Recognize that, while work has benefits, all workers can be injured, become sick, or even be killed on the job. Workers need to know how workplace risks can affect their lives and their families. (3) Identify hazards at work, evaluate the risks, and predict how workers can be injured or made sick. |
| Perceived benefits | Belief in efficacy of the advised action to reduce risk or seriousness of impact | (2) Recognize that work-related injuries and illnesses are predictable and can be prevented. |
| Perceived barriers | Belief about the tangible and psychological costs of the advised action (e.g. fear of being fired, fear of speaking up) | (6) Recognize that employers are responsible for, and workers have the right to, safe and healthy work (such as employees cannot be fired for reporting workplace hazards). (8) Demonstrate how workers can communicate with others—including people in authority roles—to ask questions or report problems or concerns when they feel unsafe or threatened. |
| Cues to action | Strategies to activate “readiness” (e.g. knowledge of child labor laws) | (3) Identify hazards at work, evaluate the risks, and predict how workers can be injured or made sick. (5) Identify emergencies at work and decide on the best ways to address them. (6) Recognize that employers are responsible for, and workers have the right to, safe and healthy work. Workers also have the responsibility for keeping themselves and coworkers safe. |
| Self-efficacy | Confidence in one’s ability to take action and successfully execute the behavior required to produce outcomes | (4) Recognize how to prevent injury and illness. Describe the best ways to address workplace hazards and apply these concepts to specific workplace problems. (5) Identify emergencies at work and decide on the best ways to address them. (7) Find resources that help keep workers safe and healthy on the job. (8) Demonstrate how workers can communicate with others—including people in authority roles—to ask questions or report problems or concerns when they feel unsafe or threatened |
Source: Adapted from Champion and Skinner (Champion & Skinner, 2008).
3.1. Perceived susceptibility
Perceived susceptibility refers to beliefs about the likelihood of experiencing a risk or getting a condition or disease. Recognizing that all workers can be injured, become sick, or even be killed on the job, aligns with the perceived susceptibility construct of the HBM. Increasing perceptions of susceptibility to job-related injury among working youth may be one pathway for helping them recognize that, while work has benefits, young workers experience a higher rate of workplace injuries when compared to adults. Research on health behaviors in young people demonstrates that perceived susceptibility predicted positive change related to certain health behaviors (Greene & Brinn, 2003; Li et al., 2003; Steers et al., 1996). Research involving children as young as ages 7 to 10 demonstrated that for young girls, perceived vulnerability (i.e. susceptibility)was the greatest predictor of whether they rated a play activity as risky (Hillier & Morrongiello, 1998). Similarly, injury prevention interventions that emphasize vulnerability to injury may be particularly useful at reframing young workers’ expectations about work-related injuries and illnesses. Youth can be engaged in safety learning that questions their safety-related beliefs (Chin et al., 2010) and through this come to understand, appreciate, and predict why and how they are at increased risk for injury and illness on the job, and the effects these incidents have on them and their families.
3.2. Perceived severity
Perceived severity refers to beliefs about the seriousness of a condition and its sequelae, including medical/health-related and possible social consequences. Young workers beliefs about the perceived severity of workplace safety and health injuries and illnesses may be shaped by the recognition that all workers can be injured, become sick, or even be killed on the job and how these injuries or illnesses could affect their lives and their families, as well as by their ability to identify hazards at work, evaluate the risks, and predict how workers can be injured or made sick.
A review of the injury literature related to young workers by Breslin and Smith (2013) suggests that contrary to popular beliefs about the cognitive function of young adults, by about age 16, an individual has the ability to appraise risk and use decision heuristics to respond (Fischhoff, 2013). Other studies of risk appraisal of health events find an absence of age-related difference between adolescents and adults (Quadrel, Fischhoff, & Davis, 1993; Weinstein, 1987). However, evidence also suggests that youth may differ from adults in terms of the recognition of the salience of potential short-term and long-term consequences (Nurmi, 1991; Reyna & Farley, 2006). Another notable difference between adolescents and adults is that young people are more susceptible to peer pressure and more oriented to the present than to the future (Steinberg, 2004). These phenomena extend to the workplace where youth are highly influenced by social contexts and their perceptions of coworkers and supervisors (Runyan et al., 2012; Westaby & Lowe, 2005). Given these findings, changes that focus on encouraging positive actions and less risk-taking on the part of all workers are necessary. Although no known research has been done to test the “perceived severity” construct of the Health Belief Model with adolescents in work settings, it is reasonable to assume that increased impressions of perceived threats within the workplace may lead to the adoption of job-related safety measures that protect current, and long-term, safety and health.
3.3. Perceived benefits
Even if an individual perceives personal susceptibility to a health threat, whether this perception leads to a behavior change will be influenced by the person’s beliefs regarding perceived benefits of the various available actions for reducing the threat (Champion & Skinner, 2008). Knowledge of the perceived benefit from taking protective actions with regards to workplace safety and health risks may be derived from the recognition that work-related injuries and illnesses are predictable and can be prevented. Numerous studies related to child and adolescent health promotion demonstrate that “perceived benefits” can provide an impetus for positive health actions, including being vaccinated (Zimet, Liau, & Fortenberry, 1997), participating in exercise and eating healthful foods (O’Dea, 2003), increasing intentions to use medicines for common health concerns (Bush & Iannotti, 1990), and engaging in heart-healthy behaviors (such as diet, exercise, and alcohol and tobacco moderation/cessation) (Mahalik & Burns, 2011). Although there is a lack of research on perceived benefits as an impetus to behavior change in occupational settings, especially as it relates to adolescents, it is possible to hypothesize that if young workers are made aware of the potential positive benefits from taking actions to prevent injury and illness, they may be more apt to enact and apply these abilities to specific workplace problems.
3.4. Perceived barriers
Perceived barriers are beliefs about the tangible and psychological costs of an advised action (Champion & Skinner, 2008). When faced with a particular health action, individuals engage in a nonconscious, cost–benefit analysis wherein they weigh the action’s expected benefit against perceived barriers (Champion & Skinner, 2008). Barriers decrease an individual’s ability to engage in the preventive behavior. Young workers may perceive the lack of control over their work environment as an impediment to improving workplace safety and health (Tucker & Turner, 2013; Zakocs et al., 1998). Adolescents often refrain from voicing their health and safety concerns to their supervisors in part because of their desire to construct an identity as a mature and independent worker (Breslin, Polzer, et al., 2007). Moreover, suppressing one’s complaints on the job may contribute to a ‘risk socialization’ process through which youth forge independent, self-sufficient, mature identities (Breslin, Polzer, et al., 2007). Research by Breslin indicates that youth view work-related injuries as “part of the job,” due in part to a lack of control over work tasks and the work environment and the discounting by employers of young workers’ health-related complaints (Breslin, Polzer, et al., 2007). Furthermore, adolescents face the real threat of being fired for “speaking up” about problems in the workplace (Tucker& Turner, 2013; Zakocs et al., 1998) and face psychological factors (such as fear) and structural factors (such as precarious employment) (Tucker & Turner, 2013) that may hinder their ability to engage in preventative behavior. Factors that may help reduce the barriers for young workers to engage in safe and healthful work and to report workplace safety and health problems include the recognition that employers are responsible for, and workers have the right to, safe and healthy work, as well as young workers having the ability to communicate with others, including people in authority, when feeling unsafe or threatened.
3.5. Cues to action
Cues to action refer to the specific stimuli needed to initiate or trigger a health behavior change (Mattson, 1999; Meillier, Lund, & Kok, 1997) or strategies to activate “readiness” (Champion & Skinner, 2008). These cues may be internal (such as symptoms/bodily events) or external (such as messages/media publicity, advice from family or friends, or the illness of a peer or loved one) and serve to create an awareness of the health threat (Champion & Skinner, 2008; Janz & Becker, 1984; Mattson, 1999; Meillier et al., 1997). In the context of the HBM, cues to action are primarily information-based (Meillier et al., 1997) and strategies to activate readiness might include providing how-to information, promoting awareness about a health issue/condition, or using appropriate reminder systems (Champion & Skinner, 2008). Cues to actions may be fostered by the ability to identify hazards at work and evaluate risk, the ability to identify emergencies at work and decide on the best ways to address them, and the knowledge that employers are responsible for, and workers have the right to, safe and healthy work. Therefore, when confronted with a workplace hazard or emergency at work, a young worker may take a protective action if he or she recognizes the potential risks in these situations. Also, knowledge of workers’ rights and the child labor laws may serve as strong cues to action if a young worker is confronted with a situation on the job that undermines these protections.
3.6. Self-efficacy
Self-efficacy refers to the confidence in one’s ability to take action and successfully execute the behavior required to produce the desired outcomes (Bandura, 1997, 2001). In other words, self-efficacy involves not only a belief that one can take a particular action but also a belief that taking that action is worth it and will ultimately lead to the desired outcome. As DeJoy notes, self-efficacy is an important factor to be considered in designing health and safety interventions in the workplace and can be developed through education/training and skill-building exercises, as well as through actual experience in performing the relevant actions (DeJoy, 1996). A number of the NIOSH core competencies contribute to developing a young worker’s self-efficacy by providing the knowledge and skills needed to increase his or her ability to feel confident about performing safety and health practices in the workplace. These competencies include equipping young workers with the knowledge and skills to recognize and understand the best ways to control workplace hazards, to identify emergencies at work and decide the best ways to address them, to find resources, and, perhaps most important, the ability to communicate with others, including people in authority roles, and to ask questions or report problems or concerns when they feel unsafe or threatened.
Young people need the opportunity to increase self-efficacy, through building skills and confidence, to overcome the barriers to taking preventative actions. This may occur by giving them positive experiences in a training environment. However, it is important that the training reflect adolescents’ reality of work, which includes their natural reticence in voicing concerns to supervisors. As the young worker experiences positive results and receives external reinforcement (including through training and interactions with supervisors and co-workers), she or he is more likely to experience self-efficacy (Runyan et al., 2012).
4. Discussion
The NIOSH 8 Core Competencies, grounded in the Health Belief Model, one of the most widely used conceptual frameworks in health behavior practice, fill a critical gap in preparing the emerging U.S. workforce to be cognizant of workplace risks and controls, and be able to participate in promoting safe and healthy workplaces. Health behavior theories, when applied to injury and illness prevention, offer great potential to improve health outcomes for vulnerable individuals—including adolescents who work. The use of a model-based approach for specifying the competencies is important for linking subsequent educational interventions with behavioral change and, ultimately, with positive health outcomes (Gielen & Sleet, 2003; Institute of Medicine, 1998; Kidd, Reed, Weaver, Westneat, & Rayens, 2003). It is the application of theory that facilitates a better understanding of the underlying causes of a health and safety problem while also identifying mechanisms of change (Gielen & Sleet, 2003). Models and theories help bridge the understanding of which behaviors and environmental factors are responsible for an injury problem and for deciding on and designing appropriate interventions to address it (Gielen & Girasek, 2001). Therefore, the application and translation of health behavior theories is vital to injury and illnesses prevention (Gielen & Sleet, 2003). However, in using these theories and models, we recognize that adolescent decision making processes are in no way uniform (Reyna & Farley, 2006) nor is adolescent risk-taking a wholly-rational or conscious process (Steinberg, 2004). Moreover, it is important to look beyond individually oriented theories of health behavior toward ecological theories that highlight the importance of the social, interpersonal, and organizational context of work (Brewer & Rimer, 2008; Hanson et al., 2005; Stokols et al., 1996). Therefore, it should be noted that although the NIOSH 8 Core Competencies are grounded in the Health Belief Model (HBM), there are aspects of them—such as advocating for coworker safety—that are not addressed by individually-oriented health behavior theories. Although there are numerous conceptual models that guide the development and implementation of occupational safety and health (OSH) programs and interventions (Cohen, Smith, & Anger, 1979; DeJoy & Southern, 1993; Wilson, DeJoy, Vandenberg, Richardson, & McGrath, 2004); little attention has been given to examining how health promotion theories—like the HBM—might apply to actions that workers take to protect themselves from job-related hazards and the social and physical environments that influence them (DeJoy, 1996). Strategies used to promote positive health change may have relevance for injury prevention (Kidd et al., 2003), yet health behavior theory has not been incorporated into the design of most young worker safety interventions in the United States (Gallagher & Rattigan, 2013). These theories could be effective if used in designing targeted programs aimed at individual knowledge or behavior change among youth in the workplace (Gallagher & Rattigan, 2013).
The proposed NIOSH Core Competencies are consistent with widely accepted definitions of competencies in the context of occupational settings, in that they address an individual’s capability to apply a set of related knowledge, skills, and abilities to successfully perform functions or tasks in a work environment. The competencies are also consistent with the broader conception of competencies that go beyond the work sphere, in that they, 1) contribute to valued outcomes for societies and individuals; 2) help individuals meet important demands in a wide variety of contexts; and are 3) important not just for specialists but for all individuals (Organisation for Economic Co-operation and Development, 2005; U.S. Department of Labor, 2008). In sum, the foundational workplace safety and health competencies developed by NIOSH and its partners are general, transferable, and portable across all jobs and industries, and although developed with young individuals in mind, are applicable as foundational skills for all individuals who work, in any capacity, whether as employer or employee. More broadly, the 8 Core Competencies could be applied to other health-related circumstances where risk-based decisions are made and therefore may be used to improve the health and safety within non-work settings such as homes, schools, and communities (Cammarota, 2011).
We recognize, in putting forth a framework for foundational knowledge, skills, and abilities for workplace safety and health that an individual’s ability to act (i.e. enact these critical competencies) is contingent on the work environment and that structural measures implemented by employers in the workplace are more effective for protecting workers than those relying on individuals actions. These structural changes, once achieved, are also more likely to be sustained (Allegrante, Hanson, Sleet, & Marks, 2012). DeJoy (1996) notes that “the importance of the environment in enabling and reinforcing safe workplace behavior cannot be overemphasized.” Therefore, it is necessary to critically examine the structural factors (or the lack thereof) for which employers are responsible, that create or contribute to unsafe working conditions for youth in the United States. The individual protective knowledge, skills and abilities obtained by young people through the Talking Safety curriculum should therefore be situated in a larger context of organizational and environmental factors that may promote, or hinder, health-related behavior change.
We also suggest, that the work environment is never free of risks. In the case of young workers for example, despite the existence of both federal and state child labor and general worker safety laws designed to protect young workers from hazards, these laws are not fully enforced and gaps exist (Castillo, Landen, & Layne, 1994; Rauscher & Myers, 2008; Runyan, Dal Santo, Schulman, Lipscomb, & Harris, 2006; Runyan et al., 2007, 2012; Suruda, Philips, Lillquist, & Sesek, 2003). Young employees are often injured, sometimes fatally, while working in illegal occupations or while performing prohibited tasks. While it is the case that young workers face a number of limitations in their ability to enact protective behaviors on the job—including power differentials between them and their employers, lack of experience, and lack of self-confidence to raise safety and health issues (Schulte et al., 2005)—equipping young workers with foundational workplace health and safety competencies should enable them to better engage in activities to protect themselves and others.
Schools have an important role to play in promoting the health of the nation as this is perhaps the only societal context in which all children can be easily reached. It is a natural setting for promoting healthful habits, discouraging unhealthy habits, and building generic self-management skills (Bandura, 1986). Because the majority of students work at some point during their high school years, the integration of foundational workplace safety and health competencies into middle school and high school curricula may be one way to ensure that every young person, before he or she enters the workforce, has the ability to be cognizant of risks on the job and be able to engage in appropriate actions for dealing with them effectively (Miller & Waehrer, 1998). Schools have proven to be a particularly effective locus for delivery of vital workplace safety and health skills (Linker, Miller, Freeman, & Burbacher, 2005; Pisaniello et al., 2013; Schulte et al., 2005). Additionally, integrating these competencies into school curricula allows for the material to be geared towards the appropriate students’ age and developmental level (Miller & Waehrer, 1998).
Middle schools and high schools classes in science, health education, family and consumer science, career exploration, career technical education (CTE), and other courses, as well as school- or community-based training programs on work readiness and/or college and career readiness may all be appropriate content areas to incorporate the NIOSH 8 Core Competencies. According to a survey of teachers in Australia, interviewees suggested that the quality of occupational safety education would be improved if it were formally integrated into curricula—making the topic compulsory and standardized, with assessment provided and credit awarded (Pisaniello et al., 2013).
A 2003 report from the European Agency for Safety and Health at Work recognized the importance of mainstreaming workplace health and safety into education indicating that children in primary and secondary education should be taught how to identify hazards and assess and manage workplace risks, and that older youth and adults in vocational education should be taught risk assessment and management principles (European Agency for Safety and Health at Work, 2004). The report also points out that mainstreaming workplace health and safety into education would allow ‘OSH thinking’ to become an intrinsic part of the way decisions are made and actions are taken in the workplace, not just considered as an add-on. This is because it is easier to achieve “OSH thinking” if workers and employers already come to the workplace with an understanding of workplace safety and health (European Agency for Safety and Health at Work, 2004).
The NIOSH Talking Safety curriculum(NIOSH, 2015) is a free resource designed to teach the NIOSH 8 core competencies and give students the career readiness skills they need to become active participants in creating safe and healthy work environments. Currently, demonstration projects are under way in two states (Florida and Oklahoma) focusing on the integration and institutionalization of the critical workplace safety and health competencies delivered through Talking Safety. Moreover, NIOSH is also exploring how the core competencies might be integrated into community-based programs. While there is evidence that school-based educational programs have the potential to increase knowledge about safety, there are currently no known studies that show that this increase in knowledge will translate to safe behavior and, ultimately, injury reduction (Pisaniello et al., 2013). Future evaluation of the NIOSH pilot projects will be important to establish the extent to which young people are able to apply the foundational workplace safety and health competencies they learn in the classroom to real-world situations.
5. Conclusion
The purpose of this paper is to introduce a theoretical framework—grounded in the Health Belief Model—for equipping young workers with foundational workplace safety and health knowledge and skills (the NIOSH 8 Core Competencies). These competencies play a critical role in preparing youth to enter the workforce as they serve as the basis for subsequent workplace safety and health learning. Most current frameworks that equip young workers with work readiness capabilities do not include competencies for safe and healthy work. This is a critical gap, and one that must be addressed. Individuals cannot be successful on the job, or in any other environment, if they do not have the knowledge and skills needed to be safe and healthy. An integrated strategy for protecting youth on the job is required that includes environmental change, legislation and enforcement, but also education and training (Towner, Dowswell, MacKereth, & Jarvis, 2001). The conceptual framework proposed in this paper recognizes that foundational workplace safety and health competencies may play an important role in protecting young workers from injury or illness and should be an essential component to all work-readiness efforts directed at preparing the current and future American workforce.
Practical applications
The foundational workplace safety and health competencies developed by NIOSH and its partners are general, transferable, and portable across all jobs and industries, and although developed with young individuals in mind, are applicable to all individuals who work, whether as employer or employee. Because the majority of students work at some point during their high school years, the integration of foundational workplace safety and health competencies into middle school and high school curricula is one way to ensure that every young person, before he or she enters the workforce, has the ability to be cognizant of risks on the job and to participate in, and benefit from, safe, healthy, and productive work. More broadly, these workplace safety and health competencies could also be applied to other health-related circumstances where risk-based decisions are made and therefore may be used to improve the health and safety within non-work settings such as homes, schools, and communities.
Acknowledgments
We thank the following individuals. For contributions to and support of this work: Carol Stephenson, Diane Bush, Robin Dewey, Chris Miara, and Susan Gallagher. For comments on versions of this article: Carol Runyan, Dawn Castillo, David Parker, Pete Hunt and Jim Emshoff. We also acknowledge the efforts of Devin Baker, Brenda Proffitt, and Barbara Cromer regarding logistical support in preparation of this article.
Biographies
Andrea H. Okun, DrPH
Dr. Okun is the Associate Director for Global Collaborations with the National Institute for Occupational Safety and Health (NIOSH), Centers for Disease Control and Prevention. Dr. Okun has 35 years’ experience in conducting strategic planning, implementation, and evaluation of occupational safety and health research programs as well the coordination of partnerships across the Institute, within the extramural community, and with global experts. Prior to this position, she served 16 years as the Deputy Director of the Education and Information Division at NIOSH. Dr. Okun serves as the co-coordinator for the NIOSH Safe-Skilled-Ready Workforce Initiative. Her current research interests focus on the integration of occupational safety and health knowledge and skills into workforce readiness programs.
Rebecca J. Guerin, MA
Ms. Guerin is a health communication specialist with the National Institute for Occupational Safety and Health (NIOSH), Centers for Disease Control and Prevention. Ms. Guerin serves as the principal investigator for the NIOSH Safe-Skilled-Ready Workforce Program. In this capacity, she is responsible for implementing and evaluating a program of research to integrate foundational workplace safety and health skills into curricula, training, and other work readiness programs for young workers and new hires. She has been involved in young worker outreach/research efforts at NIOSH for eight years. Prior to coming to NIOSH, Ms. Guerin held positions in the financial sector, including as an analyst with the New York Federal Reserve Bank.
Paul A. Schulte, PhD
Dr. Schulte is the Director of the Education and Information Division, and Co-Manager of the Nanotechnology Research Center, National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention. Dr. Schulte has 35 years’ experience in conducting research and developing guidance on occupational cancer, nanomaterials, risk communication, workplace well-being, and genetics. He is the co-editor of the textbook entitled, “Molecular Epidemiology: Principles and Practices.” He has served as guest editor of the Journal of Occupational Medicine and the American Journal of Industrial Medicine and was on the initial editorial board of Cancer Epidemiology, Biomarkers and Prevention. He currently is on the International Advisory Board of the Annals of Occupational Hygiene.
Footnotes
Disclaimer: The findings and conclusions in this report are those of the author(s) and do not necessarily represent the views of the National Institute for Occupational Safety and Health.
In the United States, federal and state child labor laws, which regulate the employment of minors, are tied to the Fair Labor Standards Act (FLSA) of 1938 (“Fair Labor Standards Act”, 1938). The FLSA limits the types of jobs youths aged 14 to 17 years are allowed to perform, the number of hours they may work, and the timing of these hours. However, national injury and fatality data usually do not include youth under age 15. http://dx.doi.org/10.1016/j.jsr.2016.09.004
References
- ACT. Work readiness standards and benchmarks: The key to differentiating America’s workforce and regaining global competitiveness. Iowa City, IA: ACT; 2013. [Google Scholar]
- Adams M, Burton J, Butcher F, Graham S, McLeod A, Rajan R, … Johri R. Aftermath: The social and economic consequences of workplace injury and illness. Wellington, New Zealand: New Zealand Department of Labour; 2002. [Google Scholar]
- Allegrante JP, Hanson DW, Sleet DA, Marks R. Ecological approaches to the prevention of unintentional injuries. Italian Journal of Public Health. 2012;7(2) [Google Scholar]
- Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall, Inc; 1986. [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York, NY: Freeman; 1997. [Google Scholar]
- Bandura A. Self-efficacy and health. In: Smelser NJ, Baltes PB, editors. International encyclopedia of the social & behavioral sciences. Oxford, UK: Pergamon; 2001. pp. 13815–13820. [Google Scholar]
- Boden LI, Biddle EA, Spieler EA. Social and economic impacts of workplace illness and injury: Current and future directions for research. American Journal of Industrial Medicine. 2001;40(4):398–402. doi: 10.1002/ajim.10013. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11598990) [DOI] [PubMed] [Google Scholar]
- Bond GG, Aiken LS, Somerville SC. The health belief model and adolescents with insulin-dependent diabetes mellitus. Health Psychology. 1992;11(3):190–198. doi: 10.1037//0278-6133.11.3.190. [DOI] [PubMed] [Google Scholar]
- Breslin FC, Smith PM. Risk factors for nonfatal work injury for young workers: A review of two relevant literatures. In: Runyan CW, Lewko J, Rauscher K, Castillo D, Brandspigel S, editors. Health and safety of young workers: Proceedings of a U.S. and Canadian series of symposia. DHHS (NIOSH) Publication No. 2013–144. Cincinnati, OH: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; 2013. pp. 80–104. [Google Scholar]
- Breslin FC, Day D, Tompa E, Irvin E, Bhattacharyya S, Clarke J, Wang A. Non-agricultural work injuries among youth: A systematic review. American Journal of Preventive Medicine. 2007a;32(2):151–162. doi: 10.1016/j.amepre.2006.10.007. http://dx.doi.org/10.1016/j.amepre.2006.10.007. [DOI] [PubMed] [Google Scholar]
- Breslin FC, Polzer J, MacEachen E, Morrongiello B, Shannon H. Workplace injury or “part of the job?”: Towards a gendered understanding of injuries and complaints among young workers. Social Science & Medicine. 2007b;64(4):782–793. doi: 10.1016/j.socscimed.2006.10.024. [DOI] [PubMed] [Google Scholar]
- Brewer NT, Rimer BK. Perspectives on health behavior theories that focus on individuals. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: Theory, research, and practice. Philadelphia, PA: John Wiley & Sons; 2008. pp. 45–65. [Google Scholar]
- Bridges D. Transferable skills: A philosophical perspective. Studies in Higher Education. 1993;18(1):43–52. [Google Scholar]
- Bronfenbrenner U. The ecology of human development. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- Brown LK, DiClemente RJ, Reynolds LA. HIV prevention for adolescents: Utility of the Health Belief Model. AIDS Education and Prevention. 1991;3(1):50–59. [PubMed] [Google Scholar]
- Brown JA, Shannon HS, Mustard CA, McDonough P. Social and economic consequences of workplace injury: A population-based study of workers in British Columbia, Canada. American Journal of Industrial Medicine. 2007;50(9):633–645. doi: 10.1002/ajim.20503. http://dx.doi.org/10.1002/ajim.20503. [DOI] [PubMed] [Google Scholar]
- Bush PJ, Iannotti RJ. A children’s health belief model. Medical Care. 1990;28(1):69–86. doi: 10.1097/00005650-199001000-00008. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/2296217) [DOI] [PubMed] [Google Scholar]
- Cammarota A. Education and training in safety and health: The European dimension. Berlin, Germany: Institute for Work and Health; 2011. [Google Scholar]
- Castillo D, Lewko J. Youth employment and the health and safety issues of young workers in the US and Canada: An overview. In: Runyan CW, Lewko J, Rauscher K, Castillo D, Brandspigel S, editors. Health and safety of young workers: Proceedings of a U.S. and Canadian series of symposia. DHHS (NIOSH) Publication No. 2013–144. Cincinnati, OH: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; 2013. pp. 4–25. [Google Scholar]
- Castillo D, Landen DD, Layne LA. Occupational injury deaths of 16- and 17-year-olds in the United States. American Journal of Public Health. 1994;84(4):646–649. doi: 10.2105/ajph.84.4.646. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/7755674) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Occupational injuries and deaths among younger workers: United States, 1998–2007. Morbidity and Mortality Weekly Report. 2010;59(15):449–455. [PubMed] [Google Scholar]
- Champion VL, Skinner CS. The health belief model. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: Theory, research, and practice. Philadelphia, PA: John Wiley & Sons; 2008. pp. 45–65. [Google Scholar]
- Chin P, DeLuca C, Poth C, Chadwick I, Hutchinson N, Munby H. Enabling youth to advocate for workplace safety. Safety Science. 2010;48(5):570–579. [Google Scholar]
- Cohen A, Smith MJ, Anger WK. Self-protective measures against workplace hazards. Journal of Safety Research. 1979;11(3):121–131. [Google Scholar]
- Darche S, Stam B. College and career readiness: what do we mean? A proposed framework. 2012 Retrieved from http://www.connectedcalifornia.org/direct/files/resources/CACR%20Version%20V1-2%20Apr%2012%202012_FINAL.PDF.
- DeJoy DM. Theoretical models of health behavior and workplace self-protective behavior. Journal of Safety Research. 1996;27(2):61–72. [Google Scholar]
- DeJoy DM, Southern DJ. An integrative perspective on work-site health promotion. Journal of Occupational Medicine. 1993;35(12):1221–1230. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8113926) [PubMed] [Google Scholar]
- Dembe AE. American Journal of Industrial Medicine. 4. Vol. 40. Education Development Center Inc Teenage Health Teaching Modules Education Development Center Inc; Newton MA: 2001. The social consequences of occupational injuries and illnesses; pp. 403–417. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11598991. [DOI] [PubMed] [Google Scholar]
- Eisen M, Zellman GL, McAlister AL. A health belief model approach to adolescents’ fertility control: some pilot program findings. Health Education & Behavior. 1985;12(2):185–210. doi: 10.1177/109019818501200205. http://dx.doi.org/10.1177/109019818501200205. [DOI] [PubMed] [Google Scholar]
- European Agency for Safety and Health at Work. Mainstreaming occupational safety and health into education: Good practice in school and vocational education. 2004 Retrieved from https://osha.europa.eu/en/tools-and-publications/publications/reports/313.
- Evensen CT, Schulman MD, Runyan CW, Zakocs RC, Dunn KA. The downside of adolescent employment: hazards and injuries among working teens in North Carolina. Journal of Adolescence. 2000;23(5):545–560. doi: 10.1006/jado.2000.0342. http://dx.doi.org/10.1006/jado.2000.0342. [DOI] [PubMed] [Google Scholar]
- Fair Labor Standards Act, 29 USC 8, §201–219 (1938).
- Fischhoff B. Assessing adolescent decision-making competence. In: Runyan CW, Lewko J, Rauscher K, Castillo D, Brandspigel S, editors. Health and safety of young workers: Proceedings of a U.S. and Canadian series of symposia. DHHS (NIOSH) Publication No. 2013–144. Cincinnati, OH: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; 2013. pp. 46–65. [Google Scholar]
- Frederick J, Lessin N. Blame the worker: The rise of behavioral-based safety programs. Multinational Monitor. 2000;21(11):10. [Google Scholar]
- Frone MR. Predictors of work injuries among employed adolescents. The Journal of Applied Psychology. 1998;83(4):565–576. doi: 10.1037/0021-9010.83.4.565. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9729926) [DOI] [PubMed] [Google Scholar]
- Gallagher S, Rattigan S. State of the art in young worker safety interventions in the United States. In: Runyan CW, Lewko J, Rauscher K, Castillo D, Brandspigel S, editors. Health and safety of young workers: Proceedings of a U.S. and Canadian series of symposia. DHHS (NIOSH) Publication No. 2013–144. Cincinnati, OH: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; 2013. pp. 147–166. [Google Scholar]
- Gielen AC, Girasek DC. Integrating perspectives on the prevention of unintentional injuries. In: Schneiderman N, Speers MA, Silva JM, Tomes H, Gentry JH, editors. Integrating behavioral and social sciences with public health. Washington, DC: American Psychological Association; 2001. pp. 203–227. [Google Scholar]
- Gielen AC, Sleet D. Application of behavior-change theories and methods to injury prevention. Epidemiologic Reviews. 2003;25:65–76. doi: 10.1093/epirev/mxg004. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12923991) [DOI] [PubMed] [Google Scholar]
- Greene K, Brinn LS. Messages influencing college women’s tanning bed use: Statistical versus narrative evidence format and a self-assessment to increase perceived susceptibility. Journal of Health Communication. 2003;8(5):443–461. doi: 10.1080/713852118. http://dx.doi.org/10.1080/713852118. [DOI] [PubMed] [Google Scholar]
- Hanson D, Hanson J, Vardon P, et al. The injury iceberg: An ecological approach to planning sustainable community safety interventions. Health Promotion Journal of Australia. 2005;16:5–15. doi: 10.1071/he05005. [DOI] [PubMed] [Google Scholar]
- Hillier LM, Morrongiello BA. Age and gender differences in school-age children’s appraisals of injury risk. Journal of Pediatric Psychology. 1998;23(4):229–238. doi: 10.1093/jpepsy/23.4.229. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9718896) [DOI] [PubMed] [Google Scholar]
- Hochbaum GM. Public participation in medical screening programs: A sociopsychological study. Washington, DC: Department of Health, Education, and Welfare; 1958. [Google Scholar]
- Institute of Medicine. Protecting Youth at Work: Health, Safety, and Development of Working Children and Adolescents in the United States. Washington, D.C: National Academy Press; 1998. [PubMed] [Google Scholar]
- Janz NK, Becker MH. The Health Belief Model: A decade later. Health Education Quarterly. 1984;11(1):1–47. doi: 10.1177/109019818401100101. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/6392204) [DOI] [PubMed] [Google Scholar]
- Kidd P, Reed D, Weaver L, Westneat S, Rayens MK. The transtheoretical model of change in adolescents: Implications for injury prevention. Journal of Safety Research. 2003;34(3):281–288. doi: 10.1016/s0022-4375(03)00029-x. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12963074) [DOI] [PubMed] [Google Scholar]
- Knight EB, Castillo DN, Layne LA. A detailed analysis of work-related injury among youth treated in emergency departments. American Journal of Industrial Medicine. 1995;27(6):793–805. doi: 10.1002/ajim.4700270604. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/7645574) [DOI] [PubMed] [Google Scholar]
- Laberge M, Ledoux E. Occupational health and safety issues affecting young workers: A literature review. Work. 2011;39(3):215–232. doi: 10.3233/WOR-2011-1170. http://dx.doi.org/10.3233/WOR-2011-1170. [DOI] [PubMed] [Google Scholar]
- Laflamme L, Menckel E. Aging and occupational accidents: A review of the literature of the last three decades. Safety Science. 1995;21:145–161. [Google Scholar]
- Lankard BA. ERIC digest no. 104: Employability—The fifth basic skill. 1990 Retrieved from http://eric.ed.gov/?id=ED325659.
- Leigh JP. Economic burden of occupational injury and illness in the United States. The Milbank Quarterly. 2011;89(4):728–772. doi: 10.1111/j.1468-0009.2011.00648.x. http://dx.doi.org/10.1111/j.1468-0009.2011.00648.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewko JH, Runyan CW, Tremblay CL, Staley JA, Volpe R. Workplace experiences of young workers in Ontario. Canadian Journal of Public Health. 2010;101(5):380–384. doi: 10.1007/BF03404857. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/21214052) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C, Unger JB, Schuster D, Rohrbach LA, Howard-Pitney B, Norman G. Youths’ exposure to environmental tobacco smoke (ETS): Associations with health beliefs and social pressure. Addictive Behaviors. 2003;28(1):39–53. doi: 10.1016/s0306-4603(01)00215-5. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12507526) [DOI] [PubMed] [Google Scholar]
- Linker D, Miller ME, Freeman KS, Burbacher T. Health and safety awareness for working teens: Developing a successful, statewide program for educating teen workers. Family & Community Health. 2005;28(3):225–238. doi: 10.1097/00003727-200507000-00004. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/15958881) [DOI] [PubMed] [Google Scholar]
- Mahalik JR, Burns SM. Predicting health behaviors in young men that put them at risk for heart disease. Psychology of Men & Masculinity. 2011;12(1):1–12. [Google Scholar]
- Mardis AL, Pratt SG. Nonfatal injuries to young workers in the retail trades and services industries in 1998. Journal of Occupational and Environmental Medicine. 2003;45(3):316–323. doi: 10.1097/01.jom.0000052964.43131.8a. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12661189) [DOI] [PubMed] [Google Scholar]
- Mattson M. Toward a reconceptualization of communication cues to action in the Health Belief Model: HIV test counseling. Communication Monographs. 1999;66(3):240–265. doi: 10.1080/03637759909376476. http://dx.doi.org/10.1080/03637759909376476. [DOI] [PubMed] [Google Scholar]
- McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Education Quarterly. 1988;15(4):351–377. doi: 10.1177/109019818801500401. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/3068205) [DOI] [PubMed] [Google Scholar]
- Meillier LK, Lund AB, Kok G. Cues to action in the process of changing lifestyle. Patient Education and Counseling. 1997;30(1):37–51. doi: 10.1016/s0738-3991(96)00957-3. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9110831) [DOI] [PubMed] [Google Scholar]
- Miara C, Gallagher S, Bush D, Dewey R. Developing an effective tool for teaching teens about workplace safety. American Journal of Health Education. 2003;34(5 September/October Supplement):30–34. [Google Scholar]
- Miller TR, Waehrer GM. Costs of occupational injuries to teenagers, United States. Injury Prevention. 1998;4(3):211–217. doi: 10.1136/ip.4.3.211. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9788093) [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Occupational Safety and Health. Child labor research needs: Recommendations from the NIOSH Child Labor Working Team. DHHS (NIOSH) Publication No. 1997-143. Cincinnati, OH: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; 1997. [Google Scholar]
- National Institute for Occupational Safety and Health. Promoting safe work for young workers—A community-based approach. DHHS (NIOSH) Publication No. 1999–141. Cincinnati, OH: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; 1999. [Google Scholar]
- National Institute for Occupational Safety and Health. Preventing deaths, injuries, and illnesses of young workers. DHHS (NIOSH) Publication No. 2003-128. Cincinnati, OH: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; 2003. [Google Scholar]
- National Institute for Occupational Safety and Health. Youth@work—Talking safety. 2015 Retrieved from http://www.cdc.gov/niosh/talkingsafety/
- New Zealand Department of Labour. How health and safety makes good business sense. 2007 Retrieved from http://www.dol.govt.nz/publications/research/good-sense/litreview.pdf.
- Nurmi JE. How do adolescents see their future? A review of the development of future orientation and planning. Developmental Review. 1991;11(1):1–59. [Google Scholar]
- Occupational Safety and Health Act, 29 USC 15, §651–678 (1970).
- O’Dea JA. Why do kids eat healthful food? Perceived benefits of and barriers to healthful eating and physical activity among children and adolescents. Journal of the American Dietetic Association. 2003;103(4):497–501. doi: 10.1053/jada.2003.50064. http://dx.doi.org/10.1053/jada.2003.50064. [DOI] [PubMed] [Google Scholar]
- Organisation for Economic Co-operation and Development. The definition and selection of key competencies: executive summary. 2005 Retrieved from http://www.oecd.org/pisa/35070367.pdf.
- Parker DL, Carl WR, French LR, Martin FB. Characteristics of adolescent work injuries reported to the Minnesota Department of Labor and Industry. American Journal of Public Health. 1994;84(4):606–611. doi: 10.2105/ajph.84.4.606. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8154564) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Partnership for 21st Century Skills. P21 framework definitions. 2009 Retrieved from http://www.p21.org/storage/documents/P21_Framework_Definitions.pdf.
- Pisaniello DL, Stewart SK, Jahan N, Pisaniello SL, Winefield H, Braunack-Mater A. The role of high schools in introductory occupational safety education—Teacher perspectives on effectiveness. Safety Science. 2013;55:53–61. [Google Scholar]
- Quadrel MJ, Fischhoff B, Davis W. Adolescent (in)vulnerability. The American Psychologist. 1993;48(2):102–116. doi: 10.1037//0003-066x.48.2.102. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8442566) [DOI] [PubMed] [Google Scholar]
- Rauscher KJ, Myers DJ. Socioeconomic disparities in the prevalence of work-related injuries among adolescents in the United States. Journal of Adolescent Health. 2008;42(1):50–57. doi: 10.1016/j.jadohealth.2007.08.003. http://dx.doi.org/10.1016/j.jadohealth.2007.08.003. [DOI] [PubMed] [Google Scholar]
- Rauscher KJ, Runyan CW. Prevalence of working conditions associated with adolescent occupational injury in the U.S.: A review of literature. In: Runyan CW, Lewko J, Rauscher K, Castillo D, Brandspigel S, editors. Health and safety of young workers: Proceedings of a U.S. and Canadian series of symposia. DHHS (NIOSH) Publication No. 2013-144. Cincinnati, OH: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; 2013. pp. 126–136. [Google Scholar]
- Reyna VF, Farley F. Risk and rationality in adolescent decision-making: Implications for theory, practice, and public policy. Psychological Science in the Public Interest. 2006;7(1):1–44. doi: 10.1111/j.1529-1006.2006.00026.x. [DOI] [PubMed] [Google Scholar]
- Richardson S, Windau J. Fatal and nonfatal assaults in the workplace, 1996 to 2000. Clinics in Occupational and Environmental Medicine. 2003;3:673–689. [Google Scholar]
- Rosenstock IM. The health belief model and preventive health behavior. Health Education Monograph. 1974;2(4):354–386. [Google Scholar]
- Runyan CW, Zakocs RC. Epidemiology and prevention of injuries among adolescent workers in the United States. Annual Review of Public Health. 2000;21:247–269. doi: 10.1146/annurev.publhealth.21.1.247. http://dx.doi.org/10.1146/annurev.publhealth.21.1.247. [DOI] [PubMed] [Google Scholar]
- Runyan CW, Dal Santo J, Schulman M, Lipscomb HJ, Harris TA. Work hazards and workplace safety violations experienced by adolescent construction workers. Archives of Pediatrics and Adolescent Medicine. 2006;160(7):721–727. doi: 10.1001/archpedi.160.7.721. http://dx.doi.org/10.1001/archpedi.160.7.721. [DOI] [PubMed] [Google Scholar]
- Runyan CW, Schulman M, Dal Santo J, Bowling JM, Agans R, Ta M. Work-related hazards and workplace safety of US adolescents employed in the retail and service sectors. Pediatrics. 2007;119(3):526–534. doi: 10.1542/peds.2006-2009. http://dx.doi.org/10.1542/peds.2006-2009. [DOI] [PubMed] [Google Scholar]
- Runyan CW, Schulman M, Hoffman CD. Understanding and preventing violence against adolescent workers: what is known and what is missing? Clinics in Occupational and Environmental Medicine. 2003;3:711–720. [Google Scholar]
- Runyan CW, Schulman MD, Scholl LE. Adolescent employment and injury in the United States. In: Liller KD, editor. Injury prevention for children and adolescents: Research, practice, and advocacy. 2. Washington, DC: American Public Health Association; 2012. pp. 189–214. [Google Scholar]
- Safe Work Australia. The cost of work-related injury and illness for Australian employers, workers and the community: 2008–09. 2012 Retrieved from http://www.safeworkaustralia.gov.au/sites/SWA/about/Publications/Documents/660/Cost%20of%20Work-related%20injury%20and%20disease.pdf.
- Sallis JF, Owen N, Fisher EB. Ecological models of health behavior. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: Theory, research, and practice. Philadelphia, PA: John Wiley & Sons; 2008. pp. 466–485. [Google Scholar]
- Salminen S. Have young workers more injuries than older ones? An international literature review. Journal of Safety Research. 2004;35(5):513–521. doi: 10.1016/j.jsr.2004.08.005. http://dx.doi.org/10.1016/j.jsr.2004.08.005. [DOI] [PubMed] [Google Scholar]
- Saterfiel TH, McLarty JR. ERIC digest: Assessing employability skills. 1995 Retrieved from http://www.counseling.org/Resources/Library/ERIC%20Digests/95-21.pdf.
- Schulte PA, Stephenson CM, Okun AH, Palassis J, Biddle E. Integrating occupational safety and health information into vocational and technical education and other workforce preparation programs. American Journal of Public Health. 2005;95(3):404–411. doi: 10.2105/AJPH.2004.047241. http://dx.doi.org/10.2105/AJPH.2004.047241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sleet DA, Ballesteros MF, Borse NN. A review of unintentional injuries in adolescents. Annual Review of Public Health. 2010;31:195–212. doi: 10.1146/annurev.publhealth.012809.103616. [DOI] [PubMed] [Google Scholar]
- Smith TD, DeJoy DM. Occupational injury in America: An analysis of risk factors using data from the General Social Survey (GSS) Journal of Safety Research. 2012;43(1):67–74. doi: 10.1016/j.jsr.2011.12.002. [DOI] [PubMed] [Google Scholar]
- Spear LP. The adolescent brain and age-related behavioral manifestations. Neuroscience and Biobehavioral Reviews. 2000;24(4):417–463. doi: 10.1016/s0149-7634(00)00014-2. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10817843) [DOI] [PubMed] [Google Scholar]
- Steers WN, Elliott E, Nemiro J, Ditman D, Oskamp S. Health beliefs as predictors of HIV-preventive behavior and ethnic differences in prediction. Journal of Social Psychology. 1996;136(1):99–110. doi: 10.1080/00224545.1996.9923032. http://dx.doi.org/10.1080/00224545.1996.9923032. [DOI] [PubMed] [Google Scholar]
- Steinberg L. Risk taking in adolescence: What changes, and why? Annals of the New York Academy of Sciences. 2004;1021:51–58. doi: 10.1196/annals.1308.005. http://dx.doi.org/10.1196/annals.1308.005. [DOI] [PubMed] [Google Scholar]
- Steinberg L. Cognitive and affective development in adolescence. Trends in Cognitive Sciences. 2005;9(2):69–74. doi: 10.1016/j.tics.2004.12.005. http://dx.doi.org/10.1016/j.tics.2004.12.005. [DOI] [PubMed] [Google Scholar]
- Steinberg L. Adolescent risk taking: A social neuroscience perspective. In: Amsel E, Smetana J, editors. Adolescent vulnerabilities and opportunities: Constructivist developmental perspectives. Cambridge, UK: Cambridge University Press; 2011. pp. 41–64. [Google Scholar]
- Stokols D, Pelletier KR, Fielding JE. The ecology of work and health: research and policy directions for the promotion of employee health. Health Education Quarterly. 1996;23(2):137–158. doi: 10.1177/109019819602300202. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8744869) [DOI] [PubMed] [Google Scholar]
- Sudhinaraset M, Blum RW. The unique developmental considerations of youth-related work injuries. International Journal of Occupational and Environmental Health. 2010;16(2):216–222. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/20465066) [PubMed] [Google Scholar]
- Suruda A, Philips P, Lillquist D, Sesek R. Fatal injuries to teenage construction workers in the US. American Journal of Industrial Medicine. 2003;44(5):510–514. doi: 10.1002/ajim.10304. http://dx.doi.org/10.1002/ajim.10304. [DOI] [PubMed] [Google Scholar]
- Symonds WC, Schwartz RB, Ferguson R. Pathways to prosperity: meeting the challenge of preparing young Americans for the 21st century. 2011 Retrieved from http://dash.harvard.edu/bitstream/handle/1/4740480/Pathways_to_Prosperity_Feb2011-1.pdf?sequence=1.
- The Conference Board, Partnership for 21st Century Skills, Corporate Voices for Working Families, & Society for Human Resource Management. Are they really ready to work? Employers’ perspectives on the basic knowledge and applied skills of new entrants to the 21st century U.S. workforce. 2006 Retrieved from http://www.conferenceboard.org/pdf_free/BED-06-Workforce.pdf.
- Towner E, Dowswell T, MacKereth C, Jarvis S. What works in preventing unintentional injuries in children and adolescents? An updated systematic review. London, UK: Health Development Agency; 2001. [Google Scholar]
- Tucker S, Turner N. Waiting for safety: Responses by young Canadian workers to unsafe work. Journal of Safety Research. 2013;45:103–110. doi: 10.1016/j.jsr.2013.01.006. http://dx.doi.org/10.1016/j.jsr.2013.01.006. [DOI] [PubMed] [Google Scholar]
- U.S. Bureau of Labor Statistics. Work activity of high school students: Data from the National Longitudinal Survey of Youth 1997. 2005 Retrieved from http://www.bls.gov/news.release/archives/nlsyth_04272005.pdf.
- U.S. Bureau of Labor Statistics. Employer-reported workplace injury and illness summary. 2014a Retrieved from http://www.bls.gov/news.release/osh.nr0.htm.
- U.S. Bureau of Labor Statistics. Labor force statistics from the current population survey. Household data annual averages: employment status of the civilian noninstitutional population by age, sex, and race. 2014b Retrieved from http://www.bls.gov/cps/demographics.htm#age\.
- U.S. Bureau of Labor Statistics. Economic news release: Census of fatal occupational injuries summary 2013. 2015 Retrieved from http://www.bls.gov/iif/oshwc/cfoi/cfch0012.pdf.
- U.S. Department of Labor. Competency models: A review of the literature and the role of the Employment and Training Administration (ETA) 2008 Retrieved from http://wdr.doleta.gov/research/FullText_Documents/Competency%20Models%20-%20A%20Review%20of%20Literature%20and%20the%20Role%20of%20the%20Employment%20and%20Training%20Administration.pdf.
- Weinstein ND. Unrealistic optimism about susceptibility to health problems: conclusions from a community-wide sample. Journal of Behavioral Medicine. 1987;10(5):481–500. doi: 10.1007/BF00846146. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/3430590) [DOI] [PubMed] [Google Scholar]
- Westaby JD, Lowe JK. Risk-taking orientation and injury among youth workers: Examining the social influence of supervisors, coworkers, and parents. Journal of Applied Psychology. 2005;90(5):1027–1035. doi: 10.1037/0021-9010.90.5.1027. http://dx.doi.org/10.1037/0021-9010.90.5.1027. [DOI] [PubMed] [Google Scholar]
- Wilson MG, DeJoy DM, Vandenberg RJ, Richardson HA, McGrath AL. Work characteristics and employee health and well-being: Test of a model of healthy work organization. Journal of Occupational and Organizational Psychology. 2004;77(4):565–588. [Google Scholar]
- World Health Organization. Introduction and guidelines to facilitate the development and implementation of life skills programs. Geneva, Switzerland: World Health Organization; 1997. Life skills education for children and adolescents in schools. [Google Scholar]
- Zakocs RC, Runyan CW, Schulman MD, Dunn KA, Evensen CT. Improving safety for teens working in the retail trade sector: Opportunities and obstacles. American Journal of Industrial Medicine. 1998;34(4):342–350. doi: 10.1002/(sici)1097-0274(199810)34:4<342::aid-ajim7>3.0.co;2-u. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9750940) [DOI] [PubMed] [Google Scholar]
- Zimet GD, Liau A, Fortenberry VD. Health beliefs and intention to get immunized for HIV. The Journal of Adolescent Health. 1997;20(5):354–359. doi: 10.1016/s1054-139x(97)00031-1. (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9168382) [DOI] [PubMed] [Google Scholar]