Abstract
OBJECTIVE
Long-term data validating glycated hemoglobin (HbA1c) in assessing the risk of type 2 diabetes in children are limited. HbA1c, fasting plasma glucose (FPG), and 2-h postload plasma glucose (2hPG) concentrations were measured in a longitudinal study of American Indians to determine their utility in predicting incident diabetes, all of which is thought to be type 2 in this population.
RESEARCH DESIGN AND METHODS
Incident diabetes (FPG ≥126 mg/dL [7.0 mmol/L], 2hPG ≥200 mg/dL [11.1 mmol/L], HbA1c ≥6.5% [8 mmol/mol], or clinical diagnosis) was determined in 2,095 children without diabetes ages 10–19 years monitored through age 39, and in 2,005 adults ages 20–39 monitored through age 59. Areas under the receiver operating characteristic (ROC) curve for HbA1c, FPG, and 2hPG in predicting diabetes within 10 years were compared.
RESULTS
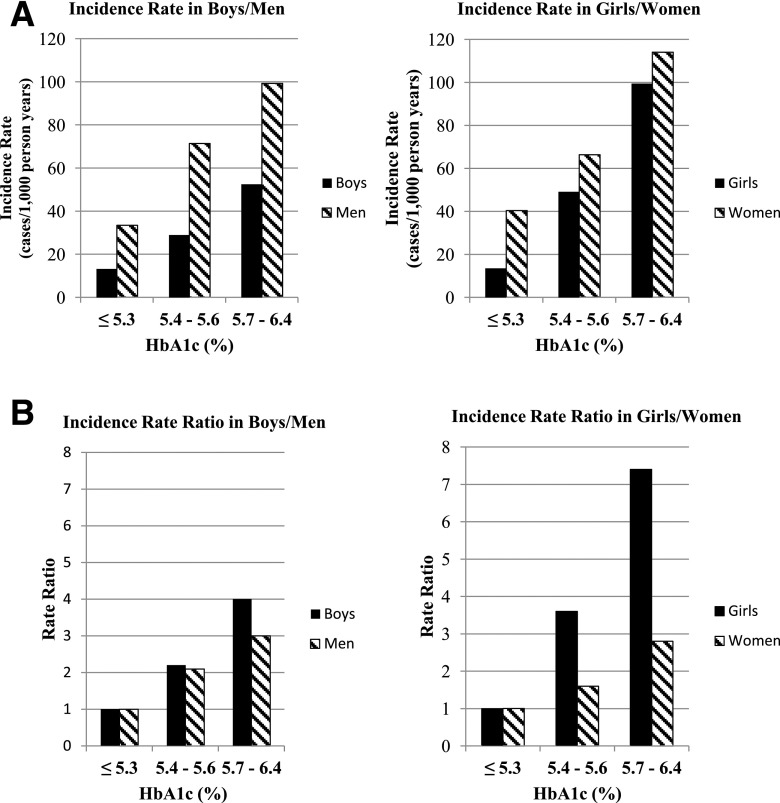
During long-term follow-up of children and adolescents who did not initially have diabetes, the incidence rate of subsequent diabetes was fourfold (in boys) as high and more than sevenfold (in girls) as high in those with HbA1c ≥5.7% as in those with HbA1c ≤5.3%—greater rate ratios than experienced by adults in the same HbA1c categories. Analyses of ROCs revealed no significant differences between HbA1c, FPG, and 2hPG in sensitivity and specificity for identifying children and adolescents who later developed diabetes.
CONCLUSIONS
HbA1c is a useful predictor of diabetes risk in children and can be used to identify prediabetes in children with other type 2 diabetes risk factors with the same predictive value as FPG and 2hPG.
Introduction
The prevalence of type 2 diabetes has increased among youth in the U.S.; between 2001 and 2009, there was a 30.5% rise in the overall prevalence of diagnosed diabetes (1,2). Many youth diagnosed with type 2 diabetes have poor glycemic control (2,3) and experience higher rates of cardiovascular disease risk markers, fatty liver disease, and early evidence of microvascular complications (2,4,5). This highlights the need for early detection of prediabetes to prevent the increase in diabetes and its associated cardiometabolic risk factors.
The American Diabetes Association (ADA) recommends glycated hemoglobin (HbA1c) as a diagnostic test for diabetes. This guideline is based on adult epidemiological studies that show an association between increased HbA1c and the risk for microvascular complications (6–8). Longitudinal studies investigating the relationship between HbA1c in childhood and the risk of developing diabetes are lacking. In addition, few pediatric studies have compared HbA1c with other measures of glycemia such as fasting plasma glucose (FPG) and 2-h postload plasma glucose (2hPG).
In the 2016 Standards of Medical Care in Diabetes, the ADA recognized that data supporting HbA1c as a diagnostic measure for diabetes are limited in children and adolescents (9) while noting that past short-term studies did not address the more pertinent relationship between HbA1c and long-term health outcomes. The ADA recommends screening for type 2 diabetes or prediabetes using HbA1c in asymptomatic children and adolescents aged ≥10 years with a BMI ≥85th percentile for age and sex, based on Centers for Disease Control and Prevention growth charts (10), and at least two additional type 2 diabetes risk factors (9). Risk factors include type 2 diabetes in a first- or second-degree relative, minority race or ethnicity, signs of insulin resistance, or maternal history of diabetes or gestational diabetes during the child’s gestation (9).
Measuring HbA1c is convenient in children because it does not require fasting, and a single test can be used to both diagnose and monitor glycemic control, thereby facilitating sample collection and compliance in children. In addition, HbA1c reflects chronic glycemia and has less preanalytical and analytical variability than FPG and 2hPG (9,11).
In our current study, HbA1c, FPG, and 2hPG were measured in a longitudinal study of American Indian children, adolescents, and adults to assess the ability of these measurements to predict the development of diabetes, as defined by the ADA. This study examined the extent to which the ADA-recommended definitions of prediabetes in children and adolescents predicted who would develop diabetes and compared the sensitivity and specificity of HbA1c, FPG, and 2hPG in predicting future diabetes.
Research Design and Methods
A longitudinal study of diabetes and related conditions was conducted among residents of an American Indian community in the southwestern U.S. from 1965 to 2007. Children ≥5 years and adults underwent comprehensive clinical examinations, which included detailed medical histories, anthropometric measurements, and biochemical tests. These children and adults were invited to return for research examinations every 2 years. All laboratory tests during the study period were performed at the National Institute of Diabetes and Digestive and Kidney Diseases laboratory located in Phoenix. HbA1c was measured from 1989 to 2000 by high-performance liquid chromatography using the Bio-Rad MDMS system; from 2001 to 2007, we used the A1C 2.2 Plus Glycohemoglobin Analyzer (Tosoh Medics, Inc.). A Bland-Altman analysis of 252 samples measured with each instrument indicated small systematic differences. Therefore, a linear regression equation was used to convert the older assay results to the newer assay: HbA1c new method = −0.1916 + (0.9829 × HbA1c old method). Our laboratory has followed the National Glycohemoglobin Standardization Program assay standardization recommendations since its inception. At each research examination, FPG and HbA1c were measured in fasting venous blood, and 2hPG was measured after a 75-g oral glucose tolerance test (OGTT).
The National Institute of Diabetes and Digestive and Kidney Diseases Institutional Review Board approved the study. Written informed consent was obtained from adults and from parents of the minors, and assent was obtained from the minors.
Criteria for inclusion in this analysis were HbA1c, FPG, and 2hPG measures performed when the participant was 10 through 19 years of age at his or her first examination without diabetes, and at least one follow-up examination before the 40th birthday, which yielded 2,095 children and adolescents. The adult comparison cohort consisted of those with a first baseline examination when they did not have diabetes from age 20 through 39 years with all three glycemic measures and a follow-up examination before the 60th birthday, which yielded 2,005 adults. A person could be counted in each cohort if seen at the appropriate ages. Subjects who gave a history of possibly taking metformin at baseline were excluded. Diabetes was defined at baseline and follow-up by the current ADA criteria: FPG ≥126 mg/dL (7.0 mmol/L), 2hPG ≥200 mg/dL (11.1 mmol/L), HbA1c ≥6.5% (48 mmol/mol) (9), or a previous clinical diagnosis. Prediabetes was defined as HbA1c levels between 5.7 and 6.4%, FPG between 100 and 125 mg/dL, or 2hPG between 140 and 199 mg/dL (9).
Statistical analyses were conducted using SAS 9.4 software (SAS Institute, Inc., Cary, NC). Diabetes incidence per 1,000 person-years was calculated using the number of incident cases of diabetes and person-years of follow-up through age 39 for the child cohort and through age 59 for the adult cohort. Sex-stratified areas under the receiver operating characteristic (ROC) curve (AUC) and standard errors for HbA1c, FPG, and 2hPG predicting diabetes were calculated by the method of Pencina and D’Agostino (12); the AUCs were compared by the method of DeLong et al. (13). AUCs allow for a quantitative comparison of the discriminatory power of the different tests. For graphical purposes, ROC curves were derived for each variable, based on predicting the cumulative incidence at 10 years. In brief, ROC curves for each test measure were drawn by modeling the survival probability with the PHREG procedure in SAS using successive detection thresholds for HbA1c (incremented by 0.1%), FPG (incremented by 2 mg/dL), or 2hPG (incremented by 5 mg/dL) and calculating the 10-year cumulative incidence of diabetes in those above and below the threshold from the baseline hazard and the hazard ratio associated with being above the threshold. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) at each threshold (at 10 years of follow-up) were calculated from these cumulative incidence values and the proportion exceeding the threshold at baseline.
Results
Baseline Characteristics
Among 2,095 children and adolescents at baseline, 588 (28.1%) were categorized as normal weight (BMI <85th percentile for age and sex), 394 (18.8%) were overweight (BMI ≥85th to <95th percentile), and 1,113 (53.1%) were obese. In the adult cohort at baseline, 143 (7.1%) had BMI <25 kg/m2, 383 (19.1%) had a BMI between 25 and 30 kg/m2, and 1,479 (73.8%) were obese with a BMI ≥30 kg/m2.
Adult and pediatric participants were classified into prediabetes (5.7–6.4%), intermediate (5.4–5.6%), or lower (≤5.3%) baseline HbA1c categories. The prevalence of prediabetes by HbA1c ≥5.7% was 3.0% in the children and adolescents and 8.4% in the adults, and by FPG ≥100 mg/dL, the prevalence was 9.2% in children and adolescents and 21.1% in adults. The prevalence of impaired glucose tolerance (2hPG ≥140 mg/dL) was 8.1% in children and adolescents and 17.3% in adults. Baseline characteristics are reported in Table 1 for the pediatric and adult cohorts, stratified by HbA1c. FPG, 2hPG, and BMI values increased with HbA1c strata in children and adults. Supplementary Table 1 lists the Spearman correlation coefficients between HbA1c, FPG, and 2hPG in children and adults. Age-sex stratified Venn diagrams representing the overlap in prediabetes definitions at baseline by HbA1c, FPG, and 2hPG are presented in Supplementary Figs. 1 and 2.
Table 1.
Baseline characteristics of child and adult cohorts, stratified by HbA1c level
| HbA1c (%) | |||
|---|---|---|---|
| ≤5.3 | 5.4–5.6 | 5.7–6.4 | |
| Children | |||
| Total (n) | 1,795 | 238 | 62 |
| Male (n) | 831 | 97 | 13 |
| Female (n) | 964 | 141 | 49 |
| Age (years) | 14.1 (12.5–16.1) | 13.8 (12–16) | 14 (11.8–15.3) |
| Follow-up (years) | 6.0 (3–10) | 3.1 (2–6.1) | 2.3 (1.9–4) |
| BMI (kg/m2) | 26.0 (22.0–31.0) | 30.0 (25.0–35.0) | 32.0 (28.0–38.0) |
| BMI (percentile) | 94.9 (79.6–98.4) | 98.2 (94.6–99.2) | 98.7 (97–99.3) |
| HbA1c (%) | 4.9 (4.6–5.1) | 5.5 (5.4–5.5) | 5.7 (5.7–5.9) |
| FPG (mg/dL) | 89 (85–94) | 91 (86–96) | 93.5 (88–98) |
| 2hPG (mg/dL) | 101 (87–116) | 107 (92–125) | 116.5 (103–149) |
| Adults | |||
| Total (n) | 1,466 | 371 | 168 |
| Male (n) | 587 | 141 | 72 |
| Female (n) | 879 | 230 | 96 |
| Age (years) | 29.0 (24.1–33.3) | 28.4 (23.6–34.1) | 29.9 (23.8–34.2) |
| Follow-up (years) | 5.2 (3.1–8.4) | 3.6 (2.2–6.3) | 3.2 (2.0–5.4) |
| BMI (kg/m2) | 33.0 (28.7–38.0) | 36.6 (32.7–42.0) | 39.1 (34.3–45.2) |
| HbA1c (%) | 4.9 (4.7–5.1) | 5.5 (5.4–5.6) | 5.8 (5.7–5.9) |
| FPG (mg/dL) | 90.0 (85.0–97.0) | 95.0 (89.0–101.0) | 98.0 (91.0–105.0) |
| 2hPG (mg/dL) | 106.0 (88.0–124.0) | 114 (93–141.0) | 120.0 (102.0–148.0) |
Data are shown as median (interquartile range) or as indicated.
Incidence of Diabetes by HbA1c
Median follow-up time to the diagnosis of diabetes or the last examination before diabetes developed in the pediatric cohort was 5.2 years (interquartile range [IQR] 2.7–9.6). Median follow-up was 4.6 years (IQR 2.8–7.9) in the adults. Total person-years of follow-up were 13,528 in children and 11,520 in adults. The sex-stratified incidence of diabetes by baseline HbA1c category in children and adults is shown in Fig. 1A. The incidence rates exhibited a similar pattern of risk increase in the higher HbA1c categories in children and adolescents and in adults (Fig. 1A). Although the incidence rates were higher in adults, the rate ratios comparing higher HbA1c categories with the lowest category of HbA1c were the same or higher in children (Fig. 1B). Male children and adolescents in the highest HbA1c category (5.7–6.4%) at baseline had a fourfold higher incidence of diabetes, and female children and adolescents in the same HbA1c range at baseline had a sevenfold higher incidence of diabetes during follow-up than their counterparts in the lowest HbA1c category (Fig. 1B).
Figure 1.
Incidence of type 2 diabetes by HbA1c category stratified by sex. Data are presented as incidence rates (cases/1,000 person-years) (A) and as incidence rate ratios (using the incidence in the lowest HbA1c category as the reference rate) (B).
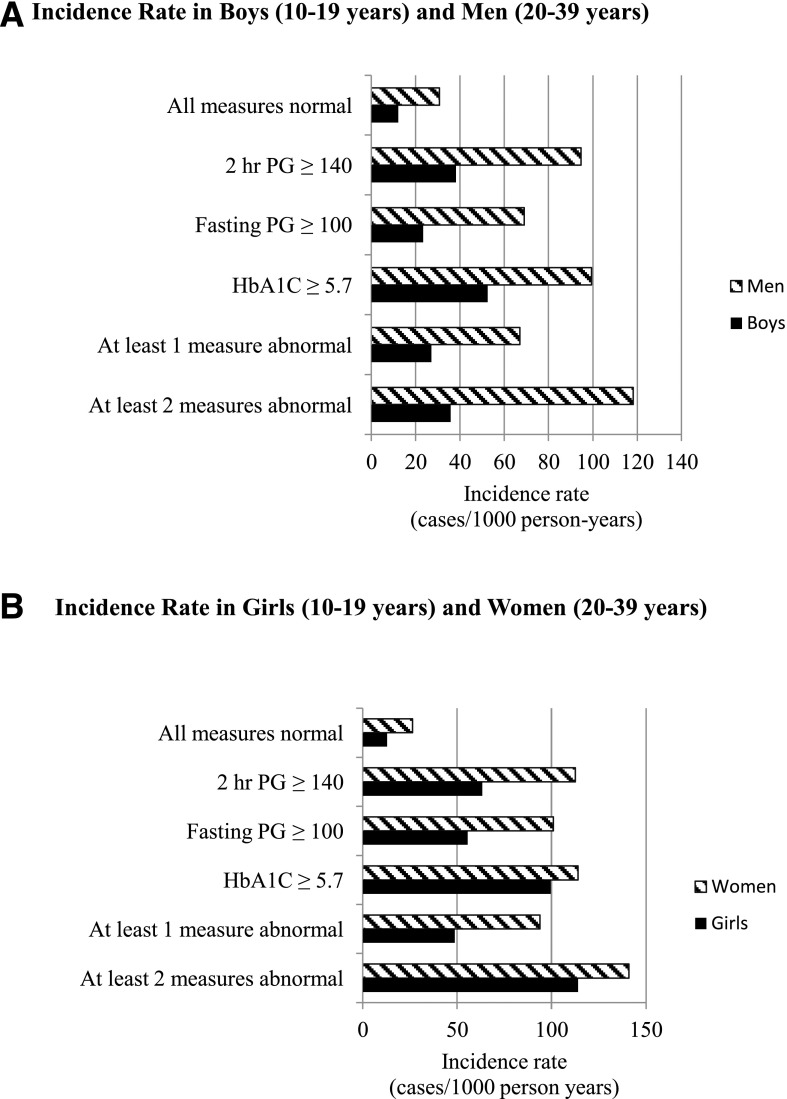
HbA1c, FPG, and 2hPG Predicting Diabetes in Children and Adults
Figure 2 shows the incidence of diabetes by different glycemic measures at baseline stratified by age and sex. Among children and adolescents in both sexes, all three glycemic measures were similarly predictive.
Figure 2.
Incidence of type 2 diabetes by various glycemic measures at baseline stratified by age and sex. PG, plasma glucose. Data are presented as incidence rates (cases/1,000 person-years)
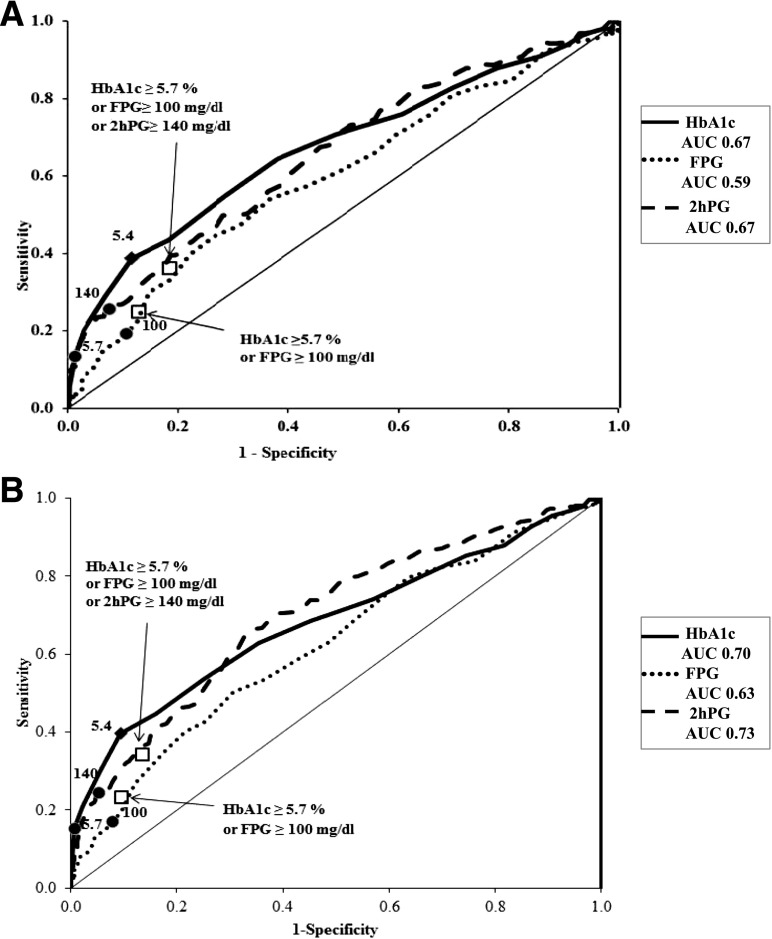
Supplementary Table 2 lists the AUCs for each of the three tests in boys, girls, men, and women. In boys, girls, and men, the AUC for HbA1c did not differ significantly from that of FPG or 2hPG. Only in women did the HbA1c have a lower AUC than 2hPG (0.63 vs. 0.70, P = 0.0012). Supplementary Table 3 reports the sensitivities and specificities from which these AUCs were derived. The lack of a significant difference in AUC between HbA1c and the glucose measures suggests that all three tests have the potential to offer the same level of sensitivity and specificity, depending on the threshold chosen.
Clinical Utility of HbA1c
Although adults may undergo HbA1c screening regardless of weight, the ADA recommends testing children and adolescents ≥10 years only if their BMI is in the overweight or obese range and if they have two additional risk factors. All children and adolescents in this study had at least one risk factor, American Indian ethnicity. We classified the pediatric subjects as having parental diabetes if at least one parent was diagnosed with diabetes before the age of 45 years. The ROC curves in Fig. 3A represent the sensitivity and specificity of HbA1c, FPG, and 2hPG within this already higher-risk population of American Indian children and adolescents who were overweight or obese and had at least one parent with diabetes. Figure 3B depicts the same curves for the full child cohort. Among the children and adolescents who met the recommended screening criteria (overweight or obese with two additional risk factors), the estimated 10-year cumulative incidence of diabetes in those with HbA1c ≥5.7% was 78% (i.e., PPV) and the 10-year cumulative incidence in those with HbA1c<5.7% was 23% (i.e., NPV = 100% – 23% = 77%). For FPG ≥100 mg/dL, the PPV was 36% and the NPV was 78%, and for 2hPG ≥140 mg/dL, the PPV was 52% and the NPV was 80%. Differences among these values generally reflect that the specific thresholds for each test differ in specificity and sensitivity; comparable PPV and NPV could be obtained by changing the thresholds.
Figure 3.
Sensitivity and specificity of HbA1c, FPG, and 2hPG in identifying persons who developed diabetes within 10 years of screening among children and adolescents meeting ADA recommended criteria for screening (A) and among all children and adolescents in the study (B). The black circles indicate the current ADA thresholds for prediabetes for each of the three tests. The squares represent the sensitivity and specificity offered by different combinations of current ADA thresholds. The diamond indicates the arbitrary HbA1c threshold of 5.4%.
The current ADA thresholds for prediabetes for each of the three tests have been depicted using circular points on the ROC curves in Fig. 3, and their proximity to each other indicates that these thresholds offer a similar sensitivity and specificity. Thus, the testing method used does not affect the sensitivity and specificity with which we are able to predict diabetes in children and adolescents. An arbitrary HbA1c threshold of 5.4% is marked with a diamond point in Fig. 3, with a higher sensitivity (40% in the high-risk group) but a lower specificity (89% in the high-risk group). The square points in Fig. 3 represent the sensitivity and specificity offered by different combinations of current ADA thresholds. These combinations do offer a higher sensitivity than any one ADA threshold alone at the expense of lower specificity.
Conclusions
Few large longitudinal studies have assessed the predictive value of HbA1c measured in childhood and adolescence in predicting incident diabetes. The prevalence of prediabetes defined by impaired fasting glucose (IFG) and IGT among 12–19 year old adolescents in the U.S. based on the 2005–2006 National Health and Nutrition Examination Survey (NHANES) was 12.7% and 3.4% respectively (14). In our current study among subjects aged 10 to 19 years, the IFG prevalence at baseline was 9.2%, and the IGT prevalence, 8.1%, was higher than in NHANES. In the current study, HbA1c was a useful predictor of future diabetes in all age and sex categories, performing as well as or better than other measures of glycemia, except in adult women, among whom 2hPG had a significantly higher AUC than HbA1c. HbA1c, FPG, and 2hPG also had very similar discriminatory power within the subset of high-risk children identified by ADA criteria.
The reason for the poorer performance of HbA1c in adult women is uncertain. Women participants were not pregnant at baseline but of reproductive age. Iron deficiency is common in women of reproductive age, and depleted iron stores affect glycation rates and elevate HbA1c. A study from the NHANES (1999–2006) showed iron deficiency was common among women (13.7%) and was associated with higher HbA1c primarily at the lower end of the HbA1c distribution (15). In the absence of iron studies in our cohort, we are unable to evaluate whether iron deficiency altered the HbA1c at baseline among the women.
Some recent studies have expressed skepticism about using adult HbA1c threshold values for diagnosing prediabetes and diabetes in children and adolescents. These studies tend to rely on cross-sectional comparisons of HbA1c with previously established measures of glycemia and showed poor correlation of HbA1c with FPG or 2hPG. Our current study differs, however, because we examined the value of HbA1c in predicting diabetes, not in associating with IFG or IGT. Clearly, there is little overlap among the three categorical definitions of prediabetes based on HbA1c, FPG, and 2hPG, as is well recognized in adults and as we found in children and adolescents as well as in adults (Supplementary Figs. 1 and 2). We suggest the goal of screening is to identify those at high risk of developing diabetes (or who already have it) rather than detecting those who have prediabetes by different criteria. In this respect, the HbA1c performs as well as the other tests.
The ADA includes HbA1c as a diagnostic measure for diabetes because of its association with long-term microvascular complications in adults, including retinopathy and diabetic nephropathy. This recommendation included adult participants from the same study population we describe here, and we reported previously that HbA1c and FPG measurements in adults were just as useful as 2hPG in predicting the risk of microvascular complications (16). Another study in this population found that a sharp rise in incidence of these complications occurred at the same level of glycemia in youth and adult cohorts; however, that study compared only FPG and 2hPG (17).
In the current study, we also stratified by ADA-recommended risk factors (9). All of the subjects had at least one risk factor, American Indian ethnicity. We further stratified the cohort based on those who had at least one parent with diabetes onset before age 45 years, those who were overweight or obese, or both. We used the parental onset age of 45 years because we previously showed that the prevalence of type 2 diabetes is particularly high in offspring whose parents both had diabetes before age 45 in this population (18). We find that the current prediabetes definition of HbA1c ≥5.7% had a sensitivity of ∼13% and a specificity of ∼99% in overweight children with two additional risk factors (one risk factor unique to our study being American Indian ethnicity) for predicting the 10-year incidence of diabetes. Of course, the sensitivity would be increased by using a lower threshold; for example, sensitivity was 39% and specificity 88% at an HbA1c ≥5.4% (Fig. 3).
Our study was conducted in a specific population group with a high prevalence of diabetes that is almost exclusively type 2 diabetes (18). Past studies have established that mutations in the maturity-onset diabetes of the young genes are not a major cause of diabetes among youth in this population (19). Though variation in HbA1c reliability has been reported among African, Mediterranean, and Southeast Asian populations, hemoglobinopathies prevalent in these populations that could interfere with the HbA1c interpretation have not been commonly reported in American Indians (20). HbA1c results also vary with red cell dynamics and assay methods (21–23). Thus, the generalizability of our results to populations with a lower prevalence of type 2 diabetes, a higher prevalence of type 1 diabetes, or a higher prevalence of hemoglobinopathies or disorders affecting hemoglobin turnover is uncertain.
The strengths of our study include both a large pediatric and adult cohort, examinations with all three glycemia tests performed at the same time, and an extensive longitudinal follow-up period. Also, all of our laboratory tests, including HbA1c assays, were performed at the same laboratory using standardized methods.
In summary, higher HbA1c at baseline predicted a higher incidence of diabetes in both children and adults. Although the absolute incidence rates were greater in adults, the incidence rate ratios were the same or greater in children. When incidence rates were compared with various abnormalities in glycemic measures (HbA1c, FPG, and 2hPG) at baseline, individually or combined, HbA1c performed as well as FPG and 2hPG in boys, girls, and men, but not as well as 2hPG in adult women. We therefore conclude that HbA1c can be used to assess risk for diabetes in children or to identify children with prediabetes with the same confidence as FPG or 2hPG.
Supplementary Material
Article Information
Acknowledgments. The authors thank the participants and their parents for participation in the study.
Funding. This research was supported by the Intramural Research Program of the National Institute of Diabetes and Digestive and Kidney Diseases.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. P.V. designed the study, performed the analyses, and assisted in drafting the manuscript. R.G.N. assisted in study design, obtained study data, and critically reviewed the manuscript. R.L.H. obtained study data and assisted in study design, data analysis, and critical review of the manuscript. W.C.K. obtained study data, conceptualized the study, assisted in study design and data analysis, and drafted the initial manuscript. M.S. conceptualized the study, assisted in study design and data analysis, drafted the initial manuscript, and had final responsibility for the decision to submit for publication. All authors approved the final manuscript as submitted. M.S. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Parts of this study were presented in abstract form as an oral presentation at the 76th Scientific Sessions of the American Diabetes Association, New Orleans, LA, 10–14 June, 2016.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc16-1358/-/DC1.
References
- 1.Dabelea D, Mayer-Davis EJ, Saydah S, et al.; SEARCH for Diabetes in Youth Study . Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA 2014;311:1778–1786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hamman RF, Bell RA, Dabelea D, et al.; SEARCH for Diabetes in Youth Study Group . The SEARCH for Diabetes in Youth study: rationale, findings, and future directions. Diabetes Care 2014;37:3336–3344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Petitti DB, Klingensmith GJ, Bell RA, et al.; SEARCH for Diabetes in Youth Study Group. Glycemic control in youth with diabetes: the SEARCH for Diabetes in Youth Study. J Pediatr 2009;155:668–672 e1-3 [DOI] [PMC free article] [PubMed]
- 4.Rodriguez BL, Fujimoto WY, Mayer-Davis EJ, et al. . Prevalence of cardiovascular disease risk factors in U.S. children and adolescents with diabetes: the SEARCH for Diabetes in Youth study. Diabetes Care 2006;29:1891–1896 [DOI] [PubMed] [Google Scholar]
- 5.Kershnar AK, Daniels SR, Imperatore G, et al. . Lipid abnormalities are prevalent in youth with type 1 and type 2 diabetes: the SEARCH for Diabetes in Youth Study. J Pediatr 2006;149:314–319 [DOI] [PubMed] [Google Scholar]
- 6.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care 2010;33(Suppl. 1):S62–S69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.International Expert Committee International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care 2009;32:1327–1334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Expert Committee on the Diagnosis and Classification of Diabetes Mellitus Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 1997;20:1183–1197 [DOI] [PubMed] [Google Scholar]
- 9.American Diabetes Association Sec. 2. Classification and diagnosis of diabetes. In Standards of Medical Care in Diabetes—2016. Diabetes Care 2016;39(Suppl. 1):S13–S22 [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Defining Childhood Obesity. Available at http://www.cdc.gov/obesity/childhood/defining.html. Accessed 9 June 2016
- 11.Lippi G, Targher G. A laboratory standpoint on the role of hemoglobin A1c for the diagnosis of diabetes in childhood: more doubts than certainties? Pediatr Diabetes 2011;12:183–186 [DOI] [PubMed] [Google Scholar]
- 12.Pencina MJ, D’Agostino RB. Overall C as a measure of discrimination in survival analysis: model specific population value and confidence interval estimation. Stat Med 2004;23:2109–2123 [DOI] [PubMed] [Google Scholar]
- 13.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 1988;44:837–845 [PubMed] [Google Scholar]
- 14.Cowie CC, Rust KF, Ford ES, et al. . Full accounting of diabetes and pre-diabetes in the U.S. population in 1988-1994 and 2005-2006. Diabetes Care 2009;32:287–294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim C, Bullard KM, Herman WH, Beckles GL. Association between iron deficiency and A1C levels among adults without diabetes in the National Health and Nutrition Examination Survey, 1999-2006. Diabetes Care 2010;33:780–785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McCance DR, Hanson RL, Charles MA, et al. . Comparison of tests for glycated haemoglobin and fasting and two hour plasma glucose concentrations as diagnostic methods for diabetes. BMJ 1994;308:1323–1328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krakoff J, Hanson RL, Kobes S, Knowler WC. Comparison of the effect of plasma glucose concentrations on microvascular disease between Pima Indian youths and adults. Diabetes Care 2001;24:1023–1028 [DOI] [PubMed] [Google Scholar]
- 18.Knowler WC, Pettitt DJ, Saad MF, Bennett PH. Diabetes mellitus in the Pima Indians: incidence, risk factors and pathogenesis. Diabetes Metab Rev 1990;6:1–27 [DOI] [PubMed] [Google Scholar]
- 19.Baier LJ, Permana PA, Traurig M, et al. . Mutations in the genes for hepatocyte nuclear factor (HNF)-1alpha, -4alpha, -1beta, and -3beta; the dimerization cofactor of HNF-1; and insulin promoter factor 1 are not common causes of early-onset type 2 diabetes in Pima Indians. Diabetes Care 2000;23:302–304 [DOI] [PubMed] [Google Scholar]
- 20.ACOG Committee on Obstetrics ACOG Practice Bulletin No. 78: hemoglobinopathies in pregnancy. Obstet Gynecol 2007;109:229–237 [DOI] [PubMed] [Google Scholar]
- 21.Cohen RM, Franco RS, Khera PK, et al. . Red cell life span heterogeneity in hematologically normal people is sufficient to alter HbA1c. Blood 2008;112:4284–4291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cohen RM, Snieder H, Lindsell CJ, et al. . Evidence for independent heritability of the glycation gap (glycosylation gap) fraction of HbA1c in nondiabetic twins. Diabetes Care 2006;29:1739–1743 [DOI] [PubMed] [Google Scholar]
- 23.Chan CL, McFann K, Newnes L, Nadeau KJ, Zeitler PS, Kelsey M. Hemoglobin A1c assay variations and implications for diabetes screening in obese youth. Pediatr Diabetes 2014;15:557–563 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.