Abstract
Background
Rates of physician burnout have increased in recent years, and high burnout levels are reported by physicians in training.
Objective
This review of the research on resident well-being seeks to identify factors associated with well-being, summarize well-being promotion interventions, and provide a framework for future research efforts.
Methods
Keywords were used to search PubMed, PsycINFO, and MEDLINE. Studies included were conducted between 1989 and 2014. The search yielded 82 articles, 26 which met inclusion criteria, and were assessed using the Medical Education Research Study Quality Instrument.
Results
Articles measured resident well-being and associated factors, predictors, effects, barriers, as well as interventions to improve well-being. Factors identified in psychological well-being research—autonomy, building of competence, and strong social relatedness—are associated with resident well-being. Sleep and time away from work are associated with greater resident well-being. Perseverance is predictive of well-being, and greater well-being is associated with increased empathy. Interventions focused on health and coping skills appear to improve well-being, although the 3 studies that examined interventions were limited by small samples and single site administration.
Conclusions
An important step in evolving research in this area entails the development of a clear definition of resident well-being and a scale for measuring the construct. The majority (n = 17, 65%) of existing studies are cross-sectional analyses of factors associated with well-being. The literature summarized in this review suggests future research should focus on factors identified in cross-sectional studies, including sleep, coping mechanisms, resident autonomy, building competence, and enhanced social relatedness.
Introduction
Physicians spend 3 to 7 years of their young adulthood in residency. Levinson,1 an adult development researcher, described ages 28 to 33 specifically as the “Age 30 Transition,” a time to complete early adulthood with pursuit of aspirations, establishment of a niche in society, and raising a family. Yet, in residency training, inherent structural constraints present barriers to satisfactory progression through this developmental stage. The intensity of training also is associated with significant reduction in well-being markers in residents, including sleep, exercise, family interactions, religious activity, and an increase in missing significant events.2 Well-being deficits that develop during residency also are present in practicing physicians. Satisfaction with work-life balance declined (48.5% versus 40.9%, P < .001) and burnout increased in physicians between 2011 and 2014. In contrast to physicians, minimal changes in satisfaction with work-life balance or in burnout were observed between 2011 and 2014 in other working US adults, demonstrating an increasing disparity in well-being among physicians relative to the general US working population.3 Furthermore, rates of burnout are increasing and more prevalent among younger physicians.4
The purpose of this study was to review the research on resident well-being, assess its quality, identify potential factors associated with resident well-being, summarize interventions that may have benefit in promoting resident well-being, and provide a framework for future research efforts in this area.
Methods
The following electronic databases were searched: MEDLINE, PubMed, and PsycINFO. Search words included “wellness,” “well-being,” and “residency,” as well as their synonyms.
Inclusion criteria of articles for review were as follows: (1) published in an English-language peer-reviewed journal from January 1989 to January 2014; (2) study was conducted no earlier than 1989; and (3) search words appear in the title and/or abstract. Studies were excluded if they did not focus primarily on well-being of residents, and if they focused specifically on duty hours. Many residency programs implemented significant changes after New York State adopted duty hour limits in 19895; therefore, 1989 was selected as the publication cutoff date.
The entire systematic review process was conducted by the author. The initial search identified 82 articles. Articles were further screened using the above inclusion criteria, and 53 were selected. Twenty-seven of these were excluded due to lack of focus on resident well-being or specific focus on duty hours. This resulted in a total of 26 articles for analysis in this review (figure 1). The Medical Education Research Study Quality Instrument (MERSQI) for quantitative studies was used to measure study quality.6
figure 1.
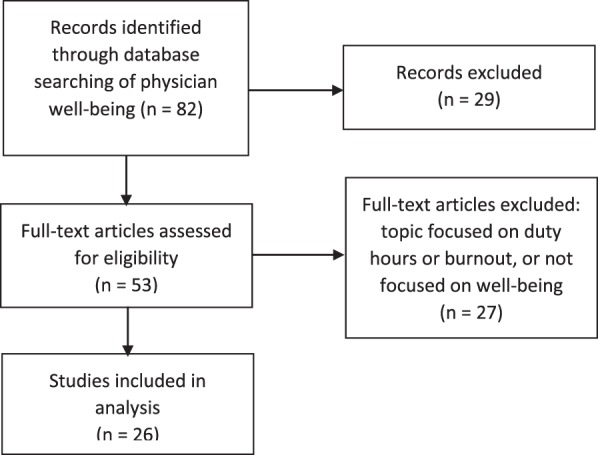
Review Selection Process and Results
Note: Twenty-nine of 82 articles were excluded after review of articles retrieved through database keyword search based on the following inclusion criteria: (1) published in an English-language peer-reviewed journal from January 1989 to January 2014 with study having been conducted since 1989; (2) search words appear in the title and/or abstract; and (3) primary well-being research with residents. Fifty-three full-text articles were assessed and were excluded if focused specifically on the issue of duty hours or burnout due to existing literature reviews that address this. This resulted in a total of 26 articles identified for inclusion.
Results
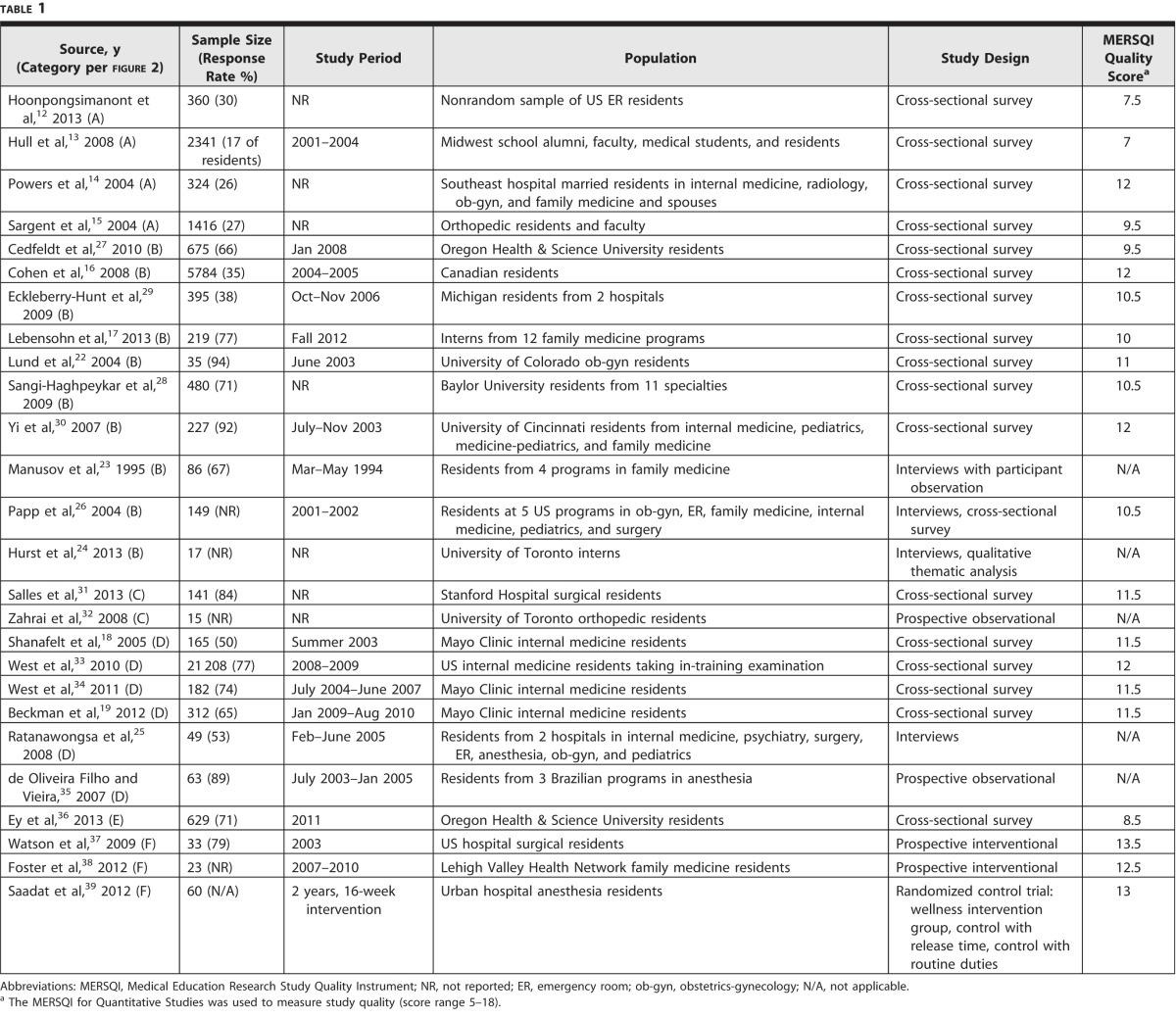
The majority (n = 17, 65%) of studies were cross-sectional, designed to determine associations between a number of personal or work characteristics and resident well-being. Twenty-one articles were quantitative research, and their average MERSQI for quantitative studies score was 10.8, with a range of 7 to 13.5 (possible MERSQI scores range from 5 to a maximum of 18). Often only specific specialties were studied, such as internal medicine, and most often studies were conducted in a single program. Tables 1 and 2 list the studies, study characteristics, measures of well-being, and significant findings of interest.
table 1.
Demographics and Characteristics of Studies Examining Resident Well-Being
table 2.
Measures and Findings of Studies Examining Resident Well-Being
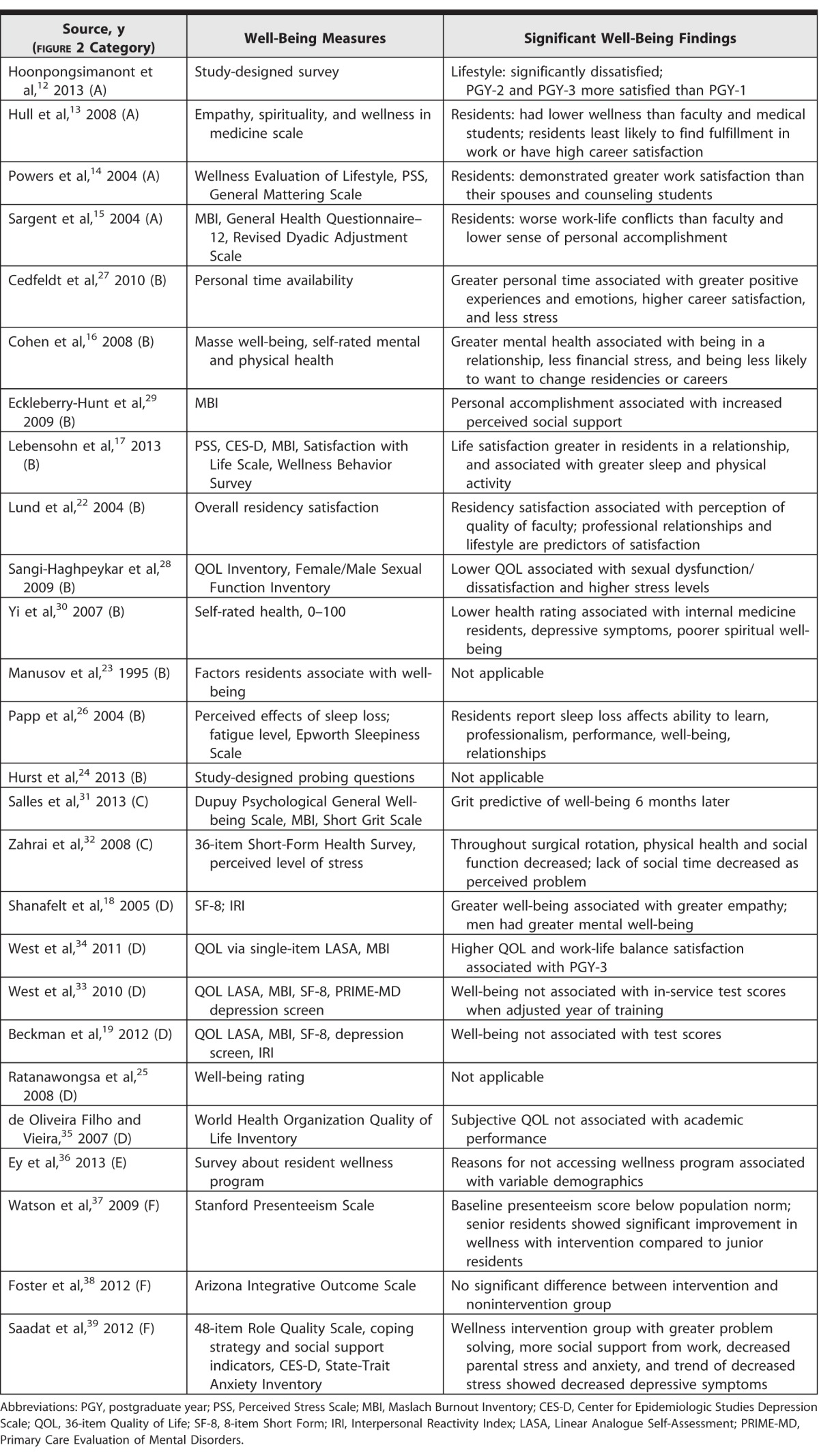
The studies used various scales to measure well-being, including the Satisfaction with Life Scale, accepted within psychology well-being research, which measures life satisfaction, positive mood, and absence of negative mood7,8; the World Health Organization–5, a well-being scale with less ceiling effect than the Short Form (SF) mental health subscale9; and the Postgraduate Hospital Education Environment Measure (PHEEM), which evaluates autonomy, teaching, and social support.10,11
Studies had several areas of focus—measurement of well-being, predictors and factors associated with well-being, effects of well-being, interventions to enhance well-being, and barriers to well-being interventions (figure 2).
figure 2.
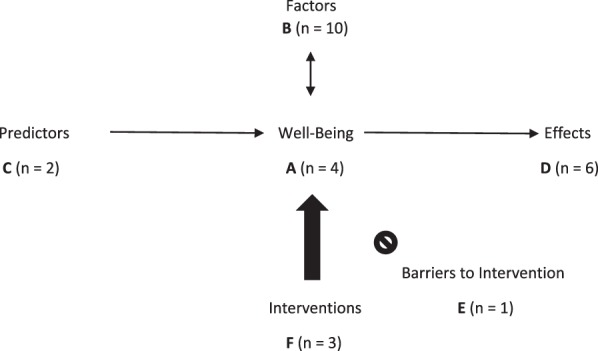
Focus Areas of Studies Investigating Resident Well-Being
Measurement of Resident Well-Being
Resident well-being overall was lower than population well-being norms in 7 of 8 studies.12–18 Comparing data that Beckman et al19 collected from 202 (63%) internal medicine residents, post hoc analysis of the SF-8 mental health subscore for residents shows lower well-being scores (mean scores 46.57 versus 50.5, respectively, P < .0001) than a similarly aged population norm.19,20 A large sample of Canadian residents self-rated their mental health lower than the Canadian population norm,16 and the mean perceived stress level in a large survey of family medicine interns was above population norms.17 Effect sizes are small and given the variety of well-being measures used across studies, no quantitative aggregate conclusions can be drawn.
Four studies drew comparisons of well-being between various groups (figure 2, group A). In a cross-sectional study comparing residents across postgraduate year (PGY), PGY-1 residents reported significantly less satisfaction with lifestyle than PGY-2 and PGY-3 residents (mean rating 1.29, 1.66, and 1.70, respectively, on a 0–4 scale, where 0 was completely dissatisfied; P < .001). There were no significant differences in their mean ratings of work relationships, work environment, or response to patients.12 Residents and their spouses did not differ in well-being or perceived stress, though response rate to this study was low at 26%.14
Two studies compared resident and faculty well-being. Residents, female residents in particular, had the lowest probability of scoring above the study population mean for well-being. They were also most likely to report frequent feelings of sadness or depression. Residents were 6 times less likely than medical students to report finding fulfillment in school or work, and residents were 13 times less likely than students to exhibit high overall career satisfaction, with attending physicians ranking between residents and students in these 2 areas.13 Similarly, in a survey of 384 orthopedic residents and 264 faculty across 64 programs, orthopedic residents reported significantly higher rates of emotional exhaustion (32% versus 28.4%, respectively; P < .04) and depersonalization (56% versus 24.8%, respectively; P < .0001) compared to faculty, and 18% of residents versus 10% of faculty scored in the low range of personal accomplishment (P < .009).
More residents reported a worse work-life balance than faculty (30% versus 17% were somewhat to extremely dissatisfied, P < .0001), indicated more work-life conflicts, and reported they felt too tired or irritable after work to participate in home life. Residents exercised less frequently (41% of residents versus 54% of faculty exercised 3 to 5 times per week, P < .002); exercise and hobbies were correlated with lower psychological symptomatology. Interestingly, faculty reported higher levels of stress and more difficulty leaving personal concerns behind when at work.21 Generalizability of these studies is limited due to low response rates (17%–30%) to the cross-sectional surveys. Thus, these are useful pilot data and require replication with a greater response rate for conclusions to be drawn.
Factors Correlated With Resident Well-Being
Several studies examined factors that correlate with well-being measures (figure 2, group B). Overall, autonomy, competence, and social relatedness were the areas found to be widely associated with greater resident well-being. Specifically, a sense of control and autonomy, pursuit and achievement of goals, opportunities for learning, increased confidence and sense of increasing mastery, positive feedback, and positive colleague relationships were all associated with greater well-being across 4 studies.21–24
A few additional factors were associated with well-being. Sleep was found to be important in several studies. A greater amount of sleep, physical activity, and time in nature were associated with measures of greater well-being or less burnout.17 Sleep deprivation was associated with increases in all measures of distress in a survey of orthopedic residents in 2009.21 In interviews conducted in 2005, residents described sleep deprivation as an important stressor that led to poorer well-being.25 Papp et al26 studied residents across 6 different specialties in 5 institutions in 2001–2002, and residents noted that sleep loss affected their personal well-being, ability to learn, professionalism, task performance, and personal relationships. In the same study, 84% of residents fell in range of the Epworth Sleepiness Scale where “clinical intervention is recommended,” and mean scores fell between the average score for patients with obstructive sleep apnea and narcolepsy.26
Time away from work was another important associated factor. In a cross-sectional survey, a score for personal time availability (PTA) was computed by averaging residents' reported ability to find time to exercise, socialize, and tend to errands. Residents scoring above the median PTA reported more positive experiences and emotions, fewer negative experiences and emotions, higher career choice satisfaction, and less perceived stress. Scoring above median PTA was also associated with working fewer hours (P < .001) and more sleep hours (P = .006), after adjustment for age, gender, and years in training.27 Due to the study design, it cannot be determined whether PTA is the factor most associated with greater well-being, or if it is a proxy measure of fewer hours of work. Interns identified that lighter rotations and vacations were associated with upswings in their well-being, and long work hours and on call were associated with downswings.24 Obstetrics-gynecology residents in 1 program rated their lifestyle low, which correlated with lower residency satisfaction.22
Being in a relationship was studied and found associated with greater well-being.16,17 In a survey of residents across 11 specialties, sexual functioning was associated with overall quality of life, and sexual dysfunction (a score less than 23 on the male and female sexual function inventories) was found to affect 49% of women and 11% of men. High stress was associated with sexual dissatisfaction (a subset measure on the male and female sexual function inventories), and male residents working over 70 hours per week were 4 times as likely to have sexual dissatisfaction (P < .001; adjusted OR = 4.35; 95% CI 1.83–11.6). Residents reported that their sexual activity frequency and partner relationship quality had decreased during residency, with also a decrease in sexual encounters per month from a mean of 10.5 prior to residency for women down to 4.4 per month during residency, and from 8.3 down to 4.2 for men (P < .001).28
Religion and spirituality were examined in 2 studies. Higher mental well-being was associated with “incorporating a life philosophy stressing balance in personal and professional life” and “nurturing religious/spiritual aspects of [oneself].”18 In a multivariate analysis, a lower health rating on a self-rated health scale was associated with poor spiritual well-being.30
One study chose to measure well-being as the opposite of burnout. They used the inverse of the submeasures of the well-validated Maslach Burnout Inventory, thus defining well-being as lower emotional exhaustion, lower depersonalization (feeling detached or cynical about patients), and higher personal accomplishment. An increase in perceived social support via family, friends, or support groups for physicians was associated with decreased emotional exhaustion and depersonalization and increased personal accomplishment. Adjustment for multiple comparisons and raw or mean scores were not reported.29 The questionnaire design asked residents to self-identify which factors protect them from burnout; this carries the implicit assumption that protection from burnout is well-being, and that residents know what protects them from burnout. Alcohol use was negatively associated with well-being in 2 other studies, and prescription drug use associated with higher depersonalization scores.16,17,21
Predictors of Resident Well-Being
Two studies, which were stronger in having a longitudinal design (figure 2, group C), examined potential predictors of well-being. In a prospective longitudinal study of surgical residents at 1 institution, “grit,” or perseverance, was found predictive of higher psychological well-being 6 months later, controlling for gender and baseline well-being (B = 0.27, P < .01).31 In a longitudinal study of orthopedic surgery residents on a trauma rotation, general health scores decreased 2 months into the rotation (mean SF-36 subscale scores 58.13–53.68, P = .015). Residents became less concerned about not having enough time to spend with friends and family, and more social time became time spent exclusively with medical colleagues.32
Potential Effects of Resident Well-Being
The next set of studies examined the correlation of well-being to hypothesized downstream effects of well-being (figure 2, group D). Shanafelt et al18 found greater mental well-being to be associated with greater empathy in internal medicine residents. Four studies examined well-being and the potential association with academic performance. When adjusted for year of training, internal medicine in-training examination scores were not correlated with well-being.33,34 Similarly, well-being and academic success were not correlated in 2 additional studies.19,35
Via semistructured interviews of residents in 2 programs, residents identified their well-being as affecting relatedness (specifically, the quality of discussions with patients and interactions with colleagues), competence (performance and decision making), and autonomy (motivation with both daily work and career).25 Directionality of effects of well-being cannot be drawn here, as the identified effects may instead be generating well-being.
Barriers to Interventions to Improve Resident Well-Being
Demographics of being a woman, under age 32, and Caucasian were each associated with not using a resident mental well-being program because of feeling unable to take time for an appointment (figure 2, group E). Men were more concerned about the potential utility of this well-being program (OR = 0.55, 95% CI 0.36–0.85), and minorities were significantly more concerned about confidentiality (OR = 0.56, 95% CI 0.28–0.92). Unwillingness to use the program was associated with concerns about helpfulness and stigma.36
Interventions to Improve Resident Well-Being
Three studies tested and evaluated interventions aimed to improve resident well-being (figure 2, group F). An intervention of providing faculty group consultation to family medicine residents on progress, goals, and well-being 2 to 3 times per year showed no difference to the prior-to-intervention group, although a true difference cannot be excluded due to the small sample size used in the study and lack of prior power calculation.38 An assumed effect of well-being—presenteeism, an ability to concentrate and maximally produce quality work while at a job—was studied before and after the well-being intervention of hospital gym access. Baseline presenteeism scores of these surgical residents were significantly below the population norm (mean Stanford Presenteeism Scale scores 17.3 versus 24, P < .0001), and senior residents demonstrated significant improvement in presenteeism with the intervention, compared to junior residents (mean 20.5 versus 16.6, P = .034).37 This study benefits from the interventional and longitudinal design but is limited by a small sample size. In a randomized controlled trial of anesthesia residents, an intervention developed around an evidence-based workplace program for strengthening coping mechanisms was delivered. One control group was given the equivalent amount of time to spend in a room together doing what they wished, and the other control group had duties as usual. There was a significant reduction in anxiety in the well-being group compared to the routine duties group (adjusted difference 7.6 on the State-Trait Anxiety Inventory [score range 20–80], P = .02).39 Limited by small numbers, these studies suggest hypotheses for future testing, but they do not provide evidence that a particular intervention should be adopted by a residency program or institution.
Discussion
The strength of the current literature is a demonstration of the factors that correlate with resident well-being. This body of literature has several methodological limitations. The vast majority of the studies are cross-sectional surveys, with associated problems of sampling, reporting, and recall bias. Only 3 studies reported the results of interventions to enhance well-being, all with small sample sizes. Due to the small sample sizes, it is difficult to determine whether failure to observe statistically significant outcomes was due to lack of intervention efficacy or lack of statistical power. The interventions studied surgical, anesthesia, and family medicine residents, limiting their generalizability to other specialties. No longitudinal studies have investigated how resident well-being evolves over the course of residency, nor have studies compared residents' current well-being to well-being preresidency or postresidency. Well-being across specialties cannot be assessed with the current data, and several specialties are not represented.
The well-being measures used were varied, with limited discussion as to why they were chosen. A consensus on appropriate well-being scales in the field would allow greater comparisons to be drawn across future studies. The Satisfaction with Life Scale8 could be considered in future studies. However, this scale may not fully capture well-being so much as happiness, and proposed additions to the scale include a subjective vitality scale, self-actualization scale, and mental health scales.40,41 The PHEEM10 is an important potential measure given the established importance of autonomy and social support in fostering well-being. Determination and validation of an appropriate well-being scale for this population is a key area for future work.
The 3 main factors associated with resident well-being in the current literature coincide with the psychological research on well-being. These factors are autonomy, competence building, and strong social connection. In the field of well-being research, Ryan and Deci40 define well-being as a sense of life satisfaction, feeling one is living in accordance with deeply held values, and feeling fully engaged with life. Ryan and Deci42 posit 3 psychological needs that lead to well-being when fulfilled: (1) autonomy, (2) competence, and (3) relatedness. This has been substantiated across observational and experimental studies; autonomy, competence, and relatedness within person are each found to be associated with well-being.43 Succeeding in an activity (high competence) while feeling pressured to do so (low autonomy) leads to happiness but not well-being, but when succeeding (high competence) at a task controlled by one's own motivation (high autonomy), greater well-being results.44 Autonomy and competence are found predictive of well-being, both between-persons and within person.45 Relatedness satisfaction is achieved by meaningful conversation and feeling understood and appreciated.43
This definition of well-being has established correlations in research on residents. Autonomy and burnout were significantly inversely correlated in a study of residents in Argentina.46 Yet, as the measure used in this study highlights, the predominant focus of research on resident functioning has been stress and burnout. Evidence supports that positive mental states are more than the absence of symptoms.47 Cowen48 notes well-being anchors one end of a continuum, while the opposing end is anchored by pathology or sickness. This continuum is highlighted to describe well-being as more than the absence of illness, and thus disease or burnout prevention is a different strategy than well-being promotion. A shift in clinical medicine from management of pathogenesis to salutogenesis, well-being promotion, has been occurring over the past few decades.49
In addition, sleep and time away from work can augment well-being. Maslow's Hierarchy of Needs places sleep at the most basic level; residents sacrifice these needs during 30-hour calls and 80-hour weeks. Adequate sleep can thus be understood as a basic prerequisite for well-being; this theory could be examined in future work by comparing the well-being of residents who have variable ratings of sleep adequacy. The second additional factor, time away from work, may allow for the building of individual coping mechanisms. Cowen48 added acquisition of effective stress coping skills as necessary on the pathway to well-being. Coping skills development for each resident may involve time to bolster physical, social, cognitive, or spiritual health, varying depending on the valence individuals place on each area.
Limitations of this review include that key articles may be missing; a single author reviewed the articles for inclusion/exclusion; bibliographies of key articles were not hand-searched; and searches using the names of authors of key articles were not done. Also, the selection of search terms may have been too restrictive to identify some important articles. The choice to omit articles focusing on duty hours may have missed some risk factors or interventions associated with well-being. The analysis did not consider different time periods, thus cohort effects across generations or potential variations pre- and post- duty hour implementation in 2003 were not evaluated.
The current literature highlights the need for more rigorous research on medical education well-being. Next steps include finding or developing a well-being scale with validity evidence for research in this population, and longitudinal examination of well-being across multiple specialties. Literature summarized in this review directs future research toward evaluating interventions focused on factors associated with resident well-being in cross-sectional studies, including autonomy, building competence, enhanced social relatedness, sleep, and coping mechanisms. Adequate statistical power and generalizability will require large intervention trials involving residents from a broad range of training specialties.
Conclusion
The major factors associated with resident well-being are autonomy, building of competence, strong social relatedness, sleep, and time away from work. Perseverance is predictive of well-being, and greater well-being is associated with increased resident empathy. Research evaluating efficacy of existing interventions is limited by small samples sizes and data from a single site or specialty. Due to these limitations, the current literature does not offer evidence for a specific intervention for programs to implement in order to enhance their residents' well-being.
References
- 1. Levinson DJ. A conception of adult development. Am Psychol. 1986; 41 1: 3– 13. [Google Scholar]
- 2. Perry MY, Osborne WE. Health and wellness in residents who matriculate into physicians training programs. Am J Obstet Gynecol. 2003; 189 3: 679– 683. [DOI] [PubMed] [Google Scholar]
- 3. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015; 90 12: 1600– 1613. [DOI] [PubMed] [Google Scholar]
- 4. Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012; 172 18: 1377– 1385. [DOI] [PubMed] [Google Scholar]
- 5. Asch DA, Parker RM. The Libby Zion case: one step forward or two steps backward? N Engl J Med. 1988; 318 12: 771– 775. [DOI] [PubMed] [Google Scholar]
- 6. Reed D, Cook D, Beckman T, et al. Association between funding and quality of published medical education research. JAMA. 2007; 298 9: 1002– 1009. [DOI] [PubMed] [Google Scholar]
- 7. Diener E. Subjective well-being: the science of happiness and a proposal for a national index. Am Psychol. 2000; 55 1: 34– 43. [PubMed] [Google Scholar]
- 8. Diener E. Understanding scores on the satisfaction with life scale. 2006. http://internal.psychology.illinois.edu/∼ediener/Documents/Understanding%20SWLS%20 Scores.pdf. Accessed August 22, 2016. [Google Scholar]
- 9. Bech P, Olsen LR, Kjoller M, et al. Measuring well-being rather than the absence of distress symptoms: a comparison of the SF-36 Mental Health subscale and the WHO-Five Well-Being Scale. Int J Methods Psychiatr Res. 2003; 12 2: 85– 91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Riquelme A, Herrera C, Aranis C, et al. Psychometric analyses and internal consistency of the PHEEM questionnaire to measure the clinical learning environment in the clerkship of a medical school in Chile. Med Teach. 2009; 31 6: e221– e225. [DOI] [PubMed] [Google Scholar]
- 11. Roff S, McAleer S, Skinner A. Development and validation of an instrument to measure the postgraduate clinical learning and teaching educational environment for hospital-based junior doctors in the UK. Med Teach. 2005; 27 4: 326– 331. [DOI] [PubMed] [Google Scholar]
- 12. Hoonpongsimanont W, Murphy M, Kim CH, et al. Emergency medicine resident well-being: stress and satisfaction. Occup Med (Lond). 2013; 64 1: 45– 48. [DOI] [PubMed] [Google Scholar]
- 13. Hull SK, DiLalla LF, Dorsey JK. Prevalence of health-related behaviors among physicians and medical trainees. Acad Psychiatry. 2008; 32 1: 31– 38. [DOI] [PubMed] [Google Scholar]
- 14. Powers AS, Myers JE, Tingle LR, et al. Wellness, perceived stress, mattering, and marital satisfaction among medical residents and their spouses: implications for education and counseling. Fam J Couns Ther Couples Fam. 2004; 12 1: 26– 36. https://libres.uncg.edu/ir/uncg/f/J_Myers_Medical%20Residents_2004.pdf. Accessed August 22, 2016. [Google Scholar]
- 15. Sargent MC, Sotile W, Sotile MO, et al. Stress and coping among orthopaedic surgery residents and faculty. J Bone Joint Surg Am. 2004; 86-A 7: 1579– 1586. [DOI] [PubMed] [Google Scholar]
- 16. Cohen JS, Leung Y, Fahey M, et al. The happy docs study: a Canadian Association of Internes and Residents well-being survey examining resident physician health and satisfaction within and outside of residency training in Canada. BMC Res Notes. 2008; 1: 105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lebensohn P, Dodds S, Benn R, et al. Resident wellness behaviors: relationship to stress, depression, and burnout. Fam Med. 2013; 45 8: 541– 549. [PubMed] [Google Scholar]
- 18. Shanafelt TD, West C, Zhao X, et al. Relationship between increased personal well-being and enhanced empathy among internal medicine residents. J Gen Intern Med. 2005; 20 7: 559– 564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Beckman TJ, Reed DA, Shanafelt TD, et al. Resident physician well-being and assessments of their knowledge and clinical performance. J Gen Intern Med. 2012; 27 3: 325– 330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Crouchley K. SF-8 Norms Health and Wellbeing Surveillance System. January 2006–July 2007. http://ww2.health.wa.gov.au/∼/media/Files/Corporate/Reports%20and%20publications/Population%20 surveys/2007-SF-8_Norms_Report.ashx. Accessed August 22, 2016. [Google Scholar]
- 21. Sargent MC, Sotile W, Sotile MO, et al. Quality of life during orthopaedic training and academic practice. Part 1: orthopaedic surgery residents and faculty. J Bone Joint Surg Am. 2009; 91 10: 2395– 2405. [DOI] [PubMed] [Google Scholar]
- 22. Lund KJ, Alvero R, Teal SB. Resident job satisfaction: will 80 hours make a difference? Am J Obstet Gynecol. 2004; 191 5: 1805– 1810. [DOI] [PubMed] [Google Scholar]
- 23. Manusov EG, Carr RJ, Rowane M, et al. Dimensions of happiness: a qualitative study of family practice residents. J Am Board Fam Pract. 1995; 8 5: 367– 375. [PubMed] [Google Scholar]
- 24. Hurst C, Kahan D, Ruetalo M, et al. A year in transition: a qualitative study examining the trajectory of first year residents' well-being. BMC Med Educ. 2013; 13: 96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ratanawongsa N, Wright SM, Carrese JA. Well-being in residency: effects on relationships with patients, interactions with colleagues, performance, and motivation. Patient Educ Couns. 2008; 72 2: 194– 200. [DOI] [PubMed] [Google Scholar]
- 26. Papp KK, Stoller EP, Sage P, et al. The effects of sleep loss and fatigue on resident–physicians: a multi-institutional, mixed-method study. Acad Med. 2004; 79 5: 394– 406. [DOI] [PubMed] [Google Scholar]
- 27. Cedfeldt AS, Bower EA, English C, et al. Personal time off and residents' career satisfaction, attitudes and emotions. Med Educ. 2010; 44 10: 977– 984. [DOI] [PubMed] [Google Scholar]
- 28. Sangi-Haghpeykar H, Ambani DS, Carson SA. Stress, workload, sexual well-being and quality of life among physician residents in training. Int J Clin Pract. 2009; 63 3: 462– 467. [DOI] [PubMed] [Google Scholar]
- 29. Eckleberry-Hunt J, Lick D, Boura J, et al. An exploratory study of resident burnout and wellness. Acad Med. 2009; 84 2: 269– 277. [DOI] [PubMed] [Google Scholar]
- 30. Yi MS, Mrus JM, Mueller CV, et al. Self-rated health of primary care house officers and its relationship to psychological and spiritual well-being. BMC Med Educ. 2007; 7: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Salles A, Cohen GL, Mueller CM. The relationship between grit and resident well-being. Am J Surg. 2013; 207 2: 251– 254. [DOI] [PubMed] [Google Scholar]
- 32. Zahrai A, Bhandari M, Varma A, et al. Residents' quality of life during an orthopedic trauma rotation: a multicentre prospective observational study. Can J Surg. 2008; 51 3: 190– 196. [PMC free article] [PubMed] [Google Scholar]
- 33. West CP, Shanafelt TD, Cook DA. Lack of association between resident doctors' well-being and medical knowledge. Med Educ. 2010; 44 12: 1224– 1231. [DOI] [PubMed] [Google Scholar]
- 34. West CP, Shanafelt TD, Kolars JC. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA. 2011; 306 9: 952– 960. [DOI] [PubMed] [Google Scholar]
- 35. de Oliveira Filho GR, Vieira JE. The relationship of learning environment, quality of life, and study strategies measures to anesthesiology resident academic performance. Anesth Analg. 2007; 104 6: 1467– 1472. [DOI] [PubMed] [Google Scholar]
- 36. Ey S, Moffit M, Kinzie JM, et al. “If you build it, they will come”: attitudes of medical residents and fellows about seeking services in a resident wellness program. J Grad Med Educ. 2013; 5 3: 486– 492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Watson DT, Long WJ, Yen D, et al. Health promotion program: a resident well-being study. Iowa Orthop J. 2009; 29: 83– 87. [PMC free article] [PubMed] [Google Scholar]
- 38. Foster E, Biery N, Dostal J, et al. Supporting resident well-being through an integrated advising and assessment process. Fam Med. 2012; 44 10: 731– 734. [PubMed] [Google Scholar]
- 39. Saadat H, Snow DL, Ottenheimer S, et al. Wellness program for anesthesiology residents: a randomized, controlled trial. Acta Anaesthesiol Scand. 2012; 56 9: 1130– 1138. [DOI] [PubMed] [Google Scholar]
- 40. Ryan RM, Deci EL. On happiness and human potentials: a review of research on hedonic and eudaimonic well-being. Annu Rev Psychol. 2001; 52: 141– 166. [DOI] [PubMed] [Google Scholar]
- 41. Ryan RM, Frederick C. On energy, personality and health: subjective vitality as a dynamic reflection of well-being. J Pers. 1997; 65 3: 529– 565. [DOI] [PubMed] [Google Scholar]
- 42. Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000; 55 1: 68– 78. [DOI] [PubMed] [Google Scholar]
- 43. Reis HT, Sheldon KM, Gable SL, et al. Daily well-being: the role of autonomy, competence, and relatedness. Pers Soc Psychol Bull. 2000; 26 4: 419– 435. [Google Scholar]
- 44. Nix GA, Ryan RM, Manly JB, et al. Revitalization through self-regulation: the effects of autonomous and controlled motivation on happiness and vitality. J Exp Soc Psychol. 1999; 35 3: 266– 284. [Google Scholar]
- 45. Sheldon KM, Ryan R, Reis HT. What makes for a good day: competence and autonomy in the day and in the person. Personal Soc Psychol Bull. 1996; 22 12: 1270– 1279. https://selfdeterminationtheory.org/SDT/documents/1996_SheldonRyanReis.pdf. Accessed August 22, 2016. [Google Scholar]
- 46. Llera J, Durante E. Correlation between the educational environment and burn-out syndrome in residency programs at a university hospital. Arch Argent Pediatr. 2014; 112 1: 6– 11. [DOI] [PubMed] [Google Scholar]
- 47. Huppert FA, Whittington JE. Evidence for the independence of positive and negative well-being: implications for quality of life assessment. Br J Health Psychol. 2003; 8 pt 1: 107– 122. [DOI] [PubMed] [Google Scholar]
- 48. Cowen EL. The enhancement of psychological wellness: challenges and opportunities. Am J Community Psychol. 1994; 22 2: 149– 179. [DOI] [PubMed] [Google Scholar]
- 49. Becker CM, Glascoff MA, Felts WM. Salutogenesis 30 years later: where do we go from here? Int Electron J Health Educ. 2010; 13: 25– 32. http://files.eric.ed.gov/fulltext/EJ895721.pdf. Accessed August 22, 2016. [Google Scholar]