Abstract
Background
Comprehensive treatment models reduce distress and suicide risk in military, university, and community populations, but are not well studied with in medical trainees and physicians in practice. Physicians face unique internal and external barriers that limit access to psychological or psychiatric treatment, which may contribute to higher rates of burnout, depression, and suicide.
Objective
Our goal is to report on the feasibility and utilization of a wellness and suicide prevention program for residents, fellows, and faculty in an academic health center.
Methods
The program provides individual counseling, psychiatric evaluation, and wellness workshops for residents/fellows (N = 906) and faculty (N = 1400). Demand for services is demonstrated by the participation rate of eligible trainees. Acceptability within the target population is examined in a 2011 survey in which trainees (N = 116, 97% participation) and program directors (N = 23, 88% participation) rated their satisfaction. Start-up costs and funding sources to sustain a wellness program are outlined.
Results
Over 10 years, utilization of services grew from 5% in the program's first year (2004–2005) to a high of 25% of eligible trainees for 2013–2014, and faculty utilization grew to 6% to 8% for 2014–2015. Trainees and program directors reported a high level of satisfaction with this wellness program. Funding for clinic space and clinical staff is provided by the hospital via the graduate medical education budget.
Conclusions
Increased utilization over 10 years, high satisfaction, and consistent institutional support suggest that this comprehensive model of care is feasible and valued.
What was known and gap
Approaches to increase well-being and reduce suicide risk in medical trainees and physicians are needed, but their efficacy has not been thoroughly assessed.
What is new
A wellness program saw an increase in trainees' use of services from 5% to 25% of all trainees seen per year over 10 years, and faculty utilization of services grew to 6% to 8% annually.
Limitations
Single institution study limits generalizability; sample size precludes the ability to detect a reduction in suicides.
Bottom line
Increased use and user satisfaction suggest the model is feasible and can overcome traditional access barriers for wellness services.
“I thought being suicidal during residency was normal . . . but then counseling helped me realize how important I am to my family and how to make changes to protect my health.”
—Second-year resident
Introduction
Medical students begin their education more psychologically healthy than their college graduate counterparts.1 However, by the third year of medical school and into residency, up to one-third of trainees may be clinically depressed,2 50% to 70% describe burnout symptoms,3 and 6% to 12% of trainees report suicidal ideation.4 Of greatest concern, suicide rates for physicians are 2 times higher than those for the general population,5 and rates appear unchanged since 2002, when an American Medical Association task force called for more preventive and interventional efforts to assist distressed physicians.6
Comprehensive mental health promotion and intervention models that reduce distress and suicide risk in military,7 university,8 and community settings9 are less available to medical trainees and faculty physicians. Most intervention studies involving physicians10 describe educational interventions that focus on reducing stress and burnout symptoms11 rather than treating depression or suicidal ideation.12 There is evidence, however, that physicians respond to professional treatment, as demonstrated in the number of physicians successfully treated within drug and alcohol diversion programs.13 Treatment response by depressed and/or suicidal physicians is less evident since many physicians do not disclose treatment, or admit on anonymous surveys that they avoid treatment.14,15
Internal and external barriers that limit access to treatment may contribute to ongoing high rates of distress in this at-risk population.4,6 These barriers include concerns about confidentiality; treatment costs; limited flexible time; uncertainty about efficacy; stigma; and questions about reporting treatment on credentialing, medical licensing, and life and disability insurance applications.16–18 As an alternative to professional treatment, highly distressed physicians may self-prescribe, turn to family for solace, or “struggle in silence.”19,20
In this article we describe components of a wellness and suicide prevention program designed to reach out to medical trainees and faculty, and to encourage them to prioritize self-care and seek professional treatment if needed. The feasibility of this Resident and Faculty Wellness Program (RFWP) is examined through (1) demand for services; (2) acceptability to the target population as seen in ratings of satisfaction; and (3) resources needed to develop and sustain a wellness program in an academic health center (AHC) setting.
Methods
Setting and Participants
The RFWP was launched in 2004–2005 to assist medical residents and fellows, was expanded in 2008 to include all full-time faculty, and in 2014 started incorporating residents from an affiliate community hospital. Currently, 906 residents and fellows and 1400 faculty are eligible for services. Program directors (N = 23, 88% participation) and trainees who accessed the RFWP (N = 116, 97% participation) completed a satisfaction survey in 2011.
Intervention
Designing and growing this program required a dedicated team of professionals experienced in treating physicians and not directly involved in assessing performance of residents or faculty. Program staffing began with 2 psychologists and 1 psychiatrist (1.0 full-time equivalent [FTE] in total) for the first few years, and gradually increased each year as utilization increased. Currently, the team includes 2 psychologists and 2 psychiatrists (2.4 FTEs in total), providing services for more than 2300 eligible trainees and faculty.
Given the demands of medical training, longer-term insight-oriented therapies are not typically offered. Instead our clinicians focus on mobilizing RFWP participants' existing strengths to address current stressors as well as helping them develop additional resilience-building strategies. Brief, evidence-based counseling approaches are emphasized (box). Unlike most employee assistance programs offering a few free sessions and then referrals to community providers, an “adequate dose” of treatment and subsequent “booster” sessions are available throughout training or employment as faculty—a model associated with greater treatment response and reduced relapse.21
box Our Model.
Educational Outreach
Wellness promotion workshops to residency/fellowship programs and faculty groups
Orientation presentations about our program and referral process for incoming trainees, chief residents, and program directors
Suicide prevention screening offered to trainees and faculty—RFWP clinicians respond online to completed surveys by providing participants with individualized feedback, resources, and in-person appointments (if needed)
Resident support groups/luncheons monthly in pediatric, neonatal, and medical ICUs and psychiatry—initially, RFWP clinicians colead with chief residents, now chiefs run with training/consultation with RFWP clinicians
Direct Care and Consultation
Individual coaching and psychological counseling approaches, such as cognitive behavioral therapies, mindfulness meditation, and brief insight-oriented treatments
Psychiatric evaluation/medication management
Consultation with GME, program leaders, and chief residents about distressed trainees/faculty
Referrals to/case coordination with community providers of specialized services (fitness for duty evaluations, neuropsychological testing, outpatient and inpatient hospitalization)
Abbreviations: RFWP, Resident and Faculty Wellness Program; ICUs, intensive care units; GME, graduate medical education.
Privacy and confidentiality concerns are addressed in campus-wide outreach communications, on our website, and in the initial treatment consent process when we explain that no information is disclosed to others unless there is imminent risk of harm to self or others or concern about impairment or patient safety. Clinical records, stored in an encrypted database and a secure location accessible only to RFWP clinicians, are not documented in the health system's electronic health record (EHR), and prescriptions can be provided, when needed, outside the EHR. Questions about reporting treatment on licensure, credentialing, or life/disability insurance applications are addressed in our outreach and individual sessions. Of note, the Oregon Medical Board and many other state boards22 no longer ask about mental health treatment and instead screen for impairment (the inability to practice medicine safely and competently due to a physical, mental, or emotional condition).
Early on, we made a decision to refer our physicians to community providers for any mandated treatment or formal fitness-for-duty evaluations. If a physician participating in the RFWP is at risk of impairment, we often recommend a medical leave of absence and refer to a community psychiatrist for a fitness-for-duty evaluation, or if indicated, to our state's health professionals' monitoring program, or to the Oregon Medical Board. Even when we refer out to other providers or programs, the RFWP clinician remains involved to advocate for the physician, coordinate care, and consult with program leadership about a return to work plan.
Incoming chief residents, program directors, and faculty leaders receive training from RFWP staff focused on recognizing signs of distress in trainees or colleagues, and intervening upstream by facilitating referrals for professional evaluation and support (box). In 2013–2014, we increased suicide prevention efforts by conducting workshops on this topic and invited trainees and faculty to complete an anonymous brief screen of stress, depression, and suicide risk, the American Foundation for Suicide Prevention's Interactive Screening Program.23
Commitment of resources by academic and hospital leadership was essential to the early development and credibility of the RFWP. Demonstrating the value and mission alignment of this new program was accomplished through strong advocacy by the program's director (M.M.) and by the associate dean of graduate medical education (GME), who successfully lobbied for funding and clinical space in a private location on-site. Institutional leaders acknowledged that a physician workforce with enhanced resilience, coping skills, and overall wellness would provide safer and higher-quality care, be more compassionate toward patients and families, and be less susceptible to burnout and attrition. This funding model also allowed for treatment to be free of charge, eliminating 2 important barriers to care: out-of-pocket costs and privacy concerns if insurance were to be billed.
Outcomes
Demand for services is reported in annual utilization rates. A psychometrically valid measure of satisfaction with psychological services, the Client Satisfaction Questionnaire (CSQ),24 was included in a 2011 anonymous survey e-mailed to all residents and fellows and completed by trainees who received RFWP services. A slightly modified residency program director version of the CSQ (to reflect consultation with and referral of trainees) was completed in 2011. Start-up costs and funding sources to develop this program are described.
This project was approved by our Institutional Review Board.
Analysis
Frequencies of visits, number of cases, and percentage of eligible trainees participating in the RFWP each year are reported. Average visits per trainee are included each year. Faculty utilization is available only for 2014–2015 due to difficulties accessing AHC archival data. Frequencies are described for program director and trainee CSQ responses.
Results
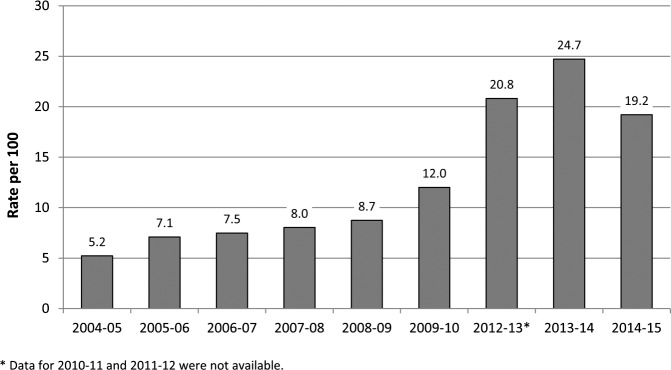
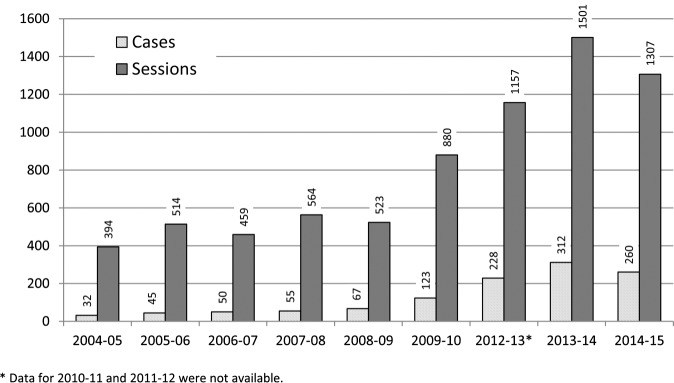
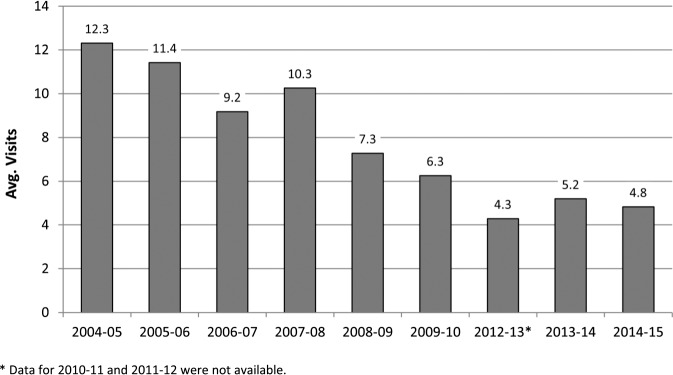
Utilization of the RFWP (figures 1 through 3) increased from 5.2% of all residents and fellows in this AHC in the first year (2004–2005) to a high of 24.7% in 2013–2014 during a new suicide prevention initiative. Currently, trainees represent approximately two-thirds of the RFWP caseload (figure 3). Even though there were no programmatic limits on the number of visits offered, in the past 3 years trainees' duration of treatment became briefer (figure 2).
figure 1.
Resident and Fellow Utilization Rate
figure 3.
Total Cases and Sessions
figure 2.
Average Visits Per Resident/Fellow
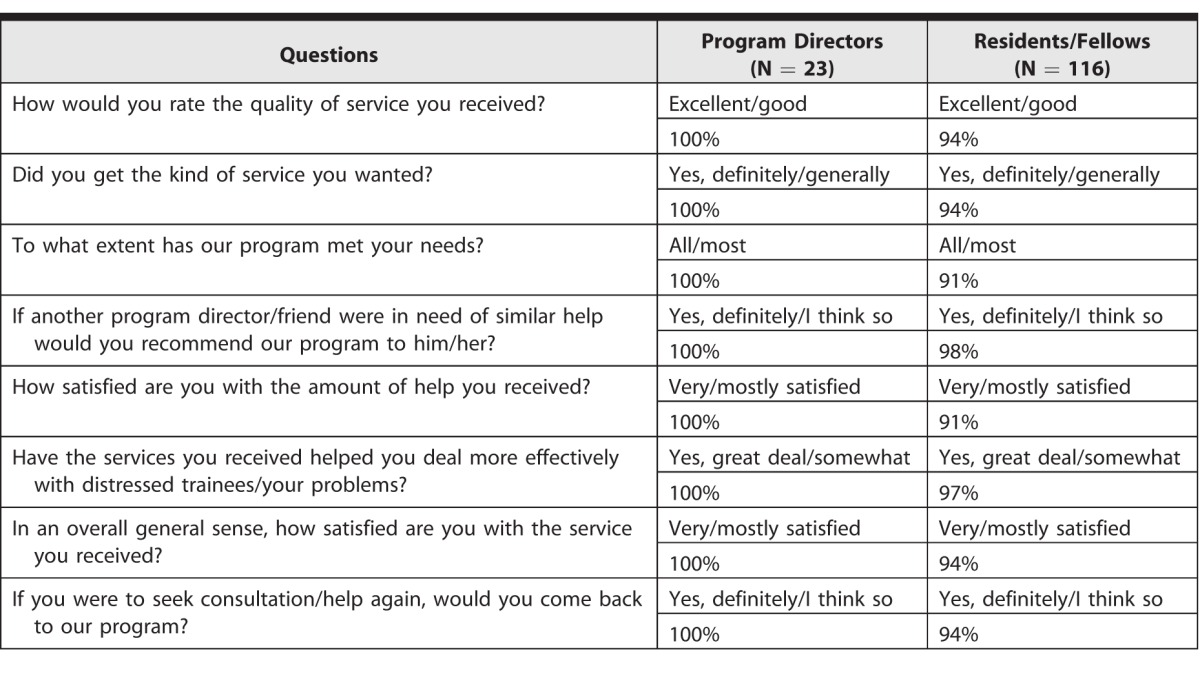
Faculty numbers (figure 3) increased steadily from 6 cases in the first year (2008–2009) to 86 cases in 2014–2015 (approximately 6% to 8% of eligible faculty in this AHC). Following a relocation of the program in January 2014, faculty visits increased by 30%, while trainee visits decreased by 26.5% from the prior year. Some trainees anecdotally reported to RFWP staff that they had more difficulty attending RFWP sessions when our clinic moved from a central location (closer to the hospital) to a more distant location on campus. On the CSQ,24 trainees who received treatment through the RFWP and program directors who consulted with and referred trainees to RFWP clinicians reported a high level of satisfaction (table).
table.
Trainee and Program Director High Level of Satisfaction
Health system funding via the GME budget is the primary source of support for the RFWP and has increased incrementally each year to now provide coverage to 2306 medical residents, fellows, and faculty. Of the current budget, 85% of the program's expenditures are for clinician FTEs, 5% for on-site clinic space, and 10% for administrative expenses. Start-up costs for a comprehensive program modeled on the RFWP would vary by geographic region and number of trainees and faculty covered but would likely require up to 1.0 clinician FTE, nearby clinic space, and administrative support. In a midsize AHC, funding a wellness program might start at $200,000 per year, and would likely increase in response to program growth.
Discussion
Contrary to prior research on residents' accessing counseling on-site,25 the majority of this AHC's trainees indicated a willingness to access our program on-site, reported fewer barriers,16 and when they did seek treatment reported a high level of satisfaction. Training program leaders, key promoters of our services, also expressed satisfaction with the RFWP. The demand for services increased each year. In the most recent year, almost 20% of trainees participated in our program—a rate higher than national rates of utilization of 10.4% for university counseling centers26 and 13.4% for US adults.27 Of note, 6.5% of employees in our AHC accessed the Employee Assistance Plan in 2015.28 Similar to another AHC's successful outreach effort,29 the highest rates of RFWP utilization occurred during the launch of our suicide prevention initiative.
Barriers to treatment still exist. Specifically, demanding clinical schedules continue to be the most frequently mentioned barrier to accessing treatment by trainees,16 even after our GME office mandated that programs allow trainees to attend personal or family health care appointments on a quarterly basis.30 Trainees typically schedule RFWP meetings outside of these protected blocks of time due to the urgency of their need. After the RFWP relocation to a more remote site in January 2014, trainee visits declined 26.5% while faculty visits increased 30%—suggesting that time away from clinical duties may be more of a barrier for trainees. Alternatively, the decline in trainee utilization rate in 2014–2015 may be a return to baseline after the suicide prevention initiative and screening launched in 2013–2014.
Trainees' average number of visits per year steadily decreased from the first 4 years of our program, although no limits were placed on treatment duration. One possible explanation may be that a broader range of trainees with different levels of need are now accessing our program, and some may require a briefer duration of treatment than earlier participants in the RFWP. During orientation, trainees are encouraged by RFWP staff and program leadership to not wait for a crisis to access counseling. In addition, as utilization increased, scheduling follow-up appointments with RFWP clinicians might have become more difficult. In 2015, our program increased clinician FTEs to offer more scheduling options.
In the past decade, we have seen encouraging signs of a paradigm shift in our AHC. Certainly the ongoing funding of this program and visible promotion of this resource by GME and health system leadership has sent an important message to trainees and faculty. Faculty leaders make strong supportive statements at grand rounds, voicing the importance of physician well-being, and disclosing that they have benefited from the RFWP. Greater connectedness and support from peers may help distressed physicians be more willing to seek professional help and also reduce the risk of suicide.31
Limitations of the study are that the results are from 1 institution and may not generalize to other AHCs. Satisfaction ratings may not include a representative group of RFWP participants over the 10 years of our program. Actual outcomes such as reductions in suicide risk require a larger sample in order to detect changes due to the low base rate of suicide.7 Engagement in treatment, however, is an important proxy variable for reducing suicide risk.9 Future research is needed to identify which physicians in training and practice engage in a wellness program and as a result demonstrate enhanced personal and professional efficacy.
Conclusion
Specifically designed to support our physician colleagues—at all stages of their careers—this on-site comprehensive wellness program was accessed by a significant number of physicians, was highly rated, and was invested in by this AHC for more than 10 years. This model of care may be adopted or adapted by other teaching institutions.
References
- 1. Brazeau CM, Shanafelt T, Durning SJ, et al. Distress among matriculating medical students relative to the general population. Acad Med. 2014; 89 11: 1520– 1525. [DOI] [PubMed] [Google Scholar]
- 2. Mata DA, Ramos MA, Bansal N, et al. Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA. 2015; 314 22: 2373– 2383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Prins JT, Gazendam-Donofrio SM, Tubben BJ, et al. Burnout in medical residents: a review. Med Educ. 2007; 41 8: 788– 800. [DOI] [PubMed] [Google Scholar]
- 4. Schwenk TL, Davis L, Wimsatt LA. Depression, stigma, and suicidal ideation in medical students. JAMA. 2010; 304 11: 1181– 1190. [DOI] [PubMed] [Google Scholar]
- 5. Schernhammer E. Taking their own lives—the high rate of physician suicide. N Engl J Med. 2005; 352 24: 2473– 2476. [DOI] [PubMed] [Google Scholar]
- 6. Center C, Davis M, Detre T, et al. Confronting depression and suicide in physicians: a consensus statement. JAMA. 2003; 289 23: 3161– 3166. [DOI] [PubMed] [Google Scholar]
- 7. Knox KL, Pflanz S, Talcott GW, et al. The US Air Force suicide prevention program: implications for public health policy. Am J Public Health. 2010; 100 12: 2457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Drum DJ, Brownson C. BurtonDenmark A, et al. New data on the nature of suicidal crises in college students: shifting the paradigm. Prof Psychol Res Pr. 2009; 40 3: 213. [Google Scholar]
- 9. Rodgers PL, Sudak HS, Silverman MM, et al. Evidence-based practices project for suicide prevention. Suicide Life Threat Behav. 2007; 37 2: 154– 164. [DOI] [PubMed] [Google Scholar]
- 10. Regehr C, Glancy D, Pitts A, et al. Interventions to reduce the consequences of stress in physicians: a review and meta-analysis. J Nerv Ment Dis. 2014; 202 5: 353– 359. [DOI] [PubMed] [Google Scholar]
- 11. West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014; 174 4: 527– 533. [DOI] [PubMed] [Google Scholar]
- 12. Goldman ML, Shah RN, Bernstein CA. Depression and suicide among physician trainees: recommendations for a national response. JAMA Psychiatry. 2015; 72 5: 411– 412. [DOI] [PubMed] [Google Scholar]
- 13. McLellan AT, Skipper GS, Campbell M, et al. Five year outcomes in a cohort study of physicians treated for substance use disorders in the United States. BMJ. 2008; 337: a2038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fridner A, Belkić K, Marini M, et al. Why don't academic physicians seek needed professional help for psychological distress. Swiss Med Wkly. 2012; 142: w13626. [DOI] [PubMed] [Google Scholar]
- 15. Carroll AE. Silence is the enemy for doctors who have depression. New York Times. January 11, 2016. http://www.nytimes.com/2016/01/12/upshot/silence-is-the-enemy-for-doctors-who-have-depression.html?_r=0. Accessed September 7, 2016. [Google Scholar]
- 16. Ey S, Moffit M, Kinzie JM, et al. “If you build it, they will come”: attitudes of medical residents and fellows about seeking services in a resident wellness program. J Grad Med Educ. 2013; 5 3: 486– 492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Guille C, Speller H, Laff R, et al. Utilization and barriers to mental health services among depressed medical interns: a prospective multisite study. J Grad Med Educ. 2010; 2 2: 210– 214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Givens JL, Tjia J. Depressed medical students' use of mental health services and barriers to use. Acad Med. 2002; 77 9: 918– 921. [DOI] [PubMed] [Google Scholar]
- 19. Shanafelt TD, Balch CM, Dyrbye L, et al. Special report: suicidal ideation among American surgeons. Arch Surg. 2011; 146 1: 54– 62. [DOI] [PubMed] [Google Scholar]
- 20. American Foundation for Suicide Prevention. Physician and medical student depression and suicide prevention. https://afsp.org/our-work/education/physician-medical-student-depression-suicide-prevention/. Accessed September 7, 2016. [Google Scholar]
- 21. Hansen NB, Lambert MJ, Forman EM. The psychotherapy dose-response effect and its implications for treatment delivery services. Clin Psychol Sci Pract. 2002; 9 3: 329– 343. [Google Scholar]
- 22. Federation of State Medical Boards. Policy on Physician Impairment. Euless, TX: Federal of State Medical Boards of the United States; 2011. [Google Scholar]
- 23. Haas A, Koestner B, Rosenberg J, et al. An interactive web-based method of outreach to college students at risk for suicide. J Am Coll Health. 2008; 57 1: 15– 22. [DOI] [PubMed] [Google Scholar]
- 24. Attkisson CC, Zwick R. The Client Satisfaction Questionnaire: psychometric properties and correlations with service utilization and psychotherapy outcome. Eval Program Plann. 1982; 5 3: 233– 237. [DOI] [PubMed] [Google Scholar]
- 25. Dunn LB, Hammond KAG, Roberts LW. Delaying care, avoiding stigma: residents' attitudes toward obtaining personal health care. Acad Med. 2009; 84 2: 242– 250. [DOI] [PubMed] [Google Scholar]
- 26. Association for University and College Counseling Center Directors. Annual survey. http://files.cmcglobal.com/AUCCCD_Monograph_Public_2013.pdf. Accessed September 7, 2016. [Google Scholar]
- 27. National Institute of Mental Health. Mental health service use/treatment among US adults. http://www.nimh.nih.gov/health/statistics/prevalence/file_148235.pdf. Accessed September 7, 2016. [Google Scholar]
- 28. Cascade Centers I. 2015 EAP Summary Report for Oregon Health & Science University. Unpublished report 2015. [Google Scholar]
- 29. Moutier C, Norcross W, Jong P, et al. The suicide prevention and depression awareness program at the University of California, San Diego School of Medicine. Acad Med. 2012; 87 3: 320– 326. [DOI] [PubMed] [Google Scholar]
- 30. Cedfeldt AS, Bower E, Flores C, et al. Promoting resident wellness: evaluation of a time-off policy to increase residents' utilization of health care services. Acad Med. 2015; 90 5: 678– 683. [DOI] [PubMed] [Google Scholar]
- 31. Richardson JD, Darte K, Grenier S, et al. Operational stress injury social support: a Canadian innovation in professional peer support. 2008. http://www.journal.forces.gc.ca/vo9/no1/09-richardson-eng.asp. Accessed September 7, 2016. [Google Scholar]