Abstract
Objective:
To examine whether non-heat acclimatized (NHA) emergency responders endure greater physiological and perceptual strain than heat acclimatized (HA) counterparts in tropical field settings.
Methods:
Eight HA and eight NHA men urban search and rescue personnel had physiological and perceptual responses compared during the initial 4 hours shift of a simulated disaster in tropical conditions (ambient temperature 34.0 °C, 48% relative humidity, wet bulb globe temperature [WBGT] 31.4 °C).
Results:
From the 90th minute through to end of shift, HA (38.5 °C) sustained a significantly higher gastrointestinal temperature than NHA (38.1 °C) (mean difference 0.4 ± 0.2 °C, 95% confidence interval [CI] 0.2 to 0.7 °C, P = 0.005) despite comparable heart rate (P = 0.30), respiratory rate (P = 0.88), and axilla skin temperature (P = 0.47). Overall, perception of body temperature was similar between cohorts (P = 0.87).
Conclusions:
The apparent tolerance of greater physiological strain by HA responders occurred in the absence of perceptual differences.
Urban search and rescue (USAR) teams of at least 40 personnel are expected to respond within a matter of hours to a disaster affected site and extricate those entrapped within collapsed structures. Teams wear protective clothing and equipment while working long hours in confined space, inclusive of day and night shifts. Deployment to austere environments, particularly the extreme climate of tropical regions, poses significant challenges to the response teams. Heat, humidity, and torrential rainfall can impact rescue operations, equipment, habitat, and transportation. More importantly, heat related illness is acknowledged as a substantial risk for USAR responders.1 South East Asia is one of the most earthquake prone regions globally,2 placing a large population at risk of a sudden onset disaster precipitating USAR response to hot and humid climates. While strategies reducing the impact of heat on responders are warranted,3 there is limited scope for resource intensive methods during a response, as essential search and rescue equipment and associated resources are prioritized for deployment. Preparation for tropical deployments should, therefore, focus on maximizing the thermal tolerance of individual responders.
Utilized predominantly in athletic and military settings, heat acclimatization is conferred by regular bouts of physical training that induce sustained elevations of core temperature. Physiological adaptations include lower resting core temperature,4 lower core temperature and heart rate for a given exercise intensity,5 and an earlier onset of sweating.6 Collectively, such adaptations augment thermal tolerance of hot conditions to increase physical performance7,8 and reduce the incidence of heat related illness.9 Initial adaptations generally develop within a 4- to 14-day period, with aerobic fitness a key factor for determining heat acclimatization status.10,11 While initial adaptations are conferred rapidly, it is likely that further adaptations manifest from extended periods of physical activity in hot climates.12 Hence, responders residing in the tropics have regular opportunity to undertake physical work in the heat for development and maintenance of long-term heat acclimatization. In contrast, cool, temperate, and subtropical climates limit opportunity for body heat storage in the natural environment outside of the summer months. For USAR personnel residing in these regions, the sudden nature of earthquakes prevent sufficient notice to develop heat acclimatization immediately prior to deployment. Laboratory research outcomes suggest that for a given workload, deployed non-heat acclimatized (NHA) responders can expect to endure greater physiological and perceptual strain than their heat acclimatized (HA) counterparts, however, this premise is yet to be tested in disaster settings. Therefore, this investigation examined whether NHA emergency responders endure greater physiological and perceptual strain than their HA counterparts during the initial shift of a simulated deployment to tropical field conditions.
METHODS
Following approval by the Human Research Ethics Committee of the Northern Territory Department of Health and the Menzies School of Health Research, 16 men USAR personnel provided written informed consent prior to participating in a simulated 24 hour exercise at the Yarrawonga training facility on the outskirts of Darwin, Northern Territory (NT), Australia. Participants were recruited from NT Fire and Rescue (n = 5), and Queensland (QLD) Fire and Emergency Services (n = 11). The NT participants and three participants from Northern QLD were considered HA. The remaining eight QLD participants from temperate or subtropical regions were considered NHA responders. Table 1 represents the mean environmental conditions of the HA and NHA participants for the 90 days prior to the study. The QLD recruits traveled to Brisbane on the day prior to the exercise, where they were briefed by teleconference. The following morning, the QLD participants were transported to Darwin, with the 4 hours commercial flight simulating travel to deployment region. Immediately following collection of equipment and supplies, the participants traveled from Darwin Airport to the USAR training facility where they met with the NT participants for onsite briefings and establishment of research equipment. Participants wore briefs and t-shirt under personal protective clothing (PPC) that consisted of boots, dark blue cotton drill overalls, knee pads, gloves, and hard hat (Fig. 1). Additionally, participants used personal protective equipment consisting of glasses, ear muffs, and P2 respiratory protection where required.
TABLE 1.
Maximum and Minimum Temperatures for the 90 Days Preceding the Study. Data are Weighted Average and Presented as Mean (SD). Data Provided by Bureau of Meteorology
| Temperature | HA | NHA |
| Maximum (°C) | 32.2 (2.6) | 24.6 (2.2) |
| Minimum (°C) | 21.9 (3.0) | 13.5 (3.6) |
HA, heat acclimatized; NHA, non-heat acclimatized; SD, standard deviation.
FIGURE 1.

Study participants rescuing a moulaged victim.
The exercise was conducted during November, known for its harsh tropical environment with high ambient temperatures and elevated humidity, replicating conditions experienced within South East Asia. Two groups of eight USAR personnel with equal allocation of HA and NHA participants to each group, worked in unison for the initial 4 hours shift commencing at 1330, permitting comparison of physiological, perceptual, and fluid balance responses.
Disaster Simulation
A purpose built network of tunnels mimicking passages within a collapsed structure was utilized for the earthquake simulation. The disaster site was covered by rubble, car wrecks, and debris with the top of the “pile” fully exposed to sunlight. The USAR teams were briefed on their mission prior to commencement of exercise, with their primary objective to rescue the entrapped moulaged and weighted manikin victims. Tasks included establishing the base of operations by manually moving all required equipment from storage on site to the worksite, followed by a coordinated search, maneuvring through confined space, carrying equipment, operating tools, and extricating and carrying victims. The teams applied the common approach of “blitzing” the worksite for the first operational period, with all resources committed to the rescue operation for the first 4 hours followed by one team standing down to transition into a continuous operational shift rotation mode for the remaining 20 hours of the exercise. The rotation of teams between work and rest periods resulted in each participant working between 14.5 and 15.5 hours during of the 24-hour exercise. Prior to exercise commencement, the participants were informed of the exercise duration and that both teams would be working together for the initial shift. To prevent pacing related to differing shift lengths, participants were not informed of which team would continue working following the initial shift until cessation of that shift. All operations were carried out in compliance with international minimum standards as defined within the International Search and Rescue Advisory Group (INSARAG) Guidelines.13
Physiological Measures
Gastrointestinal temperature (Tgi) was utilized as a surrogate of core temperature and measured by an ingestible temperature sensor (Jonah, VitalSense, Respronics, Pittsburgh, PA) consumed with food ∼45 minutes prior to exercise commencement. It is likely that the ingestible pill transmitted stomach temperature during the initial stages of the exercise. Domitrovich et al14 demonstrated the validity of pill consumption 40 minutes prior to monitoring albeit in the absence of fluid consumption. While cold water (5 to 8 °C) consumption detrimentally influences Tgi accuracy,15 this potential confounder was minimized by storage of bottled water in ambient conditions that limited the gradient between Tgi and water temperature. The ingestible pill transmitted Tgi to a wearable receiver (EQ02, Equivital, Hidalgo Ltd, Cambridge, UK) that also measured and recorded heart rate (HR), respiratory rate (RR), and axilla skin temperature (Tsk) for storage every 5 seconds and was analyzed as the mean of 5-minute intervals. The EQ02 provides valid and reliable Tgi, HR and RR data during physical activity (Liu et al).16 While less information is available regarding the Infrared thermometer used for axilla skin temperature, infrared thermometry is a valid and reliable method of skin temperature assessment.17 Heart rate was expressed as absolute values and percentage of predicted maximum.18 Heart rate and Tgi were input into the modified physiological strain index (PSI) of Moran et al19 with initial Tgi assumed to be 37.0 °C for all participants.
Fluid Balance Variables
Urine specific gravity (USG) was assessed with a calibrated refractometer (Atago UG-α, Tokyo, Japan) as an indice of hydration status pre shift. Prior to commencing the exercise, participants were weighed semi-nude on a portable calibrated platform scale (UC321 A&D Mercury, Adelaide, SA, Australia), accurate to 0.05 kg. Post shift, participants removed attire and toweled non-evaporated perspiration from the skin and hair prior to body mass measurement. The resultant dehydration estimation was expressed as a percentage of pre-exercise body mass.
Participants had ad libitum access to bottled water and/or fluid reservoir during the exercise. Bottled water was provided for participants and stored at ambient conditions within the “clean zone,” remote from operations. Each team delivered water to personnel in the “work zone” at regular intervals. Fluid consumption was monitored by determining the mass of individual hydration reservoir and/or bottle(s) pre- and post-consumption. It was assumed that 1 kg equaled 1 L of fluid, and the difference in mass was the volume of fluid consumed. Participants were instructed to exclusively use the bottled water for consumption. Fully clothed body mass was determined immediately prior to, and following toilet breaks, with the body mass difference equaling urine volume. Fluid consumption, sweat rate, and sweat loss were calculated as per Brearley et al.20
Perceptual Variables
Perceptual ratings of thermal sensation and thermal discomfort were assessed prior to and immediately post shift via the modified numeric and descriptive scales of Gagge et al.21 Participants were instructed to rate overall thermal sensation and discomfort during the exercise when assessed post shift.
Environmental Conditions
Ambient dry bulb temperature, wet bulb temperature, relative humidity (RH), and black globe temperature were continuously assessed and recorded at 30-minute intervals from an environmental monitor (QuesTemp 36, Quest Technologies, Onoconomac, WI). The unit was positioned in full sunlight adjacent to the work zone throughout the study. The monitor calculated the Wet Bulb Globe Temperature (WBGT). Since environmental conditions within the pile could not be monitored during the exercise, ambient temperature and RH (DS1923 iButton, Maxim, Sunnyvale, CA) were measured and recorded at 30-minute intervals over 20 days for three positions within the pile, top, midpoint, and bottom. Mean (standard deviation [SD]) ambient temperature and RH data for 1330 to 1730 time period were 34.3 °C (3.9), 74.9% (15.8) at the top of the pile, 30.8 °C (2.4), 85.8% (12.8) at the midpoint of the pile, and 29.4 °C (1.5), 95.5% (5.5) at the bottom of the pile.
Statistical Analysis
Multivariate linear regression models, clustered by participant to control for repeated measures, were generated for the outcomes of Tgi, HR, RR, Tsk, and PSI. The mean Tgi of the HA and NHA groups demonstrated a biphasic response, intersecting at the 85th minute of shift. Therefore, separate models were produced for 0 to 85 minutes (phase 1), and 90 to 235 minutes (phase 2). The initial models included the potential confounders of body mass, height, and age. Differences between groups for height and age were not statistically significant (P > 0.10), resulting in their removal from the model in a stepwise manner. The resultant models were composed of the predictor variables of time (5-minute intervals), HA status, and body mass. Standardized effect size (Cohen d) analysis was used to interpret the magnitude of differences between groups. A Wilcoxon/Mann–Whitney U test assessed for differences in thermal sensation and thermal discomfort between groups at the start and during shift. The aforementioned analyses were performed by Stata (version 13.1, StataCorp, College Station, TX) with statistical significance set at P < 0.05. A statistical trend was identified as 0.05 < P < 0.10.
The area under the Tgi curves for HA and NHA was calculated by Prism 6 software (GraphPad, La Jolla, CA). An unpaired t test with Welch's correction tested differences between HA and NHA groups for area under the Tgi curve, participant characteristics, pre-exercise USG, sweat rate (mL hour−1 kg body mass−1), fluid consumption (mL hour−1 kg body mass−1), and dehydration (% body mass).
RESULTS
Participant Characteristics
Characteristics of the HA and NHA groups are summarized by Table 2. The NHA group had significantly higher body mass than the HA group (P = 0.049).
TABLE 2.
Participant Characteristics. Data are Mean (SD)
| Variable | HA | NHA | P |
| Age (yrs) | 37.9 (4.7) | 41.3 (6.6) | 0.26 |
| Body mass (kg) | 86.2 (5.1) | 95.7 (11.9) | 0.049* |
| Height (m) | 1.79 (0.05) | 1.83 (0.05) | 0.21 |
| Body mass index (kg m−2) | 26.5 (1.8) | 28.7 (3.2) | 0.11 |
HA, heat acclimatized; NHA, non-heat acclimatized; SD, standard deviation.
*Denotes significantly different (P < 0.05).
Physiological and Perceptual Responses
During the initial 30 minutes of shift, participant Tgi data demonstrated influence of fluid consumption, and were, therefore, excluded from analysis. Overall, 15 of the 16 participants attained or exceeded a Tgi of 38.5 °C, six participants exceeded 39.0 °C during the shift, and the maximal Tgi observed was 39.6 °C. After adjusting for body mass, the HA exhibited a significantly higher mean Tgi (38.3 °C) across the shift than NHA (38.0 °C) (P = 0.043), while sustaining similar mean Tsk (P = 0.27), mean HR (P = 0.84), and RR (P = 0.24) (Table 3). During the shift, area under the Tgi curve was significantly greater for HA than NHA (P = 0.027). When expressed as a percentage of predicted maximum, mean HR equated to 69.9% and 71.3% for HA and NHA groups, respectively (P = 0.20).
TABLE 3.
Summary of Physiological and Perceptual Responses. Data are Mean (SD)
| Phase | Physiological Variable | HA | NHA | ES | 95% CI | P |
| Overall | Tgi (°C) | 38.3 (0.6) | 38.0 (0.4) | 0.63 | 0.0–0.5 | 0.043* |
| HR (beats min−1) | 129.5 (27.6) | 129.5 (20.4) | 0.00 | −15.0–13.0 | 0.84 | |
| RR (breaths min−1) | 25.1 (7.1) | 26.6 (6.0) | 0.23 | −5.7–1.5 | 0.24 | |
| Tsk (°C) | 36.5 (1.0) | 37.1 (0.6) | 0.73 | −0.9–0.3 | 0.27 | |
| PSI | 5.4 (2.2) | 4.7 (1.4) | 0.38 | −0.3–1.2 | 0.20 | |
| Area under Tgi curve (°C min) | 552.7 (81.1) | 435.5 (83.8) | 1.42 | 16.1–218.2 | 0.027* | |
| Thermal sensation | 10.2 (1.0) | 10.1 (0.8) | 0.11 | −0.9–1.0 | 0.87 | |
| Thermal discomfort | 3.0 (1.1) | 3.1 (0.7) | 0.11 | −1.0–0.9 | 0.89 | |
| Phase 1 | Tgi (°C) | 37.8 (0.5) | 37.9 (0.5) | 0.14 | −0.5–0.5 | 0.97 |
| HR (beats min−1) | 108.9 (28.8) | 119.1 (15.4) | 0.44 | −36.9–11.6 | 0.28 | |
| RR (breaths min−1) | 22.5 (6.6) | 26.2 (5.6) | 0.61 | −8.1–1.2 | 0.012* | |
| Tsk (°C) | 36.9 (0.4) | 37.1 (0.6) | 0.39 | −1.0–0.2 | 0.13 | |
| PSI | 3.5 (2.1) | 4.0 (1.6) | 0.27 | −2.3–1.0 | 0.40 | |
| Area under Tgi curve (°C min) | 86.1 (46.3) | 93.4 (38.2) | 0.17 | −60.5–45.8 | 0.76 | |
| Phase 2 | Tgi (°C) | 38.5 (0.5) | 38.1 (0.3) | 0.99 | 0.2–0.7 | 0.005* |
| HR (beats min−1) | 141.2 (16.8) | 135.5 (17.5) | 0.33 | −6.2–18.7 | 0.30 | |
| RR (breaths min−1) | 26.6 (6.5) | 26.9 (6.1) | 0.04 | −5.2–4.5 | 0.88 | |
| Tsk (°C) | 36.2 (1.2) | 36.3 (1.1) | 0.09 | −1.1–0.5 | 0.47 | |
| PSI | 6.2 (1.7) | 5.0 (1.2) | 0.82 | 0.1–2.0 | 0.027* | |
| area under Tgi curve (°C min) | 465.4 (94.2) | 340.9 (49.6) | 1.65 | 24.1–224.7 | 0.022* |
CI, confidence interval; ES, effect size; HA, heat acclimatized; HR, heart rate; NHA, non-heat acclimatized; PSI, physiological strain index; RR, respiratory rate; SD, standard deviation; Tgi, gastrointestinal temperature; Tsk, axilla skin temperature.
*Denotes a statistical difference (P < 0.05).
Phase 1 ended at the 85th minute of shift where mean Tgi of the groups intersected at 38.2 °C. Thereafter, a relative mean Tgi plateau was observed for NHA, peaking at 38.4 °C 110 minutes into shift. Whereas mean Tgi of the HA group continued rising to plateau at 38.8 °C 5 minutes later. The phase 1 and 2 data are summarized by Table 3. The respiratory rate of NHA was significantly higher than HA during phase 1 (P = 0.012) as demonstrated by Fig. 2, while Tgi (P = 0.005), PSI (P = 0.027), and area under the Tgi curve (P = 0.022) were significantly higher for HA during phase 2. When expressed as a percentage of predicted maximum, HR was similar between groups during phase 1 (HA 58.4 ± 11.7, NHA 65.1 ± 11.1, P = 0.16) and phase 2 (HA 76.2 ± 8.2, NHA 74.7 ± 8.8, P = 0.91).
FIGURE 2.
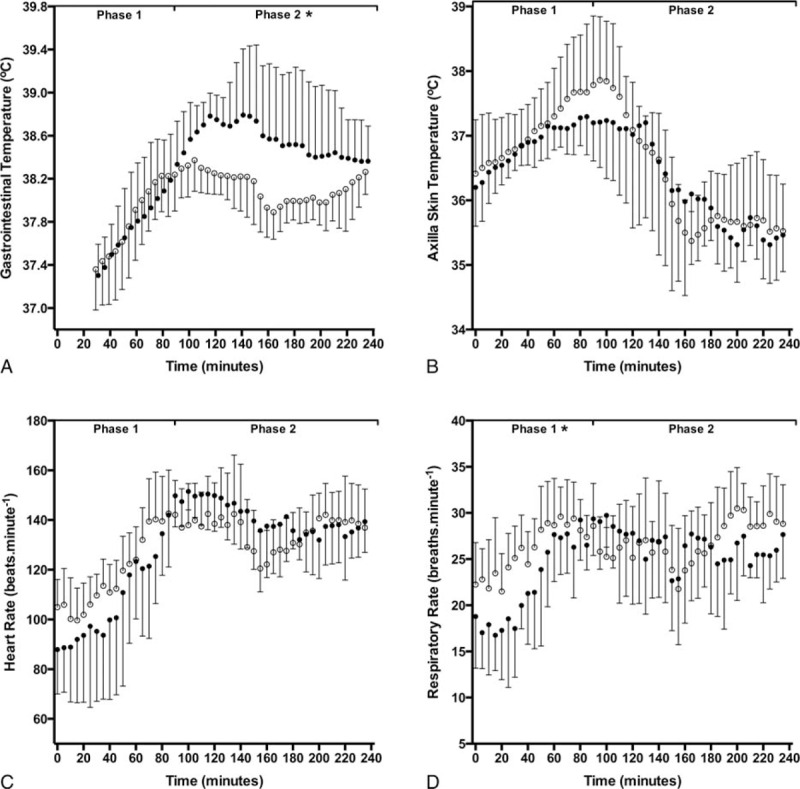
Mean gastrointestinal (A), axilla skin temperature (B), heart rate (C), and respiratory rate (D) responses to workshift for HA (●) and NHA (○) responders. Error bars represent SD. HA, heat acclimatized; NHA, non-heat acclimatized; SD, standard deviation. ∗Denotes a statistical difference (P < 0.05).
Thermal sensation (mean difference −0.5 [1.0], 95% confidence interval [CI] −0.5 to 1.5, P = 0.28, ES = 0.59) and thermal discomfort (mean difference −0.1 [0.7], 95% CI −0.4 to 0.5, P = 0.77, ES = 0.28) were not different between groups prior to start of shift. During shift, both groups rated their body temperature as hot (HA 3.1, NHA 3.0, P = 0.87), causing them the feel uncomfortable (HA 10.2, NHA 10.1, P = 0.89).
Fluid Balance
Pre-shift USG was similar between groups (P = 0.32). Sweat losses during shift ranged between 3.0 and 7.5 L, with mean sweat rate of 0.98 L hour−1 for HA, and 0.84 L hour−1 for NHA (Table 4). When expressed as a factor of body mass, sweat rate was 11.0 mL hour−1 per kg body mass for HA that trended higher (P = 0.08) than the 8.8 mL hour−1 per kg body mass for NHA. Fluid consumption was similar between groups (HA 9.6 v NHA 8.1 mL hour−1 kg−1, P = 0.22), resulting in replacement of ∼87% (HA) and ∼92% (NHA) of sweat losses, respectively. Overall, dehydration was comparable between groups (HA 0.8, NHA 0.5%, P = 0.64).
TABLE 4.
Summary of Fluid Balance Responses
| Fluid Balance Variable | HA | NHA | ES | 95% CI | P |
| Pre shift USG | 1.014 (0.009) | 1.010 (0.008) | 0.47 | −0.004–0.013 | 0.32 |
| Fluid consumption (L h−1) | 0.83 (0.19) | 0.77 (0.21) | — | — | — |
| Fluid consumption (mL h−1 kg−1) | 9.5 (1.9) | 8.1 (2.5) | 0.63 | −1.0–3.8 | 0.22 |
| Sweat rate (L h−1) | 0.98 (0.31) | 0.84 (0.12) | — | — | — |
| Sweat rate (mL h−1 kg−1) | 11.0 (3.2) | 8.8 (0.9) | 0.94 | −0.2–4.6 | 0.08* |
| Dehydration (%) | 0.8 (0.8) | 0.5 (1.0) | 0.35 | −0.8–1.3 | 0.64 |
CI, confidence interval; HA, heat acclimatized; NHA, non-heat acclimatized; USG, urine specific gravity.
*Denotes a statistical trend (P < 0.10).
Environmental Conditions
The mean (SD) environmental conditions of the shift were 34.0 °C (0.7) ambient dry bulb temperature, 48.0% (1.5) RH and WBGT of 31.4 °C (0.5).
DISCUSSION
Overall Thermal Response
This study simulated deployment of USAR personnel to an earthquake affected tropical region, with the workshift permitting comparison of physiological, perceptual, and fluid balance responses between HA and NHA groups. Based upon mean HR data, a moderate workload was sustained during the shift. The physical workload and concomitant metabolic heat production contributed to substantial elevations in Tgi, beyond the respective recommended limits of 38.0 °C for NHA, and 38.5 °C for HA.22 If the responses reported by this investigation were replicated during the aftermath of a sudden onset disaster, heat related illness would be a risk for USAR responders.1 As the initial account of physiological responses during USAR field operations, it is not possible to determine whether the reported responses are typical for tropical region deployments. The current investigation reported higher Tgi than the rectal temperature (mean, 37.0 to 38.4 °C) of HA soldiers undertaking patrol (2 hours) and reconnaissance (1.5 hours) in similar tropical field conditions.23 While the soldiers wore comparable PPC to the USAR personnel with the addition of weapon and webbing or pack, the exercises seemingly permitted some pacing of effort. Greater thermal strain was reported when soldiers of varied HA status undertook 20 km pack marching in slightly cooler tropical field settings (WBGT 27.6 °C). Target duration of less than 4 hours permitted less self-pacing and resulted in higher Tgi (mean 39.1 °C at end of exercise) and thermal sensation than either USAR group.24 The aforementioned military settings vary from the moderate physiological perturbation reported for HA medical responders (mean Tgi peaked at 37.8 °C).25 During a 3 hours simulated disaster in milder tropical conditions, the medical team wore lightweight ventilated PPC and did not perform physically arduous tasks. These factors were reflected by their substantially lower HR and overall physiological strain than for the USAR groups. Simulated firefighting tasks require a greater physical workload that is more comparable to USAR work rates than medical response, and results in rapid body heat storage when combined with insulative PPC in the tropics. Mean Tgi of HA firefighters during such simulations reached 38.5 °C within 30 minutes.26 While similarly rapid increases of Tgi were not observed for USAR personnel, the longer shift permitted development of higher peak Tgi for HA (38.8 °C), but not NHA (38.4 °C) during the current investigation.
Work rate is an important consideration for tropical deployments as it is a primary determinant of Tgi response in hot and humid conditions.27 The relatively high Tgi values reported by the current investigation were likely to be influenced by the authentic nature of the disaster scenario contributing to selection of workload. Based upon the limited research available, HA emergency responders/soldiers working in tropical field conditions endure substantially elevated core temperatures that are seemingly well tolerated where self-pacing is possible. We cannot exclude the possibility of USAR personnel consciously ignoring sensations of high body temperature and therefore cues to lessen workload, particularly where their actions may be lifesaving. In doing so, the USAR responders may develop Tgi considerably higher than reported by this investigation. Should that scenario eventuate, the thermal load is likely to be better tolerated by HA than NHA responders.
Heat Acclimatization
Divergent Tgi responses between HA and NHA groups classified the analysis of workshift into two phases. Phase 1 was characterized by NHA exhibiting a significantly higher RR (mean difference 3.7 breaths minute−1). Ventilation volume and RR are closely linked to metabolic rate, and the moderate effect for HR (mean difference 10.2 beats minute−1) provides evidence of similar to slightly higher cardiovascular and respiratory load for NHA during phase 1. However, no differences between groups for mean Tgi or area under the Tgi curve were observed during this phase. The significantly higher Tgi for HA (38.5 °C) compared with NHA (38.1 °C) during phase 2 resulted in ∼37% higher total thermal load, as represented by area under the Tgi curve. The phase 2 Tgi disparity between groups is the key finding of this investigation, and the first report of HA personnel sustaining higher core temperature than NHA in occupational field settings.
Adaptations conferred by HA are widely recognized to reduce the deep tissue temperature response to a given workload in hot conditions,3 rendering these Tgi results counterintuitive if workloads were comparable between groups. While HA and NHA personnel were equally distributed between the two working teams, opportunities existed to volunteer for physically arduous tasks within each group. Speculation of distinct work rate adjustments between groups cannot be verified, as workload measurement was not possible in the USAR setting. However, if the similar “Tgi to total work done” correlation from competitive sport in the heat28 were applied to this investigation, the results are indicative of a greater workload for HA responders during phase 2. Despite the higher Tgi for HA, the comparable thermal sensation (hot) and thermal discomfort (uncomfortable) during shift are symbolic of both groups regulating their work output according to how hot they felt.29 The apparent dissociation between Tgi and thermal sensation may be explained by the HA groups greater exposure to hot working conditions. The two-fold effect would not only promote regular elevations of Tgi to develop and maintain HA status (physiological adaptation), but also provide opportunities to refine pacing strategies in the heat (behavioral adaptation).
The environmental conditions, work tasks, and PPC were conducive to attainment of high deep tissue temperatures, as evidenced by six participants exceeding Tgi of 39.0 °C. Mean Tgi during the second phase of shift approximated the upper limit for HA and NHA workers,22 and approached the 38.6 to 39.7 °C Tgi range coinciding with volitional exhaustion in very hot conditions.3,11,27 Selection of workload by the USAR responders was likely mediated by a combination of physiological and psychological factors30 to prevent excessively high Tgi for extended periods. In addition to thermal sensation,29 personal experience and knowledge that the exercise had ∼20 hours remaining, of which each participant would work ∼11 hours in shifts were likely contributors.31
While athletes demonstrate less physiological perturbation at fixed workloads in the heat following HA,4 adoption of higher exercise intensity by HA would increase HR, RR, Tsk, and Tgi values as observed during phase 2. The significantly higher Tgi for HA responders may reflect limited efficiency of their excess sweat production and presumed higher cutaneous blood flow due to the tropical climate and PPC. A similar dissociation between HR and Tgi responses has been reported for team sport athletes during competition in hot conditions.28 Overall, chronic exposure to hot working conditions likely explains tolerance of higher Tgi by HA during phase 2.11
Fluid Balance
It is unclear whether the HA groups trend for higher sweat rate was due to the enhanced sweat production conferred by HA7 and/or the higher Tgi of the HA group.32 Despite HA adaptations promoting a greater evaporation efficiency of sweat,33 ambient water vapor and USAR PPC would both inhibit heat loss by evaporation. Hot and humid climates are synonymous with the accumulation of non-evaporated sweat in clothing,34 creating a humid microclimate within PPC. The high sweat rates can manifest in dehydration, however both groups replaced a high proportion of sweat losses as reported for field workers in the tropics,35 indicative of adequate access to water. Such fluid consumption rates are not likely to be matched during deployment unless a similarly structured approach to fluid provision is implemented. To assess the adequacy of fluid provision, pre and post shift body mass assessment is recommended, providing USAR management and responders daily feedback on hydration status.36
Limitations
A limitation of the current investigation was the classification of HA based upon climatic zones rather than physiological responses to heat tolerance testing (HTT).37 Adopting this approach is prone to error, as simply residing in the tropics is considered inadequate to confer HA status without regular bouts of sustained body heat storage.38 However, this limitation was partially mitigated by studying firefighters, as the occupational requirements of firefighting dictate frequent exposure to the environment while wearing protective clothing. In this regard, acclimatization to heat has been observed during a fire season for wildland firefighters.39 Partial HA during summer months is possible for responders based in non-tropical regions, yet adaptation is likely to be inferior to that developed as a result of the year round exposure of tropical based responders.
Unlike the vast majority of heat acclimatization investigations, this study compared the responses of HA and NHA participants in a field setting. While replicating a disaster scenario provided ecological validity, this study incorporated assessment of responses to working in the field, and was, therefore, not as controlled as laboratory investigations of HA status.
Speculation of pacing could be overcome by quantification of work rate. Disaster settings require tasks that ensure structural integrity of the rescue site, requiring high workloads while personnel are not moving in relation to their latitude/longitudinal position. Replicating this investigation in occupational settings where movement is indicative of workload would permit use of global positioning system (GPS) to simplify workload measurement.
This investigation assessed USAR responders during a 4-hour shift, representing less than half a shift during deployment. Hence, responses of HA and NHA personnel to full shifts and multi day deployments remain to be described.
Lastly, the commercial flight undertaken prior to the simulation by the Queensland based participants (three HA, eight NHA) may have influenced the results of this investigation. However, the short duration flight in an east to northwest direction only required a one time zone adjustment and is, therefore, expected to have minimal impact upon the USAR responders.40
Implications for Deployment
A consequence of deploying NHA responders is likely to be self-selected lower work rates and/or greater physiological perturbation than HA for a given workload. These outcomes should be factored into the operational capability of teams deploying NHA personnel. Such disadvantages may be offset by regulation of work tasks, however, that approach is not compatible with operational requirements.
If greater physiological perturbation than reported by this investigation eventuates, NHA responders will be particularly susceptible to acute and cumulative heat related illnesses. The risk of heat related illness for NHA would be amplified where pacing of effort is compromised such as during high priority assignments. Emergency tasks are most probable during the initial days of deployment, the time period that coincides with greatest vulnerability for heat related illness.41 While recommendations exist for graded exposure to hot working conditions,42 these are not tenable for the initial deployment team. Where deployments require rotation of USAR personnel, relieving teams could undertake physical training to maximize HA once notified of their impending deployment. In this regard, the provision of individual guidelines for heat acclimatization prior to deployment are worthy of consideration.43
Regular testing to quantify physiological readiness of USAR personnel for deployment is warranted. Options for testing include assessment of maximal aerobic power (or its prediction) in thermoneutral conditions, and HTT. The latter is typically undertaken in a controlled hot climate and used in military settings as part of the return to work of heat stroke sufferers. Responses to HTT and heat exposure in general are primarily determined by maximal aerobic power.44,45 Given that deployment of low fitness personnel increases the risk of heat related illness,46 operational readiness demands year round physical training. Tests that measure or accurately predict maximal aerobic power would provide USAR management insight into a candidate's physical training status and suitability for deployment to a tropical climate.
CONCLUSIONS
The novel finding of this study is that in a self-paced occupational field setting, HA personnel sustain higher core temperatures and physiological strain than NHA counterparts. The higher core temperatures translated to ∼37% greater total thermal load for HA than NHA, despite comparable perception of body temperature. Assisting NHA responders develop heat acclimatization in the home environment is warranted, ensuring physiological readiness for deployment to tropical climates.
RECOMMENDATIONS
Based upon the findings of this study, we recommend the annual delivery of heat awareness and management training to USAR personnel, and year round physical training inducing serial elevations of core temperature to maintain a base level of HA irrespective of season. Guidelines to develop HA status are also recommended for NHA personnel with sufficient notice of impending deployment.
Acknowledgments
The research team acknowledge the commitment of NTFRS and QFES firefighters and management to this project. The authors thank Julie Moore, Jody May Jones, and Brendan Mott for assistance with data collection.
Footnotes
This project was funded by a Trauma and Disaster Management (TRADIM) research grant.
The authors were funded by their respective employers and have no conflict of interest to declare.
REFERENCES
- 1.Goodman CS, Hogan DE. Hogan DE, Burstein JL. Urban search and rescue. Disaster Medicine. Philadelphia: Lippincott, Williams and Wilkins; 2007. 72–85.ISBN 0781726255. [Google Scholar]
- 2.Dilley M, Chen RS, Deichmann U, et al. Natural Disaster Hotspots: A Global Risk Analysis. Disaster Risk Management Series, Issue No. 5. Washington: The World Bank; 2005. [Google Scholar]
- 3.Brearley M, Walker A. Water immersion for post incident cooling of firefighters; a review of practical fire ground cooling modalities. Extrem Physiol Med 2015; 4:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burk A, Timpmann S, Kreegipuu K, Tamm M, Unt E, Oöpik V. Effects of heat acclimation on endurance capacity and prolactin response to exercise in the heat. Eur J Appl Physiol 2012; 112:4091–4101. [DOI] [PubMed] [Google Scholar]
- 5.Garrett AT, Creasy R, Rehrer NJ, Patterson MJ, Cotter JD. Effectiveness of short-term heat acclimation for highly trained athletes. Eur J Appl Physiol 2012; 112:1827–1837. [DOI] [PubMed] [Google Scholar]
- 6.Shido O, Sugimoto N, Tanabe M, Sakurada S. Core temperature and sweating onset in humans acclimated to heat given at a fixed daily time. Am J Physiol 1999; 276:R1095–R1101. [DOI] [PubMed] [Google Scholar]
- 7.Kobayashi Y, Ando Y, Takeuchi S, et al. Effects of heat acclimation of distance runners in a moderately hot environment. Eur J Appl Physiol Occup Physiol 1980; 45:189–198. [DOI] [PubMed] [Google Scholar]
- 8.Lorenzo S, Halliwill JR, Sawka MN, Minson CT. Heat acclimation improves exercise performance. J Appl Physiol 2010; 109:1140–1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wyndham CH. A survey of causal factors in heat stroke and of their prevention in the gold mining industry. SA J Inst Min Metall 1965; 66:125–155. [Google Scholar]
- 10.Pandolf KB, Burse RL, Goldman RF. Role of physical fitness in heat acclimatisation, decay and reinduction. Ergonomics 1977; 20:399–408. [DOI] [PubMed] [Google Scholar]
- 11.Cheung SS, McLellan TM. Heat acclimation, aerobic fitness, and hydration effects on tolerance during uncompensable heat stress. J Appl Physiol 1998; 84:1731–1739. [DOI] [PubMed] [Google Scholar]
- 12.Sawka MN, Latzka WA, Montain SJ, et al. Physiologic tolerance to uncompensable heat: intermittent exercise, field vs laboratory. Med Sci Sports Exer 2001; 33:422–430. [DOI] [PubMed] [Google Scholar]
- 13.United Nations Office for the Coordination of Humanitarian Affairs, International Search and Rescue Advisory Group. INSARAG Guidelines. Volume II: Preparedness and Response. 2015; Available at: http://www.insarag.org/en/methodology/guidelines.html (accessed 18 May, 2015). [Google Scholar]
- 14.Domitrovich JW, Cuddy JS, Ruby BC. Core-temperature sensor ingestion timing and measurement variability. J Athl Train 2010; 45:594–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilkinson DM, Carter JM, Richmond VL, Blacker SD, Rayson MP. The effect of cool water ingestion on gastrointestinal pill temperature. Med Sci Sports Exerc 2008; 40:523–528. [DOI] [PubMed] [Google Scholar]
- 16.Liu Y, Zhu SH, Wang GH, Ye F, Li PZ. Validity and reliability of multiparameter physiological measurements recorded by the Equivital LifeMonitor during activities of various intensities. J Occup Environ Hyg 2013; 10:78–85. [DOI] [PubMed] [Google Scholar]
- 17.Burnham RS, McKinley RS, Vincent DD. Three types of skin-surface thermometers: a comparison of reliability, validity, and responsiveness. Am J Phys Med Rehabil 2006; 85:553–558. [DOI] [PubMed] [Google Scholar]
- 18.Tanaka H, Monahan KD, Seals DR. Age-predicted maximal heart rate revisited. J Am Coll Cardiol 2001; 37:153–156. [DOI] [PubMed] [Google Scholar]
- 19.Moran DS, Shitzer A, Pandolf KB. A physiological strain index to evaluate heat stress. Am J Physiol 1998; 275:R129–R134. [DOI] [PubMed] [Google Scholar]
- 20.Brearley M, Norton I, Kingsbury D, Maas S. Responses of elite road motorcyclists to racing in tropical conditions: a case study. Int J Sports Physiol Perform 2014; 9:887–890. [DOI] [PubMed] [Google Scholar]
- 21.Gagge AP, Stolwijk JA, Hardy JD. Comfort and thermal sensations and associated physiological responses at various ambient temperatures. Environ Res 1967; 1:1–20. [DOI] [PubMed] [Google Scholar]
- 22.International Organisation for Standardisation. ISO 9886: 2004(E). Ergonomics—Evaluation of Thermal Strain by Physiological Measurements. Geneva: International Organisation for Standardisation; 2004. [Google Scholar]
- 23.Amos D, Hansen R, Lau WM, Michalski JT. Physiological and cognitive performance of soldiers conducting routine patrol and reconnaissance operations in the tropics. Mil Med 2000; 165:961–966. [PubMed] [Google Scholar]
- 24.Cotter JD, Roberts WS, Amos D, Lau WM, Prigg SK. Soldier Performance and Heat Strain During Evaluation of a Combat Fitness Assessment in Northern Australia. No. DSTO-TR-1023. Canberra: Defence Science and Technology Organisation; 2000. [Google Scholar]
- 25.Brearley MB, Heaney MF, Norton IN. Physiological responses of medical team members to a simulated emergency in tropical field conditions. Prehosp Disaster Med 2013; 28:139–144. [DOI] [PubMed] [Google Scholar]
- 26.Brearley M, Norton I, Trewin T, Mitchell C. Fire Fighter Cooling in Tropical Field Conditions. Darwin: National Critical Care and Trauma Response Centre; 2011. [Google Scholar]
- 27.Montain SJ, Sawka MN, Cadarette BS, Quigley MD, McKay JM. Physiological tolerance to uncompensable heat stress: effects of exercise intensity, protective clothing, and climate. J Appl Physiol 1994; 77:216–222. [DOI] [PubMed] [Google Scholar]
- 28.Mohr M, Nybo L, Grantham J, Racinais S. Physiological responses and physical performance during football in the heat. PLoS One 2012; 7:e39202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schlader ZJ, Simmons SE, Stannard SR, Mündel T. The independent roles of temperature and thermal perception in the control of human thermoregulatory behavior. Physiol Behav 2011; 103:217–224. [DOI] [PubMed] [Google Scholar]
- 30.Hartley GL, Flouris AD, Plyley MJ, Cheung SS. The effect of a covert manipulation of ambient temperature on heat storage and voluntary exercise intensity. Physiol Behav 2012; 105:1194–1201. [DOI] [PubMed] [Google Scholar]
- 31.Baden DA, McLean TL, Tucker R, Noakes TD, St Clair Gibson A. Effect of anticipation during unknown or unexpected exercise duration on rating of perceived exertion, affect, and physiological function. Br J Sports Med 2005; 39:742–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Galloway SD, Maughan RJ. Effects of ambient temperature on the capacity to perform prolonged cycle exercise in man. Med Sci Sports Exerc 1997; 29:1240–1249. [DOI] [PubMed] [Google Scholar]
- 33.Taylor NA. Human heat adaptation. Compr Physiol 2014; 4:325–365. [DOI] [PubMed] [Google Scholar]
- 34.Candas V, Hoeft A. Clothing, assessment and effects on thermophysiological responses of man working in humid heat. Ergonomics 1995; 38:115–127. [DOI] [PubMed] [Google Scholar]
- 35.Brearley M, Harrington P, Lee D, Taylor R. Working in hot conditions-a study of electrical utility workers in the northern territory of Australia. J Occup Environ Hyg 2015; 12:156–162. [DOI] [PubMed] [Google Scholar]
- 36.Cheuvront SN, Kenefick RW. Dehydration: physiology, assessment, and performance effects. Compr Physiol 2014; 4:257–285. [DOI] [PubMed] [Google Scholar]
- 37.Moran DS, Erlich T, Epstein Y. The heat tolerance test: an efficient screening tool for evaluating susceptibility to heat. J Sport Rehabil 2007; 20:215–221. [DOI] [PubMed] [Google Scholar]
- 38.Saat M, Sirisinghe RG, Singh R, Tochihara Y. Effects of short-term exercise in the heat on thermoregulation, blood parameters, sweat secretion and sweat composition of tropic-dwelling subjects. J Physiol Anthropol Appl Hum Sci 2005; 24:541–549. [DOI] [PubMed] [Google Scholar]
- 39.Lui B, Cuddy JS, Hailes WS, Ruby BC. Seasonal heat acclimatization in wildland firefighters. J Therm Biol 2014; 45:134–140. [DOI] [PubMed] [Google Scholar]
- 40.Leatherwood WE, Dragoo JL. Effect of airline travel on performance: a review of the literature. Br J Sports Med 2013; 47:561–567. [DOI] [PubMed] [Google Scholar]
- 41.Yamazaki F. Effectiveness of exercise-heat acclimation for preventing heat illness in the workplace. J UOEH 2013; 35:183–192. [DOI] [PubMed] [Google Scholar]
- 42.Occupational Safety and Health Administration, US Department of Labor. Section III, Chapter 4, Heat Stress: OSHA Technical Manual. Washington, DC: Occupational Safety and Health Administration, US Department of Labor; 1999. [Google Scholar]
- 43.Brearley M. Pre-deployment heat acclimatisation guidelines for disaster responders. Prehosp Disaster Med 2016; 31:85–89. [DOI] [PubMed] [Google Scholar]
- 44.Lisman P, Kazman JB, O’Connor FG, Heled Y, Duester PA. Heat tolerance testing: association between heat intolerance and anthropometric and fitness measurements. Mil Med 2014; 179:1339–1346. [DOI] [PubMed] [Google Scholar]
- 45.Cheung SS, McLellan TM. Comparison of short-term aerobic training and high aerobic power on tolerance to uncompensable heat stress. Aviat Space Environ Med 1999; 70:637–643. [PubMed] [Google Scholar]
- 46.Bedno SA, Urban N, Boivin MR, Cowan DN. Obesity and risk of heat illness among army trainees. Occup Med 2014; 64:461–467. [DOI] [PubMed] [Google Scholar]


