Abstract
Purpose:
Approximately 20% of hospitalized Medicare beneficiaries are discharged from the hospital to skilled nursing facilities (SNFs); and up to 23% of SNF patients return to the hospital within 30 days of hospital discharge, with pain as one of the most common symptoms precipitating hospital readmission. We sought to examine the prevalence of moderate to severe pain at hospital discharge to SNF, the incidence of new moderate to severe pain (relative to prehospitalization), and satisfaction with pain management among older acute care patients discharged to SNF.
Design and Methods:
Structured patient interviews were conducted with 188 Medicare beneficiaries discharged to 23 area SNFs from an academic medical center. Pain level (0–10) and satisfaction with pain management were assessed upon hospital admission, discharge, and within 1 week after transition to SNF.
Results:
There was a high prevalence of moderate to severe pain at each time point including prehospital (51%), hospital discharge (38%), and following SNF admission (53%). Twenty-eight percent of participants reported new moderate to severe pain at hospital discharge, whereas 44% reported new moderate to severe pain following SNF admission. Most participants reported being “satisfied” with their pain treatment, even in the context of moderate to severe pain.
Implications:
Moderate to severe pain is a common problem among hospitalized older adults discharged to SNF and continues during their SNF stay. Pain assessment and management should involve a specific, planned process between hospital and SNF clinicians at the point of care transition, even if patients express “satisfaction” with current pain management.
Key words: Acute care, Postacute care, Geriatrics, Pain assessment, Pain management
In 2011, 20% of all hospitalized Medicare beneficiaries were discharged from the hospital to skilled nursing facilities (SNFs) at a cost of $32 billion annually, with up to 23% of SNF patients returning to the hospital within 30 days (Medicare Payment Advisory Commission, 2012). Numerous studies have shown that older patients discharged from the hospital are at high risk for functional decline and loss of independence (Boyd et al., 2008; Covinsky et al., 2003; Ehlenbach et al., 2010). Moreover, pain has been identified as one of the most common symptoms precipitating hospital readmissions (Dombrowski, Yoos, Neufeld, & Tarshish, 2012) and/or returns to the emergency room shortly after hospital discharge (Milbrett & Halm, 2009; White, Kaplan, & Eddy, 2011).
Although pain is known to be common among older adults (Donald & Foy, 2004; Gibson & Lussier, 2012; Shega et al., 2013; Thielke et al., 2012), there is minimal information about the patient’s pain experience among hospitalized older patients discharged to SNF care settings. Available evidence suggests that pain is often poorly assessed and inadequately treated for older adults across a variety of health care settings including acute care and SNF (Gibson & Lussier, 2012). Moreover, recent evidence suggests that the discharge information sent to SNF providers from hospitals often lacks important clinical information related to many aspects of care including pain severity and management during the hospital stay thus potentially hindering timely, effective pain treatment at the SNF following hospital discharge (King et al., 2013). Recent studies, in fact, have highlighted multiple gaps in communication of important clinical information during the transition from hospital to SNF care settings (Gandara et al., 2009; King et al., 2013).
To our knowledge, there are currently no published studies that identify the proportion of hospitalized older patients discharged from acute care to SNF with moderate to severe pain. It is also unclear if patients’ pain levels at hospital discharge or following SNF admission reflect new or worsening pain relative to their prehospital pain levels. Finally, there is limited information about older patients’ satisfaction with pain management. A few studies have explored the relationship between pain level and satisfaction with pain management among select groups of adult acute care patients, and these findings are somewhat paradoxical, with patients often reporting satisfaction in the context of moderate to severe pain (Chung & Lui, 2003; Phillips, Gift, Gelot, Duong, & Tapp, 2013; Sauaia et al., 2005). These findings could be contradictory due to other influences on patients’ reports of satisfaction, such as recovery time or patient expectations.
Related to expectations, a survey study with community-dwelling older adults revealed that more than half of the survey respondents expected to experience more pain as a result of aging; and, low expectations regarding aging was independently associated with this older cohort placing less importance on seeking health care services for symptom management (Sarkisian, Hays, & Mangione, 2002). Other evidence suggests that older adults are more likely than younger adults to report satisfaction with their health care services, even in the context of unmet needs and/or suboptimal care quality (Jaipaul & Rosenthal, 2003; Levy-Storms, Schnelle, & Simmons, 2002; Simmons & Ouslander, 2005; Sun et al., 2000; Young, Meterko, & Desai, 2000).
These studies suggest that there may be a tendency for older acute care patients to report satisfaction with their pain management in the context of moderate to severe pain which could, in turn, decrease the likelihood that this patient population will seek changes in their pain treatment following hospital discharge, even if such changes are clinically warranted and potentially efficacious. Moreover, health care providers may not further evaluate and alter pain treatment if patients continue to report satisfaction with their current treatment. Lack of effective pain management after hospital discharge could place patients with new onset of moderate to severe pain at higher risk for developing chronic pain and/or pain-related functional decline (e.g., self-imposed restrictions to their daily physical and/or social activities due to pain) (Gibson & Lussier, 2012). The tendency for elderly patients to minimize their pain complaints to their health care providers has even been the focus of recent national media attention, wherein immobility, depression, sleep problems, loss of appetite, and social isolation were all cited as potential consequences of poor pain management (Brody, 2014).
Based on the literature to date, pain interview questions that capture not only a patient’s current pain level but also whether this pain level is different from their goal and/or prehospital pain levels may reveal more unmet needs in this patient population. This, in turn, could stimulate efforts by both health care providers and patients to evaluate their current pain management strategies. The purpose of the current project was to understand the trajectory of pain in older hospitalized patients during the transition from the hospital to SNF. In order to accomplish this, we assessed the prevalence of moderate to severe pain upon hospital admission and discharge to SNF, the incidence of new moderate to severe pain (relative to prehospitalization), and satisfaction with pain management in both the hospital and SNF care settings. The implications of these findings are discussed in the context of potential interventions during the transition from hospital to SNF that may reduce the probability that new or worsening pain will be accepted by patients as normal.
Methods
Participants and Setting
All Medicare patients discharged from one large university hospital to 23 area SNFs were prospectively included in this project from September 2013 through March 2014. Patients discharged to hospice (end-of-life) care were not eligible for SNF and were, thus, excluded from this project. Although most Medicare patients are older adults (≥65), there was not an exclusionary criterion based on age. There also was not an exclusionary criterion based on cognitive status, although patients who were unable (e.g., due to severe cognitive impairment or delirium) or unwilling (e.g., refusal) to respond to the interview questions at each time point were excluded from the analyses. The 23 SNFs were located in the middle Tennessee area and had an average total bed capacity of 118 (short + long-stay beds) and average total staffing (licensed nurses + nurse aides) of 4.18hr per resident per day (hprd). Both bed capacity and staffing levels were slightly higher than the average for SNFs throughout the state (TN state average = 114 beds and 3.97 total hprd) based on publicly reported data during the project period (http://www.medicare.gov/nursinghomecompare).
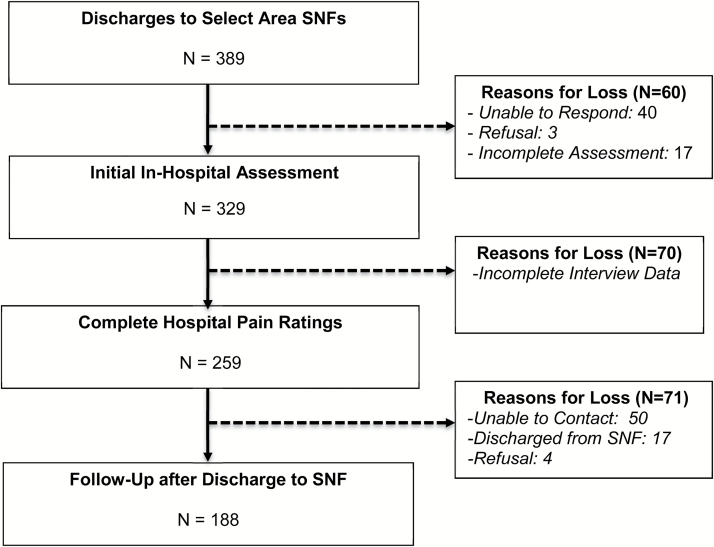
This project was funded by the Centers for Medicare and Medicaid Services (CMS) as a quality improvement project to reduce hospital readmissions among Medicare beneficiaries. The larger CMS-funded project required trained clinical personnel to conduct a standardized medical record review in conjunction with multiple interview-based assessments related to geriatric syndromes, one of which was pain. The university-affiliated Institutional Review Board provided approval for this project and waived the requirement for written, informed consent. Instead, eligible patients were provided a standardized description of the project by trained clinical personnel (at the time of their referral to one of the participating SNFs) and had the right to refuse the interview. If a patient completed the interview during his/her hospital stay, he/she was asked for permission to be contacted for interview again following transition to SNF. The sample for this project was defined as participants who had complete responses to all pain assessments at each time point (see Figure 1).
Figure 1.
Flow of participants.
Patient Characteristics
Trained clinical personnel reviewed participants’ medical records upon hospital admission and discharge for demographic information, admission diagnosis; length of hospital stay, discharge service, location of pain, and treatment were documented by nurses (e.g., scheduled and prescribed as needed [PRN] pain medications). Medical record data were supplemented by standardized in-person assessments of depression and cognitive status, using the five-item Geriatric Depression scale (GDS) and the Brief Interview for Mental Status (BIMS), respectively. The five-item GDS provides a total score between 0 (no symptoms) and 5 (all five depression symptoms endorsed) (Hoyl et al., 1999; Rinaldi et al., 2003). The BIMS is a short, validated screening tool for cognitive impairment with a total score range from 0 to 15 (0–7: severe impairment; 8–12: moderate impairment; 13–15: cognitively intact) (Chodosh et al., 2008; Saliba et al., 2012). Prior studies have demonstrated that older adults with mild to moderate cognitive impairment remain capable of reliably responding to structured interview questions about pain, so pain assessments were attempted with all participants (Cadogan et al., 2006; Chibnall & Tait, 2001; Chu, Schnelle, Cadogan, & Simmons, 2004). As part of this study, patients who had an unplanned readmission to the university-affiliated hospital within 30 days of hospital discharge were tracked and re-assessed for pain within 24-hr of hospital admission.
Pain Assessment
The primary purpose of the pain assessments in this project was to identify clinically important changes in pain from hospital admission to hospital discharge and following admission to SNF. A standardized interview protocol was used to ask patients about their pain at the following time points: initial in-hospital assessment (following referral to SNF and including a prehospital assessment), pain within 24-hr of hospital discharge and approximately 1 week (mean = 6.20 days ± 3.97) after SNF admission. Assessments following discharge to SNF were conducted via telephone interview for all patients who completed the in-hospital pain assessments and provided verbal permission to be contacted at the SNF. Three attempts were made to contact the patient. For those who did not provide contact information and also did not have an SNF room phone, project personnel interviewed the assigned SNF nurse to inquire about the patient’s most recent pain level documented in their SNF medical record, per licensed SNF nurses routine (i.e., daily per shift) pain assessments.
Pain was scored on an 11-point numeric rating scale from 0 (no pain) to 10 (worst pain imaginable) or categorized (none, mild, moderate, severe, or very severe/horrible) for the small number of patients who were unable to provide a numeric rating. An 11-point pain rating scale was used in this project because this is the same scale used by the participating hospital and required by SNFs (Research Triangle Institute [RTI] International, 2012). However, the following additional standardized questions also were asked to identify changes in pain from prehospitalization to hospital discharge and following SNF admission: (1) “Rate your worst pain over the last 5 days.” (2) “Rate your current pain on the same scale.” (3) “What is your goal pain score?” (4) “What was your usual pain, prior to being admitted to the hospital?” and (5) “Are you satisfied with the way your pain has been treated during your stay in the hospital?” Questions related to current pain (Question 2) and satisfaction (Question 5) were repeated within 24hr prior to and 1 week following hospital discharge, with Question 5 reworded to refer to satisfaction with pain treatment during the patient’s SNF stay. A direct satisfaction question was included in this project because similar types of satisfaction questions are commonly posed to patients and families in both the hospital and SNF care settings.
New Onset of Moderate to Severe Pain
New onset (i.e., acute) of moderate to severe pain was defined when the patient’s self-reported, prehospital pain level (Question 1) was <5 and their current pain level at either hospital discharge or after SNF admission (Question 2) was ≥5. New onset of moderate to severe pain for the subgroup of patients who responded to the pain questions using the categorical scale was defined as a change from no or mild pain to moderate, severe, or very severe/horrible. A numeric pain score of ≥5 was considered clinically significant pain for several reasons. First, federal regulations that guide pain assessments in the SNF care setting define an episode of moderate to severe pain as 5 or greater using the same 0–11 scale (RTI, 2012). In addition, multiple studies have similarly defined “significant pain” as a numeric rating of 5 or higher (Jones, Vojir, Hutt, & Fink, 2007; Jensen, Smith, Ehde, & Robinsin, 2001; Mendoza et al., 2004; Serlin, Mendoza, Nakamura, Edwards, & Cleeland, 1995), and one study showed that pain at this level interferes with functional status (Jones et al., 2007).
Satisfaction and Unmet Needs
Unmet needs related to pain treatment were defined in two ways: (1) if a participant reported dissatisfaction with pain treatment (Question 5 response = “no”) or (2) if a participant reported a current pain level (at hospital discharge or after SNF admission) that exceeded their goal pain level (i.e., comparison of responses between Questions 2 and 3), which yielded a numeric discrepancy score of 1, 2, 3, or more than 3 points (e.g., current pain of 5 vs. goal pain of two yields a discrepancy score of 3). Studies have shown that discrepancy indices capture unmet needs among older adults in a manner less influenced by acquiescent response bias than is true with direct satisfaction questions (Levy-Storms et al., 2002; Simmons & Ouslander, 2005).
Data Analysis
The responses of participants who provided numeric ratings were merged with those of the small subset of participants who provided only categorical ratings (N = 15). This was done by combining numeric responses equal to or greater than five (i.e., 5–10) with categorical responses of moderate to severe (or very severe/horrible). Chi-square analyses were used to compare the proportion of participants who reported moderate to severe pain at hospital discharge relative to 1 week after SNF admission for participants who provided complete pain ratings at each time point (Figure 1, N = 188). Comparisons also were conducted between those who completed all assessments (N = 188) versus those lost to SNF follow-up (Figure 1, N = 71). There also were two subanalyses to compare pain ratings among surgical (N = 84) versus nonsurgical patients (N = 104) and patients with severe cognitive impairment (BIMS ≤ 7; N = 8) or documented Delirium (Table 1, N = 9) versus those who were cognitively intact or mildly impaired (BIMS ≥ 8; N = 171).
Table 1.
Participant Characteristics (N = 188)
| Measure | Percent (n) or mean (±SD) |
|---|---|
| Demographic characteristics | |
| Sex, female | 55.9% (105) |
| Race, White | 85.1% (160) |
| Age (in years) | 74.6 (±12.2) |
| Proportion ≥65 years of age | 84.6% (159) |
| Length of hospital stay (in days) | 8.0 (±5.5) |
| Days between referral and discharge | 2.9 (±3.0) |
| Medical characteristics | |
| Percent GDS ≥ 2a | 43% (78 of 181) |
| BIMS total scoreb | 13.0 (±2.8) |
| Proportion with BIMS ≥13 | 75% (141) |
| Pain medications during hospital stay | |
| Scheduled medication only | 0.5% (1) |
| PRN medication only | 63.8% (120) |
| Both scheduled and PRN | 24.5% (46) |
| Pain medications at discharge | |
| Scheduled medication only | 6.9% (13) |
| PRN medication only | 48.4% (91) |
| Both scheduled and PRN | 32.4% (61) |
| Discharge services (most common) | |
| Orthopedic surgery | 26.2% (49) |
| General medicine | 18.2% (34) |
| Geriatric | 8.6% (16) |
Notes: BIMS = Brief Interview for Mental Status; GDS = Geriatric Depression scale.
aSeven participants had invalid GDS scores due to incomplete assessment.
bNine participants had invalid BIMS scores due to documented delirium.
Results
Participants
Figure 1 illustrates the derivation of the final sample of 188 participants who had complete data for all pain assessments. A total of 389 patients were discharged to one of 23 area SNFs during the data collection time period. An initial in-hospital assessment was completed for 329 (84.6%) participants. Complete interview data were obtained for all hospital-based assessments for 259 patients (78.7%). Pain ratings following discharge to SNF were obtained for 188 patients (72.6%). There were no significant differences in the average quantitative ratings for any of the hospital-based pain assessments when scores of participants who completed all assessments (N = 188) were compared to those lost to SNF follow-up (Figure 1, N = 71).
Table 1 shows the characteristics of the final sample of 188 participants who were predominately female (56%) and White (85%), with an average age of 75 (±12) years (85%, ≥65). Their average length of stay in the hospital was 8 (±5.5) days, but the initial hospital pain assessment did not occur until referral to SNF, which was approximately 5 days following hospital admission. Thus, in most cases, the participant’s response to (Question 1), “Rate your worst pain over the last 5 days…” reflected the period of time close to hospital admission. Forty-three percent of participants had a GDS score indicative of probable depression. The average BIMS score of 13 indicates that most participants (75%) were cognitively intact (BIMS ≥ 13).
Most participants received either PRN (64%) or both PRN and scheduled (25%) pain medications during their hospital stay. Discharge orders listed pain medications for most of these same patients. The most common admission diagnoses were: falls and fractures (24%), osteoarthritis (17%), and infections (13%). The most common discharge service was orthopedic surgery (Table 1). Forty-two percent reported pain at more than one body location and 13% reported generalized pain upon hospital discharge.
Pain Assessments
Table 2 shows the proportion of participants who reported moderate to severe pain (column 2) and new pain (column 3) during their hospital stay (rows 1–3) and following discharge to SNF (row 4). Column 2 shows these pain reports for the entire sample of 188 participants, whereas column 3 shows these pain reports for the subset of participants (N = 92) who reported their “usual pain” prior to hospital admission at a level of none to mild (i.e., <5) and, hence, could have experienced a new onset of moderate to severe pain in the hospital and/or following discharge to SNF. Results were comparable when the small subset of participants (N = 17) with severe cognitive impairment (BIMS ≤ 7) or documented delirium were excluded from these analyses. Results also were comparable between surgical and nonsurgical participants. Thus, the results are presented for the overall group of 188 participants.
Table 2.
Proportion of Participants With Moderate to Severe Pain and New Pain
| Location | Percent (n) with moderate/severe/ very severe pain (N = 188) | Percent (n) with new onseta of moderate/ severe/very severe pain (N = 92) | |
|---|---|---|---|
| In hospital | Worst pain in the last 5 days | 85.1% (160) | 76.1% (70) |
| Usual pain before hospital | 51.1% (96) | — | |
| Pain at discharge | 37.8% (71) | 28.3% (26) | |
| In skilled nursing facility | Pain at follow-up | 53.2% (100) | 43.5% (40) |
Note: aNew onset of moderate to severe pain was defined when the patient’s self-reported, prehospital pain level (Question 1) was <5 and their current pain level at either hospital discharge or after SNF admission (Question 2) was ≥5.
Of the overall group (N = 188), 85% reported their “worst pain in the last 5 days” as moderate to severe, whereas 51% (N = 96) reported their “usual pain” prior to hospital admission as moderate to severe. The proportion of participants who reported moderate to severe pain significantly declined to 38% (N = 71) within 24hr of hospital discharge (χ2 = 6.93, p < .01); however, this proportion significantly increased to 53% (N = 100) within 1 week following SNF admission (χ2 = 18.42, p < .001), which was comparable to prehospital pain levels. Across the entire sample, 16.5% (31 of 188) experienced an unplanned readmission to the hospital within 30 days of hospital discharge, and 41.9% (13 of 31) of those readmitted reported moderate to severe pain on the day of hospital readmission.
For the subset of participants who reported new onset of moderate to severe pain (Table 2, N = 92), 76% (n = 70) endorsed this level as their “worst pain in the last 5 days” upon initial hospital assessment, whereas only 28% (N = 26) endorsed this level at hospital discharge. Following SNF admission, however, the proportion of participants with new onset of moderate to severe pain significantly increased to 44% (N = 40) relative to hospital discharge (χ2 = 7.08, p < .01).
Unmet Needs With Pain Management
Overall, the majority of participants reported satisfaction with their pain treatment both in the hospital and SNF care settings (93% and 94%, respectively). These proportions were comparable among the subsets of participants who endorsed moderate to severe pain in each care setting, patients with new pain and those who reported a continuation of significant prehospital pain. These proportions also were comparable among both surgical and nonsurgical patients. In contrast, the discrepancy between participants’ expressed “goal” and “current” pain levels indicated a much higher level of unmet need. Specifically, 40% of participants reported current pain that exceeded their goal pain by more than 4 points (on the 0–10 numeric scale) either at hospital discharge and/or after SNF admission. The average discrepancy between participants’ current and goal pain levels in the hospital and SNF care settings were 2.96 (±3.22) and 3.63 (±3.27), respectively, with a mode of 4 in both care settings.
Discussion
To our knowledge, this is the first descriptive study to document that a significant proportion of older patients discharged to SNF left the hospital with moderate to severe pain, and which, for many, reflected a level of pain that was higher than their usual, or prehospital, pain level. Moreover, the proportion of participants who endorsed new onset of moderate to severe pain increased from hospital discharge to 1 week after SNF admission. These findings highlight a need to effectively communicate clinically important information about pain during the transition from hospital to SNF and develop patient-centered interventions related to pain management for both care settings.
In addition, the overwhelming majority of participants reported “satisfaction” with their pain treatment even in the context of moderate to severe pain and despite a significant discrepancy between their current and goal pain levels. This finding is clinically important because, if patients believe that nothing more can be done to treat or manage their pain, they may be less likely to report their pain symptoms to subsequent care providers or seek alternative treatments (Sarkisian et al., 2002). This may, in turn, increase the likelihood that a new onset of moderate to severe pain will become chronic or precipitate a hospital readmission, for at least some patients (Dombrowski et al., 2012). This phenomenon of patient-reported satisfaction in the context of suboptimal care quality has been reported in multiple studies (Brody, 2014; Levy-Storms et al., 2002; Simmons & Ouslander, 2005); thus, this finding is not surprising. However, there is a risk that older patients who experience multiple transitions in care may continue to receive suboptimal pain management in each care setting due to their own reduced expectations (Brody, 2014; Levy-Storms et al., 2002; Sarkisian et al., 2002; Simmons & Ouslander, 2005) combined with gaps in communication among providers (Gandara et al., 2009; King et al., 2013).
In light of these findings, a potential next step would be to evaluate interventions that include patient education about potential pain management strategies, including non-pharmacological treatments, as well as the potential risks of continuing to live with chronic pain such as a reduction in physical activity and associated functional decline, depression, and other aspects of quality of life (Boyd, et al., 2008; Brody, 2014; Covinsky et al., 2003; Donald & Foy, 2004; Ehlenbach et al., 2010). Although all hospitalized older patients who endorse pain symptoms may benefit from this type of intervention, patients discharged from the hospital with a new onset of moderate to severe pain may be a higher risk group (Dombrowski et al., 2012; Gibson & Lussier, 2012; Shega et al., 2013). Moreover, the fact that many patients who reported satisfaction also expressed a discrepancy between their goal and current pain levels suggests that these patients may be receptive to educational efforts to improve their pain management. Future work should explore patients’ underlying fears and assumptions related to pain management via an in-depth qualitative interview approach to better understand their treatment preferences as well as potential gaps in their knowledge of alternative treatments.
There are several important limitations of this project. First, this project was conducted in one university hospital and 23 area SNFs with mostly cognitively intact older patients. Thus, results may not be generalizable to other hospital and SNF settings or cognitively impaired older patients, although the prevalence of prehospital pain in this project was comparable to estimates reported in other studies (Elliott, Smith, Penny, Smith, & Chambers, 1999; Gibson & Lussier, 2012; Shega et al.,; Thielke et al., 2012). Second, this project did not include a standardized evaluation of existing pain treatments; thus, it is unknown to what extent alternative treatments and/or non-pharmacological approaches may have been appropriate for this patient population. Related to non-pharmacological approaches, the pain interview also did not include questions about patients’ awareness of alternative approaches to manage their pain. Third, this project did not include follow-up assessments beyond the first week after SNF admission. Data also were not collected related to the extent to which pain may have affected patients’ functional status and quality of life. Other studies have shown that moderate to severe pain levels significantly affect functional status and quality of life among older adults (Gibson & Lussier, 2012; Shega et al., 2013; Thielke et al., 2012), and a recent study showed that pain in more than one body location predicts functional decline among community-dwelling older adults (Eggermont et al., 2014). Finally, we did not examine the impact of moderate to severe pain on hospital readmissions or other health care utilization (Dombrowski et al., 2012; Milbrett & Halm, 2009; White et al., 2011).
Despite these limitations, however, there are at least two important implications of these findings. First, these data suggest that patient-centered education interventions about pain management should be initiated in the hospital and continue during the transition from the hospital to SNF to help ensure optimal pain management for all patients, but, in particular for those with moderate to severe pain, those with new onset of pain and those who express a discrepancy between their current and goal pain levels. These patients may be best identified by using a series of screening questions similar to those used in this project. In short, it is not sufficient to simply ask patients to rate their current pain and overall satisfaction with pain management. Instead, providers in both the hospital and SNF care settings should inquire about patients’ preferences related to pain management to ensure understanding of patients’ concerns and expectations to inform better pain management in this population.
Second, related to the transition from acute care to SNF, there is evidence that the information sent to SNFs from acute care often lacks important clinical information related to pain severity and pain management (Gandara et al., 2009; King et al., 2013). Thus, hospital discharge information sent to SNFs should highlight when a patient is being discharged from the hospital with moderate to severe pain and/or a new onset of pain to foster timely, effective pain treatment. In particular, hospitals need to improve the coordination of pain management at the point of care transition to inform follow-up pain management at the SNF. A few studies focused on improving care transitions for hospitalized older adults have utilized nurses or other trained staff to support patients during care transitions and facilitate timely communicate with key providers at the next level of care to reduce hospital readmissions or other health care utilization (Coleman, Parry, Chalmers, & Min, 2006; Jack et al., 2009; Manderson, Mcmurray, Piraino, & Stolee, 2012). A similar strategy potentially could be used to improve pain management across care settings. In addition to timely pain management, this information is critical to SNF providers so that they can continue patient education efforts initiated in the hospital to prevent new or worsening pain from being accepted by patients or becoming chronic.
Acknowledgments
This research was supported by the Department of Health and Human Services, Centers for Medicare & Medicaid Services (grant no. 1C1CMS331006) awarded to Principal Investigator, Dr. J. F. Schnelle, PhD. Dr. E. E. Vasilevskis was supported by the National Institute on Aging of the National Institutes of Health award (grant no. K23AG040157), the Veterans Affairs Clinical Research Center of Excellence, and the Geriatric Research, Education and Clinical Center (GRECC). Dr. S. Bell was supported by K12HD043483-11 from NIH/NICHD and by the Eisenstein Women’s Heart Fund. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the U.S. Department of Health and Human Services or any of its agencies, the National Institutes of Health or the Department of Veterans’ Affairs. Each coauthor contributed significantly to the manuscript. None of the authors have significant conflicts of interest to report related to this project or the results reported within this manuscript.
References
- Boyd C. M. Landefeld C. S. Counsell S. R. Palmer R. M. Fortinsky R. H. Kresevic D.,…Covinsky K. E (2008). Recovery of activities of daily living in older adults after hospitalization for acute medical illness. Journal of the American Geriatric Society, 56, 2171–2179. doi:10.1111/j.1532-5415.2008.02023.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody J. E. (2014, March 3). The perils of toughing it out. The New York Times. Retrieved from http://well.blogs.nytimes.com/
- Cadogan M. P. Schnelle J. F. Al-Sammarrai N. R. Yamamoto-Mitani N. Cabrera G. Osterweil D., & Simmons S. F (2006). A standardized quality assessment system to evaluate pain detection and management in the nursing home. Journal of the American Medical Association, 7, S11–S19. doi:10.1016/j.jamda.2005.12.011 [DOI] [PubMed] [Google Scholar]
- Chibnall J. T., & Tait R. C (2001). Pain assessment in cognitively impaired and unimpaired older adults: A comparison of four scales. Pain, 92, 173–186. doi:10.1016/S0304-3959(00)00485-1 [DOI] [PubMed] [Google Scholar]
- Chodosh J. Edelen M. O. Buchanan J. L. Yosef J. A. Ouslander J. G. Berlowitz D. R.,…Saliba D (2008). Nursing home assessment of cognitive impairment: Development and testing of a brief instrument of mental status. Journal of the American Geriatric Society, 56, 2069–2075. doi:10.1111/j.1532-5415.2008.01944.x [DOI] [PubMed] [Google Scholar]
- Chu L. Schnelle J. F. Cadogan M. P., & Simmons S. F (2004). Using the minimum data set to select nursing home residents for interview about pain. Journal of the American Geriatric Society, 52, 2057–2061. doi:10.1111/j.1532-5415.2004.52565.x [DOI] [PubMed] [Google Scholar]
- Chung J. W., & Lui J. C (2003). Postoperative pain management: Study of patients’ level of pain and satisfaction with health care providers’ responsiveness to their reports of pain. Nursing and Health Sciences, 5, 13–21. doi:10.1046/j.1442-2018.2003.00130.x [DOI] [PubMed] [Google Scholar]
- Coleman E. A. Parry C. Chalmers S., & Min S. J (2006). The care transitions intervention: Results of a randomized controlled trial. Archives of Internal Medicine, 166, 1822–1828. [DOI] [PubMed] [Google Scholar]
- Covinsky K. E., Palmer R. M., Fortinsky R. H., Counsell S. R., Stewart A.L., Kresevic D., …Landefeld C. S. (2003). Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: Increased vulnerability with age. Journal of the American Geriatric Society, 51, 451–458. doi:10.1046/j.1532-5415.2003.51152.x [DOI] [PubMed] [Google Scholar]
- Dombrowski W. Yoos J. L. Neufeld R., & Tarshish C. Y (2012). Factors predicting rehospitalization of elderly patients in a postacute skilled nursing facility rehabilitation program. Archives of Physical Medicine and Rehabilitation, 93, 1808–1813. doi:10.1016/j.apmr.2012.04.018 [DOI] [PubMed] [Google Scholar]
- Donald I. P., & Foy C (2004). A longitudinal study of joint pain in older people. Rheumatology, 43, 1256–1260. doi:10.1093/rheumatology/keh298 [DOI] [PubMed] [Google Scholar]
- Eggermont L. H., Leveille S. G., Shi L., Kiely D. K., Shmerling R. H., Jones R. N., …Bean J. F. (2014). Pain characteristics associated with the onset of disability in older adults: The maintenance of balance, independent living, intellect, and zest in the elderly Boston study. Journal of the American Geriatric Society, 62, 1007–1016. doi:10.1111/jgs.12848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlenbach W. J. Hough C. L. Crane P. K. Haneuse S. J. Carson S. S. Curtis J. R., & Larson E. B (2010). Association between acute care and critical illness hospitalization and cognitive function in older adults. Journal of the American Medical Association, 303, 763–770. doi:10.1001/jama.2010.167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott A. M. Smith B. H. Penny K. I. Smith W. C., & Chambers W. A (1999). The epidemiology of chronic pain in the community. The Lancet, 354, 1248–1252. doi:10.1016/S0140-6736(99)03057-3 [DOI] [PubMed] [Google Scholar]
- Gandara E. Moniz T. Ungar J. Lee J. Chan- Macrae M. O’Malley T., & Schnipper J. L (2009). Communication and information deficits in patients discharged to rehabilitation facilities: An evaluation of five acute care hospitals. Journal of Hospital Medicine, 4, E28–E33. doi:10.1002/jhm.474 [DOI] [PubMed] [Google Scholar]
- Gibson S.J., & Lussier D (2012). Prevalence and relevance of pain in older persons. Pain Med, 13 (Suppl. 2), S23–S26. doi:10.1111/j.1526-4637.2012.01349.x [DOI] [PubMed] [Google Scholar]
- Hoyl M. T. Alessi C. A. Harker J. O. Josephson K. R. Pietruszka F. M. Koelfgen M.,…Rubenstein L. Z (1999). Development and testing of a five-item version of the geriatric depression scale. Journal of the American Geriatric Society, 47, 873–878. [DOI] [PubMed] [Google Scholar]
- Jack B. W. Veerappa K. C. Anthony D. Greenwald J. L. Sanchez G. M. Johnson A.…Culpepper L (2009). A reengineered hospital discharge program to decrease rehospitalization: A randomized trial. Annals of Internal Medicine, 150, 178–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaipaul C. K., & Rosenthal G. E (2003). Are older patients more satisfied with hospital care than younger patients? Journal of General Internal Medicine, 18, 23–30. doi:10.1046/j.1525-1497.2003.20114.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen M. P. Smith D. G. Ehde D. M., & Robinsin L. R (2001). Pain site and the effects of amputation pain: Further clarification of the meaning of mild, moderate, and severe pain. Pain, 91, 317–322. doi:10.1016/S0304-3959(00)00459-0 [DOI] [PubMed] [Google Scholar]
- Jones K. R. Vojir C. P. Hutt E., & Fink R (2007). Determining mild, moderate, and severe pain equivalency across pain-intensity tools in nursing home residents. Journal of Rehabilitation Research and Development, 44, 305. doi:10.1682/JRRD.2006.05.0051 [DOI] [PubMed] [Google Scholar]
- King B. J. Gilmore- Bykovskyi A. L. Roiland R. A. Polnaszek B. E. Bowers B. J., & Kind A. J (2013). The consequences of poor communication during transitions from hospital to skilled nursing facility: A qualitative study. Journal of the American Geriatric Society, 61, 1095–1102. doi:10.1111/jgs.12328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy-Storms L. Schnelle J. F., & Simmons S. F (2002). A comparison of methods to assess nursing home residents’ unmet needs. The Gerontologist, 42, 454–461. doi:10.1093/geront/42.4.454 [DOI] [PubMed] [Google Scholar]
- Manderson B. Mcmurray J. Piraino E., & Stolee P (2012). Navigation roles support chronically ill older adults through healthcare transitions: A systematic review of the literature. Health and Social Care in the Community, 20, 113–127. doi:10.1111/j.1365-2524.2011.01032.x [DOI] [PubMed] [Google Scholar]
- Medicare Payment Advisory Commission (US). (2012). Report to the Congress: Medicare payment policy. Washington, DC: Medicare Payment Advisory Commission. [Google Scholar]
- Mendoza T. R., Chen C., Brugger A., Hubbard R., Snabes M., Palmer S. N., …Cleeland C.S. (2004). Lessons learned from a multiple-dose post-operative analgesic trial. Pain, 109, 103–109. doi:10.1016/j.pain.2004.01.015 [DOI] [PubMed] [Google Scholar]
- Milbrett P., & Halm M (2009). Characteristics and predictors of frequent utilization of emergency services. Journal of Emergency Nursing, 35, 191–198. doi:10.1016/j.jen.2008.04.032 [DOI] [PubMed] [Google Scholar]
- Phillips S. Gift M. Gelot S. Duong M., & Tapp H (2013). Assessing the relationship between the level of pain control and patient satisfaction. Journal of Pain Research, 6, 683–689. doi:10.2147/JPR.S42262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Research Triangle Institute (RTI) International (US). (2012). MDS 3.0 quality measures: User’s manual. Research Triangle Park, NC: Research Triangle Institute International. [Google Scholar]
- Rinaldi P., Mecocci P., Benedetti C., Ercolani S., Bregnocchi M., Menculini G., …Cherubini A. (2003). Validation of the five‐item geriatric depression scale in elderly subjects in three different settings. Journal of the American Geriatric Society, 51, 694–698. doi:10.1034/j.1600-0579.2003.00216.x [DOI] [PubMed] [Google Scholar]
- Saliba D., Buchanan J., Edelen M. O., Streim J., Ouslander J., Berlowitz D., Chodosh J. (2012). MDS 3.0: Brief interview for mental status. Journal of American Medical Directors Association, 13, 611–617. doi:10.1016/j.jamda.2012.06.004 [DOI] [PubMed] [Google Scholar]
- Sarkisian C.A. Hays R. D., & Mangione C. M (2002). Do older adults expect to age successfully? The association between expectations regarding aging and beliefs regarding healthcare seeking among older adults. Journal of the American Geriatric Society, 50, 1837–1843. doi:10.1046/j.1532-5415.2002.50513.x [DOI] [PubMed] [Google Scholar]
- Sauaia A. Min S. J. Leber C. Erbacher K. Abrams F., & Fink R (2005). Postoperative pain management in elderly patients: Correlation between adherence to treatment guidelines and patient satisfaction. Journal of the American Geriatrics Society, 53, 274–282. doi:10.1111/j.1532-5415.2005.53114.x [DOI] [PubMed] [Google Scholar]
- Serlin R. C. Mendoza T. R. Nakamura Y. Edwards K. R., & Cleeland C.S (1995). When is cancer pain mild, moderate or severe? Grading pain severity by its interference with function. Pain, 61, 277–284. doi:10.1016/0304-3959(94)00178-H [DOI] [PubMed] [Google Scholar]
- Shega J. W., Andrew M., Kotwal A., Lau D. T., Herr K., Ersek M., …Dale W. (2013). Relationship between persistent pain and 5-year mortality: A population-based prospective cohort study. Journal of the American Geriatric Society, 61, 2135–2141. doi:10.1111/jgs.12554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmons S. F., & Ouslander J. G (2005). Resident and family satisfaction with incontinence and mobility care: Sensitivity to intervention effects? The Gerontologist, 45, 318–326. doi:10.1093/geront/45.3.318 [DOI] [PubMed] [Google Scholar]
- Sun B. C. Adams J. Orav E. J. Rucker D. W. Brennan T. A., & Burstin H. R (2000). Determinants of patient satisfaction and willingness to return with emergency care. Annals of Emergency Medicine, 35, 426–434. doi:10.1067/mem.2000.104195 [PubMed] [Google Scholar]
- Thielke S. M., Whitson H., Diehr P., O’Hare A., Kearney P. M., Chaudry S. I., …Newman A. (2012). Persistence and remission of musculoskeletal pain in community‐dwelling older adults: Results from the cardiovascular health study. Journal of the American Geriatric Society, 60, 1393–1400. doi:10.1111/j.1532-5415.2012.04082.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- White D. Kaplan L., & Eddy L (2011). Characteristics of patients who return to the emergency department within 72 hours in one community hospital. Advanced Emergency Nursing Journal, 33, 344–353. doi:10.1097/TME.0b013e31823438d6 [DOI] [PubMed] [Google Scholar]
- Young G. J. Meterko M., & Desai K. R (2000). Patient satisfaction with hospital care: Effects of demographic and institutional characteristics. Medical Care, 38, 325–334. [DOI] [PubMed] [Google Scholar]