Abstract
Background
In Afghanistan, Médecins Sans Frontières provided specialised trauma care in Kunduz Trauma Centre (KTC), including physiotherapy. In this study, we describe the development of an adapted functional score for patient outcome monitoring, and document the rehabilitation care provided and patient outcomes in relation to this functional score.
Methods
A descriptive cohort study was done, including all patients admitted in the KTC inpatient department (IPD) between January and June 2015. The adapted functional score was collected at four points in time: admission and discharge from both IPD and outpatient department (OPD).
Results
Out of the 1528 admitted patients, 92.3% (n = 1410) received at least one physiotherapy session. A total of 1022 patients sustained either lower limb fracture, upper limb fracture, traumatic brain injury or multiple injury. Among them, 966 patients received physiotherapy in IPD, of whom 596 (61.7%) received IPD sessions within 2 days of admission; 696 patients received physiotherapy in OPD. Functional independence increased over time; among patients having a functional score taken at admission and discharge from IPD, 32.2% (172/535) were independent at discharge, and among patients having a functional score at OPD admission and discharge, 79% (75/95) were independent at discharge.
Conclusions
The provision of physiotherapy was feasible in this humanitarian setting, and the tailored functional score appeared to be relevant.
Keywords: Function, MSF, Operational Research, Outcome measure, Rehabilitation, Trauma
Introduction
Trauma represents an important burden in low and middle income countries (LMIC).1 Increased quality of care has led to a higher survival rate of severely injured patients, leaving more individuals with long term disabilities.2 Functional recovery is critical in LMIC, as the individual's physical capacities influence their ability to access essential services and support their family–particularly so in crisis contexts, where the environment is exceptionally challenging.3 However, physiotherapy services are usually scarce in LMICs and not systematically implemented within trauma teams,4,5 despite strong recommendations for early rehabilitation and continuum of care at community level.6,7 Two recent literature reviews on ‘injury and rehabilitation in crisis contexts’8,9 outlined the lack of evidence-based literature in LMIC, and in particular, the tendency towards having studies focusing on one particular medical condition or body region (i.e., spinal cord injury,10 amputation,11 lower limb injury12), a lack of consensus on outcome measures,9 and the strong focus on surgical and medical care (versus rehabilitation).8
Monitoring of trauma care programmes has traditionally focused on indicators such as mortality, complications (i.e., infection, mal-union), and length of hospital stay, with limited attention to functional recovery.13,14 Over the past decades, and only more recently in the humanitarian field, there has been a progressive switch towards assessing patient functionality, both for management of individual patients and for monitoring and evaluation of surgical and rehabilitation programme performance.13-15 Different tools have been validated for this purpose, including generic tools such as the Functional Independence Measure (FIM), the Barthel Index, the European Quality of Life 5D (EQ-5D) and the Short Musculoskeletal Function Assessment (SMFA); or body region/condition-specific tools such as the Disability Arm Shoulder and Hand score (DASH) and the Harris Hip Score (HHS). Limitations of their use in trauma care have been underlined: generic tools may not be sensitive enough for all conditions, while condition-specific tools may be challenging when dealing with various types of trauma and the multiple injured.16,17 Moreover, none of those tools were designed for emergency humanitarian contexts,4 and are seen as impractical in such contexts, due to either their lengthy administration time, requirement for trained staff, lack of intercultural validity, and inadequacy for largely illiterate populations in the case of self-reported tools (e.g., SMFA).18 The lack of adapted tools represents a challenge to patient management and programme monitoring and evaluation. In response to this gap,4 Handicap International has adapted existing measures to design a tailored, simplified tool, allowing assessment of functional recovery of complex trauma patients in humanitarian settings.
In the conflict context of Afghanistan, Médecins Sans Frontières (MSF) initiated a partnership with Handicap International in 2011 to integrate physiotherapy in the Kunduz Trauma Centre (KTC), where this adapted functional score was introduced.
This study was therefore conducted to describe the characteristics of trauma patients who received physiotherapy care in KTC and the feasibility of providing such care in a resource-limited setting, as well as describe the relevance of the adapted functional score and the evolution of functional recovery among patients at KTC.
Materials and methods
Study design and setting
This was a retrospective cohort study, using routinely collected program data.
MSF opened KTC in 2011 in the Kunduz province of Northern Afghanistan. The province has about one million inhabitants and is an area of active conflict, particularly following the withdrawal of foreign troops from 2012. In KTC, care was provided to all trauma cases presenting within 30 days of injury, regardless of the cause of injury (violent trauma, road traffic accidents, domestic injuries) and the type of trauma, with the exception of patients with burns or spinal cord injuries, who were referred to other health centres. The package of care comprised an emergency department, operating department providing bone fixation (internal and external), intensive care unit, inpatient department (IPD) and outpatient department (OPD), as well as mental health and physiotherapy services, provided both in IPD and OPD. KTC was the only specialised trauma centre functioning in Northern Afghanistan; however, the US bombing of the hospital on 3 October 2015, during which 42 people lost their lives, destroyed essential parts of the hospital and brought an end to these services, denying the population access to quality trauma care.
Physiotherapy programme
The physiotherapy department was set up in KTC in October 2011, in a country where, even though physiotherapy is a growing field,19 physical and functional rehabilitation services are still not widely available at hospital or community level. By 2015, the department was managed by a team of eight national physiotherapists, providing rehabilitation care in IPD (including intensive care unit) and OPD, to trauma patients with reduced mobility (of one or several limbs), post-surgery and/or breathing difficulties. Their objective was to allow patients to regain function and to prevent secondary complications, through the provision of physical and functional rehabilitation, including education of caregivers. Patients were discharged from OPD physiotherapy care once the functional goals set by the multidisciplinary team were reached.
Physiotherapy indicators
Physiotherapists were trained on performing a full physiotherapy assessment, assessing the patients’ physical and functional limitations, in order to tailor the treatment plan.
Functional independence was measured by direct observation, assessing the affected limb function, and relied on a tool adapted from the FIM in order to be culturally adapted and sensitive to changes in trauma patients, as explained in Box 1 and Figure 1. The tool was first implemented in 2011, and underwent several iterations of evaluation and re-implementation since, in dialogue with the national physiotherapy team. However, it has not undergone a formal validation process as yet. In total, 20 items were included in the score, divided into two sub-scores for the upper and lower limb function, respectively; this allows more sensitivity in case only one limb was injured, while the total score allows assessment of the patient as a whole. The full score ranged from 10 to 100, where a low score indicated high dependence, stratified in four categories: high dependence (20 to 39), moderate dependence (40 to 59), mild dependence (60 to 79) and independence (80 to 100). The functional score is shown in Box 2. Both sub-scores were recorded for all patients at the first and last physiotherapy session in IPD and OPD.
Box 1. Adaptations done to the Functional Independence Measure (FIM), to obtain an adapted functional score for Afghan acute trauma patients.
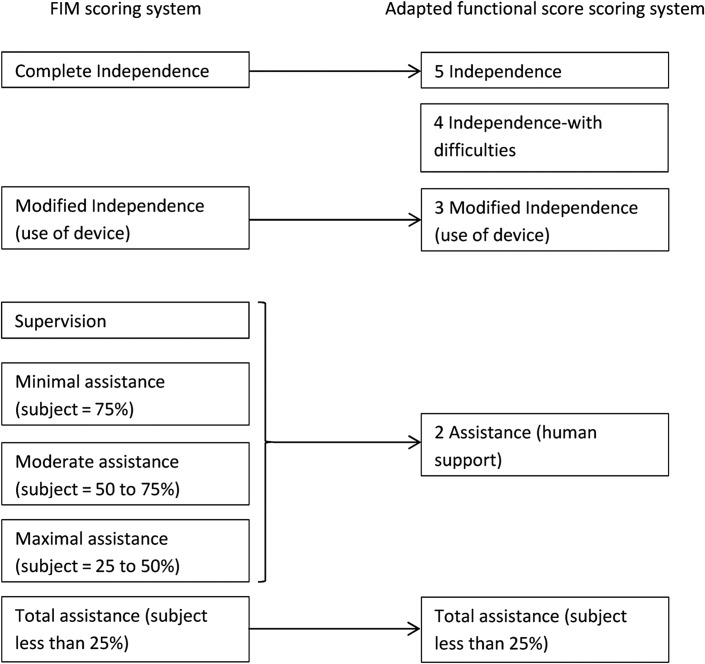
Simplification of scoring system (see Figure 1)
- Addition/adaptation of items:
- Cultural adaptation: addition of activities important to Afghan daily life: squatting (used in social life and self-care) and kneeling (used in social life and praying); and adaptation of items: eating with hands, washing body parts (the Afghans rarely use shower/tub).
- Specificity of upper limb: addition of items to cover full functional range of motion (washing back, carry overhead), to assess fine motor tasks independently of elbow and shoulder (opposition of the fifth finger; grabbing a cup; grabbing a pen) and assess hand strength (opening a jar).
- Specificity of lower limb: addition of items to cover the increased functional range of motion required in Asia/Middle east (i.e., squatting and kneeling); given the acute trauma settings and the context, items were split up to provide more precision (climb up and down stairs, bed mobility items); and one item was added (walking around over 50 meters).
Suppression of items (sphincter control and cognitive items): importance of those items are recognised, but were assessed only when appropriate, and in concertation with other team members.
Figure 1.
Scoring system of the adapted functional score, adapted from the scoring system used in the Functional Independence Measure (FIM).
Box 2. Adapted Functional Independence Measure used with acute trauma patients, in the Médecins sans Frontières Kunduz Trauma Centre.
| Lower limb sub-score | Upper limb sub-score | ||
| Locomotion: | Hygiene: | ||
| Walk around (less than 50 meters) | 1 2 3 4 5 | Wash your back | 1 2 3 4 5 |
| Walk around (over 50 meters) | 1 2 3 4 5 | Dexterity: | |
| Go up stairs | 1 2 3 4 5 | Grab cup of tea | 1 2 3 4 5 |
| Go down stairs | 1 2 3 4 5 | Open a jar | 1 2 3 4 5 |
| Transfers: | Opposition thumb-5th finger | 1 2 3 4 5 | |
| Sit up | 1 2 3 4 5 | Grab pen | 1 2 3 4 5 |
| Stand up | 1 2 3 4 5 | Eating | 1 2 3 4 5 |
| Sit down | 1 2 3 4 5 | Upper limb activities: | |
| Lie down | 1 2 3 4 5 | Carry object overhead | 1 2 3 4 5 |
| Toilet: | Comb hair | 1 2 3 4 5 | |
| Full squat | 1 2 3 4 5 | Put on pants | 1 2 3 4 5 |
| Pray: | Put on shirt | 1 2 3 4 5 | |
| Kneeling (sitting) | 1 2 3 4 5 | ||
| TOTAL Lower limb sub-score | ____/ 50 | TOTAL Upper limb sub-score | ____/ 50 |
Since pain can considerably influence function and recovery,20 which is not reflected in the functional score, we chose to assess pain dynamically, asking the patient to score their pain while performing activities adjusted to their activity level. Pain was assessed using a simplified version of the pain sub-scale of the University of California, Los Angeles (UCLA) shoulder scale, an outcome measure designed initially for shoulder. This functional pain sub-scale was considered to be appropriate for trauma patients, regardless the site of trauma, and it was thus empirically taken in use; however, such use of the sub-scale had not been previously reported. The sub-scale was simplified; the functional pain was graded in six categories according to frequency and intensity of pain in relationship with different degrees of functional activities: no pain (0), occasional and slight pain (1), pain present during heavy activities (2), pain present during light activities (3), pain always present, but bearable (4), and pain always present, unbearable (5).
Study population
This study included all patients admitted to KTC between January and June 2015. Patients were categorised by type/site of trauma: lower limb fracture (LLF; including pelvis fracture), upper limb fracture (ULF; including scapula and clavicular fracture), traumatic brain injury (i.e., patients diagnosed with traumatic brain injury, no matter their Glasgow Coma Scale [GCS] at admission), multiple injury (i.e., patients with either more than one fracture, or those having traumatic brain injury together with at least one fracture) and other trauma (e.g. open wound, sprain, dislocation, internal injury, and contusion). When assessing the evolution of functional recovery of patients, ‘other trauma’ cases were excluded, as the group was considered too heterogeneous. Functional recovery was assessed separately in IPD and OPD, and only in patients with the respective admission and discharge functional scores. We excluded patients with less than 2 days inpatient stay and patients with less than 6 days in the outpatient programme.
Since the data was anonymised and routinely-collected, consent was not required.
Data analysis and statistics
Data was sourced from the existing standardized electronic registers used in the different departments (emergency department, operating department, IPD, intensive care unit, OPD, physiotherapy). The data was compiled from these sources into a designated Excel database (Microsoft Excel spreadsheet software, Microsoft Corp., Redmond, WA, USA). Frequencies and proportions, and where applicable means and SD or medians and IQRs, were generated. Comparison between proportions was performed using the χ2 test; p<0.05 was considered significant. Analysis was performed using EpiData Analysis v.2.2.2. (EpiData Association, Odense, Denmark) and Stata v.12 (StatCorp, College Station, TX, USA).
Results
Socio-demographic and clinical characteristics
A total of 1528 patients were admitted to KTC during the study period, and 1410 (92.3%) received at least one physiotherapy session (Table 1). Among the patients receiving physiotherapy, the majority were male (82.1%; 1158/1410) and 42.6% (601/1410) were children aged <18 years. One thousand and eighty-one patients (76.7%; 1081/1410) were triaged in the emergency department as in need for immediate attention due to the severity of their injuries, using the South African Triage Scale (SATS).21 The main cause of injury was accidental trauma (60.2%; 848/1410). The majority of patients (52.0%; 733/1410) had a single limb fracture, 30.3% (427/1410) had a lower limb fracture, 21.7% (306/1410) an upper limb fracture. Of all, 70.6% (996/1410) underwent at least one surgical intervention.
Table 1.
Socio-demographic and clinical characteristics, and physiotherapy care coverage of patients admitted to Kunduz Trauma Centre, between January and June 2015 (n=1528)
| Variable | Received physiotherapy | No physiotherapy |
|---|---|---|
| n (%) | n (%) | |
| Total | 1410 (92.3) | 118 (7.7) |
| Sex | ||
| Female | 252 (17.9) | 21 (17.8) |
| Male | 1158 (82.1) | 97 (82.2) |
| Age group | ||
| <5 | 110 (7.8) | 9 (7.6) |
| 5–17 | 491 (34.8) | 32 (27.1) |
| 18–45 | 665 (47.2) | 60 (50.9) |
| 46–65 | 122 (8.6) | 13 (11.1) |
| >65 | 22 (1.6) | 4 (3.3) |
| SATS score | ||
| Red | 362 (25.7) | 42 (35.6) |
| Orange | 719 (51) | 52 (44.1) |
| Yellow | 326 (23.1) | 23 (19.5) |
| Green | 3 (0.2) | 1 (0.8) |
| Cause of trauma | ||
| Violent trauma | ||
| Blast | 219 (15.5) | 28 (23.7) |
| Assault | 43 (3) | 10 (8.5) |
| Gun shot | 300 (21.3) | 28 (23.7) |
| Accidental trauma | ||
| Road traffic accident | 374 (26.6) | 19 (16.1) |
| Other accident | 474 (33.6) | 33 (28) |
| Type of injury | ||
| Lower limb fracture | 427 (30.3) | 13 (11) |
| Upper limb fracture | 306 (21.7) | 25 (21.2) |
| Traumatic brain injury | 118 (8.4) | 15 (12.7) |
| Multiple injury | 171 (12.1) | 17 (14.4) |
| Internal injury | 155 (11) | 11 (9.3) |
| Other | 233 (16.5) | 37 (31.4) |
| Total surgical interventions | ||
| 0 | 414 (29.4) | 56 (47.5) |
| 1–2 | 798 (56.6) | 61 (51.7) |
| >2 | 198 (14) | 1 (0.8) |
| Fixation | ||
| No fixation | 1038 (73.6) | 106 (89.8) |
| Only internal fixation | 130 (9.2) | 3 (2.5) |
| Only external fixation | 229 (16.2) | 9 (7.7) |
| Internal and external fixation | 13 (0.9) | 0 (0) |
SATS: South African Triage Scale21
Provision of physiotherapy care
Out of the 1528, most of the patients (49.4%; 755/1528) received physiotherapy in both the IPD and OPD, 38.7% (591/1528) only in the IPD and 4.2% (64/1528) only in the OPD. Patients with accidental trauma (p=0.0006), lower limb fractures (p<0.0001), and multiple surgeries (p<0.0001) were more likely to receive physiotherapy.
A total of 10 500 physiotherapy sessions were provided to the 1410 patients, with a majority in IPD (74.1%; 7781/10 500), followed by OPD (19.1%; 2003/10 500) and intensive care unit (6.8%; 716/10 500). Risk factors for not having any follow-up sessions in OPD included being a more severe case (red or orange triage score; p<0.0001), being aged 18–45 (p=0.02), having a traumatic brain injury or internal injury (p<0.0001), and having suffered violent trauma (p<0.0001). Patients not attending OPD physiotherapy were significantly more independent at IPD discharge than patients attending OPD (median 80 and 73, respectively). More specifically, patients with traumatic brain injury only receiving IPD physiotherapy tended to have higher GCS score and a relatively better IPD discharge functional score (median GCS 12, score 89) than patients with traumatic brain injury receiving both IPD and OPD physiotherapy (median GCS 8, score 78), however no significant difference was observed.
Out of the patients who received physiotherapy, 27.5% (388/1410) had only internal injuries and/or soft tissue injuries, and were excluded from subsequent analyses. Across the four remaining subgroups (1022), 966 patients received IPD physiotherapy, with the majority (61.7%; 596/966) receiving a session within 2 days of admission. Overall, patients received an average of 6.6 IPD/intensive care unit sessions, with a median length of stay of 5 days (IQR 3–10). Six hundred and ninety-six patients received OPD physiotherapy. The delay between the IPD discharge and the first OPD session varied: 31.8% (221/696) arrived in the OPD after one month of discharge while 36.9% (257/696) within two weeks. Patients received on average 2.5 OPD sessions, at a median of one every 3.1 weeks (IQR 1.9–4.9) (Tables 2 and 3).
Table 2.
Characteristics of physiotherapy provision in Inpatient Department, for patients of the four subgroups, admitted to Kunduz Trauma Centre, between January and June 2015 in KTC (n=966)
| LLF | ULF | TBI | MI | Total | |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | |
| Total | 411 (42.6) | 272 (28.2) | 116 (12.0) | 167 (17.3) | 966 |
| Time between admission and first IPD session (days) | |||||
| 0–1 | 253 (61.6) | 164 (60.3) | 66 (56.9) | 113 (67.7) | 596 (61.7) |
| 2–3 | 136 (33.1) | 89 (32.7) | 46 (39.7) | 47 (28.1) | 318 (32.9) |
| ≥4 | 22 (5.4) | 19 (7) | 4 (3.4) | 7 (4.2) | 52 (5.4) |
| Number of IPD physiotherapy sessions | |||||
| 1–4 | 190 (46.2) | 209 (76.8) | 51 (44) | 56 (33.5) | 506 (52.4) |
| 5–9 | 116 (28.2) | 47 (17.3) | 34 (29.3) | 59 (35.3) | 256 (26.5) |
| ≥10 | 105 (25.5) | 16 (5.9) | 31 (26.7) | 52 (31.1) | 204 (21.1) |
| Length of stay IPD (days) | |||||
| ≤7 | 233 (56.7) | 221 (81.3) | 59 (50.9) | 72 (43.1) | 585 (60.6) |
| 8–13 | 117 (28.5) | 29 (10.7) | 31 (26.7) | 49 (29.3) | 226 (23.4) |
| ≥14 | 61 (14.8) | 19 (7) | 26 (22.4) | 44 (26.3) | 150 (15.5) |
| Missing | 0 | 3 (1.1) | 0 | 2 (1.2) | 5 (0.5) |
IPD: Inpatient Department; LLF: Lower limb fracture; MI: multiple injury; TBI: traumatic brain injury; ULF: Upper limb fracture
Table 3.
Characteristics of physiotherapy provision in Outpatient Department, for patients of the four subgroups, admitted to Kunduz Trauma Centre, between January and June 2015 (n=696)
| LLF | ULF | TBI | MI | Total | |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | |
| Total | 309 (44.4) | 225 (32.3) | 43 (6.2) | 119 (17.1) | 696 |
| Time between IPD discharge and first OPD session (days) | |||||
| 0–14 | 127 (41.1) | 51 (22.7) | 34 (79.1) | 45 (37.8) | 257 (36.9) |
| 15–29 | 80 (25.9) | 92 (40.9) | 6 (14) | 36 (30.3) | 214 (30.7) |
| ≥30 | 102 (33) | 79 (35.1) | 3 (7) | 37 (31.1) | 221 (31.8) |
| Missing | 0 | 3 (1.3) | 0 | 1 (0.8) | 4 (0.6) |
| Number of OPD sessions | |||||
| 1–2 | 187 (60.5) | 169 (75.1) | 37 (86) | 73 (61.3) | 466 (67) |
| 3–9 | 117 (37.9) | 51 (22.7) | 5 (11.6) | 43 (36.1) | 216 (31) |
| ≥10 | 5 (1.6) | 5 (2.2) | 1 (2.3) | 3 (2.5) | 14 (2) |
| Length of OPD course (days) | |||||
| ≤14 | 128 (41.4) | 155 (68.9) | 32 (74.4) | 55 (46.2) | 370 (53.2) |
| 15–29 | 39 (12.6) | 24 (10.7) | 4 (9.3) | 10 (8.4) | 77 (11.1) |
| ≥30 | 142 (46) | 46 (20.4) | 7 (16.3) | 54 (45.4) | 249 (35.8) |
IPD: Inpatient Department; LLF: Lower limb fracture; MI: multiple injury; OPD: Outpatient Department; TBI: traumatic brain injury; ULF: Upper limb fracture
Evolution of functional recovery
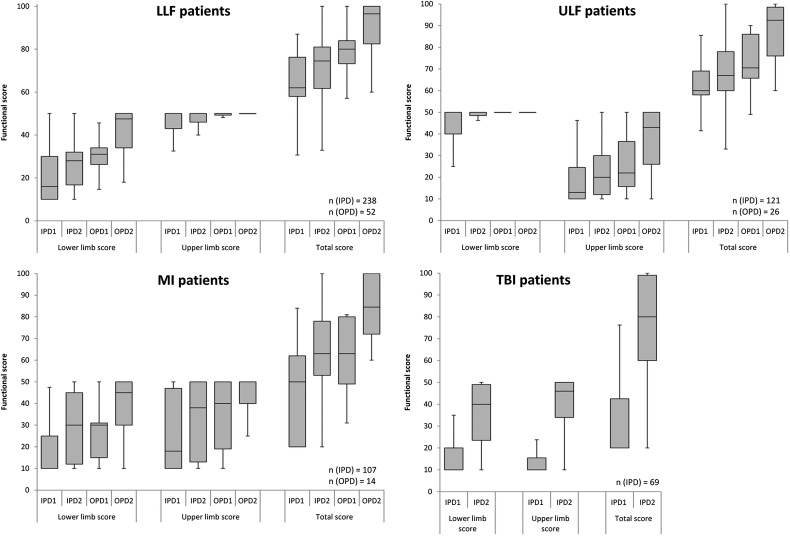
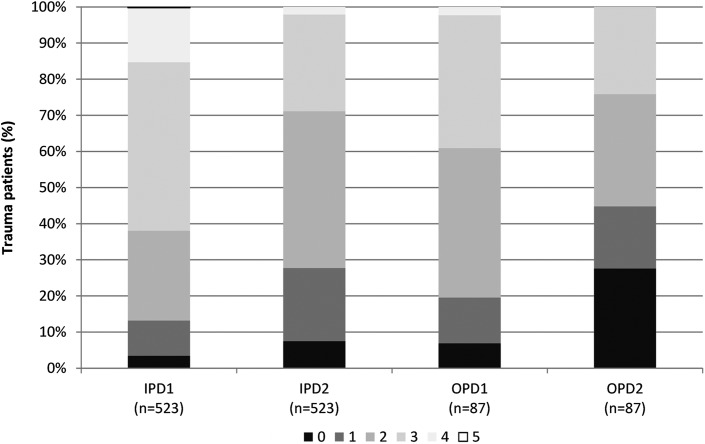
A trend was observed towards functional independence and less pain throughout the course of IPD and OPD treatment (Figures 2 and 3) for each patient type, the increase in functional score of the affected limb was statistically significant. Out of 966 patients who received IPD physiotherapy, 954 (98.8%) had an IPD admission functional score, and 535 patients had a functional score taken at both IPD admission and discharge, as well as an IPD stay of at least two days. At IPD discharge, their mean functional score was 69 (SD 17), 32.1% (172/535) were independent, while 49.9% (267/535) patients remained with a mild dependence and 5.8% (31/535) were highly dependent. Patients with lower limb fracture and upper limb fracture tended to have similar patterns, with the respective sub-score increasing over time, and the other sub-score rapidly reached the maximum. For patients with multiple injuries, both sub-scores and total scores evolved similarly, however those patients tended to be less independent than those with limb fractures, both at IPD admission and discharge. Patients with traumatic brain injury (n = 69) showed a different pattern, with proportionally more patients being independent (52%; 36/69) but also more patients being highly dependent (16%; 11/69) than in the other groups; independence was associated with a higher GCS score in these patients (data not shown). Patients with more than one injury of the same extremity had IPD admission sub-scores significantly lower than patients with only one injury (lower limb sub-score for patients with lower limb fracture[s], 16 and 21 respectively (p=0.001); upper limb sub-score for patients with upper limb fracture[s], 15 and 19 (p=0.04). While the majority of patients (43.4%; 227/523) were discharged from IPD with pain present only during heavy activities, 27.7% (145/523) had either no pain or only occasional and slight pain.
Figure 2.
Functional independence of four subgroups of trauma patients admitted to MSF Kunduz Trauma Centre between January and June 2015, at admission and discharge from IPD and OPD physiotherapy, using the adapted functional score. n is the number of patients with both admission and discharge functional scores. IPD: Inpatient Department; IPD1: admission to IPD physiotherapy; IPD2: discharge from IPD physiotherapy; LLF: lower limb fracture; MI: multiple injury; OPD: Outpatient Department; OPD1: admission to OPD physiotherapy; OPD2: discharge from OPD physiotherapy; TBI: traumatic brain injury; ULF: upper limb fracture.
Figure 3.
Pain score of trauma patients admitted to MSF Kunduz Trauma Centre between January and June 2015, at admission and discharge from IPD and OPD physiotherapy, using adapted functional pain score.
IPD: Inpatient Department; IPD1: admission to IPD physiotherapy; IPD2: discharge from IPD physiotherapy; OPD: Outpatient Department; OPD1: admission to OPD physiotherapy; OPD2: discharge from OPD physiotherapy. Pain score 0: none; 1: occasional and slight; 2: present during heavy activities; 3: present during light activities; 4: present always but bearable; 5: present always, unbearable.
Out of 696 patients who received OPD physiotherapy, 490 (70.4%) had a functional score at OPD admission, with 95 patients having scores taken at both OPD admission and discharge and an OPD course longer than 6 days. Their mean total functional score at OPD discharge was 89 (SD 12), 79% (75/95) were independent, and no patients were highly or moderately dependent. However, patients with multiple injuries tended to be discharged with a lower score than those with upper limb and lower limb fractures. At OPD discharge, most (45%; 39/95) had either no or occasional/slight pain, and no patients experienced pain constantly.
Discussion
To our knowledge, this is the first study focusing on early rehabilitation as well as functional outcomes of various types of acute trauma patients in an active conflict context. This study demonstrates the feasibility and need of the provision of physiotherapy in such setting, and the relevance of the use of the adapted functional score for trauma patients with different types of injury.
The integration of a team of physiotherapists within the MSF KTC allowed the provision of physiotherapy to the great majority of admitted patients (92%), in a context where physiotherapy is still rare within health facilities. In KTC, a multidisciplinary approach was applied throughout the patient treatment course, where physiotherapy service was widely used by the medical team, which confirms its relevance in such settings. To our knowledge, only Christian et al.22 reported on physiotherapy provision for acute trauma patients in LMIC, only 17% of eligible patients received physiotherapy services in a Ghanaian trauma centre. Various barriers already reported in the literature might explain delays observed before the first OPD physiotherapy session and the low proportion of patients receiving OPD care: financial, geographical and security barriers hinder access to health care in Afghanistan.23 Additionally, the lack of awareness or cultural beliefs of both patients and medical staff regarding the important impact of early rehabilitation care after IPD discharge probably further influenced OPD attendance.22 This appears to be even evident in patients with traumatic brain injury, as observed by Zhang et al.24 The heterogeneity of patients with traumatic brain injury, with various levels of severity, might have also played a role, with patients recovering faster from injury already in IPD, and therefore not considered in critical need of OPD treatment. Patients aged 18 and 45 years were less likely to attend OPD, which could be explained by the competing priorities of such group to provide for their families. Based on SATS, more severe patients were less likely to receive OPD care; however, based on their functional score at IPD discharge, patients not attending OPD were those with a better independence, therefore potentially less in need of care. Home visits could have been appropriate to address some of the abovementioned barriers, but were precluded because of security constraints. Some local rehabilitation services were available at community level, but were not always specialised in acute trauma care management. A step-down facility, as defined by WHO as an inpatient facility to provide interim care for medically stable patients to prepare them for discharge into the community,6 would allow provision of transitional multidisciplinary rehabilitation care and would be a great asset to such trauma centres, ensuring proper follow-up of the most severe cases.
The adapted functional score facilitated assessment of functional recovery and addressed the limitations of other validated scales. It is a generic tool, sensitive to changes in all types of trauma patients while maintaining specificity, as observed in patients with one limb fracture. It is shorter than most tools described in the literature, widely used by the team, and therefore, a practical routine tool. Finally, it is culturally relevant, being an observation based tool and encompassing important cultural activities. While not described here, it also helped in goal setting and guidance over the course of treatment, as well as in the discharge process.
Restoring functional independence is one of the main objectives in trauma care. Overall, one must bear in mind that recovery from trauma is a multifaceted process, positive patient evolution cannot be entirely attributed to physiotherapy,25 even though it has been proven to influence the outcomes.26 Based on the adapted tool, most of the patients’ function improved over the course of treatment. However, the scarce literature on functional outcomes of trauma patients in LMICs limits comparison with other various outcome measures, among different populations characteristics (age, gender, types of injuries) and type of rehabilitation care.10,12,24,26-28 Holbrook et al.29 has underlined that a patient can reach functional independence but still have a poor quality of well-being due to other factors, such as pain,13.26 psychosocial distress and low level of social integration.29 In our study, very few patients had constant pain in IPD, which decreased further over the course of OPD care—similar or better than other studies.13,30
The study's strengths include: the study population size was large compared to other studies in LMICs and it included trauma patients with various causes and types of injury, allowing better generalization. Moreover, this study took place in a setting with high quality medical and surgical care provided from the acute stages of trauma to after patient discharge. This study describes the functional recovery of trauma patients in a challenging conflict context; however, all patients received the same level of pre-physiotherapy care, in contrast with other contexts where pre-rehabilitation treatment varies (e.g., in the Syrian crisis,12 and following natural disasters11,24). The functional score used in this study was a routine tool for years, and was thus adapted based on the reality on the ground; for most other studies, scores were only used under more controlled study conditions.
This study has some limitations including missing patient files, which is closely linked to the destruction of the hospital on 3 October 2015, where patient file archives were destroyed. This precluded analysis of the individual 20 items constituting the functional score and the intermediary scores collected between IPD admission and OPD discharge (not routinely encoded electronically). Another limitation was the decrease of population size from IPD to OPD, which hampered conclusions regarding OPD functional recovery. It is partially due to missing files but also to the low OPD attendance, particularly for patients with traumatic brain injury. Moreover, no information on patients’ eligibility for physiotherapy was available, precluding the assessment of rehabilitation needs coverage. Patients were not assessed following a fixed schedule (as done in most of the prospective studies). Lastly, it must be noted that KTC provided a relatively high level of care compared to other settings in LMICs, therefore the present results may not be fully representative of such contexts.
Future studies should include assessment of outcomes at fixed schedules, including longer term outcomes (>1 year), looking at different characteristics influencing these outcomes. Patients’ eligibility for physiotherapy as well as physiotherapy provision should be documented in diverse LMICs settings, in order to assess the rehabilitation needs coverage. Other aspects of recovery such as quality of life, community integration, psychosocial factors and caregiver burden should also be taken into account in future research. The use of the UCLA pain sub-scale for trauma patients should be further documented, in comparison with other pain scores. To allow further development of the adapted functional score and its validation, future studies should include comparisons with validated tools, analysis of the performance of individual components of the tool to refine both the scoring system and its items. In addition, administration characteristics and evaluations across different cultures and contexts should be assessed (i.e., non-conflict LMIC setting or less resourced or specialised health facilities, but also at community level) to ensure its cross-cultural validity and generalisability. Furthermore, the tool needs to be more specifically evaluated among patients with neurological conditions.
Conclusions
Given the feasibility and utilisation of physiotherapy in this context, the integration of physiotherapists within any trauma medical team is a necessity. Raising the awareness of medical teams on the importance of physiotherapy and the criteria for prescribing physiotherapy is essential to ensure a good quality of care, allowing patients’ optimal functional recovery. Due to different barriers experienced by patients to access the OPD, physiotherapists should adjust their treatment goals accordingly, emphasizing education of patients and caregivers on basic rehabilitation. Moreover, a link with community based rehabilitation services is essential and, if appropriate, building up of their capacities to provide specialised physiotherapy to trauma patients is strongly recommended. The use of the adapted functional score was shown to be feasible for complex trauma patients with different types of injury in a humanitarian setting. The relevance of the adapted score requires further evaluation and validation in different settings, including in non-conflict LMIC settings, to tailor it to continual new challenges faced in humanitarian settings.
Acknowledgments
Authors' contributions: MMN, EW, MN and BG developed the adapted functional score; MMN, MN, BG were involved in the routine data collection and ensure its technical quality; MT, CVO, RVdB, EA, SC, PS, PF and BG were involved in the design of the project; RVdB and ES carried out data analyses. EA, RVdB, ES and BG drafted the first manuscript; PF, EW, PS, CVO, MT, SC, MMN, MN critically revised the manuscript. All authors read and approved the final paper. BG is guarantor of the paper
Acknowledgments: The authors would also like to acknowledge and thank the MSF physiotherapy team, for their dedication and quality work throughout the project, when the situation was already challenging. This research was supported through an operational research course, which was jointly developed and run by the Centre for Operational Research, International Union Against Tuberculosis and Lung Disease, and the Operational Research Unit, Médecins sans Frontières, Brussels.
Funding: None.
Competing interests: None declared.
Ethical approval: This study met the Médecins Sans Frontières’ Ethics Review Board-approved criteria for analysis of routinely collected program data. Additionally, it was approved by the Afghanistan National Public Health Institute's Institutional Review Board.
References
- 1.Gosselin R, Spiegel D, Coughlin R, Zirkle L.. Injuries: the neglected burden in developing countries. Bull World Health Organ 2009;87:246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Landry MD, O'Connell C, Tardif G, Burns A.. Post-earthquake Haiti: the critical role for rehabilitation services following a humanitarian crisis. Disabil Rehabil 2010;32:1616–8. [DOI] [PubMed] [Google Scholar]
- 3.May-Teerink T. A survey of rehabilitative services and people coping with physical disabilities in Uganda, East Africa. Int J Rehabil Res 1999;22:311–6. [DOI] [PubMed] [Google Scholar]
- 4.WCPT WCPT Report : The Role of Physical Therapists in Disaster Management. London: World Confederation for Physical Therapy; 2016. http://www.wcpt.org/sites/wcpt.org/files/files/resources/reports/WCPT_DisasterManagementReport_FINAL_March2016.pdf [accessed 1 April 2016].
- 5.Rathore FA, Gosney JE, Reinhardt JD et al. Medical rehabilitation after natural disasters : why, when, and how . Arch Phys Med Rehabil 2012;93:1875–81. [DOI] [PubMed] [Google Scholar]
- 6.WHO Minimum Standards for Rehabilitation-Emergency Medical Teams. Geneva: World Health Organization; Forthcoming. [Google Scholar]
- 7.Giannou C, Baldan M. War Surgery: Working With Limited Resources in Armed Conflict and Other Situations of Violence. Geneva: International Committee of the Red Cross; 2010. https://www.icrc.org/eng/assets/files/other/icrc-002-0973.pdf [accessed 4 December 2013].
- 8.Smith J, Roberts B, Knight A et al. A systematic literature review of the quality of evidence for injury and rehabilitation interventions in humanitarian crises. Int J Public Health 2015;60:865–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khan F, Amatya B, Gosney J et al. Medical rehabilitation in natural disasters: a review. Arch Phys Med Rehabil 2015;96:1709–27. [DOI] [PubMed] [Google Scholar]
- 10.Armstrong JC, Nichols BE, Wilson JM et al. Spinal cord injury in the emergency context: review of program outcomes of a spinal cord injury rehabilitation program in Sri Lanka. Confl Health 2014;8:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Delauche MC, Blackwell N, Le Perff H et al. A prospective study of the outcome of patients with limb trauma following the Haitian earthquake in 2010 at one- and two- year (The SuTra2 Study). PLoS Curr 2013:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Teicher C, Foote NL, Al Ani AMK et al. The short musculoskeletal functional assessment (SMFA) score amongst surgical patients with reconstructive lower limb injuries in war wounded civilians. Injury 2014;45:1996–2001. [DOI] [PubMed] [Google Scholar]
- 13.Holtslag HR, van Beeck EF, Lindeman E, Leenen LPH.. Determinants of long-term functional consequences after major trauma. J Trauma 2007;62:919–27. [DOI] [PubMed] [Google Scholar]
- 14.Ardolino A, Sleat G, Willett K.. Outcome measurements in major trauma - results of a consensus meeting. Injury 2012;43:1662–6. [DOI] [PubMed] [Google Scholar]
- 15.Cohen ME, Marino RJ.. The tools of disability outcomes research functional status measures. Arch Phys Med Rehabil 2000;81:S21–9. [DOI] [PubMed] [Google Scholar]
- 16.Balogh ZJ, Reumann MK, Gruen RL et al. Advances and future directions for management of trauma patients with musculoskeletal injuries. Lancet 2012;380:1109–19. [DOI] [PubMed] [Google Scholar]
- 17.McNair PJ, Prapavessis H, Collier J et al. The Lower-Limb Tasks Questionnaire: an assessment of validity, reliability, responsiveness, and minimal important differences. Arch Phys Med Rehabil 2007;88:993–1001. [DOI] [PubMed] [Google Scholar]
- 18.Reinhardt JD, Li J, Gosney J et al. Disability and health-related rehabilitation in international disaster relief. Glob Health Action 2011;4:7191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wickford J. Physiotherapists in Afghanistan. Exploring, Encouraging and Experiencing Professional Development in the Afghan Development Context. [PhD thesis] Gothenburg: University of Gothenburg; 2010. https://gupea.ub.gu.se/handle/2077/22922 [accessed 8 November 2015].
- 20.McDonald W, Bell E.. Acute Pain Management, Measurement Toolkit. Victoria, Australia: Victorian Quality Council; 2007. [Google Scholar]
- 21.Twomey M, Wallis LA, Thompson M, Myers JE.. The South African Triage Scale (adult version) provides reliable acuity ratings. Int Emerg Nurs 2012;20:142–50. [DOI] [PubMed] [Google Scholar]
- 22.Christian A, Gonzalez-Fernandez M, Mayer RS, Haig AJ.. Rehabilitation needs of persons discharged from an African trauma center. Pan Afr Med J 2011;10. [PMC free article] [PubMed] [Google Scholar]
- 23.Nic N, De Gryse B, Sattar A et al. Patients struggle to access effective health care due to ongoing violence, distance, costs and health service performance in Afghanistan. Int Health 2015;7:169–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang X, Reinhardt JD, Gosney JE, Li J.. The NHV Rehabilitation Services Program improves long-term physical functioning in survivors of the 2008 Sichuan earthquake: a longitudinal quasi experiment. PLoS One 2013;8:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goldberg CKF, Green B, Moore J et al. Integrated musculoskeletal rehabilitation care at a comprehensive combat and complex casualty care program. J Manipulative Physiol Ther 2009;32:781–91. [DOI] [PubMed] [Google Scholar]
- 26.Zhang X, Hu XR, Reinhardt JD et al. Functional outcomes and health-related quality of life in fracture victims 27 months after the Sichuan earthquake. J Rehabil Med 2012;44:206–9. [DOI] [PubMed] [Google Scholar]
- 27.Jandric S. Injury severity and functional outcome following paediatric trauma in war conditions. Pediatr Rehabil 2001;4:169–75. [DOI] [PubMed] [Google Scholar]
- 28.Schneider M. War wounded and victims of traffic accidents in a surgical hospital in africa: an observation on injuries. Prehosp Disaster Med 2015;30:618–20. [DOI] [PubMed] [Google Scholar]
- 29.Holbrook TL, Anderson JP, Sieber WJ et al. Outcome after major trauma: 12-month and 18-month follow-up results from the trauma recovery project. J Trauma-Injury Infect Crit Care 1999;46:765–73. [DOI] [PubMed] [Google Scholar]
- 30.Ponsford J, Hill B, Karamitsios M, Bahar-Fuchs A.. Factors influencing outcome after orthopedic trauma. J Trauma 2008;64:1001–9. [DOI] [PubMed] [Google Scholar]