Abstract
Study Objectives:
In this study, we investigated the prevalence of symptoms of restless legs syndrome (RLS) in biological caregivers of children with a diagnosis of autism spectrum disorder (ASD).The relationship of RLS symptoms to caregiver health-related quality of life (HRQoL) was also examined. Finally, we compared the sleep quality and daytime behaviors of children with ASD in caregivers with and without symptoms of RLS.
Methods:
Biological caregivers (n = 50) of children ages 6 to 11 y with a diagnosis of ASD completed a Sleep Habits Questionnaire (SHQ) that included RLS as determined by four questions. HRQoL was assessed using the Medical Outcomes Survey (MOS) 12-Item Short Form (SF-12). Caregivers also completed the Children's Sleep Habits Questionnaire (CSHQ) and Child Behavior Checklist (CBCL6/18).
Results:
Eleven caregivers (22%) fit the criteria for RLS symptomatology and caregivers with RLS reported poorer mental health. Caregivers with RLS described more night waking and greater internalized behavior problems in their children with ASD than the caregivers without RLS.
Conclusions:
Biological caregivers of children with ASD demonstrated a high prevalence of RLS symptoms and poorer mental health. RLS is known as a sleep disorder that has strong heritability, and it is possible that many of the children with ASD also have symptoms of RLS. RLS as a possible disruptor of sleep should be considered in caregivers and in their children with ASD.
Citation:
Russell M, Baldwin CM, McClain D, Matthews N, Smith C, Quan SF. Symptoms of restless legs syndrome in biological caregivers of children with autism spectrum disorders. J Clin Sleep Med. 2017;13(1):105–113.
Keywords: autism spectrum disorder, caregivers, health-related quality of life, restless legs syndrome
INTRODUCTION
Autism spectrum disorder (ASD) is a complex developmental disorder that has an estimated prevalence of 1 in 68 children in the United States.1 ASD is characterized by challenges in many areas of early development such as communication, socialization, learning, and adaptive behavior.1 Parents of children with ASD often report lower health-related quality of life (HRQoL) than the general population in the United States2 and lower HRQoL than the parents or caregivers of typically developing children.3 A possible contributor to poor HRQoL in caregivers of children with ASD may be their own sleep needs, as well as any persistent sleep problems of their children.2 Sleep disturbances in children with ASD are reported by their parents at a prevalence of 50% to 80%.4,5 It appears that there is a bidirectional relationship between sleep and severity of ASD symptoms in children with ASD, as children with more sleep problems tend to have more aberrant daytime behaviors. In turn, children with behavioral problems may have more difficulty settling for sleep and maintaining sleep throughout the night.6 Greater sleep problems in children with ASD are also associated with greater sleep problems in their parents.7 It is suggested that parents of children with autism may tend to be hypervigilant at night due to the possibility of unsafe activity by their children with ASD that may result in nighttime behaviors such as self-injury, property damage, or escape from their homes.8
BRIEF SUMMARY
Current Knowledge/Study Rationale: Restless legs syndrome is a sleep disorder known to have strong heritability and is often associated with other health conditions. RLS may be under-diagnosed in the biological caregivers of children with ASD, and RLS may contribute to poorer sleep quality in these caregivers.
Study Impact: This study suggests that biological caregivers of children with ASD may be at risk for RLS and poorer mental health. Education of caregivers concerning sleep hygiene and possible sleep disruptors in their own sleep and in the sleep of their children with ASD is vital.
One sleep disorder that can affect sleep quality is restless legs syndrome (RLS), also known as Willis-Ekbom disease. RLS is a neurological sensorimotor disorder with a prevalence in the general population of European and American adults of 7%.9 Persons with RLS self-report sleep disturbances that include reduced sleep,10 disrupted sleep onset and/or sleep maintenance, and excessive daytime sleepiness.9 Polysomnographic studies support the existence of sleep disturbances in individuals with RLS and indicate longer adjusted mean sleep latency, shorter total sleep time, lower sleep efficiency, higher number of stage shifts, longer rapid eye movement sleep latency, and a high arousal index.11,12 In addition to sleep disturbances, RLS can have a profound effect on HRQoL with both physical and mental HRQoL significantly decreased in studies of adults with the disorder.9,12
Many adults with RLS report the onset of their symptoms of RLS as children,13 and the criterion for diagnosis of RLS in children recognizes the strong hereditary link in this disorder. One study indicated that 71% of the children having RLS symptoms had at least one biological parent with RLS.14 As in the adult population, in samples of children and adolescents, RLS symptoms were associated with sleep disturbances including sleep onset or sleep maintenance insomnia.14
To our knowledge, there are no extant studies that have investigated the presence of RLS in biological caregivers of children with ASD or the relationships of these symptoms to caregiver HRQoL. In addition, associations between caregivers with RLS symptoms and child sleep or child behavior have not been sufficiently investigated in this population. Thus, the aim of this study was to explore the presence of RLS symptoms in the biological caregivers of children with a diagnosis of ASD and the relationship of the RLS symptoms to care-giver HRQoL. Additionally, we compared the sleep problems and aberrant behaviors of the children with ASD who had biological caregivers with RLS symptoms compared to biological caregivers who did not have RLS symptoms.
METHODS
Participants
The sample consisted of family caregivers of children with ASD who were participants in Southwest Autism Research and Resource Center (SARRC) clinical or research programs in Phoenix, AZ. SARRC promotes best practices and early intervention for individuals with autism through integrative research, educational outreach, model programs, and collaborative initiatives.15 Participants were the primary family care-givers for a child between ages 6 and 11 y with a diagnosis of ASD confirmed by the prior administration of the Autism Diagnostic Observation Schedule16 or the Autism Diagnostic Observation Schedule, 2nd edition17 by research reliable raters at SARRC. Prospective participants were excluded from this study if the child with ASD had another primary diagnosis such as cerebral palsy or Down syndrome. Participants were also excluded if they lived outside of the United States or if they did not read and write in English.
Family caregivers who met the inclusion criteria were invited to participate in the study investigating the relationship of sleep in caregivers of children with ASD to quality of life. Of the 159 eligible families who were contacted and invited to participate, 86 agreed to participate. They were given the option of completing a questionnaire packet either through a secure online link or by mail. A total of 64 surveys were returned, with two of the surveys eliminated due to large amounts of incomplete information. A total of 62 caregivers of children with ASD between the ages of 6 and 11 y completed all questionnaires used in this study, resulting in a 39% overall response rate. Caregivers who responded to this survey (participants) did not differ significantly from caregivers who did not respond or did not complete this survey (nonparticipants) regarding the sex of their child with ASD or their reported race/ethnicity. Additionally, based on mailing ZIP codes there was a similar distribution of families living in Arizona compared to families living in another state, with 94% of the participants and 99% of the nonparticipants living in Arizona. The ZIP codes of all potential participants were coded as “high, middle, or low income” based on the reported median household income of the ZIP code as described by the US Census Bureau.18,19 There were no significant differences between the income levels as determined by ZIP codes of participants and the ZIP codes of nonparticipants. The ages of the children with ASD were significantly different between groups, and participants tended to have younger children (median = 7.5) while nonparticipants tended to have older children (median = 9.0), Mann-Whitney U (test of significant differences between medians) = 1,638.50, p = 0.001.
Of the 62 participants, 50 caregivers (81%) were selected for further examination of variables related to symptoms of RLS. Three of the 12 caregivers who were eliminated from the RLS subgroup analysis were not biological parents of the child with ASD. Because other medical or behavioral conditions can mimic symptoms of RLS and in order to improve specificity in the diagnosis of RLS, it has been recommended by the International Restless Legs Syndrome Study Group that certain conditions be considered in the differential diagnosis.20 As a result, an additional nine participants who indicated that they had arthritis, anxiety, or peripheral neuropathy on a health history questionnaire were excluded from this analysis. Three of the nine participants who met the other criteria for RLS were eliminated, one who reported arthritis and two who reported anxiety. Data were collected from March to August 2014. Human subjects consent was obtained through the Arizona State University Human Subjects Institutional Review Board prior to the implementation of the study.
Measures
Demographic questionnaire and health history
Information was requested concerning the age and the sex of the primary caregiver and the age and sex of the child with ASD. A brief health history of the caregiver was obtained by asking the caregivers if a healthcare provider had ever told the participant that he or she had any of the 10 most common health problems. This stem sentence was stated in this manner to elicit provider-diagnosed versus self-reported health issues. The participant was also asked to write in any additional health problems that were not listed. Demographic information was requested concerning family income, race/ethnicity, and marital and education status of the primary caregiver.
Sleep Habits Questionnaire
This survey study examined sleep disorder symptoms and sleep disruptors in caregivers of children with ASD using the Sleep Habits Questionnaire (SHQ), developed for use in the Sleep Heart Health Study.21 This questionnaire is intended to be used with individuals with unidentified sleep disorders, and addresses sleep duration and seven aspects of sleep disorders including symptoms of RLS. The questionnaire has been validated in English and Spanish, and it is used in a variety of investigations as an appropriate means of characterizing sleep health. In a bilingual (English/Spanish) translation and validation of the SHQ, Cronbach α was ≥ 0.70 for sleep duration, snoring/apnea, insomnia and sleep symptoms, sleep disruptors, and RLS items for both language measures. Additionally, 68% of the variance on the English version was accounted for by four factors: (1) sleep duration, (2) snoring and apnea, (3) sleep symptoms, and (4) RLS.22
Caregivers were asked about their average sleep duration during the weekday and on the weekends. The 7-day average sleep duration of the caregivers was calculated by multiplying the average weekday sleep hours by 5 and the average weekend sleep hours by 2. The total sleep duration for the week was divided by 7 to establish the average sleep duration per night.
Symptoms of RLS were identified from responses to a series of questions on the SHQ and reflect the diagnostic criteria recommended by the International Restless Legs Syndrome Study Group.20 Three questions required a “yes” or “no” response and included the following: “In the past year, while sitting or lying down, have you had the urge to move your legs?”; “Are the symptoms worse when you are sitting or lying down than when you are moving around or walking?”; “Do the symptoms improve if you get up and start walking?” A “yes” response was required for all three of these questions to identify symptoms of RLS. Additionally, a multiple choice question asked participants “What time of day do these symptoms generally occur?” The time of day of the symptoms was reported as one of the following: “I don't have these symptoms”, “daytime only (before 18:00),” “bedtime only,” evening or nighttime only (after 18:00),” and “both day and night.” Participants who responded “yes” to the three preceding questions and reported symptoms which occurred either at “bedtime only,” evening or nighttime,” or “both day and night” were considered to meet the criteria for RLS symptoms. Additionally, participants were asked to give a “yes” or “no” response to the two following questions: “ Has anyone in your family had these unpleasant or uncomfortable feelings in their legs (e.g., grandparents, mother, father, brothers, sisters, nieces/nephews, cousins)?”; “Has a doctor or healthcare provider ever told you that you have Restless Legs Syndrome?”
Short Form-12
The Medical Outcomes Study 12-Item Short Form (SF-12) is a multipurpose short-form generic measure of health status that was developed to be a much shorter, yet valid, alternative to the Short Form-36 for use in large surveys of general and specific populations as well as large longitudinal studies of health outcomes.23,24 All SF-12 items were derived from the Short Form-36. Physical and mental regression weights and a constant for both measures come from the general US population. Both the Physical Composite Scale and Mental Composite Scale are transformed to have a mean of 50 and a standard deviation of 10 in the general US population, with higher scores indicating better physical and mental health.25
Children's Sleep Habits Questionnaire
Information concerning the sleep habits and sleep disruptors of the child with ASD, as reported by the caregiver participant, was described using the Children's Sleep Habits Questionnaire (CSHQ),26 a commonly used measure for identifying sleep problems in children with ASD.4 The Autism Treatment Network Sleep Committee, which consists of pediatric sleep medicine specialists, developmental pediatricians, neurologists, and psychiatrists, recommends the CSHQ to screen for insomnia and other sleep disorders in children with ASD.27 This screening instrument consists of 33 questions used to derive the total sleep disturbance score that includes the following subscales: bedtime resistance, sleep onset delay, sleep duration, sleep anxiety, night waking, parasomnias, sleep disordered breathing, and daytime sleepiness. Items are rated on a three-point scale (1 = Rarely or zero to one times a week, 2 = Sometimes or two to four times a week, and 3 = Usually or five to seven times a week), based on parent's recall of sleep behaviors occurring over a typical week. Higher scores indicate more sleep problems, and the standard cutoff score for the presence of sleep problems is a total sleep disturbance score of 41.26 Although the CSHQ was standardized on children ages 4 to 10 y, subsequent research found that this instrument is appropriate for screening for sleep problems in children with ASD ages 11 to 18 y.4
Child Behavior Checklist
The Child Behavior Checklist (CBCL6/18)28 is a norm-referenced parent report measure used to measure daytime behavior in children ages 6 to 18 y. The CBCL6/18 consists of eight syndrome scales that contribute to broad internalizing or externalizing problem domains and indicates overall patterns of aberrant behavior. The syndrome scales include: anxious/ depressed, somatic complaints, withdrawn, attention problems, aggressive behavior, social problems, thought problems, and rule breaking behavior. Parents rate their child's behavior during the previous 2 mo on a scale of 0 (not true) to 2 (very true or often true) with higher scores indicating more aberrant behaviors. Test-retest reliability, interparent reliability, and internal reliability are good to excellent. The CBCL correlates with other measures of child behavior problems.28
Statistical Analysis
All data were analyzed using SPSS version 22 (SPSS Inc., Chicago, IL). Descriptive statistics were computed for all variables. Means and standard deviations (SD) were calculated for continuous normally distributed variables and medians and interquartile range were calculated for continuous non-normally distributed variables. Percentages were reported for categorical variables. Dichotomized variables were created from RLS data collected from the SHQ. The t-test and the Mann-Whitney U test were used to test for significant differences between groups for parametric and nonparametric data, respectively. For the non-normally distributed variables, the effect size (r) was calculated when there was a significant difference between groups. In the analysis of categorical variables, the Pearson chi-square test or the Fisher exact test were used due to small numbers in some of the cells. The level of statistical significance was established at 0.05 and unadjusted for multiple comparisons due to the exploratory nature of this cross-sectional study.
RESULTS
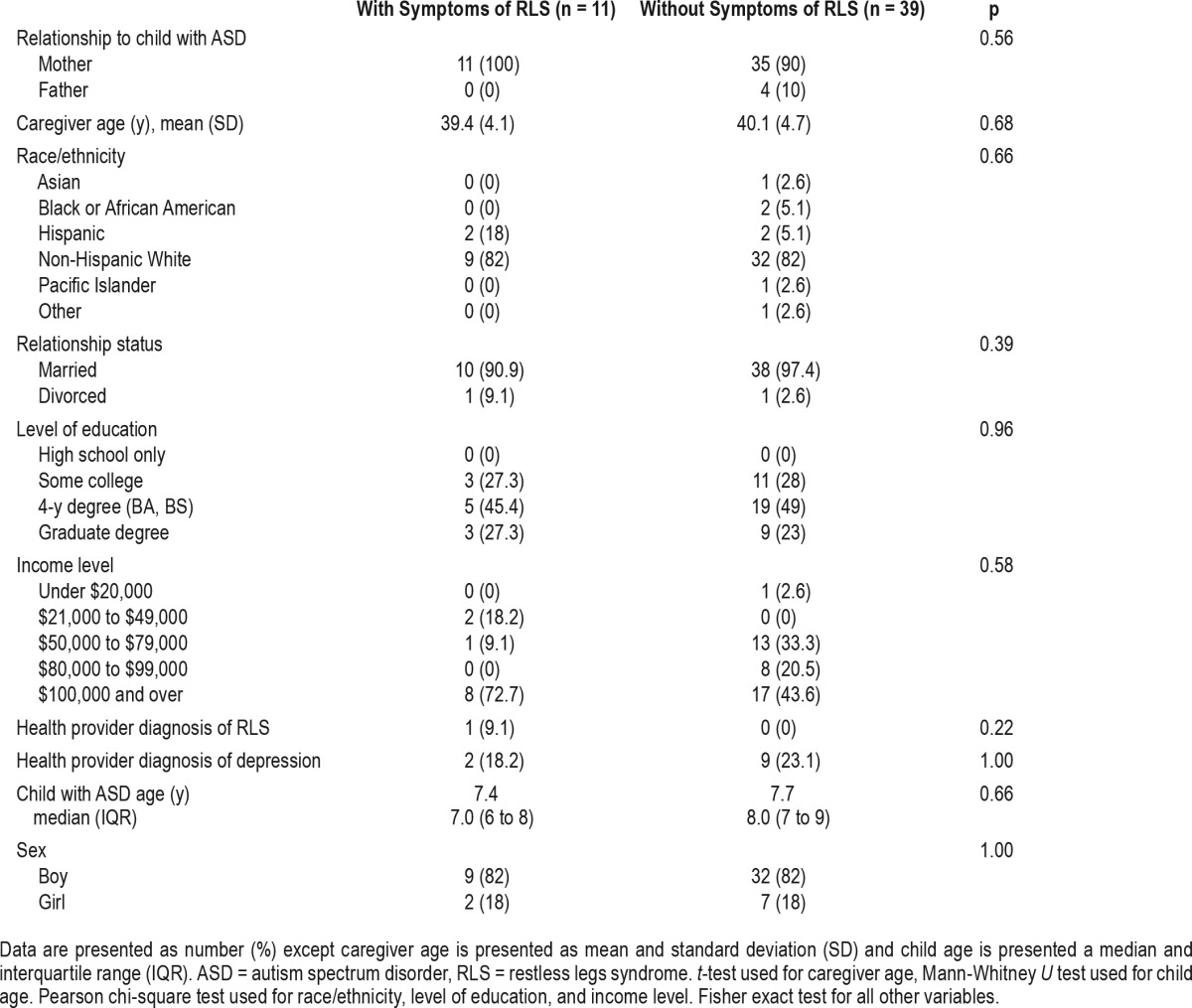
Descriptive characteristics of the study sample of caregivers and their children with ASD are presented in Table 1. Of the 50 participants, 11 (22%) indicated that they had RLS symptoms by their responses to the four key questions on the SHQ. The caregivers who reported symptoms of RLS were not significantly different in sex, age, ethnicity, education, or income, nor did their children with ASD differ in sex or age from the care-givers who did not report symptoms of RLS. Of the 11 participants who reported RLS, 4 of the participants, or 36%, stated that they had a relative with RLS symptoms. Only 1 of the 11 participants who indicated having symptoms of RLS reported a diagnosis of RLS from a healthcare provider. Four of the 11 participants indicated that their symptoms were present both “day and night”, which may indicate severe RLS or another condition that mimics RLS. One of these four participants indicated that she has a close relative with RLS. One of the four participants reported than she has had these symptoms since childhood and the remaining three participants report the presence of these symptoms for the past 1 to 5 y. A sensitivity analysis was completed that excluded only adoptive parents and included all 59 of the biological caregivers regardless of reported medical conditions. This analysis yielded results that were similar to the results with the nine caregivers excluded for medical conditions. Significant differences were found in the same variables between participants who reported RLS symptoms and those who did not report symptoms.
Table 1.
Demographics of caregivers and their children with autism spectrum disorder.
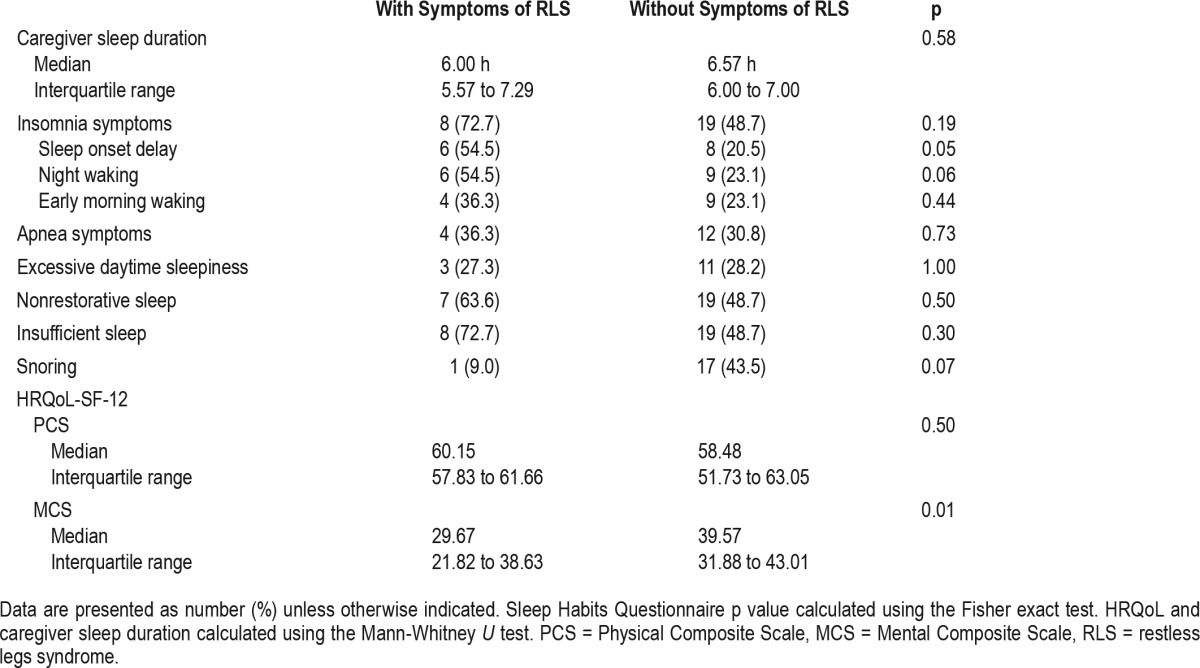
Caregiver's sleep duration, other sleep disorder symptoms, and HRQoL scores are characterized in Table 2. There were no significant differences between caregivers with RLS symptoms and caregivers without RLS symptoms in sleep duration and most sleep disorder symptoms. However, caregivers with RLS symptoms reported more sleep onset delay than caregivers without RLS symptoms. Although physical HRQoL was high and equivalent for both groups, mental HRQoL was poorer for caregivers with RLS symptoms (median = 29.67) than for caregivers without RLS symptoms (median = 39.58), U = 108.50, p = 0.01, r = 0.35.
Table 2.
Caregiver sleep disorder symptoms, sleep duration, and health-related quality of life.
The CSHQ is summarized in Table 3. There were significant differences in one subscale, which indicated more nightwaking for the children with ASD whose biological caregivers reported RLS symptoms (median = 6.0) compared to children of caregivers without RLS symptoms (median = 4.0), U = 133.50, p = 0.05, r = 0.28. There were no significant differences be -tween the children of the caregivers with RLS and caregivers without RLS in any of the other subscales or in the total score of the CSHQ. A total sleep disturbance score of 41 on the CSHQ indicated child sleep problems. In this sample, 82% of the children with caregivers who reported RLS symptoms scored above the cutoff of score 41 (median = 48.00) on the CSHQ compared to 69% of the children of caregivers without RLS (median = 45.00). The difference between these two groups was not significant. The CSHQ contains only one question regarding restless sleep in children; “Child is restless and moves a lot during sleep.” Seventy-three percent of the care-givers with RLS symptoms reported their children had restless sleep “sometimes” (two to four times a week) or “usually” (five to seven times a week). However, this finding did not achieve a level of significance.
Table 3.
Sleep and behavior scales for children with autism spectrum disorder.
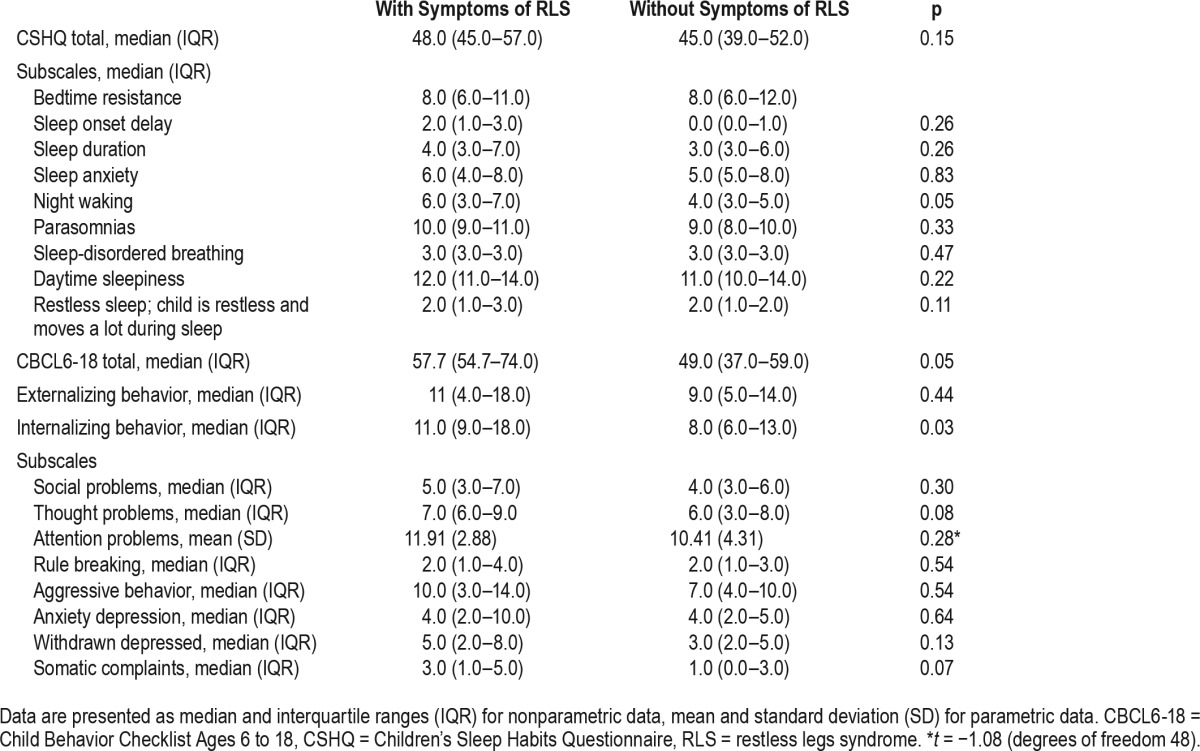
Table 3 also summarizes the behavior scores of the children with ASD on the CBCL6/18. Children of caregivers with RLS symptoms scored higher on the Internalizing Behavior Scale (median = 11.00) than children of caregivers without RLS (median = 8.00), U = 121.50, p = 0.03, r = 0.31, demonstrating more behaviors such as anxiety, depression, and somatic complaints. Higher total scores on the CBCL6/18 or more aberrant behaviors in their children with ASD were reported by care-givers with RLS symptoms (median = 57.75) compared to care-givers without RLS symptoms (median = 49.00), U = 130.00, p = 0.05, r = 0.28.
DISCUSSION
This exploratory study reported the prevalence of RLS symptoms among biological caregivers of children aged 6 to 11 y with a diagnosis of ASD. An unexpected finding in this study was the relatively high percentage of biological caregivers who reported symptoms of RLS. The reported 22% of caregivers with RLS symptoms is much higher than the 7% prevalence from an epidemiology study of the general population in the United States and Europe.9
There were no differences for physical HRQoL for both groups. Notably, their scores were slightly higher than the US norms for adults aged 35 to 44 y.29 Our results are unlike a previous study of parents aged 35 to 44 y who had children with ASD. That study found lower physical HRQoL using the SF-12 version 2 among the parents of children with ASD compared to US population norms.2 Our results also differed from studies that found that the physical HRQoL of persons with RLS was poorer than the general US population norms.30 The better physical health of our sample may reflect the higher income bracket as many of the participants reported an annual family income of over $100,000. In comparison, only 10.5% of the participants in the study of the HRQoL of parents of children with ASD stated that their income was greater than $100,000 per year.2 Although no information was provided about access to health care in our study, it is well established that in the United States, individuals with higher incomes generally have better health care access and report better physical health.31 In our study, participants reported poorer mental HRQoL below the norms for the US general population,29 and consistent with other studies of caregivers of children with ASD.2 Furthermore, the mental HRQoL for caregivers with RLS symptoms was significantly lower than the biological caregivers without RLS symptoms. This is similar to other research findings that associated RLS in adults with poorer mental HRQoL.9,12
RLS is known as a sleep disorder that has strong heritability.14 Symptoms of RLS in parents may signal risk of possible RLS in the children of these parents, an often undetected condition that can affect sleep quality. This study also provided preliminary information concerning relationships between caregivers with and without RLS symptoms and their children's sleep. Caregivers with RLS symptoms were more likely to report that their children with ASD had more nightwaking. It is possible that many of these children may have RLS symptoms but lack the verbal ability to describe their symptoms. RLS may contribute to a poor sleep quality and to more frequent night-waking.14 Unfortunately, the CSHQ contains only one item that addressed restless sleep in children; therefore, this measure may not have provided caregivers adequate opportunity to report symptoms that may relate to RLS. Caregivers of children with ASD may also perceive restless behaviors prior to and during sleep as a symptom of ASD rather than as a symptom of a discrete sleep disorder. This did not achieve statistical significance, perhaps due to the small sample size, and it suggests a need to further explore restless sleep in this population.
Research has indicated a higher prevalence of RLS in children with other health conditions, including attention deficit hyperactivity disorder (ADHD). A literature review examined associations between RLS and ADHD and found that up to 44% of study participants with ADHD also reported RLS. Additional studies found that up to 26% of participants with RLS had ADHD or ADHD symptoms.32 ADHD was found to be the second most common comorbid disorder in individuals with a diagnosis of ASD.33 Although there has been no research on the prevalence of RLS in children with ASD, one study found the prevalence of periodic limb movement disorder, a condition often associated with RLS, to be 47% in children with ASD compared to 8% in typically developing control patients.34 The pathogenesis of RLS, ASD, and ADHD are uncertain, although the dopamine-opiate system and iron as a cofactor have been implicated in each of these disorders.32,34–36 Given these linkages, it is suggested that future bench and clinical research examine further these relationships that could expand our knowledge of the complex relationships between these disorders and lead to interventions to ameliorate symptoms and improve child and family quality of life.
In this study, the children of caregivers with RLS symptoms were more likely to exhibit more withdrawal, depression, anxiety, and somatic complaints than the children of caregivers without RLS symptoms. Notably there was no significant relationship between RLS symptoms and a health provider diagnosis of depression in the caregivers. Prior research has reported relationships between RLS and some features of depression in adults10,37 and associations in children and adolescents between RLS and negative mood, and RLS and comorbid depression or anxiety disorders.14 Although a causal mechanism for the relationship between RLS and depression has not been established in either direction,37 there may be several factors that link depression and RLS. As with RLS, dopamine neurotransmission has been linked to depression. Altered dopaminergic function may underlie depression and persistent exacerbations of the symptoms of depression may promote further dopamine dysregulation.38 Other factors that may influence the relationship between depression and RLS may be higher scores on somatic items of depression scales related to sleep disturbances and loss of energy10 or possible aggravation of RLS through the use of antidepressants.39 Further research is needed to understand the associations and mechanisms that link depression and RLS in adults and children. An additional concern in a population of caregivers of children with ASD is their susceptibility to depression and psychological distress in comparison with caregivers of typically developing children40 and children with other disabilities.41 Optimal care for children with ASD depends on the good physical and psychological health of their caregivers. Attention to caregiver mental health needs within the intervention process is important to achieve positive outcomes for the child with ASD and the family unit.42
As with any study, there are limitations to this research. First, this study consisted of a small convenience sample of parents of children with ASD, and these results cannot be generalized to other caregivers of children with ASD. The demographics of our sample do not closely reflect families who have children with ASD in the United States or in Arizona. The majority or 82% of our participants identified as being non-Hispanic White compared to 48% of families in Arizona and 53% of families of children with ASD in the United States.43 Nevertheless, this study mirrors other published research with children with ASD in which minorities have been underrepresented.44
Second, our low response rate may reflect some self-selection of caregivers who have sleep problems. However, income level estimate, sex of the child, and ethnicity did not differ between participants and nonparticipants, mitigating potential bias. Nonetheless, our participants generally had younger children with ASD compared to our nonparticipants and younger children with ASD are reported to have more sleep problems such as night waking that disrupt parent sleep,4 thus potentially influencing our findings.
Third, the cross-sectional nature of this study is a limitation as it captured the caregiver's perceptions at only one point in time. Fourth, this study relied on the self-report by caregivers of their own sleep disturbances as well as the sleep quality and behavior problems of their children with ASD. In particular, the ascertainment of RLS symptoms was based on questionnaire responses, and this may have resulted in some diagnostic imprecision. It is possible that the three participants who were excluded because of RLS mimics of anxiety and arthritis also had RLS. It was also impossible to determine if the participants who reported RLS symptoms “both day and night” had severe RLS or had another condition that mimics RLS. Fifth, parent reports of child sleep disturbances have not always been supported in studies by objective information.45 Therefore, actigraphy and polysomnography would corroborate information obtained by parent report concerning child sleep disturbances. Finally, because of the descriptive nature of this study, no causality can be inferred. If adjustments were made for multiple comparisons, some results would not achieve significance at the 0.05 level. The small sample size lacked power, and the effects of significant variables were all small to medium (0.28 to 0.35).
Despite these limitations, there are several major strengths of this study, including a confirmed diagnosis of ASD through an Autism Diagnostic Observation Schedule or Autism Diagnostic Observation Schedule 2 that have strong sensitivity and specificity for diagnoses.46 The poorer mental health of the caregivers with RLS even compared to their non-RLS cohorts makes a new contribution to the growing body of evidence regarding RLS and HRQoL literature. Importantly, to our knowledge, this is the first study of its kind to examine caregivers with and without RLS and the sleep and behavior of their children with ASD. Taken together, these findings can provide a springboard for future research of families of children with ASD.
In conclusion, the current study found a high prevalence of self-reported symptoms of RLS in biological caregivers of children with ASD. Associations between RLS symptoms and poorer mental health were found in this sample of care-givers. Additionally, parents with symptoms of RLS reported more nightwaking and greater internalized behavior problems in their children with ASD than parents without symptoms of RLS. This study underscores the importance of compiling information concerning caregiver sleep problems and HRQoL that may guide interventions to support caregivers in fulfilling their daily responsibilities to their children. Additionally, biological caregivers may offer insights into the sleep disruptions that may be common to them and to their children with ASD who may be unable to articulate their symptoms. Sleep problems in children with ASD and their caregivers may be linked by common genetic and environmental influences. Education of caregivers concerning sleep hygiene and possible sleep disruptors in their own sleep and in the sleep of their children with ASD is essential.
DISCLOSURE STATEMENT
This paper was presented, in part, at the Associated Professional Sleep Societies 29th Annual Meeting, Seattle, WA, June 2015. This was not an industry supported study. Dr. Russell is a stockholder in and consultant for Northland Rural Therapy Associates. Dr. Quan is a consultant for Global Corporate Challenge; a stockholder in Merck and Pfizer; and has received honorarium from Harvard Health Publications. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank the families from Southwest Autism Research and Resource Center for their participation in this study.
ABBREVIATIONS
- ADOS
autism diagnostic observation schedule
- ASD
autism spectrum disorder
- ADHD
attention deficit hyperactivity disorder
- CBCL6/18
child behavior checklist (ages 6–18)
- CSHQ
children's sleep habits questionnaire
- HRQoL
health related quality of life
- IQR
interquartile range
- MCS
mental composite scale
- mo
month(s)
- MOS
medical outcomes study
- PCS
physical composite scale
- r
effect size
- RLS
restless legs syndrome
- SARRC
southwest autism research and resource center
- SD
standard deviation
- SF-12
short form-12
- SHQ
sleep habits questionnaire
- U
Mann-Whitney U test
- US
United States
- y
year(s)
REFERENCES
- 1.Autism and Developmental Disabilities Monitoring Network. Community Report on Autism 2014. Center for Disease Control and Prevention Web site. [Accessed September 12, 2015]. http://www.cdc.gov/ncbddd/autism/states/comm_report_autism_2014.pdf. Published March 28, 2014.
- 2.Khanna R, Madhavan SS, Smith MJ, Patrick JH, Tworek C, Becker-Cottrill B. Assessment of health-related quality of life among primary caregivers of children with autism spectrum disorders. J Autism Dev Disord. 2011;41(9):1214–1227. doi: 10.1007/s10803-010-1140-6. [DOI] [PubMed] [Google Scholar]
- 3.Lee GK, Lopata C, Volker MA, et al. Health-related quality of life of parents of children with high-functioning autism spectrum disorders. Focus Autism Other Dev Disabil. 2009;24(4):227–239. [Google Scholar]
- 4.Goldman SE, Richdale AL, Clemons T, Malow BA. Parental sleep concerns in autism spectrum disorders: variations from childhood to adolescence. J Autism Dev Disord. 2012;42(4):531–538. doi: 10.1007/s10803-011-1270-5. [DOI] [PubMed] [Google Scholar]
- 5.Richdale AL, Schreck KA. Sleep problems in autism spectrum disorders: prevalence, nature, & possible biopsychosocial aetiologies. Sleep Med Rev. 2009;13(6):403–411. doi: 10.1016/j.smrv.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 6.Adams HL, Matson JL, Cervantes PE, Goldin RL. The relationship between autism symptom severity and sleep problems: should bidirectionality be considered? Res Autism Spect Dis. 2014;8(3):193–199. [Google Scholar]
- 7.Hoffman CD, Sweeney DP, Lopez-Wagner M, Hodge D, Nam CY, Botts BH. Children with autism: sleep problems and mothers' stress. Focus Autism Other Dev Disabil. 2008;23(3):155–165. [Google Scholar]
- 8.Lopez-Wagner M, Hoffman CD, Sweeney DP, Hodge D, Gilliam J. Sleep problems of parents of typically developing children and parents of children with autism. J Genet Psychol. 2008;169(3):245–258. doi: 10.3200/GNTP.169.3.245-260. [DOI] [PubMed] [Google Scholar]
- 9.Allen RP, Walters AS, Montplaisir J, et al. Restless legs syndrome: prevalence and impact: REST general population study. Arch Intern Med. 2005;165(11):1286–1292. doi: 10.1001/archinte.165.11.1286. [DOI] [PubMed] [Google Scholar]
- 10.Hornyak M, Kopasz M, Berger M, Rieramm D, Voderholzer U. Impact of sleep-related complaints on depressive symptoms in patients with restless legs syndrome. J Clin Psychiatr. 2005;66(9):1139–1145. doi: 10.4088/jcp.v66n0909. [DOI] [PubMed] [Google Scholar]
- 11.Hornyak M, Feige B, Voderholzer U, Philipsen A, Riemann D. Polysomnography findings in patients with restless legs syndrome and in healthy controls: a comparative observational study. Sleep. 2007;30(7):861–865. doi: 10.1093/sleep/30.7.861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Winkelman JW, Redline S, Baldwin CM, Resnick HE, Newman AB, Gottlieb DJ. Polysomnographic and health-related quality of life correlates of restless legs syndrome in the Sleep Heart Health Study. Sleep. 2009;32(6):772–778. doi: 10.1093/sleep/32.6.772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Walters AS, Hickey K, Malzman J, et al. A questionnaire study of 138 patients with restless legs syndrome; the ‘Night-Walkers’ survey. Neurology. 1996;46(1):92–95. doi: 10.1212/wnl.46.1.92. [DOI] [PubMed] [Google Scholar]
- 14.Picchietti D, Allen RP, Walters AS, Davidson JE, Myers A, Ferini-Strambi L. Restless legs syndrome: prevalence and impact in children and adolescents-the Peds REST study. Pediatrics. 2007;120(2):253–266. doi: 10.1542/peds.2006-2767. [DOI] [PubMed] [Google Scholar]
- 15.Southwest Autism Research & Resource Center. About SARRC. Southwest Autism Research and Resource Center Web site. [Accessed September 12, 2015]. https://www.autismcenter.org/about-sarrc.
- 16.Lord C, Rutter M, DiLavore PC, Risi S. Autism Diagnostic Observation Schedule Manual. Los Angeles, CA: Western Psychological Services; 1999. [Google Scholar]
- 17.Lord C, Rutter M, DiLavore PC, Risi S, Gotham K, Bishop SL. ADOS-2 Manual. Torrance, CA: Western Psychological Services; 2012. [Google Scholar]
- 18.American Community Survey 2010-2014, 5 year estimates, median household income. United States Census Bureau Web site. American Fact Finder. [Accessed June 16, 2016]. http://www.factfinder.census.gov.
- 19.Renwick T, Short K. Examining the middle class in the United States using the lens of the supplemental poverty measure. United States Census Bureau Web site. [Accessed June 16, 2016]. https://www.census.gov/hhes/povmeas/publications/other/renwick_short-SPM.pdf. Published September 30, 2014.
- 20.Allen RP, Picchietti DL, Garcia-Borreguero D, et al. Restless legs syndrome/Willis-ekbom disease diagnostic criteria: updated international restless legs syndrome study group (IRLSSG) consensus criteria - history, rationale, description, and significance. Sleep Med. 2014;15(8):860–873. doi: 10.1016/j.sleep.2014.03.025. [DOI] [PubMed] [Google Scholar]
- 21.Quan SF, Howard BV, Iber C, et al. The sleep heart health study: design, rationale, and methods. Sleep. 1997;20:1077–1085. [PubMed] [Google Scholar]
- 22.Baldwin CM, Choi M, Bonds McClain D, Celaya A, Quan SF. Spanish translation and cross-language validation of a sleep habits questionnaire for use in clinical research settings. J Clin Sleep Med. 2012;8:137–146. doi: 10.5664/jcsm.1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jenkinson C, Layte R, Jenkinson D, et al. A shorter form health survey: can the SF-12 replicate results from the SF-36 in longitudinal studies? J Public Health Med. 1997;19:179–186. doi: 10.1093/oxfordjournals.pubmed.a024606. [DOI] [PubMed] [Google Scholar]
- 24.Ware JE, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Ware JE, Kosinski M, Keller SD. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales. 2nd ed. Boston, MA: Health Institute, New England Medical Center; 1995. [Google Scholar]
- 26.Owens JA, Spirito A, McGuinn M. The children's sleep habits questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep. 2000;23(8):1043–1051. [PubMed] [Google Scholar]
- 27.Malow BA, Byars K, Johnson K, et al. Practice pathway for the identification, evaluation, and management of insomnia in children and adolescents with autism spectrum disorders. Pediatrics. 2012;130:S106–S124. doi: 10.1542/peds.2012-0900I. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Achenbach TM. Manual for Child Behavior Checklist/4-18 and 1991 Profile. Burlington, VT: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- 29.Ware JE, Kosinski M, Keller SD. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales. 3rd ed. Lincoln, RI: QualityMetric Incorporated; 1998. [Google Scholar]
- 30.Kushida C, Martin M, Nikam P, et al. Burden of restless legs syndrome on health-related quality of life. Qual Life Res. 2007;16(4):617–624. doi: 10.1007/s11136-006-9142-8. [DOI] [PubMed] [Google Scholar]
- 31.National Center for Health Statistics. Health, United States, 2011: With Special Feature on Socioeconomic Status and Health. Hyattsville, MD: National Center for Health Statistics; 2012. [PubMed] [Google Scholar]
- 32.Cortese S, Konofal E, Lecendreux M, et al. Restless legs syndrome and attention-deficit/hyperactivity disorder: a review of the literature. Sleep. 2005;28(8):1007–1013. doi: 10.1093/sleep/28.8.1007. [DOI] [PubMed] [Google Scholar]
- 33.Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Psychol. 2008;47(8):921–929. doi: 10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- 34.Youssef J, Singh K, Huntington N, Becker R, Kothare SV. Relationship of serum ferritin levels to sleep fragmentation and periodic limb movements of sleep on polysomnography in autism spectrum disorders. Pediatr Neurol. 2013;49(4):274–278. doi: 10.1016/j.pediatrneurol.2013.06.012. [DOI] [PubMed] [Google Scholar]
- 35.Nguyen M, Roth A, Kyzar EJ, et al. Decoding the contribution of dopaminergic genes and pathways to autism spectrum disorder (ASD) NeuroChem Int. 2014;66:15–26. doi: 10.1016/j.neuint.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 36.Wang J, O'Reilly B, Venkataraman R, Mysliewiec V, Mysliewiec A. Efficacy of oral iron in patients with restless legs syndrome and a low-normal ferritin: a randomized, double-blind, placebo-controlled study. Sleep Med. 2009;10:973–975. doi: 10.1016/j.sleep.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 37.Winkelman JW, Finn L, Young T. Prevalence and correlates of restless legs syndrome symptoms in the Wisconsin Sleep Cohort. Sleep Med. 2006;7(7):545–552. doi: 10.1016/j.sleep.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 38.Finan PH, Smith MT. The comorbidity of insomnia, chronic pain, and depression: dopamine as a putative mechanism. Sleep Med Rev. 2013;17(3):174–183. doi: 10.1016/j.smrv.2012.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ohayon MM, Roth T. Prevalence of restless legs syndrome and periodic limb movement disorder in the general population. J Psychosom Res. 2002;53(1):547–554. doi: 10.1016/s0022-3999(02)00443-9. [DOI] [PubMed] [Google Scholar]
- 40.Hoffman CD, Sweeney DP, Hodge D, Lopez-Wagner M, Looney L. Parenting stress and closeness: mothers of typically developing children and mothers of children with autism. Focus Autism Other Dev Disabil. 2009;24(3):178–187. [Google Scholar]
- 41.Abbeduto L, Seltzer MM, Shattuck P, Krauss MW, Orsmond G, Murphy MM. Psychological well-being and coping in mothers of youths with autism, down syndrome, or fragile X syndrome. Am J Ment Retard. 2004;109(3):237–254. doi: 10.1352/0895-8017(2004)109<237:PWACIM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 42.Benjak T, Vuletić Mavrinac G, Pavić Simetin I. Comparative study on self-perceived health of parents of children with autism spectrum disorders and parents of non-disabled children in Croatia. Croat Med J. 2009;50(4):403–409. doi: 10.3325/cmj.2009.50.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Christensen DL, Baio J, Van Naarden Braun K, et al. Prevalence and characteristics of autism spectrum disorder among children aged 8 years-autism and developmental disabilities monitoring network, 11 sites, United States, 2012. MMWR Surveill Summ. 2016;65(3):1–23. doi: 10.15585/mmwr.ss6503a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hilton CL, Fitzgerald RT, Jackson KM, et al. Brief report: Under-representation of African Americans in autism genetic research: a rationale for inclusion of subjects representing diverse family structures. J Autism Dev Disord. 2010;40(5):633–639. doi: 10.1007/s10803-009-0905-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Martin BT, Williamson BD, Edwards N, Teng AY. Parental symptom report and periodic limb movements of sleep in children. J Clin Sleep Med. 2008;4(1):57–61. [PMC free article] [PubMed] [Google Scholar]
- 46.Gotham K, Risi S, Pickles A, Lord C. The autism diagnostic observation schedule: revised algorithms for improved diagnostic validity. J Autism Dev Disord. 2007;37(4):613–627. doi: 10.1007/s10803-006-0280-1. [DOI] [PubMed] [Google Scholar]


