Abstract
Study Objectives:
Short and long sleep durations have been found to be associated with chronic conditions like diabetes mellitus, hypertension and cardiovascular disease. However, most studies were conducted in developed countries and the results were inconsistent. The aim of this study is to investigate the association between sleep duration and self-reported health status in a developing country setting.
Methods:
We conducted secondary data analysis of the 2010 Gross National Happiness study of Bhutan, which was a nationwide cross sectional study with representative samples from rural and urban areas. The study included 6476 participants aged 15–98 y. The main outcome variable of interest was self-reported health status. Sleep duration was categorized as ≤ 6 h, 7 h, 8 h, 9 h, 10 h, and ≥ 11 h. Multiple logistic regressions were conducted to investigate the association between sleep duration and self-reported health status.
Results:
The mean sleep duration was 8.5 (± 1.65) h. Only 9% of the respondents slept for 7 h; 6% were short sleepers (≤ 6 h) and 84% were long sleepers (21%, 8 h; 28%, 9 h; 22%, 10 h; 13%, ≥ 11 h). We found that both short (≤ 6 h) and long sleep duration (≥ 11 h) were independently associated with poor self-reported health status.
Conclusions:
This study found that people with shorter and longer sleep durations were more likely to report poorer health status.
Citation:
Sithey G, Wen LM, Kelly P, Li M. Association between sleep duration and self-reported health status: findings from the Bhutan's gross national happiness study. J Clin Sleep Med. 2017;13(1):33–38.
Keywords: sleep, sleep duration, self-reported health status, developing country, rural population
INTRODUCTION
Sleep duration is reportedly associated with perceived physical and mental health status.1–3 There is increasing evidence that too little or too much sleep is associated with adverse health outcomes including mortality and morbidity.4–10 Many studies report a U-shaped association between sleep duration and increased health risks.11–15 In addition, systematic reviews and meta-analyses show that both long and short sleep durations are associated with non-communicable diseases (NCDs) such as diabetes,16–18 hypertension,8 cardiovascular disease,19,20 and obesity.21,22 While we know the important association between sleep duration and various health risks, little is known about the relationship between sleep duration and self-reported health status.
Self-reported health status is a subjective measure of an individual's health and is commonly used in monitoring public health programs and epidemiological studies. It is an inexpensive method which can assess important and valid indicators of an individual's health status. It is recommended as a health indicator by the World Health Organization.23–25 In addition, self-reported health status is strongly associated with morbidity,26 and it is a strong independent predictor of mortality,27 not only in the elderly group but also in the middle-aged population.28 Studies from high-income countries also indicate that too little and too much sleep are associated with chronic health conditions.8,9,18
BRIEF SUMMARY
Current Knowledge/Study Rationale: The association between sleep duration and self-reported health status has been mostly investigated in developed countries; results were inconsistent. To our knowledge, this is the first study using the nationally representative survey data to investigate the association between sleep duration and self-reported health status in a developing country setting.
Study Impact: We found that both shorter and longer sleep durations were associated with poor self-reported health status. This finding is significant as it highlights sleep duration as an emerging lifestyle related health risk behaviour even in a developing country.
Furthermore, some studies have indicated that sleep duration was associated with poor self-reported health status, but they were mostly conducted in developed countries and the results were not consistent. For example, large nationally represented studies from Korea (≥ 19 y),29 Australia (45–74 y)30 and United States (≥ 18 y)31 found that both short (≤ 5 h, ≤ 6 h, and ≤ 6 h, respectively) and long (≥ 9 h, ≥ 9 h, and ≥ 8 h, respectively) sleep durations were associated with poor self-reported health status. Conversely, a study conducted among elderly population (> 60 y) in Lima, Peru and a large multi-country study among university students aged 17–30 y found that only short sleep duration (< 6 h and < 7 h, respectively) was associated with poor self-reported health status32,33; whereas Jean-Louis et al. found no association between sleep duration and the health-related quality-of-life score in a small sample size (273 respondents) study.34 In addition a large-scale, multi-national study among eight countries in Asia and Africa highlighted that sleep problems might represent a significant and unrecognized public health issue in low income settings.35
In this context, the aim of this study is to examine the association between sleep duration and self-reported health status using data from the 2010 Gross National Happiness Study, a nationally represented Bhutanese sample. This study is different from previously reported studies because 60% of the survey respondents were farmers residing in the remote rural villages. Only 20% and 51% of the respondents had access to internet and television, respectively. Also, the sample size is nationally representative encompassing all groups aged above 15 y.
METHODS
Study Design
We conducted secondary data analysis using data extracted from the 2010 Gross National Happiness (GNH) study conducted by The Centre for Bhutan Studies and GNH Research, Royal Government of Bhutan. It was a nationwide cross sectional study designed to produce statistically reliable estimates of people's happiness (using the Gross National Happiness Index) at the national level with representative samples from rural and urban areas of each of the 20 districts. The study background and the details of the study design, questionnaire and methods are described in the World Happiness Report 201236 and in the Report titled “An Extensive Analysis of GNH Index.”37 In brief, it was a multi-stage, stratified cluster sampling study design, using the 2005 national census data for sampling frame and selection of clusters. The primary sampling units (PSU) were selected using probability proportional to sampling (PPS) method. The households listing for the PSUs were taken from the districts immigration office and selected by random systematic selection procedures.
Survey Respondents and Instrument
The survey was conducted between April and December 2010 by trained enumerators through household visits. The survey questionnaire had nine domains, including “Time use and balance.” Totalling 7,142 respondents aged 15–98 y were surveyed with mean age of 41 y. Of the total sample surveyed, 6,476 (91%) had complete information on sleep duration and they were included in this analysis.
Main Variable of Interest
The main outcome variable of interest of this study was the self-reported health status which was determined by a single question; “In general, would you say your health is excellent, very good, good, fair or poor?” In this analysis we have combined the responses into a binary outcome, good health (i.e., excellent, very good, and good) and poor health (i.e., fair and poor).
Sleep Duration
Under the survey domain, “Time use and balance,” the respondents were asked how they spent their time during the previous day, “beginning with when you woke up, can you please recount various activities you performed and how long they took?” From this 24-h recall period, the sleep duration was recorded as continuous variable in minutes and converted into hours with one decimal place, then they were categorized into ≤ 6 h, 7 h, 8 h, 9 h, 10 h, and ≥ 11 h. These categories were consistent with previous studies on sleep and self-reported health status.1 Seven hours is used as a reference category because the majority of the studies have used 7 h as the reference category14,29,31,38 and 7 to 8 h sleep is also reportedly associated with the lowest risk of morbidity and mortality.4,14,39
Other Main Covariates
Sociodemographic factors like age, gender, household income and household size were included in the analysis. Age was assessed as a continuous variable and was also divided into six groups 15–24 y, 25–34 y, 35–44 y, 45–54 y, 55–64 y, and ≥ 65 y. Health-related behaviors such as consumption of alcohol and chewing betel nuts during the past 12 mo were also included in the model, as well as subjective well-being and number of working hours per day. Subjective well-being was assessed on a Likert scale 0 to 10, where 0 is not a very happy person and 10 being very happy person.
Statistical Analysis
We examined the characteristics of the respondents by categories of sleep duration with χ2 test. Bivariate association between self-reported health status and categorical covariates were examined by χ2 test. We estimated crude odds ratio and 95% confidence intervals (CI) for the relationship between poor self-reported health status and each of the covariates using simple logistic regression models.
Multiple logistic regression models were fitted to assess the association of sleep duration (predictor) with poor self-reported health status (outcome). In these models we categorized sleep into 6 groups: ≤ 6 h, 7 h, 8 h, 9 h, 10 h, and ≥ 11 h, and used 7 h as the referent group. A total of 16 variables with p value of < 0.25 based on the Wald χ2 statistics from the univariate analysis were included in the multivariate analysis. A value of p < 0.25 was chosen to allow for maximum potential confounders to be included in the model. Data were checked for collinearity. Backward elimination technique was performed. Demographic variables like place of residence (rural and urban), education level, occupation, marital status, spirituality, household size, and health-related behavior such as smoking and chewing tobacco were statistically not significant (p > 0.05), therefore removed from the final model. Their removal from the model did not result in any substantial (< 10%) change in the parameter estimate. The final adjusted model consisted of 8 variables, i.e., sleep duration, age, gender, total household cash income, working hours, subjective well-being, alcohol consumption, and chewing betel nuts.
The adjusted odds ratio and 95% confidence interval (CI) of sleep duration associated with poor health (poor and fair) were calculated. The data were analyzed using SAS 9.4 and the results were reported as adjusted odds ratios and 95% confidence intervals, with a p value < 0.05 considered statistically significant. There were no significant interaction terms.
RESULTS
Table 1 presents characteristics of the study population. Of the 6,476 respondents, 48% were male and 52% were females. Seventy-eight percent of them were from rural and 22% from urban area. Sixty-five percent had no formal education, and 60% of the respondents were farmers by occupation.
Table 1.
Characteristic of the study population by sleep duration based on the 2010 Gross National Happiness (GNH) study.
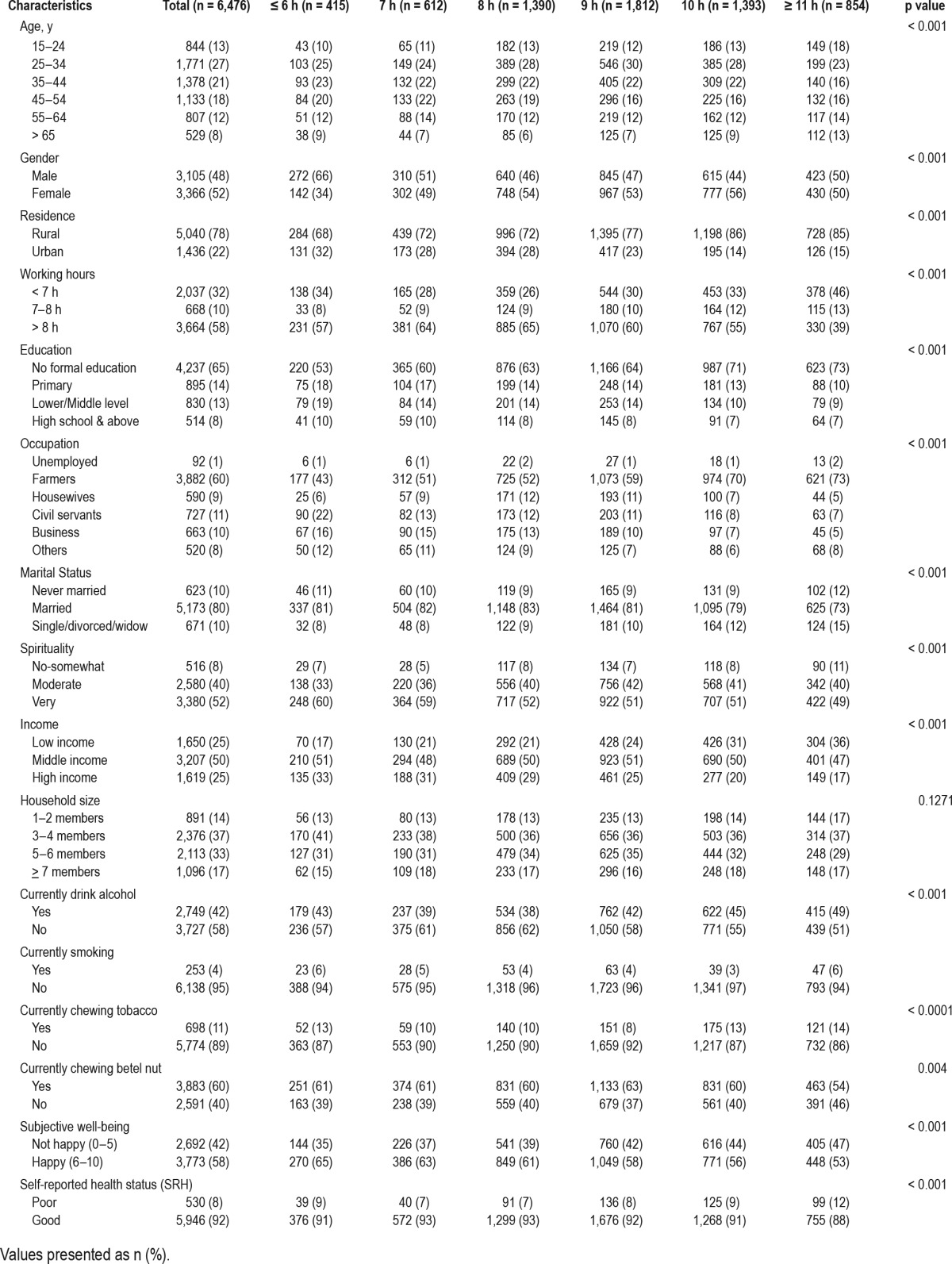
A total of 415 respondents (6%) were sleeping ≤ 6 h, 612 (9%) were sleeping 7 h, and 5,499 (84%) were sleeping 8 h or more (21% 8 h; 28% 9 h; 22% 10 h and 13% ≥ 11 h). The mean sleep duration was 8.5 (± 1.65) h. Table 1 also shows very strong overall associations (p < 0.001) of sleep duration with sociodemographic characteristics, health-related behaviors (smoking, alcohol consumption, chewing betel nut), subjective well-being and self-reported health status.
Sleep duration and other characteristics of the 530 (8%) respondents with poor health status (poor and fair) are presented in Table 2. Among them 39 (7%) reported sleeping ≤ 6 h, 40 (8%) sleeping for 7 h, and 451 (85%) were sleeping ≥ 8 h (17%, 8 h; 26%, 9h; 24%, 10 h, and 19% ≥ 11 h).
Table 2.
Association between sleep duration and self-reported poor health (poor/fair) using logistic regression models.
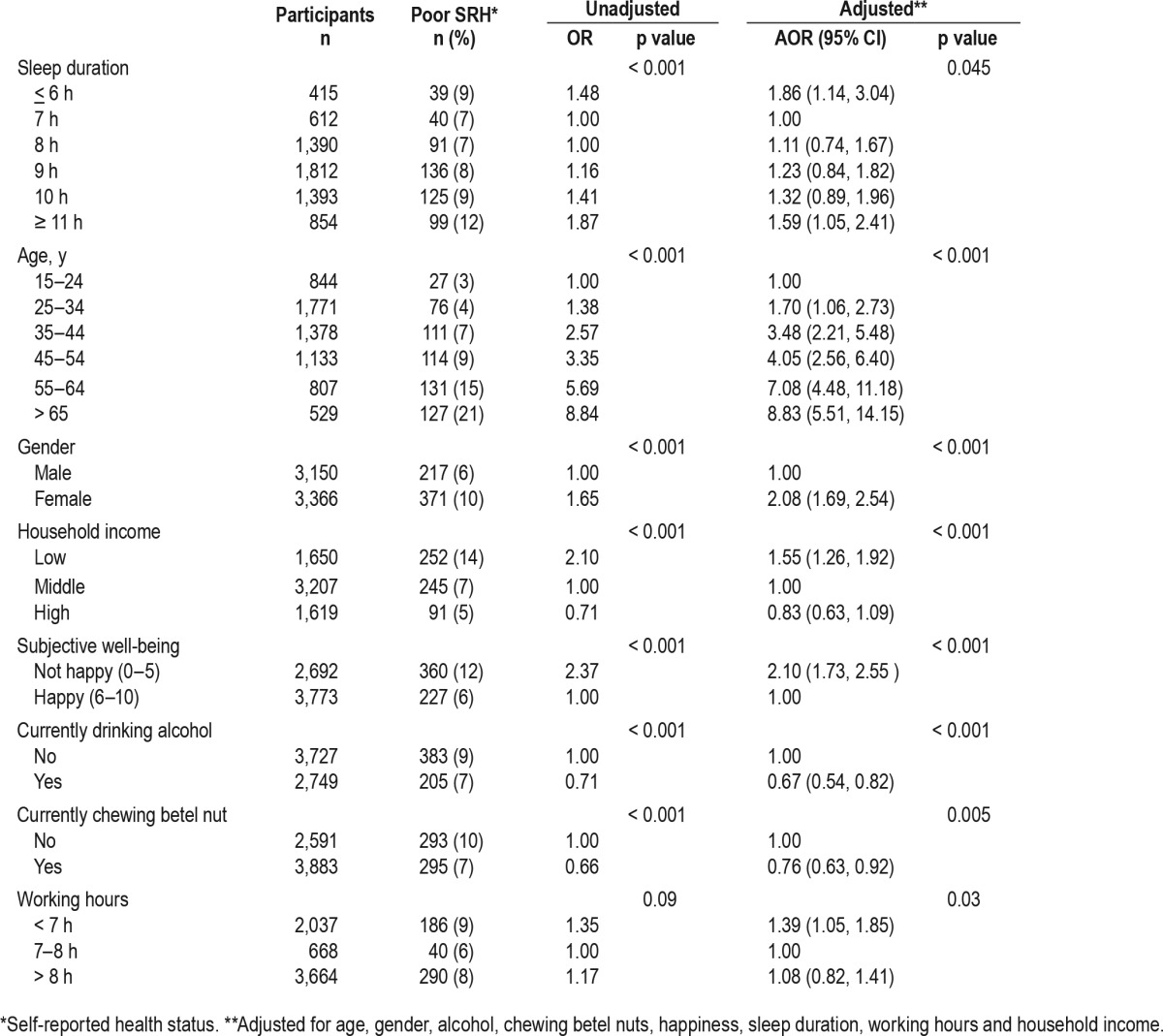
Table 2 also presents the association between sleep duration and self-reported health status showing the unadjusted and adjusted results from the logistic regression models. After adjusting for gender, age, total cash income, alcohol consumption, chewing betel nut, subjective well-being, and working hours, poor health status was positively associated with respondents sleeping ≤ 6 or sleeping ≥ 11 h. The adjusted odds of reporting poor self-reported health status was 1.86 times (95% CI: 1.14, 3.04) or 1.59 times (95% CI: 1.05, 2.41) higher in those sleeping ≤ 6 h or those sleeping ≥ 11 h than those having sleep duration of 7 h, respectively.
When taking 15–24 y as the reference age group, there was a trend of significant increase in the odds of reporting poor health with aging. Furthermore, female respondents were more likely to report poor health status with adjusted odds of 2.08 (95% CI: 1.69, 2.54) compared with males.
The model also shows that respondents who were drinking alcohol or chewing betel nuts were less likely to report poor health status with adjusted odds of 0.67 (95% CI: 0.54, 0.82) or 0.76 (95% CI: 0.63, 0.92), respectively. The adjusted odds of reporting poor health was 1.55 times (95% CI: 1.26, 1.92) higher in low income groups (< 25th percentile) than those in middle income group (50 percentile).
There was also a statistically significant association between working hours and poor health status. Respondents working < 7 h were more likely to report poor self-reported health status with adjusted odds of 1.39 (95% CI: 1.05, 1.85) compared with those working 7–8 h.
DISCUSSION
This secondary data analysis of the 2010 Gross National Happiness study found that people having both short (≤ 6 h) and long (≥ 11 h) sleep durations were more likely to report poor health status (poor and fair) compared to those having 7 h of sleep duration. This association was found to be independent of the factors including age, gender, household income, alcohol consumption, chewing betel nut, subjective well-being and working hours.
This study for the first time shows that the prevalence of sleep duration, and those characteristics associated with sleep duration in a low-income country with a predominantly (78%) rural sample, and 66% of the respondents without formal education. This, to our knowledge, is also the first study to investigate the association between sleep duration and self-reported health status from a developing country, with a nationally representative sample encompassing all groups aged above 15 y. Previously, almost all studies on sleep duration and self-reported health status were from developed or high income countries,1 except for one study with university students from a number of low income countries.40
Sleep duration, both long and short, has been shown to be associated with adverse health effects. Our study found that a large proportion (63%) of the Bhutanese population was sleeping for a longer duration (≥ 9 h), and this proportion was larger than that of other countries. For instance, cross-sectional studies from Korea, United States and Australia revealed that only 8%, 9%, and 17% of surveyed population slept ≥ 9 h, respectively.29–31 In addition, Bhutan's average sleep time of 8.5 h is high when compared to other nationally representative studies from Finland (7.5 h), Austria (7 h), Korea (6.7 h), and United States (7.2 h).19,41–43 The high proportion of long sleepers in Bhutan could be because the majority of the respondents were from the rural areas without formal education. Furthermore, only 20% and 51% had access to internet and television, respectively, and 42% of the respondents were drinking alcohol.
Our findings provide further evidence that both short and long sleep durations are significantly associated with poor self-reported health status. These findings are important because both long and short sleep durations are reportedly associated with adverse health outcomes such as diabetes, hypertension, obesity, and cardiovascular diseases.8,16,19,22 Further, a systematic review and meta-analysis conducted by Cappuccio et al. showed that short sleepers (commonly < 7 h per night, often < 5 h per night) and long sleepers (commonly > 8 h or 9 h per night) have a 12% and a 30% greater risk of dying, respectively, than those sleeping 7 to 8 h per night.20
As the evidences suggest, sleep duration is an emerging public health problem related to life style.35 In addition, awareness among general public and health care providers on the importance of sleep is low. Therefore, public health interventions to raise awareness on sleep health may play an important role in promoting health and well-being of the population.
The main strengths of the study are the large nationally representative sample size from all 20 districts encompassing all age groups above 15 y of age of both rural and urban communities of Bhutan; in addition to sleep duration, a range of sociodemographic factors are taken into account in the multivariate analyses. There were several limitations to our study. First, the Gross National Happiness Study was a cross-sectional study, so we cannot establish any causal relationship between sleep duration and self-reported health status. A future prospective longitudinal study is required to establish the causal relationship. Second, the sleep duration was measured subjectively, which could have introduced recall bias. A more objective measure will help to minimise the misclassification of sleep duration. Third, the choice of 7 h as the sleep reference category is based on limited evidence on the association of sleep duration and self-reported health status. The optimal sleep duration for various populations needs to be further explored.
CONCLUSIONS
In summary, this study has shown that people with shorter or longer sleep durations were more likely to report fair or poor health status. In particular, longer sleep duration reflects the current life style of the Bhutanese population which could be due to limited access to television, internet and high proportion of illiterate respondents. At the same time, we recommend the need for public awareness on the importance of adequate sleep duration and its health benefits.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank Dasho Karma Ura, Executive Director and Ms. Tshoki Zangmo, of the Centre for Bhutan Studies and GNH Research, Royal Government of Bhutan for providing the data and rendering all possible support.
ABBREVIATIONS
- CI
confidence intervals
- GNH
gross national happiness
- NCD
non-communicable diseases
- PSU
primary sampling units
- PPS
probability proportional to sampling
- SRH
self-reported health status
- WHO
World Health Organization
REFERENCES
- 1.Frange C, de Queiroz SS, da Silva Prado JM, Tufik S, de Mello MT. The impact of sleep duration on self-rated health. Sleep Sci. 2014;7(2):107–113. doi: 10.1016/j.slsci.2014.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reid KJ, Martinovich Z, Finkel S, et al. Sleep: a marker of physical and mental health in the elderly. Am J Geriatr Psychiatry. 2006;14(10):860–866. doi: 10.1097/01.JGP.0000206164.56404.ba. [DOI] [PubMed] [Google Scholar]
- 3.Alvarez GG, Ayas NT. The impact of daily sleep duration on health: a review of the literature. Prog Cardiovasc Nurs. 2004;19(2):56–59. doi: 10.1111/j.0889-7204.2004.02422.x. [DOI] [PubMed] [Google Scholar]
- 4.Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res. 2009;18(2):148–158. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- 5.Lee JS, Auyeung TW, Leung J, et al. Long sleep duration is associated with higher mortality in older people independent of frailty: a 5-year cohort study. J Am Med Dir Assoc. 2014;15(9):649–654. doi: 10.1016/j.jamda.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 6.Grandner MA, Drummond SP. Who are the long sleepers? Towards an understanding of the mortality relationship. Sleep Med Rev. 2007;11(5):341–360. doi: 10.1016/j.smrv.2007.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kronholm E, Laatikainen T, Peltonen M, Sippola R, Partonen T. Self-reported sleep duration, all-cause mortality, cardiovascular mortality and morbidity in Finland. Sleep Med. 2011;12(3):215–221. doi: 10.1016/j.sleep.2010.07.021. [DOI] [PubMed] [Google Scholar]
- 8.Guo X, Zheng L, Wang J, et al. Epidemiological evidence for the link between sleep duration and high blood pressure: a systematic review and meta-analysis. Sleep Med. 2013;14(4):324–332. doi: 10.1016/j.sleep.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Lima MG, Bergamo Francisco PMS, de Azevedo Barros MB. Sleep duration pattern and chronic diseases in Brazilian adults (ISACAMP, 2008/09) Sleep Med. 2012;13(2):139–144. doi: 10.1016/j.sleep.2011.07.011. [DOI] [PubMed] [Google Scholar]
- 10.Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. 2010;71(5):1027–1036. doi: 10.1016/j.socscimed.2010.05.041. [DOI] [PubMed] [Google Scholar]
- 11.Kakizaki M, Kuriyama S, Nakaya N, et al. Long sleep duration and cause-specific mortality according to physical function and self-rated health: the Ohsaki Cohort Study. J Sleep Res. 2013;22(2):209–216. doi: 10.1111/j.1365-2869.2012.01053.x. [DOI] [PubMed] [Google Scholar]
- 12.Grandner MA, Hale L, Moore M, Patel NP. Mortality associated with short sleep duration: the evidence, the possible mechanisms, and the future. Sleep Med Rev. 2010;14(3):191–203. doi: 10.1016/j.smrv.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ferrie JE, Shipley MJ, Cappuccio FP, et al. A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort. Sleep. 2007;30(12):1659–1666. doi: 10.1093/sleep/30.12.1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33(5):585–592. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tamakoshi A, Ohno Y, Group JS. Self-reported sleep duration as a predictor of all-cause mortality: results from the JACC study, Japan. Sleep. 2004;27(1):51–54. [PubMed] [Google Scholar]
- 16.Shan Z, Ma H, Xie M, et al. Sleep duration and risk of type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care. 2015;38(3):529–537. doi: 10.2337/dc14-2073. [DOI] [PubMed] [Google Scholar]
- 17.Yaggi HK, Araujo AB, McKinlay JB. Sleep duration as a risk factor for the development of type 2 diabetes. Diabetes Care. 2006;29(3):657–661. doi: 10.2337/diacare.29.03.06.dc05-0879. [DOI] [PubMed] [Google Scholar]
- 18.Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2010;33(2):414–420. doi: 10.2337/dc09-1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ford ES. Habitual sleep duration and predicted 10-year cardiovascular risk using the pooled cohort risk equations among US adults. J Am Heart Assoc. 2014;3(6):e001454. doi: 10.1161/JAHA.114.001454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cappuccio FP, Cooper D, D'Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J. 2011;32(12):1484–1492. doi: 10.1093/eurheartj/ehr007. [DOI] [PubMed] [Google Scholar]
- 21.Kohatsu ND, Tsai R, Young T, et al. Sleep duration and body mass index in a rural population. Arch Intern Med. 2006;166:1701–1705. doi: 10.1001/archinte.166.16.1701. [DOI] [PubMed] [Google Scholar]
- 22.Knutson KL, Van Cauter E. Associations between sleep loss and increased risk of obesity and diabetes. Ann N Y Acad Sci. 2008;1129:287–304. doi: 10.1196/annals.1417.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fayers PM, Sprangers MA. Understanding self-rated health. Lancet. 2002;359(9302):187–188. doi: 10.1016/S0140-6736(02)07466-4. [DOI] [PubMed] [Google Scholar]
- 24.Subramanian SV, Huijts T, Avendano M. Self-reported health assessments in the 2002 World Health Survey: how do they correlate with education? Bull World Health Organ. 2010;88(2):131–138. doi: 10.2471/BLT.09.067058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.de Bruin A, Picavet HS, Nossikov A. Health interview surveys. Towards international harmonization of methods and instruments. WHO Reg Publ Eur Ser. 1996;58:i–xiii, 1-161. [PubMed] [Google Scholar]
- 26.Goldberg P, Gueguen A, Schmaus A, Nakache JP, Goldberg M. Longitudinal study of associations between perceived health status and self reported diseases in the French Gazel cohort. J Epidemiol Community Health. 2001;55(4):233–238. doi: 10.1136/jech.55.4.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38(1):21–37. [PubMed] [Google Scholar]
- 28.Miilunpalo S, Vuori I, Oja P, Pasanen M, Urponen H. Self-rated health status as a health measure: the predictive value of self-reported health status on the use of physician services and on mortality in the working-age population. J Clin Epidemiol. 1997;50(5):517–528. doi: 10.1016/s0895-4356(97)00045-0. [DOI] [PubMed] [Google Scholar]
- 29.Kim JH, Kim KR, Cho KH, Yoo KB, Kwon JA, Park EC. The association between sleep duration and self-rated health in the Korean general population. J Clin Sleep Med. 2013;9(10):1057–1064. doi: 10.5664/jcsm.3082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Magee CA, Caputi P, Iverson DC. Relationships between self-rated health, quality of life and sleep duration in middle aged and elderly Australians. Sleep Med. 2011;12(4):346–350. doi: 10.1016/j.sleep.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 31.Shankar A, Charumathi S, Kalidindi S. Sleep duration and self-rated health: the national health interview survey 2008. Sleep. 2011;34(9):1173–1177. doi: 10.5665/SLEEP.1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lima MG, Barros MBdA, Alves MCGP. Sleep duration and health status self-assessment (SF-36) in the elderly: a population-based study (ISA-Camp 2008) Cad Saude Publica. 2012;28(9):1674–1684. doi: 10.1590/s0102-311x2012000900007. [DOI] [PubMed] [Google Scholar]
- 33.Steptoe A, Peacey V, Wardle J. Sleep duration and health in young adults. Arch Intern Med. 2006;166(16):1689–1692. doi: 10.1001/archinte.166.16.1689. [DOI] [PubMed] [Google Scholar]
- 34.Jean-Louis G, Kripke DF, Ancoli-Israel S. Sleep and quality of well-being. Sleep. 2000;23(8):1115–1121. [PubMed] [Google Scholar]
- 35.Stranges S, Tigbe W, Gomez-Olive FX, Thorogood M, Kandala NB. Sleep problems: an emerging global epidemic? Findings from the INDEPTH WHO-SAGE study among more than 40,000 older adults from 8 countries across Africa and Asia. Sleep. 2012;35(8):1173–1181. doi: 10.5665/sleep.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Helliwell JF, Layard R, Sachs J. World Happiness Report 2012. Available at http://worldhappiness.report/ed/2012/
- 37.Ura K, Alkire S, Zangmo T, Wangdi K. An Extensive Analysis of GNH Index. Thimphu, Bhutan: The Centre for Bhutan Studies; 2012. [Google Scholar]
- 38.Magee CA, Iverson DC, Caputi P. Factors associated with short and long sleep. Prev Med. 2009;49(6):461–467. doi: 10.1016/j.ypmed.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 39.Hublin C, Partinen M, Koskenvuo M, Kaprio J. Sleep and mortality: a population-based 22-year follow-up study. Sleep. 2007;30(10):1245–1253. doi: 10.1093/sleep/30.10.1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Peltzer K, Pengpid S. Sleep duration and health correlates among university students in 26 countries. Psycho Health Med. 2016;21(6):208–220. doi: 10.1080/13548506.2014.998687. [DOI] [PubMed] [Google Scholar]
- 41.Kronholm E, HÄRmÄ M, Hublin C, Aro AR, Partonen T. Self-reported sleep duration in Finnish general population. J Sleep Res. 2006;15(3):276–290. doi: 10.1111/j.1365-2869.2006.00543.x. [DOI] [PubMed] [Google Scholar]
- 42.Tribl GG, Schmeiser-Rieder A, Rosenberger A, et al. Sleeping habits in the Austrian population. Sleep Med. 2002;3(1):21–28. doi: 10.1016/s1389-9457(01)00117-4. [DOI] [PubMed] [Google Scholar]
- 43.Kim YY, Kim UN, Lee JS, Park JH. The effect of sleep duration on the risk of unintentional injury in Korean adults. J Prev Med Public Health. 2014;47(3):150–157. doi: 10.3961/jpmph.2014.47.3.150. [DOI] [PMC free article] [PubMed] [Google Scholar]


