A review of 76 studies found strong evidence that ROM and strengthening exercises and joint mobilizations can improve function and decrease pain for adults with shoulder conditions.
Abstract
People with musculoskeletal disorders of the shoulder commonly experience pain, decreased strength, and restricted range of motion (ROM) that limit participation in meaningful occupational activities. The purpose of this systematic review was to evaluate the current evidence for interventions within the occupational therapy scope of practice that address pain reduction and increase participation in functional activities. Seventy-six studies were reviewed for this study—67 of Level I evidence, 7 of Level II evidence, and 2 of Level III evidence. Strong evidence was found that ROM, strengthening exercises, and joint mobilizations can improve function and decrease pain. The evidence to support physical modalities is moderate to mixed, depending on the shoulder disorder. Occupational therapy practitioners can use this evidence to guide daily clinical decision making.
The U.S. Bureau of Labor Statistics (2014) has estimated that 8.2% of musculoskeletal injuries are shoulder related, and shoulder pain among older adults has been estimated at 21% (Hermoso & Calvo, 2009). Upper-limb dysfunction affects daily physical function (Walker-Bone, Palmer, Reading, Coggon, & Cooper, 2004), and disorders of the shoulder lead to acute and chronic pain. Nearly half the population will have a yearly episode of shoulder pain (Brox, 2003), which is associated with limitations in occupational domains such as sleep, activities of daily living, and overall quality of life (Ostör, Richards, Prevost, Speed, & Hazleman, 2005).
Given the impact of shoulder dysfunction on occupational domains, occupational therapy practitioners have a distinct role in the treatment of these disorders. Many interventions for shoulder disorders aim to promote functional activity through preparatory methods. The Occupational Therapy Practice Framework: Domain and Process (3rd ed.; American Occupational Therapy Association [AOTA], 2014) describes a cyclical relationship among preparatory methods and tasks, activities, and occupations that affects client factors. Preparatory methods and tasks are part of treatment to prepare clients to engage in occupational performance (AOTA, 2014). Preparatory methods and tasks can be viewed as a means to an end. The means are evidence-based interventions, and the ends are clients participating in daily occupations. Occupational therapy practitioners use preparatory methods to affect body structures with the ultimate goal of promoting performance in occupations.
It is critically important that occupational therapy practitioners and educators use evidence-based interventions to advance occupational therapy as a viable profession (AOTA, 2007). Since 1998, AOTA has instituted a series of evidence-based practice (EBP) projects to assist members with meeting the challenge of finding and reviewing the literature to identify occupational therapy evidence and, in turn, using this evidence to inform practice (Lieberman & Scheer, 2002). A major focus of AOTA’s EBP projects is an ongoing program of systematic review of the multidisciplinary scientific literature, using focused questions and standardized procedures to identify occupational therapy–relevant evidence and discuss its implications for practice, education, and research. An earlier review (von der Hyde, 2011) covered occupational therapy interventions for shoulder conditions from 1986 through 2005.
This systematic review updates the earlier review by summarizing the literature published from May 2006 through July 2014. The review was conducted to address the following focused question: What is the evidence for the effect of occupational therapy interventions for adults with musculoskeletal disorders of the shoulder?
Method
Search Strategy
Search terms for the review were developed by the methodology consultant to the AOTA EBP Project and AOTA staff, in consultation with the review authors and the advisory group. The search terms were developed not only to capture pertinent articles but also to make sure that the terms relevant to the specific thesaurus of each database were included. The original search strategy for musculoskeletal disorders of the upper extremity (UE; von der Hyde, 2011) was used for the updated review (see Supplemental Appendix 1, available online at http://otjournal.net; navigate to this article, and click on “Supplemental Materials”). Additional search terms were added to ensure maximum coverage of the focused question. Table 1 lists the search terms related to population (musculoskeletal disorders of the UE) and the types of interventions included in the systematic review. A medical research librarian with experience in completing systematic review searches conducted all searches and confirmed and improved the search strategies.
Table 1.
Search Terms for Musculoskeletal Disorders
| Category | Key Search Terms |
| Diagnoses/injuries/clinical conditions—hand/wrist/forearm, elbow, shoulder | adhesive capsulitis, amputation—above elbow, amputations (below elbow, transradial, thumb, finger, with wrist disarticulation), arthritis, arthrogryposis, athletic injuries, axilla, biceps tendon rupture, bicipital tendonitis, brachial plexus injury, burn, calcific shoulder, camptodactly, carpal instability, carpal tunnel syndrome, collateral ligament—strain, Colles’ fracture (closed and open), complex regional pain syndrome, crushing injury—upper arm (wrist, hand, and finger), cubital tunnel syndrome, cumulative trauma, degenerative joint disease, DeQuervain’s tenosynovitis, digit, digital injuries, dislocated finger, dislocation, dislocation—glenohumeral, Dupuytren’s contracture, elbow, elbow joint, extensor tendon rupture, finger, finger injuries, flexor tendon rupture, forearm, fracture anatomical head humerus, fracture greater tuberosity humerus—open, fracture humerus shaft—closed, glenohumeral, hand, hand injuries, joint, Kienbocks disease, lacerating tendon, lateral epicondylitis, mallet finger, medial epicondylitis, multiple fractures hand (closed and open), open wound (finger and hand), pronator teres syndrome, radial and ulnar fractures, radial head fracture, radial tunnel syndrome, reflex sympathetic dystrophy, repetitive strain injury, rotator cuff syndrome shoulder, rotator cuff tear, scapulothoracic articulation, shoulder impingement, shoulder joint, shoulder pain, shoulder strain, shoulder tendonitis, sprain elbow, sprain radiohumeral joint, sprains and strains—rotator cuff, subacromial bursitis, tennis elbow, tenosynovitis elbow, tenosynovitis—hand and wrist, thumb, thumb injuries, triangular fibrocartilage complex (TFCC), trigger finger, ulnar, ulnar nerve syndrome, wounds and injuries—elbow, wounds and injuries—shoulder, wrist, wrist injuries |
| Intervention | AAROM, activities of daily living, adaptation, adaptive equipment, AROM, arthrokinematics, assistive technology, athletic training, back school, biofeedback, body awareness, body mechanics, cognitive behavior therapy, compensation, create, driving adaptations, durable medical equipment, edema control, education, energy conservation, ergonomics, establish, exercise, functional training, hand therapy, home modification, industrial rehabilitation, interventions, job coaching, job modification, job retraining, joint protection, limb reshaping, modify, occupational medicine, occupational therapy, orthotics, physical agent modalities, physical therapy, postural training, preprosthetic and prosthetic training, prevention, problem solving, PROM, promotion, rehabilitation, relaxation techniques, restore, scapulohumeral rhythm, splint, sports medicine, stretching, therapeutic management, therapy, training, treatment, work hardening, work/occupational rehabilitation, work reconditioning/conditioning |
Databases and sites searched included MEDLINE, PsycINFO, CINAHL, Ergonomics Abstracts, and OTseeker. In addition, consolidated information sources, such as the Cochrane Database of Systematic Reviews, were included in the search. These databases contain peer-reviewed summaries of journal articles and provide a system for clinicians and scientists to conduct systematic reviews of selected clinical questions and topics. Moreover, reference lists from articles included in the systematic reviews were examined for potential articles, and selected journals were hand searched to ensure that all appropriate articles were included.
Studies Included
Inclusion and exclusion criteria are critical to the systematic review process because they provide the structure for the quality, type, and years of publication of the literature that is incorporated into a review. This review was limited to peer-reviewed scientific literature published in English between May 2006 and July 2014. The intervention approaches examined were within the scope of practice of occupational therapy. Studies were included if the outcome measures included pain assessment or patient-centered questionnaires measuring function. The literature included in this review included study participants with musculoskeletal disorders of the shoulder. The review excluded data from presentations, conference proceedings, non–peer-reviewed research literature, dissertations, and theses. Studies included in the review are Levels I, II, and III evidence.
The search resulted in 5,139 references addressing the focused question. The consultant to the EBP Project completed the first step of eliminating references on the basis of citation and abstract. In collaboration with a review author for the forearm, hand, and wrist, the results were then subdivided by body region. This systematic review of articles pertaining to the shoulder was carried out by an individual reviewer (Tambra L. Marik), who completed the next step of eliminating references on the basis of citations and abstracts. The second author (Shawn C. Roll) was consulted when needed to determine whether articles met the inclusion criteria. The full-text versions of potential articles were retrieved, and the reviewer determined final inclusion in the review on the basis of predetermined inclusion and exclusion criteria.
Analysis
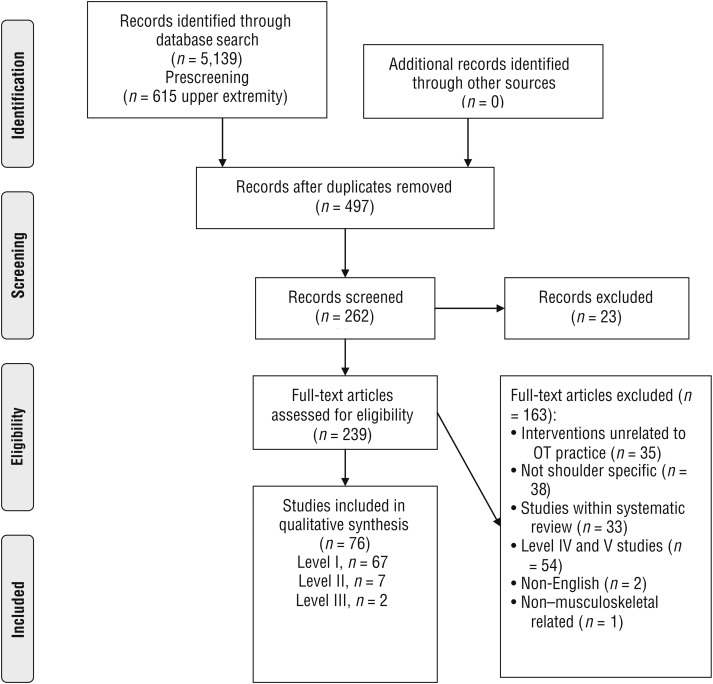
A total of 76 articles were included in the final review for shoulder disorders: 67 Level I studies, 7 Level II studies, and 2 Level III studies (Figure 1). The articles were reviewed according to their quality (scientific rigor and lack of bias) and levels of evidence. Each article included in the review was then abstracted using an evidence table that provides a summary of the methods and findings of each article. AOTA staff and the EBP Project consultant reviewed the evidence table (Supplemental Table 1, online) to ensure quality control. The method for assessing the risk of bias of systematic reviews (Supplemental Table 2, online) was based on the measurement tool developed by Shea et al. (2007). The risk of bias of individual studies (Supplemental Table 3, online) was assessed using the methods described by Higgins and colleagues (2011).
Figure 1.
Flow diagram for studies included in the systematic review.
Note. OT = occupational therapy. Format from “Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement,” by D. Moher, A. Liberati, J. Tetzlaff, and D. G. Altman; The PRISMA Group, 2009, PLoS Medicine, 6(6), e1000097. https://doi.org/10.1371/journal.pmed.1000097
Results
The majority of studies in this review used a systematic review or a randomized controlled trial (RCT) design. The most common risks of bias in the systematic reviews were an unclear description of how conflicts of interest were addressed, inclusion of lower level studies (Level III), and lack of statistical testing to combine results for homogeneity. The most common risks of bias in the RCTs were lack of proper allocation techniques and lack of blinding of outcome assessors and participants. Blinding of participants usually was not possible because participants were physically involved with their rehabilitation. In addition, many of the RCTs had no long-term follow-up. Details on risk of bias for all studies can be found in Supplemental Tables 2 and 3.
The 76 articles were grouped into six categories of studies examining the effectiveness of interventions addressing (1) bone (humeral) fractures, (2) joint disorders resulting in adhesive capsulitis and stiffness, (3) neck and shoulder pain, (4) pain specific to the shoulder (general shoulder pain), (5) rotator cuff tears, and (6) subacromial impingement syndrome (SIS).
Effectiveness of Interventions for Fractures
Two systematic reviews provided strong evidence that supported range of motion (ROM) exercises with the wearing of an immobilization sling for nondisplaced humeral fractures (Bruder, Taylor, Dodd, & Shields, 2011; Handoll, Ollivere, & Rollins, 2012). The evidence regarding the type of sling (Gilchrist vs. Desault) was inconclusive (Handoll et al., 2012). In addition, the evidence regarding the benefits of a home exercise program versus a supervised therapy exercise program was inconclusive (Bruder et al., 2011).
Effectiveness of Interventions for Adhesive Capsulitis
Eight Level I studies and 3 Level II studies concerned interventions for adhesive capsulitis. Three Level 1 studies (Blanchard, Barr, & Cerisola, 2010; Favejee, Huisstede, & Koes, 2011; Maund et al., 2012) provided strong evidence supporting ROM exercises and joint mobilization interventions combined with steroid injections for decreased pain and improved functional outcome scores. The evidence for cryotherapy (Ma, Je, Jeong, Kim, & Kim, 2013), laser therapy, and electrotherapy (Favejee et al., 2011) was limited. It is difficult to reach a conclusion concerning the efficacy of physical modalities in participants with adhesive capsulitis because studies used multiple therapy interventions with their intervention groups. Promising research from 3 Level III studies (Dempsey, Mills, Karsch, & Branch, 2011; Gleyze, Clavert, et al., 2011; Gleyze, Georges, et al., 2011) provides preliminary support for exercises beyond the pain threshold.
Effectiveness of Interventions for Neck and Shoulder Pain
Seven Level I RCTs and 1 Level II nonrandomized cohort study examined the efficacy of interventions to decrease pain and improve function in adults with general neck and shoulder pain. Overall, resistive exercise was supported for short- and long-term increases in function and decreased pain. The evidence from 1 RCT supporting a magnetotherapeutic device (Kanai, Taniguchi, & Okano, 2011) and 1 RCT supporting biofeedback (Ma et al., 2011) was moderate but limited. The evidence was insufficient to support relaxation programs for short-term pain relief (Skoglund, Josephson, Wahlstedt, Lampa, & Norbäck, 2011).
Effectiveness of Interventions for General Shoulder Pain
Five Level I systematic reviews, 5 Level I RCTs, and 1 Level II case-control study were appraised for the outcomes of decreased pain and increased function in participants with general shoulder pain. The majority of the Level I studies provided strong evidence supporting resistive exercise. Three Level I studies provided strong evidence (Brudvig, Kulkarni, & Shah, 2011; Ho, Sole, & Munn, 2009; Yiasemides, Halaki, Cathers, & Ginn, 2011) supporting the addition of manual techniques with resistive exercise programs. The evidence to support specific exercise programming was inconclusive, but there was limited evidence to support high-dosage exercise programming (Marinko, Chacko, Dalton, & Chacko, 2011). The evidence to support ultrasound for pain reduction in participants with shoulder pain related to calcific tendinitis was limited (Alexander, Gilman, Brown, Brown, & Houghton, 2010).
Effectiveness of Interventions for Rotator Cuff Tears
Moderate evidence for progressive strengthening exercises, ROM, and joint mobilizations was provided by 2 Level I systematic reviews (Ainsworth & Lewis, 2007; Seida et al., 2010) and 1 Level III (Baydar et al., 2009) study for conservative management of rotator cuff tears. One Level I systematic review (Seida et al., 2010) provided strong evidence to support rehabilitation interventions for postsurgical rotator cuff tears that include progressive tendon forces and standard rehabilitation programs. The evidence from 2 Level I studies (Du Plessis et al., 2011; Seida et al., 2010) and 1 Level II study (Brady, Redfern, Macdougal, & Williams, 2008) was inconclusive for other specific postsurgical rehabilitation programs that include continuous passive motion, supervised versus unsupervised therapy, land- versus aquatic-based therapy, and video-based versus therapist-guided programs. Two Level I RCTs (Düzgün, Baltacı, & Atay, 2011; Keener, Galatz, Stobbs-Cucchi, Patton, & Yamaguchi, 2014) provided mixed evidence regarding the efficacy of long-term outcomes from accelerated therapy progressions versus slow progression in postsurgical rotator cuff tears.
Effectiveness of Interventions for Subacromial Impingement Syndrome
Eight Level I systematic reviews, 1 of which included a meta-analysis of outcomes (Hanratty et al., 2012), and 26 Level I RCTs evaluated the effects of interventions for SIS. The majority of these studies provided strong evidence regarding short- and long-term outcomes of exercise activities for people with SIS (Hanratty et al., 2012; Kelly, Wrightson, & Meads, 2010; Kromer, de Bie, & Bastiaenen, 2013; Kuhn, 2009). Studies comparing the evidence for exercise versus arthroscopic surgery provided mixed evidence regarding the impact on long-term functional outcomes (Dorrestijn, Stevens, Winters, van der Meer, & Diercks, 2009; Hanratty et al., 2012; Littlewood, Ashton, Chance-Larsen, May, & Sturrock, 2012). However, the use of exercise therapy after arthroscopic surgery to reduce pain and improve function was strongly supported in both systematic reviews (Dorrestijn et al., 2009; Kelly et al., 2010; Kromer, Tautenhahn, de Bie, Staal, & Bastiaenen, 2009; Kuhn, 2009) and individual RCTs (Holmgren, Öberg, Sjöberg, & Johansson, 2012; Hultenheim Klintberg, Gunnarsson, Styf, & Karlsson, 2008).
Many articles investigated exercises combined with one or more additional interventions, which made it difficult to determine whether outcomes were related to a specific intervention or a combination of interventions. However, the evidence for all combinations supported improvements in pain and functional outcomes. These interventions included exercise combined with (1) physical modalities such as laser (Kromer et al., 2009) and electrotherapy (Nyberg, Jonsson, & Sundelin, 2010), (2) neuromuscular reeducation (Nakra, Quddus, Khan, Kumar & Meena, 2013); (3) steroid injections (Crawshaw et al., 2010; Jowett et al., 2013), and (4) joint mobilizations (Beaudreuil et al., 2011; Bennell et al., 2010; Białoszewski & Zaborowski, 2011; Kromer et al., 2013;Trampas & Kitsios, 2006).
In addition to exercise, mixed evidence exists for various other therapeutic interventions. Multiple studies supported the use of laser treatment for short-term pain reduction (Abrisham et al., 2011; Eslamian, Shakouri, Ghojazadeh, Nobari, & Eftekharsadat, 2012; Otadi, Hadian, Olyaei, & Jalaie, 2012). Two RCTs provided limited evidence to support the use of radial shock-wave therapy for improved functional outcomes (Cacchio et al., 2006; Galasso, Amelio, Riccelli, & Gasparini, 2012). The use of elastic taping for short-term pain relief was moderately supported by 3 RCTs (Djordjevic, Vukicevic, Katunac, & Jovic, 2012; Şimşeck, Balki, Keklik, Öztürk, & Elden, 2013; Thelen, Dauber, & Stoneman, 2008).
Discussion
The purpose of this systematic review was to establish the evidence for the effectiveness of interventions within the scope of occupational therapy practice to increase function and decrease pain in people with musculoskeletal shoulder conditions. Although the previous systematic review (von der Hyde, 2011) found only limited evidence of effectiveness, this review found strong evidence from Level I studies supporting a wide spectrum of interventions depending on the type of shoulder disorder. Reasons for the differences in findings are twofold: (1) The previous review was limited to work-related shoulder conditions, whereas this review included any musculoskeletal shoulder condition in the adult population, and (2) this review included a large number of Level I studies published from May 2006 through July 2014 that evaluated these conditions, resulting in a significantly larger evidence base on which to base final conclusions.
The current body of evidence suggests that several preparatory occupational therapy interventions can improve function and decrease pain in people with musculoskeletal shoulder disorders, with strongest evidence for exercise interventions. Findings of this review support the following occupational therapy interventions for specific conditions of the shoulder:
A combination of exercise (ROM and stretching), joint mobilizations, cryotherapy, and electrotherapy for people with adhesive capsulitis
Early controlled ROM therapy with short-term sling wear for nondisplaced proximal humeral fractures
Graded resistive training specifically of the neck and shoulder region in people with combined neck and shoulder pain
A combination of stretching, strengthening exercises, and joint mobilization techniques for people with general shoulder pain
Exercise (ROM, stretching, and strengthening), neuromuscular reeducation, and joint mobilizations for people with SIS, although steroid injections may provide some additional benefit for pain reduction
A combination of ROM exercises, joint mobilizations, and progressive tendon force exercises of the rotator cuff after rotator cuff repair.
This review contributes to the body of occupational therapy research by providing a qualitative synthesis of the evidence-based interventions for musculoskeletal disorders of the shoulder. Although the strongest evidence is for varying forms of exercise, a gap in the literature exists with respect to specific exercise dosage and specific exercise prescription. Another gap in the literature relevant to occupational therapy is the efficacy of occupation-based interventions combined with traditional preparatory interventions for treatment of orthopedic conditions. Occupation-based interventions incorporate meaningful functional activities identified by the client. An emerging body of research (Bachman, 2016; Jack & Estes, 2010; Powell & von der Heyde, 2014) has supported occupation-based interventions for improved patient outcomes. Occupation-based interventions benefit clients by facilitating functional activities and meaningful therapeutic experiences and providing a holistic approach to therapy (Colaianni & Provident, 2010). Future high-quality research is needed to study the outcomes of combining preparatory activities with occupation-based activities.
Limitations of the studies in this review include lack of appropriate methods to combine the findings of studies, lack of graphic aids or statistical tests in reporting outcomes, and no clear conflict-of-interest statements in some of the systematic reviews. Limitations of the RCTs include lack of proper allocation techniques and lack of blinding of outcome assessors and participants. We also acknowledge that the final stages of this review were conducted by a single reviewer, which could increase the risk of bias. In an attempt to minimize bias by the reviewer, each study was extensively reviewed and considered, and the AOTA EBP Project staff and the AOTA review author for the hand, wrist, and forearm were consulted for second opinions when any decision regarding inclusion of individual articles was unclear. Another limitation of this review is the lack of economic analysis with respect to daily practice. Future studies should assess the cost-effectiveness of the different interventions to inform the development of a decision model of treatment.
Implications for Occupational Therapy Practice and Research
The interventions included in this review are primarily classified as preparatory activities by the Occupational Therapy Practice Framework, with a focus on client factors and performance skills (AOTA, 2014). Occupational therapy practitioners providing interventions for orthopedic shoulder conditions can use this review to implement evidence-based preparatory activities that are within the scope of occupational therapy. A need exists to expand the evidence supporting additional occupation-based interventions used by occupational therapy practitioners. Specific implications include the following:
Occupational therapy practitioners should incorporate preparatory interventions into daily clinical practice when providing treatment to people with musculoskeletal shoulder disorders to decrease pain and increase function.
Preparatory evidence-based interventions supported in the current body of literature are exercises, mobilization and manual techniques, and physical modalities (laser, electrotherapy, cryotherapy). The evidence for ultrasound and radio shock-wave therapy is moderate.
Further research is required to measure functional outcomes of combined preparatory interventions with occupation-based interventions.
Evidence-based interventions in this review are specific to musculoskeletal shoulder disorders, and specific intervention recommendations vary depending on the shoulder condition.
Supplementary Material
Acknowledgments
Dr. Roll was funded by the National Institutes of Health Rehabilitation Research Career Development Program (Grant K12 HD055929) at the time this article was prepared. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health. We thank Deborah Lieberman and Marian Arbesman of AOTA’s EBP Project for their guidance and support. Preliminary results of this study were presented at the 2015 AOTA Annual Conference & Expo in Nashville, TN.
Footnotes
Indicates studies that were systematically reviewed for this article.
Contributor Information
Tambra L. Marik, Tambra L. Marik, OTD, OTR/L, CHT, is Hand Therapy Elective Track Director, Rocky Mountain University for Health Professions, Provo, UT, and Staff Therapist, ATI Physical Therapy, Tacoma, WA; tambraasht@gmail.com
Shawn C. Roll, Shawn C. Roll, PhD, OTR/L, RMSKS, FAOTA, is Assistant Professor, Mrs. T. H. Chan Division of Occupational Science and Occupational Therapy, University of Southern California, Los Angeles
References
- *.Abdelshafi M. E., Yosry M., Elmulla A. F., Al-Shahawy E. A., Adou Aly M., & Eliewa E. A. (2011). Relief of chronic shoulder pain: A comparative study of three approaches. Middle East Journal of Anaesthesiology, 21, 83–92. [PubMed] [Google Scholar]
- *.Abrisham S. M. J., Kermani-Alghoraishi M., Ghahramani R., Jabbari L., Jomeh H., & Zare M. (2011). Additive effects of low-level laser therapy with exercise on subacromial syndrome: A randomised, double-blind, controlled trial. Clinical Rheumatology, 30, 1341–1346. https://doi.org/10.1007/s10067-011-1757-7 [DOI] [PubMed] [Google Scholar]
- *.Ainsworth R., & Lewis J. S. (2007). Exercise therapy for the conservative management of full thickness tears of the rotator cuff: A systematic review. British Journal of Sports Medicine, 41, 200–210. https://doi.org/10.1136/bjsm.2006.032524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Akyol Y., Ulus Y., Durmus D., Canturk F., Bilgici A., Kuru O., & Bek Y. (2012). Effectiveness of microwave diathermy on pain, functional capacity, muscle strength, quality of life, and depression in patients with subacromial impingement syndrome: A randomized placebo-controlled clinical study. Rheumatology International, 32, 3007–3016. https://doi.org/10.1007/s00296-011-2097-2 [DOI] [PubMed] [Google Scholar]
- *.Alexander L. D., Gilman D. R., Brown D. R., Brown J. L., & Houghton P. E. (2010). Exposure to low amounts of ultrasound energy does not improve soft tissue shoulder pathology: A systematic review. Physical Therapy, 90, 14–25. https://doi.org/10.2522/ptj.20080272 [DOI] [PubMed] [Google Scholar]
- American Occupational Therapy Association. (2007). AOTA’s Centennial Vision and executive summary. American Journal of Occupational Therapy, 61, 613–614. https://doi.org/10.5014/ajot.61.6.613 [DOI] [PubMed] [Google Scholar]
- American Occupational Therapy Association. (2014). Occupational therapy practice framework: Domain and process (3rd ed.). American Journal of Occupational Therapy, 68(Suppl. 1), S1–S48. https://doi.org/10.5014/ajot.2014.682006 [PubMed] [Google Scholar]
- *.Andersen C. H., Andersen L. L., Gram B., Pedersen M. T., Mortensen O. S., Zebis M. K., & Sjøgaard G. (2012). Influence of frequency and duration of strength training for effective management of neck and shoulder pain: A randomised controlled trial. British Journal of Sports Medicine, 46, 1004–1010. https://doi.org/10.1136/bjsports-2011-090813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Andersen L. L., Jørgensen M. B., Blangsted A. K., Pedersen M. T., Hansen E. A., & Sjøgaard G. (2008). A randomized controlled intervention trial to relieve and prevent neck/shoulder pain. Medicine and Science in Sports and Exercise, 40, 983–990. https://doi.org/10.1249/MSS.0b013e3181676640 [DOI] [PubMed] [Google Scholar]
- *.Ang B. O., Monnier A., & Harms-Ringdahl K. (2009). Neck/shoulder exercise for neck pain in Air Force helicopter pilots: A randomized controlled trial. Spine, 34, E544–E551. https://doi.org/10.1097/BRS.0b013e3181aa6870 [DOI] [PubMed] [Google Scholar]
- Bachman S. (2016). Evidence-based approach to treating lateral epicondylitis using the Occupational Adaptation model. American Journal of Occupational Therapy, 70, 7002360010. https://doi.org/10.5014/ajot.2016.016972 [DOI] [PubMed] [Google Scholar]
- *.Bae Y. H., Lee G. C., Shin W. S., Kim T. H., & Lee S. M. (2011). Effect of motor control and strengthening exercises on pain, function, strength and the range of motion of patients with shoulder impingement syndrome. Journal of Physical Therapy Science, 23, 687–692. https://doi.org/10.1589/jpts.23.687 [Google Scholar]
- *.Başkurt Z., Başkurt F., Gelecek N., & Özkan M. H. (2011). The effectiveness of scapular stabilization exercise in the patients with subacromial impingement syndrome. Journal of Back and Musculoskeletal Rehabilitation, 24, 173–179. https://doi.org/10.3233/BMR-2011-0291 [DOI] [PubMed] [Google Scholar]
- *.Baydar M., Akalin E., El O., Gulbahar S., Bircan C., Akgul O., . . . Kizil R. (2009). The efficacy of conservative treatment in patients with full-thickness rotator cuff tears. Rheumatology International, 29, 623–628. https://doi.org/10.1007/s00296-008-0733-2 [DOI] [PubMed] [Google Scholar]
- *.Beaudreuil J., Lasbleiz S., Richette P., Seguin G., Rastel C., Aout M., . . . Orcel P. (2011). Assessment of dynamic humeral centering in shoulder pain with impingement syndrome: A randomised clinical trial. Annals of the Rheumatic Diseases, 70, 1613–1618. https://doi.org/10.1136/ard.2010.14769 [DOI] [PubMed] [Google Scholar]
- *.Bennell K., Wee E., Coburn S., Green S., Harris A., Staples M., . . . Buchbinder R. (2010). Efficacy of standardised manual therapy and home exercise programme for chronic rotator cuff disease: Randomised placebo controlled trial. BMJ, 340, c2756 https://doi.org/10.1136/bmj.c2756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Białoszewski D., & Zaborowski G. (2011). Usefulness of manual therapy in the rehabilitation of patients with chronic rotator cuff injuries: Preliminary report. Ortopedia, Traumatologia, Rehabilitacja, 13, 9–20. https://doi.org/10.5604/15093492.933789 [DOI] [PubMed] [Google Scholar]
- *.Blanchard V., Barr S., & Cerisola F. L. (2010). The effectiveness of corticosteroid injections compared with physiotherapeutic interventions for adhesive capsulitis: A systematic review. Physiotherapy, 96, 95–107. https://doi.org/10.1016/j.physio.2009.09.003 [DOI] [PubMed] [Google Scholar]
- *.Brady B., Redfern J., Macdougal G., & Williams J. (2008). The addition of aquatic therapy to rehabilitation following surgical rotator cuff repair: A feasibility study. Physiotherapy Research International, 13, 153–161. https://doi.org/10.1002/pri.403 [DOI] [PubMed] [Google Scholar]
- Brox J. (2003). Shoulder pain. Best Practice and Research Clinical Rheumatology, 17(1), 33–56. https://doi.org/10.1016/S1521-6942(02)00101-8 [DOI] [PubMed] [Google Scholar]
- *.Bruder A., Taylor N. F., Dodd K. J., & Shields N. (2011). Exercise reduces impairment and improves activity in people after some upper limb fractures: A systematic review. Journal of Physiotherapy, 57, 71–82. https://doi.org/10.1016/S1836-9553(11)70017-0 [DOI] [PubMed] [Google Scholar]
- *.Brudvig T. J., Kulkarni H., & Shah S. (2011). The effect of therapeutic exercise and mobilization on patients with shoulder dysfunction: A systematic review with meta-analysis. Journal of Orthopaedic and Sports Physical Therapy, 41, 734–748. https://doi.org/10.2519/jospt.2011.3440 [DOI] [PubMed] [Google Scholar]
- *.Cacchio A., Paoloni M., Barile A., Don R., de Paulis F., Calvisi V., . . . Spacca G. (2006). Effectiveness of radial shock-wave therapy for calcific tendinitis of the shoulder: Single-blind, randomized clinical study. Physical Therapy, 86, 672–682. [PubMed] [Google Scholar]
- *.Camarinos J., & Marinko L. (2009). Effectiveness of manual physical therapy for painful shoulder conditions: A systematic review. Journal of Manual and Manipulative Therapy, 17, 206–215. https://doi.org/10.1179/106698109791352076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Celik D. (2010). Comparison of the outcomes of two different exercise programs on frozen shoulder. Acta Orthopaedica et Traumatologica Turcica, 44, 285–292. https://doi.org/10.3944/AOTT.2010.2367 [DOI] [PubMed] [Google Scholar]
- Colaianni D., & Provident I. (2010). The benefits of and challenges to the use of occupation in hand therapy. Occupational Therapy in Health Care, 24, 130–146. https://doi.org/10.3109/07380570903349378 [DOI] [PubMed] [Google Scholar]
- *.Crawshaw D. P., Helliwell P. S., Hensor E. M., Hay E. M., Aldous S. J., & Conaghan P. G. (2010). Exercise therapy after corticosteroid injection for moderate to severe shoulder pain: Large pragmatic randomised trial. BMJ, 340, c3037 https://doi.org/10.1136/bmj.c3037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Damian M., & Zalpour C. (2011). Trigger point treatment with radial shock waves in musicians with nonspecific shoulder–neck pain: Data from a special physio outpatient clinic for musicians. Medical Problems of Performing Artists, 26, 211–217. [PubMed] [Google Scholar]
- *.Dempsey A. L., Mills T., Karsch R. M., & Branch T. P. (2011). Maximizing total end range time is safe and effective for the conservative treatment of frozen shoulder patients. American Journal of Physical Medicine and Rehabilitation, 90, 738–745. https://doi.org/10.1097/PHM.0b013e318214ed0d [DOI] [PubMed] [Google Scholar]
- *.Djordjevic O. C., Vukicevic D., Katunac L., & Jovic S. (2012). Mobilization with movement and kinesiotaping compared with a supervised exercise program for painful shoulder: Results of a clinical trial. Journal of Manipulative and Physiological Therapeutics, 35, 454–463. https://doi.org/10.1016/j.jmpt.2012.07.006 [DOI] [PubMed] [Google Scholar]
- *.Dogru H., Basaran S., & Sarpel T. (2008). Effectiveness of therapeutic ultrasound in adhesive capsulitis. Joint Bone Spine, 75, 445–450. https://doi.org/10.1016/j.jbspin.2007.07.016 [DOI] [PubMed] [Google Scholar]
- *.Dorrestijn O., Stevens M., Winters J. C., van der Meer K., & Diercks R. L. (2009). Conservative or surgical treatment for subacromial impingement syndrome? A systematic review. Journal of Shoulder and Elbow Surgery, 18, 652–660. https://doi.org/10.1016/j.jse.2009.01.010 [DOI] [PubMed] [Google Scholar]
- *.Du Plessis M., Eksteen E., Jenneker A., Kriel E., Mentoor C., Stucky T., . . . Morris L. D. (2011). The effectiveness of continuous passive motion on range of motion, pain and muscle strength following rotator cuff repair: A systematic review. Clinical Rehabilitation, 25, 291–302. https://doi.org/10.1177/0269215510380835 [DOI] [PubMed] [Google Scholar]
- *.Düzgün I., Baltacı G., & Atay O. A. (2011). Comparison of slow and accelerated rehabilitation protocol after arthroscopic rotator cuff repair: Pain and functional activity. Acta Orthopaedica et Traumatologica Turcica, 45, 23–33. https://doi.org/10.3944/AOTT.2011.2386 [DOI] [PubMed] [Google Scholar]
- *.Eslamian F., Shakouri S. K., Ghojazadeh M., Nobari O. E., & Eftekharsadat B. (2012). Effects of low-level laser therapy in combination with physiotherapy in the management of rotator cuff tendinitis. Lasers in Medical Science, 27, 951–958. https://doi.org/10.1007/s10103-011-1001-3 [DOI] [PubMed] [Google Scholar]
- *.Favejee M. M., Huisstede B. M. A., & Koes B. W. (2011). Frozen shoulder: The effectiveness of conservative and surgical interventions—Systematic review. British Journal of Sports Medicine, 45, 49–56. https://doi.org/10.1136/bjsm.2010.071431 [DOI] [PubMed] [Google Scholar]
- *.Galasso O., Amelio E., Riccelli D. A., & Gasparini G. (2012). Short-term outcomes of extracorporeal shock wave therapy for the treatment of chronic non-calcific tendinopathy of the supraspinatus: A double-blind, randomized, placebo-controlled trial. BMC Musculoskeletal Disorders, 13, 86 https://doi.org/10.1186/1471-2474-13-86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Gleyze P., Clavert P., Flurin P. H., Laprelle E., Katz D., Toussaint B., . . . Lévigne C.; French Arthroscopy Society. (2011). Management of the stiff shoulder: A prospective multicenter comparative study of the six main techniques in use: 235 cases. Orthopaedics and Traumatology: Surgery and Research, 97(Suppl.), S167–S181. https://doi.org/10.1016/j.otsr.2011.09.004 [DOI] [PubMed] [Google Scholar]
- *.Gleyze P., Georges T., Flurin P. H., Laprelle E., Katz D., Clavert P., . . . Lévigne C.; French Arthroscopy Society. (2011). Comparison and critical evaluation of rehabilitation and home-based exercises for treating shoulder stiffness: Prospective, multicenter study with 148 cases. Orthopaedics and Traumatology: Surgery and Research, 97(Suppl.), S182–S194. https://doi.org/10.1016/j.otsr.2011.09.005 [DOI] [PubMed] [Google Scholar]
- *.Hains G., Descarreaux M., & Hains F. (2010). Chronic shoulder pain of myofascial origin: A randomized clinical trial using ischemic compression therapy. Journal of Manipulative and Physiological Therapeutics, 33, 362–369. https://doi.org/10.1016/j.jmpt.2010.05.003 [DOI] [PubMed] [Google Scholar]
- *.Handoll H. H., Ollivere B. J., & Rollins K. E. (2012). Interventions for treating proximal humeral fractures in adults. Cochrane Database of Systematic Reviews, 2012, CD000434 https://doi.org/10.1002/14651858.CD000434.pub3 [DOI] [PubMed] [Google Scholar]
- *.Hanratty C. E., McVeigh J. G., Kerr D. P., Basford J. R., Finch M. B., Pendleton A., & Sim J. (2012). The effectiveness of physiotherapy exercises in subacromial impingement syndrome: A systematic review and meta-analysis. Seminars in Arthritis and Rheumatism, 42, 297–316. https://doi.org/10.1016/j.semarthrit.2012.03.015 [DOI] [PubMed] [Google Scholar]
- Hermoso F. E., & Calvo E. (2009). Shoulder pain in the elderly. Aging Health, 5, 711–718. https://doi.org/10.2217/ahe.09.48 [Google Scholar]
- Higgins J. P., Altman D. G., Gøtzsche P. C., Jüni P., Moher D., Oxman A. D., . . . Sterne J. A.; Cochrane Bias Methods Group; Cochrane Statistical Methods Group. (2011). The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ, 343, d5928 https://doi.org/10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Ho C. Y. C., Sole G., & Munn J. (2009). The effectiveness of manual therapy in the management of musculoskeletal disorders of the shoulder: A systematic review. Manual Therapy, 14, 463–474. https://doi.org/10.1016/j.math.2009.03.008 [DOI] [PubMed] [Google Scholar]
- *.Holmgren T., Öberg B., Sjöberg I., & Johansson K. (2012). Supervised strengthening exercises versus home-based movement exercises after arthroscopic acromioplasty: A randomized clinical trial. Journal of Rehabilitation Medicine, 44, 12–18. https://doi.org/10.2340/16501977-0889 [DOI] [PubMed] [Google Scholar]
- *.Hultenheim Klintberg I., Gunnarsson A. C., Styf J., & Karlsson J. (2008). Early activation or a more protective regime after arthroscopic subacromial decompression—A description of clinical changes with two different physiotherapy treatment protocols—A prospective, randomized pilot study with a two-year follow-up. Clinical Rehabilitation, 22, 951–965. https://doi.org/10.1177/0269215508090771 [DOI] [PubMed] [Google Scholar]
- *.Ibrahim M. I., Johnson A. J., Pivec R., Issa K., Naziri Q., Kapadia B. H., & Mont M. A. (2012). Treatment of adhesive capsulitis of the shoulder with a static progressive stretch device: A prospective, randomized study. Journal of Long-Term Effects of Medical Implants, 22, 281–291. https://doi.org/10.1615/JLongTermEffMedImplants.2013007061 [DOI] [PubMed] [Google Scholar]
- Jack J., & Estes R. I. (2010). Documenting progress: Hand therapy treatment shift from biomechanical to Occupational Adaptation. American Journal of Occupational Therapy, 64, 82–87. https://doi.org/10.5014/ajot.64.1.82 [DOI] [PubMed] [Google Scholar]
- *.Jowett S., Crawshaw D. P., Helliwell P. S., Hensor E. M., Hay E. M., & Conaghan P. G. (2013). Cost-effectiveness of exercise therapy after corticosteroid injection for moderate to severe shoulder pain due to subacromial impingement syndrome: A trial-based analysis. Rheumatology, 52, 1485–1491. https://doi.org/10.1093/rheumatology/ket149 [DOI] [PubMed] [Google Scholar]
- *.Kanai S., Taniguchi N., & Okano H. (2011). Effect of magnetotherapeutic device on pain associated with neck and shoulder stiffness. Alternative Therapies in Health and Medicine, 17, 44–48. [PubMed] [Google Scholar]
- *.Kassolik K., Andrzejewski W., Brzozowski M., Wilk I., Górecka-Midura L., Ostrowska B., . . . Kurpas D. (2013). Comparison of massage based on the tensegrity principle and classic massage in treating chronic shoulder pain. Journal of Manipulative and Physiological Therapeutics, 36, 418–427. https://doi.org/10.1016/j.jmpt.2013.06.004 [DOI] [PubMed] [Google Scholar]
- *.Kaya E., Zinnuroglu M., & Tugcu I. (2011). Kinesio taping compared to physical therapy modalities for the treatment of shoulder impingement syndrome. Clinical Rheumatology, 30, 201–207. https://doi.org/10.1007/s10067-010-1475-6 [DOI] [PubMed] [Google Scholar]
- *.Keener J. D., Galatz L. M., Stobbs-Cucchi G., Patton R., & Yamaguchi K. (2014). Rehabilitation following arthroscopic rotator cuff repair: A prospective randomized trial of immobilization compared with early motion. Journal of Bone and Joint Surgery, 96, 11–19. https://doi.org/10.2106/JBJS.M.00034 [DOI] [PubMed] [Google Scholar]
- *.Kelly S. M., Wrightson P. A., & Meads C. A. (2010). Clinical outcomes of exercise in the management of subacromial impingement syndrome: A systematic review. Clinical Rehabilitation, 24, 99–109. https://doi.org/10.1177/0269215509342336 [DOI] [PubMed] [Google Scholar]
- *.Krischak G., Gebhard F., Reichel H., Friemert B., Schneider F., Fisser C., . . . Kraus M. (2013). A prospective randomized controlled trial comparing occupational therapy with home-based exercises in conservative treatment of rotator cuff tears. Journal of Shoulder and Elbow Surgery, 22, 1173–1179. https://doi.org/10.1016/j.jse.2013.01.008 [DOI] [PubMed] [Google Scholar]
- *.Kromer T. O., de Bie R. A., & Bastiaenen C. H. (2013). Physiotherapy in patients with clinical signs of shoulder impingement syndrome: A randomized controlled trial. Journal of Rehabilitation Medicine, 45, 488–497. https://doi.org/10.2340/16501977-1142 [DOI] [PubMed] [Google Scholar]
- *.Kromer T. O., Tautenhahn U. G., de Bie R. A., Staal J. B., & Bastiaenen C. H. (2009). Effects of physiotherapy in patients with shoulder impingement syndrome: A systematic review of the literature. Journal of Rehabilitation Medicine, 41, 870–880. https://doi.org/10.2340/16501977-0453 [DOI] [PubMed] [Google Scholar]
- *.Kuhn J. E. (2009). Exercise in the treatment of rotator cuff impingement: A systematic review and a synthesized evidence-based rehabilitation protocol. Journal of Shoulder and Elbow Surgery, 18, 138–160. https://doi.org/10.1016/j.jse.2008.06.004 [DOI] [PubMed] [Google Scholar]
- *.Lange B., Toft P., Myburgh C., & Sjøgaard G. (2013). Effect of targeted strength, endurance, and coordination exercise on neck and shoulder pain among fighter pilots: A randomized-controlled trial. Clinical Journal of Pain, 29, 50–59. https://doi.org/10.1097/AJP.0b013e3182478678 [DOI] [PubMed] [Google Scholar]
- Lieberman D., & Scheer J. (2002). AOTA’s Evidence-Based Literature Review Project: An overview. American Journal of Occupational Therapy, 56, 344–349. https://doi.org/10.5014/ajot.56.3.344 [DOI] [PubMed] [Google Scholar]
- *.Littlewood C., Ashton J., Chance-Larsen K., May S., & Sturrock B. (2012). Exercise for rotator cuff tendinopathy: A systematic review. Physiotherapy, 98, 101–109. https://doi.org/10.1016/j.physio.2011.08.002 [DOI] [PubMed] [Google Scholar]
- *.Ma C., Szeto G. P., Yan T., Wu S., Lin C., & Li L. (2011). Comparing biofeedback with active exercise and passive treatment for the management of work-related neck and shoulder pain: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation, 92, 849–858. https://doi.org/10.1016/j.apmr.2010.12.037 [DOI] [PubMed] [Google Scholar]
- *.Ma S. Y., Je H. D., Jeong J. H., Kim H. Y., & Kim H. D. (2013). Effects of whole-body cryotherapy in the management of adhesive capsulitis of the shoulder. Archives of Physical Medicine and Rehabilitation, 94, 9–16. https://doi.org/10.1016/j.apmr.2012.07.013 [DOI] [PubMed] [Google Scholar]
- *.Maenhout A. G., Mahieu N. N., De Muynck M., De Wilde L. F., & Cools A. M. (2013). Does adding heavy load eccentric training to rehabilitation of patients with unilateral subacromial impingement result in better outcome? A randomized, clinical trial. Knee Surgery, Sports Traumatology, Arthroscopy, 21, 1158–1167. https://doi.org/10.1007/s00167-012-2012-8 [DOI] [PubMed] [Google Scholar]
- *.Marinko L. N., Chacko J. M., Dalton D., & Chacko C. C. (2011). The effectiveness of therapeutic exercise for painful shoulder conditions: A meta-analysis. Journal of Shoulder and Elbow Surgery, 20, 1351–1359. https://doi.org/10.1016/j.jse.2011.05.013 [DOI] [PubMed] [Google Scholar]
- *.Martins L. V., & Marziale M. H. (2012). Assessment of proprioceptive exercises in the treatment of rotator cuff disorders in nursing professionals: A randomized controlled clinical trial. Brazilian Journal of Physical Therapy, 16, 502–509. https://doi.org/10.1590/S1413-35552012005000057 [DOI] [PubMed] [Google Scholar]
- *.Maund E., Craig D., Suekarran S., Neilson A., Wright K., Brealey S., . . . McDaid C. (2012). Management of frozen shoulder: A systematic review and cost-effectiveness analysis. Health Technology Assessment, 16, 1–264. https://doi.org/10.3310/hta16110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., & Altman D. G.;. The PRISMA Group. (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA statement. PLoS Medicine, 6(6), e1000097 https://doi.org/10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Montes-Molina R., Martínez-Rodríguez M. E., Rodríguez A. B. R., Martínez-Ruiz F., & Prieto-Baquero A. (2012). Interferential light therapy in the treatment of shoulder tendinopathies: A randomized controlled pilot study. Clinical Rehabilitation, 26, 1114–1122. https://doi.org/10.1177/0269215512445068 [DOI] [PubMed] [Google Scholar]
- *.Nakra N., Quddus N., Khan S., Kumar S., & Meena R. (2013). Efficacy of proprioceptive neuromuscular facilitation on shoulder function in secondary impingement. International Journal of Therapy and Rehabilitation, 20, 450–458. https://doi.org/10.12968/ijtr.2013.20.9.450 [Google Scholar]
- *.Nyberg A., Jonsson P., & Sundelin G. (2010). Limited scientific evidence supports the use of conservative treatment interventions for pain and function in patients with subacromial impingement syndrome: Randomized control trials. Physical Therapy Review, 15, 436–452. https://doi.org/10.1179/1743288X10Y.0000000016 [Google Scholar]
- *.Østerås H., Torstensen T. A., & Østerås B. (2010). High-dosage medical exercise therapy in patients with long-term subacromial shoulder pain: A randomized controlled trial. Physiotherapy Research International, 15, 232–242. https://doi.org/10.1002/pri.468 [DOI] [PubMed] [Google Scholar]
- Ostör A. J., Richards C. A., Prevost A. T., Speed C. A., & Hazleman B. L. (2005). Diagnosis and relation to general health of shoulder disorders presenting to primary care. Rheumatology, 44, 800–805. https://doi.org/10.1093/rheumatology/keh598 [DOI] [PubMed] [Google Scholar]
- *.Otadi K., Hadian M. R., Olyaei G., & Jalaie S. (2012). The beneficial effects of adding low level laser to ultrasound and exercise in Iranian women with shoulder tendonitis: A randomized clinical trial. Journal of Back and Musculoskeletal Rehabilitation, 25, 13–19. https://doi.org/10.3233/BMR-2012-0305 [DOI] [PubMed] [Google Scholar]
- Powell R. K., & von der Heyde R. L. (2014). The inclusion of activities of daily living in flexor tendon rehabilitation: A survey. Journal of Hand Therapy, 27, 23–29. https://doi.org/10.1016/j.jht.2013.09.007 [DOI] [PubMed] [Google Scholar]
- *.Seida J. C., LeBlanc C., Schouten J. R., Mousavi S. S., Hartling L., Vandermeer B., . . . Sheps D. M. (2010). Systematic review: Nonoperative and operative treatments for rotator cuff tears. Annals of Internal Medicine, 153, 246–255. https://doi.org/10.7326/0003-4819-153-4-201008170-00263 [DOI] [PubMed] [Google Scholar]
- Shea B. J., Grimshaw J. M., Wells G. A., Boers M., Andersson N., Hamel C., . . . Bouter L. M. (2007). Development of AMSTAR: A measurement tool to assess the methodological quality of systematic reviews. BMC Medical Research Methodology, 7, 10 https://doi.org/10.1186/1471-2288-7-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Şimşek H. H., Balki S., Keklik S. S., Öztürk H., & Elden H. (2013). Does kinesio taping in addition to exercise therapy improve the outcomes in subacromial impingement syndrome? A randomized, double-blind, controlled clinical trial. Acta Orthopaedica et Traumatologica Turcica, 47, 104–110. https://doi.org/10.3944/AOTT.2013.2782 [DOI] [PubMed] [Google Scholar]
- *.Skoglund L., Josephson M., Wahlstedt K., Lampa E., & Norbäck D. (2011). Qigong training and effects on stress, neck-shoulder pain and life quality in a computerised office environment. Complementary Therapies in Clinical Practice, 17, 54–57. https://doi.org/10.1016/j.ctcp.2010.09.003 [DOI] [PubMed] [Google Scholar]
- *.Struyf F., Nijs J., Mollekens S., Jeurissen I., Truijen S., Mottram S., & Meeusen R. (2013). Scapular-focused treatment in patients with shoulder impingement syndrome: A randomized clinical trial. Clinical Rheumatology, 32, 73–85. https://doi.org/10.1007/s10067-012-2093-2 [DOI] [PubMed] [Google Scholar]
- *.Surenkok O., Aytar A., & Baltaci G. (2009). Acute effects of scapular mobilization in shoulder dysfunction: A double-blind randomized placebo-controlled trial. Journal of Sport Rehabilitation, 18, 493–501. https://doi.org/10.1123/jsr.2013-0120 [DOI] [PubMed] [Google Scholar]
- *.Taskaynatan M. A., Ozgul A., Ozdemir A., Tan A. K., & Kalyon T. A. (2007). Effects of steroid iontophoresis and electrotherapy on bicipital tendonitis. Journal of Musculoskeletal Pain, 15, 47–54. https://doi.org/10.1300/J094v15n04_06 [Google Scholar]
- *.Thelen M. D., Dauber J. A., & Stoneman P. D. (2008). The clinical efficacy of kinesio tape for shoulder pain: A randomized, double-blinded, clinical trial. Journal of Orthopaedic and Sports Physical Therapy, 38, 389–395. https://doi.org/10.2519/jospt.2008.2791 [DOI] [PubMed] [Google Scholar]
- *.Trampas A., & Kitsios A. (2006). Exercise and manual therapy for the treatment of impingement syndrome of the shoulder: A systematic review. Physical Therapy Review, 11, 125–142. https://doi.org/10.1179/108331906X99065 [Google Scholar]
- U.S. Bureau of Labor Statistics. (2014). Nonfatal occupational injuries and illness requiring days away from work, 2014 (USDL 15-2205) [News release]. Retrieved from http://www.bls.gov/news.release/pdf/osh2.pdf
- von der Hyde R. L. (2011). Occupational therapy interventions for shoulder conditions: A systematic review. American Journal of Occupational Therapy, 65, 16–23. https://doi.org/10.5014/ajot.2011.09184 [DOI] [PubMed] [Google Scholar]
- Walker-Bone K., Palmer K. T., Reading I., Coggon D., & Cooper C. (2004). Prevalence and impact of musculoskeletal disorders of the upper limb in the general population. Arthritis Care and Research, 51, 642–651. https://doi.org/10.1002/art.20535 [DOI] [PubMed] [Google Scholar]
- *.Yang J. L., Chen S. Y., Hsieh C. L., & Lin J. J. (2012). Effects and predictors of shoulder muscle massage for patients with posterior shoulder tightness. BMC Musculoskeletal Disorders, 13, 46 https://doi.org/10.1186/1471-2474-13-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Yang J. L., Jan M. H., Chang C. W., & Lin J. J. (2012). Effectiveness of the end-range mobilization and scapular mobilization approach in a subgroup of subjects with frozen shoulder syndrome: A randomized control trial. Manual Therapy, 17, 47–52. https://doi.org/10.1016/j.math.2011.08.006 [DOI] [PubMed] [Google Scholar]
- *.Yiasemides R., Halaki M., Cathers I., & Ginn K. A. (2011). Does passive mobilization of shoulder region joints provide additional benefit over advice and exercise alone for people who have shoulder pain and minimal movement restriction? A randomized controlled trial. Physical Therapy, 91, 178–189. https://doi.org/10.2522/ptj.20100111 [DOI] [PubMed] [Google Scholar]
- *.Yildirim M. A., Ones K., & Celik E. C. (2013). Comparison of ultrasound therapy of various durations in the treatment of subacromial impingement syndrome. Journal of Physical Therapy Science, 25, 1151–1154. https://doi.org/10.1589/jpts.25.1151 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.